Abstract
Although self-tracking offers potential for a more complete, accurate, and longer-term understanding of personal health, many people struggle with or fail to achieve their goals for health-related self-tracking. This paper investigates how to address challenges that result from current self-tracking tools leaving a person’s goals for their data unstated and lacking explicit support. We examine supporting people and health providers in expressing and pursuing their tracking-related goals via goal-directed self-tracking, a novel method to represent relationships between tracking goals and underlying data. Informed by a reanalysis of data from a prior study of migraine tracking goals, we created a paper prototype to explore whether and how goal-directed self-tracking could address current disconnects between the goals people have for data in their chronic condition management and the tools they use to support such goals. We examined this prototype in interviews with 14 people with migraine and 5 health providers. Our findings indicate the potential for scaffolding goal-directed self-tracking to: 1) elicit different types and hierarchies of management and tracking goals; 2) help people prepare for all stages of self-tracking towards a specific goal; and 3) contribute additional expertise in patient-provider collaboration. Based on our findings, we present implications for the design of tools that explicitly represent and support an individual’s specific self-tracking goals.
Keywords: Personal Informatics, Health, Patient-Provider Collaboration, Chronic Conditions, Migraine
1. INTRODUCTION
Chronic health conditions are the leading cause of sickness, disability, and death worldwide, accounting for 60% of the global burden of disease [66]. Health technology plays an increasingly vital role in helping people understand and manage chronic conditions (e.g., [36, 43]). These technologies often include self-tracking (e.g, [15, 35]), as many patients and providers believe self-tracked data has the potential to capture a more complete understanding of patient health [16, 17, 85]. Providers therefore often recommend patient self-tracking [1, 3, 16, 36, 83].
Unfortunately, self-tracking tools often leave the goals people have for chronic condition management unstated and lacking explicit support. For example, people often want to better understand how habits and behaviors affect their symptoms [3, 60], but tools tend to emphasize the data itself without providing such insights (e.g., in charts and timelines that primarily show the magnitude of data) [30]. Providers also struggle with their goals for patient-tracked data, as they often lack time to analyze the data or feel unequipped to interpret it [16, 85].
Due to the disconnects between the goals people have and the designs of the tools they use, people often:
find self-tracking overwhelming and without purpose (i.e., struggle to define tracking goals) [31];
find self-tracked data does not support their questions (i.e., struggle to align data with their goals) [14];
find tools fail to support their goals over time (i.e., struggle to adapt tracking to evolving goals) [33];
find collaboration with providers difficult (i.e., struggle with the multiple goals of patients and providers) [17].
To help people and health providers overcomes these challenges, we explore how designs can support people in expressing and pursuing condition management and tracking goals via goal-directed self-tracking. We focus on the domain of migraine, a prevalent and debilitating condition that severely affects quality of life and productivity [79]. To investigate support for tracking towards specific migraine-related goals, we first reanalyzed data from prior work characterizing categories of goals that people with migraine and providers often have for migraine-related data [74]. Based on that reanalysis, we contribute goal-directed self-tracking as a novel method to scaffold the process of deciding what, when, and how to track toward a specific goal, together with goal-appropriate analyses and visualizations of resulting data. Using a paper prototype to present design ideas for goal-directed self-tracking, we conducted interviews with 14 people with migraine and 5 health providers. Our findings indicate goal-directed self-tracking can improve tool support for: 1) eliciting different types and hierarchies of management and tracking goals; 2) helping people consider and prepare for every stage of self-tracking; and 3) contributing additional expertise in patient-provider collaboration. These attributes could help address disconnects between the goals people have for data in their chronic condition management and the tools they use to support such goals. We also find potential pitfalls, such as encouraging negative aspects of goal creep and failing to prevent unrealistic goals. Based on these opportunities and pitfalls, we discuss design implications for future implementations of goal-directed self-tracking systems within and beyond migraine management.
2. BACKGROUND AND RELATED WORK
This section summarizes related work and provides background information about our study context (i.e., migraine). We focus on differentiating past work, which has investigated the importance of considering goals in self-tracking and patient-provider collaboration, versus our current contribution, which is to explore how designs can explicitly elicit, represent, and support an individual’s self-tracking goals in a self-tracking system.
2.1. Self-Tracking and Health
Although self-tracking is increasingly popular, many self-trackers struggle to find value in their data [54]. Li et al. developed a five-stage model of personal informatics, highlighting barriers in each stage and how challenges cascade into later stages [54]. Rooksby et al. then introduced “lived informatics” to characterize the different styles, variations, and goals people bring to everyday tracking [72]. The lived informatics model extends Li et al.’s model, emphasizing the failure of current tools to support many realities of everyday tracking [33]. The model includes three stages: 1) deciding and selecting, in which people choose why and how to track; 2) tracking and acting, in which people engage in the ongoing process of collecting, integrating, and reflecting on data; and 3) lapsing and resuming, in which people forget, intentionally skip, or suspend tracking. Our research examines how goal-directed self-tracking can support people in preparing for and addressing barriers in each of these stages.
Setting personalized and realistic self-tracking goals and showing progress towards those goals can help encourage healthy behaviors (e.g., [21, 22, 63]). However, current tools often fail to support the personalized and evolving goals individuals want to pursue [8, 52, 55]. Gulotta et al. found current tools generally fail to support setting, pursuing, reflecting on, and modifying goals [37]. Current tools also often fail to support tracking for longer-term self-expression and remembering [29]. Tools sometimes even encourage behaviors that are contrary to a person’s goals (e.g., people tracking food using commercial journaling tools reported the relative ease of tracking foods with barcodes encouraged them to eat processed foods, contrary to their healthy eating goals [23]). Setting unrealistic goals can also be detrimental (e.g., people with obesity that have unreasonable expectations for their weight loss are more likely to discontinue treatment [24]). The tracker goal evolution model characterizes relationships between qualitative goals (e.g., losing weight, having a healthy lifestyle) and quantitative goals (e.g., meeting a certain step count, eating a specific diet) and describes challenges people face when attempting to define appropriate quantitative goals based on their qualitative goals [64]. We examine how eliciting and supporting the goals people have via goal-directed self-tracking can help them navigate similar challenges in setting appropriate tracking goals based on their condition management goals.
People with chronic conditions often want to track myriad related factors [74, 75], but tools often silo data [33, 34]. Prior research investigated importing data from multiple tools (e.g., [42, 56]), which enables analysis but cannot support earlier self-tracking stages. Semi-automated tracking combines automated tracking (e.g., through devices and sensors) with manual tracking (e.g., of data that cannot be automatically tracked, of data that brings positive awareness when manually tracked) to lower burden while preserving benefits [13]. OmniTrack builds on the concept of semi-automated tracking to support customization of a self-tracking tool [51]. Although these approaches can help people track exactly and only their desired data, they do not provide guidance or support in identifying, expressing, or pursuing goals for data. Our research builds upon this prior work to examine how goal-directed self-tracking can help people overcome challenges in how to customize such tools.
Prior research has supported self-tracking for individualized insights to manage chronic conditions (e.g., irritable bowel syndrome [45, 75], diabetes [19, 35, 47, 61], multiple sclerosis [5, 88]). However, intensive tracking is burdensome and unsustainable [14, 23, 31], with tools often failing to support lapsing and resumption [20, 31, 33]. Even semi-automated tracking can be burdensome when it fails to accommodate evolving tracking routines and goals [12]. The prospect of tracking for long-term condition management can therefore be daunting. Individuals may also have different goals for condition management, depending on their habits, priorities, behaviors, experiences, and approaches. For example, a study with overweight and obese women found a need for tools to support personalized goals rather than emphasizing weight loss (e.g., more energy, better stamina, consistent exercise routines, myriad definitions of healthier eating) [8]. We investigate how explicit support for defining, pursuing, and lapsing in tracking towards personalized goals can better facilitate an individual’s condition management.
2.2. Seeking Expert Help in Interpreting Health Data
People often turn to health providers for help interpreting self-tracked data [17, 28, 36, 89]. Data can clarify and contextualize patient health [83], foster collaboration [7, 75], and improve diagnoses, treatments, and outcomes [16, 65, 80]. Collaborative review can help people identify trends, hypothesize about symptom contributors, generate action plans, and identify new information needs [68, 75]. However, despite potential and enthusiasm for clinical use of self-tracked data, patients and providers struggle to get value from such data. Providers lack time to review data or feel unequipped to interpret it [11, 16, 85, 86]. Current tools do not support data sharing in provider workflows [16, 36]. Because no validated method exists for providers to interpret self-tracked data, the process is difficult and error-prone [39, 44]. Collaboration around self-tracked data often breaks down when patients and providers have different goals or expectations [17, 69, 71]. Chung et al. investigated goals patients and providers bring to collaborative review of patient-generated data and discussed the value of modifying food tracking protocols according to an individual’s goals [17]. They also suggested that collaboratively designing a tracking routine could help patients and providers align and fulfill goals. Luo et al. had dietitians construct patient profiles and design custom tracking routines for those profiles, similarly finding a need to help patients and providers collaboratively design tracking routines that best fit individuals and their goals [58]. Other recent work includes a pre-visit note through which patients can summarize their tracking and communicate goals for a clinic appointment [18]. West et al. developed a 6-stage model for using self-tracked data in clinical settings, with each stage having associated barriers: aligning objectives, evaluating data quality, judging data utility, rearranging the data, interpreting the data, and acting on the data [87]. We propose and examine goal-directed self-tracking to support people with chronic conditions and their providers in aligning goals and expectations before data is collected, aiming to help them: 1) understand each other’s goals, 2) collect data they need with respect to those goals, and 3) review analyses and visualizations appropriate for those goals.
2.3. Study Context: Migraine
Migraine is characterized by debilitating symptoms that can be “triggered” by a range of contributors (e.g., diet, environmental factors, sleep, stress) [2, 50]. Contributors affect people differently, so people often attempt to identify personal contributors [60]. However, multiple contributors often must accumulate before precipitating symptoms [50, 84]. Approaches that focus on individual “triggers”, rather than considering multiple potential contributors, can therefore be misleading (e.g., identifying spurious correlations due to confounds) and prevent symptom management [4]. Successful management often requires identifying a range of contributors and avoiding simultaneous exposure. As some may be unavoidable (e.g., changes in weather), people develop strategies to defend against symptoms (e.g., lifestyle changes that reduce symptom likelihood despite exposure to contributors).
Because successful management relies on patient-reported information, providers often encourage patients to track migraine-related data [78]. However, self-tracking in migraine is particularly difficult due to unpredictable, intermittent, and poorly-understood symptoms, as well as the wide range and cumulative effects of potential contributors [67]. Although some people use apps to track migraine-related data, prior work has found current tools often fail to support migraine tracking goals [74]. People report that current apps offer insufficient customization, resulting in them: 1) feeling forced to track data they do not want to track (i.e., increasing burden for data irrelevant to their goals), and 2) feeling unable to track data they do want to track (i.e., preventing tracking of data necessary for their goals). Some people attempt to use multiple apps, but integrating the resulting siloed data introduces new challenges. Although some migraine tracking apps include configuration capabilities (e.g., Migraine Buddy, the only migraine tracking app used by more than 10 people in [74]), they do not scaffold the process of deciding exactly and only what a person needs to track to achieve their goals. As a result, people often abandon migraine apps without achieving their goals, instead using alternate methods (e.g., paper journals, customized spreadsheets, calendars) or abandoning tracking altogether. We build upon this research, identifying pitfalls people encounter when pursuing distinct migraine tracking goals and developing goal-directed self-tracking to address those challenges. In Section 6.6, we discuss implications for these techniques in other domains.
3. DEVELOPMENT OF GOAL-DIRECTED SELF-TRACKING
This section first describes our reanalysis and new findings in data from a prior study of migraine tracking goals [74]. We then introduce goal-directed self-tracking, a new method to scaffold the process of deciding what, when, and how to track for a specific goal. Finally, we discuss our iterative design process for a goal-directed self-tracking system and present the paper prototype design we used in our interviews.
3.1. Characterizing Differences in Tracking Routines Between Migraine Tracking Goals
Our approach to goal-directed self-tracking builds directly on prior HCI research in migraine management. Park and Chen first characterized common needs of people with migraine, including: determining whether symptoms are due to migraine, identifying triggers, developing management strategies, and coordinating social recognition and assistance [67]. We then examined self-tracking by people with migraine, surveying 279 people with migraine and conducting semi-structured interviews with 13 survey respondents and 6 providers [74]. They identified a number of needs and opportunities, including four distinct categories of migraine tracking goals. Participants often had simultaneous goals, and goals often evolved over the course of a person’s migraine management.
To investigate how a system could explicitly support the goals people have for migraine tracking, we reanalyzed our interview data. In contrast to our previous bottom-up approach focused on general practices and challenges in migraine tracking, we focused on the particular tracking habits people described as they pursued different categories of goals. For each interview participant, we re-examined the original interview transcript to identify: 1) categories of goals the participant described pursuing, and 2) what and when they described tracking and wanting to track toward each stated goal (Table 1). We therefore expand on our previously-identified goal categories to characterize resulting differences in tracking routines (i.e., what, when, and how to track). Given the limited number of participants, these goal categories may not be comprehensive of every possible migraine-related tracking goal. However, the range of categories allow us to investigate how to explicitly distinguish and design for goals people bring to self-tracking for chronic condition management. Many participants described multiple goals, due to goal evolution over time or simultaneous goals. We briefly summarize the four distinct goal categories identified in our prior work, together with our new findings of what, when, and how participants wanted to track in pursuit of those goal categories. Table 2 summarizes the final set of goals and subgoals supported in our design.
Table 1.
What and when participants from [74] described tracking and wanting to track to pursue their stated migraine tracking goal categories. M=participants with migraine, P=provider participants.
| Goal Category (Why) | Participants | Types of Data (What) | Tracking Frequency (When) |
|---|---|---|---|
| Answering Questions | 12 M (all but 19); 3 P (P2, P4, P6) | Symptoms (12 M, 3 P), Treatments (4 M, 3 P), Contributors (12 M, 3 P) | Daily (8 M, 1 P), After Symptoms Occurred (4 M, 2 P) |
| Predicting and Preventing | 3 M (It, 16,17) | Symptoms (3 M), Treatments (3 M), Contributors (3 M) | Daily (3 M) |
| Monitoring Over Time | 12 M (all but I8); 3 P (PI, P3, P5) | Symptoms (12 M, 3 P), Treatments (6 M, 2 P), Contributors (6 M, 2 P) | Daily (4 M), Every 2–3 Days (1 M), After Symptoms Occurred (7 M, 3 P) |
Table 2.
Hierarchy of the migraine tracking goal categories and subcategories supported in the final paper prototype.
| Supported Tracking Goals and Subgoals |
|---|
| 1. Learning about their migraines (usually medium effort: regular tracking of many data types) a. Learning what factors may affect their symptoms (i.e., identifying potential contributors) b. Learning the frequency of their symptoms or related factors (an alias for Goal 3 to support an alternate framing) c. Learning how a change affects their symptoms (i.e., a before/after test) |
| 2. Predicting whether they are at risk for a migraine (usually high effort: daily tracking of maximum data types) |
| 3. Monitoring migraine-related data (usually low effort: infrequent tracking of fewer data types) |
Answering Questions about their Migraines
“You basically turn your life into a control of an experiment and try to change one thing at a time and see what works.” (I11)
Many participants tracked to answer specific questions about their migraines (e.g., which factors contributed to or alleviated symptoms). Our reanalysis revealed participants pursuing this goal often tracked more types of data and more frequently than those pursuing a monitoring goal. We also found two subgoals: identifying contributors, pursued by eight participants (i.e., discovering what factors affect symptoms), and before/after tests, pursued by six (i.e., examining whether symptoms improved after a change, such as starting a new medication or eliminating a hypothesized contributor). In contrast to recent work investigating self-experimentation (e.g., [9, 25, 26, 45, 46, 53]), before/after tests are susceptible to confounds. However, self-experimentation is often infeasible for migraine, because: 1) self-experimentation requires contributors to be controllable and actionable [46], and 2) due to the severity of symptoms, people are often reluctant to risk inducing a migraine in an experiment [74]. People with migraine therefore often pursue less rigorous methods when attempting to identify contributors.
Predicting and Preventing Migraines
“[When I know the barometric pressure is going to drop] I make sure that everything else in my body is as healthy as possible so that hopefully I can ride through that weather front without any other [contributors].” (I06)
After identifying personal contributors, some participants tracked exposure to those personal contributors to predict the likelihood of symptoms so they could prepare for or attempt to prevent those symptoms. Based on our reanalysis, this goal category required the most effort, with all participants who pursued it tracking symptoms, treatments, and contributors on a daily basis. No providers described a predicting goal, perhaps because providers generally focus on overall symptom frequency rather than the consequences of symptoms on a particular day.
Monitoring Migraines Over Time
“[my provider saw my symptom calendar] and was like, ‘That’s too many headaches ... if you’re still getting six or seven headaches a month in a couple months, we’re gonna talk about doing something else’.” (I02)
Long-term tracking is important in monitoring a person’s condition over time (e.g., to notice changes in symptoms, to ensure management strategies remain effective). In our reanalysis, we found participants described tracking less data, less often. Although four tracked daily, two were also pursuing predicting goals, which may explain their more frequent tracking. Participants sometimes framed this goal as learning the frequency of migraines. To ensure we explicitly support goals in the way people find most intuitive, we therefore added a third subgoal to answering questions: learning the frequency of migraines and related factors.
Enabling Motivation and Social Recognition
“[A patient] might think, ‘I’m doing so horrible, I’m doing so horrible’, and then you look at it, and you’re like ‘you actually cut back your severity by 50%’. . . you kind of shift your perspective as you go on, and the new horrible becomes just the same horrible, even though it’s improved. So, it’s helpful to show that improvement more than anything.” (P3)
Participants also described seeking support as they develop personalized management strategies. Successful management often requires difficult lifestyle changes (e.g., in diet, exercise, sleep), so this goal category can help foster motivation and support needed to commit to those changes. However, our reanalysis revealed this goal was consistently secondary to one of the other categories. For example, many people with migraine described primary goals of monitoring, but also wanted to show their data to friends, family, or coworkers to share how they were doing. Similarly, provider participants were often primarily concerned with monitoring a patient’s symptoms and treatments to inform future treatment recommendations, with a secondary goal of providing motivation by showing symptom improvement. Our reanalysis therefore suggests that motivation and sharing should be available across tracking goals (e.g., by including shareable data visualizations, by supporting reflection on progress toward goals, by recommending and encouraging behavior changes that can reduce migraines).
3.2. Characterizing Data Elements Tracked Across Migraine Tracking Goals
Although the types of data participants tracked (i.e., symptoms, treatments, contributors) often depended on their goals, specific data elements (i.e., the particular symptoms, treatments, and contributors) depended more on the individual. For example, the specific contributors participants tracked varied according to personal characteristics (e.g., people who do not menstruate do not track their menstrual cycle), habits (e.g., people who do not consume caffeine do not track caffeine), and hypotheses (e.g., people who suspect particular foods or drinks correlate with their symptoms often track those specific foods and drinks). Similarly, the specific symptoms participants tracked depended on personal experiences with migraine (e.g., only some people experience aura, “brain fog”, or fatigue). Our reanalysis therefore suggests that the particular data elements people want to track are orthogonal to their goals: individuals tracking the same data element may have different goals, and individuals with the same goal may want to track different data elements. The one characteristic of data elements that did seem to correlate with goal type is the granularity of data: people who wanted to learn about an element often tracked more details than people monitoring that element. For example, people who wanted to learn about their migraines often wanted to track details about symptom severity and duration, while people who wanted to monitor often only recorded that they had a migraine. However, even the granularity sometimes depended more on an individual’s experiences: participants who felt their migraines varied often described tracking more details, even if their primary goal was to monitor. Table 3 provides examples of data elements and granularities participants tracked for each data type.
Table 3.
Example data elements and granularities participants from [74] described tracking for each data type. Data elements were generally orthogonal to a participant’s goal, depending more on their habits and experiences.
| Data Type | Example Data Element | Example Granularity |
|---|---|---|
| Symptoms | Migraine | Binary |
| Duration | ||
| Location | ||
| Severity from 1–10 | ||
| MIDAS score (i.e., a validated scale to characterize severity [81]) | ||
| Aura | Binary | |
| Nausea | Binary | |
| Treatments | Medications | Binary (i.e., for specific medications) |
| Number of pills | ||
| Supplements | Binary (i.e., for specific supplements) | |
| Yoga | Binary | |
| Mindfulness | Unspecified | |
| Exercise | Number of steps | |
| Fitbit reports | ||
| Minutes | ||
| Contributors | Caffeine | Binary |
| Number of milligrams | ||
| Menstruation | Using a menstrual tracking app | |
| Diet | Everything they ate | |
| Whether they ate a specific thing (e.g., corn, dairy, wheat, tannins, nitrates) | ||
| Sleep quality | Using a Fitbit | |
| Scale from 1–10 |
3.3. Scaffolding Tracking towards Individualized Goals via Goal-Directed Self-Tracking
Based on the specific goals and sub-goals (corresponding to different tracking needs) and data elements (corresponding to personalized characteristics, habits, and hypotheses) identified in our reanalysis, we next formulated design requirements for goal-directed self-tracking tools. These tools should scaffold the process of deciding what, when, and how to track toward a specific set of goals and provide goal-appropriate support for interpreting resulting data. We refer to this new method of explicitly eliciting and supporting an individual’s goals throughout all stages of self-tracking as goal-directed self-tracking.
Although many participants pursuing a given goal category described tracking similar types of data with similar frequency, some had divergent tracking practices (e.g., the majority of participants with monitoring goals tracked only when symptoms occurred, but some chose to track more regularly). A requirement for goal-directed self-tracking tools is therefore to recommend what, when, and how to track toward goals, while providing flexibility to support people in tracking however they feel will be useful for their goals. People can therefore receive guidance in configuring appropriate tracking routines for their goals while avoiding pitfalls in which tools: 1) do not support tracking data a person wants, or 2) require tracking data a person does not want, both of which can lead to abandonment [31, 33]. Tools should then also provide goal-appropriate analyses and visualizations, helping people and their health providers avoid pitfalls in interpreting collected data [14, 17, 30].
Participants also described goals that varied over time, consistent with existing models of self-tracking [33, 64]. A second requirement for goal-directed self-tracking tools is therefore to support an individual’s specific circumstances and tracking needs over time. Tools can represent a person’s tracking needs as a set goals the person has explicitly selected and configured, and the person’s total tracking routine is then the combination of tracking they have configured for each goal. As a person’s understanding and goals evolve over time, tools can support adding, modifying, or removing goals. A goal-directed self-tracking tool can thus be adjusted to a person’s evolving needs over time, rather than requiring the person seek out new tools as their needs evolve.
3.4. System Design
To investigate goal-directed self-tracking, we created a preliminary design for supporting the goal categories identified in Section 3.1. The design was initially expressed through a flowchart representing goal selection, configuration within each goal, and post-configuration features. We iterated on the design in pilot studies with four people with migraine, identifying problems with flow or clarity as well as gaps in supported features. Pilot testing revealed a need to enhance each goal category with educational information, examples, and decision-making support, as individuals may not know what goals are possible or understand which best describe their personal goals. We also added a way to express a goal in a person’s own words before selecting and configuring based on a goal category, to encourage open-ended consideration of why a person wants to track migraine-related information.
After our initial iterations, we designed a paper prototype to elicit needs, ideas, and feedback in our interviews (see Figure 1). Such low-fidelity prototypes can elicit valuable feedback about content and sequence of steps before investing in higher-fidelity prototypes [73]. We conducted pilot studies with five colleagues in human-centered design and engineering, computer science, and medicine to iterate on the paper prototype, again focusing on improving clarity and flow while adding or expanding on features as needed.
Fig. 1.
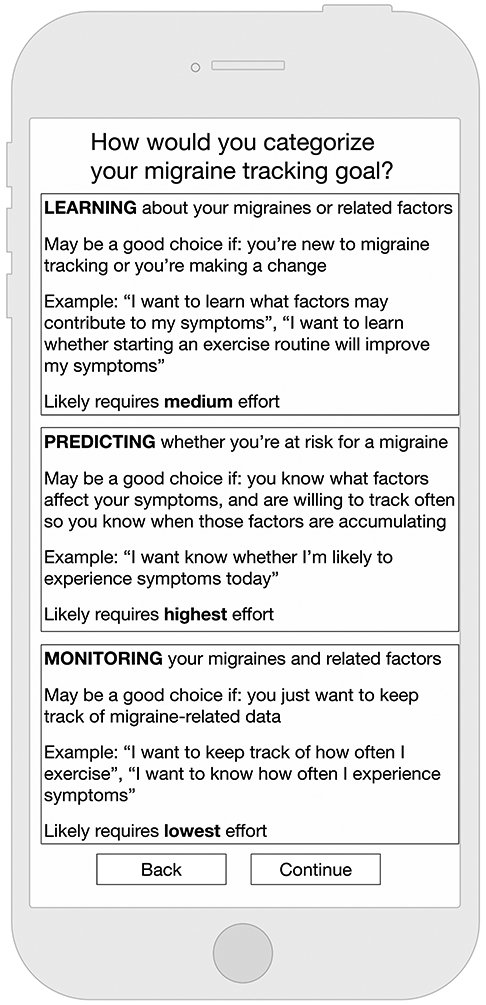




Our paper prototype walks people through selecting a goal, configuring tracking towards that goal, and collecting and interpreting data for that goal. The full prototype can be found in the supplementary materials.
3.4.1. Initial Goal Selection.
The first step in the prototype is to add a goal. A person begins by stating why they want to track migraine-related data in their own words. They then select the supported goal category that best describes that goal (see Table 2, recalling Goal 1b is an alias for Goal 3). To help people select the most appropriate goal, each category includes a brief explanation, specific examples, and an indication of likely relative effort.
3.4.2. Goal Configuration.
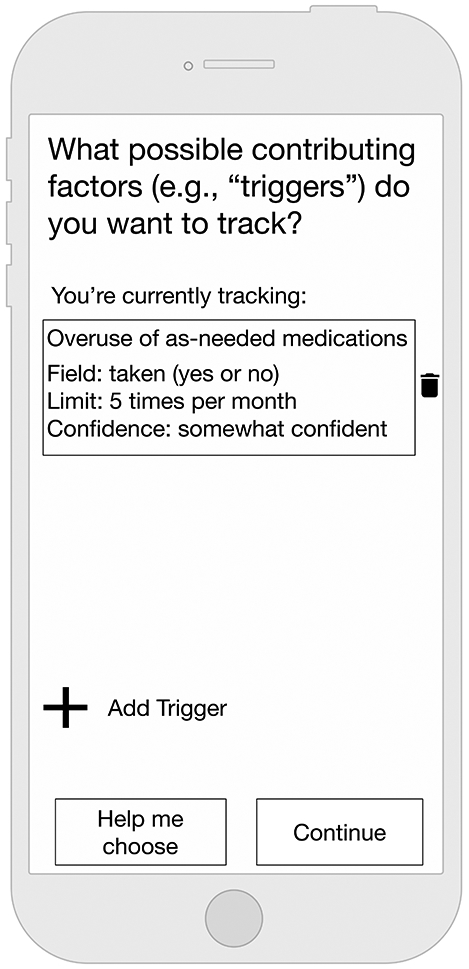
After selecting a goal category, the prototype walks a person through selecting what data to track for the goal. For most categories, they configure any symptoms, contributors, and treatments they want to track. Data types are ordered and recommended based on their importance to that goal. For example, for monitoring (Goal 3), the prototype assumes symptoms are the only necessary data type, so a person always configures those first. For identifying contributors (Goal 1a), the prototype assumes a person will track potential contributors and configures those first. For learning how a change affects symptoms (Goal 1c), a person configures only the changes they want to make and the related symptoms they want to examine (i.e., without configuring other treatments or contributors, which would be irrelevant to the specific goal).
A person can configure data manually or via Help Me Choose pages that list common migraine-related data. They can also configure semi-automated tracking routines [13], including data automatically synced from other devices and services (e.g., Fitbit, local weather). When configuring contributors, the app recommends tracking for overuse of as-needed medication, a common and often-overlooked factor that experts often recommend tracking [57, 74]. A person also configures how to track by specifying fields (e.g., binaries, categorical scales, numbers, text). They finally select when to track, configuring notifications to prompt them to track at fixed intervals (e.g., daily, weekly) or to remind them to track additional information after any indication of symptoms. Such post-symptom tracking enables people to quickly indicate presence of symptoms without completing a full tracking routine, minimizing screen time during any period of light sensitivity while creating cues to later add information necessary for their goal. If a person has multiple tracking goals, they can add additional goals after configuring the first.
3.4.3. Post-Configuration App Features.
Although we focus on tracking configuration, we also wanted to explore possible post-configuration features. After a goal is configured, the prototype includes:
quick trackers on the landing page to allow quick indication of symptoms or as-needed medication use;
data collection, customized according to the configuration;
data views, including a calendar and data summary, for quickly reviewing data;
a treatment flowchart, added because pilot study participants expressed difficulty deciding what treatments to pursue when experiencing symptoms (other than as-needed medications);
an FAQ page, to provide general information about migraine;
a goal configuration page, for adding or removing goals and viewing past goals; and
a lapsing page that enables taking explicit breaks from tracking, with optional support for recording a reason and/or scheduling a resumption date.
Finally, we included goal-specific web-based analyses and visualizations to support interpretation and collaboration: calendars and graphs over time for monitoring (Goals 1b and 3); charts that state and illustrate correlations between symptoms and potential contributors for learning contributors and predicting (Goals 1a and 2); and charts that examine symptoms before and after a change for learning how a change affects symptoms (Goal 1c).
4. INTERVIEW METHODS
We used our paper prototype in interviews to elicit feedback on scaffolded goal-directed self-tracking. Our study was approved by our Institutional Review Board. Protocols can be found in our supplementary materials.
4.1. Participants with Migraine
We recruited 14 participants with migraine via a website for connecting health-focused research teams to the community, as well as via email lists and fliers posted in medical centers. All participants self-identified as having migraine, and all either tracked related data or had considered doing so. 12 participants were female, a gender distribution that reflects migraine diagnosis [70]. Participant ages ranged from 20 to 61 (x=34).
We designed a semi-structured interview protocol to investigate whether and how our system could support migraine-related goals. We first asked about migraine and tracking experiences, then worked through the prototype to configure a tracking routine based on the participant’s selected goal. Finally, we asked about the system as a whole, including whether and how they anticipated it would support their goals and how they would feel about using it collaboratively with a provider. Following the blank page technique [82], participants were provided with blank phone and laptop “screens” on which they could sketch their ideas. Sessions were approximately 90 minutes, compensated with a $30 Amazon gift card. We refer to these participants as M#.
A third-party service transcribed the audio recordings. To analyze the data, we took a bottom-up approach in which a group of eight researchers first divided and read transcripts, extracting relevant notes. The researchers included a mix of people familiar with the project and people who were further removed, to solicit a range of perspectives in the analysis. Three researchers then created an affinity diagram [41], iterating on themes via novel findings from the interview transcripts as well as discussion among members of the research team.
4.2. Provider Participants
We recruited 5 health providers via colleagues of the medical providers on our research team and snowball sampling (see Table 4 for health provider details). All had experience working with people with migraine, and all regularly recommend their patients with migraine self-track. The protocol followed a similar structure in which we asked about experiences working with people with migraine before walking through the prototype. However, instead of choosing a single goal, we discussed all goal categories to understand what they thought of the included set. We investigated whether providers believed the system would help people with migraine, as well as whether providers believed it would help them collaborate with and treat their patients. Sessions were approximately 60 minutes, compensated with a $50 Amazon gift card. We refer to the providers as P#.
Table 4.
Identifiers, areas of practice, and positions of employment for the five provider participants we interviewed.
| Provider | Areas of Practice | Position |
|---|---|---|
| P1 | Headache Clinic | Nurse Practitioner |
| P2 | Headache Clinic, Neurology | Fellow |
| P3 | Headache Clinic, Neurology | Neurologist |
| P4 | Neighborhood Clinic | Physician Lead for Clinical Informatics |
| P5 | Headache Clinic | Fellow |
Data analysis similarly consisted of transcribing audio recordings and conducting an affinity diagramming analysis. We started with previously-identified categories and notes from the sessions with people with migraine, adding notes that reflected provider perspectives and iterating on the affinity diagram. As we finalized the affinity diagram, we re-examined transcripts to identify any additional data that supported or contradicted the emergent themes. Our final affinity diagram included 59 notes in 6 categories, available in the supplementary materials.
4.3. Limitations
Our participants skewed WEIRD (Western, Educated, Industrialized, Rich, and Democratic; [40]), likely because our interviews were conducted in person with our paper prototype at our US institution. Our institution is in a city, and all participants lived in an urban environment; people in rural areas may have different experiences and perspectives [6, 59]. Care must therefore be taken when attempting to generalize our findings. Our inclusion criteria also required participants to have tracked migraine-related data or seriously considered doing so, to ensure their feedback on the paper prototype was grounded in their experiences with tracking or consideration of tracking. Four participants had never tracked, but all had considered doing so. We therefore cannot characterize whether and how people who had not previously considered tracking might use such a system. Finally, our methods directly examined the deciding and selecting stage of the lived informatics model [33] by investigating participant migraine-related goals and their configuration of tracking routines based on those goals. We did not directly observe later tracking stages, as participants did not track according to their configured routines. However, configuration of goal-directed self-tracking prompted participants to discuss anticipating and planning for later stages of tracking. Our results therefore inform future in-the-wild deployments to further examine how goal-directed self-tracking supports goals through later stages of tracking. Similarly, our paper prototype allowed rapid examination of how its design might influence configuration of goals and tracking routines and how people envision using it, but deployment of a functional prototype would be required to examine ongoing use or non-use.
5. RESULTS
All participants felt the design supported configuring tracking exactly and only what they needed for their goals, and all said they would use a goal-directed self-tracking system. This section describes benefits and pitfalls participants encountered and anticipated while interacting with the prototype. Our results reveal opportunities to address disconnects between goals people have for data in chronic condition management and the tools they use toward such goals, specifically the potential for a system to: 1) elicit different types and hierarchies of management and tracking goals; 2) help consider and prepare for all stages of self-tracking; and 3) contribute additional expertise in patient-provider collaboration. We report how many participants expressed particular perspectives, but our open-ended protocol means not every participant was explicitly prompted about every topic. Additional participants may have agreed with a perspective if asked. To avoid implying by omission that any individual did not hold a particular view, we do not indicate which participants discussed which topics.
5.1. Eliciting Different Types and Hierarchies of Goals
All participants thought the goal categories encompassed their migraine tracking goals. Four participants with migraine and four providers described beginning with a goal as motivating; M5 liked the idea of “starting off with the goal and having something in your mind that you’re looking forward to or trying to achieve”. Nine participants with migraine selected a primary goal of learning (eight with the subgoal of identifying contributors (Goal 1a) and one of before/after tests (Goal 1c)), three chose predicting (Goal 2), and two monitoring (Goal 3). Providers were primarily interested in monitoring (Goal 3). Eliciting goals as the first step in configuration also helped people develop and express multiple types and hierarchies of migraine-related goals. Specifically, participants articulated differences between management versus tracking goals, immediate versus future goals, goals for awareness versus taking action, and personal versus provider goals. This section discusses these nuances.
5.1.1. Management vs Tracking Goals.
Of the fourteen participants with migraine, thirteen discussed management goals, often in having fewer or less severe symptoms. Four providers said they developed management goals with patients, generally including implementing behavior changes to reduce symptoms. Although most participants saw the critical path between their management goals and tracking goals, some initially had trouble defining specific tracking goals. When asked to state her tracking goal in her own words, M4 said, “I don’t know. I just want to know how to get rid of them faster”. Ml also struggled to express why she wanted to track migraine-related data.
However, explicit goal categories helped people define tracking goals that complemented their management goals. When M4 saw the goal categories, she selected identifying contributors, saying “the example down below, I read that and I was like, ‘this would be very useful’ ”. Ml similarly felt examples helped her define a tracking goal. Listed categories sometimes prompted people to modify their tracking goals to better fit their management goals. Four participants initially described monitoring goals, but then selected the category of learning, explaining that such a goal would help more with their ultimate management goals. Seven people with migraine and four providers said they would want to pursue multiple goals simultaneously. Overall, the explicit goal categories seemed to help participants understand how specific tracking goals could help them reach their management goals.
5.1.2. Immediate vs Future Goals.
In addition to goals they configured during the study, the list of goals led some participants to hypothesize about migraine tracking goals they might want to pursue in the future. Eight people with migraine and two providers said they would want to start with one goal before progressing to another, usually because they felt success of the future goal depended on fulfilling their current goal(s). M3 explained:
The most relevant one would be learning because my goal is trying to understand what causes them. But then once I’ve gotten past this stage and understood what essential triggers are or anything like that, then monitoring and predicting would play a higher role than learning.
Although most people described future goals as dependent on fulfilling current goals, M14 defined hers based on tracking habits. Despite an ultimate goal of learning (Goal 1), she selected monitoring (Goal 3) because she wanted to “get good” at a lower-effort goal before “tackling” a higher-effort goal. She then chose to track some contributors and get daily tracking notifications, requiring more effort than many monitoring goals, to “see how it went”.
5.1.3. Goals for Awareness vs Taking Action.
Across all goal categories, participants described goals focused on awareness that might evolve into goals focusing on action. Eleven people with migraine and three providers discussed goals focused on gaining awareness about their symptoms, habits, and behaviors so they could identify specific changes they might make in the future. For example, M7 said, “it would be nice to see what precursors might be related to having a migraine so that I could reduce those in the future”. Three believed the act of tracking could help them take action; they wanted to track behaviors they intended to change because they thought tracking would remind and encourage them to commit to the changes (e.g., avoiding medication overuse, taking recommended supplements, increasing mindfulness, exercising regularly).
5.1.4. Personal vs Provider Goals.
The prototype also elicited differences between goals people had for themselves and those they pursued for providers. All participants with migraine described provider-related goals (e.g., tracking because their provider asked them to, tracking so they could more accurately answer questions their providers asked). In some cases, participants did not consider personal goals until interacting with the prototype. M3 commented:
I’ve never actually thought about... what I want to accomplish aside from just being able to illustrate to my doctor what’s been going on. But I think that having either a goal that you collaborate to create or separate goals and then come together to create one is a really cool idea.
Some providers had similarly never considered patients having personal tracking goals. P5 stated, “To be honest, I have never really extensively talked to a patient about what their tracking goals are. I usually tell them ‘this is my goal, at least please do this’... I’m not sure what other goals they might have”.
In general, people with migraine and providers thought that learning about each other’s goals would be helpful. P1 encouraged patient goals because “it can be empowering to patients to better understand what’s going on with their body and to be able to recognize some of those things and not just feel like their body is out of their control”. However, all providers wanted to ensure their expertise and advice were accounted for in the goals the patient pursued. In this paper, we refer to any hypothetical goals a provider would want a patient to pursue that are distinct from the patient’s initial priorities as provider goals. Although the majority of participants with migraine were open to pursuing provider goals, M3 felt it would be “frustrating” if a provider asked her to modify her goal. Even though this was the same participant who had never considered having a personal goal, once she had identified one, she said she would “want the doctor to take [her] concerns into creating this goal more than anything else”. Three others similarly wanted to collaborate and understand their provider’s rationale for modifying their goals. All participants thought simultaneously pursuing both goals could be a good compromise.
5.2. Goal-Directed Tracking Across Tracking Stages
We designed our prototype to support goals throughout self-tracking, so we wanted to determine how our participants anticipated goal-directed self-tracking could support the stages described in the lived informatics model [33]. This section considers participant reactions in the context of each stage of the model. Our methods directly examined only the deciding and selecting stage (e.g., goal selection, tracking routine configuration). Participants then anticipated and planned for later stages, discussing how they envisioned using the system. These anticipated uses and barriers inform how a goal-directed system could support later stages of self-tracking.
5.2.1. Deciding and Selecting Stage.
In this first stage of the lived informatics model, people choose why and how to track. Our prototype’s configuration section scaffolds this stage: people select a goal and configure what, when, and how to track toward that goal. Some participants knew what they wanted to track; all independently configured at least one type of data, and two configured all data without even looking at suggestions in the Help Me Choose pages. However, most selected some data to track based on the prototype’s suggestions. Some selected data they “hadn’t thought of before” (M11) but wanted to investigate upon seeing. When selecting potential contributors, M3 and M6 said they would “ just say all of them”. Others felt suggestions helped them remember factors they had already wanted to track; Mil explained, “if I get a question I have to give an answer just off the top my brain, that’s harder than when it’s multiple choice. Multiple choice is like, ‘Oh yeah. It’s right there.’ Then you can start thinking about other ones because it’s there”. M9 similarly described being reminded of her desire to track alcohol.
Regardless of why they selected data from Help Me Choose pages, participants often felt the pages encouraged tracking more data. Mil felt she “probably would have had maybe four [contributors] compared to, well, how many of them. Eight. Nine”. She configured extra tracking because she felt the prototype “makes me realize I have been slacking... You make it look so easy”. After configuration, all participants felt their routine was exactly and only what they wanted to track for their goal; when asked whether they had configured anything they did not feel was important, everyone responded that they had not. However, Ml said, “some days, I feel like [the configured tracking routine] would be a little daunting”. P2 was similarly worried that patients might select too much:
I might limit someone to five categories to track at a time... someone might be very interested in like,“Oh, yeah, I’m gonna track all of these,” and then it becomes too burdensome and they stop tracking.
Participants were particularly likely to expand their tracking when additional data could be automatically tracked. All participants wanted to track some data automatically. Our design included syncing with outside data sources so people who already tracked with those sources could use their data. However, P7 did not have a Fitbit, but said, “if it automatically went to this, I might [get one]”. In some cases, providers were hesitant about some syncable data elements. For example, we include syncing to local weather data because weather can affect migraines. Every participant with migraine chose at least one weather-related field, and P2 and P5 were also interested. However, Pi and P3 felt that focusing on an uncontrollable factor may not ultimately be helpful. Similarly, P4 did not want people focusing on blood pressure data because “it would create an assumption that if it’s a little bit high today, that means that your headache might be explained by that, which I think would be a false assumption”.
5.2.2. Tracking and Acting Stage.
In the tracking and acting stage of the lived informatics model, people collect, integrate, and reflect on their data. Tracking routines configured by participants varied widely, with participants configuring tracking of 1–7 symptoms (median=3.5), 2–9 treatments (median=4), and 0–16 contributors (median=6). They generally appreciated the ability to control how to track by specifying fields, although all wanted the tool to recommend appropriate defaults during configuration. Three planned to track only when they had symptoms; the rest planned to track daily. Providers had different levels of interest in contributors but generally wanted their patients to focus on tracking symptoms and treatments (e.g., medications, lifestyle changes).
Although participants with migraine all reported wanting to pursue the tracking routines they had configured, they anticipated their tracking would evolve over time. As described in Section 5.1.2, some wanted to pursue future goals after fulfilling their current goals. But in addition to evolution of goals, people expected evolution within goals as their experiences and understanding changed. Four participants intentionally configured more than they would want to track, with the intent to narrow their routine after reflecting on their data. M6 explained:
what I’d probably do is start off with all of these and then ... realize there was a couple of questions I’m either like constantly answering the same thing or just kind of, it makes me pause like how do I answer this?... I suggested irritability, but I might drop that one because it [might make me] irritable.
Conversely, two participants wanted to start narrow and later expand their routines. Mi3 wanted to make behavior changes her provider recommended and thought trying too many at once would be overwhelming, saying, “if I just did one thing and then if its good, I mean [after] two or three weeks, add something else. And if that’s good, add another routine”. Three mentioned feeling they needed more domain expertise, such as knowledge of what dietary factors commonly could contribute to symptoms, before they could focus on learning about whether those factors may contribute to their individual symptoms. M2 explained, “I don’t feel like I have enough information about the contributing aspects of dietary factors to know what should I be tracking”. Overall, the prototype helped people make informed decisions about what data to track, both immediately and in the future, to best fulfill their goals. However, even with that support, some participants felt they needed access to more domain expertise to collect, reflect on, and act on the data in the context of their migraine management goals.
Participants also discussed how goal-directed self-tracking would inform how they acted on their data. Thirteen participants with migraine and one provider mentioned wanting to explicitly check in with their goals to reflect on their progress, review what they had learned, and decide whether anything needed to change. The other providers wanted to discuss goals in an appointment and have the patients independently make any changes in the app. Participants also anticipated goal-related data analyses and visualizations would support reflection towards their goals. Both patients and providers liked the calendar and data summary pages, to get “a real quick glance at what you have been experiencing” (M1). Some participants expected the calendar would also help them identify trends; M9 commented, “[with the calendar] you could correlate, maybe if you’re stressed out at work, when you worked on Monday, and then you had this headache Monday too”. Participants also generally liked the web-based analyses and visualizations. P1 explained the visualizations would help them notice more complex and longer-term trends, “to see symptoms over time and to see in relation to changes or in relation to triggers”. However, M10 was afraid the visualizations would be too complicated, and M11 thought she would not be able to interpret them without help. M5 similarly emphasized simplicity, stating, “whatever graph is the easiest to see is the one you guys should go for. One with a lot of words and lots of axis, they’re really hard to tell at a glance.” Many participants acknowledged the tension between prioritizing interpretability and visualizing all important data for a particular tracking goal. Some felt customizability of the generated visualizations could support exploration while limiting complexity; M7 explained, “I would want to select from a dropdown like, ‘Here are all the things you’ve tracked. Select two or a few, or select pairs to see, to generate [a visualization]’ ”. However, M3 warned that while “being able to directly say, ‘okay, this is the only thing I want to look at’ and disregard all the other data might be helpful”, doing so could also “get potentially confusing” by hiding confounds and leading people to incorrect conclusions.
5.2.3. Lapsing and Resuming Stage.
People often exit and re-enter the tracking and acting stage of the lived informatics model via lapsing and resuming. However, current tools generally fail to support lapsing and resumption (see Section 2.1). We designed our prototype to support explicitly taking intentional breaks, with the ability to optionally configure reminders to return to tracking at a particular date. To investigate whether participants anticipated circumstances in which they might want to lapse, we asked whether and when participants thought they would use such functionality. All participants anticipated scenarios in which they would lapse in tracking their full routine. However, rather than lapsing altogether, seven participants with migraine and three providers described wanting the ability to reduce tracking to only a subset of their configured routine. For example, M1 configured an extensive routine, but wanted to be able to “answer the questions as I feel like I have the time to do”. Similarly, M2 ideally wanted to track the number of alcoholic beverages she consumed, but with an option to indicate a binary of alcohol consumption “if number of drinks isn’t something that calculable in the moment”. As described in Section 5.2.2, people anticipated modifying their tracking routines as their goals change; these changes might include lapsing in tracking types of data that are no longer relevant. However, they also wanted to prioritize certain data on a day-to-day basis, according to their experiences on those days. M2 explained:
when I would see myself taking a break would be during finals week, or a really busy application season or something. Which, due to the nature of that might actually be when I’m getting more symptoms... I could see myself taking a break from maybe more of like the background symptoms and... just saying, “Okay, for this week I’m just going to track these really critical symptoms.”
Although lapsing has generally been considered an unexpected and often undesired stage of tracking, our participants were able to predict situations in which they might want to lapse and to suggest ways to do so while continuing to pursue their goals. By expecting and supporting this kind of non-binary lapsing (i.e., lapsing by reducing tracking to only a subset of their configured routine), a system could help people configure a more comprehensive tracking routine while still providing flexibility in their lived experience. How often people would engage in this kind of lapsing should be investigated, but such functionality could support people in pursuing their goals despite varying circumstances and time constraints that might otherwise lead to abandonment.
5.3. Expertise in a Goal-Directed Self-Tracking System
We intended our design to help patients and providers communicate and collaborate around data. However, the design also created expectations that could influence patient-provider relationships. Our prototype included information about migraine (e.g., lists of commonly-tracked data, an explanation of as-needed medication overuse). Because the system included this information, participants described expecting the system to contribute expertise in migraine management. In addition, because the prototype was designed anticipating patient-provider collaboration in goal setting and data interpretation, participants expected that providers would be able to help patients use the system. Our participants discussed potential benefits and pitfalls of these design decisions.
5.3.1. System Support of Patient and Provider Expertise.
All participants felt a system based on our design would support communication and collaboration around their experiences and goals. M5 explained, “showing a graph like this is better than me trying to explain, ‘Oh, I usually have this kind of symptoms,’ or ‘I think I have four a week.’ If [providers] can see a graph I think they’ll be able to help a lot more”. However, M2 was afraid the system would replace her role in her care, rather than support it: “I would want to have the opportunity to have a discussion about [my experiences] and not just base it on what they’ve seen in the charts”. P2 similarly wanted to discuss data with patients: “I always verify, just because I know that I’m not always 100% accurate when I enter something..! don’t know that we need to go through and pull it up, but to say, ‘This is what your app sent over. Does this sound right to you?’”.
Participants also thought having data would corroborate their claims to each other. People with migraine felt data would provide “solid evidence” (M1) that would help providers understand and believe their experiences. For example, M9 wanted her providers to know she was following their recommendations: “I’m like, ‘Yes, I do all those things, but I still get migraines.’ So, yeah I would like to prove [that I’m doing them]”. Providers similarly felt the data would support their recommendations. For example, the page for configuring when to track included an explanation of why people might want to track at different frequencies. P2 said, “I mean obviously I like my patients to track every day, but I think this is a really good screen. I’m really glad that it’s included since this way you can get reminders and something that’s realistic for the patient and they can see the pros and cons”. P1 thought having data would help show patients that certain factors were unrelated to their migraines, explaining, “I don’t feel like it’s always as helpful to try to convince someone that it’s not a trigger if they’re really convinced it’s a trigger”. She similarly felt data could help people understand why their treatment might not be working:
Sometimes, especially if people are having a hard time committing to a daily therapy, it’s good to see exactly how many days they’re skipping or missing. Good for them to see so they know why their therapy might not be helping, and so I can see and help them out.
5.3.2. System Expertise in Managing Health.
Although we designed our prototype anticipating collaboration with providers, participants felt a system could and should support education to help people manage their migraine independently All felt a system would be helpful even without a provider, and eleven participants with migraine mentioned they had learned about migraine during configuration. M6 explained: “I felt like I was already learning a little more about migraine tracking in a simple way where it didn’t feel like I was reading a textbook”.
Five participants with migraine believed expertise embedded in a system could help them avoid seeing a doctor. For example, M2 said, “if I was experiencing symptoms but maybe not so much so that I wanted to go into the doctor this might help me do a mini-revision of how I’m approaching things”. Although the ability to independently fulfill health goals could be helpful, people do sometimes need medical advice. P4 mentioned, “I don’t mind if [patients] track things... It’s the decision making part afterwards that is the high risk area.”. One way to discourage people from making medical decisions without support may be to explicitly suggest when to see a doctor. Five participants with migraine and one provider thought a system should tell people when to seek professional medical advice, and five participants mentioned wanting to be able to message their provider within a system.
5.3.3. Health Provider Expertise in Using a System.
Despite wanting a system to contain sufficient information to be used independently by people with migraine, participants generally expected that providers would help with any issues patients encountered. All participants with migraine and three providers mentioned expecting providers would be able to help patients use the tool. Three people with migraine and three providers mentioned wanting to collaborate to ensure the patient pursued realistic tracking and management goals. Nine participants with migraine described wanting providers to answer their questions, make suggestions, and help them interpret their data. Participants also felt a provider could verify information a system contained. For example, M3 explained, “being able to have [providers] say, ‘Oh yeah, this is definitely a trigger for you. Oh, this could be. Oh, that’s most likely not.’ could save you a lot of stress and time”. However, P4 was worried providers might not be able to meet patient expectations, saying “it is incredibly impressive how many [providers] just don’t know basic computing”.
6. DISCUSSION
Our findings indicate the potential for goal-directed self-tracking systems to address common pitfalls in self-tracking and patient-provider collaboration. We further discuss implications for future design and implementation of goal-directed self-tracking, including the characterization of the system as part of the care team, the need to support evolution between and within tracking and management goals, and dangers of goal creep in configuration. Although we focus on design implications in terms of health and wellness, we expect these themes will transfer to other domains in which people struggle to define, pursue, or collaborate around tracking goals.
6.1. Addressing Common Self-Tracking Pitfalls with Goal-Directed Self-Tracking
Goal-directed self-tracking aims to address common pitfalls in self-tracking, and our participants discussed anticipating and navigating some of these pitfalls. For example, people often find self-tracking overwhelming and without purpose [31]. Even when people have qualitative goals (e.g., losing weight, having a healthy lifestyle), they often struggle to define appropriate quantitative goals (e.g., meeting a certain step count, eating a specific diet), preventing them from developing realistic and useful tracking routines [64]. However, our participants were able to navigate different types and hierarchies of goals, understand the critical path between goals, and set appropriate tracking goals based on their overall management goals. By explicitly asking people to consider why they wanted to track, the system helped them navigate these challenges and formulate their migraine tracking goals.
Although we could only directly observe how goal-directed self-tracking could support the Deciding and Selecting stage, participants also expected such a system would support them in subsequent stages. Participants felt their configured tracking routines were personalized to their goals and would allow them to track exactly and only what they needed for those goals. Participants were also able to anticipate and plan for scenarios in which they would want to lapse. By supporting explicit and purposeful lapsing, our design helped people consider when and how they could lapse in their tracking without sacrificing their goals, in contrast to current tools that generally fail to account for such lapsing [33]. Participants also appreciated having analyses and visualizations that could help them interpret their data in the context of their goals, although future research is needed to examine which analyses and presentations of results can best support the questions people want to ask about their migraine-related data and balance tensions between simplicity and expressiveness. Overall, our findings suggest potential for goal-directed self-tracking to help people overcome common pitfalls in all stages of self-tracking.
6.2. Supporting Patient-Provider Collaboration
When discussing how they would interact with and collaborate using a goal-directed self-tracking system, both people with migraine and provider participants described anticipating a system would help them verify and communicate their beliefs and experiences. Participants wanted to use a system to support their claims, but they also wanted to talk to each other to verify recommendations and data. These accounts are consistent with prior research finding that self-tracked data can ground and provide objectivity in clinic consultations (e.g., [17, 32, 75]) and can foster collaboration by emphasizing both the medical expertise a provider contributes and the detailed experiential knowledge of a patient [7, 75]. Participants also described appreciating the opportunity to consider a collaborator’s goals for self-tracked data. People with migraine often wanted their provider to help ensure their goals were realistic and useful, and providers generally felt that patients who had concrete goals would feel more empowered to manage their migraine. Patient-provider collaboration can often break down when goals or expectations differ [17, 69, 71], so helping people understand and align their goals can help foster collaboration.
Although our findings suggest a goal-directed self-tracking system could improve communication and collaboration, they also reveal potential tensions. Some providers worried about unrealistic patient expectations regarding a provider’s ability to use the system and interpret the data, echoing concerns raised in prior work [75]. Patients and providers also wanted to ensure their goals are considered and pursued, which could prompt disagreement and frustration if patient and provider goals are not easily aligned. Although our design supports simultaneous goals, tracking too much data could increase burdens and lead to abandonment [31]. Tools designed to support both patient and provider goals should therefore help people explain, align, and prioritize goals. Tools could also reveal any increased burden associated with an additional goal. For example, most predicting (Goal 2) goals require strictly more data than monitoring (Goal 3) goals, so a patient who wanted to pursue a predicting goal could likely simultaneously pursue a provider’s monitoring goal without additional burden. Tools could also produce analyses and visualizations for both goals, allowing the patient and the provider to review and discuss data as it relates to their goals. Pre-visit notes can also help providers focus on patient goals and questions [18], so communicating patient goals before a clinic appointment could also support collaboration to align goals.
6.3. System as a Member of the Care Team
Although people with migraine and providers felt goal-directed self-tracking could support collaboration, both wanted a system to contribute its own expertise. Participants wanted a system to include educational information, so people could use it to independently learn about migraine and migraine-related tracking. Research in mental health has suggested apps can feel like an always-available member of a care team [10, 77]. Our findings suggest this feeling extends to other health domains, as people considered the system an expert they could learn from.
In some cases, our design intentionally provided expertise. For example, we included a pop-up that recommended tracking as-needed medication usage, important because overuse is a common contributing factor that many people find counter-intuitive [74]. However, some content was not designed with an intent to teach people about migraine, and such content could create misunderstandings if interpreted as educational or personalized. For example, the Help Me Choose pages list common migraine-related data. However, migraine is personalized, so some factors will be irrelevant for an individual and no list can characterize all potential factors. We included a note that additional factors may be relevant, but did not remind people that some listed factors may not apply to them. A system should therefore differentiate content designed to provide expertise (e.g., FAQ pages, informative pop-ups) from content that requires outside expertise (e.g., configuration pages that assume knowledge of personally relevant data). In addition, although a system could better support some types of expertise (e.g., realistic management goals), others cannot be realistically incorporated (e.g., answers to the wide variety of health-related questions an individual might have). A system therefore should convey when it cannot provide expertise, so people and health providers know the limits of the technology in their collaboration.
Another key area of expertise a goal-directed self-tracking system should support is in tracking itself. Our design conveyed some recommendations based on past research in self-tracking. For example, when participants configured tracking frequency, the system lists pros and cons, acknowledging burdens and encouraging the minimum tracking necessary to achieve their specific goals. However, our findings reveal that both patients and providers could benefit from additional scaffolding of tracking expertise. For example, many wanted to track more data than may be feasible, and people generally wanted the system to have smart defaults for how to track because they did not know what would reasonably balance burden and usefulness. Including such tracking expertise in a tool itself can help guide both people and providers in decisions about self-tracking data and goals.
6.4. Supporting Evolution Within and Between Goals
Self-tracking goals are varied and tend to evolve, both in migraine [74] and in other domains (e.g., healthy eating [15], financial tracking [49], menstrual tracking [32]). For example, we previously found that people with migraine often started tracking toward a data-intensive learning goal before changing to a less-burdensome monitoring goal [74]. Many would also transition back to a learning goal if their symptoms or management approaches changed. Current apps generally fail to support this evolution of goals, forcing people to add or change tracking tools as their goals change. Informed by this prior work, we designed our prototype to: 1) include different categories of tracking goals; 2) facilitate differentiation between current and future goals (e.g., by explaining that prediction requires knowledge of one’s personal contributors); and 3) support evolution between goals. However, participants identified types and hierarchies of goals that our design did not explicitly support, resulting in challenges when people attempted to express their migraine-related goals. For example, some participants initially expressed management goals but then struggled to define corresponding tracking goals. Some also worried about their ability to independently define management or tracking goals that were realistic or feasible. Additional support for defining and differentiating management and tracking goals, and for helping people define realistic subgoals, may help people better understand and navigate these different types and hierarchies of goals.
We also found a need to support evolution within goals, not just between them. People often mentioned wanting to be able to modify their tracking routine as they reflected on their data and gained understanding within a goal. Our configuration process also assumed people would define and then pursue a goal, but some participants discussed the possibility of having retroactive goals. For example, we discussed in Section 5.1.2 that M14 ultimately wanted to learn about her migraines but selected a monitoring goal (Goal 3) because monitoring goals require lower effort. She then additionally chose to track some contributors and wanted to attempt daily tracking. Supposing she did track consistently enough to support learning goals (Goal 1), she may ultimately want to view collected data through learning-specific analyses and visualizations despite not originally selecting that goal type. If a system supported such retroactive goals, people could use their existing collected data in the manner most appropriate for their goals at any given time. Similarly, our design supported before/after tests so people can examine their symptoms before and after making a change, but the current design assumes the change has not yet occurred. By allowing people to indicate a change that happened in the past, a system could support before/after tests even if a person did not explicitly pursue that goal, or retroactively realized they made a change. A system might even automatically detect when a person’s collected data could support goals they have not explicitly configured, giving an option to examine their data in light of other possible goals. Considering goal-directed self-tracking not only as a method to enable progressions from a goal to data to analyses and visualizations, but instead as a framework for reasoning about relationships between goals and data elements, could therefore enable systems that better support data re-use, simultaneous goals, and evolution between goal categories.
6.5. Awareness of Goal Creep During Configuration
Although goal-directed self-tracking helped participants define appropriate tracking goals, Help Me Choose pages also often prompted participants to track more data than they might have otherwise configured. Similarly, although participants proposed configuring a tracking routine that ensured both patient and provider goals were met, such compromises would likely introduce additional tracking. We do not want to discourage people from tracking data they think is necessary for their goals, but attempting to track too many things is a common barrier that can lead to abandonment [14, 23, 31]. Although people may naturally want to add to their tracking routine as they learn, doing so could distract from their primary goals, creating a goal creep that makes their goals too broad to be feasibly pursued. This goal creep seemed particularly likely when people configured automatically-tracked data, which they seemed to consider “free” without associated burdens. However, even automatically-tracked data can introduce burdens (e.g., the necessity to charge and wear a Fitbit, the battery life consequences of location tracking) [33, 38]. To balance a tendency people may have for expanding tracking as they learn about factors that could relate to their migraines, a system should help people understand the burdens associated with additional data. For example, a system could estimate how long a tracking routine would take each day and help a person prioritize and deprioritize data elements until they have a routine they are comfortable pursuing.
Deprioritizing data does not require abandoning it altogether. Many participants wanted support for non-binary lapsing, in which they could decide whether to track specific data elements depending on how they were feeling on a given day. A key opportunity is exploring how a system can support non-binary lapsing that encourages people to track data necessary for their goals. One possibility is dynamically defining subsets of a person’s full tracking routine, allowing them to pursue as complex of a routine as their goals require while minimizing tracking burdens on a day-to-day basis (e.g., narrowing their tracking to focus on symptoms during particularly stressful time periods). Designing for longer-term use, a system could also help people set future goals, starting with a limited tracking routine (e.g., as P2 suggested) and prompting them to add other data elements they are interested in investigating over time. Conversely, a system could also reduce tracking burden by encouraging lapsing after a tracking goal is achieved. A system could thus support the positive aspects of goal creep (e.g., adjusting tracking routines based on educational information or greater understanding developed over time) while avoiding potential pitfalls (e.g., adding burdensome or irrelevant data to track based on overly ambitious or broad recommendations).
6.6. Goal-Directed Self-Tracking in Other Health Domains
Although we focus on migraine, the principles of goal-directed self-tracking likely extend to domains within and beyond chronic condition management. For example, a review of commonly-used diabetes self-management apps found many implicitly support some goals while failing to support others [48]. Some designs were best suited to longer-term data collection to identify trends or to use in a medical appointment, others better supported daily overviews, and a common goal of situated decision support was not well-supported by any of the apps. A goal-directed self-tracking tool in this domain could help people better understand and navigate these goals with their data. Similarly, people with Parkinson’s disease often self-track for a variety of goals that may require different data and representations (e.g., to monitor and plan for the long-term progression, to understand effects of new medications and identify any need for adjustment, to combat denial by providing an objective record) [62]. A recent study of the goals people have for self-experimentation, a form of self-tracking in which people perform n-of-1 experiments to answer specific questions, also identified distinct goals corresponding to different data collection, analysis, and visualization needs that could be supported by goal-directed self-tracking tools [76].
Goal-directed self-tracking could also reduce challenges people encounter when application designers assume certain goals. For example, some menstrual tracking apps assume a pregnancy-related goal, which can be frustrating or painful for people not pursuing that goal [32]. Similarly, people with chronic fatigue syndrome often use activity tracking apps with a goal of limiting their physical activity; however, those apps generally encourage them to be more active, shaming them for activity levels that match their goals [27]. In general, domains in which people self-track for distinct purposes that require different data elements, granularity, frequency, or analysis and visualization could benefit from explicitly expressing and pursuing goals via a goal-directed self-tracking system. Self-tracking not focused on a goal, or in domains where there is less variety in or evolution of goals (e.g., documentary or fetishized tracking [72]), seems less likely to benefit from goal-directed self-tracking.
One important consideration in developing a goal-directed self-tracking system is to determine the set of goals that can be feasibly supported within the domain or tool. Expecting designers to implement every feature needed to support every potential goal is unreasonable, as is requiring people to take the time to explicitly customize all such features. Some goals that people would like to pursue are also infeasible given current technology and knowledge limitations (e.g., no current system could collect and model data to prevent every migraine). In addition, designing support for a specific goal can still be valuable; for example, people with IBS who think a certain nutrient may cause their symptoms and want to perform an self-experiment to establish causality would benefit from TummyTrials [45], a system designed to support exactly that goal. Designers of such a system should not be expected to necessarily include support for all other IBS-related goals. Designs that focus on a subset of goals can nonetheless benefit from a goal-directed perspective by better communicating the set of goals the tool can and cannot support. Where feasible, a tool even could suggest alternative resources for unsupported goals. This support could help people understand the limitations of a system, decide whether the system is a match for their goals, and configure and use the system toward their goals. Such a goal-directed perspective might also help app designers attract people who will actually benefit, leading to higher overall satisfaction with a tool.
7. CONCLUSION
We contribute goal-directed self-tracking, a new method to help people and health providers express and pursue tracking goals they want to pursue for their chronic condition management. Goal-directed self-tracking is designed to support people in deciding what, when, and how to track toward specific goals and to provide analyses and visualizations of the resulting data that support those goals. We reanalyzed data characterizing migraine tracking goals, iteratively designed a paper prototype for a system to support goal-directed self-tracking for migraine management, and used that prototype to conduct interviews with people with migraine and health providers. We found that such a system could elicit many different types and hierarchies of management and tracking goals, help people prepare for all stages of self-tracking, and contribute additional expertise in patient-provider collaboration. We also found pitfalls people may encounter when relying on a system’s expertise or attempting to define and navigate appropriate tracking goals. We present these findings together with design implications for future implementations of goal-directed self-tracking systems, including: 1) the importance of considering all sources of expertise when designing a system that may be considered a member of a patient’s care team; 2) the necessity of supporting evolution between and within different types and hierarchies of goals; and 3) the challenges of goal creep as people configure self-tracking routines and potential approaches to avoiding its negative aspects, such as enabling non-binary lapsing and recommending that some goals be deferred for future pursuit. Finally, we describe how goal-directed self-tracking represents an important design and research opportunity in and beyond chronic condition management. We believe designers of future self-tracking tools that aim to support the specific goals people may have for their data could benefit from this explicit goal-directed perspective.
Supplementary Material
ACKNOWLEDGMENTS
Thanks to Ridley Jones, Yoojung Kim, Sam Kolovson, Esther Chien, and Daniel Epstein for their help with the data analysis; Melissa Schorn and Allison Cole for their help recruiting participants; and Allison Cole, Sonali Mishra, Megan Hofmann, Jane Hoffswell, Daniel Epstein, and the reviewers for their paper feedback. This research was supported in part by the National Science Foundation under awards IIS-1813675, IIS-1553167, and DGE-1256082; the National Institutes of Health under award R01 LM012810; and the National Center For Advancing Translational Sciences of the National Institutes of Health under award UL1 TR002319. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the National Science Foundation.
Contributor Information
JESSICA SCHROEDER, Computer Science & Engineering, University of Washington.
RAVI KARKAR, Computer Science & Engineering, University of Washington.
NATALIA MURINOVA, Headache Clinic, University of Washington.
JAMES FOGARTY, Computer Science & Engineering, University of Washington.
SEAN A. MUNSON, Human Centered Design & Engineering, University of Washington
REFERENCES
- [1].Aarhus Rikke, Ballegaard Stinne Aalokke, and Hansen Thomas Riisgaard. 2009. The eDiary: Bridging Home and Hospital through Healthcare Technology. In The European Conference on Computer-Supported Cooperative Work Springer, 63–83. 10.1007/978-1-84882-854-4_4 [DOI] [Google Scholar]
- [2].Andress-Rothrock Diane, King Wesley, and Rothrock John. 2010. An Analysis of Migraine Triggers in a Clinic-Based Population. Headache: The Journal of Head and Face Pain 50, 8 (2010), 1366–1370. 10.1111/j.1526-4610.2010.01753.x [DOI] [PubMed] [Google Scholar]
- [3].American Gastroenterology Association. 2002. American Gastroenterological Association Medical Position Statement: Irritable Bowel Syndrome. Gastroenterology 123, 6 (2002), 2105 10.1053/gast.2002.37095b [DOI] [PubMed] [Google Scholar]
- [4].Aukerman Glen, Knutson Doug, and Miser William F. 2002. Management of the Acute Migraine Headache. American Family Physician 66, 11 (2002), 2123–2130. https://www.ncbi.nlm.nih.gov/pubmed/12484694 [PubMed] [Google Scholar]
- [5].Ayobi Amid, Marshall Paul, Cox Anna L, and Chen Yunan. 2017. Quantifying The Body and Caring for The Mind: Self-Tracking in Multiple Sclerosis. In Proceedings of the ACM Conference on Human Factors in Computing Systems ACM, 6889–6901. 10.1145/3025453.3025869 [DOI] [Google Scholar]
- [6].Bahensky James A, Jaana Mirou, and Ward Marcia M. 2008. Health Care Information Technology in Rural America: Electronic Medical Record Adoption Status in Meeting the National Agenda. The Journal of Rural Health 24, 2 (2008), 101–105. 10.1111/j.1748-0361.2008.00145.x [DOI] [PubMed] [Google Scholar]
- [7].Ballegaard Stinne Aalokke, Hansen Thomas Riisgaard, and Kyng Morten. 2008. Healthcare in Everyday Life: Designing Healthcare Services for Daily Life. In Proceedings of the ACM Conference on Human Factors in Computing Systems ACM, 1807–1816. http://doi.acm.org/10.1145/1357054.1357336 [Google Scholar]
- [8].Barbarin Andrea M., Saslow Laura R., Ackerman Mark S., and Veinot Tiffany C.. 2018. Toward Health Information Technology that Supports Overweight/Obese Women in Addressing Emotion-and Stress-Related Eating. In Proceedings of the ACM Conference on Human Factors in Computing Systems New York, NY, USA, Article 321, 321:1–321:14 pages. 10.1145/3173574.3173895 [DOI] [Google Scholar]
- [9].Barr Colin, Marois Maria, Sim Ida, Christopher H Schmid Barth Wilsey, Ward Deborah, Duan Naihua, Ron D Hays Joshua Selsky, Servadio Joseph, et al. 2015. The PREEMPT study-Evaluating Smartphone-Assisted n-of-1 Trials in Patients with Chronic Pain: Study Protocol for a Randomized Controlled Trial. Trials 16, 1 (2015), 67 http://doi.org/10/b2h5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Berry Katherine, Salter Amy, Morris Rohan, James Susannah, and Bucci Sandra. 2018. Assessing Therapeutic Alliance in the Context of mHealth Interventions for Mental Health Problems: Development of the Mobile Agnew Relationship Measure (mARM) Questionnaire. Journal of medical Internet research 20, 4 (2018). https://dx.doi.org/10.2196%2Fjmir.8252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Burden Sorrel. 2001. Dietary Treatment of Irritable Bowel Syndrome: Current Evidence and Guidelines for Future Practice. Journal of Human Nutrition and Dietetics 14, 3 (2001), 231–241. https://www.ncbi.nlm.nih.gov/pubmed/11424515 [DOI] [PubMed] [Google Scholar]
- [12].Buyuktur Ayse G, Ackerman Mark S, Newman Mark W, and Hung Pei-Yao. 2017. Design considerations for Semi-Automated Tracking: Self-Care Plans in Spinal Cord Injury. In Proceedings of the 11th EAI International Conference on Pervasive Computing Technologies for Healthcare ACM, 183–192. 10.1145/3154862.3154870 [DOI] [Google Scholar]
- [13].Choe Eun Kyoung, Abdullah Saeed, Rabbi Mashfiqui, Thomaz Edison, Epstein Daniel A, Cordeiro Felicia, Kay Matthew, Abowd Gregory D, Choudhury Tanzeem, Fogarty James, et al. 2017. Semi-Automated Tracking: a Balanced Approach for Self-Monitoring Applications. IEEE Pervasive Computing 16, 1 (2017), 74–84. 10.1109/MPRV.2017.18 [DOI] [Google Scholar]
- [14].Choe Eun Kyoung, Lee Nicole B, Lee Bongshin, Pratt Wanda, and Kientz Julie A. 2014. Understanding Quantified-Selfers’ Practices in Collecting and Exploring Personal Data. In Proceedings of the ACM Conference on Human Factors in Computing Systems ACM, 1143–1152. http://doi.acm.org/10.1145/2556288.2557372 [Google Scholar]
- [15].Chung Chia-Fang, Agapie Elena, Schroeder Jessica, Mishra Sonali, Fogarty James, and Munson Sean A. 2017. When Personal Tracking Becomes Social: Examining the Use of Instagram for Healthy Eating. In Proceedings of the ACM Conference on Human Factors in Computing Systems ACM, 1674–1687. 10.1145/3025453.3025747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Chung Chia-Fang, Cook Jonathan, Bales Elizabeth, Zia Jasmine, and Munson Sean A. 2015. More Than Telemonitoring: Health Provider Use and Nonuse of Life-Log Data in Irritable Bowel Syndrome and Weight Management. Journal of Medical Internet Research 17, 8 (2015), E203 10.2196/jmir.4364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Chung Chia-Fang, Dew Kristin, Cole Allison, Zia Jasmine K, Fogarty James, Kientz Julie A, and Munson Sean A. 2016. Boundary Negotiating Artifacts in Personal Informatics: Patient-Provider Collaboration with Patient-Generated Data. In Proceedings of the ACM Conference on Computer-Supported Cooperative Work and Social Computing http://doi.acm.org/10.1145/2818048.2819926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Chung Chia-Fang, Wang Qiaosi, Schroeder Jessica, Cole Allison, Zia Jasmine, Fogarty James, and Munson Sean A.. 2019. Identifying and Planning for Individualized Change: Patient-Provider Collaboration Using Lightweight Food Diaries in Healthy Eating and Irritable Bowel Syndrome. Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies 3, 1, Article 7 (2019), 27 pages. http://doi.acm.org/10.1145/3314394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Clar Christine, Barnard Katharine D, Cummins Ewen, Royle Pamela, and Waugh Norman. 2010. Self-Monitoring of Blood Glucose in Type 2 Diabetes: Systematic Review. Health Technology Assessment 14, 12 (2010), 1–140. 10.3310/hta14120 [DOI] [PubMed] [Google Scholar]
- [20].Clawson James, Pater Jessica, Miller Andrew D., Mynatt Elizabeth D., and Mamykina Lena. 2015. No Longer Wearing: Investigating The Abandonment of Personal Health-Tracking Technologies on Craigslist. In Proceedings of the ACM Conference on Ubiquitous Computing ACM; 10.1145/2750858.2807554 [DOI] [Google Scholar]
- [21].Consolvo Sunny, Klasnja Predrag, McDonald David W, and Landay James A. 2009. Goal-Setting Considerations for Persuasive Technologies that Encourage Physical Activity. In Proceedings of the 4th international Conference on Persuasive Technology ACM, 8 10.1145/1541948.1541960 [DOI] [Google Scholar]
- [22].Consolvo Sunny, McDonald David W, Toscos Tammy, Chen Mike Y, Froehlich Jon, Harrison Beverly, Klasnja Predrag, Lamarca Anthony, Legrand Louis, Libby Ryan, Smith Ian, and Landay James A. 2008. Activity Sensing in the Wild: A Field Trial of UbiFit Garden. In Proceedings of the ACM Conference on Human Factors in Computing Systems ACM, 1797–1806. 10.1145/1357054.1357335 [DOI] [Google Scholar]
- [23].Cordeiro Felicia, Epstein Daniel A, Thomaz Edison, Bales Elizabeth, Jagannathan Arvind K, Abowd Gregory D, and Fogarty James. 2015. Barriers and Negative Nudges: Exploring Challenges in Food Journaling. In Proceedings of the ACM Conference on Human Factors in Computing Systems ACM, 1159–1162. 10.1145/2702123.2702155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Grave Riccardo Dalle, Calugi Simona, Molinari Enrico, Petroni Maria Letizia, Bondi Mario, Compare Angelo, and Marchesini Giulio. 2005. Weight Loss Expectations in Obese Patients and Treatment Attrition: An Observational Multicenter Study. Obesity Research 13, 11 (2005), 1961–1969. 10.1038/oby.2005.241 [DOI] [PubMed] [Google Scholar]
- [25].Daskalova Nediyana, Desingh Karthik, Jin Young Kim Lixiang Zhang, Papoutsaki Alexandra, and Huang Jeff. 2017. Lessons Learned from Two Cohorts of Personal Informatics Self-Experiments. In Proceedings of the ACM Conference on Ubiquitous Computing, Vol. 1 ACM, 46 10.1145/3130911 [DOI] [Google Scholar]
- [26].Daskalova Nediyana, Danae Metaxa-Kakavouli Adrienne Tran, Nugent Nicole, Boergers Julie, McGeary John, and Huang Jeff. 2016. SleepCoacher: A Personalized Automated Self-Experimentation System for Sleep Recommendations. In Proceedings of the Symposium on User Interface Software and Technology ACM, 347–358. http://doi.org/bwt4 [Google Scholar]
- [27].Davies Tabby, Jones Simon L., and Kelly Ryan M.. 2019. Patient Perspectives on Self-Management Technologies for Chronic Fatigue Syndrome. In Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems Article 222, 13 pages. http://doi.acm.org/10.1145/3290605.3300452 [Google Scholar]
- [28].Deering Mary Jo, Siminerio Erin, and Weinstein Scott. 2013. Issue Brief: Patient-Generated Health Data and Health IT. Office of the National Coordinator for Health Information Technology; (2013). [Google Scholar]
- [29].Elsden Chris, Durrant Abigail C, Chatting David, and Kirk David S. 2017. Designing Documentary Informatics. In Proceedings of the Conference on Designing Interactive Systems ACM, 649–661. 10.1145/3064663.3064714 [DOI] [Google Scholar]
- [30].Epstein Daniel, Cordeiro Felicia, Bales Elizabeth, Fogarty James, and Munson Sean. 2014. Taming Data Complexity in Lifelogs: Exploring Visual Cuts of Personal Informatics Data. In Proceedings of the Conference on Designing Interactive Systems ACM, 667–676. http://doi.acm.org/10.1145/2598510.2598558 [Google Scholar]
- [31].Epstein Daniel A, Caraway Monica, Johnston Chuck, Ping An, Fogarty James, and Munson Sean A. 2016. Beyond Abandonment To Next Steps: Understanding and Designing for Life After Personal Informatics Tool Use. In Proceedings of the ACM Conference on Human Factors in Computing Systems ACM, 1109–1113. 10.1145/2858036.2858045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Epstein Daniel A, Lee Nicole B, Kang Jennifer H, Agapie Elena, Schroeder Jessica, Pina Laura R, Fogarty James, Kientz Julie A, and Munson Sean. 2017. Examining Menstrual Tracking To Inform The Design of Personal Informatics Tools. In Proceedings of the ACM Conference on Human Factors in Computing Systems ACM, 6876–6888. 10.1145/3025453.3025635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Epstein Daniel A, Ping An, Fogarty James, and Munson Sean A. 2015. A Lived Informatics Model of Personal Informatics. In Proceedings of the ACM International Joint Conference on Pervasive and Ubiquitous Computing ACM, 731–742. 10.1145/2750858.2804250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Estrin Deborah and Sim Ida. 2010. Open mHealth Architecture: An Engine for Health Care Innovation. Science 330, 6005 (2010), 759–760. 10.1126/science.1196187 [DOI] [PubMed] [Google Scholar]
- [35].Farmer Aojg, Gibson Oj, Tarassenko L, and Neil A. 2005. A Systematic Review of Telemedicine Interventions To Support Blood Glucose Self-Monitoring in Diabetes. Diabetic Medicine 22, 10 (2005), 1372–1378. 10.1111/j.1464-5491.2005.01627.x [DOI] [PubMed] [Google Scholar]
- [36].The Robert Wood Johnson Foundation. 2014. Personal Data for the Public Good: New Opportunities to Enrich Understanding of Individual and Population Health. Health Data Exploration Project; (2014). http://www.rwjf.org/en/library/research/2014/03/personal-data-for-the-public-good.html [Google Scholar]
- [37].Gulotta Rebecca, Forlizzi Jodi, Yang Rayoung, and Newman Mark Wah. 2016. Fostering Engagement with Personal Informatics Systems. In Proceedings of the ACM Conference on Designing Interactive Systems ACM, 286–300. 10.1145/2901790.2901803 [DOI] [Google Scholar]
- [38].Harrison Daniel, Marshall Paul, Bianchi-Berthouze Nadia, and Bird Jon. 2015. Activity Tracking: Barriers, Workarounds and Customisation. In Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing ACM, 617–621. 10.1145/2750858.2805832 [DOI] [Google Scholar]
- [39].Heinonen Reetta, Luoto Riitta, Lindfors Pirjo, and Nygard Clas-Hakan. 2012. Usability and Feasibility of Mobile Phone Diaries in an Experimental Physical Exercise Study. Telemedicine and E-Health 18, 2 (2012), 115–119. 10.1089/tmj.2011.0087 [DOI] [PubMed] [Google Scholar]
- [40].Henrich Joseph, Heine Steven J, and Norenzayan Ara. 2010. The Weirdest People in the World? Behavioral and Brain Sciences 33, 2–3 (2010), 61–83. 10.1017/S0140525X0999152X [DOI] [PubMed] [Google Scholar]
- [41].Holtzblatt Karen, Wendell Jessamyn Burns, and Wood Shelley. 2004. Rapid Contextual Design: a How-To Guide to Key Techniques for User-Centered Design. Elsevier. [Google Scholar]
- [42].Hsieh Cheng-Kang, Tangmunarunkit Hongsuda, Alquaddoomi Faisal, Jenkins John, Kang Jinha, Ketcham Cameron, Longstaff Brent, Selsky Joshua, Dawson Betta, Swendeman Dallas, et al. 2013. Lifestreams: A Modular Sense-Making Toolset for Identifying Important Patterns from Everyday Life. In Proceedings of the ACM Conference on Embedded Networked Sensor Systems ACM, 5 10.1145/2517351.2517368 [DOI] [Google Scholar]
- [43].Janson Susan L, McGrath Kelly Wong, Covington Jack K, Cheng Su-Chun, and Boushey Homer A. 2009. Individualized Asthma Self-Management Improves Medication Adherence and Markers of Asthma Control. Journal of Allergy and Clinical Immunology 123, 4 (2009), 840–846. https://doi.org/10.10167j.jaci.2009.01.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Jhaveri Mehul and Lee Elizabeth. 2007. Performance of Electronic Diaries in Diabetes Clinical Trials Measured Through Overall Satisfaction of Site Coordinators. Journal of Diabetes Science and Technology 1, 4 (2007), 522–530. 10.1177/193229680700100410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Karkar Ravi, Schroeder Jessica, Epstein Daniel A, Pina Laura R, Scofield Jeffrey, Fogarty James, Kientz Julie A, Munson Sean A, Vilardaga Roger, and Zia Jasmine. 2017. TummyTrials: A Feasibility Study of Using Self-Experimentation To Detect Individualized Food Triggers. In Proceedings of the ACM Conference on Human Factors in Computing Systems ACM, 6850–6863. 10.1145/3025453.3025480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Karkar Ravi, Zia Jasmine, Vilardaga Roger, Mishra Sonali R, Fogarty James, Munson Sean A, and Kientz Julie A. 2015. A Framework for Self-Experimentation in Personalized Health. Journal of the American Medical Informatics Association (2015). 10.1093/jamia/ocv150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Katz Dmitri S., Price Blaine A., Holland Simon, and Dalton Nicholas Sheep. 2018. Data, Data Everywhere, and Still Too Hard to Link: Insights from User Interactions with Diabetes Apps. In Proceedings of the ACM Conference on Human Factors in Computing Systems 503:1–503:12. http://doi.acm.org/10.1145/3173574.3174077 [Google Scholar]
- [48].Katz Dmitri S., Price Blaine A., Holland Simon, and Dalton Nicholas Sheep. 2018. Data, Data Everywhere, and Still Too Hard to Link: Insights from User Interactions with Diabetes Apps. In Proceedings ofthe CHI Conference on Human Factors in Computing Systems http://doi.acm.org/10.1145/3173574.3174077 [Google Scholar]
- [49].Kaye Joseph (Jofish), Mccuistion Mary, Gulotta Rebecca, and Shamma David A. 2014. Money Talks: Tracking Personal Finances. In Proceedings of the ACM Conference on Human Factors in Computing Systems ACM, 521–530. 10.1145/2556288.2556975 [DOI] [Google Scholar]
- [50].Kelman L. 2007. The Triggers or Precipitants of the Acute Migraine Attack. Cephalalgia 27, 5 (2007), 394–402. 10.1111/j.1468-2982.2007.01303.x [DOI] [PubMed] [Google Scholar]
- [51].Kim Young-Ho, Jeon Jae Ho, Lee Bongshin, Choe Eun Kyoung, and Seo Jinwook. 2017. OmniTrack: A Flexible Self-Tracking Approach Leveraging Semi-Automated Tracking. Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies 1, 3 (2017), 67 10.1145/3130930 [DOI] [Google Scholar]
- [52].Lazar Amanda, Koehler Christian, Tanenbaum Joshua, and Nguyen David H. 2015. Why We Use and Abandon Smart Devices. In Proceedings of the ACM International Joint Conference on Pervasive and Ubiquitous Computing ACM, 635–646. 10.1145/2750858.2804288 [DOI] [Google Scholar]
- [53].Lee Jisoo, Walker Erin, Burleson Winslow, Kay Matthew, Buman Matthew, and Hekler Eric B. 2017. Self-Experimentation for Behavior Change: Design and Formative Evaluation of Two Approaches. In Proceedings of the ACM Conference on Human Factors in Computing Systems ACM, 6837–6849. 10.1145/3025453.3026038 [DOI] [Google Scholar]
- [54].Li Ian, Dey Anind, and Forlizzi Jodi. 2010. A Stage-Based Model of Personal Informatics Systems. In Proceedings ofthe ACM Conference on Human Factors in Computing Systems ACM, 557–566. http://doi.acm.org/10.1145/1753326.1753409 [Google Scholar]
- [55].Li Ian, Dey Anind K., and Forlizzi Jodi. 2011. Understanding My Data, Myself: Supporting Self-Reflection with Ubicomp Technologies. In Proceedings of the International Conference on Ubiquitous Computing (UbiComp ‘11) 405–414. http://doi.acm.org/10.1145/2030112.2030166 [Google Scholar]
- [56].Li Ian, Dey Anind K, and Forlizzi Jodi. 2012. Using Context to Reveal Factors that Affect Physical Activity. ACM Transactions on Computer-Human Interaction (TOCHI) 19, 1 (2012), 7 10.1145/2147783.2147790 [DOI] [Google Scholar]
- [57].Lipton Richard B. 2015. Risk Factors for and Management of Medication-Overuse Headache. Continuum: Lifelong Learning in Neurology 21, 4, Headache (2015), 1118–1131. 10.1212/CON.0000000000000216 [DOI] [PubMed] [Google Scholar]
- [58].Luo Yuhan, Liu Peiyi, and Choe Eun Kyoung. 2019. Co-Designing Food Trackers with Dietitians: Identifying Design Opportunities for Food Tracker Customization. In Proceedings of the CHI Conference on Human Factors in Computing Systems ACM, 592 10.1145/3290605.3300822 [DOI] [Google Scholar]
- [59].MacLeod Haley, Jelen Ben, Prabhakar Annu, Oehlberg Lora, Siek Katie, and Connelly Kay. 2016. Asynchronous Remote Communities (ARC) for Researching Distributed Populations. In EAI International Conference on Pervasive Computing Technologies for Healthcare http://dLacm.org/citation.cfm?id=3021319.3021320 [Google Scholar]
- [60].Maizels Morris. 1998. The Clinician’s Approach To The Management of Headache. Western Journal of Medicine 168, 3 (1998), 203 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1304871/ [PMC free article] [PubMed] [Google Scholar]
- [61].Mamykina Lena, Heitkemper Elizabeth M, Smaldone Arlene M, Kukafka Rita, Cole-Lewis Heather J, Davidson Patricia G, Mynatt Elizabeth D, Cassells Andrea, Tobin Jonathan N, and Hripcsak George. 2017. Personal Discovery in Diabetes Self-Management: Discovering Cause and Effect Using Self-Monitoring Data. Journal of biomedical informatics 76 (2017), 1–8. 10.1016/j.jbi.2017.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Mishra Sonali R., Klasnja Predrag, Woodburn John MacDuffie, Eric B. Hekler, Omberg Larsson, Kellen Michael, and Mangravite Lara. 2019. Supporting Coping with Parkinson’s Disease Through Self Tracking. In Proceedings of the CHI Conference on Human Factors in Computing Systems Article 107, 16 pages. http://doi.acm.org/10.1145/3290605.3300337 [Google Scholar]
- [63].Munson Sean A and Consolvo Sunny. 2012. Exploring Goal-Setting, Rewards, Self-Monitoring, and Sharing to Motivate Physical Activity. In International Conference on Pervasive Computing Technologies for Healthcare 10.4108/icst.pervasivehealth.2012.248691 [DOI] [Google Scholar]
- [64].Niess Jasmin and Wozniak Pawel W.. 2018. Supporting Meaningful Personal Fitness: The Tracker Goal Evolution Model. In Proceedings of the ACM Conferenceon Human Factors in Computing Systems Article 171,171:1–171:12 pages. http://doi.acm.org/10.1145/3173574.3173745 [Google Scholar]
- [65].Ong Lucille ML, De Haes Johanna CJM, Hoos Alaysia M, and Lammes Frits B. 1995. Doctor-Patient Communication: A Review of the Literature. Social Science &Medicine 40, 7 (1995), 903–918. https://www.ncbi.nlm.nih.gov/pubmed/7792630 [DOI] [PubMed] [Google Scholar]
- [66].World Health Organization. 2018. Integrated Chronic Disease Prevention and Control. http://www.who.int/chp/about/integrated_cd/en/
- [67].Park Sun Young and Chen Yunan. 2015. Individual and Social Recognition: Challenges and Opportunities in Migraine Management. In Proceedings of the ACM Conference on Computer Supported Cooperative Work & Social Computing ACM, 1540–1551. 10.1145/2675133.2675248 [DOI] [Google Scholar]
- [68].Raj Shriti, Lee Joyce M, Garrity Ashley, and Newman Mark W. 2019. Clinical Data in Context: Towards Sensemaking Tools for Interpreting Personal Health Data. Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies 3, 1 (2019), 22 10.1145/3314409 [DOI] [Google Scholar]
- [69].Raj Shriti, Newman Mark W., Lee Joyce M., and Ackerman Mark S.. 2017. Understanding Individual and Collaborative Problem-Solving with Patient-Generated Data: Challenges and Opportunities. Proceedings of the ACM on Human-Computer Interaction (2017), 88:1–88:18. http://doi.acm.org/10.1145/3134723 [Google Scholar]
- [70].Rasmussen Birthe Krogh, Jensen Rigmor, Schroll Marianne, and Olesen Jes. 1991. Epidemiology of Headache in a General Population—A Prevalence Study. Journal of Clinical Epidemiology 44, 11 (1991), 1147–1157. https://www.ncbi.nlm.nih.gov/pubmed/1941010 [DOI] [PubMed] [Google Scholar]
- [71].Reading Meghan J and Merrill Jacqueline A. 2018. Converging and Diverging Needs between Patients and Providers who are Collecting and Using Patient-Generated Health Data: An Integrative Review. Journal of the American Medical Informatics Association 25, 6 (2018), 759–771. 10.1093/jamia/ocy006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Rooksby John, Rost Mattias, Morrison Alistair, and Chalmers Matthew Chalmers. 2014. Personal Tracking As Lived Informatics. In Proceedings of the ACM Conference on Human Factors in Computing Systems ACM, 1163–1172. 10.1145/2556288.2557039 [DOI] [Google Scholar]
- [73].Rudd Jim, Stern Ken, and Isensee Scott. 1996. Low vs. High-Fidelity Prototyping Debate. Interactions 3, 1 (1996), 76–85. 10.1145/223500.223514 [DOI] [Google Scholar]
- [74].Schroeder Jessica, Chung Chia-Fang, Epstein A. Daniel, Karkar Ravi, Parsons Adele, Murinova Natalia, Fogarty James, and Munson Sean A.. 2018. Examining Self-Tracking by People with Migraine: Goals, Needs, and Opportunities in a Chronic Health Condition. In Designing Interactive Systems. 135–148. 10.1145/3196709.3196738 [DOI] [Google Scholar]
- [75].Schroeder Jessica, Hoffswell Jane, Chung Chia-Fang, Fogarty James, Munson Sean, and Zia Jasmine. 2017. Supporting Patient-Provider Collaboration To Identify Individual Triggers Using Food and Symptom Journals. In Proceedings of the ACM Conference on Computer-Supported Cooperative Work & Social Computing ACM, 1726–1739. 10.1145/2998181.2998276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Schroeder Jessica, Karkar Ravi, Fogarty James, Kientz Julie A., Kay Matthew, and Munson Sean A.. 2018. A Patient-Centered Proposal for Bayesian Analysis of Self-Experiments for Health. In Journal of Healthcare Informatics Research. 10.1007/s41666-018-0033-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Schroeder Jessica, Wilks Chelsey, Rowan Kael, Toledo Arturo, Paradiso Ann, Czerwinski Mary, Mark Gloria, and Linehan Marsha M.. 2018. Pocket Skills: A Conversational Mobile Web App To Support Dialectical Behavioral Therapy. In Proceedings of the ACM Conference on Human Factors in Computing Systems 398 10.1145/3173574.3173972 [DOI] [Google Scholar]
- [78].Silberstein Stephen D and The US Headache Consortium. 2000. Practice Parameter: Evidence-Based Guidelines for Migraine Headache (An Evidence-Based Review) Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 55, 6 (2000), 754–762. 10.1212/WNL.55.6.754 [DOI] [PubMed] [Google Scholar]
- [79].Solomon GD and Price KL. 1997. Burden of Migraine. Pharmacoeconomics 11, 1 (1997), 1–10. 10.2165/00019053-199700111-00003 [DOI] [PubMed] [Google Scholar]
- [80].Stewart Moira A. 1995. Effective Physician-Patient Communication and Health Outcomes: A Review. CMAJ: Canadian Medical Association Journal 152, 9 (1995),1423 https://www.ncbi.nlm.nih.gov/pubmed/7728691 [PMC free article] [PubMed] [Google Scholar]
- [81].Stewart Walter F, Lipton Richard B, Whyte J, Dowson A, Kolodner K, Liberman JN, and Sawyer J. 1999. An International Study to Assess Reliability of the Migraine Disability Assessment (MIDAS) Score. Neurology 53, 5 (1999), 988–988. 10.1212/WNL.53.5.988 [DOI] [PubMed] [Google Scholar]
- [82].Still Brian and Morris John. 2010. The Blank-Page Technique: Reinvigorating Paper Prototyping in Usability Testing. IEEE Transactions on Professional Communication 53, 2 (2010), 144–157. 10.1109/TPC.2010.2046100 [DOI] [Google Scholar]
- [83].Storni Cristiano. 2011. Complexity in an Uncertain and Cosmopolitan World. Rethinking Personal Health Technology in Diabetes with The Tag-It-Yourself. PsychNology Journal 9, 2 (2011), 165–185. [Google Scholar]
- [84].Ward Thomas N. 2012. Migraine Diagnosis and Pathophysiology. Continuum: Lifelong Learning in Neurology 18, 4, Headache (2012), 753–763. 10.1212/01.CON.0000418640.07405.31 [DOI] [PubMed] [Google Scholar]
- [85].West Peter, Giordano Richard, Van Kleek Max, and Shadbolt Nigel. 2016. The Quantified Patient in the Doctor’s Office: Challenges & Opportunities. In Proceedings of the ACM Conference on Human Factors in Computing Systems ACM, 3066–3078. http://doi.acm.org/10.1145/2858036.2858445 [Google Scholar]
- [86].West Peter, Max Van Kleek Richard Giordano, Weal Mark, and Shadbolt Nigel. 2017. Information Quality Challenges of Patient-Generated Data in Clinical Practice. Frontiers in Public Health 5 (2017), 284 https://dx.doi.org/10.3389%2Ffpubh.2017.00284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].West Peter, Van Kleek Max, Giordano Richard, Weal Mark J., and Shadbolt Nigel. 2018. Common Barriers to the Use of Patient-Generated Data Across Clinical Settings. In Proceedings of the ACM Conference on Human Factors in Computing Systems 484 http://doi.acm.org/10.1145/3173574.3174058 [Google Scholar]
- [88].Yorkston Kathryn, Johnson Kurt, Klasner Estelle, Amtmann Dagmar, Kuehn Carrie, and Dudgeon Brian. 2003. Getting the Work Done: A Qualitative Study of Individuals with Multiple Sclerosis. Disability and Rehabilitation 25, 8 (2003), 369–379. 10.1080/0963828031000090506 [DOI] [PubMed] [Google Scholar]
- [89].Zhu Haining, Colgan Joanna, Reddy Madhu, and Choe Eun Kyoung. 2016. Sharing Patient-Generated Data in Clinical Practice: An Interview Study. Proceedings of the American Medical Informatics Association (2016), 1303–1312. https://www.ncbi.nlm.nih.gov/pubmed/28269928 [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


