Abstract
During the COVID-19 pandemic, we are likely to see a significant increase in the requests for rapid assessment of cardiac function, due to the frequent pre-existence of cardiac pathologies in patients admitted to hospital, and to the emergence of specific cardiac manifestations of this infection, such as myocarditis, sepsis related cardiomyopathy, stress induced cardiomyopathy and acute coronary syndromes. Hand-held, point-of-care ultrasound (HH-POCUS) is particularly suited for the provision of rapid, focused, integrated assessments of the heart and lungs. We present a review of the indications and protocols for focused HH-POCUS use in an acute setting and formulate proposals for streamlining their application in the COVID-19 context towards guiding optimum management of these patients while at the same time allowing adherence to robust infection control measures to provide safety to both the patient and our clinical staff.
Keywords: COVID-19, Hand-held ultrasound, Echocardiography, Pandemic, Cardiovascular imaging, Coronavirus
Abbreviations: ALI, Acute lung injury; ARDS, Acute respiratory distress syndrome; COVID-19, Coronavirus disease 2019; CV, Cardiovascular; HH, Hand-held; HHUS, Hand-held ultrasound; ICU, Intensive care unit; LUS, Lung ultrasonography; LV, Left ventricle; LVEF, Left ventricular ejection-fraction; POCUS, Point of care ultrasound; PPE, Personal protective equipment; RV, Right ventricular
Patients who become critically ill during a pandemic, such as with Coronavirus disease 2019 (COVID-19), often have underlying cardiovascular (CV) disease or develop CV complications.1 Cardiac imaging with echocardiography plays a key role in guiding assessment and management of these critically ill patients. Recommendations from national and international societies including the British Society of Echocardiography, American Society of Echocardiography and European Association of Cardiovascular Imaging are being updated to guide the use of CV imaging during this pandemic.2 There is, however, limited reference to the role of hand-held (HH) point of care ultrasound (POCUS) for assessment of cardiac and pulmonary assessment, which in a large proportion of cases may provide sufficient information to answer immediate clinical questions, act as a gatekeeper to more detailed imaging where needed and allow adherence to robust infection control thus providing safety to both the patient and our clinical staff.
CV Impact of COVID-19
COVID-19 has been associated with symptomatic and asymptomatic troponin release (differentials of myocarditis, sepsis- or stress-related cardiomyopathy, acute coronary syndrome), pericardial effusions, arrhythmias and venous thromboembolism. A large proportion of patients admitted with COVID-19 have CV comorbidities, which have a significant adverse impact on survival.3 COVID-19 patients can develop diffuse interstitial and alveolar damage as part of the acute lung injury (ALI)/acute respiratory distress syndrome (ARDS), commonly coexisting with heart failure and possibly complicated by acute right ventricular (RV) dysfunction, thus necessitating repeated assessment of ventricular function, particularly in those who require non-invasive or invasive mechanical ventilation.
Role of hand-held ultrasound (HHUS)
Due to the speed of image availability and the immediate bedside interpretation, POCUS with small, pocket-sized dedicated devices and, more recently, ‘plug and play’ probes that can be interfaced with ‘smart’ phones/tablets, provides rapid, ‘real-time’ information that often directly impacts on immediate patient management.4
HH echocardiography has a high accuracy compared to standard machines for quantification of left ventricular (LV) and RV systolic function and valve dysfunction.5 Recently, transpulmonary intravenous contrast achieved substantial improvement of endocardial border definition for the assessment of LV ejection-fraction (LVEF) even with HHUS.6
When and how to use HHUS
Detailed recommendations are available on all aspects of HHUS imaging and on the use of echocardiography in emergency settings.7 , 8 An integrated lung-heart-inferior vena cava scanning protocol achieved excellent discrimination of cardiac versus lung-related causes of dyspnea in the emergency department.9
HH POCUS imaging protocols for the heart
Imaging protocols adapt to the limitations of the HH hardware, with, at most, semi-quantitative assessment of valvular pathologies, in the absence of spectral Doppler. Table 1 compares the advantages and limitations of HHUS versus conventional or portable echocardiography.
Table 1.
Advantages and limitations of hand-held ultrasound for cardiac assessment over conventional or portable echocardiograms.
| Hand-held ultrasound | |
|---|---|
| Advantages | Limitations |
| Portability (easy access, no need for power sockets, easily used in field hospitals) | Limited quantification capabilities (no spectral Doppler, no quantitative valve assessment, pulmonary pressures and diastolic function) |
| Infection control (easy to sheath, disinfect) | Lower resolution and limited image optimization |
| Affordable (availability in poorer economies) | Limited to 2-dimensional |
| Screening/triaging in remote areas | Small screen size |
| Staff safety | Reimbursement |
| Time taken for study | Equivocal findings need confirmation by standard echocardiography |
| Serial monitoring | |
Non-urgent setting
Level 1 protocol
The British Society of Echocardiography level 1 protocol requires acquisition of parasternal long-axis (+/− colour) and parasternal short-axis images at all 3 levels, apical four-chamber (+/− colour), apical 5-chamber, subcostal views, and M-mode for tricuspid annular plane systolic excursion or TAPSE and for inferior vena cava calibre and respiratory variation. It assesses volume status, LV/RV dysfunction/dilatation, aortic valve / mitral valve dysfunction, and pericardial effusion.
Focused, limited protocols for use in an urgent/emergency setting
Focused echocardiography in emergency life support (FEEL)
Peri-resuscitation echocardiography is implemented during an advanced life support -conformed interruption of cardiopulmonary resuscitation of <10 s by minimally-trained operators. Three standard views (subcostal, parasternal or apical) are used to assess cardiac motion, ventricular function, RV dilatation or pericardial collection.10
Focused intensive care echo (FICE)
This protocol aims to identify relevant LV and RV pathology and pericardial or pleural fluid. It has been validated in intensive care unit (ICU) patients where it provided new data with impact on clinical management in more than two-third of cases.11
Focused assessment transthoracic echocardiography (FATE)
This requires parasternal, apical and subcostal images, and bilateral pleural views. The goals are to exclude major cardiac pathology, to assess LV wall thickness, internal dimensions and LVEF, and to visualise the pleura bilaterally. This protocol demonstrated significant positive clinical impact on outcomes in ICU patients.12
Focused assessment with sonography for trauma (FAST)
Images are acquired from the abdomen in patients with signs of shock or suspicion of abdominal injury, and subcostal images are used to assess the heart and to detect haemopericardium or haemoperitoneum.13
HH POCUS protocols for the lungs
In the COVID-19 pandemic there have been calls to replace the stethoscope by wireless HH POCUS of the chest.14 Lung ultrasonography (LUS) is one of the easiest applications of HHUS, requiring minimal technical skills and < 2 min of time to be performed. LUS yields high accuracy in the diagnosis of interstitial syndromes, especially in critically ill and emergency medicine patients. In pulmonary oedema, the presence of lung comets, or B-lines, high sensitivity and specificity for extravascular lung water,15 and correlate to progression of lung congestion and to the effects of diuretics. We recommend a standardized 10-sectors approach for LUS in suspected/confirmed COVID-19 patients including scanning of basal and upper quadrants on mid-clavicular and mid-axillary lines and basal quadrants on the posterior paravertebral line on both sides of the chest (10 s per sector).15 In critical care settings and for patients unable to maintain the sitting position, the posterior areas might be difficult to be evaluated, although considered a “hot-area” for COVID-19 pneumonia. The presence of bilateral B-lines arising from a smooth and thin pleural line in ≥2 quadrants is diagnostic of pulmonary oedema.9 Conversely, the presence of an indented or broken pleural line associated with small sub-pleural consolidations and heterogeneous distribution of B-lines is in general indicative of non-cardiogenic pulmonary oedema (ALI/ARDS).16
Operator selection, staff safety and infection control measures
Cardiac HH POCUS should be performed only by operators with adequate training. Ideally this should be transthoracic echocardiography accreditation from a national or international body or focused echocardiography accreditation such as FICE. With staff shortages or increasing demand, flexibility with this recommendation may be required so long as senior review is available. Left-handed scanning should be encouraged where feasible to limit proximity to the patient's airway. Key infection control elements are thorough hand-washing with soap and water and scrupulous donning and doffing of appropriate personal protective equipment (PPE), according to contagion risk and to aerosol-generating procedures. National and international organisations and medical societies including The World Health Organisation are regularly updating their PPE for healthcare provider recommendations regularly.17
Where available disposable probe sheaths should be used. Appropriate decontamination of echocardiography equipment is required after each patient. Handheld machines, compact and without multiple transducers, ports and ECG cable are easier to clean and can be more easily shielded with protective covering for better infection control.
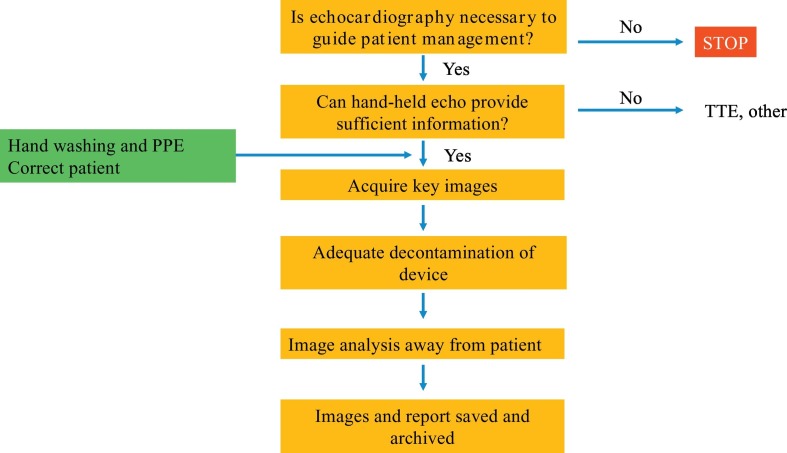
Suggested brief protocol/ minimum dataset
Echocardiography (either using HH or more advanced scanners) for patients with confirmed or suspected COVID-19 should be performed on the wards whenever possible and should be focused on acquiring the diagnostic information to answer a specific clinical question, but should aim to be comprehensive enough to avoid repeat scanning. Requests for echo should contain a specific clinical question with demonstrable impact on clinical management. The decision to request scanning should be taken by senior clinicians (ideally after discussion of the potential clinical impact of testing between referrer and echocardiographer) with clear clinical information, including patient COVID status. Each study should be tailored to its indication, with advanced planning of the images necessary to answer the clinical question, while minimising exposure to the risk of infection. Table 2 provides an abbreviated protocol of essential and optional images that could be undertaken in approximately 5 min by an experienced operator, along with a proposed algorithm for streamlined HHUS imaging during a pandemic (Fig. 1 ).
Table 2.
Suggested abbreviated protocol for hand-held cardiopulmonary ultrasound study in suspected or confirmed COVID patients.
| HH-POCUS Protocol | 2D | Colour flow | Key information |
|---|---|---|---|
 Parasternal Long Axis |
LV and RV Aortic root Pericardium Ascending aorta LA size |
MV AV |
Size (LV, RV) and function (LV, RV, AV, MV) Pericardial and pleural effusion |
 Parasternal Short Axis |
Basal, mid and apical LV AV level and RVOT |
– | Size (LV, RV) and function (LV, RV and AV) |
 Apical four chamber |
LV and RV LA and RA |
MV TV |
Size (LV and RV, RA, LA) and function (LV and RV, RA, LA, MV and TV). |
 Apical 5 chamber |
AV | AV | Function (AV) |
 Apical two chamber |
LV | MV | Size and function (LV) |
 Apical three chamber |
LV AV and MV |
– | Size (LV) and function (LV, RV, AV and MV) |
 Subcostal view |
Pericardium IVC size and respiratory dynamics |
– | Pericardial effusion RA pressure estimation (IVC size and dynamics) |
 Midaxillary, midclavicular, paravertebral lines |
A or B-lines Pleural line (10 quadrants) |
– | Interstitial syndromes (pulmonary odema, ALI/ARDS) |
Bold text – recommended abbreviated dataset. Normal font – optional images depending on abnormal preceding images of those structures.
Fig. 1.
Proposed algorithm for streamlined hand-held ultrasound imaging during a pandemic.
Image saving and storage
Saving and archiving images should be systematically done to allow review, guide future imaging studies and provide a baseline for sequential studies. In some cases, there will be an indication for more advanced imaging (using a mobile, rather than a hand-held scanner, e.g. for wall motion and quantitative valvular assessment or if available CV magnetic resonance or computed tomography).
Future perspectives
Research into the effectiveness of HHUS compared to portable or conventional TTE during the COVID-19 pandemic may help refine current strategies and optimise protocols not just in pandemics or natural disasters but also in routine clinical cardiology. The impact on management and the need for additional imaging following HHUS POCUS should be systematically documented, to quantify the incremental clinical benefit of the initial POCUS. Incremental benefit in patient management from additional detailed imaging should also be recorded to help identify those who may not benefit from an initial HHUS approach. COVID-19 could be a catalyst for implementation of telemedicine and home care programs, further enhancing the role of robotics in managing public health and infectious disease including performance of remote echocardiography, especially in the setting of highly contagious disease, using robotic assistance to acquire images at the bedside with remote review by a sonographer, might play a greater role in the future and should be systematically assessed for feasibility and accuracy.18
Conclusions
Hand-held ultrasound is likely to play a key role in the diagnosis and management of patients during COVID-19 and other potential pandemics due to its versatility, availability and its inherent advantages in infection control and staff safety. We have reviewed the literature and suggest a rapid ~5-min protocol for a focused study generating sufficient information to guide optimum, safe and efficient management. Training in HHUS should be encouraged and further study of its effectiveness and limitations is justified.
Author contributions
MYK and AI contributed to the conception or design of the work. MK, AI drafted the manuscript. MK, FR, RSP, AAC, SB, VG, JN and AI critically revised the manuscript. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Funding
No specific funding was provided for this work.
Dr. Patel is funded by a British Heart Foundation Intermediate Fellowship (FS/14/76/30933).
Declaration of Competing Interest
None.
References
- 1.Guo T., Fan Y., Chen M., et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skulstad H., Cosyns B., Popescu B.A., et al. COVID-19 pandemic and cardiac imaging: EACVI recommendations on precautions, indications, prioritization, and protection for patients and healthcare personnel. Eur Heart J Cardiovasc Imaging. 2020;395:514. doi: 10.1093/ehjci/jeaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan W.-J., Liang W.-H., Zhao Y., et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: a Nationwide analysis. Eur Respir J. 2020 doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Narula J., Chandrashekhar Y., Braunwald E. Time to add a fifth pillar to bedside physical examination: inspection, palpation, percussion, auscultation, and Insonation. JAMA Cardiol. 2018;3:346–350. doi: 10.1001/jamacardio.2018.0001. [DOI] [PubMed] [Google Scholar]
- 5.Andersen G.N., Haugen B.O., Graven T., Salvesen O., Mjølstad O.C., Dalen H. Feasibility and reliability of point-of-care pocket-sized echocardiography. Eur J Echocardiogr. 2011;12:665–670. doi: 10.1093/ejechocard/jer108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramirez R., Patel Y., Hobson S., Talebi S., Narula J., Argulian E. Bedside assessment of left ventricular emptying using contrast-enhanced handheld ultrasound: a pilot study. J Am Soc Echocardiogr. 2019;32:1367–1369. doi: 10.1016/j.echo.2019.05.026. [DOI] [PubMed] [Google Scholar]
- 7.Cardim N., Dalen H., Voigt J.-U., et al. The use of handheld ultrasound devices: a position statement of the European Association of Cardiovascular Imaging (2018 update) Eur Heart J Cardiovasc Imaging. 2019;20:245–252. doi: 10.1093/ehjci/jey145. [DOI] [PubMed] [Google Scholar]
- 8.Neskovic A.N., Hagendorff A., Lancellotti P., et al. Emergency echocardiography: the European Association of Cardiovascular Imaging recommendations. Eur Heart J Cardiovasc Imaging. 2013;14:1–11. doi: 10.1093/ehjci/jes193. [DOI] [PubMed] [Google Scholar]
- 9.Kajimoto K., Madeen K., Nakayama T., Tsudo H., Kuroda T., Abe T. Rapid evaluation by lung-cardiac-inferior vena cava (LCI) integrated ultrasound for differentiating heart failure from pulmonary disease as the cause of acute dyspnea in the emergency setting. Cardiovasc Ultrasound. 2012;10:49. doi: 10.1186/1476-7120-10-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Breitkreutz R., Price S., Steiger H.V., et al. Focused echocardiographic evaluation in life support and peri-resuscitation of emergency patients: a prospective trial. Resuscitation. 2010;81:1527–1533. doi: 10.1016/j.resuscitation.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 11.Hall D.P., Jordan H., Alam S., Gillies M.A. The impact of focused echocardiography using the focused intensive care Echo protocol on the management of critically ill patients, and comparison with full echocardiographic studies by BSE-accredited sonographers. J Intensive Care Soc. 2017;18:206–211. doi: 10.1177/1751143717700911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jensen M.B., Sloth E., Larsen K.M., Schmidt M.B. Transthoracic echocardiography for cardiopulmonary monitoring in intensive care. Eur J Anaesthesiol. 2004;21:700–707. doi: 10.1017/s0265021504009068. [DOI] [PubMed] [Google Scholar]
- 13.Price S., Via G., Sloth E., et al. Echocardiography practice, training and accreditation in the intensive care: document for the world interactive network focused on critical ultrasound (WINFOCUS) Cardiovasc Ultrasound. 2008;6:49. doi: 10.1186/1476-7120-6-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buonsenso D., Pata D., Chiaretti A. COVID-19 outbreak: less stethoscope, more ultrasound. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30120-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Picano E., Pellikka P.A. Ultrasound of extravascular lung water: a new standard for pulmonary congestion. Eur Heart J. 2016;37:2097–2104. doi: 10.1093/eurheartj/ehw164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ricci F., Aquilani R., Radico F., et al. Role and importance of ultrasound lung comets in acute cardiac care. Eur Heart J Acute Cardiovasc Care. 2015;4:103–112. doi: 10.1177/2048872614553166. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization . 2020. Rational use of personal protective equipment for coronavirus disease (COVID-19): interim guidance, 27 February 2020. [Google Scholar]
- 18.Boman K., Olofsson M., Berggren P., Sengupta P.P., Narula J. Robot-assisted remote echocardiographic examination and teleconsultation: a randomized comparison of time to diagnosis with standard of care referral approach. JACC Cardiovasc Imaging. 2014;7:799–803. doi: 10.1016/j.jcmg.2014.05.006. [DOI] [PubMed] [Google Scholar]