Dear Editor,
The Covid-19 pandemic have spread to 185 countries affecting almost 5 million patients worldwide with more than two million recovering and more than 300 thousand deaths globally as of 17th May [1].
The main cause of death is acute respiratory insufficiency with or without Acute Respiratory Distress syndrome (ARDS).
Recent evidence, over concurrent coagulation disorders, has emerged with reported cases of pulmonary embolism and clinical worsening due to disseminated intravascular coagulation (DIC) [2,3]; moreover most reported thrombophilic conditions affecting these patients are acute pulmonary embolism (PE), deep-vein thrombosis (DVT), ischemic stroke, myocardial infarction or systemic arterial embolism and cerebral vein thrombosis without hemorrage [4,5]; in consideration of these observations the administration of low-molecular-weight-heparin (LWMH) has been introduced recently as adjuvant therapy [6].
Moreover, evidence of central and peripheral neurological symptoms have been recently described in Covid-19 patients in Wuhan (30,2–45-5%) with higher prevalence in cases of severe pulmonary infection, with report of two cerebral hemorrhages (1,8%) [7]; in these series, heparin was not administered as support therapy.
From 20th-April to the 29th April, in 4 different hospitals in Italy, six (n=6) Covid-19 positive patients presented intraparenchymal cerebral hemorrhage related to cerebral vein thrombosis. Patients characteristics are summarized in Table. 1 .
Table 1.
Patients characteristics, CT findings, neurological symptoms and therapeutical management. (I.U. International Unit).
| Patient | Age (years) | Gender | ICU | Thrombosis/hemorrhagic site | Prior LWMH therapy YES/NO (I.U.) | Symptoms | LWMH therapy after diagnosis (I.U.) |
|---|---|---|---|---|---|---|---|
| 1 | 64 | M | YES | Right parietal (Right transverse sinus and sagittal sinus) | 4000 × 2 | Epileptic Seizure | 8000 × 2 |
| 2 | 75 | F | NO | Left parietal | NO | Headache, hemiplegia, TIA | 8000 × 2 |
| 3 | 52 | M | NO | Right parietal | 4000 × 2 | TIA, Headache | 8000 × 2 |
| 4 | 65 | M | YES | Right parieto-occipital and temporal | 4000 × 2 | GCS 5 | 8000 × 2 |
| 5 | 61 | F | YES | Left parietal | 6000 × 2 | GCS 6 | 8000 × 2 |
| 6 | 75 | F | YES | Right temporal | 6000 × 2 | ND for mechanical ventilation | 8000 × 2 |
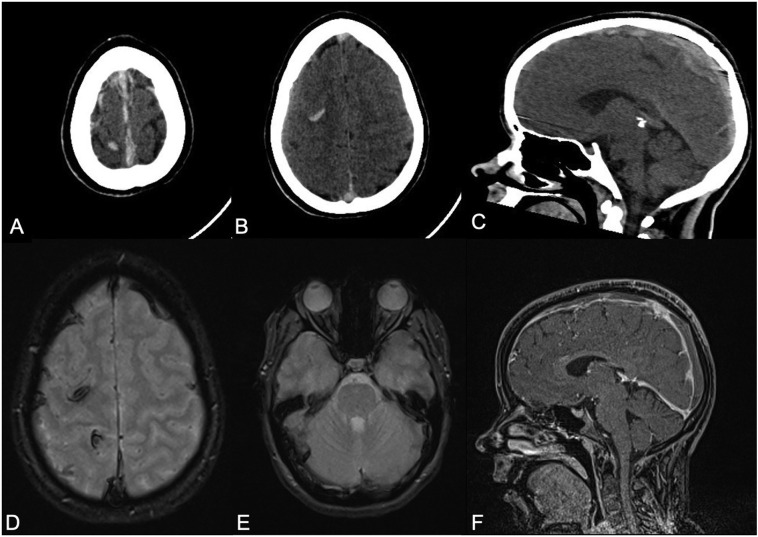
In all patients an unhenaced CT scan was acquired and in 2 patients an adjunctive pre and post-contrast MRI was acquired. (see Fig. 1 )
Fig. 1.
A) and B) Unehnanced axial brain CT scan shows hyperdense appearance along the superior sagittal sinus with intracerebral hemorrhagic infarction in the right parietal and frontal lobes. C) CT sagittal reconstruction depicts the extension of sagittal sinus hyperdensity. D) and E) T2 GRE MRI confirms hemorrhagic foci in parietal and frontal lobes; to note the thrombosis of the superior sagittal sinus and right transverse sinus. F) T1-FFE 3D MRI after administration of contrast medium showed extension of thrombosis in sagittal sinus.
In 4 patients the site of hemorrhage was single; in 2 patients multiple sites were reported.
4 patients were in Intensive Care Unit (ICU) with mechanical ventilation and 1 patient was under oxygen support therapy; in the last patient, asymptomatic for respiratory alterations, cerebral hemorrhage was the first symptom discovered, with further development of typical lung CT patterns and positive Real-Time Reverse Transcriptase-Polymerase Chain Reaction assay for COVID-19 from the nasopharyngeal swab specimen.
Not-ICU patients presented the following symptoms: headache (100%) hemiplegia (50%), seizure (50%), TIA (50 %); in one of these patients, neurological symptoms (transient hemiplegia) were the first clinical alteration of COVID-19 infection.
In 5/6 patient LWMH was previously added in therapy prior to the diagnose of cerebral hemorrhage (at least 3 days before) at a dosage of 4000-6000 × 2. All patients implemented LMWH to therapeutical dosage (8000 × 2).
The only patient with a diagnose of cerebral hemorrhage as first symptom of Covid-19 disease started LWMH at a dosage of 8000 × 2. In two ICU-patients, diagnosis of neurological symptoms and cerebral hemorrhage was done at the time of attempt of extubation with clinical evidence of central neurological symptoms (GCS 6 and 5) that required re-intubation.
Any patients included in this series did not presented contemporary evidence of Pulmonary Thromboembolism.
It's has been recently discovered and discussed the prevalence of thrombotic events in COVID patients. Despite this evidence, to date, no reported case regarding cerebral hemorrhage due to cortical vein thrombosis had been described.
The observations of this clinical situation might have several implications:
-
•
In this emergency scenario, the availability of dedicated CT rooms and time-spot for radiological examination in Covid-19 patients led to organizational problem affecting Radiological Departments. Due to the high number of exams required and to the necessity of room disinfection protocol (around 1 h between every patient) the availability of CT-room can be reduced [8.
In order to optimize patients care, and only in selected cases with pulmonary and neurological impairment, concomitant chest and brain CT scan might be helpful. These observations can play a pivot role, in particular in mechanically ventilated patients, due to the possible co-existence of acute hidden underlying neurological alteration.
-
•
Knowledge of incidence of cerebral hemorrhage linked to cerebral vein thrombosis matches the evidence of pro-coagulation disorders and DIC as co-factor in Covid-19 patients with corroboration of LWMH as an essential treatment; moreover, patients admitted in intensive care unit having higher thrombotic risk might benefit from LMWH therapy.
In conclusion, brain CT examination can be suggested in selected cases especially in ICU and mechanically ventilated patients without significantly increasing of time and radiation dose. The present protocol could help to avoid waste of resources in this emergency healthcare condition. Evidence described could also play a crucial role in clinical practice to detect rapidly and more accurately patients who require modification of LMVH therapy.
Compliance with ethical standards
For all authors there is no potential conflict of interest that could be perceived to bias our work.
This study was not supported by any funding.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all individual participants included in the study.
Consent for publication was obtained for every individual person's data included in the study.
Authors had full control of all the data and information presented in this manuscript.
References
- 1.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. Epub 2020 Feb 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen T., Wu D., Chen H. Vol. 368. 2020. Clinical Characteristics of 113 Deceased Patients with Coronavirus Disease 2019: Retrospective Study; p. m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rotzinger D.C., Beigelman-Aubry C., von Garnier C., Qanadli S.D. Pulmonary embolism in patients with COVID-19: Time to change the paradigm of computed tomography. Thromb. Res. 2020 Apr 11;190:58–59. doi: 10.1016/j.thromres.2020.04.011. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garaci F., Di Giuliano F., Picchi E., Da Ros V., Floris R. Venous cerebral thrombosis in COVID-19 patient. J. Neurol. Sci. 2020 May 1;414 doi: 10.1016/j.jns.2020.116871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thachil J., Tang N., Gando S. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J. Thromb. Haemost. 2020;18(5):1023–1026. doi: 10.1111/jth.14810. Epub 2020 Apr 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mao L., Jin H., Wang M., Hu Y., Chen S., He Q., Chang J., Hong C., Zhou Y., Wang D., Miao X., Li Y., Hu B. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020 Apr 10 doi: 10.1001/jamaneurol.2020.1127. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nakajima K., Kato H., Yamashiro T. COVID-19 pneumonia: infection control protocol inside computed tomography suites. Jpn. J. Radiol. 2020;38(5):391–393. doi: 10.1007/s11604-020-00948-y. [DOI] [PMC free article] [PubMed] [Google Scholar]