Abstract
Oncologist well-being is critical to initiating and maintaining the physician-patient relationship, yet many oncologists suffer from symptoms of burnout. Burnout has been linked to poor physical and mental health, as well as increased medical errors, patient dissatisfaction, and workforce attrition. In this Call to Action article, we discuss causes of and interventions for burnout and moral distress in oncology, highlight existing interventions, and provide recommendations for addressing burnout and improving well-being at the individual and organizational levels to deliver ethical, quality cancer care.
INTRODUCTION: THE ETHICAL IMPERATIVE: ATTEND TO ONCOLOGIST BURNOUT TO PROMOTE WELL-BEING
Burnout and the related occupation-associated stress issues of moral distress and compassion fatigue occur frequently among oncology clinicians, stemming from the significant cognitive, emotional, and administrative demands related to delivering highly complex cancer care.1-4 Unaddressed burnout may affect oncology clinicians’ physical and mental health, their capacity to make optimal treatment recommendations, and the quality of the clinician-patient relationship.3 Burnout is also associated with increased turnover, reduced work hours or absenteeism, and early retirement from clinical practice. These organizational changes carry economic costs to individual practices and the larger health care system, while contributing to shortages of practicing oncologists.1,5,6 High levels of oncologist burnout suggest the health care system is failing to provide healthy workplace environments that support clinician well-being and facilitate high-quality cancer care.7,8 Therefore, the cancer community has an ethical imperative to develop and support organizational, system-wide, and individual interventions to directly address burnout in clinical oncology.7,9,10
The ASCO Ethics Committee convened the Burnout and Moral Distress in Oncology Roundtable in May 2019. The goal was to explore ethical considerations related to burnout and moral distress in oncology practice, identify factors that require further attention, and make recommendations for action. Meeting participants included clinicians, bioethicists, researchers, administrators, and other individuals with expertise or a dedicated interest in clinician burnout. After the meeting, a panel of experts met to summarize roundtable discussions and develop an action plan. This article summarizes these discussions and recommendations for addressing burnout in oncology clinicians and physicians in training. Although the authors recognize that all members of the oncology team are at risk for burnout,3,4,11,12 a wider discussion is beyond the scope of this article.
THE PROBLEM
Burnout in Health Care Professionals
WHO defines burnout as an occupation-related clinical syndrome resulting from chronic, unresolved, occupation-related stress.13 It is characterized by physical and/or emotional exhaustion, cynicism and/or depersonalization, and inefficacy or low sense of professional accomplishment.13 Burnout is more common in physicians than other US workers and is estimated to affect 50% of physicians at some point in their career.5,14,15 Symptoms arise when a mismatch between occupational demands and available resources causes physical, psychological, and emotional stress.8 Risk factors include both occupation-related factors (eg, high patient loads, increased administrative responsibilities, use of electronic medical records (EMRs), lack of social support) and individual factors (eg, female sex, younger age, or single, unmarried/nonpartnered status).3 Initial symptoms of physician burnout tend to develop slowly and in stages,16 culminating in the final burnout syndrome.3,4 Symptoms may initially appear in medical school, increase in intensity over time during residency or fellowship training,4,10,17-20 and persist for prolonged periods. They may resolve when clinicians develop new coping strategies, workplace stressors are reduced, or working conditions improve or after a job change.3,10 However, when clinicians attempt to “tough it out” or ignore stress, burnout symptoms become chronic.3
Burnout in Oncology
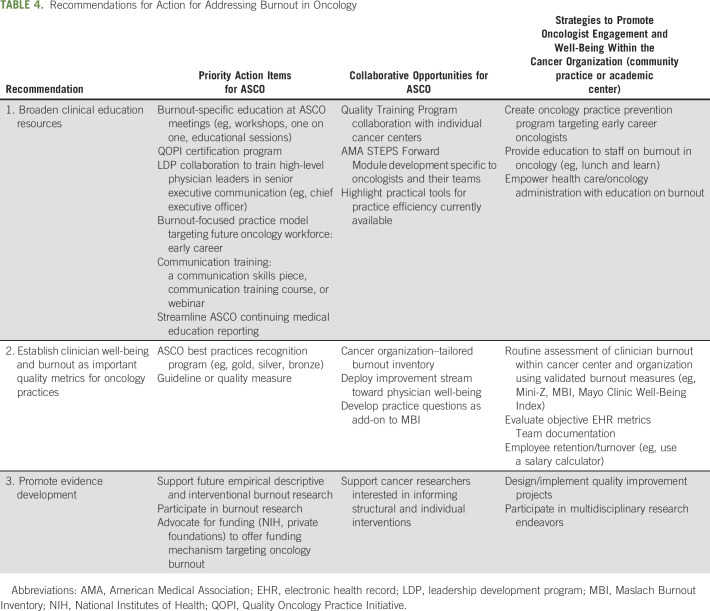
In a recent survey of ASCO member medical oncologists, 45% of respondents reported experiencing emotional exhaustion and/or depersonalization related to burnout, signs that previous studies indicate may persist.7,21-23 Oncology clinician burnout arises from a combination of individual factors and organizational, systems-level factors. Some of these are prevalent across all medical specialties, whereas others are specific to oncology3 (Table 1). The evolving medical landscape and changing practice demands have significantly affected how care is delivered, documented, and reimbursed, contributing to clinician stress across practice areas.8,10 For example, a recent study examining workplace characteristics associated with burnout found that hours worked per week, number of hours spent seeing patients per week, and high patient load were all associated with burnout in oncologists.2 Similarly, the time required for using EMRs takes time away from patient care and is associated with high levels of burnout.24 Other administrative responsibilities associated with finding affordable treatment options, matching patients with clinical trials, and negotiating with insurance and pharmacy benefit managers have increased, with physicians spending an average of 2 hours on administrative duties for every hour of patient care.25,26 High staff turnover, the departure of key physicians and staff, and unfilled vacancies also increase workload and contribute to work-related stress.2
TABLE 1.
Recognized Organizational Factors Associated With Burnout in Oncology
The practice of oncology also has unique occupational challenges. Patients with cancer may be in a psychological or medical crisis at every point across the cancer trajectory from diagnosis to end of life, and continuous exposure to life-threatening illness, limited treatment options, and treatment failure make clinicians particularly vulnerable to psychological distress and burnout.12,27 Growing numbers of long-term survivors of cancer and older patients with chronic health conditions pose unique treatment challenges,28,29 and oncologists are often in ethically challenging situations related to differences in patient, family, and colleague values and preferences in end-of-life care. These may include requests for nonbeneficial treatment or refusal of potentially beneficial interventions.30 Finally, a sense of personal failure and grief upon the death of a patient are key drivers of burnout in oncology clinicians.30
CONSEQUENCES OF ONCOLOGIST BURNOUT
Personal and Professional Consequences of Burnout
Burnout may have profound effects on both personal health and professional performance. Chronic burnout is associated with physical health conditions (eg, cardiovascular disease, chronic fatigue, cognitive dysfunction, insomnia, GI issues) and mental health issues (eg, depression, anxiety, substance dependence, suicide).2,5,10,31-33 Personal life disruptions (eg, marital conflict, family disruption, or divorce) are also common.2,5,10 The connection between workload or productivity and personal consequences is multifaceted. For example, long workdays and heavy administrative load have been found to contribute to significant work-home conflicts, resulting in issues balancing professional and family roles,3,10 whereas the connection between burnout and suicide, as well as burnout and cardiovascular disease, may explain why burnout is associated with shortened life expectancy.34
Although burnout is not classified as a psychological condition, it shares symptomology with several psychiatric disorders4 and is often accompanied by overlapping syndromes, such as moral distress and compassion fatigue.3,4 Moral distress, a type of work stress that frequently occurs with burnout, is defined as psychological pain or anguish in response to situations where health care professionals are unable to act in accordance with their moral values as a result of real or perceived constraints.35-39 Life and death decision making and perceived futility of treatment have been identified as common ethical challenges leading to moral distress.12 Prolonged, continuous, and intense patient contact may also lead to compassion fatigue, which is characterized by tension and preoccupation with the individual or cumulative trauma of one’s patients. Compassion fatigue manifests in three major domains (hyperarousal, avoidance, and re-experiencing) that parallel symptoms of posttraumatic stress disorders.9,40,41 Depression and moral distress have been described as both precursors to and consequences of burnout.4 Some research suggests that moral distress should be identified as an ethical root cause of clinician burnout.10 However, these are generally identified as unique—albeit related—entities.
In addition to personal consequences, chronic burnout often has deleterious effects on occupational skills (eg, problem solving and decision making) that may jeopardize patient care.42-44 Research demonstrates a relationship between physician burnout and self-reported medical errors,10,12,42,45,46 suboptimal care,47,48 decreased productivity,5,49 low professionalism, and unethical behavior.50 Not surprisingly, these negative effects are associated with poor treatment outcomes and lower patient satisfaction10,42 and affect the relationships between physicians and patients, families, and other oncology professionals.51 Although an eroded sense of purpose is a risk factor, burnout itself may undermine the clinician’s sense of purpose, identity, and altruism, which may further undermine care.6,10 Recent evidence reveals that professional burnout is associated with self-reported unprofessional behaviors and less cost-conscious attitudes among physicians.48 Similarly, cynicism, loss of engagement, and decreased professional satisfaction strongly influence trainees’ decisions to choose oncology and clinicians’ decisions to change employment or retire.20,52,53
Organizational and System-Wide Consequences
The effects of burnout on the oncologist-patient relationship and the lost revenue associated with decreased productivity and compromised care are costly to the health care system.5,6 Lowered quality of care, staff shortages, decreased patient satisfaction, and safety concerns quickly diminish the reputation of practices and organizations, causing lost business and threats to long-term viability.5 Burnout-associated absenteeism and decreased workload productivity result in lower revenues6,7 and create institutional problems with recruitment and retention of staff.2 The loss of oncologists through early retirement is also a concern for the oncology community, which projects a shortage of oncologists in the coming years.54-60 Physician burnout costs the US health care system an estimated $4.6 billion a year as a result of reduced clinical hours and physician turnover.10
BURNOUT INTERVENTIONS
Interventions for burnout have been categorized as organizational, systems-level interventions that target the workplace and individual interventions focused on the clinician.21,61 Research comparing the effectiveness of individual versus organizational interventions suggests that institutional interventions are more effective than individual approaches alone,21 but both approaches may be needed to support clinicians, change institutional culture, and reduce workplace stressors.
Organizational, Systematic Interventions
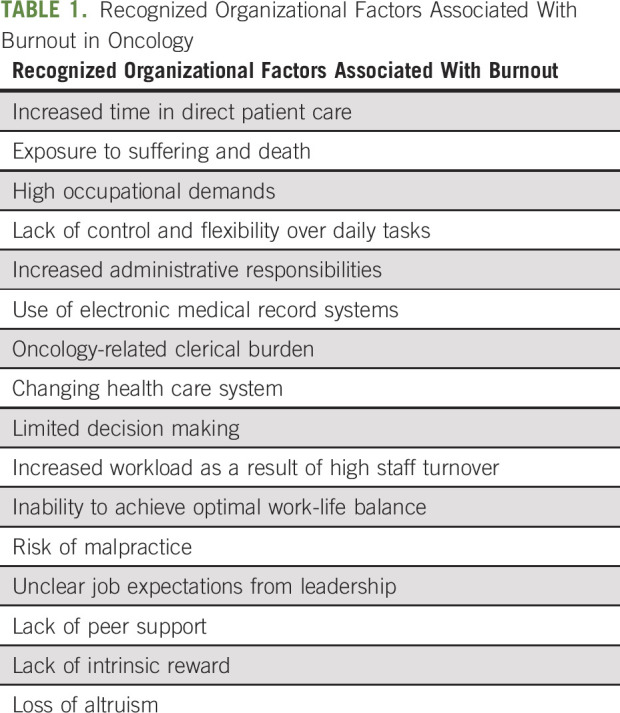
Institutional, system-level interventions aim to reduce or eliminate environmental stressors and promote healthy workplace environments.62,63 A range of individual studies, systematic analyses, and meta-analyses have demonstrated the efficacy of organizational efforts to reduce burnout5,21,61,62 (Table 2). Some environmental interventions are designed to reduce stress by streamlining work flow and reducing administrative burden.5,62 For example, the University of Colorado APEX system teamwork model incorporated medical assistants to decrease administrative burdens on clinicians6,64 and found that burnout decreased from 53% to 13%, efficiency and productivity increased, and patient waiting times decreased. Other strategies focus on changing practice culture and ethics3,4,12,65,66 and fostering community and engagement with colleagues.4,12,40,67-69 Organizational interventions include stand-alone programs addressing specific institutional areas as well as programs designed to address multiple institutional levels or to work in tandem with individual interventions.3,4,9,10,38,70 For example, the open access American Medical Association (AMA) STEPS Forward Program module71 recommends the following nine strategies: engagement of leadership; acknowledgment and routine longitudinal burnout assessment; creation of infrastructure for implementation of individual and system-level interventions; workflow efficiency; reduction in administrative burdens; support for health of the workforce; strengthening of local leadership; tracking organizational costs of burnout; and routine assessment of interventions to promote organizational health and employee well-being.62,63
TABLE 2.
Efficacy of Tested Organizational Efforts and Solutions to Reduce Burnout
Individual Interventions
In addition to organizational interventions, interventions targeting individual clinicians have been empirically studied.7,12,43 These interventions provide resources to help clinicians recognize, minimize, or manage burnout symptoms; alleviate distress; and/or promote resilience and improve well-being.3 Individual interventions include education, cognitive-behavioral therapy, social support and work-life integration, mindfulness-based stress reduction, communication skills training, health promotion, and promoting activism to change the work environment. For example, cognitive-behavioral interventions help clinicians recognize stress levels and deploy coping strategies.3,4 Skill-based interventions such as improving communication skills and reducing stress during difficult patient conversations have also been described.67,72 Self-compassion has been identified as a mechanism to improve clinician well-being.73
Literature on the effectiveness of individual interventions is growing, but studies specific to oncologists remain limited. Most examine the effects of a single treatment modality on one or more symptoms of burnout or well-being, and the results are varied. For example, 2 studies indicate that mindfulness training can influence burnout, empathy, and well-being,3 whereas the results of a randomized controlled trial showed limited impacts of communication skills training on stress and burnout.74 However, the communication training involved a single session and targeted a predetermined communication challenge, which may have limited the impact on stress and burnout. Providing skills training that targets oncologists’ self-determined communication challenges and offering longitudinal booster sessions to reinforce skills have the potential to bolster the impact of training. A recent meta-analysis that combined physician-directed interventions reported small but significant reductions in burnout across interventions,21,61 suggesting that individuals can receive similar benefits from a variety of approaches10 and that interventions delivered concurrently may increase efficacy. Although burnout interventions are not equivalent to those directed at job satisfaction or quality of life, research suggests that reducing burnout may improve quality of life and job satisfaction.10 For example, a recent randomized clinical trial investigating an individualized coaching intervention targeting well-being and distress found significant reductions in emotional exhaustion and burnout and improvements in overall quality of life and resilience.6,65 In summary, research suggests that a spectrum of interventions addressing different dimensions of burnout can successfully reduce or eliminate burnout symptoms and improve quality of life in health care professionals.9,21 However, because research findings are limited and inconsistent, further investigation in oncology settings is warranted.
Medical and Professional Organization Initiatives
Professional medical associations have also developed programs and initiatives to reduce physician burnout and promote wellness.10 Working groups within the National Academies of Sciences, Engineering, and Medicine (NASEM) have created a knowledge hub, a series of discussion papers, and a conceptual model75 and have assembled an action collaborative of > 60 organizations committed to reversing burnout.76 The AMA has produced multiple studies, hosted conferences, and conducted institutional assessments of burnout levels and the links between burnout and stressors such as EMR usability (eg, EHRSeeWhatWeMean.org).77 For example, AMA STEPS Forward Program offers specific practice improvement strategies to increase workflow efficiency, promote team-based care, decrease administrative burden, and increase clinician wellness and personal resilience.71 Similarly, the American College of Physicians has created a task force and extensive practice resources promoting physician wellness and professional satisfaction.78 The American Medical Women’s Association has introduced multiple interorganizational efforts and resources to address burnout in women physicians and advocate for well-being during residency. The Society of Gynecologic Oncology has created a Wellness Task Force, an evidence-based review, and a wellness curriculum targeted at fellows and early career oncologists.79-81
ASCO Burnout Initiatives to Date
ASCO has addressed burnout in the clinical oncology community by providing resources that support professional development, quality improvement, and education for physicians and practices. These resources align with goals from the strategic plan by offering member services to “redefine the needs of ASCO’s members and key constituents” and “deliver better support for the modern oncology professional.”82 ASCO’s educational offerings include formal presentations, interactive sessions, and facilitated group discussions at the annual meetings, thematic meetings, and symposia. For example, ASCO’s 2015 Supportive Care Symposium incorporated Death Cafes, which are informal, group-directed discussions about death,83 and a comprehensive review of burnout in oncology was presented at the ASCO annual meeting in 2016 and published as an ASCO Educational Book.3 ASCO’s professional development programming piloted a resilience skills training program for hematology/oncology fellows,84 and online resources offer clinicians tools to relieve burnout.85 More recently, ASCO has begun addressing workplace factors by providing resources to practices. For example, ASCO launched the Quality Training Program (QTP) in the summer of 2019. This innovative program is designed to assist teams from oncology practices address the factors leading to clinician burnout.86 Other publications and presentations include the Care Delivery Report,87 Journal of Clinical Oncology Report,20 ASCO Perspective,88 blog posts,89 and surveys.22
FUTURE DIRECTIONS
Mobilizing Resources and Research to Maximize Oncologist Well-Being
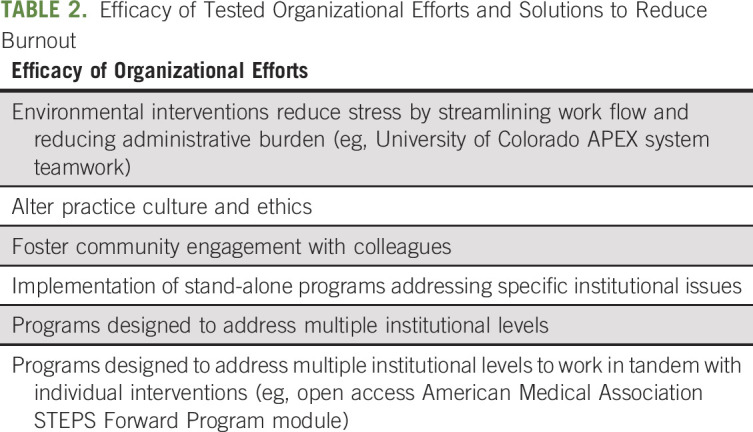
Although oncology clinician burnout has been widely discussed and resources and education for professionals and practices have increased, the global prevalence of burnout in oncology clinicians has increased over the past decade, and more resources are needed to promote clinician health and well-being and optimal clinical environments.14 It is vital that the organization use specific efforts to address burnout in oncology including recognizing the importance of oncology physician well-being to achieving its mission; assessing burnout routinely; proactively engaging organizational leaders and physicians in collaborative action planning; optimizing the clinical practice environment and institutional culture; and providing well-being resources (Table 3). Improvement can only occur if effective interventions are implemented over the short term because culture takes time to change. Therefore, the ASCO Ethics Committee Roundtable Burnout Experts believe it is critical to provide cancer leaders, administrators, and organizations with substantial guidance and recommendations based on empirical evidence noted in this work on critical collaborative actions they must take to address burnout in both the immediate short term and the long term. These recommendations for action are summarized in Table 4 and include priority action items that ASCO may be particularly well suited to address, additional collaborative opportunities for ASCO to partner with other organizations (eg, medical professional societies, independent oncology community practices, and academic cancer centers), and strategies to promote oncologist engagement and well-being within the oncology organization (community practice or cancer center) to strengthen burnout and resilience efforts independently within independent institutions.
TABLE 3.
Proposed Organizational Interventions to Address Burnout in Oncology
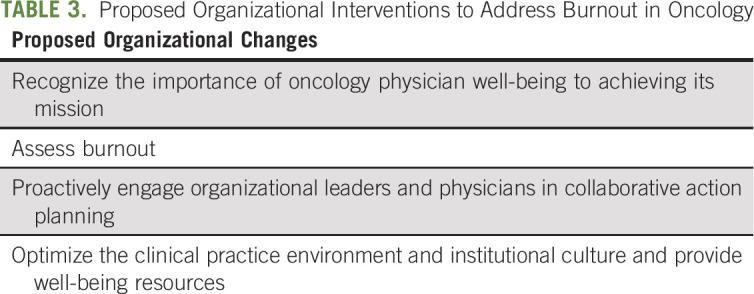
TABLE 4.
Recommendations for Action for Addressing Burnout in Oncology
To help prioritize recommendations, identify unmet needs, foster existing efforts, and expand opportunities to partner with other organizations, the roundtable urges ASCO to create a dedicated Task Force on Burnout, Well-Being, and Professional Satisfaction. Task force membership could combine ASCO volunteers with burnout experts from across medicine and include program administrators and fellowship directors. This task force could consider adopting NASEM recommendations for medical professional societies, such as advocacy with state licensing bodies to reduce the professional impact of seeking mental health treatment.8 The following recommendations highlight areas where a task force could work within ASCO and with medical societies and cancer organizations (oncology community practices and academic cancer centers) to direct and combine resources. These recommendations are based on a small number of studies from single institutions, and thus, information sharing across institutions is essential to refine these efforts further. In summary, the final recommendations for action (Table 4) are as follows.
Recommendation 1: Broaden Clinician Education Resources
Although ASCO and other medical organizations have increased educational offerings in recent years, roundtable participants recommended expanding oncology-specific resources for practicing clinicians and developing new resources for oncology fellows and early-career clinicians to help prevent burnout. The following subrecommendations outline suggested strategies:
Recommendation 1a: To solidify its commitment to member well-being and practice health, ASCO should continue to integrate burnout, professional satisfaction, and well-being into the educational curriculum (eg, educational sessions, workshops, training sessions) at ASCO annual and thematic meetings and expand webinar and online resources.
Recommendation 1b: ASCO could use existing leadership and educational programs (eg, Leadership Development Program and Education Scholars Program) and other venues to promote discussion between clinicians, practice administrators, and educators on topics related to burnout and the moral issues faced by oncologists.
Recommendation 1c: ASCO could create a set of burnout-related resources for physicians in training. These could include a toolkit for developing professional skills (eg, patient communication, ethical decision making, combating moral distress and compassion fatigue) and a best practices or physician wellness checklist to help job applicants evaluate organizational stressors (eg, staffing ratios, EMR requirements, documentation support) and workplace wellness in potential employers.
Recommendation 2: Establish Physician Well-Being and Burnout as Important Quality Metrics for Oncology Practices
An important part of addressing burnout at the cancer organization and individual institutional level is using validated and standardized measures to assess and report on employee well-being and burnout.8 The following subrecommendations address the deficiencies in available resources for organizational leaders and administrators43,83 and propose steps to address these deficiencies:
Recommendation 2a: ASCO could create or support the creation of a specific pathway for administrative leaders on how to promote resilience and well-being and reduce burnout. The proposed Task Force on Burnout could work with other ASCO committees to create specific criteria or guidelines for designing and managing a positive practice environment.
Recommendation 2b: ASCO could expand successful programs such as the QTP Collaboration (eg, QTP-hosted session on burnout) and publish results in formats that can be accessed by other practices. To widen their impact, these programs could be expanded for practice managers, delivered in other formats (eg, online modules or distance presentations), or published to reach a broader audience.
Recommendation 2c: ASCO could offer a Best Practices Recognition Program similar to the AMA Joy in Medicine Recognition Program to recognize exemplary institutions and practice environments63 and highlight awardees as “bright spots” or “inspiring stories” on the ASCO Web site (see AMA STEPS Forward Program for examples). The proposed ASCO Task Force on Burnout, Well-Being, and Professional Satisfaction could be tasked with developing criteria and metrics.
Recommendation 2d: ASCO could support the creation and testing of quality measures of burnout, resilience, and positive or negative workplace environment for inclusion in its quality measurements programs (Quality Oncology Practice Initiative [QOPI] or QOPI Certification Program). Because measures of workplace environment are not currently included as process or outcomes measures, there is a need to develop and pilot measures. The proposed task force could partner with ASCO experts, practice administrators, and other stakeholders in quality measurement to develop these measures. The AMA has published steps for organizations that could provide structure and could be linked to ASCO initiatives.5,62
Recommendation 3: Promote Research
Research on burnout in oncology remains limited and largely descriptive, and more studies are needed to clarify the causes of burnout; the relationships between burnout, moral distress, and compassion fatigue; and the effects of individual versus organizational interventions on reducing oncologist burnout and improving well-being. Workshop suggestions for future research are listed in the following subrecommendations.
Recommendation 3a: ASCO could collaborate with other cancer organizations and institutions to investigate how institutional stressors differ by setting and career experience. These descriptive data could be published in an existing annual ASCO report or other ASCO publications and used for further hypothesis-driven research (see recommendation 3b)
Recommendation 3b: ASCO and the cancer community should support descriptive and hypothesis-driven research to expand understanding of oncologist burnout, moral distress, and intervention outcomes. Descriptive studies are needed to understand risk factors, including common moral dilemmas faced by oncologists. Hypothesis-driven studies are needed to test associations between risk factors, interventions (structural and individual), and outcomes (eg, practice health, clinician well-being). Research studies could use qualitative and quantitative methods and data from retrospective (existing data repositories) and prospective designs.
CONCLUSION
As the previous discussion makes clear, burnout compromises clinician health and well-being, patient safety and quality of care, the economic strength of practices and institutions, and the future oncology workforce. Because the effects are so widespread, individual physicians, oncology practices and health care employers, professional societies such as ASCO, and other stakeholders (eg, Centers for Medicare and Medicaid Services, state medical boards, payers, regulators, and electronic health record vendors) all share responsibility for addressing the problem.5,6,8
ACKNOWLEDGMENT
The authors participated in and/or contributed to the ASCO Ethics Committee Roundtable: Burnout and Moral Distress at the 2019 ASCO annual meeting. Some authors are members of the ASCO Ethics Committee and acknowledge the support and feedback of committee members to this article. The authors would also like to acknowledge the contributions of the following participants who were not authors on this paper, but shared their knowledge and expertise at the Roundtable: Thomas LeBlanc, MD, MA; Piyush Srivastava, MD; Walter Birch, MBA;, John Cox, DO; Susana Banerjee, MA, MBBS, PhD; Kurt Demel, MD, MBA; Stephen Grubbs, MD.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Administrative support: Molly M. McGinnis
Provision of study materials: All authors
Collection and assembly of data: All authors
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
A Call to Action: Ethics Committee Roundtable Recommendations for Addressing Burnout and Moral Distress in Oncology
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jop/site/ifc/journal-policies.html.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Lynne P. Taylor
Research Funding: NeOnc Technologies (Inst), ImmunoCellular Therapeutics (Inst), Arbor Pharmaceuticals (Inst)
Jonathan M. Marron
Open Payments Link: https://openpaymentsdata.cms.gov/physician/802634/summary
Eric D. Tetzlaff
Consulting or Advisory Role: Blueprint Medicines
Travel, Accommodations, Expenses: Blue Print Pharmaceuticals
Konstantin Dragnev
Research Funding: G1 Therapeutics (Inst), Eli Lilly (Inst), Merck (Inst), Genentech (Inst), Novartis (Inst), Pharma Mar SA (Inst), Io Therapeutics (Inst)
Linda D. Bosserman
Employment: Front Line Medical Communications
Stock and Other Ownership Interests: Navigating Cancer
Honoraria: AstraZeneca, Genentech, Puma Biotechnology, National Comprehensive Cancer Network
Consulting or Advisory Role: UpToDate, Puma Biotechnology, NDP Partners, IntegraConnect, Bio Ascend, M3 USA
Speakers' Bureau: Puma Biotechnology
Sonali Smith
Consulting or Advisory Role: Pharmacyclics, Kite Pharma, AbbVie/Genentech, Gilead Sciences, Celgene, TG Therapeutics, Portola Pharmaceuticals, AstraZeneca, Bayer, Seattle Genetics, Bristol-Myers Squibb
Research Funding: Celgene, Pharmacyclics/Janssen, Acerta Pharma/AstraZeneca
Manali A. Patel
Consulting or Advisory Role: Celgene
Merry J. Markham
Research Funding: Aduro Biotech (Inst), Eli Lilly (Inst), Tesaro (Inst), Novartis (Inst), VBL Therapeutics (Inst)
Open Payments Link: https://openpaymentsdata.cms.gov/physician/890992/summary
Eduardo Bruera
Research Funding: Helsinn Healthcare (Inst)
Marie Brown
Employment: Edwards Lifesciences (I)
Stock and Other Ownership Interests: Edwards Lifesciences (I)
Honoraria: GlaxoSmithKline, Sanofi, Happify
Consulting or Advisory Role: Edwards Lifesciences (I), GORE (I), Boston Scientific (I), Happify
Research Funding: Edwards Lifesciences (I), GORE (I), Boston Scientific (I)
Travel, Accommodations, Expenses: Edwards Lifesciences (I), GORE (I), Boston Scientific (I)
Tait D. Shanafelt
Research Funding: Pharmacyclics (Inst), GlaxoSmithKline (Inst), Genentech (Inst), Celgene (Inst), Hospira (Inst), Cephalon (Inst), Polyphenon E International (Inst)
Patents, Royalties, Other Intellectual Property: Dr Shanafelt is co-inventor of the Physician Well-Being Index, Medical Student Well-Being Index, Nurse Well-Being Index, Well-Being Index, and the Participatory Management Leadership Index. Mayo Clinic holds the copyright to these instruments and has licensed them for use outside of Mayo Clinic. Dr. Shanafelt receives a portion of any royalties paid to Mayo Clinic.
Arif H. Kamal
Employment: Prepped Health, Acclivity Health
Leadership: Prepped Health, Acclivity Health
Stock and Other Ownership Interests: Acclivity Health
Consulting or Advisory Role: Insys Therapeutics, Medtronic, Huron Therapeutics, New Century Health, Compassus Hospice, AstraZeneca, Janssen Oncology, United Health Group
Research Funding: Cambia Health Foundation
Travel, Accommodations, Expenses: Janssen Oncology
No other potential conflicts of interest were reported.
REFERENCES
- 1.ASCO: Recognizing and preventing physician burnout ASCO Practice Central. https://practice.asco.org/practice-support/staff-recruiting-development/recognizing-preventing-physician-burnout.
- 2.Shanafelt TD, Gradishar WJ, Kosty M, et al. Burnout and career satisfaction among US oncologists. J Clin Oncol. 2014;32:678–686. doi: 10.1200/JCO.2013.51.8480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hlubocky FJ, Back AL, Shanafelt TD. Addressing burnout in oncology: Why cancer care clinicians are at risk, what individuals can do, and how organizations can respond. Am Soc Clin Oncol Educ Book. 2016;35:271–279. doi: 10.1200/EDBK_156120. [DOI] [PubMed] [Google Scholar]
- 4.Hlubocky FJ, Rose M, Epstein RM. Mastering resilience in oncology: Learn to thrive in the face of burnout. Am Soc Clin Oncol Educ Book. 2017;37:771–781. doi: 10.1200/EDBK_173874. [DOI] [PubMed] [Google Scholar]
- 5.Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177:1826–1832. doi: 10.1001/jamainternmed.2017.4340. [DOI] [PubMed] [Google Scholar]
- 6.Han S, Shanafelt TD, Sinsky CA, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170:784–790. doi: 10.7326/M18-1422. [DOI] [PubMed] [Google Scholar]
- 7.Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302:1284–1293. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- 8.National Academies of Sciences, Engineering, and Medicine . Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. Washington, DC: The National Academies Press; 2019. [PubMed] [Google Scholar]
- 9.Back AL, Deignan PF, Potter PA. Compassion, compassion fatigue, and burnout: Key insights for oncology professionals. Am Soc Clin Oncol Educ Book. 2019;34:e454–e459. doi: 10.14694/EdBook_AM.2014.34.e454. [DOI] [PubMed] [Google Scholar]
- 10.Shanafelt T, Dyrbye L. Oncologist burnout: Causes, consequences, and responses. J Clin Oncol. 2012;30:1235–1241. doi: 10.1200/JCO.2011.39.7380. [DOI] [PubMed] [Google Scholar]
- 11.Rushton C: UK Moral Distress Education Project http://moraldistressproject.med.uky.edu/sites/default/files/moral_distress_transcripts/Cynda%20Rushton.pdf
- 12.Dzeng E, Curtis JR. Understanding ethical climate, moral distress, and burnout: A novel tool and a conceptual framework. BMJ Qual Saf. 2018;27:766–770. doi: 10.1136/bmjqs-2018-007905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO: Burn-out an “occupational phenomenon”: International Classification of Diseases https://www.who.int/mental_health/evidence/burn-out/en/
- 14.Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600–1613. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 15.Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc. 2019;94:1681–1694. doi: 10.1016/j.mayocp.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 16.Bährer-Kohler S. New York, NY: Springer; 2013. Burnout for Experts: Prevention in the Context of Living and Working. [Google Scholar]
- 17.Brazeau CM, Shanafelt T, Durning SJ, et al. Distress among matriculating medical students relative to the general population. Acad Med. 2014;89:1520–1525. doi: 10.1097/ACM.0000000000000482. [DOI] [PubMed] [Google Scholar]
- 18.Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89:443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 19.West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: A prospective longitudinal study. JAMA. 2006;296:1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 20.Shanafelt TD, Raymond M, Horn L, et al. Oncology fellows’ career plans, expectations, and well-being: Do fellows know what they are getting into? J Clin Oncol. 2014;32:2991–2997. doi: 10.1200/JCO.2014.56.2827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: A systematic review and meta-analysis. JAMA Intern Med. 2017;177:195–205. doi: 10.1001/jamainternmed.2016.7674. [DOI] [PubMed] [Google Scholar]
- 22.Cavallo J. ASCO survey of oncologists finds high overall career satisfaction, but nearly half report burnout. https://www.ascopost.com/News/12904.
- 23.Allegra CJ, Hall R, Yothers G. Prevalence of burnout in the U.S. oncology community: Results of a 2003 survey. J Oncol Pract. 2005;1:140–147. doi: 10.1200/jop.2005.1.4.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91:836–848. doi: 10.1016/j.mayocp.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 25.Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: A time and motion study in 4 specialties. Ann Intern Med. 2016;165:753–760. doi: 10.7326/M16-0961. [DOI] [PubMed] [Google Scholar]
- 26.ASCO: American Society of Clinical Oncology position statement Pharmacy benefit managers and their impact on cancer care. https://www.ncoda.org/wp-content/uploads/2018/09/ASCO-Position-Statement-PBMs-Aug.-2018.pdf.
- 27.Bourdeanu L, Pieper BB, Cannistraci P, et al. Burnout among hematology/oncology nurse practitioners; Presented at the STTI 43rd Biennial Convention, Las Vegas, NV, November 7-11, 2015. [Google Scholar]
- 28.Hurria A, Lichtman SM, Gardes J.et aIdentifying vulnerable older adults with cancer: Integrating geriatric assessment into oncology practice J Am Geriatr Soc 551604–1608.2007 [DOI] [PubMed] [Google Scholar]
- 29.Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69:363–385. doi: 10.3322/caac.21565. [DOI] [PubMed] [Google Scholar]
- 30.Laor-Maayany R, Goldzweig G, Hasson-Ohayon I, et al. Compassion fatigue among oncologists: The role of grief, sense of failure, and exposure to suffering and death. Support Care Cancer. 2020;28:2025–2031. doi: 10.1007/s00520-019-05009-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oreskovich MR, Shanafelt T, Dyrbye LN, et al. The prevalence of substance use disorders in American physicians. Am J Addict. 2015;24:30–38. doi: 10.1111/ajad.12173. [DOI] [PubMed] [Google Scholar]
- 32.Oreskovich MR, Kaups KL, Balch CM, et al. Prevalence of alcohol use disorders among American surgeons. Arch Surg. 2012;147:168–174. doi: 10.1001/archsurg.2011.1481. [DOI] [PubMed] [Google Scholar]
- 33.Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: Suicidal ideation among American surgeons. Arch Surg. 2011;146:54–62. doi: 10.1001/archsurg.2010.292. [DOI] [PubMed] [Google Scholar]
- 34.Ahola K, Väänänen A, Koskinen A, et al. Burnout as a predictor of all-cause mortality among industrial employees: A 10-year prospective register-linkage study. J Psychosom Res. 2010;69:51–57. doi: 10.1016/j.jpsychores.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 35.Jameton A. Englewood Cliffs, NJ: Prentice-Hall; 1984. Nursing Practice: The Ethical Issues. [Google Scholar]
- 36.Rushton CH, Kaszniak AW, Halifax JS. A framework for understanding moral distress among palliative care clinicians. J Palliat Med. 2013;16:1074–1079. doi: 10.1089/jpm.2012.0490. [DOI] [PubMed] [Google Scholar]
- 37.Corley MC, Elswick RK, Gorman M, et al. Development and evaluation of a moral distress scale. J Adv Nurs. 2001;33:250–256. doi: 10.1046/j.1365-2648.2001.01658.x. [DOI] [PubMed] [Google Scholar]
- 38.Epstein EG, Hamric AB. Moral distress, moral residue, and the crescendo effect. J Clin Ethics. 2009;20:330–342. [PubMed] [Google Scholar]
- 39.Dudzinski DM. Navigating moral distress using the moral distress map. J Med Ethics. 2016;42:321–324. doi: 10.1136/medethics-2015-103156. [DOI] [PubMed] [Google Scholar]
- 40.Butcher L. Wellness: How neurologists in independent and academic practices are tackling burnout. https://journals.lww.com/neurotodayonline/Fulltext/2017/12070/Wellness__How_Neurologists_in_Independent_and.8.aspx.
- 41.Figley CR. Compassion Fatigue: Coping With Secondary Traumatic Stress Disorder in Those Who Treat the Traumatized. New York: Routledge; 1995. [Google Scholar]
- 42.Panagioti M, Geraghty K, Johnson J, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: A systematic review and meta-analysis. JAMA Intern Med. 2018;178:1317–1330. doi: 10.1001/jamainternmed.2018.3713. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 43.Montgomery A, Panagopoulou E, Esmail A, et al. Burnout in healthcare: The case for organizational change. BMJ. 2019;366:l4774. doi: 10.1136/bmj.l4774. [DOI] [PubMed] [Google Scholar]
- 44.Tawfik DS, Scheid A, Profit J, et al. Evidence relating health care provider burnout and quality of care: A systematic review and meta-analysis. Ann Intern Med. 2019;171:555. doi: 10.7326/M19-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 46.Tawfik DS, Profit J, Morgenthaler TI, et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clin Proc. 2018;93:1571–1580. doi: 10.1016/j.mayocp.2018.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358–367. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 48.Dyrbye LN, West CP, Hunderfund AL, et al. Relationship between burnout, professional behaviors, and cost-conscious attitudes among US physicians. J Gen Intern Med. doi: 10.1007/s11606-019-05376-x. [epub ahead of print on November 16, 2019] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shanafelt TD, Mungo M, Schmitgen J, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016;91:422–431. doi: 10.1016/j.mayocp.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 50.Windover AK, Martinez K, Mercer MB, et al. Correlates and outcomes of physician burnout within a large academic medical center. JAMA Intern Med. 2018;178:856–858. doi: 10.1001/jamainternmed.2018.0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.West CP, Dyrbye LN, Shanafelt TD. Physician burnout: Contributors, consequences and solutions. J Intern Med. 2018;283:516–529. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- 52.Faivre JC, Bibault JE, Bellesoeur A, et al. Choosing a career in oncology: Results of a nationwide cross-sectional study. BMC Med Educ. 2018;18:15. doi: 10.1186/s12909-018-1117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shanafelt TD, Raymond M, Kosty M, et al. Satisfaction with work-life balance and the career and retirement plans of US oncologists. J Clin Oncol. 2014;32:1127–1135. doi: 10.1200/JCO.2013.53.4560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mathew A. Global survey of clinical oncology workforce. J Glob Oncol. 2018;4:1–12. doi: 10.1200/JGO.17.00188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Institute of Medicine National Cancer Policy Forum . Ensuring Quality Cancer Care through the Oncology Workforce: Sustaining Care in the 21st Century—Workshop Summary. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 56.Yang W, Williams JH, Hogan PF, et al. Projected supply of and demand for oncologists and radiation oncologists through 2025: An aging, better-insured population will result in shortage. J Oncol Pract. 2014;10:39–45. doi: 10.1200/JOP.2013.001319. [DOI] [PubMed] [Google Scholar]
- 57.Debono D. Coping with the oncology workforce shortage: Transitioning oncology follow-up care to primary care providers. J Oncol Pract. 2010;6:203–205. doi: 10.1200/JOP.777005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kirkwood MK, Bruinooge SS, Goldstein MA, et al. American Society of Clinical Oncology workforce information system with geographic distribution of oncologists and comparison of data sources for the number of practicing oncologists. J Oncol Pract. 2014;10:32–38. doi: 10.1200/JOP.2013.001311. [DOI] [PubMed] [Google Scholar]
- 59.Doximity: 2018 Oncologist National Workforce Study https://www.doximity.com/oncologist_workforce_study
- 60.American Society of Clinical Oncology The state of cancer care in America, 2017: A report by the American Society of Clinical Oncology. J Oncol Pract. 2017;13:e353–e394. doi: 10.1200/JOP.2016.020743. [DOI] [PubMed] [Google Scholar]
- 61.West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016;388:2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 62.Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Mayo Clin Proc. 2017;92:129–146. doi: 10.1016/j.mayocp.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 63.American Medical Association Creating the organizational foundation for joy in medicine. https://edhub.ama-assn.org/steps-forward/module/2702510.
- 64.Wright AA, Katz IT. Beyond burnout: Redesigning care to restore meaning and sanity for physicians. N Engl J Med. 2018;378:309–311. doi: 10.1056/NEJMp1716845. [DOI] [PubMed] [Google Scholar]
- 65.Dyrbye LN, Shanafelt TD, Gill PR, et al. Effect of a professional coaching intervention on the well-being and distress of physicians: A pilot randomized clinical trial. JAMA Intern Med. doi: 10.1001/jamainternmed.2019.2425. [epub ahead of print on August 5, 2019] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Shanafelt TD, Schein E, Minor LB, et al. Healing the professional culture of medicine. Mayo Clin Proc. 2019;94:1556–1566. doi: 10.1016/j.mayocp.2019.03.026. [DOI] [PubMed] [Google Scholar]
- 67.Managing stress and burnout in oncology Focus on staff. J Oncol Pract 2006;2:130–131. doi: 10.1200/jop.2006.2.3.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: A randomized clinical trial. JAMA Intern Med. 2014;174:527–533. doi: 10.1001/jamainternmed.2013.14387. [DOI] [PubMed] [Google Scholar]
- 69.Shanafelt TD, Gorringe G, Menaker R, et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90:432–440. doi: 10.1016/j.mayocp.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 70.Potter P, Deshields T, Berger JA, et al. Evaluation of a compassion fatigue resiliency program for oncology nurses. Oncol Nurs Forum. 2013;40:180–187. doi: 10.1188/13.ONF.180-187. [DOI] [PubMed] [Google Scholar]
- 71.American Medical Association STEPS Forward. https://edhub.ama-assn.org/steps-forward.
- 72.Ramirez AJ, Graham J, Richards MA, et al. Mental health of hospital consultants: The effects of stress and satisfaction at work. Lancet. 1996;347:724–728. doi: 10.1016/s0140-6736(96)90077-x. [DOI] [PubMed] [Google Scholar]
- 73.Trockel MT, Hamidi MS, Menon NK, et al. Self-valuation: Attending to the most important instrument in the practice of medicine. Mayo Clin Proc. 2019;94:2022–2031. doi: 10.1016/j.mayocp.2019.04.040. [DOI] [PubMed] [Google Scholar]
- 74.Brown RF, Butow P, Aldridge J, et al. The impact of consultations skills training in shared decision-making on doctor behavior, confidence and stress and burnout: A randomized controlled trial. Psychooncology. 2014;23:148–149. [Google Scholar]
- 75.National Academy of Medicine Taking action against clinician burnout: A systems approach to professional well-being. https://nam.edu/systems-approaches-to-improve-patient-care-by-supporting-clinician-well-being/ [PubMed]
- 76.American Academy of Family Physicians National Academy of Medicine: Action Collaborative on Clinician Well-Being and Resilience. https://www.aafp.org/membership/benefits/physician-health-first/phf/nam-collaborative.html.
- 77.National Center for Human Factors in Healthcare Electronic health record (EHR) safety and usability: See what we mean. https://ehrseewhatwemean.org/
- 78.American College of Physicians Physician well-being and professional fulfillment. https://www.acponline.org/practice-resources/physician-well-being-and-professional-fulfillment.
- 79.Cass I, Duska LR, Blank SV, et al. Stress and burnout among gynecologic oncologists: A Society of Gynecologic Oncology evidence-based review and recommendations. Gynecol Oncol. 2016;143:421–427. doi: 10.1016/j.ygyno.2016.08.319. [DOI] [PubMed] [Google Scholar]
- 80.Society of Gynecologic Oncology SGO wellness initiative: Finding work-life balance. https://www.sgo.org/clinical-practice/sgo-wellness/
- 81.Society of Gynecologic Oncology SGO wellness perspectives. https://www.sgo.org/clinical-practice/sgo-wellness/sgo-wellness-initiatives/
- 82. ASCO: ASCO 2019-2023 strategic plan. https://www.asco.org/sites/new-www.asco.org/files/content-files/about-asco/pdf/2018-ASCO.org-Strategic-Plan.pdf.
- 83. ASCO: ASCO publications: Burnout. https://ascopubs.org/action/doSearch?SeriesKey=edbk&AllField=burnout&ConceptID=
- 84.Cotton K. Resilience while caring for seriously ill patients: Skills and strategies to prevent burnout. https://connection.asco.org/tec/career/resilience-while-caring-for-seriously-ill-patients.
- 85. ASCO: Physician wellness and professional burnout. https://connection.asco.org/physician-wellness.
- 86. ASCO Practice Central: ASCO Quality Training Program. https://practice.asco.org/quality-improvement/quality-programs/quality-training-program.
- 87.Tetzlaff ED, Hylton HM, DeMora L, et al. National study of burnout and career satisfaction among physician assistants in oncology: Implications for team-based care. J Oncol Pract. 2018;14:e11–e22. doi: 10.1200/JOP.2017.025544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. ASCO: More than one-third of physician assistants in oncology experience burnout, despite high rate of career satisfaction. https://www.asco.org/about-asco/press-center/news-releases/more-one-third-physician-assistants-oncology-experience.
- 89.Lee SY. Adapting oncology fellowship to reflect contemporary practice. J Oncol Pract. 2019;15:1–2. doi: 10.1200/JOP.18.00551. [DOI] [PubMed] [Google Scholar]