Abstract
Introduction
Despite 40 randomised controlled trials (RCTs) investigating preoperative oral antibiotics (OA) and mechanical bowel preparation (MBP) to reduce surgical site infection (SSI) rate following colon surgery, there has never been an RCT published comparing OA alone versus no preparation. Of the four possible regimens (OA alone, MBP alone, OA plus MBP and no preparation), randomised evidence is conflicting for studied groups. Furthermore, guidelines vary, with recommendations for OA alone, OA plus MBP or no preparation. The National Surgical Quality Improvement Program (NSQIP) has automated data collection for surgical patients. Similarly, the ‘REthinking Clinical Trials’ (REaCT) platform increases RCT enrolment by simplifying pragmatic trial design. In this novel RCT protocol, we combine REaCT and NSQIP to compare OA alone versus no preparation for SSI rate reduction in elective colon surgery. To our knowledge, this is the first published RCT protocol that leverages NSQIP for data collection. In our feasibility study, 67 of 74 eligible patients (90%) were enrolled and 63 of 67 (94%) were adherent to protocol. The ‘REaCT–NSQIP’ trial design has great potential to efficiently generate level I evidence for other perioperative interventions.
Methods and analysis
SSI rates following elective colorectal surgery after preoperative OA or no preparation will be compared. We predict 45% relative rate reduction of SSI, improvement in length of stay, reduced costs and increased quality of life, with similar antibiotic-related complications. Consent, using the ‘integrated consent model’, and randomisation on a mobile device are completed by the surgeon in a single clinical encounter. Data collection for the primary end point is automatic through NSQIP. Analysis of cost per weighted case, cost utility and quality-adjusted life years will be done.
Ethics and dissemination
This study is approved by The Ontario Cancer Research Ethics Board. Results will be disseminated in surgical conferences and peer-reviewed journals.
Trial registration number
NCT03663504; Pre-results, recruitment phase.
Keywords: colorectal surgery, clinical trials, wound management, infection control, statistics & research methods
Strengths and limitations of this study.
The intervention groups in this randomised controlled trial (oral antibiotics (OA) alone and no preparation) have never been directly compared in a prospective, randomised trial.
The REthinking Clinical Trials (REaCT) design with integrated oral consent and web-based randomisation dramatically improves enrolment of eligible patients.
The use of validated and established automatic data collection methods via National Surgical Quality Improvement Program (NSQIP) maximises trial efficiency and reduces cost.
Only two standard-of-care perioperative interventions, for which there is clinical equipoise, can be compared in the REaCT–NSQIP trial design.
The number of eligible patients limits the study power necessary to perform a three-arm trial of OA plus mechanical bowel preparation, OA alone and no preparation—interventions not directly compared in historical trials.
Introduction
Surgical site infections after elective colon surgery are frequent, serious and costly. Approximately 20% of patients undergoing colorectal surgery will suffer from surgical site infection (SSI).1 2 SSIs are associated with significant morbidity, 7–10 days increased length of stay (LOS),3 twofold to threefold higher healthcare costs3–5 and mortality.6 In addition to standard-of-care intravenous antibiotic (IVA) prophylaxis, there are four possible bowel preparation regimens for SSI prevention prior to colorectal surgery: (1) oral antibiotics (OA) alone, (2) mechanical bowel preparation (MBP) alone, (3) OA plus MBP and (4) no preparation. In previous studies, OA includes three doses of oral neomycin and metronidazole given the day before surgery.7–9 MBP commonly refers to either oral polyethylene glycol or sodium phosphate solution to cleanse the entire colon.10–13 Both interventions are aimed at reducing the faecal bacterial load, theoretically preventing SSI after colon resection.
Despite over 40 randomised controlled trials (RCTs), there is still clinical equipoise regarding the optimal preoperative bowel preparation regimen to prevent SSI after colon surgery. For example, The American Society of Colon and Rectal Surgeons,14 WHO15 and American College of Surgeons16 recommend OA plus MBP. The WHO cites an absence of randomised evidence regarding the use of OA alone, while the American College of Surgeons does not recommend OA alone. Additionally, the Canadian Society of Colorectal Surgeons17 and the UK National Institute for Health and Care Excellence18 recommend against the use of MBP, without specific mention of the role of OA.
Historically, the use of MBP prior to colon surgery was common. This rationale was based on consensus opinion assuming an association between reducing faecal bacterial load and the incidence of SSI.19–21 Since that time, a series of retrospective studies, followed by RCTs questioned the benefit of MBP. At present, a total of 13 published RCTs,10 12 13 22–31 8 meta-analyses32–39 and a Cochrane review40 have confirmed that there is no statistically significant evidence that elective colon surgery patients benefit from preoperative MBP alone, and in fact MBP may be associated with an increased SSI rate.25 30 Furthermore, MBP is associated with significant side effects, including abdominal pain and bloating (12%–22%),41 electrolyte disturbances (28%)42 43 and dehydration, particularly in patients greater than 60 years old,44 which is the median age of elective colon surgery patients.45
During the same time period, OA were added to MBP in an effort to further reduce the faecal bacterial load. In the 1970s, Clarke and colleagues completed a series of clinical trials comparing MBP plus or minus OA versus MBP plus IV antibiotics, concluding OA to be important in SSI prevention.19 46–48 In 1969, Polk et al published a landmark paper showing the benefit of IV antibiotic prophylaxis in intestinal surgery,49 a finding that has been extensively replicated.50 Thereafter, OA fell out of favour, replaced by IVA, despite an absence of high-quality randomised evidence to support the elimination of OA from the preoperative regimen.9
More recently, there has been a resurgence of interest in OA to reduce SSI incidence after colon surgery. For instance, three meta-analyses of 7, 11 and 14 RCTs, respectively, demonstrated a reduction in SSI rate of approximately 45% with the use of OA plus MBP as compared with MBP alone.51–53 Additionally, a recent network meta-analysis of relevant RCTs has also suggested an SSI rate reduction for OA plus MBP as compared with MBP alone. In the absence of direct RCT comparisons, this meta-analysis suggests a reduced rate of SSI for the OA group as compared with no preparation, and possible equivalence of the OA and OA plus MBP groups.54 Remarkably, of the four possible bowel preparation regimens aimed at reducing SSI rate before colon surgery, there has never been an RCT published comparing OA alone with no preparation. Furthermore, there is only a single, recent RCT comparing OA plus MBP with no preparation, which reported no significant difference in SSI rate.7 This highlights a significant gap in the level I evidence comparing OA alone or OA plus MBP versus no preparation for SSI prevention after colon surgery. Retrospectively, two large studies from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) (>30 000 patients) and one large meta-analysis of prospective studies (69 000 patients) have confirmed that many centres are using OA alone as a standard of care for colorectal surgery patients.45 55 56 These studies suggested that OA alone is associated with similar SSI rates to OA plus MBP, and lower SSI rates as compared with both MBP alone and no preparation. Additionally, the rate of antibiotic resistance or Clostridium difficile infection is similar between the OA alone, no preparation and OA plus MBP groups.57 It is important to note that in all relevant studies, appropriate IVA prophylaxis was administered, and this continues to be the standard practice for all patients.
To summarise the randomised evidence: (1) no preparation is favoured to MBP alone and (2) OA plus MBP is favoured to MBP alone. Based on this, and the retrospective evidence that OA containing regimens yield lower SSI rates versus no preparation, some experts have advocated for a shift in practice from no preparation to OA alone, ostensibly reducing SSI rates, while avoiding the side effects of MBP.
This is a provocative hypothesis without supporting randomised evidence which warrants evaluation in a well-designed RCT. The trial protocol reported here will fill that crucial knowledge gap.
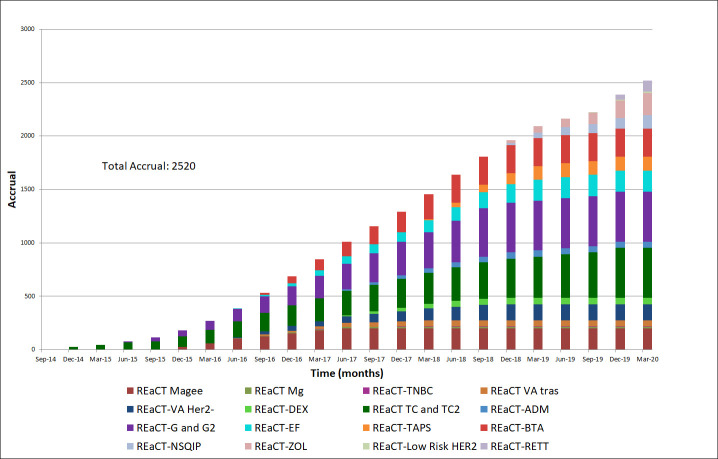
REthinking Clinical Trials (REaCT) is a streamlined pragmatic trial platform designed to address falling numbers in clinical trial enrolment.58 In Canada, less than 5.8% of eligible cancer patients are enrolled in clinical trials.59 Aimed at comparing two standard-of-care interventions for which there is known clinical equipoise, the REaCT platform streamlines trial conduct using an ‘integrated consent model’, practical data capture and web-based randomisation.60 First conceptualised at The Ottawa Hospital, the REaCT programme has been highly successful at overcoming regulatory and financial barriers—to date there are over 15 ongoing REaCT studies, with >2500 patients randomised in just 5 years61 (figure 1). On average, ≈80% of eligible patients participate in REaCT, far above the enrolment rates for eligible cancer patients in Canada.59 Given the clinical equipoise between the two standard-of-care interventions (OA alone vs no preparation) compared in this trial, the REaCT platform is well suited to investigate this perioperative intervention.
Figure 1.
The REaCT platform has been highly successful over the past 5 years, with 15 completed or ongoing pragmatic trials and over 2500 patients enrolled to date (April 2020). NSQIP, National Surgical Quality Improvement Program; REaCT, REthinking Clinical Trials.
Standardised quality improvement infrastructure such as NSQIP and Enhanced Recovery After Surgery (ERAS) have become integral to perioperative care. ERAS is a widely adopted, multimodal programme of perioperative interventions, supported by level I evidence.62 63 These interventions can accelerate recovery, decrease complications and result in earlier discharge. Often, the quality metrics and outcomes of the ERAS programme are measured through data collected as part of the NSQIP.64 NSQIP is the leading, validated, risk-adjusted outcome measurement programme aimed at improving the quality of surgical care in North America.65 Using trained surgical clinical reviewers (SCRs), NSQIP centres collect perioperative data from the medical record, including clinical variables, procedure data and 30-day outcomes. Currently, more than 600 hospitals in the world and 47 Ontario hospitals participate in NSQIP.65–67 Infrastructure such as NSQIP and ERAS present an opportunity to collect data not only for quality improvement initiatives, but also for perioperative pragmatic trials. In this novel REaCT–NSQIP trial design, we have leveraged the ease and rigour of real-time data collection through NSQIP and combined it with the streamlined trial methodology of REaCT. To our knowledge, this is the first published RCT protocol to have used NSQIP in this fashion. The REaCT–NSQIP design could easily be adopted at other centres as an efficient way to generate level I evidence for other perioperative quality improvement strategies.
Our institution has completed a single-centred feasibility study from October 2018 to June 2019 with a primary end point of >80% enrolment and >80% adherence to treatment for eligible patients. Secondary end points include >90% automatic NSQIP data capture and <5% loss to follow-up. Over the 8-month period, the study demonstrated remarkable enrolment of 67 of 74 eligible patients (90%). Only four patients were non-compliant (94% protocol compliance) (figure 2). There were zero losses to follow-up for the primary end point. NSQIP automatic data capture was successful 100% of the time. Having exceeded our benchmark for feasibility, we have undertaken a multicentre trial at four other high-volume hospitals. In this novel, multicentre, pragmatic RCT, we will compare SSI rates in elective colon surgery patients for preoperative OA alone versus no preparation. By combining the REaCT platform with automatic NSQIP data collection, the REaCT–NSQIP protocol is a model for randomised trial efficiency (figure 3). The successful completion of this trial will highlight the potential for the REaCT–NSQIP design to improve the value and quality of surgical care by efficiently generating level I evidence for other perioperative interventions.
Figure 2.
Cumulative total of eligible versus enrolled patients in the 8-month, single centred, REaCT–NSQIP feasibility trial. In our pilot feasibility trial at The Ottawa Hospital, we enrolled 67 patients over 8 months, out of a total of 74 eligible patients (>90% enrolment rate). Adherence to preoperative OA as per protocol was 94%. NSQIP, National Surgical Quality Improvement Program; OA, oral antibiotics; RCT, randomised controlled trial; REaCT, REthinking Clinical Trials.
Figure 3.
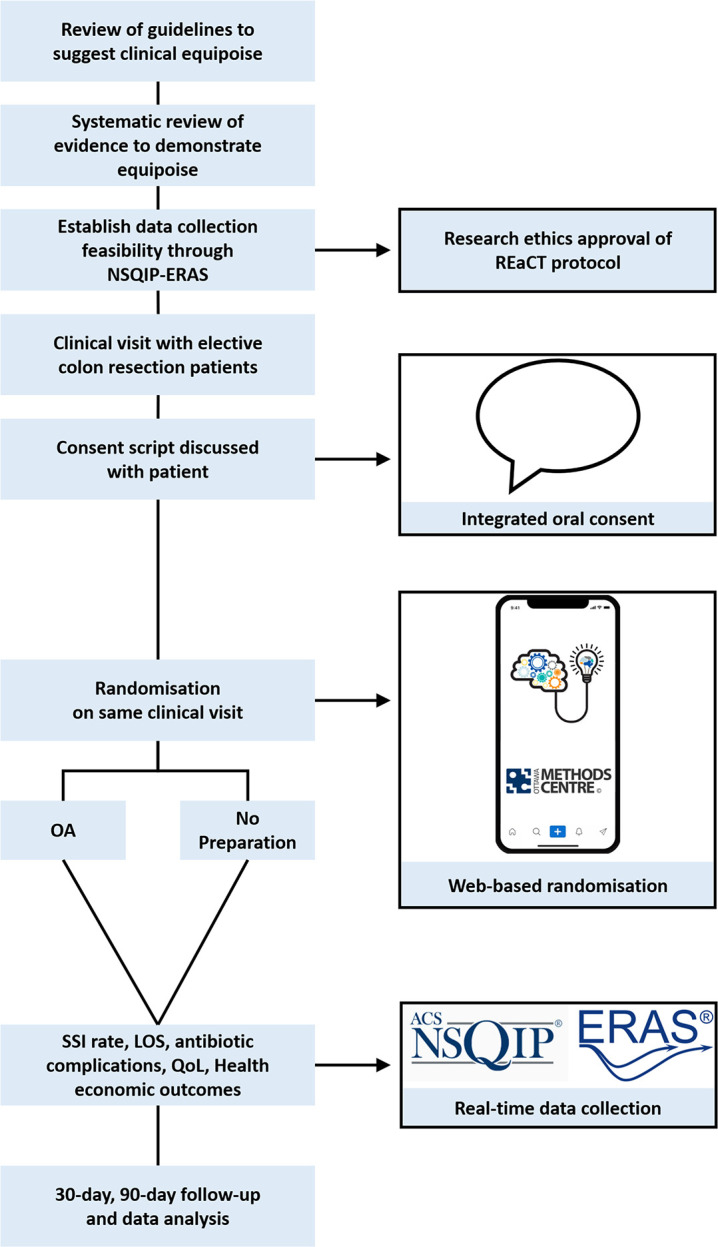
REaCT–NSQIP trial enrolment flow chart highlighting the integrated oral consent, web-based randomisation and automatic data collection through NSQIP–ERAS. *Adapted from Hilton et al58. ERAS, Enhanced Recovery After Surgery; LOS, length of stay; NSQIP, National Surgical Quality Improvement Program; QoL, quality of life; REaCT, REthinking Clinical Trials; SSI, surgical site infection.
Methods and analysis
Study design
The REaCT–NSQIP trial is a multicentre, prospective, single-blinded, pragmatic RCT comparing OA alone versus no preparation for surgical site infection rates in elective colon surgery. The novel REaCT–NSQIP design embeds the research question in clinical practice, controlling only the studied intervention, increasing the generalisability of the trial results.
Intervention
Patients will be randomised to either:
ARM A—no preparation
or
ARM B—OA alone; neomycin and metronidazole, 1 g of each, administered at 13:00, 15:00 and 20:00 hours the day before surgery.
Both arms will receive pre-incision IVA prophylaxis according to the standard of care at the treating centre. Neither arm will receive a MBP.
Hypothesis
The use of OA alone compared with no preparation will result in a 45% relative risk reduction of SSI, with an associated decrease in postoperative LOS, hospital costs and increased patient quality of life (QoL), with no increase in antibiotic-related adverse events.
Study population
All patients 18 years or older undergoing elective colon resection (partial or total colectomy with or without anastomosis, or abdominal perineal resection) at participating NSQIP centres will be eligible for enrolment. Patients will be excluded if they cannot provide oral consent; OAs are contraindicated (ie, adverse or allergic reaction); an active infection requiring antibiotics is present; there is a requirement for MBP (rectal resection with anastomosis, transanal excision, intraoperative colonoscopy or surgeon discretion) or they are undergoing emergency colon surgery with no opportunity to administer OA the day before surgery.
Screening, consent and randomisation
Patients will be screened, consented and randomised using the REaCT platform during the clinical encounter when consent for surgery is obtained. Informed consent for trial participation will be verbally obtained by the surgical team (online supplementary appendix 1) and documented directly in the medical record as part of the visit note (online supplementary appendix 2). The patient is then given a copy of the consent template. This method of oral trial consent is called the integrated consent model and is one of the hallmarks of the REaCT platform. Importantly, the integrated consent model negates the need for separate points of contact to enrol and randomise patients. Site-stratified, permuted-block randomisation of eligible and consented patients is done in real time, in the clinic, through a secure, web-based interface on the surgeon’s or REaCT coordinator’s mobile device. Through a web-based checklist on the REaCT interface, eligibility criteria are ensured, a study ID is automatically generated and the patient is administratively enrolled. Randomisation and group allocation occur immediately. Patients in the OA arm receive a prescription and instructions on administration of preoperative OAs.
bmjopen-2020-036866supp001.pdf (195.5KB, pdf)
bmjopen-2020-036866supp002.pdf (95.9KB, pdf)
Study outcomes and data collection
Primary outcome
The primary outcome of this study is a reduction in SSI rate at 30 days postoperatively (the time frame for perioperative data collection through NSQIP).
Secondary outcomes
The secondary outcomes of this study are LOS, incidence of C. difficile infection at 90 days, antibiotic-resistant infectious complications at 30 days, QoL, incremental cost-effectiveness ratio and incidence of subgroup infectious complications at 30 days (deep SSI, superficial SSI, organ space SSI, anastomotic leak and non-SSIs).
The primary and secondary outcomes, as well as all other relevant clinical variables will be extracted from the NSQIP-linked clinical or administrative chart by trained, blinded SCRs at NSQIP centres. These data are collected automatically regardless of trial enrolment, as a part of NSQIP. Secondary outcomes not collected by NSQIP will be retrieved from the clinical chart via a custom algorithm and linked to the NSQIP data. Patient compliance with OA and determination of antibiotic-related side effects will be ascertained by a clinical research assistant (CRA). To minimise bias, patients in both groups will be asked open-ended questions by telephone regarding symptoms on the day before surgery. The patient reported QoL, measured using the SF-36 and EQ-5D-5L questionnaire at baseline and at 30 days postoperatively, will also be collected by a CRA.68 69 In keeping with the pragmatic nature of the study, trial follow-up will be no different than standard surgical follow-up that occurs at 4–6 weeks.
Data analysis
The data analysis will be undertaken by the Ottawa Methods Centre. A report will also be generated after enrolment of 100 patients each to be reviewed by the Data Safety Monitoring Board (DSMB).
Projected reduction in SSI rate and sample size calculation
Based on the published data, we estimate a 45% relative reduction in SSI rates with preoperative OA alone as compared with the no preparation group.45 51–53 57 70 With the NSQIP Ontario Collaborative (NSQIP-ON) SSI rate for colorectal patients at 13%,64 a sample size of 828 patients (414 patients per arm) provides 80% power to detect a 45% relative risk reduction (two-sided α 5%). Given the >99% 30-day follow-up rate of colorectal cases in Ontario NSQIP centres in 2016–2017, we expect <5% loss to follow-up.
The sample size will be reassessed at ½ trial accrual using the NSQIP-ON Collaborative SSI rate, thereby avoiding an interim analysis. NSQIP-ON is a group of >40 hospitals in Ontario, Canada which collect data via NSQIP and publish yearly reports of quality improvement metrics including SSI rate for colon surgery. Centres participating in the REaCT–NSQIP multicentre trial are members of NSQIP-ON. Consequently, the NSQIP-ON SSI rate is taken from a significantly larger patient population, which includes, but is not limited to, the sample of patients participating in the REaCT–NSQIP trial.
Reduction in LOS
Given the current sample size, based on a mean LOS of 7.2 days (SD 5.0),64 this study has an >80% power to detect an absolute decrease of 1.0 days in mean LOS.
Patient-reported QoL
The SF-36 has been validated as a measure of postoperative recovery in patients undergoing colorectal surgery.69 71 The EQ-5D-5L allows direct estimation of health utility values.68 72 Baseline and postoperative scores will be compared using the standardised response means, and the magnitude of the postoperative change will be considered in relation to the minimal clinically important difference, which represents the smallest change that would influence patient management.73 74
C. difficile and antibiotic resistance complications
NSQIP data will be linked to postoperative C. difficile, antibiotic sensitivity results and antibiotic resistance complications and these will be directly compared between the two study arms.
Descriptive analysis
Baseline characteristics of each treatment group will be presented as means (continuous measures) or proportions (categorical or ordinal data) with 95% CIs.
Intention-to-treat analysis
All statistical analyses will be done in an intention-to-treat fashion, based on all subjects who underwent randomisation. Additionally, a per-protocol analysis of the primary and secondary outcomes based on treatment received will be conducted.
Analysis of primary outcomes
The primary outcome (incidence of SSI) will be measured dichotomously as a combination of deep and superficial SSI. The risk difference will be calculated with a 95% CI.
Analysis of secondary outcomes
Relative risk and mean differences will be calculated and presented with 95% CIs. This will include a subgroup analysis of deep, superficial, organ space and non-SSI rates if event number allows.
Health economic analysis
Using individual case costing, we will compare the total cost per weighted case between the groups. Given that the fiscal year 2015/2016 mean total cost per weighted case at our local centre was $C7133 (SD $C636) and case weight 2.75, we have >90% power to detect a cost saving of $C190 per weighted case ($C522 per patient). A cost-utility analysis will be also conducted from a perspective of the publicly funded healthcare system. Specifically, the costs and health outcomes including the number of SSI cases prevented and quality-adjusted life years (QALYs) will be compared. Analysis will incorporate data on efficacy, resource use and patients’ utility values up to 3 months postsurgery. QALYs will be estimated for each patient within the clinical trial using the total area under the curve method.75 76 The incremental cost and QALYs gained will be estimated using regression analysis. Uncertainty in the analysis will be addressed by estimating 95% CIs using a non-parametric bootstrapping method. Results from bootstrapping will also be used to depict cost-effectiveness acceptability curves, which link the probability of the intervention being cost-effective over a range of potential threshold values (λ) that the health system may be willing to pay for an additional unit of effect. The cost-effectiveness analysis will adhere to the best practices for conducting and reporting of health economic evaluations.77
Compliance and loss to follow-up
Secondary analyses will be considered to understand the influence of compliance and losses to follow-up on the robustness of the intention-to-treat analysis. In general, a per-protocol analysis of primary and secondary outcomes will be performed and compared with the intention-to-treat analysis. Due to the pragmatic nature of the REaCT–NSQIP trial, the aim of this study is assessing utility of the intervention in a real-world setting. Consequently, it is imperative that methods to improve compliance not be specific to the clinical trial setting (eg, a CRA phone call reminder that would happen only within the context of the trial, but not during routine clinical care). The trial does, however, use information sheets similar to teaching brochures that are commonly provided to patients as part of routine surgical care.
Data storage, custodianship and availability
Data will be anonymised with study ID, stored, encrypted and password-protected at The Ottawa Hospital Research Institute, REaCT section. It will be accessible to the Ottawa Methods Centre, the DSMB and study authors involved in data interpretation, analysis and knowledge translation. Raw, anonymised data will be kept for a total of 10 years. Any data with identifying information will be securely destroyed 1 year after study completion. Technical appendix, statistical code and data set will be available by specific request through The Ottawa Hospital Research Institute and Ottawa Methods Centre (Trial: OTT18-03 REaCT–NSQIP, methodscentre@toh.ca).
Study timeline
Enrolment
Four external participating high-volume Ontario hospitals have completed site administrative enrolment in the REaCT–NSQIP study reported here. Enrolment of patients at external sites is anticipated in 2020. Given that current enrolment at the primary site is 130 patients, and projected external site enrolment ranges from 50 to 100 patients/year, we anticipate full trial enrolment (828 patients) in 2023 (figure 4).
Figure 4.
The REaCT–NSQIP single-centred feasibility study was completed in Q2 2019. Given that the statistical power of the study is dependent on the baseline SSI rate across participating sites, the SSI rate of the NSQIP-ON Collaborative (which includes >40 hospitals in the trial region of Ontario) will be reassessed at the midpoint of trial enrolment (≈Q3 2021), allowing for adjustment of the final sample size. NSQIP, National Surgical Quality Improvement Program; REaCT, REthinking Clinical Trials; SSI, surgical site infection.
Analysis, interpretation and knowledge translation
Data extraction, transfer, cleaning and locking and analysis will begin 4 months after the last patient undergoes surgical intervention, allowing for 30-day and 90-day follow-up. Analysis by The Ottawa Methods Centre (primary and secondary outcomes) and the Ottawa Hospital Research Institute (economic and QoL outcomes) will be completed thereafter. Interpretation, knowledge translation and publication will be completed by 2024.
REaCT–NSQIP trial steering committee
The REaCT–NSQIP Trial Steering Committee consists of the principal investigator, co-investigators, colorectal surgeons, a statistician and patient with lived experience. This body has international experts in perioperative trial design, clinical trials, the REaCT platform, statistical analysis and methodology, NSQIP, colorectal surgery, infectious diseases and economic analysis. The steering committee will oversee adherence to the protocol and monitor trial progress, safety and protocol amendments. Persons who attend committee meetings, but do not vote, include the REaCT CRAs. The committee will meet under the following circumstances: (1) at trial start-up, quarterly via teleconference, (2) at external site initiation and (3) if unforeseen problems arise affecting trial progress. The trial sponsor (The Ottawa Hospital Research Institute) will oversee the DSMB, which is independent of trial investigators. This board will consist of internal and external reviewers, facilitated by the trial sponsor.
Patient and public involvement
This protocol is based on the REaCT pragmatic trial design. The REaCT methodology addresses clinical questions for which there is equipoise identified by both the treating physicians and the participating patient population. The conduct of this study, including the usage of the integrated consent model, was developed in conjunction with patient stakeholders. Moreover, REaCT is focused on selecting outcomes that have demonstrated value to patients.58 In the current study, the primary outcome measure (SSI rate) is a quality improvement target identified by Health Quality Ontario (HQO) (https://www.hqontario.ca). HQO is a provincial advisor on health quality issues which directly involves patients in its leadership, mandate, structure and strategic plan. Furthermore, clinical outcomes and QoL measures will be reported to HQO, highlighting the patient experience in this study.
Ethics and dissemination
This study was approved by The Ontario Cancer Research Ethics Board (OCREB) on 14 May 2018 (Ethics ID: CTO 1481). Any necessary protocol amendments will be made formally in conjunction with the trial sponsor, OCREB and clinical trial registries (clinicaltrials.gov). The results of this trial will be disseminated through oral and poster presentations at international surgical conferences. At least two publications in peer-reviewed journals will be authored, focusing on the clinical, economic and QoL outcomes. Results will also be discussed at quality improvement meetings of relevant stakeholders such as the Ontario Surgical Quality Improvement Network, Health Quality Ontario and the Canadian Association of General Surgeons Clinical Practice Committee.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Deanna Rothwell of Performance Measurement at The Ottawa Hospital, The Ottawa Methods Centre for statistical and methods assistance, The Ottawa Hospital Clinical Care leads for colorectal and surgical oncology, and our other collaborating sites: Dr Joel Weaver
—The Queensway Carleton Hospital (Ottawa, ON), Dr Mantaj Brar—Mount Sinai Hospital (Toronto, ON), Dr Sami Chadi—Toronto Western Hospital (Toronto, ON) and Dr Usmaan Hameed—North York General Hospital (Toronto, ON).
Footnotes
Contributors: SSA is a clinical surgical fellow and co-investigator who wrote the manuscript, is responsible for the trial protocol, trial coordination, data analysis, interpretation and knowledge translation. HM is a surgeon and co-investigator who helped with trial conceptualisation and protocol design and is responsible for data analysis and interpretation. AJ is a research coordinator who helped write the manuscript and is responsible for trial progress, daily trial management and data analysis. ML and LV are research coordinators who are responsible for trial coordination and initiation. KS is a clinician investigator and infectious diseases expert who helped with protocol design and is responsible for data analysis and interpretation. KT is a clinical epidemiologist who helped with protocol design and is responsible for the health economic analysis and data interpretation. DAF is a clinical epidemiologist and REaCT expert who helped with protocol design and is responsible for the statistical plan, data analysis and interpretation. MC is an oncologist, clinician investigator and REaCT expert who helped with protocol design and is responsible for data analysis and interpretation. RCA is the principal investigator and corresponding author who conceptualised the study, designed the study protocol, wrote the manuscript and coordinated the trial and is responsible for data analysis, interpretation and knowledge translation.
Funding: Health Sciences Centres of Ontario. The trial sponsor and funding sources have no role or ultimate authority in study design: collection, management, analysis, data interpretation, manuscript writing or decision to submit the manuscript for publication.
Competing interests: RCA, SSA, HM, AJ, KS and KT do not have any conflicts of interests to disclose. DAF is a senior scientist at Ottawa Methods Centre. DAF and MC are the founders and leads of the Ottawa REaCT study platform.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Konishi T, Watanabe T, Kishimoto J, et al. Elective colon and rectal surgery differ in risk factors for wound infection: results of prospective surveillance. Ann Surg 2006;244:758–63. 10.1097/01.sla.0000219017.78611.49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith RL, Bohl JK, McElearney ST, et al. Wound infection after elective colorectal resection. Ann Surg 2004;239:599–607. 10.1097/01.sla.0000124292.21605.99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gantz O, Zagadailov P, Merchant AM. The cost of surgical site infections after colorectal surgery in the United States from 2001 to 2012: a longitudinal analysis. Am Surg 2019;85:142–9. 10.1177/000313481908500219 [DOI] [PubMed] [Google Scholar]
- 4.Keenan JE, Speicher PJ, Thacker JKM, et al. The preventive surgical site infection bundle in colorectal surgery: an effective approach to surgical site infection reduction and health care cost savings. JAMA Surg 2014;149:1045–52. 10.1001/jamasurg.2014.346 [DOI] [PubMed] [Google Scholar]
- 5.Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med 2013;173:2039–46. 10.1001/jamainternmed.2013.9763 [DOI] [PubMed] [Google Scholar]
- 6.Astagneau P, Rioux C, Golliot F, et al. Morbidity and mortality associated with surgical site infections: results from the 1997–1999 INCISO surveillance. J Hosp Infect 2001;48:267–74. 10.1053/jhin.2001.1003 [DOI] [PubMed] [Google Scholar]
- 7.Koskenvuo L, Lehtonen T, Koskensalo S, et al. Mechanical and oral antibiotic bowel preparation versus no bowel preparation for elective colectomy (mobile): a multicentre, randomised, parallel, single-blinded trial. Lancet 2019;394:840–8. 10.1016/S0140-6736(19)31269-3 [DOI] [PubMed] [Google Scholar]
- 8.Espin-Basany E, Sanchez-Garcia JL, Lopez-Cano M, et al. Prospective, randomised study on antibiotic prophylaxis in colorectal surgery. Is it really necessary to use oral antibiotics? Int J Colorectal Dis 2005;20:542–6. 10.1007/s00384-004-0736-8 [DOI] [PubMed] [Google Scholar]
- 9.Lewis RT. Oral versus systemic antibiotic prophylaxis in elective colon surgery: a randomized study and meta-analysis send a message from the 1990s. Can J Surg 2002;45:173–80. [PMC free article] [PubMed] [Google Scholar]
- 10.Bhat AH, Parray FQ, Chowdri NA, et al. Mechanical bowel preparation versus no preparation in elective colorectal surgery: a prospective randomized study. International Journal of Surgery Open 2016;2:26–30. 10.1016/j.ijso.2016.02.010 [DOI] [Google Scholar]
- 11.Contant CME, Hop WCJ, van't Sant HP, et al. Mechanical bowel preparation for elective colorectal surgery: a multicentre randomised trial. Lancet 2007;370:2112–7. 10.1016/S0140-6736(07)61905-9 [DOI] [PubMed] [Google Scholar]
- 12.Fa-Si-Oen P, Roumen R, Buitenweg J, et al. Mechanical bowel preparation or not? outcome of a multicenter, randomized trial in elective open colon surgery. Dis Colon Rectum 2005;48:1509–16. 10.1007/s10350-005-0068-y [DOI] [PubMed] [Google Scholar]
- 13.Miettinen RP, Laitinen ST, Mäkelä JT, et al. Bowel preparation with oral polyethylene glycol electrolyte solution vs. no preparation in elective open colorectal surgery: prospective, randomized study. Dis Colon Rectum 2000;43:669–75. 10.1007/BF02235585 [DOI] [PubMed] [Google Scholar]
- 14.Migaly J, Bafford AC, Francone TD, et al. The American Society of colon and rectal surgeons clinical practice guidelines for the use of bowel preparation in elective colon and rectal surgery. Dis Colon Rectum 2019;62:3–8. 10.1097/DCR.0000000000001238 [DOI] [PubMed] [Google Scholar]
- 15.Allegranzi B, Bischoff P, de Jonge S, et al. New who recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 2016;16:e276–87. 10.1016/S1473-3099(16)30398-X [DOI] [PubMed] [Google Scholar]
- 16.Ban KA, Minei JP, Laronga C, et al. American College of surgeons and surgical infection Society: surgical site infection guidelines, 2016 update. J Am Coll Surg 2017;224:59–74. 10.1016/j.jamcollsurg.2016.10.029 [DOI] [PubMed] [Google Scholar]
- 17.Eskicioglu C, Forbes SS, Fenech DS, et al. Preoperative bowel preparation for patients undergoing elective colorectal surgery: a clinical practice guideline endorsed by the Canadian Society of colon and rectal surgeons. Can J Surg 2010;53:385–95. [PMC free article] [PubMed] [Google Scholar]
- 18.Leaper D, Burman-Roy S, Palanca A, et al. Prevention and treatment of surgical site infection: summary of NICE guidance. BMJ 1924;2008. [DOI] [PubMed] [Google Scholar]
- 19.Clarke JS, Condon RE, Bartlett JG, et al. Preoperative oral antibiotics reduce septic complications of colon operations: results of prospective, randomized, double-blind clinical study. Ann Surg 1977;186:251–9. 10.1097/00000658-197709000-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Polacek MA, Sanfelippo P. Oral antibiotic bowel preparation and complications in colon surgery. Arch Surg 1968;97:412–7. 10.1001/archsurg.1968.01340030072005 [DOI] [PubMed] [Google Scholar]
- 21.Nichols RL, Condon RE. Preoperative preparation of the colon. Surg Gynecol Obstet 1971;132:323–37. [PubMed] [Google Scholar]
- 22.Ali M. Randomized prospective clinical trial of NO preparation versus mechanical bowel preparation before elective colorectal surgery. Med Channel 2007;13:32–5. [Google Scholar]
- 23.Bertani E, Chiappa A, Biffi R, et al. Comparison of oral polyethylene glycol plus a large volume glycerine enema with a large volume glycerine enema alone in patients undergoing colorectal surgery for malignancy: a randomized clinical trial. Colorectal Dis 2011;13:e327–34. 10.1111/j.1463-1318.2011.02689.x [DOI] [PubMed] [Google Scholar]
- 24.Bhattacharjee PK, Chakraborty S. An open-label prospective randomized controlled trial of mechanical bowel preparation vs Nonmechanical bowel preparation in elective colorectal surgery: personal experience. Indian J Surg 2015;77:1233–6. 10.1007/s12262-015-1262-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bucher P, Gervaz P, Soravia C, et al. Randomized clinical trial of mechanical bowel preparation versus no preparation before elective left-sided colorectal surgery. Br J Surg 2005;92:409–14. 10.1002/bjs.4900 [DOI] [PubMed] [Google Scholar]
- 26.Burke P, Mealy K, Gillen P, et al. Requirement for bowel preparation in colorectal surgery. Br J Surg 1994;81:907–10. 10.1002/bjs.1800810639 [DOI] [PubMed] [Google Scholar]
- 27.Pena-Soria MJ, Mayol JM, Anula R, et al. Single-blinded randomized trial of mechanical bowel preparation for colon surgery with primary intraperitoneal anastomosis. J Gastrointest Surg 2008;12:2103–9. 10.1007/s11605-008-0706-5 [DOI] [PubMed] [Google Scholar]
- 28.Ram E, Sherman Y, Weil R, et al. Is mechanical bowel preparation mandatory for elective colon surgery? A prospective randomized study. Arch Surg 2005;140:285–8. 10.1001/archsurg.140.3.285 [DOI] [PubMed] [Google Scholar]
- 29.Saha AK, Chowdhury F, Jha AK, et al. Mechanical bowel preparation versus no preparation before colorectal surgery: a randomized prospective trial in a tertiary care Institute. J Nat Sci Biol Med 2014;5:421–4. 10.4103/0976-9668.136214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Santos JC, Batista J, Sirimarco MT, Sirimarco MT, et al. Prospective randomized trial of mechanical bowel preparation in patients undergoing elective colorectal surgery. Br J Surg 1994;81:1673–6. 10.1002/bjs.1800811139 [DOI] [PubMed] [Google Scholar]
- 31.Sasaki J, Matsumoto S, Kan H, et al. Objective assessment of postoperative gastrointestinal motility in elective colonic resection using a radiopaque marker provides an evidence for the abandonment of preoperative mechanical bowel preparation. J Nippon Med Sch 2012;79:259–66. 10.1272/jnms.79.259 [DOI] [PubMed] [Google Scholar]
- 32.Bucher P, Mermillod B, Gervaz P, et al. Mechanical bowel preparation for elective colorectal surgery: a meta-analysis. Arch Surg 2004;139:1359–64. 10.1001/archsurg.139.12.1359 [DOI] [PubMed] [Google Scholar]
- 33.Courtney DE, Kelly ME, Burke JP, et al. Postoperative outcomes following mechanical bowel preparation before proctectomy: a meta-analysis. Colorectal Dis 2015;17:862–9. 10.1111/codi.13026 [DOI] [PubMed] [Google Scholar]
- 34.Dahabreh IJ, Steele DW, Shah N, et al. Oral mechanical bowel preparation for colorectal surgery: systematic review and meta-analysis. Dis Colon Rectum 2015;58:698–707. 10.1097/DCR.0000000000000375 [DOI] [PubMed] [Google Scholar]
- 35.Pineda CE, Shelton AA, Hernandez-Boussard T, et al. Mechanical bowel preparation in intestinal surgery: a meta-analysis and review of the literature. J Gastrointest Surg 2008;12:2037–44. 10.1007/s11605-008-0594-8 [DOI] [PubMed] [Google Scholar]
- 36.Rollins KE, Javanmard-Emamghissi H, Lobo DN. Impact of mechanical bowel preparation in elective colorectal surgery: a meta-analysis. World J Gastroenterol 2018;24:519–36. 10.3748/wjg.v24.i4.519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Slim K, Vicaut E, Launay-Savary M-V, et al. Updated systematic review and meta-analysis of randomized clinical trials on the role of mechanical bowel preparation before colorectal surgery. Ann Surg 2009;249:203–9. 10.1097/SLA.0b013e318193425a [DOI] [PubMed] [Google Scholar]
- 38.Wille-Jørgensen P, Guenaga KF, Matos D, et al. Pre-operative mechanical bowel cleansing or not? an updated meta-analysis. Colorectal Dis 2005;7:304–10. 10.1111/j.1463-1318.2005.00804.x [DOI] [PubMed] [Google Scholar]
- 39.Leenen JPL, Hentzen JEKR, Ockhuijsen HDL. Effectiveness of mechanical bowel preparation versus no preparation on anastomotic leakage in colorectal surgery: a systematic review and meta-analysis. Updates Surg 2019;71:227–36. 10.1007/s13304-018-0526-4 [DOI] [PubMed] [Google Scholar]
- 40.Güenaga KF, Matos D, Wille-Jørgensen P. Mechanical bowel preparation for elective colorectal surgery. Cochrane Database Syst Rev 2011:CD001544.. 10.1002/14651858.CD001544.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Oliveira L, Wexner SD, Daniel N, et al. Mechanical bowel preparation for elective colorectal surgery. A prospective, randomized, surgeon-blinded trial comparing sodium phosphate and polyethylene glycol-based oral lavage solutions. Dis Colon Rectum 1997;40:585–91. 10.1007/BF02055384 [DOI] [PubMed] [Google Scholar]
- 42.Lieberman DA, Ghormley J, Flora K. Effect of oral sodium phosphate colon preparation on serum electrolytes in patients with normal serum creatinine. Gastrointest Endosc 1996;43:467–9. 10.1016/S0016-5107(96)70287-0 [DOI] [PubMed] [Google Scholar]
- 43.Shapira Z, Feldman L, Lavy R, et al. Bowel preparation: comparing metabolic and electrolyte changes when using sodium phosphate/polyethylene glycol. Int J Surg 2010;8:356–8. 10.1016/j.ijsu.2010.04.009 [DOI] [PubMed] [Google Scholar]
- 44.Beloosesky Y, Grinblat J, Weiss A, et al. Electrolyte disorders following oral sodium phosphate administration for bowel cleansing in elderly patients. Arch Intern Med 2003;163:803–8. 10.1001/archinte.163.7.803 [DOI] [PubMed] [Google Scholar]
- 45.Garfinkle R, Abou-Khalil J, Morin N, et al. Is there a role for oral antibiotic preparation alone before colorectal surgery? ACS-NSQIP analysis by Coarsened exact matching. Dis Colon Rectum 2017;60:729–37. 10.1097/DCR.0000000000000851 [DOI] [PubMed] [Google Scholar]
- 46.Barber MS, Hirschberg BC, Rice CL, et al. Parenteral antibiotics in elective colon surgery? A prospective, controlled clinical study. Surgery 1979;86:23–9. [PubMed] [Google Scholar]
- 47.Condon RE, Bartlett JG, Nichols RL, et al. Preoperative prophylactic cephalothin fails to control septic complications of colorectal operations: results of controlled clinical trial. A Veterans administration Cooperative study. Am J Surg 1979;137:68–74. 10.1016/0002-9610(79)90013-8 [DOI] [PubMed] [Google Scholar]
- 48.Nichols RL, Broido P, Condon RE, et al. Effect of preoperative neomycin-erythromycin intestinal preparation on the incidence of infectious complications following colon surgery. Ann Surg 1973;178:453–62. 10.1097/00000658-197310000-00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Polk HC, Lopez-Mayor JF, Jr. Postoperative wound infection: a prospective study of determinant factors and prevention. Surgery 1969;66:97–103. [PubMed] [Google Scholar]
- 50.Song F, Glenny AM. Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomized controlled trials. Br J Surg 1998;85:1232–41. 10.1046/j.1365-2168.1998.00883.x [DOI] [PubMed] [Google Scholar]
- 51.Chen M, Song X, Chen L-Z, et al. Comparing mechanical bowel preparation with both oral and systemic antibiotics versus mechanical bowel preparation and systemic antibiotics alone for the prevention of surgical site infection after elective colorectal surgery: a meta-analysis of randomized controlled clinical trials. Dis Colon Rectum 2016;59:70–8. 10.1097/DCR.0000000000000524 [DOI] [PubMed] [Google Scholar]
- 52.McSorley ST, Steele CW, McMahon AJ. Meta-Analysis of oral antibiotics, in combination with preoperative intravenous antibiotics and mechanical bowel preparation the day before surgery, compared with intravenous antibiotics and mechanical bowel preparation alone to reduce surgical-site infections in elective colorectal surgery. BJS Open 2018;2:185–94. 10.1002/bjs5.68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.WHO Global guidelines for the prevention of surgical site infection, web appendix 6. global guidelines for the prevention of surgical site infection. Geneva, 2018. [Google Scholar]
- 54.Toh JWT, Phan K, Hitos K, et al. Association of mechanical bowel preparation and oral antibiotics before elective colorectal surgery with surgical site infection: a network meta-analysis. JAMA Netw Open 2018;1:e183226. 10.1001/jamanetworkopen.2018.3226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Koller SE, Bauer KW, Egleston BL, et al. Comparative effectiveness and risks of bowel preparation before elective colorectal surgery. Ann Surg 2018;267:734–42. 10.1097/SLA.0000000000002159 [DOI] [PubMed] [Google Scholar]
- 56.Rollins KE, Javanmard-Emamghissi H, Acheson AG, et al. The role of oral antibiotic preparation in elective colorectal surgery: a meta-analysis. Ann Surg 2019;270:43–58. 10.1097/SLA.0000000000003145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mulder T, Kluytmans JAJW. Oral antibiotics prior to colorectal surgery: do they have to be combined with mechanical bowel preparation? Infect Control Hosp Epidemiol 2019;40:922–7. 10.1017/ice.2019.157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hilton J, Mazzarello S, Fergusson D, et al. Novel methodology for comparing standard-of-care interventions in patients with cancer. J Oncol Pract 2016;12:e1016–24. 10.1200/JOP.2016.013474 [DOI] [PubMed] [Google Scholar]
- 59.Canadian cancer systems Canadian cancer systems performance report, 2018. Available: https://www.systemperformance.ca/report/2018-cancer-system-performance-report/ [Accessed 29 Oct 2019].
- 60.Kim SYH, Miller FG. Informed consent for pragmatic trials—the integrated consent model. N Engl J Med 2014;370:769–72. 10.1056/NEJMhle1312508 [DOI] [PubMed] [Google Scholar]
- 61.Basulaiman B, Awan AA, Fergusson D, et al. Creating a pragmatic trials program for breast cancer patients: rethinking clinical trials (react). Breast Cancer Res Treat 2019;177:93–101. 10.1007/s10549-019-05274-0 [DOI] [PubMed] [Google Scholar]
- 62.Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for Perioperative Care in Elective Colorectal Surgery: Enhanced Recovery After Surgery (ERAS®) Society Recommendations: 2018. World J Surg 2019;43:659–95. 10.1007/s00268-018-4844-y [DOI] [PubMed] [Google Scholar]
- 63.ERAS Society ERAS Society - Associated Sites, 2019. Available: http://erassociety.org/national/associated-sites/ [Accessed 19 Sep 2019].
- 64.Gresham LM, Sadiq M, Gresham G, et al. Evaluation of the effectiveness of an enhanced recovery after surgery program using data from the National surgical quality improvement program. Cjs 2019;62:175–81. 10.1503/cjs.003518 [DOI] [Google Scholar]
- 65.ACS Acs national surgical quality improvement Program® (ACS NSQIP®, 2017. [Google Scholar]
- 66.Ministry of Health Ontario Quality-Based procedures clinical Handbook for cancer surgery, 2016. http://www.health.gov.on.ca/en/pro/programs/ecfa/docs/qbp_cancer_surgery.pdf [Google Scholar]
- 67.Health Quality Ontario Surgical quality improvement network, 2017. Available: http://www.hqontario.ca/Quality-Improvement/Quality-Improvement-in-Action/Surgical-Quality-Improvement-in-Ontario [Accessed 1 Jun 2019].
- 68.Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727–36. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ware JE, Sherbourne CD. The mos 36-item short-form health survey (SF-36). I. conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 70.Cannon JA, Altom LK, Deierhoi RJ, et al. Preoperative oral antibiotics reduce surgical site infection following elective colorectal resections. Dis Colon Rectum 2012;55:1160–6. 10.1097/DCR.0b013e3182684fac [DOI] [PubMed] [Google Scholar]
- 71.Antonescu I, Carli F, Mayo NE, et al. Validation of the SF-36 as a measure of postoperative recovery after colorectal surgery. Surg Endosc 2014;28:3168–78. 10.1007/s00464-014-3577-8 [DOI] [PubMed] [Google Scholar]
- 72.EQ EQ-5D-5L User Guide—Basic information on how to use the EQ-5D-5L instrument., 2015. Available: https://euroqol.org/docs/EQ-5D-5L-User-Guide.pdf [Accessed 19 Jun 2019].
- 73.Copay AG, Subach BR, Glassman SD, et al. Understanding the minimum clinically important difference: a review of concepts and methods. Spine J 2007;7:541–6. 10.1016/j.spinee.2007.01.008 [DOI] [PubMed] [Google Scholar]
- 74.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. ascertaining the minimal clinically important difference. Control Clin Trials 1989;10:407–15. 10.1016/0197-2456(89)90005-6 [DOI] [PubMed] [Google Scholar]
- 75.Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487–96. 10.1002/hec.944 [DOI] [PubMed] [Google Scholar]
- 76.Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull 2010;96:5–21. 10.1093/bmb/ldq033 [DOI] [PubMed] [Google Scholar]
- 77.Glick HA, Doshi JA, Sonnad SS. Economic evaluation in clinical trials. 2nd ed Oxford, UK: Oxford University Press, 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-036866supp001.pdf (195.5KB, pdf)
bmjopen-2020-036866supp002.pdf (95.9KB, pdf)