Significance Statement
Health care–associated infections during previous serious coronavirus epidemics resulted from human-to-human transmission in hemodialysis (HD) facilities. The authors analyzed the effect of a strategy of HD with cohort isolation on the secondary transmission of coronavirus disease 2019 (COVID-19) in HD facilities in Korea, which involves administering an immediate screening test for COVID-19 to all close contacts (patients on HD and health care workers) and strict maintenance of cohort isolation. Epidemiologic investigation and immediate screening tests across 11 HD centers identified 302 close contacts. HD with cohort isolation was maintained for a median of 14 days, and the transmission rate was 0.66% inside HD units. Clinical practice guidelines for HD with cohort isolation during COVID-19 outbreaks may successfully prevent secondary transmission through HD units.
Keywords: coronavirus, hemodialysis units, end-stage renal disease, quarantine, cohort isolation, COVID-19
Abstract
Background
Health care–associated infections during previous coronavirus epidemics involving severe acute respiratory syndrome and Middle East respiratory syndrome resulted from human-to-human transmission in hemodialysis (HD) facilities. The effect of a strategy of HD with cohort isolation—separate dialysis sessions for close contacts of patients with confirmed coronavirus disease 2019 (COVID-19)—on the prevention of secondary transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in HD units is unknown.
Methods
Our multicenter cohort study of an HD with cohort isolation strategy enrolled close contacts of patients with confirmed COVID-19, including patients on HD and health care workers in HD units. Close contacts had been identified by epidemiologic investigation and tested negative on an immediate screening test for SARS-CoV-2.
Results
As of March 14, 11 patients on HD and 7 health care workers from 11 HD centers were diagnosed as having COVID-19. The immediate screening test was performed in 306 people, and among them, 302 close contacts with negative test results were enrolled. HD with cohort isolation was performed among all close contacts for a median of 14 days in seven centers. During cohort isolation, nine patients showed symptoms but tested negative for SARS-CoV-2. Two health care workers in the HD units (0.66% of the total group) were diagnosed at the termination test for SARS-CoV-2.
Conclusions
The transmission of COVID-19 can be controlled without closure of HD centers by implementing preemptive activities, including early detection with rapid testing, cohort isolation, collaboration between institutions, and continuous monitoring of infection. Our strategy and experience may provide helpful guidance for circumstances involving the rapid spread of infectious diseases such as COVID-19.
The coronavirus disease 2019 (COVID-19) outbreak first occurred in Wuhan, China, in December 2019.1–3 COVID-19 was found to be caused by a novel betacoronavirus, namely severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).4–6 As the outbreak has spread worldwide, the World Health Organization declared COVID-19 the second pandemic of the 21st century on March 11, 2020.7 As of March 14, 142,534 cases of COVID-19 and 5392 deaths have been reported in 134 countries.8
The two previous coronavirus epidemics, severe acute respiratory syndrome coronavirus9,10 and Middle East respiratory syndrome coronavirus (MERS-CoV),11,12 led to the occurrence of health care–associated infections as a result of human-to-human transmission in hemodialysis (HD) facilities. HD requires long and close contact in a narrow space, which increases the possibility of spread of infectious diseases. Patients undergoing HD have a higher mortality rate because of an impaired immune response against infection.13,14 Therefore, more attention should be paid to the rapid transmission of infection and high mortality rates among the patients on HD.
One of the main differences of SARS-CoV-2 compared with severe acute respiratory syndrome coronavirus and MERS-CoV is that the former has a higher infectivity rate, which is indicated by its high reproduction rate.15,16 However, how the rapid spread of this infectious disease affects the transmission rate in HD units remains unknown. Fortunately, the Korean Society of Nephrology (KSN) and the Korean Society of Dialysis have had experience with the MERS-CoV outbreak and published clinical practice guidelines for HD facilities.17 Therefore, the KSN was able to respond promptly to COVID-19 when the first patient on dialysis was confirmed as having COVID-19 in Daegu, South Korea. Here, we aimed to determine the effect of HD with cohort isolation on the prevention of secondary transmission of COVID-19 in HD units.
Methods
Joint Committee for HD during the COVID-19 Outbreak
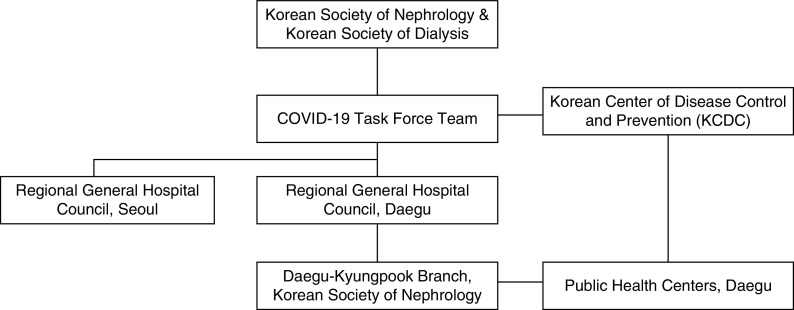
On February 19, 2020, a joint committee for HD was formed when the first patient on HD was diagnosed as having COVID-19 in Daegu. The joint committee included nephrologists and government authorities with the intention to perform collaborative activities for the safety and benefit of patients on HD during the COVID-19 outbreak (Figure 1).
Figure 1.
Organizational chart of the joint committee for patients on HD in the COVID-19 outbreak. A joint committee was established with nephrologists and government authorities to take the collaborative activities for HD patients in COVID-19 outbreak when the first HD patient was diagnosed with COVID-19 in Daegu, Korea.
Nephrologists from the KSN and the Korean Society of Dialysis led the committee and made up the COVID-19 Task Force Team, which headed this collaborative effort. The COVID-19 Task Force Team developed COVID-19 clinical practice guidelines for patients on HD, relayed the policies of the Korean Centers for Disease Control and Prevention (KCDC) to regional nephrologists in Daegu, arranged the transfer of patients outside Daegu, and connected with public health centers in Daegu and HD facilities with confirmed patients. The KCDC prepared policies for the COVID-19 outbreak and counted the number of confirmed cases in South Korea. The Regional General Hospital Council in Daegu managed confirmed patients in a single negative-pressure room with a portable dialysis machine. HD centers in the Daegu-Kyungpook Branch of the KSN received reports of confirmed patients from public health centers in Daegu. The public health centers were responsible for epidemiologic investigation of close contacts and initial disinfection of the HD units.
On February 21, 2020, the joint committee announced the first draft of the COVID-19 clinical practice guidelines for HD facilities, which were on the basis of previous clinical recommendations.17,18 The guidelines aimed to prevent transmission and minimize the spread of COVID-19 and included information on case definitions of COVID-19 and response methods of HD facilities. The Korean clinical practice guidelines for preventing transmission of COVID-19 in HD facilities had been recently released (Table 1).19
Table 1.
COVID-19 clinical practice guideline for HD facilities
| Key Recommendations for Dealing with Patients on HD Associated with COVID-19a |
|---|
| Standard, contact, and droplet precautions should be appropriately performed by all patients and health care workers in HD facilities. The waiting room or resting area should be closed, and surgical masks and hand sanitizers should be available and ready for patients to use before entering the HD unit. |
| All patients should check their body temperature and respiratory symptoms before coming to the HD facilities. If they have a fever ≥37.5°C or respiratory symptoms such as dry cough, sore throat, or shortness of breath, they should not visit the HD unit but notify health care workers in advance before visiting the HD facility. |
| A patient with suspected or confirmed COVID-19 should be transferred to a health care facility with an isolation room and portable dialysis machine. The transportation and management plans should be discussed with the public health center and infection control division of the hospital. |
| Close contacts are defined as the patients on HD and health care workers who have been in contact with the patient with a confirmed case. Close contacts should be monitored for body temperature and presence of respiratory symptoms every day. Close contacts without fever or respiratory symptoms should be subjected to self-quarantine and HD with cohort isolation for 14 d from the last exposure. All transport between home and the HD facility should be provided by the disease prevention authority. |
| Interhospital transfer is basically prohibited during outbreak. If referral to another hospital is inevitable, the attending physician should transfer the patients after careful discussion with regional disease prevention authority and the designated hospital. The patient transfer should be performed only when there is solid evidence that the patient is not infected. |
Extracted from the Korean clinical practice guidelines for preventing transmission of COVID-19 in hemodialysis facilities.19
Data Source
Data on the total number of cases in Korea and the number of cases in Daegu were obtained from the KCDC. Information on the number of confirmed cases associated with HD was obtained from the Regional General Hospitals Council of Daegu and the Daegu-Kyungpook Branch of the KSN. Data regarding close contacts were obtained from the public health centers of Daegu city. Data on patients’ sex, age, recent exposure history, clinical symptoms, and interval from diagnosis to admission were extracted from electronic medical records. The cutoff date of the study was March 14, 2020. This study was reviewed and approved by the institutional review board (institutional review board no. 2020–03–076), and it was conducted in accordance with the Declaration of Helsinki.
Laboratory Confirmation of SARS-CoV-2
Specimens were obtained through nasopharyngeal and oropharyngeal swabs. The specimens were placed in a collection tube with 150 μl of virus preservation solution, and real-time RT-PCR (rRT-PCR) was used to detect SARS-CoV-2. RNA was extracted from the clinical samples using the Allplex 2019-nCoV assay (Seegene, Seoul, South Korea) according to the manufacturer’s protocol. The primer and probe sequences used for RNA-dependent RNA polymerase gene detection were as follows: 5′-GTGARATGGTCATGTGTGGCGG-3′ (forward), 5′-CARATGTTAAASACACTATTAGC ATA-3′ (reverse), and 5′-CAGGTGGAACCTCATCAGGAGATGC-3′ (probe in 5-FAM/3′-BHQ format). Meanwhile, the primer and probe sequences used for E gene detection were as follows: 5′-ACAGGTACGTTAATAGTTAATAGCGT-3′ (forward), 5′-ATATTGCAGCAGTACGCACACA-3′ (reverse), and 5′-ACACTAGCCATCCTTACTGCGCTTCG-3′ (probe in 5-FAM/3′-BHQ format). The primer and probe sequences used for the N gene detection were as follows: 5′-CACATTGGCACCCGCAATC-3′ (forward), 5′-GAGGAACGAGAAGAGGCTTG-3′ (reverse), and 5′-ACTTCCTCAAGGAACAACATTGCCA-3′ (probe in 5-FAM/3′-BHQ format). The cycle threshold (Ct) values of rRT-PCR were converted into RNA copy number of SARS-CoV-2. The RNA copy number was calculated from a standard curve on the basis of the Ct values of plasmid DNA. Each dilution of plasmid DNA was tested in duplicate to produce the standard curve. Samples were considered as negative if the Ct values exceeded 37 cycles. The detection limit of quantitative PCR reaction was 100 copies per microliter. The RNA copy number of SARS-CoV-2 was converted from Ct values of rRT-PCR. The test result was considered positive if the Ct values were <37 cycles, and the limit of detection was −100 copies per microliter.
Classification of Patient and Exposure
Confirmed cases were defined as either patients on HD or health care workers (physicians, nurses, or nonmedical staff) in the HD facility who were confirmed as being infected on the basis of SARS-CoV-2 rRT-PCR results, regardless of the clinical manifestation. Close contact refers to a patient on HD or health care worker who made contact with a confirmed patient inside or outside the HD facility. Contact was defined as a contact with the confirmed patients from the time of onset of their signs or symptoms. Close contacts inside the HD facility were determined by epidemiologic investigation and defined in more detail as one of following: an individual who (1) underwent dialysis at the same time as the confirmed patient, (2) was in close proximity with the confirmed patient at the same time, or (3) had undergone dialysis in the same HD room as the confirmed patient, without proper environmental disinfection after dialysis of the confirmed patient. If the participants tested positive in the immediate screening test and exposures outside the HD facility were identified by epidemiologic investigation, the participants were defined as nonclose contacts.
Confirmed patients on HD were transferred to a hospital with an isolation room and a portable dialysis machine. Confirmed health care workers were admitted to a hospital with an isolation room or COVID-19 care centers, or they practiced home isolation. The Korean government assigned some of the national institutes the responsibility to handle the COVID-19 care centers in order to manage the rapidly increasing number of confirmed patients. Confirmed patients without severe signs or symptoms were admitted to COVID-19 care centers or practiced home isolation. All close contacts were tested for SARS-CoV-2 as soon as possible after identification of confirmed cases.
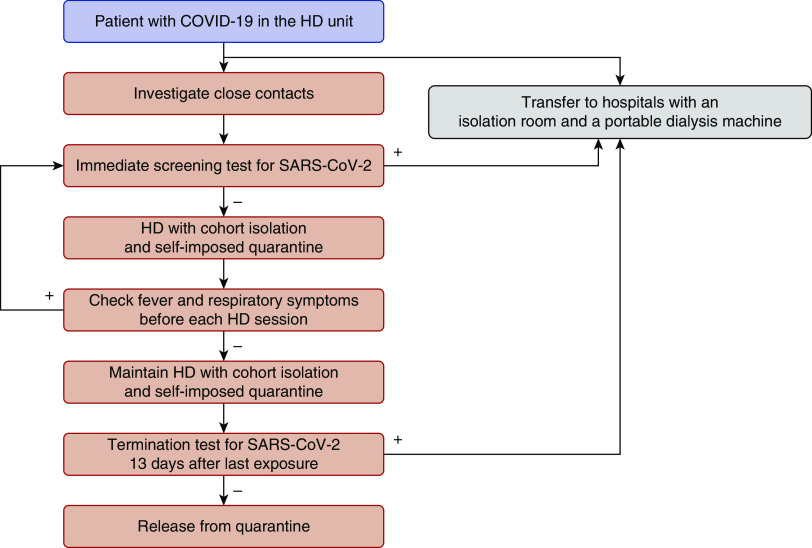
Specific Measure of HD with Cohort Isolation and Definition of Secondary Transmission
HD with cohort isolation was defined as a separate dialysis treatment for close contacts at a different time from HD for other noncontact patients on dialysis. For HD with cohort isolation, it was a prerequisite that close contacts of the confirmed patients be determined through epidemiologic investigation and tested negative for SARS-CoV-2 rRT-PCR. During cohort isolation, the body temperature and respiratory symptoms of all patients on HD and health care workers should be checked before entering the HD unit. If a close contact developed a fever or respiratory symptoms, an immediate test for SARS-CoV-2 was performed before dialysis treatment. Interhospital transfer of patients on HD was prohibited during the period of cohort isolation. Repeat confirmatory tests were performed 13 days after the last exposure to determine whether cohort isolation could be terminated. HD with cohort isolation was discontinued when the close contact showed negative results for the termination test for COVID-19 unless another exposure had occurred. The algorithm for HD with cohort isolation to prevent transmission of COVID-19 in HD facility is depicted in Figure 2.
Figure 2.
Algorithm of HD with cohort isolation to protect transmission of COVID-19 in an HD facility. Close contacts of the confirmed patients were identified by epidemiologic investigation and underwent immediate screening test for SARS-CoV-2. During cohort isolation, test for SARS-CoV-2 was immediately performed to a close contact who developed any symptoms before dialysis. Termination tests for SARS-CoV-2 were performed to determine the termination of cohort isolation.
Health care workers wore personal protective equipment, including N95 masks, gloves, goggles (or face shields), and gowns, to prevent transmission. Hand hygiene was performed before and after every patient contact, and adequate space was maintained between beds. The dialysis machine and HD room were disinfected after every dialysis session.
Secondary transmission was defined on the basis of positive rRT-PCR test results for SARS-CoV-2 within 14 days after the last contact with the confirmed patient in the HD facility. The transmission rate was calculated on the basis of the number of patients who acquired COVID-19 among the total close contacts who tested negative at the immediate screening test.
Statistical Analyses
Data were expressed as the median (range) for continuous variables and number (percentage) for categorical variables. The Mann–Whitney U test was used to analyze continuous variables, whereas the Pearson chi-squared or the Fisher exact test was used to analyze categorical variables. All statistical analyses were performed using SPSS version 25.0 (SPSS, Chicago, IL). P<0.05 was considered significant.
Results
On January 20, 2020, the first patient with COVID-19 was confirmed in South Korea. The daily number of confirmed patients did not exceed ten until February 18, 2020 when the first confirmed patient was reported in Daegu. However, 5 days after the first report, the daily number of confirmed patients in Daegu surged over 100, with associations between particular religious groups. As of March 14, the total number of patients in Daegu reached 5990, which is 74.1% of the 8086 total patients in South Korea (Figure 3).
Figure 3.
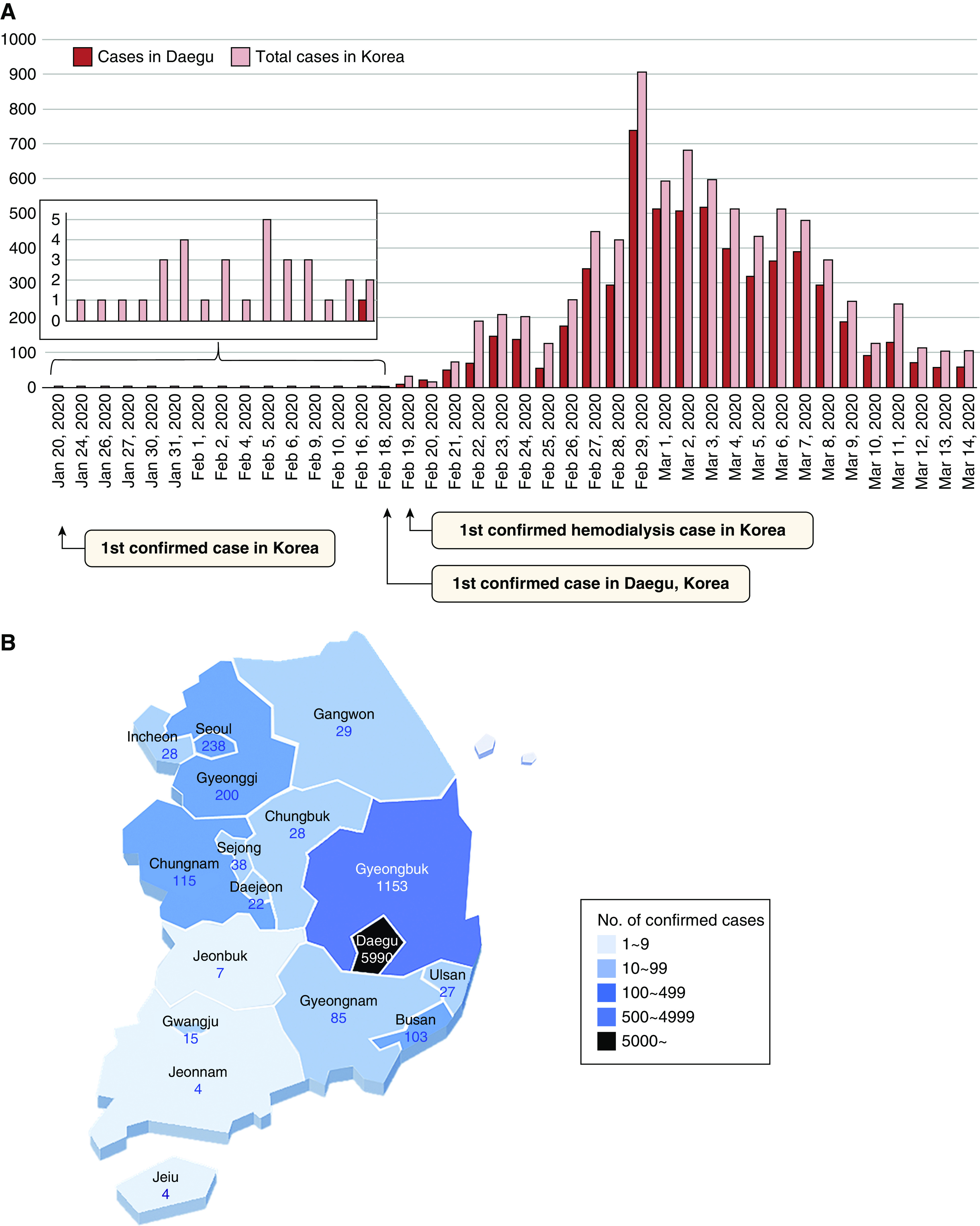
Distribution of laboratory-confirmed cases of COVID-19 in Korea. (A) Daily number of confirmed cases. (B) Regional distribution of confirmed cases.
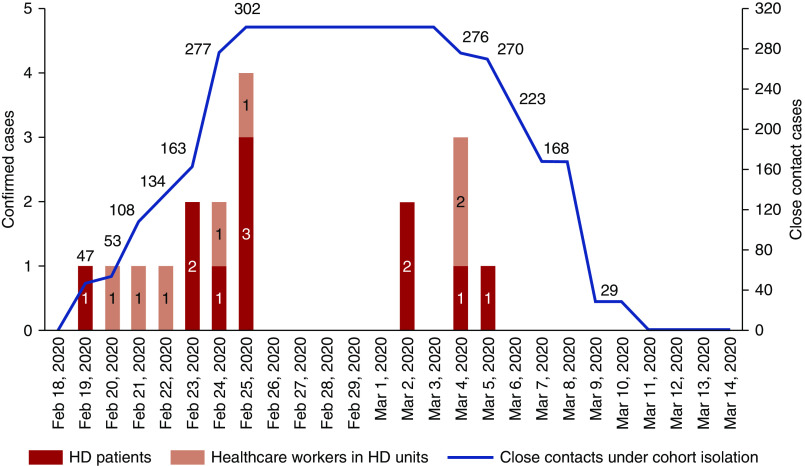
The first patient on HD was confirmed in Daegu on February 19, 2020. As of March 14, 2020, a total of 11 patients on HD and 7 health care workers in 11 HD units were diagnosed as having COVID-19. The total numbers of patients on HD and health care workers in 11 HD units were 1175 and 278, respectively. The incidence rates of confirmed cases in 11 HD units were 0.9% (11 of 1175) among patients on HD and 2.5% (7 of 278) among health care workers. After the first confirmed case, the number of close contacts increased steeply to 302 on February 25 and maintained a plateau until March 3. No additional confirmed cases were reported after March 5 (Figure 4).
Figure 4.
Daily numbers of laboratory-confirmed cases and close contacts under cohort isolation for COVID-19 in Daegu. Confirmed patients on HD are shown with dark red bars. Confirmed health care workers are shown with light red bars. Close contacts under the cohort isolation in HD units are shown with the linear graph.
Table 2 shows the characteristics of confirmed patients in HD units. The patients on HD were significantly older than health care workers. No significant differences were observed in sex, contact history, main signs or symptoms on presentation, interval from onset to diagnosis, and number of close contacts between patients on HD and health care workers. All confirmed participants were isolated immediately after diagnosis. All of the confirmed patients on HD were admitted to six hospitals to undergo isolated portable dialysis 1 (0–2) day after diagnosis. Three confirmed health care workers were admitted in the hospital, three were admitted in the COVID-19 care centers, and one without signs or symptoms practiced home isolation. The interval from diagnosis to admission was longer in health care workers than in patients on HD. This is probably due to the fact that patients without any obvious symptoms were initially placed under home isolation.
Table 2.
Characteristics of confirmed patients
| Characteristics | Total Patients | Patients on HD, n=11 | Health Care Workers, n=7 | P Value |
|---|---|---|---|---|
| Age, yr | 55.5 (24–63) | 57 (29–63) | 37.5 (24–56) | 0.01 |
| Sex | 0.07 | |||
| Men | 8 (44.4%) | 7 (63.6%) | 1 (14.3%) | |
| Women | 10 (55.6%) | 4 (36.4%) | 6 (85.7%) | |
| Source of infection | 0.05 | |||
| Visit to China | 0 | 0 | 0 | |
| Contact of patient | 9 (50%) | 3 (27.3%) | 6 (85.7%) | |
| No obvious history | 9 (50%) | 8 (72.7%) | 1 (14.3%) | |
| Signs or symptoms on presentation | 0.98 | |||
| Fever | 10 (55.6%) | 6 (54.5%) | 4 (57.1%) | |
| URI symptoma | 3 (16.7%) | 2 (18.2%) | 1 (14.3%) | |
| No obvious symptom | 6 (27.8%) | 3 (27.3%) | 2 (28.6%) | |
| Days from onset to diagnosis | 2 (0–6) | 2 (0–6) | 2 (0–5) | 0.93 |
| Days from diagnosis to quarantine | 0 | 0 | 0 | — |
| Patient management | 0.02 | |||
| Admission to hospital | 14 (77.8%) | 11 (100%) | 3 (42.9%) | |
| Admission to COVID-19 care center | 3 (16.7%) | 0 | 3 (42.9%) | |
| Home isolation | 1 (5.6%) | 0 | 1 (14.3%) | |
| Days from diagnosis to admission | 2 (0–14) | 1 (0–2) | 3 (2–14) | 0.002 |
| No. of close contacts in HD unitb | 12.5 (0–115) | 0 (0–115) | 27 (0–55) | 0.54 |
URI, upper respiratory infection.
URI symptom means symptoms of URI without fever.
The number of close contacts in HD units was determined on the basis of the number of first confirmed patients, and data of other confirmed participants within one center were considered as censored data.
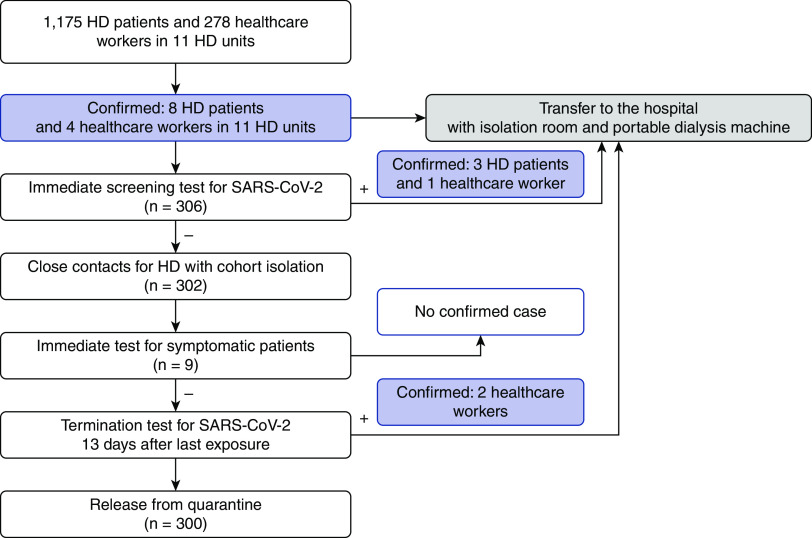
Figure 5 shows the time course of symptoms, diagnosis of COVID-19, and HD with cohort isolation. A total of 306 people were identified and underwent immediate screening tests. With the exception of center C, all immediate screening tests for close contacts were performed within 24 hours after the identification of a confirmed case. Center C performed immediate screening tests over the course of 2 days.
Figure 5.
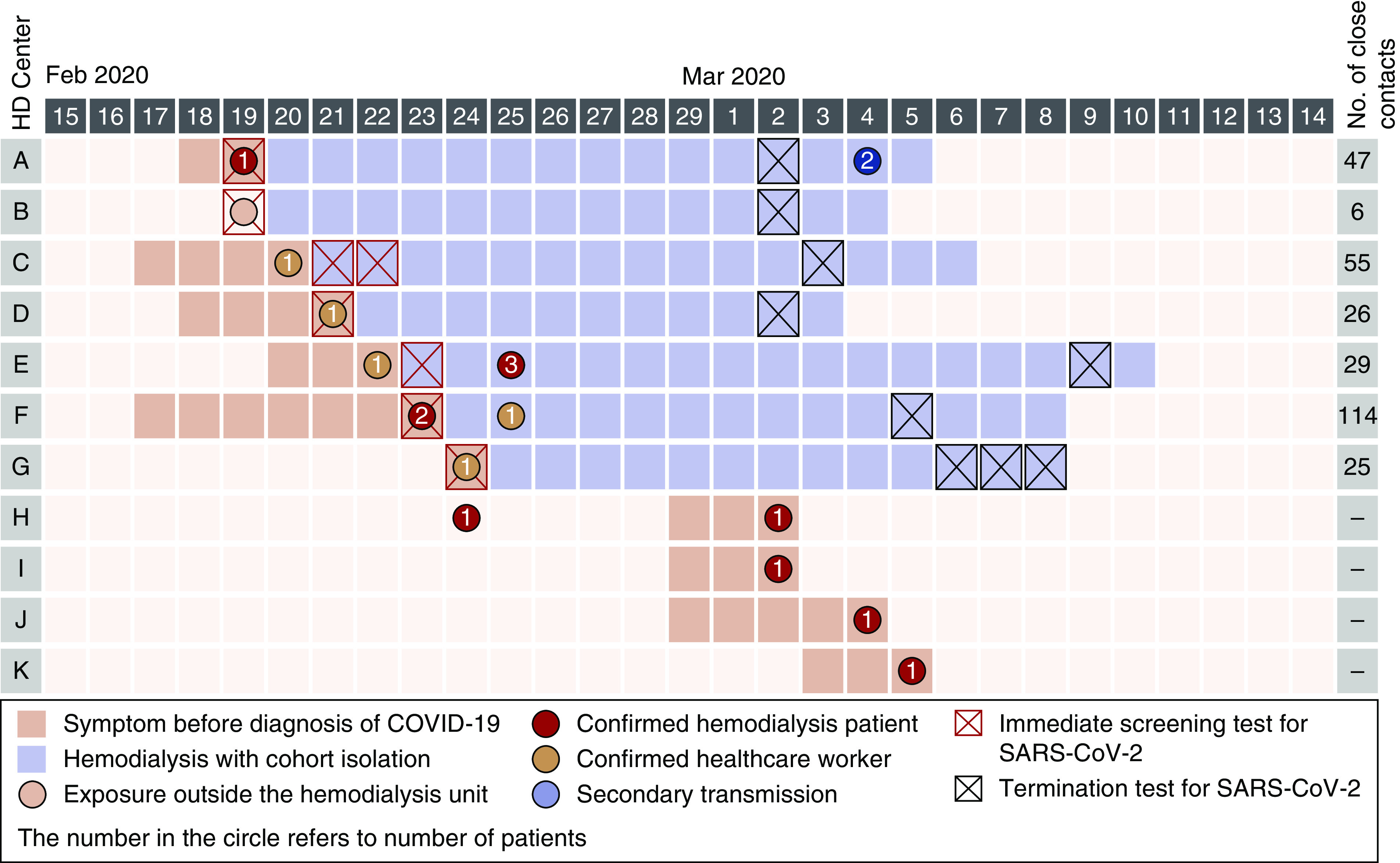
Time course of symptoms, diagnosis of COVID-19, and isolation HD. A total of 207 patients on HD and 95 health care workers were classified as close contacts among 11 HD units during the study period.
Among them, three HD (center E) patients and one nurse (center F) were confirmed as having COVID-19 and classified as nonclose contacts but were identified as having exposures, regardless of HD facility. Among 306 people receiving immediate screening tests, 302 people were recognized as close contacts. All close contacts in center B were exposed to a patient in the emergency room regardless of HD unit. The first confirmed patient on HD of center H was asymptomatic and was not considered as having had any close contacts. HD with cohort isolation was maintained for 14 (11–17) days in seven centers. Since March, no close contact has been reported, even after the diagnosis of confirmed patients because those with fever or respiratory symptoms were prohibited from visiting the HD unit (centers H to K). Epidemiologic investigation revealed that the second confirmed patient on HD of center H was exposed to a patient outside the HD unit.
Figure 6 is a flowchart showing the process of diagnosing patients with COVID-19, HD with cohort isolation, and secondary transmission. Among the 302 close contacts, 9 manifested symptoms but tested negative during the period of cohort isolation. With the exception of G, all termination tests were performed 1 day before the termination of isolation. Center G performed termination tests for 2 days. Two health care workers were diagnosed as having COVID-19 after the termination test (center A in Figure 5). Our study showed a low secondary transmission rate (0.66%) inside HD units after implementation of HD with cohort isolation.
Figure 6.
Flowchart of the process of diagnosing COVID-19, HD with cohort isolation, and secondary transmission. Among the 302 close contacts, nine manifested symptoms, but tested negative. Two healthcare workers were diagnosed as COVID-19 at the termination test.
Discussion
We showed the development in the status of patients with COVID-19 and a concomitant rapid increase in the number of close contacts in HD facilities in Daegu. The joint committee for patients on HD managed COVID-19 through collaborative activities and suggested the clinical practice guidelines for HD with cohort isolation from the early stage of the outbreak. Immediate screening tests for close contacts and strict maintenance of cohort isolation successfully prevented the secondary transmission of COVID-19 in HD facilities.
Previous epidemics of coronavirus gave rise to human-to-human transmission in HD facilities.9,11,12 A recent report from an HD center in Wuhan also showed the emergence of epidemic among patients on dialysis.20 From one confirmed patient on HD, a total of 37 patients on HD and 4 medical staff members were infected with COVID-19, resulting in seven deaths. Because the HD center started to screen all patients and staff 21 days after diagnosis of the first confirmed patient, the report emphasized the importance of preventive measures in the early stage of the epidemic.
As of March 9, 2020, South Korea had the highest number of confirmed cases outside China, and Daegu, a city with 2.4 million people, was the center of the South Korean COVID-19 outbreak.21 The abrupt surge of COVID-19 cases in Daegu was one of the most prominent features in the recent outbreak. In the case of a rapid spread of infectious disease, we were able to evaluate the transmission of COVID-19 and the effect of early cohort isolation on the development of additional confirmed patients among close contacts in HD facilities.
The difference between the current SARS-CoV-2 and MERS-CoV outbreaks is that SARS-CoV-2 has a higher transmissibility but lower pathogenicity than those of MERS-CoV.15,16,22 The basic reproduction number of SARS-CoV-2 ranged from 2.24 to 3.58 in the early phase of the outbreak,23 whereas the basic reproduction number of MERS-CoV was suggested to be <1.24 Patients who undergo HD treatment have an increased risk of acquiring the infection in HD units, where they have to be in regular and close contact with other patients for several hours. Therefore, patients on dialysis need more strict management of transmission than other patient groups. In a mathematical model shown by Hellewell et al.,25 isolation is highly effective in controlling the outbreak of COVID-19, and cohort isolation should be applied to prevent transmission while maintaining accessibility to the dialysis facility.
There are three main purposes of cohort isolation. The most important one is to prevent the transmission of additional diseases. The transmission of infection to patients in other dialysis rooms is preventable by inhibiting the outflow of patients from the cohort of close contacts. Another aim of cohort isolation is the immediate diagnosis and isolation of additional confirmed patients. In cases of symptomatic close contact during the isolation period, an immediate test can be performed to determine the need to transfer a certain patient to an isolation room. Cohort isolation also protects patients on dialysis from exposure to additional sources of infection by preventing the influx of patients outside. The recommended duration of cohort isolation is 14 days because a recent study reported that 97.5% of patients develop symptoms within 11.5 days.26
The essential requirements for the application of this strategy are immediate screening testing for COVID-19 in patients on dialysis and collaborative activities between HD units and health care authorities. Because South Korea performed more tests per million people than any other country,27,28 suspected patients could be confirmed rapidly. If the capacity of the confirmative test is insufficient, patients on dialysis should be prioritized in the testing. In cases where immediate screening test of close contacts is difficult to perform, delayed dialysis, preventive quarantine, and selective testing for symptomatic patients could be suitable alternatives until infection is confirmed. The collaborative activities are also necessary for the transfer of confirmed patients and continuous monitoring of cohorts. The KSN and the Korean Society of Dialysis performed cohort isolation at the time of the MERS-CoV outbreak and published clinical practice guidelines on the basis of the experience.17,29 With this experience and knowledge, we promptly organized the committee and cooperated with the health care authorities. In the event that this type of immediate response is not feasible, local nephrologists could start replaying real-time information to the confirmed patients or implement telemedicine in order to avoid exposure.30 Even in those cases, it is necessary to develop guidelines appropriate to the environment of each country; this will allow countries to prepare for the current outbreak and other pandemics that we may encounter in the future.
In this study, we demonstrated that continuous monitoring of infection could prevent additional close contacts. The majority of patients on dialysis will be checked to determine their body temperature and assess for presence of symptoms before entering the HD units during the COVID-19 outbreak. However, a single visit from an infected patient can cause exposure to health care workers without full protection or HD centers not undergoing cohort isolation. Thus, our guideline suggests that febrile or symptomatic patients on dialysis should notify in advance when they plan to visit their HD center. As shown in our investigation, the preemptive method of “notify first” prevented the contact from confirmed patients in HD centers without cohort isolation, such as in centers H, I, J, and K. This method could be applied to environments where immediate confirmative tests are unavailable if patient cooperation could be achieved through education.
This study has several limitations. First, there was no control group to compare the effect of cohort isolation. However, we manifested a very low secondary transmission rate in HD facilities despite the large number of close contacts. In addition, all dialysis units used the same preventive measures without difficulty under the guidance of the joint committee, which is considered applicable in other HD units. Second, the study duration was relatively short, and some of the close contacts may require longer observations. Considering the exceptional cases of asymptomatic carriers, longer incubation periods, or recurrence,26,31,32 continuous infection control is required in HD units during the epidemic. In addition, this study has a small sample of patients with confirmed disease and contacts. Nevertheless, this study is the first to report the implementation of preemptive collaborative activities for HD with cohort isolation during the COVID-19 epidemic and suggested the effect on secondary transmission in HD facilities.
In conclusion, we demonstrated that the transmission of COVID-19 could be controlled through a preexisting deployment plan before the epidemic, early detection with rapid rRT-PCR testing, collaboration between institutions, and continuous monitoring of infection without closure of HD centers. Our strategy and experience will be helpful, especially in the situation of a rapidly spreading outbreak such as COVID-19.
Disclosures
All authors have nothing to disclose.
Funding
This research was supported by the Korea Health Technology Research and Development Project through Korea Health Industry Development Institute grant HI15C0001 funded by the Ministry of Health & Welfare, Republic of Korea and by the Medical Research Center Program through National Research Foundation of Korea grant 2015R1A5A2009124 funded by Ministry of Science, Information and Communication Technologies, and Future Planning.
Acknowledgments
We express our gratitude to the following nephrology medical staff members for their dedicated efforts during the COVID-19 epidemic: S.H. Lee at Daehan Medical Clinic; C.D. Kim, J.Y. Choi, H.Y. Jung, and J.H. Lim at Kyungpook National University Hospital; E.S. Lee at Yonsei Hospital; Y.J. Kang at Suseong Hospital; K.S. Ahn and I.H. Lee at Daegu Catholic University Hospital; K.D. Hong at Daegu Gyeongsang Hospital; S. Han, W.Y. Park, J.H. Paek, and Y. Kim at Keimyung University Dongsan Hospital; H.C. Kim and E.A. Hwang at Kim’s Renal Clinic; K.H. Cho at Yeungnam University Medical Center; D.K. Cho at Dr. Cho’s Medical Clinic; and S.B. Jeong at Seongdo Medical Clinic.
The sponsors of this study were not involved in the study design or in the collection, analysis, or interpretation of data. They were also not involved in writing the report or in the decision to submit the report for publication.
Dr. Cho and Dr. S.H. Kang were responsible for the research idea and study design; Dr. Do, Dr. Jin, Dr. G.W. Kang, Dr. D.K. Kim, Dr. M.S. Kim, Dr. S.N. Kim, Dr. S.-H. Lee, and Dr. J.W. Park were responsible for data acquisition; Dr. Y.-L. Kim, Dr. H.C. Park, and Dr. S.-H. Park were responsible for data analysis/interpretation; Dr. Cho and Dr. S.H. Kang wrote the paper; Dr. Y.-K. Lee provided supervision or mentorship; and Dr. Cho, Dr. Do, Dr. Jin, Dr. G.W. Kang, Dr. S.H. Kang, Dr. D.K. Kim, Dr. M.S. Kim, Dr. S.N. Kim, Dr. Y.-L. Kim, Dr. Y.-K. Lee, Dr. S.-H. Lee, Dr. H.C. Park, Dr. J.W. Park, and Dr. S.-H. Park contributed to and reviewed the manuscript.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
References
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al.: Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395: 497–506, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al.: Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China [published online ahead of print February 7, 2020]. JAMA doi:10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. China Medical Treatment Expert Group for Covid-19 : Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382: 1708–1720, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al.: Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 395: 565–574, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. China Novel Coronavirus Investigating and Research Team : A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382: 727–733, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim JM, Chung YS, Jo HJ, Lee NJ, Kim MS, Woo SH, et al.: Identification of coronavirus isolated from a patient in Korea with COVID-19. Osong Public Health Res Perspect 11: 3–7, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization: Novel Coronavirus (2019-nCoV) Situation Report—51, 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10. Accessed March 15, 2020
- 8.World Health Organization: Novel Coronavirus (2019-nCoV) Situation Report—54, 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200314-sitrep-54-covid-19.pdf?sfvrsn=dcd46351_8. Accessed March 15, 2020
- 9.Kwan BC, Leung CB, Szeto CC, Wong VW, Cheng YL, Yu AW, et al.: Severe acute respiratory syndrome in dialysis patients. J Am Soc Nephrol 15: 1883–1888, 2004. [DOI] [PubMed] [Google Scholar]
- 10.Wong PN, Mak SK, Lo KY, Tong GM, Wong Y, Watt CL, et al.: Clinical presentation and outcome of severe acute respiratory syndrome in dialysis patients. Am J Kidney Dis 42: 1075–1081, 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Assiri A, McGeer A, Perl TM, Price CS, Al Rabeeah AA, Cummings DA, et al. KSA MERS-CoV Investigation Team : Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med 369: 407–416, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmed AE, Alshukairi AN, Al-Jahdali H, Alaqeel M, Siddiq SS, Alsaab HA, et al.: Development of a risk-prediction model for Middle East respiratory syndrome coronavirus infection in dialysis patients. Hemodial Int 22: 474–479, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Korea Centers for Disease Control and Prevention : Middle East respiratory syndrome coronavirus outbreak in the Republic of Korea, 2015 [published correction appears in Osong Public Health Res Perspect 7: 138, 2016]. Osong Public Health Res Perspect 6: 269–278, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Assiri A, Abedi GR, Bin Saeed AA, Abdalla MA, al-Masry M, Choudhry AJ, et al.: Multifacility outbreak of Middle East respiratory syndrome in taif, Saudi Arabia. Emerg Infect Dis 22: 32–40, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boldog P, Tekeli T, Vizi Z, Dénes A, Bartha FA, Röst G: Risk Assessment of novel coronavirus COVID-19 outbreaks outside China. J Clin Med 9: E571, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rocklöv J, Sjödin H, Wilder-Smith A: COVID-19 outbreak on the Diamond Princess cruise ship: Estimating the epidemic potential and effectiveness of public health countermeasures [published online ahead of print February 28, 2020]. J Travel Med doi:10.1093/jtm/taaa030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park HC, Lee YK, Lee SH, Yoo KD, Jeon HJ, Ryu DR, et al. Korean Society of Nephrology MERS-CoV Task Force Team : Middle East respiratory syndrome clinical practice guideline for hemodialysis facilities. Kidney Res Clin Pract 36: 111–116, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park HC, Lee YK, Yoo KD, Jeon HJ, Kim SJ, Cho A, et al.: Korean clinical practice guidelines for preventing the transmission of infections in hemodialysis facilities. Kidney Res Clin Pract 37: 8–19, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park HC, Kim DH, Yoo KD, Kim Y-G, Lee S-H, Yoon HE, et al. Korean Society of Nephrology COVID-19 Task Force Team : Korean clinical practice guidelines for preventing transmission of coronavirus disease 2019 (COVID-19) in hemodialysis facilities. Kidney Res Clin Pract 10.23876/j.krcp.20.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ma Y, Diao B, Lv X, Zhu J, Liang W, Liu L, et al. : 2019 novel coronavirus disease in hemodialysis (HD) patients: Report from one HD center in Wuhan, China. MedRxiv doi:10.1101/2020.02.24.20027201 [Google Scholar]
- 21.World Health Organization: Novel Coronavirus (2019-nCoV) Situation Report—49, 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200309-sitrep-49-covid-19.pdf?sfvrsn=70dabe61_4. Accessed March 15, 2020
- 22.Wang Y, Wang Y, Chen Y, Qin Q: Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures [published online ahead of print March 5, 2020]. J Med Virol doi:10.1002/jmv.25748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhao S, Lin Q, Ran J, Musa SS, Yang G, Wang W, et al.: Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: A data-driven analysis in the early phase of the outbreak. Int J Infect Dis 92: 214–217, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bauch CT, Oraby T: Assessing the pandemic potential of MERS-CoV. Lancet 382: 662–664, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hellewell J, Abbott S, Gimma A, Bosse NI, Jarvis CI, Russell TW, et al. Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group : Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health 8: e488–e496, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al.: The Incubation Period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application [published online ahead of print March 10, 2020]. Ann Intern Med doi:10.7326/M20-0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Korean Center for Disease Control (KCDC): The updates on COVID-19 in Korea as of 13 March, 2020. Available at: https://www.cdc.go.kr/board/board.es?mid=&bid=0030. Accessed March 15, 2020
- 28.Our World in Data: Coronavirus Testing—Source Data, 2020. Available at: https://ourworldindata.org/coronavirus-data. Accessed March 15, 2020
- 29.Park HC, Lee SH, Kim J, Kim DH, Cho A, Jeon HJ, et al.: Effect of isolation practice on the transmission of middle east respiratory syndrome coronavirus among hemodialysis patients: A 2-year prospective cohort study. Medicine (Baltimore) 99: e18782, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hollander JE, Carr BG: Virtually perfect? Telemedicine for Covid-19. N Engl J Med 382: 1679–1681, 2020. [DOI] [PubMed] [Google Scholar]
- 31.Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, et al.: Presumed asymptomatic carrier transmission of COVID-19 [published online ahead of print February 21, 2020]. JAMA doi:10.1001/jama.2020.2565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen D, Xu W, Lei Z, Huang Z, Liu J, Gao Z, et al.: Recurrence of positive SARS-CoV-2 RNA in COVID-19: A case report. Int J Infect Dis 93: 297–299, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]