Abstract
Health researchers have investigated the association between racial segregation and racial health disparities with multilevel approaches. This study systematically reviews these multilevel studies and identifies broad trends and potential directions for future research on racial segregation and health disparities in the US. After searching databases including CINAHL and MEDLINE, we identified and systematically reviewed 66 articles published between 2003 and 2019 and found four major gaps in racial/ethnic segregation and health disparities: (a) the concept of segregation was rarely operationalized at the neighborhood level, (b) except for the evenness and exposure dimension, other dimensions of segregation are overlooked, (c) little attention was paid to the segregation between whites and non-black minorities, particularly Hispanics and Asians, and (d) mental health outcomes were largely absent. Future directions and opportunities include: First, other segregation dimensions should be explored. Second, the spatial scales for segregation measures should be clarified. Third, the theoretical frameworks for black and non-black minorities should be tested. Fourth, mental health, substance use, and the use of mental health care should be examined. Fifth, the long-term health effect of segregation has to be investigated, and finally, other competing explanations for why segregation matters at the neighborhood level should be answered.
Keywords: racial/ethnic segregation, health disparities, minority health, neighborhood
Introduction
The association between segregation and health have been explored with ecological data analysis. While this approach provides some insight, its findings cannot be generalized to individual level due to factors such as the ecological fallacy. Thus, the mechanisms linking segregation to individual health outcomes were underexplored (Acevedo-Garcia, Lochner, Osypuk, & Subramanian, 2003). However, with the rapid growth in geographical data and advances in research methods multilevel modeling allows researchers to nest individuals within different levels of residential context. This offers the opportunity to investigate how segregation “gets under the skin” and as such multilevel modeling emerged as a major analytic approach in the literature of segregation and health (Entwisle, 2007).
In 2003, Acevedo-Garcia and colleagues called for the development of a multilevel research framework that could be used to clarify the associations of racial/ethnic residential segregation (hereafter racial/ethnic segregation) with individual health outcomes. They also suggested that there was a need to examine how racial/ethnic segregation affects the health of non-black minorities, particularly Hispanics and Asians (Acevedo-Garcia et al., 2003). These recommendations not only correspond to the argument that racial/ethnic segregation should be regarded as a fundamental cause of health disparities between blacks and whites (Williams & Collins, 2001), but also underscore the insufficient attention to the health disparities between rapidly growing minority groups and the dominant group.
This systematic review has three goals: First, to review the literature that has been published since 2003 that used a multilevel research framework to investigate the relationships between racial/ethnic segregation and health; second, to evaluate the extent to which racial/ethnic segregation may account for health disparities, and third, to discuss future research directions in this area.
In contrast to other reviews (Kramer & Hogue, 2009; White & Borrell, 2011), this study is unique in the following ways. We proposed two theoretical frameworks drawn from the segregation and migration literature for black and non-black groups, respectively, which may guide future research. Furthermore, this study pays extra attention to the units of analysis and spatial scale of segregation measures. Finally, our review allows us to identify current existing gaps in the racial/ethnic segregation and health disparities literature, and to recommend several avenues for future work.
Before launching in to the strategy used in our systematic review, additional context is required. We focus on three main themes. First, racial/ethnic health disparities are defined as the differences in an array of health outcomes and behaviors across race/ethnicity groups (DHHS, 2010) that are commonly interpreted as whites sharing a better health profile than do minorities, especially blacks, in the United States (US). This common perception is reflected by previous studies on the relationships between racial/ethnic segregation and health disparities (Kramer & Hogue, 2009; Williams & Collins, 2001). However, racial/ethnic health disparities vary by health indicators and minorities outperform whites in some outcomes. For example, asthma attacks among persons with current asthma and suicide rates are the lowest among blacks, Hispanics have the lowest stroke death and hypertension rates, and Asians report the lowest prevalence of binge drinking and coronary heart disease death rates (CDC, 2013). These variations should be further incorporated into the notion that racial/ethnic segregation is a fundamental cause of racial/ethnic health disparities (Williams & Collins, 2001).
Second, the concept of segregation is defined as the extent to which two or more social groups are spatially differentiated across subunits that comprise a main unit of interest, typically a metropolitan area (Massey & Denton, 1988). It is important to note that racial/ethnic segregation and racial/ethnic composition (i.e., diversity) are conceptually different (Lee, Iceland, & Farrell, 2014). The former is concerned about how two or more race/ethnicity groups distribute spatially across neighborhoods within a large area (e.g., a metropolitan area), whereas the latter refers to the relative size of race/ethnicity groups in an area (i.e., racial composition). A diverse metropolitan area may be more or less segregated if members of various races live in isolation or share the same neighborhoods. Researchers have found modest empirical associations between diversity and segregation (DeFina & Hannon, 2009). Segregation and diversity may be related but they do not necessarily affect each other in the same way.
Third, since the work of Massy and Denton (1988), segregation is seen as consisting of five dimensions, namely evenness, exposure, concentration, centralization, and clustering. Evenness captures the level of differential spatial distribution of groups across the main units (e.g., metropolitan areas or counties); exposure refers to the probability of interacting with other groups; concentration measures the physical space inhabited by certain groups; centralization indicates the degree to which a group is located at the center of an area; and clustering refers to the level to which the subunits occupied by minority members adjoin one another within the main unit. Each dimension represents a unique spatial distribution pattern of race/ethnicity groups within an area (Iceland & Weinberg, 2002; Reardon & O’Sullivan, 2004) and the five dimensions may not be highly related to one another (Wilkes & Iceland, 2004). Most of the measures are created for metropolitan areas or large unit statistics, rather than neighborhood (or other smaller) levels. Thus, their relationships with racial/ethnic health disparities may be discordant.
Review Articles Selection Process
We created a custom search tool to conduct bibliographic searches of databases, such as MEDLINE, CINAHL, ERIC, Health Sources, Social Science, JSTOR, and Psychology and Behavioral Sciences Collection (the complete list is available upon request). The literature search process is similar to previous studies (Haley et al., 2016; Kramer & Hogue, 2009) and the so-called scoping reviews (Levac, Colquhoun, & O’Brien, 2010). We focus on papers published between January 1, 2003, and December 31, 2019, i.e., papers published in the same year as Acevedo-Garcia and colleagues’ paper and thereafter. We conducted a general search where the indexing terms “segregation,” “health,” and “multilevel” were used. Variants or alternatives of these three terms were also applied to ensure a thorough coverage, such as “multi-level,” “mortality,” and “morbidity.”
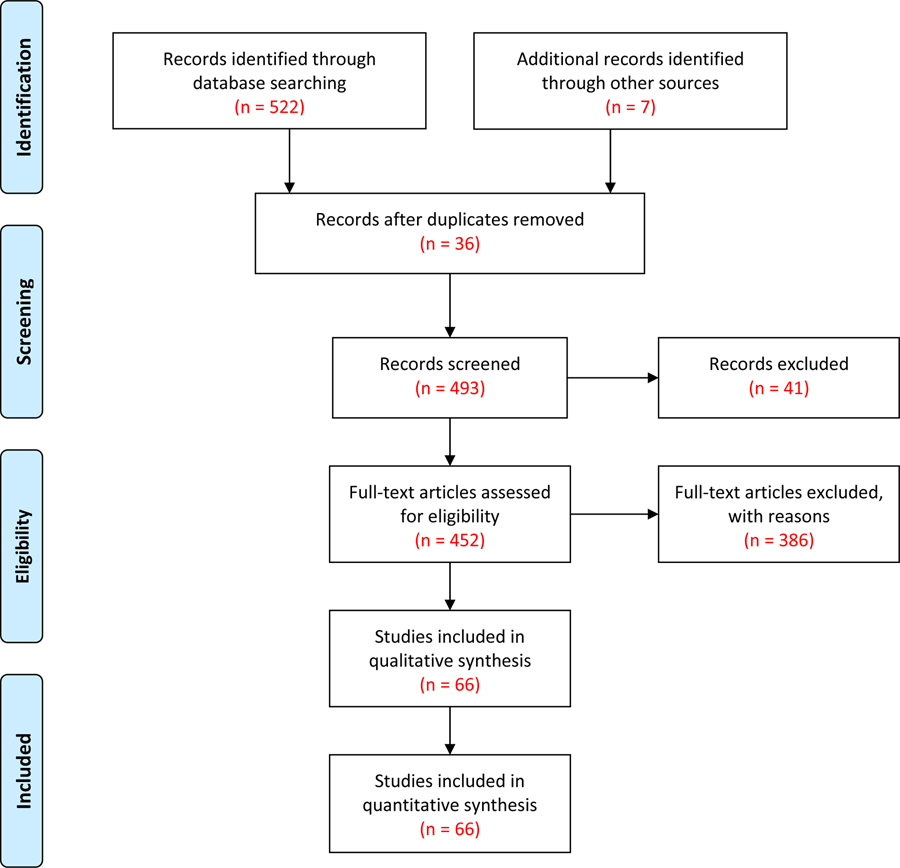
The initial search yielded 529 articles of which we excluded 36 duplicated articles and 41 articles that used the term “segregation” to describe the molecular, genetic, cell, and chromosome clusters. We reviewed the remaining 452 articles and found that (a) 86 articles did not focus on the US, (b) 48 articles were not empirical studies, (c) 57 articles did not use health outcomes or behaviors as their dependent variables, (d) 170 articles employed the segregation measures that did not reflect the definition of segregation discussed previously (also see below), and (e) 25 articles did not adopt a multilevel analysis approach (i.e., individuals within an area). These articles are excluded and the selection process is shown in Figure 1. At the end of the process, 66 articles remained and these then form the basis of our systematic review.
Figure 1.
PRISMA Flow Diagram of This Study
Results
The 66 articles that met our criteria are listed in chronological order of publication date in Table 1. Table 1 catalogues the author(s) and the main dimensions of each individual study (geographical units, segregation measures, comparison groups, health outcomes, and key findings). We summarize our observation on each of these five dimensions below.
Table 1.
Summary of reviewed studies that used multilevel modeling to investigate the relationship between racial segregation and health
| Authors (Year) | Geographic Unit (Neighborhood Unit) | Segregation Measure | Comparison Groups | Health Outcome | Key Findings |
| Subramanian et al. (2005) | Metropolitan area (Census tract) | Dissimilarity index (evenness) Isolation index (exposure) | Dissimilarity: Blacks vs. Whites. Isolation: Blacks vs. Others. | Self-rated health | 1. High black isolation was associated with increased odds of poor self-rated health among blacks (using cross-level interaction between black isolation index and black). |
| Bell et al. (2006) | Metropolitan area (Census tract) | Isolation index (exposure) Spatial proximity (clustering) | Blacks vs. Whites. | Birth weight; Preterm birth; Intrauterine growth restriction | 1. Higher isolation was related to lower birth weight, higher odds of prematurity and higher rates of fetal growth restriction. 2. Higher clustering was associated with higher birth weight and lower odds of premature birth. |
| Chang (2006) | Metropolitan area (Census tract) | Isolation index (exposure) | Blacks vs. Whites. | Body mass index (BMI) | 1. Among non-Hispanic blacks, racial isolation increased BMI and odds of being overweight. No association was found for non-Hispanic whites. |
| Grady (2006) | New York City (Census tract) | Local spatial segregation index (exposure with consideration of spatial structure) | Blacks vs. Others. | Low birth weight | 1. Neighborhood segregation was positively associated with the odds of being low birth weight (< 2,500 grams). |
| Lopez (2006) | Metropolitan area (Census tract) | Dissimilarity index (evenness) | Blacks vs. Whites. | Physical activity (<10 minutes/week of moderate or vigorous physical activity) | 1. Segregation was positively related to the risk of being physically inactive and this relationship was found for Whites. |
| Mobley et al. (2006) | ZIP code (Neighborhood definition not specified) | Isolation index (exposure) *(a) | Not Specified. | Body mass index; Coronary heart disease risk (CHD) | 1. Segregation was negatively associated with CHD risk among Black, Hispanic, and Asian women and positively associated with CHD risk among American Indian women. This finding was found using interaction between individual race/ethnicity and isolation index. |
| Robert & Ruel (2006) | County (Census tract) | Dissimilarity index (evenness) | Blacks vs. Whites. | Self-rated health | 1. In the NSFH (National Survey of Families and Households), there was a positive association between county racial segregation and poorer self-rated health among Whites but not Blacks. 2. In the ACL (Americans’ Changing Lives), there was no statistically significant association between racial segregation and self-rated health. |
| Grady & McLafferty (2007) | New York City (Census tract) | Local spatial segregation index (exposure with a consideration of spatial structure) | Blacks vs. Others. | Low birth weight | 1. For U.S.-born Black women, segregation was associated with a higher odds of being low birth weight. |
| Lee & Ferraro (2007) | Neighborhood Cluster *(b) (Census block) | Isolation index and Interaction index (both exposure) | Isolation: Puerto Rican American vs. Others. Mexican American vs. Others. Interaction: Puerto Rican American vs. African American. Mexican American vs. African American. |
Acute physical symptoms and Disability (instrumental activities of daily living) | 1. Segregation was positively related to health problems for Puerto Rican Americans (not for Mexican Americans). 2. Cross-level interaction between generation and origin showed that segregation protects second or later generation of Mexican Americans from disability and physical symptoms. |
| Grady & Ramirez (2008) | New York City (Census tract) | Local spatial segregation index (exposure with a consideration of spatial structure) | Blacks vs. Whites. | Maternal and infant risk factors (Low birth weight) | 1. Segregation was positively associated with the odds of having a low birth weight infant for African-American and White women. |
| Osypuk & Acevedo-Garcia (2008) | Metropolitan area (Census tract) | Hypersegregation *(c) | Blacks vs. Whites. | Preterm birth (PTB) | 1. Black infants in hypersegregated metropolitan areas were more likely to be preterm than Black infants in non-hypersegregated metropolitan areas. 2. Hypersegregaion was positively associated with Black-White PTB disparities. 3. The age-PTB association for blacks was worse in hypersegregated areas (3-way interaction). |
| Haas et al. (2008) | County (Census tract) | Isolation index (exposure) | Blacks vs. Whites. Hispanics vs. Whites. | Breast Cancer Care and Mortality | 1. Higher black segregation were associated with worse breast cancer care for both blacks and whites, but not associated with mortality. 2. Higher Hispanics segregation were associated with worse breast cancer care for both Hispanics and whites, but not associated with mortality. |
| Haas et al. (2008) | County (Census tract) | Isolation index (exposure) | Blacks vs. Whites. Hispanics vs. Whites. | Early versus. Late stage diagnosis of cancer (breast, colorectal, prostate, and lung) | 1. Black/white disparities in early-stage cancer diagnosis (except lung) are the largest in low segregation areas. 2. Hispanic/white disparity in early-stage diagnosis was less obvious, but the largest disparity in breast cancer was observed in low segregation areas. |
| Lee (2009) | Neighborhood Cluster *(b) (Census block) | Isolation index (exposure) | Puertorican American vs. Others. Mexican American vs. Others. | Depressive symptoms and anxiety | 1. Neighborhood segregation was positively associated with depressive symptoms and anxiety among Mexican Americans, rather than Puerto Rican Americans. |
| Walton (2009) | Metropolitan area (Census tract) | Isolation index (exposure) Spatial proximity (clustering) | Isolation: Asian vs. Whites. Hispanics vs. Whites. Blacks vs. Whites. Spatial Proximity (clustering): Asian vs. Whites. Hispanics vs. Whites. Blacks vs. Whites. |
Birth weight | 1. Segregation was negatively related to the odds of having a low birth weight baby among Asian Americans. 2. Segregation marginally increased the odds of low birth weight among African Americans after taking poverty into account. Segregation does not affect birth weight among Latino Americans. |
| Grady (2010) | Detroit Metropolitan Area (Automated zone) *(d) | Spatial isolation index (exposure with a consideration of spatial structure) G* (clustering) | Blacks vs. Others. | Low birth weight | 1. High segregation was associated with a higher risk of having low birth weight infants and the disparities in having low birth weight infants between black mothers and others was less in racially isolated areas. 2. Segregation was also related to a higher odds of having preterm births and the disparities in having preterm births between black mothers and others was reduced in racially clustered areas. |
| Kramer et al. (2010) | Metropolitan area (Census tract) | Isolation index (exposure) Dissimilarity index (evenness) both consider spatial structure | Blacks vs. Others. Whites vs. Others. | Preterm birth | 1. For Black mothers, isolation was associated with very preterm birth and moderately preterm birth. |
| Mellerson et al. (2010) | Metropolitan area (Census tract) | Dissimilarity index (evenness) | Hispanics vs. Whites. | Exercise | 1. For Hispanics, the odds of exercise was lower when living in highly segregated areas than in non-segregated areas. |
| Osypuk et al. (2010) | Metropolitan area (Census tract) | Interaction index (exposure) | Mexican Immigrant vs. other Mexican Immigrant. Mexican Immigrant vs. US-born Mexican-origin. US-born Mexican-origin vs. US-born Mexican-origin. US-born Mexican-origin vs. Mexican Immigrant. |
Birth weight | 1. Living in metropolitan areas with high segregation of US-born Mexican-origin residents was associated with lower infant birth weights for US-born Mexican-origin mothers. |
| Bellatorre et al. (2011) | Metropolitan area (Census tract) | Dissimilarity index (evenness) Interaction index (exposure) | Multi-group measures but not specified | Total allostatic load (AL) and inflammatory response AL | 1. Inflammatory response AL was positively related to both the evenness and exposure domains of segregation and this relationship did not differ by race/ethnicity. 2. The positive relationship between total AL and segregation was not found till the cross-level interactions between race/ethnicity and segregation measures were considered. |
| Debbink & Bader (2011) | Michigan Metropolitan area (Census tract) | Local isolation index (exposure with a consideration of spatial structure) | Blacks vs. Whites. | Low birth weight | 1. Odds of low birth weight was higher in segregated neighborhoods in Michigan metropolitan area. |
| Hao et al. (2011) | County (Census block) | Isolation index (exposure) | Blacks vs. Whites. | Health-related quality of life (HRQOL) *(e) | 1. HRQOL was poorer among cancer survivors living in highly segregated counties, whereas individual race/ethnicity was no longer significant. |
| Kershaw et al. (2011) | Metropolitan area (Census tract) | Isolation index (exposure) | Blacks vs. Whites. | Black-White disparities in hypertension | 1. Racial disparities in the odds of hypertension were significantly smaller in low-than in high-segregation areas. 2. Race-segregation interaction showed that the race-hypertension association was modified by racial segregation, increasing hypertension for blacks but decreasing for whites. |
| Anderson (2012) | Metropolitan area (Census tract) | Isolation index (exposure) | Blacks vs. Whites. | Health-care coverage | 1. For blacks, higher segregation was associated with lower odds of having health insurance. |
| Corral et al. (2012) | Metropolitan area (Census tract) | Isolation index (exposure) | Blacks vs. Whites. | Overweight/Obesity, exercise and fruit/vegetable consumption | 1. African Americans living in moderate segregation areas were more likely to consume 5+fruit or vegetable per day than their counterparts in low segregation areas. 2. African Americans in high segregation areas were more likely to be obese/overweight than those in low segregation areas. |
| Russell et al. (2012) | Metropolitan area/Micropolitan area[MiA] (Census tract) | Theil’s information theory index (evenness) | Not specified. | Breast cancer mortality, all-cause mortality | 1. For black women, as MA/MiA segregation increased, the risk for breast cancer mortality increased. Interaction between race and segregation was used to find the racial difference. |
| Biello et al. (2013) | Metropolitan area (Census tract) | Hypersegregation *(c) | Blacks vs. Whites. | Sexually transmitted infections (STIs) | 1. Hypersegregation was not associated with the sex risk index. |
| Biello et al. (2013) | Metropolitan area (Census tract) | Dissimilarity index (evenness) Isolation index (exposure) Relative concentration index (concentration) Absolute centralization index (centralization) Spatial proximity index (clustering) Hypersegregation *(d) | Blacks vs. Whites (implicit). | Age at first sexual intercourse | 1. High segregation was related to early age at first sexual intercourse, but isolation seems to show a U-shape effect on the dependent variable. 2. The interaction between individual race and segregation, to some extent, suggested that segregation may modify the relationship between race and age at first intercourse. 3. The adverse effect of segregation was multiplied in hypersegregated areas. |
| Britton & Shin (2013) | Metropolitan area (Census tract) | P-star index (isolation/exposure) Dissimilarity index (evenness) | P-star index: Mexican Immigrants vs. US-born Mexican-origin residents. Blacks vs. others. Dissimilarity: Blacks vs. Whites. Mexican immigrant vs. Whites. US-born Mexican vs. Whites. |
Very preterm birth | 1. Segregation was positively associated with very preterm birth for both African American and Mexican-origin women, but this association was robust across different measures of segregation only for African Americans. |
| Jones (2013) | Metropolitan area (Census tract) | Hypersegregation *(c) | Blacks vs. Whites. | Hypertension | 1. Segregation was positively related to hypertension and contributed to hypotension more in extremely hypersegregated areas than do individual characteristics. |
| Kershaw et al. (2013) | Metropolitan area (Census tract) | Isolation index (exposure) | Blacks vs. Others. Hispanics vs. Others. | Obesity (BMI) | 1. There was no relationship between segregation and obesity among men. For black women, high segregation was associated with high obesity. 2. Mexican-American women living in high segregation areas had lower obesity. |
| Mendez et al. (2013) | Metropolitan area (Census tract) | Dissimilarity (evenness) Isolation and interaction index (both exposure) | Blacks vs. Whites. | Preterm birth | 1. Residential segregation was not associated with preterm birth among this sample of women. |
| Nelson (2013) | Metropolitan area (Census tract) | Dissimilarity (evenness) | Hispanic vs. Whites. | Self-rated health (SRH) | 1. Residential Segregation was associated with poorer SRH for Hispanics and Mexicans. 2. For Cubans, residential segregation was related to better SRH. |
| Anderson & Fullerton (2014) | Metropolitan area (Census tract) | Isolation index (exposure) | Latino vs. Others. | Self-rated health (SRH) Personal Physician Health-care Coverage | 1. For Latinos, Latino segregation was associated with poorer SRH and lower odds of having a personal physician and health insurance. 2. For Whites, Latino segregation was not related to the outcomes. |
| Corral et al. (2014) | Metropolitan area (Census tract) | Isolation index (exposure) | Hispanic vs. Whites. | Obesity (BMI) | 1. Living in highly segregated metropolitan areas increased the odds of being obese for Hispanics. |
| Greer et al. (2014) | Metropolitan area (Census tract) | Isolation index (exposure) | Blacks vs. Others. | Cardiovascular mortality | 1. Among blacks, segregation was positively related to heart disease mortality rates in young and old age groups. But it was only associated with stroke mortality rates in old age group. 2. Among whites, segregation was associated with heart disease mortality rates in young and old age groups. |
| Kershaw et al. (2014) | Metropolitan or Micropolitan area (Census tract) | Isolation index (exposure) | Hispanics vs. Others. | Obesity (BMI) | 1. Among Hispanic men, segregation was unassociated with BMI. 2. Segregation was positively related to BMI among Hispanic whites but negatively associated with BMI among Hispanic Blacks. |
| Plascak et al. (2014) | City or Town (place- level) (Neighborhood definition not specified) |
Gini coefficient (evenness) | Blacks vs. Whites. | Diagnostic time to resolution | 1. Living in segregated area was not associated with diagnostic time to resolution following an abnormal breast or cervical cancer screening test. |
| Yang et al. (2014) | County (Census tract) | Interaction index (exposure) | Blacks vs. Whites. Asians vs. Whites. Hispanics vs. Whites. | Maternal Smoking during pregnancy | 1. Living in a less racially segregated area was related to a lower probability of smoking during pregnancy for black women. 2. Living in a racially segregated area increased the probability of maternal smoking for Asian women and Hispanic women. |
| Yi et al. (2014) | United Hospital Fund (UHF) Neighborhood in New York City (Zip code) | Isolation index (exposure) | Blacks vs. Others. Hispanics vs. Others. Asians vs. Others. | Biomarkers of sodium and potassium consumption | 1. Higher Hispanic segregation was related to lower potassium intake. 2. Higher Black and Hispanic segregation was associated with higher sodium-potassium ratio. 3. Higher Asian segregation was related to lower sodium-potassium ratio. |
| Bower et al. (2015) | Metropolitan area (Census tract) | Isolation index (exposure) | Blacks vs. Others. | Obesity | 1. Among black women, residential segregation was positively associated with odds of obesity. |
| Britton & Velez (2015) | Metropolitan area (Census tract) | P-Star index (isolation/exposure) Dissimilarity index (evenness) | Puerto Rican. Vs. Others. Puerto Rican. Vs. Anglos. | Preterm birth | 1. Among Puerto Rican women, Puerto Rican residential segregation was positively related to the risk of very preterm birth. 2. Among US-born women, it was not related to preterm birth outcomes. |
| Grigsby-Toussaint et al. (2015) | Metropolitan area (Neighborhood definition not specified) | Hypersegregation *(c) | Latinos vs. Whites. | Diabetes risk | 1. Among Latinos, level of segregation was not associated with diabetes risk. |
| Kovalchik et al. (2015) | County (Census tract) | Isolation index (exposure) | Blacks vs. Whites. Hispanics vs. Whites. | Cognitive ageing | 1. Higher Hispanic segregation was associated with greater cognitive function at baseline and higher cognitive decline over 10-year period. 2. Black segregation was not related to cognitive ageing. |
| Lutfi et al. (2015) | Core-based statistical areas (CBSAs) (Census tract) | Dissimilarity index (evenness) Isolation index (exposure) Relative concentration index (concentration) Absolute centralization index (centralization) Spatial proximity index (clustering) Hypersegregation *(d) | Blacks vs. Whites. | Risky sexual behavior 1. # of partners in the past year 2. condom use at last sex 3. Composite index of the previous two |
1. Among non-Hispanic blacks, higher centralization and concentration showed strong associations with risky sexual behavior. |
| Piontak et al. (2016) | County (Census tract) | Dissimilarity index (evenness) | Blacks vs. Whites. Hispanics vs. Whites. | Childhood obesity | 1. For students, living in minority-segregated area was higher associated with obesity than those in less segregated area. 2. The association was not statistically significant once school-level poverty was controlled. |
| Plascak et al. (2016) | Zip-Code (Census block) | Gini coefficient (evenness) | Latinos vs. Whites. | Self-rated health (SRH) | 1. The relationship between the Latino residential segregation and SRH was U shaped. 2. In lower segregated area, increases in Latino segregation was negatively associated with SRH, while in higher segregated area, increases in Latino segregation was positively associated with SRH. |
| Caldwell et al. (2017) | County (Census tract) | Isolation index (exposure) | Blacks vs. others Hispanics vs. others | Access to healthcare | 1. Living in rural areas with high segregation was associated with worse access to health care among both blacks and Hispanics. 2. Living in rural areas with high segregation was positively associated with the odds of reporting their health care needs were met among both blacks and Hispanics. |
| Harvey et al. (2017) | County (Census tract) | Dissimilarity index (evenness) | Hispanics vs. Others | Late stage melanoma diagnosis (LSMD) | 1. Segregation was not associated with the odds of LSMD. |
| Mobley et al. (2017) | County (Neighborhood definition not specified) | Isolation index (exposure) | Blacks vs. whites Hispanics vs. whites Asians vs. whites | Breast cancer mammography use | 1. Living in highly segregated Hispanic neighborhood was associated with increased odds of mammography use. 2. Living in highly segregated black or Asian neighborhood was associated with decreased odds of mammography use. |
| Mobley et al. (2017) | County (Census tract) | Isolation index (exposure) | Blacks vs. others Hispanics vs. others Asians vs. others | Colorectal cancer (CRC) diagnosis | 1. Living in highly segregated black neighborhood was associated with lower odds of late-stage CRC diagnosis. 2. Living in highly segregated Asian neighborhood was associated with higher odds of late-stage CRC diagnosis. 3. Living in highly segregated Hispanic neighborhood showed no significant association. |
| Mobley et al. (2017) | County (Census tract) | Isolation index (exposure) | Whites vs. others Blacks vs. others Hispanics vs. others Asians vs. others | Breast cancer diagnosis | 1. Living in a highly isolated Asian community was associated with lower odds of late-stage breast cancer diagnosis. 2. Living in a highly isolated White community was associated with higher odds of late-stage breast cancer diagnosis. |
| Nobles et al. (2017) | Metropolitan area (Census tract) | Dissimilarity index (evenness) Isolation index (exposure) | Latinos vs. Others | Mental distress | 1. Higher Latino isolation was associated with lower level of mental distress. 2. Higher dissimilarity index was associated with lower level of mental distress among men, but not among women. |
| Ojinnaka et al. (2017) | County (Census tract) | Isolation index (exposure) | Blacks vs. whites | Surgical treatment of early-stage breast cancer | 1. Living in highly segregated areas was associated reduced odds of surgical treatment of early-stage breast cancer. 2. Blacks living in highly segregated areas were less likely to receive surgical treatment than their counterparts living in areas with lower level of segregation. |
| Pennap et al. (2017) | County (Neighborhood definition not specified) | Isolation index (exposure) | Hispanics vs. Others | Attention-deficit/hyperactivity disorder (ADHD) diagnosis and stimulant use | 1. Hispanics living in segregated areas are less likely to receive an ADHD diagnosis and stimulant use than Hispanics living in less segregated areas. |
| Yang et al. (2017) | Census tract (Census block) | Entropy (evenness) Isolation (exposure) Absolute centralization index (centralization) Delta index (concentration) Spatial proximity index (clustering) | Whites vs. Blacks Whites vs. Hispanics | Self-rated health (SRH) | 1. High white/black concentration widened the SRH disparities between whites and blacks. 2. Higher levels of white/Hispanic centralization were associated with narrower gaps in SRH. 3. There was no single dimension of segregation that statistically outperforms others. |
| Goodman et al. (2018) | County (Census tract) | Dissimilarity & Entropy (evenness) Isolation, Correlation, & Local spatial segregation index (exposure) | Blacks vs. Whites | Body mass index | 1. Racial residential segregation (evenness and exposure) was positively associated with individual body mass index. |
| Lutfi et al. (2018) | Core-based statistical areas (CBSAs) (Census tract) | Dissimilarity index (evenness) Isolation index (exposure) Relative concentration index (concentration) Absolute centralization index (centralization) Spatial Proximity (clustering) | Blacks vs. Whites | STI diagnosis | 1. High segregation was associated with the odds of STI diagnosis. 2. The associations were the strongest when segregation was measured by dissimilarity and relative concentration indices. 3. The associations were stronger among males than females, but there was no age group pattern. |
| Mayne et al. (2018) | Chicago Metropolitan area (Census tract) | Local Getis-Ord Gi* statistic | Blacks vs. Others | Hypertensive disorder of pregnancy (HDP) | 1. Segregation was positively associated with odds of having HDP only among black women living in higher poverty neighborhoods. |
| Salow et al. (2018) | Chicago Metropolitan area (Census tract) | Local Getis-Ord Gi* statistic | Blacks vs. Others | Adverse pregnancy outcomes | 1. Overall and spontaneous preterm births are more prevalent in high segregation areas than low segregation areas. |
| Williams et al. (2018) | Hospital Reference Regions (Zip Code Tabulation Area: ZCTA) | Dissimilarity index (evenness) Isolation index (exposure) | Blacks vs. Whites | Stillbirth | 1. Low segregation was associated with decreased odds of stillbirth among blacks than among whites. 2. Decreasing segregation was associated with a reduction in odds of stillbirth among blacks, but not whites. |
| Yu et al. (2018) | County (Census tract) | Dissimilarity index (evenness) Isolation index (exposure) Concentration index (concentration) | Dissimilarity: Blacks vs. Whites Hispanics vs. Whites Asians vs. Whites Isolation: Whites vs. others Blacks vs. others Hispanics vs. others Asians vs. others | Obesity | 1. Blacks and Hispanics residing in segregated areas were more likely to be obese. These relationships were not found among Whites and Asians. |
| Bravo et al. (2019) | Census block (Neighborhood definition not specified) | Local, spatial index of racial isolation (exposure) | Blacks vs. Others | Type 2 diabetes mellitus | 1. Higher isolation of black residents was associated with increased risk of diabetes for whites and blacks. |
| Noah et al. (2019) | Census tract (blockgroup) | Isolation index (exposure) Delta index (concentration) | Blacks vs. Whites | Sexually transmitted diseases (STDs) during pregnancy | 1. Living in segregated neighborhood was associated with mother’s STDs during pregnancy. 2. White mothers living in segregated area were likely to have higher odds of acquiring STDs during pregnancy than black mothers. 3. Black mothers residing in segregated area were less likely to have acquired STDs during pregnancy than white mothers, if they live with co-ethnics. |
| Tempalski et al. (2019) | Metropolitan area (Census tract) | Isolation index (exposure) | Blacks vs. Others Latinos vs. Others | HIV testing | 1. For both blacks and Latinos, higher isolation was not associated with the odds of an individual getting tested for HIV. |
| Thomas-Hawkins et al. (2019) | County (Census tract) | Dissimilarity index (evenness) | Blacks vs. Whites | Emergency departments (ED) revisit | 1. Living in high segregation areas increased the odds of revisiting emergency departments (ED). 2. Blacks living in high segregation are more likely to revisit ED, compared to their white counterparts. |
The author called it index of racial segregation; Kramer and Hogue (2009) categorized it as isolation index.
Neighborhood Clusters (NC) are defined as the sampling unit for the Project on Human Development in Chicago Neighborhoods (PHDCN) community survey.
NCs consist of one or more geographically contiguous census tracts. Chicago’s 865 inhabited census tracts were aggregated to form 343 NCs.
Hypersegregation is defined as highly segregation on ≥ 4 of 5 dimensions based on the work by Wilkes and Iceland (2004).
The census tract boundary file was used in the development of Automated Zone Matching zones. AZM operates by recombining census tracts into a smaller set of output zones using an iterative process by which one tract is randomly selected and attribute constraint parameter(s) are evaluated.
Health-related quality of life (HRQOL) was measured by the General Health subscale of the Short Form-36, which consists of five items that assess survivors’ perception of their health in general on 5-point Likert-type scales.
Geographical Units:
The unit of analysis is particularly important for multilevel modeling as individuals are nested within different levels of contexts. Without clarifying the unit of analysis used to assess segregation, it may not be feasible to situate new empirical findings into the extant literature. In addition, the variation in the unit of analysis may explain why segregation matters more when it is measured at the metropolitan or county level than at the census tract or blockgroup level. That is, the impact of segregation on health may vary by unit of analysis. Massey and Denton (1988) did not, as such, suggest which unit of analysis is most appropriate and our discussion below reports on how scholars have chosen the unit of analysis.
In our review, census-based areal units are widely adopted to measure racial/ethnic segregation due to readily available data. Specifically, the concept of neighborhood has been operationalized as the census tract in 52 studies (79%). Using census tracts as the subunits, 47 out of the 52 studies measured racial/ethnic segregation at either county or metropolitan statistical area (MSA) level and investigated the effect of racial/ethnic segregation on health. Six studies (Debbink & Bader, 2011; Grady, 2006; Grady & McLafferty, 2007; Grady & Ramírez, 2008; Mayne, Yellayi, Pool, Grobman, & Kershaw, 2018; Salow, Pool, Grobman, & Kershaw, 2018) did not aggregate tracts into a higher areal level to create a measure of segregation because they focused on just a single MSA and did not compare the relationship between racial/ethnic segregation and health across metropolitan areas. To overcome this problem, these studies employed a local approach to assessing racial/ethnic segregation at the tract level (Krivo, Bryon, Calder, & Kwan, 2007; Wong, 2002) and their analyses embedded individuals within their neighborhoods (i.e., tracts) rather than a larger geographic area (e.g., MSAs or counties). Two studies used either blocks or blockgroups to calculate segregation at the census tract level (Noah, Yang, & Wang, 2018; Yang, Zhao, & Song, 2017) and Williams and colleagues (2018) used ZIP code data to assess segregation for hospital reference regions. Beyond the conventional census-based areal units, two studies in Chicago (Lee, 2009; Lee & Ferraro, 2007) created “neighborhood clusters” by combining contiguous census tracts together in order to better reflect an individual’s living environment and maximize the homogeneity across tracts within a neighborhood cluster. In order to gauge the extent to which race/ethnicity groups are segregated in a neighborhood cluster, census blocks were used as the subunits that demonstrate the spatial distribution of the majority and minority group members within a neighborhood cluster (i.e., the main unit of interest). Similarly, Grady (2010) applied the automated zone-matching (AZM) methodology to the census tracts in the Detroit MSA and the AZM combines census tracts into zones, which serves as the definition of neighborhood. The main purpose of creating these zones is to maximize the homogeneity within a zone and the heterogeneity across zones. Only two studies measured segregation at the ZIP code level (Mobley et al., 2006; Plascak, Molina, Wu-Georges, Idris, & Thompson, 2016).
Segregation Measures:
The concept of “segregation” has been mixed with “diversity” or “composition” in prior research. To fully understand how an individual’s life chance can be affected by the spatial arrangement of racial/ethnic groups within an area, it is imperative to clarify the dimensions or measures of segregation. Furthermore, there has been an interest in developing new measures of residential segregation (Reardon & O’Sullivan, 2004; Wong, 2002), but little is known about how these new measures have been used in the literature. Our attention to this topic fills this gap.
Though segregation has been conceptualized with five dimensions (Massey & Denton, 1988), the published literature has heavily relied on the exposure dimension. Forty-nine of the 66 studies (74%) employed an indicator that captures the exposure dimension, such as the isolation/interaction index. The second most common dimension of racial/ethnic segregation is the evenness dimension, which was included in 24 studies. The clustering dimension appeared in 7 studies (Bell, Zimmerman, Almgren, Mayer, & Huebner, 2006; Biello, Ickovics, Niccolai, Lin, & Kershaw, 2013; Grady, 2010; Lutfi, Trepka, Fennie, Ibañez, & Gladwin, 2018; Lutfi, Trepka, Fennie, Ibanez, & Gladwin, 2015; Walton, 2009; Yang et al., 2017), and both the concentration and centralization dimensions were included in four studies (Biello, Ickovics, et al., 2013; Lutfi et al., 2018; Lutfi et al., 2015; Yang et al., 2017). Six studies used the work by Massey and Denton (1988) to define hypersegregated MSAs as those areas with at least four dimensions that suggested high black/white segregation (Biello, Ickovics, et al., 2013; Biello, Niccolai, Kershaw, Lin, & Ickovics, 2013; Grigsby-Toussaint, Jones, Kubo, & Bradford, 2015; Jones, 2013; Lutfi et al., 2015; Osypuk & Acevedo-Garcia, 2008). While the segregation measures that take spatial relationships among areal units into account have been used to explore their relationships with health (Bravo, Anthopolos, Kimbro, & Miranda, 2018; Debbink & Bader, 2011; Grady, 2006; Grady, 2010; Grady & McLafferty, 2007; Grady & Ramírez, 2008; Kramer, Cooper, Drews-Botsch, Waller, & Hogue, 2010; Mayne et al., 2018; Salow et al., 2018), most of the segregation indicators in the selected studies presume that the subunits within the main unit of interest are spatially independent.
Comparison Groups:
despite the fact that several segregation indicators have been extended to more than two race/ethnicity groups (Reardon & Firebaugh, 2002), only one out of the 66 studies used a multi-group segregation measure (Bellatorre, Finch, Phuong, Bird, & Beck, 2011). Two studies did not discuss the race/ethnicity groups (Mobley et al., 2006; Russell et al., 2012). Among the 63 studies that explained the racial/ethnic groups for two-group segregation measures, 48 studies dealt with the level of segregation for blacks and 29 studies on the extent to which Hispanics were segregated from others (or whites). Among the 29 studies, 24 were published after 2013, indicating that more attention has been paid to the largest minority group in the US. Only seven studies explicitly assessed segregation between Asians and whites (Mobley, Kuo, Scott, Rutherford, & Bose, 2017; Mobley, Scott, Rutherford, & Kuo, 2017; Mobley, Subramanian, et al., 2017; Walton, 2009; Yang, Shoff, Noah, Black, & Sparks, 2014; Yi, Ruff, Jung, & Waddell, 2014; Yu, Woo, Hawkins, & Iman, 2018).
Health Outcomes:
Regarding the health outcomes studied in our review, the literature mainly focused on maternal and infant health and obesity-related outcomes. Specifically, approximately 27 percent of the studies were concerned with maternal or infant health outcomes, such as birth weight (Bell et al., 2006; Debbink & Bader, 2011; Grady, 2006; Grady, 2010; Grady & McLafferty, 2007; Grady & Ramírez, 2008; Osypuk, Bates, & Acevedo-Garcia, 2010; Walton, 2009), preterm birth (Bell et al., 2006; Britton & Shin, 2013; Britton & Velez, 2015; Kramer et al., 2010; Mendez, Hogan, & Culhane, 2013; Osypuk & Acevedo-Garcia, 2008; Salow et al., 2018), hypertensive disorder of pregnancy (Mayne et al., 2018), stillbirth (Williams et al., 2018), and maternal smoking (Yang et al., 2014). Another 20 percent of our reviewed articles investigated the relationships between segregation and obesity-related outcomes, such as body mass index (Bower et al., 2015; Chang, 2006; Corral, Landrine, & Zhao, 2014; Goodman, Lyons, Dean, Arroyo, & Hipp, 2018; Kershaw & Albrecht, 2014; Kershaw, Albrecht, & Carnethon, 2013; Mobley et al., 2006; Piontak & Schulman, 2016; Yu et al., 2018), physical activity (Corral et al., 2012; Lopez, 2005; Mellerson et al., 2010), and type II diabetes (Bravo et al., 2018). Most of the other health outcomes studied in our reviews were physical health measures, including self-rated health (Anderson & Fullerton, 2014; Nelson, 2013; Plascak et al., 2016; Robert & Ruel, 2006; Subramanian, Acevedo-Garcia, & Osypuk, 2005; Yang et al., 2017), cancer diagnosis and mortality (Greer, Kramer, Cook-Smith, & Casper, 2014; Haas, Earle, Orav, Brawarsky, Keohane, et al., 2008; Haas, Earle, Orav, Brawarsky, Neville, et al., 2008; Harvey, Enos, Chen, Galadima, & Eschbach, 2017; Mobley, Kuo, et al., 2017; Mobley, Scott, et al., 2017; Mobley, Subramanian, et al., 2017; Plascak, Llanos, Pennell, Weier, & Paskett, 2014; Russell et al., 2012), cardiovascular diseases and hypertension (Jones, 2013; Kershaw et al., 2011; Mobley et al., 2006), sexual behaviors (Biello, Ickovics, et al., 2013; Biello, Niccolai, et al., 2013; Lutfi et al., 2018; Lutfi et al., 2015; Noah et al., 2018), and physical disability (Lee & Ferraro, 2007).
Only two studies explored whether racial/ethnic segregation is a determinant of mental health (i.e., depressive symptoms and anxiety) (Lee, 2009; Nobles et al., 2017). Bellatorre and colleagues (2011) are among the first to empirically link segregation to allostatic load and Hao et al (2011) extended segregation to cancer survivors’ health-related quality of life, though Massey (2004) already proposed a theoretical connection between segregation and allostatic load. It should be noted that since 2017, several scholars have reported that segregation is related to the availability of health care resources (Caldwell, Ford, Wallace, Wang, & Takahashi, 2017), health behaviors (Tempalski et al., 2019; Thomas-Hawkins, Flynn, Zha, & Savage, 2019), and neurological disorder (Pennap, Burcu, Safer, & Zito, 2017).
Key Findings:
The majority of studies we examined (56 out of 66) reported that segregation adversely relates to health outcomes and/or widens racial/ethnic health disparities, particularly between blacks and whites. Five studies found that segregation improves health outcomes among blacks or narrows racial/ethnic health disparities (Bell et al., 2006; Corral et al., 2012; Grady, 2010; Haas, Earle, Orav, Brawarsky, Neville, et al., 2008; Mobley et al., 2006).1 Among Hispanics, the protective effect of segregation has been found on coronary heart disease risk (Mobley et al., 2006), physical disability (Lee & Ferraro, 2007), the disparities in early diagnosis of breast cancer (Haas, Earle, Orav, Brawarsky, Neville, et al., 2008; Mobley, Subramanian, et al., 2017), obesity (Kershaw et al., 2013), self-rated health (Nelson, 2013; Yang et al., 2017), mental distress (Nobles et al., 2017), and maternal smoking (Yang et al., 2014). Four of the seven studies that explicitly measured white/Asians segregation found that Asians benefited from high segregation in terms of low risk of having a low birth weight baby and smoking during pregnancy (Walton, 2009; Yang et al., 2014), low odds of late-stage breast cancer diagnosis (Mobley, Kuo, et al., 2017) and early-stage breast cancer surgery (Ojinnaka, Luo, Ory, McMaughan, & Bolin, 2017), and low sodium-potassium ratio (Yi et al., 2014). Thirteen studies did not find a significant relationship between racial/ethnic segregation and health disparities (Anderson & Fullerton, 2014; Biello, Niccolai, et al., 2013; Britton & Velez, 2015; Grigsby-Toussaint et al., 2015; Haas, Earle, Orav, Brawarsky, Keohane, et al., 2008; Harvey et al., 2017; Kershaw & Albrecht, 2014; Kershaw et al., 2013; Kovalchik, Slaughter, Miles, Friedman, & Shih, 2015; Mendez et al., 2013; Piontak & Schulman, 2016; Plascak et al., 2014; Tempalski et al., 2019).
Discussion and Future Research Needs
Based on the review results above, we propose six areas that merit attention in future research on racial/ethnic segregation and health disparities.
1. Clarifying the dimensions of the measures of racial/ethnic segregation:
Reviewing the article selection process, almost 55 percent of the studies that used the term “segregation” did not measure racial/ethnic segregation based on the standard definition proposed by Massey and Denton (1988). It is important to distinguish racial/ethnic diversity from racial/ethnic segregation as these two concepts are fundamentally different. High diversity may not be translated into low segregation as the spatial distribution of minority group members within the larger area of interest (e.g., MSA) is not taken into account. That is, racial/ethnic segregation attends to how two or more racial/ethnic groups distribute within an area, whereas racial/ethnic diversity (or composition) only cares about the total number of members of each racial/ethnic group. As Massey and Denton (1988) clearly pointed out, different dimensions of segregation reflect different spatial patterns of living arrangements among racial/ethnic groups. The distinction between these two concepts should be further emphasized in future research.
Moreover, the literature did not clearly provide explanations for why different dimensions of segregation may have different implications for health disparities. We suggested that there are several factors that could answer this question. First, the determinants of each segregation dimension are different and the common factors, such as income inequality and native-born population, are found to better explain evenness and exposure than other dimensions (Wilkes & Iceland, 2004). The divergent processes that form various dimensions of segregation may affect the distribution of resources within an area and in turn lead to disparate opportunities or life chances (e.g., availability of high-quality schools and accessibility to green space) for local populations.
Second, each segregation dimension is proposed to capture a unique pattern of segregation and different patterns may offer different insight into health research. For example, the exposure dimension of segregation aims to estimate the probability of interaction between groups, which could be used to examine the risk exposure theory (LaVeist, 2005). Should one racial/ethnic group exhibit poor health behaviors or outcomes, high exposure to this racial/ethnic group may undermine an individual’s health behaviors or outcomes (or at least limit the exposure to healthier racial/ethnic groups), which ultimately widens racial/ethnic health disparities in these health outcomes. This relationship could be used to understand the prevalence of transmissible diseases among minorities. By contrast, centralization assesses the degree to which a minority group is located at the center of an area (typically a large MSA) and this measure may capture any unequal access to public services and opportunities between racial/ethnic groups.
Third, it has been reported that some segregation dimensions (e.g., evenness and exposure) have non-linear relationships with health outcomes but others do not (Biello, Ickovics, et al., 2013; Plascak et al., 2016). That is, racial/ethnic health disparities may be widened with the increase in some dimensions of segregation but this pattern may be reversed once segregation reaches a certain level, which is often denoted as a U-shape (or inverse U, depending on the outcomes) relationship between segregation and health. The non-linear relationship suggests that segregation may be both beneficial and detrimental to health, and the level and dimension of segregation may determine its impact on health. To address health disparities, it becomes crucial to have a thorough understanding of how each dimension affects health.
Only four studies in our review investigated the differences in the relationships between dimensions of segregation and health (Biello, Ickovics, et al., 2013; Lutfi et al., 2018; Lutfi et al., 2015; Yang et al., 2017). At least two reasons can explain the scarcity of research in this area. One is the lack of a standardized scale that can be applied to different segregation measures. Some indicators may range between 0 and 1 (e.g., dissimilarity index), whereas others span from −1 to 1 (e.g., absolute centralization index) or can take any real value (e.g., spatial proximity index). This variation makes it hard to interpret and compare findings across dimensions of segregation. A related issue is that it takes data from different geographical levels to calculate segregation indices, which may be a barrier in this research area. In addition, while it is known that each dimension of segregation captures a unique spatial distribution pattern (Massey & Denton, 1988), it remains unclear how the patterns affect the distribution of important factors across space, such as medical resources, social cohesion, and social ties. Prior research may treat each dimension of segregation in the same way and overlook the potential differences across dimensions of segregation. Efforts are warranted to examine whether the effects of racial/ethnic segregation on health vary by the dimensions or types of health outcomes.2
2. Clarifying the spatial scales when measuring segregation:
In our review, while 52 (out of 66) articles operationalized neighborhoods with census tracts, only 6 studies assessed the degree of segregation at the neighborhood (i.e., tract) level and others measured segregation at either county or MSA level. That said, the majority of the significant relationships between segregation and health are in fact MSA effects, rather than the so-called “neighborhood effects” (Diez Roux, 2001). Similar to the aforementioned difference between racial/ethnic diversity and racial/ethnic segregation, if one’s interest is in how two or more racial/ethnic groups are spatially segregated within a “neighborhood,” one should either use the subunits within a neighborhood to gauge segregation or employ a local perspective to obtain segregation measures at the neighborhood level (Wong, 2002).
There are some advantages of using the local segregation measures. For one, local segregation measures can be applied to the subunits within a main area. It could avoid the potential small area estimation problem (i.e., some subunits having few minorities) faced by other conventional/global segregation measures. Second, local segregation measures take into account the spatial relationships among subunits, which better reflects the spatial distribution of racial/ethnic groups in the large context. Third, local segregation measures can be assessed with various spatial weight matrices, which goes beyond the subunits’ boundaries and allows researchers to create a meso-level context between the main and subunit (Wong, 2002). Despite these advantages, only eight articles in our review used local measures of segregations. Future research should compare the findings drawn from the conventional measures with those based on the local segregation measures.3
The spatial misalignment between the measures of “segregation” and the so-called “neighborhood effect” perhaps indicates uncritical adoption of how segregation is conceptualized and operationalized among health researchers. Future research should clearly define and justify the main spatial scale of interest (e.g., tract) that will be included in the hierarchical research framework. Doing so will help researchers identify the subunit (e.g., block) that will be used to calculate conventional segregation measures or to obtain the spatial structures or relationships among the main geographic units that can be applied to other local segregation measures (Reardon et al., 2008). Different spatial scales may imply different pathways from segregation to individual health within a hierarchical framework. For example, should segregation be measured at the MSA level and found to be important, the answers to why segregation matters would be concentrated on the differences across MSAs. If the spatial scale is changed to the census tract, then the mechanisms through which racial/ethnic segregation affects health disparities could be the disparate exposure to the characteristics of residential tract and issues related to environmental injustice (Brulle & Pellow, 2006).
Another important issue related to spatial scales is that the readily available data for calculating segregation may not be precise enough. Specifically, many scholars have argued that the American Community Surveys, a commonly used data source maintained by the US Census Bureau, are subject to large margins of errors (MOE) (Wei, Tong, & Phillips, 2017; Wong & Sun, 2013) and this data limitation may influence the measurement of segregation indicators. While the MOE issue has been acknowledged in the literature, little research on segregation and health takes it into account till a recent study (Arcaya et al., 2016). Future studies should at least recognize different levels of reliability related by MOE (Sun & Wong, 2010) and determine if MOEs change the estimates of segregation and their relationship with health.
It should also be emphasized that the destinations for Asian and Hispanic immigrants have changed from traditional gateway areas (e.g., New York City) to the so-called “new destinations”, which includes small metropolitan areas, suburban places, and rural towns (Hall, 2013; Lichter, Parisi, Taquino, & Grice, 2010). The shift has led to the question of how to properly measure segregation in areas with relatively small number of minority groups. Previous studies usually limit their research areas to those with at least 1,000 (or 500) minorities (at the smallest geographical resolution), but this approach could be problematic particularly for rural areas where the racial/ethnic compositions are homogeneous and the commonly used segregation indicators cannot be calculated correctly. While the approach to measuring local spatial segregation (Grady & Darden, 2012) is an alternative, more effort is warranted to tackle this methodological issue.
3. Applying different theoretical frameworks to black and non-black minorities:
Our literature review indicates that most prior research reported an adverse relationship between black/white segregation and black/white health disparities; however, there is also evidence suggesting that Hispanic/white or Asians/white segregation may be beneficial to Hispanics or Asians. This finding, to some extent, challenges the conventional belief that racial/ethnic segregation is bad for health (Kramer & Hogue, 2009). Drawing from the segregation literature, we proposed two theoretical frameworks that may help to understand the difference between blacks and non-black minorities.
Blacks:
The conventional wisdom that racial/ethnic segregation is negatively associated with health is arguably rooted in the ethnic stratification perspective (Logan, 1978). Since racial/ethnic segregation in the US can be understood as a structural manifestation of racial discrimination against minority groups, particularly blacks (Collins & Williams, 1999; Massey & Denton, 1993), the consequences of racial/ethnic segregation could hence be reflected in the social and built environment of a neighborhood as follows. First, areas with high levels of racial/ethnic segregation (particularly black/white) have been found to be marked by high crime and poverty rates (Collins & Williams, 1999; Williams & Collins, 2001) and these areas are more likely to be neglected and lack the investment in infrastructure or public services than their integrated counterparts (Greenberg & Schneider, 1994; LeClere, Rogers, & Peters, 1997). Second, racial/ethnic segregation is associated with political alienation and powerlessness and these factors can lead to relatively few resources being channeled into such an area. Hence, the residents living in a racially segregated area may have little access to educational and employment opportunities (Dickerson, 2007; Howell-Moroney, 2005). Third, racially segregated areas tend to have an unhealthy built environment, such as high densities of liquor stores (Kwate, 2008). As Logan suggested (1978), ethnic stratification is a means of maintaining advantages for the dominant racial/ethnic group and thus racial/ethnic segregation, from this perspective, could effectively minimize the mobility of resources for promoting health. These poor environmental factors in a racially segregated area expose residents to multiple health risks, which leads to the conclusion that residential segregation is adversely related to health (Brulle & Pellow, 2006).
The ethnic stratification perspective explains the contemporary patterns of racial/ethnic segregation in the US, especially between whites and blacks. A report (Glaeser & Vigdor, 2012) investigated the changing racial/ethnic segregation trend in the US between 1890 and 2010 and attributed the ongoing decrease in racial/ethnic segregation since 1970 to the Civil Rights Revolution and subsequent changes in the political environment. In the era of legal discrimination (1910–1960), blacks encountered numerous barriers to living arrangements such as discrimination by landlords, realtors, and housing authorities. The legal and social restrictions on housing subsided with the continuous fight for African Americans’ freedom (Glaeser & Vigdor, 2012). While there are other potential explanations for the decrease in segregation, the effectiveness of Civil Rights Act may be the most important factor (Glaeser & Vigdor, 2001; Rothstein, 2017). The ethnic stratification perspective should essentially be applied to the historic black/white segregation and explain the findings that racial/ethnic segregation is a barrier to health in our review.
Asians and Hispanics:
In the past three decades, the minority composition in the US has been changed dramatically by immigration from Latin American and Asian (Hobbs & Stoops, 2002) and the segregation patterns for Hispanics and Asians have transformed. Their segregation processes from non-Hispanic white are different from blacks’ experience. The spatial assimilation perspective suggests that racial/ethnic segregation tends to be favored when Hispanics and Asians enter the US. Due to their limited social connections and resources, new arrivals may opt to live in an ethnically bound neighborhood which helps them to improve their social and economic situations and then assimilate into mainstream society (Massey, 1985). Two types of neighborhood (broadly construed) can be derived from this perspective: ethnic enclave and ethnic community (Logan, Zhang, & Alba, 2002). The former suggests that racial/ethnic segregation should be transitional and temporary, whereas the latter indicates that racial/ethnic segregation is a result of personal intention. While the distinction between these two neighborhood structures is grounded in the motives, the pivotal function to help minorities to thrive or accumulate social and financial capital is shared by both types of neighborhood. In contrast to Hispanics and Asians, blacks have experienced a longer history of forced segregation and the structural discrimination against blacks is more deeply rooted in the society. Even with the same increase in income, blacks are less likely to be integrated into white communities than Hispanics and Asians (Intrator, Tannen, & Massey, 2016). In light of the fact that the spatial distributions of Hispanics and Asians differ greatly, we noted that the larger context (e.g., state level) may play a role in understanding the relationship between segregation and racial/ethnic health disparities (Lee, Martin, Matthews, & Farrell, 2017).
The ethnic enclave/community perspective derived from the spatial assimilation model helps us to understand the protective effect of racial/ethnic segregation on health outcomes among Hispanics and Asians. First, for Hispanics and Asians, living in an ethnic enclave/community can be translated into increased social support, frequent social engagement with people of the same race/ethnicity, and a lesser impact presented by language barrier (LeClere et al., 1997). These factors foster strong social cohesion or solidarity in a neighborhood that helps non-black minorities to accommodate to the US society. Second, parallel to the previous point, an ethnic enclave/community may provide great social, economic, and structural resources generated by the close-knit social connections or among residents of the same race/ethnicity (Eschbach, Ostir, Patel, Markides, & Goodwin, 2004; Lee & Ferraro, 2007). That is, for Hispanics and Asians, living in an area segregated from whites limits the exposure to acculturation and access to educational, informational, and occupational opportunities in an ethnic enclave/community may be better than those found in a racially integrated area.
Third, being segregated from the dominant racial/ethnic group indicates a low level of exposure to direct racial discrimination, and in such a neighborhood, the norm that racial discrimination is intolerable would prevail thanks to a strong ethnic identity (Bécares, Nazroo, & Stafford, 2009; Whitley, Prince, McKenzie, & Stewart, 2006). In fact, this perspective counterbalances the argument that segregation is a consequence of racial discrimination (Williams & Collins, 2001) and indicates that segregation for non-black minorities is to avoid discrimination. The aforementioned benefits of living in Hispanic or Asian enclaves/communities suggest several underlying mechanisms between racial/ethnic segregation and health that are comparable to the pathways between social capital and health (Kawachi & Berkman, 2000; Yang, Jensen, & Haran, 2011). Ethnic enclaves/communities can draw both tangible and invisible resources from social support or social relationships, directly facilitating an individual’s health. In addition, being segregated from whites and free of racial discrimination may be regarded as a source of self-esteem and mutual respect among residents, subsequently promoting the health of Hispanics and Asians.
We would like to emphasize that the theoretical frameworks above may depend on the larger geographic or administrative unit. For example, the unequal distribution of Hispanic population in the US may change the state-level immigration policies, which has been found to have implications for mental health and morbidity among Latinos (Hatzenbuehler et al., 2017).
4. Exploring the relationship between mental health and racial/ethnic segregation:
Only two studies in our review investigated the relationship between racial/ethnic segregation and individual mental health outcomes (Lee, 2009; Nobles et al., 2017) and no previous study has explored whether drug/substance abuse or dependence and use of mental health care services are related to segregation. More efforts should be made to advance our understanding of whether racial/ethnic segregation is a determinant of racial/ethnic disparities in these health behavior and mental health measures. This suggestion is particularly important given the findings about racial/ethnic disparities in mental disorders and mental health care. Minorities, in general, demonstrated equal or better mental health than whites; however, they were less likely to receive mental health care services (McGuire & Miranda, 2008). This research need is directly related to the aforementioned frameworks. Specifically, following the theoretical frameworks, living in a segregated neighborhood could be beneficial to the mental health of Asians and Hispanics because of lesser exposure to discrimination and acculturation. Among blacks, being segregated from the majority could be translated into social and physical neighborhood environmental stress due to social inequality and structural conditions (Schulz et al., 2008), which may eventually lead to mental health issues. In addition, high segregation may suggest the strong influence of co-ethics on an individual’s health outcomes or behaviors. Should a minority group exhibit poor health behaviors, segregation may contribute to racial/ethnic health disparities. For example, the prevalence of illicit drug use is higher among blacks than whites (NCHS, 2013); living in an area with high black/white segregation may indicate high exposure to individuals who use illicit drugs, increasing the risk of illicit drug use for the residents living in this area. By contrast, when the majority exhibit poor health behaviors, such as tobacco use (NCHS, 2013), segregation from the majority may be protective for minority group members (Yang et al., 2014).
Furthermore, while the literature provides strong evidence for the adverse impact of racial/ethnic segregation on physical health (particularly for blacks), little is known about whether the relationship between racial/ethnic segregation and physical health is mediated by mental health. Previous studies on segregation and health did not attempt to untangle the intertwined relationships among physical health, mental health, and health behaviors. A plausible mechanism through which racial/ethnic segregation gets under the skin is to affect an individual’s mental health (e.g., stress) and then change behaviors (e.g., smoking and use of preventive health care). Exploring the roles of mental health outcomes or health behaviors will help health researchers to explore the pathways from segregation to individual physical health outcomes, providing important implications for possible interventions that could minimize racial/ethnic health disparities.
5. Investigating the longitudinal effect of racial/ethnic segregation on health:
No study in our review examined the effect of racial/ethnic segregation on health longitudinally. Although Biello and colleagues (2013) used a panel dataset, only the baseline place of residence was taken into account when hypersegregation was calculated. That said, several important questions remained unanswered in the literature, such as whether the effect of segregation on health can be cumulative and whether, from the life course perspective, the segregation experience at a certain life stage (e.g., childhood) is more important than that at a different stage (e.g., adulthood). The temporal nature of the effect of segregation on health is crucial as many health concerns or unhealthy behaviors develop over time and cross-sectional research fails to distinguish a longer stay from a shorter stay in a particular area. This point-in-time approach may misestimate the association between segregation and health. Due to the concern about individual privacy and data confidentiality, an individual’s residential history may not be easily acquired (yet some datasets provide restricted access to such information); however, to advance our understanding of why and how racial/ethnic segregation is a fundamental cause of health disparities (Williams & Collins, 2001), researchers should investigate the temporal dimension of the effect of racial/ethnic segregation on health.
Beyond the long-term effect of segregation on health, it is also important to investigate whether the change in segregation over time within a neighborhood is associated with the health outcomes of the residents. For those who do not move between neighborhoods, if the dynamics of neighborhood segregation is related to their health, researchers may obtain strong evidence to support the idea that segregation matters. Similarly, for those who move between neighborhoods, exploring whether the change in health corresponds to the change in neighborhood segregation will advance out understanding of how racial/ethnic segregation matters.
The discussion above is related to the concept of gentrification, which has received limited attention in the literature (Schnake-Mahl, Jahn, Subramanian, Waters, & Arcaya, 2020). Racial residential segregation is closely related to intentional socioeconomic disinvestment from predominantly non-white neighborhoods (Ellen & Steil, 2019), making these neighborhoods over-representative of low-income communities and hence eligible for gentrification in the long-run. The longitudinal impact of segregation on health may operate through or be modified by gentrification. In addition, gentrification involves in the process of spatially reorganizing disadvantaged/advantaged population (Smith, 2010). The dissolution of racially isolated low-income communities in central cities and the emergence of poverty-riddled neighborhoods in suburbs may alter our understanding of the long-term impact of segregation on health due to the interplay between the past and concurrent segregation. As such, gentrification may be increasingly important in exploring the longitudinal impact of segregation on health.
6. Considering other explanations for the segregation-health relationship:
Several neighborhood factors associated with health outcomes have not been commonly used to explain why racial/ethnic segregation affects health disparities. First, the neighborhood built environment factors that promote health may mediate the association between segregation and obesity-related measures, such as access to open space and walkability. As noted previously, about one-fifth of the studies in our review focused on obesity and physical activity, but none of them considered whether neighborhood built environment accounts for the adverse impact of segregation on obesity.4 To examine whether segregation is the culprit, incorporating this factor into analysis becomes crucial. Our call for attention to the built environment factors in future research is indeed based on the argument that segregation leads to structural inequality in the distribution of social resources and life chances (Logan, 1978; Massey & Denton, 1993). Should this argument stand, taking related factors into account would decrease, if not eliminate, the effect of segregation on obesity.
Second, the concept of social capital should be better measured at the neighborhood level and included in future studies in order to test whether the protective effect of segregation on health among non-black minorities can be attributed to social capital. As a neighborhood is often operationalized with a census tract in the literature, it becomes difficult to examine the research framework that we proposed previously. It should be noted that there is no agreement on how to measure social capital, especially at the ecological level, due to the diverse conceptualizations. However, some scholars have adopted a social network approach at the individual level to operationalize social capital (Song & Lin, 2009). As the social network approach is directly associated with social support and resources embedded in interpersonal relationships, this could be an alternative to the development of neighborhood-level social capital measure. To some extent, the multilevel analytic approach (i.e., embedding people into neighborhoods) seems to provide a potential solution to the measurement issue. If the theoretical framework for understanding the segregation-health relationship among non-black minorities is valid, the inclusion of social capital would further account for the impact of segregation on health.
Third, when a multilevel analytic approach was proposed for segregation and health research (Acevedo-Garcia et al., 2003), the emphasis was placed on how an individual’s health outcomes are associated with neighborhood segregation. The importance of housing quality or conditions has been overlooked. We suggest that housing quality or conditions should be further included into the multilevel perspective because one of the consequences of racial/ethnic segregation is that minorities are more likely to experience poor housing conditions that eventually affect health. The substandard housing conditions would trigger diseases (e.g., asthma) or at least become stressors for occupants. None of the papers included in our review took an individual’s housing conditions into account in order to investigate whether housing conditions would explain the association between segregation and health. As housing is the level between individual and neighborhood, the multilevel analysis framework may need to be expanded in the future.
Limitations and Conclusions
One main limitation of this study is the exclusion of the studies of segregation and health outside the US as the history of racial/ethnic segregation and public health concerns are qualitatively different between the US and other countries, such as South Africa (Coovadia, Jewkes, Barron, Sanders, & McIntyre, 2009). In addition, the studies using an ecological perspective were not considered because this study is built upon the call for a hierarchical analytic perspective in segregation and health research (Acevedo-Garcia et al., 2003). Finally, while various keywords related to “health” or “hierarchical modeling” were used in the selection process, we may still have missed some published articles in our review.
Despite the limitations above, this study contributes to the literature by systematically reviewing the studies published from 2003 to 2019 and based off of our review we offer several suggestions for future research. More specifically, we argue that two major shortcomings are prevalent in the literature. First, the definition of racial/ethnic health disparities is still focused on the differences between blacks and whites; the differences between whites and the two fast growing race/ethnicity groups, Hispanics and Asians, are largely overlooked. Second, urban sociologists have discussed the complexity of segregation and identified five unique dimensions (Massey & Denton, 1988), but few health scholars have taken this complexity into account.
Summary
Six overall recommendations are drawn from the gaps above: First, future research should explore other racial/ethnic segregation dimensions, particularly beyond exposure and evenness. More studies should also compare whether different approaches to measuring neighborhood segregation change the findings. Second, there is a need to clarify the spatial scales for segregation measures. Third, the literature suggests that the effect of segregation on health differs by race/ethnicity groups with blacks suffering from segregation and non-blacks (i.e., Hispanics and Asians) benefitting from segregation. Following this result, we contend that it is imperative to investigate the relationship between segregation and health with different theoretical perspectives. Fourth, the scope of health outcomes should be further expanded to include mental health, substance use, and use of mental health care. Fifth, due to the lack of longitudinal research design, the question of whether segregation carries a long-term effect on health remains unanswered. Finally, other competing explanations for why segregation matters at the neighborhood level should be included into future analysis.
Acknowledgement:
We acknowledge the assistance from the Center for Social and Demographic Analysis at the University at Albany, State University of New York, which receives core funding from NICHD [R24-HD044943].
Footnotes
Conflict of Interest Statement: All authors declare no potential conflict of interest.
There are some possible explanations for the beneficial effects. First, the five studies used either exposure or clustering dimension to assess segregation. In contrast to other dimensions, exposure and clustering may be more closely related to the formation of political power empowerment or institutions (e.g., non-profit organizations), instrumental support, and social ties (Bell et al., 2006), which exert a protective impact on health among blacks. Second, thanks to stronger emotional support and empathy from individuals from similar backgrounds, blacks living with co-ethnics have better health outcomes than those living in predominantly white neighborhoods (Pickett & Wilkinson, 2008). Third, the diffusion of health information or preventive health care services may be faster among blacks in segregated areas as social trust is higher than in communities with low segregation (Haas, Earle, Orav, Brawarsky, Neville, et al., 2008).
Another related issue is that the same dimension of segregation can be measured with different indicators, which may yield divergent findings about how segregation affects health. Though this issue is beyond the scope of this study, we suggest that this is an underexplored area and should receive more attention in the future.
Krieger and colleagues (2017) used the index of concentration at the extremes (ICE) to calculate segregation. However, ICE considers neither the larger context (i.e., main unit) nor neighboring units. As such, we do not include their works in our review.
Goodman et al (2018) included food environment index that assessed how many food retailers selling healthy food. This index does not reflect open space or walkability.
Contributor Information
Tse-Chuan Yang, Department of Sociology, University at Albany, State University of New York, 315 AS, 1400 Washington Avenue, Albany, NY 12222
Kiwoong Park, Department of Sociology & Criminology, University of Arkansas, 211 Old Main, University of Arkansas Fayetteville, AR 72701
Stephen A. Matthews, Department of Sociology & Criminology, Pennsylvania State University, 211 Oswald Tower, University Park, PA 16802
References
- Acevedo-Garcia D, Lochner KA, Osypuk TL, & Subramanian SV (2003). Future directions in residential segregation and health research: a multilevel approach. American Journal of Public Health, 93(2), 215–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson KF, & Fullerton AS (2014). Residential segregation, health, and health care: answering the Latino question. Race and social problems, 6(3), 262–279. [Google Scholar]
- Arcaya MC, Tucker-Seeley RD, Kim R, Schnake-Mahl A, So M, & Subramanian S (2016). Research on neighborhood effects on health in the United States: a systematic review of study characteristics. Social Science & Medicine, 168, 16–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bécares L, Nazroo J, & Stafford M (2009). The buffering effects of ethnic density on experienced racism and health. Health & Place, 15(3), 700–708. [DOI] [PubMed] [Google Scholar]
- Bell JF, Zimmerman FJ, Almgren GR, Mayer JD, & Huebner CE (2006). Birth outcomes among urban African-American women: a multilevel analysis of the role of racial residential segregation. Social Science & Medicine, 63(12), 3030–3045. [DOI] [PubMed] [Google Scholar]
- Bellatorre A, Finch BK, Phuong DD, Bird CE, & Beck AN (2011). Contextual Predictors of Cumulative Biological Risk: Segregation and Allostatic Load. Social Science Quarterly (Wiley-Blackwell), 92(5), 1338–1362. [Google Scholar]
- Biello KB, Ickovics J, Niccolai L, Lin H, & Kershaw T (2013). Racial differences in age at first sexual intercourse: residential racial segregation and the black-white disparity among U.S. adolescents. Public Health Reports (Washington, D.C.: 1974), 128 Suppl 1, 23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biello KB, Niccolai L, Kershaw TS, Lin H, & Ickovics J (2013). Residential racial segregation and racial differences in sexual behaviours: an 11-year longitudinal study of sexual risk of adolescents transitioning to adulthood. Journal Of Epidemiology And Community Health, 67(1), 28–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower KM, Thorpe RJ, Yenokyan G, McGinty EEE, Dubay L, & Gaskin DJ (2015). Racial residential segregation and disparities in obesity among women. Journal of Urban Health, 92(5), 843–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravo MA, Anthopolos R, Kimbro RT, & Miranda ML (2018). Residential racial isolation and spatial patterning of type 2 diabetes mellitus in Durham, North Carolina. American Journal Of Epidemiology, 187(7), 1467–1476. [DOI] [PubMed] [Google Scholar]
- Britton ML, & Shin H (2013). Metropolitan residential segregation and very preterm birth among African American and Mexican-origin women. Social Science & Medicine, 98, 37–45. [DOI] [PubMed] [Google Scholar]
- Britton ML, & Velez W (2015). Boricuas, barrios and birth outcomes: residential segregation and preterm birth among Puerto Ricans in the United States. Centro Journal, 27(1), 70. [Google Scholar]
- Brulle RJ, & Pellow DN (2006). Environmental justice: human health and environmental inequalities. Annu. Rev. Public Health, 27, 103–124. [DOI] [PubMed] [Google Scholar]
- Caldwell JT, Ford CL, Wallace SP, Wang MC, & Takahashi LM (2017). Racial and ethnic residential segregation and access to health care in rural areas. Health & Place, 43, 104–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. (2013). CDC Health Disparities and Inequalities Report-United States, 2013. MMWR, 62(3), 1–187. [PubMed] [Google Scholar]
- Chang VW (2006). Racial residential segregation and weight status among US adults. Social Science & Medicine, 63(5), 1289–1303. [DOI] [PubMed] [Google Scholar]
- Collins CA, & Williams DR (1999). Segregation and mortality: The deadly effects of racism? Paper presented at the Sociological Forum. [Google Scholar]
- Coovadia H, Jewkes R, Barron P, Sanders D, & McIntyre D (2009). The health and health system of South Africa: historical roots of current public health challenges. The Lancet, 374, 817–834. [DOI] [PubMed] [Google Scholar]
- Corral I, Landrine H, Hao Y, Zhao L, Mellerson JL, & Cooper DL (2012). Residential segregation, health behavior and overweight/obesity among a national sample of African American adults. Journal Of Health Psychology, 17(3), 371–378. [DOI] [PubMed] [Google Scholar]
- Corral I, Landrine H, & Zhao L (2014). Residential segregation and obesity among a national sample of Hispanic adults. Journal Of Health Psychology, 19(4), 503–508. [DOI] [PubMed] [Google Scholar]
- Debbink MP, & Bader MDM (2011). Racial Residential Segregation and Low Birth Weight in Michigan’s Metropolitan Areas. American Journal of Public Health, 101(9), 1714–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeFina R, & Hannon L (2009). Diversity, racial threat and metropolitan housing segregation. Social forces, 88(1), 373–394. [Google Scholar]
- DHHS. (2010). Disparities. Retrieved from http://www.healthypeople.gov/2020/about/DisparitiesAbout.aspx
- Dickerson NT (2007). Black employment, segregation, and the social organization of metropolitan labor markets. Economic Geography, 83(3), 283–307. [Google Scholar]
- Diez Roux AV (2001). Investigating neighborhood and area effects on health. American Journal of Public Health, 91(11), 1783–1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellen IG, & Steil J (2019). The Dream Revisited: Contemporary Debates about Housing, Segregation, and Opportunity in the Twenty-first Century: Columbia University Press. [Google Scholar]
- Entwisle B (2007). Putting people into place. Demography, 44(4), 687–703. [DOI] [PubMed] [Google Scholar]
- Eschbach K, Ostir GV, Patel KV, Markides KS, & Goodwin JS (2004). Neighborhood context and mortality among older Mexican Americans: is there a barrio advantage? Journal Information, 94(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaeser E, & Vigdor J (2012). The End of the Segregated Century: Racial Separation in America’s Neighborhoods, 1890–2010: Manhattan Institute for Policy Research. [Google Scholar]
- Glaeser E, & Vigdor JL (2001). Racial segregation in the 2000 census: Promising news: Brookings Institution, Center on Urban and Metropolitan Policy. [Google Scholar]
- Goodman M, Lyons S, Dean LT, Arroyo C, & Hipp JA (2018). How segregation makes us fat: Food behaviors and food environment as mediators of the relationship between residential segregation and individual body mass index. Frontiers in public health, 6, 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grady S, & Darden J (2012). Spatial methods to study local racial residential segregation and infant health in Detroit, Michigan. Annals of the Association of American Geographers, 102(5), 922–931. [Google Scholar]
- Grady SC (2006). Racial disparities in low birthweight and the contribution of residential segregation: A multilevel analysis. Social Science & Medicine, 63(12), 3013–3029. [DOI] [PubMed] [Google Scholar]
- Grady SC (2010). Racial residential segregation impacts on low birth weight using improved neighborhood boundary definitions. Spatial and spatio-temporal epidemiology, 1(4), 239–249. [DOI] [PubMed] [Google Scholar]
- Grady SC, & McLafferty S (2007). Segregation, Nativity, and Health: Reproductive Health Inequalities for Immigrant and Native-Born Black Women in New York City. Urban Geography, 28(4), 377–397. [Google Scholar]
- Grady SC, & Ramírez IJ (2008). Mediating medical risk factors in the residential segregation and low birthweight relationship by race in New York City. Health & Place, 14(4), 661–677. [DOI] [PubMed] [Google Scholar]
- Greenberg M, & Schneider D (1994). Violence in American cities: young black males in the answer, but what was the question? Social Science & Medicine, 39(2), 179–187. [DOI] [PubMed] [Google Scholar]
- Greer S, Kramer MR, Cook-Smith JN, & Casper ML (2014). Metropolitan racial residential segregation and cardiovascular mortality: exploring pathways. Journal of Urban Health, 91(3), 499–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigsby-Toussaint DS, Jones A, Kubo J, & Bradford N (2015). Residential Segregation and Diabetes Risk among Latinos. Ethnicity & Disease, 25(4), 451–458. 10.18865/ed.25.4.451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas JS, Earle CC, Orav JE, Brawarsky P, Keohane M, Neville BA, & Williams DR (2008). Racial segregation and disparities in breast cancer care and mortality. Cancer, 113(8), 2166–2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas JS, Earle CC, Orav JE, Brawarsky P, Neville BA, & Williams DR (2008). Racial segregation and disparities in cancer stage for seniors. Journal of general internal medicine, 23(5), 699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley DF, Matthews SA, Cooper HL, Haardörfer R, Adimora AA, Wingood GM, & Kramer MR (2016). Confidentiality considerations for use of social-spatial data on the social determinants of health: Sexual and reproductive health case study. Social Science & Medicine, 166, 49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall M (2013). Residential integration on the new frontier: Immigrant segregation in established and new destinations. Demography, 50(5), 1873–1896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao Y, Landrine H, Smith T, Kaw C, Corral I, & Stein K (2011). Residential Segregation and Disparities in Health-Related Quality of Life Among Black and White Cancer Survivors. Health Psychology, 30(2), 137–144. [DOI] [PubMed] [Google Scholar]
- Harvey VM, Enos CW, Chen JT, Galadima H, & Eschbach K (2017). The role of neighborhood characteristics in late stage melanoma diagnosis among hispanic men in California, Texas, and Florida, 1996–2012. Journal of cancer epidemiology, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Prins SJ, Flake M, Philbin M, Frazer MS, Hagen D, & Hirsch J (2017). Immigration policies and mental health morbidity among Latinos: A state-level analysis. Social Science & Medicine, 174, 169–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobbs F, & Stoops N (2002). Demographic trends in the 20th century (Vol. 4): US Census Bureau. [Google Scholar]
- Howell-Moroney M (2005). The geography of opportunity and unemployment: an integrated model of residential segregation and spatial mismatch. Journal of urban affairs, 27(4), 353–377. [Google Scholar]
- Iceland J, & Weinberg DH (2002). Racial and ethnic residential segregation in the United States 1980–2000: Bureau of Census. [Google Scholar]
- Intrator J, Tannen J, & Massey DS (2016). Segregation by race and income in the United States 1970–2010. Social science research, 60, 45–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A (2013). Segregation and cardiovascular illness: The role of individual and metropolitan socioeconomic status. Health and Place, 22(Complete), 56–67. [DOI] [PubMed] [Google Scholar]
- Kawachi I, & Berkman L (2000). Social cohesion, social capital, and health. Social epidemiology, 174–190.
- Kershaw KN, & Albrecht SS (2014). Metropolitan-level ethnic residential segregation, racial identity, and body mass index among US Hispanic adults: a multilevel cross-sectional study. BMC public health, 14(1), 283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw KN, Albrecht SS, & Carnethon MR (2013). Racial and ethnic residential segregation, the neighborhood socioeconomic environment, and obesity among Blacks and Mexican Americans. American Journal Of Epidemiology, 177(4), 299–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw KN, V, Burgard SA, Lisabeth LD, Mujahid MS, & Schulz AJ (2011). Metropolitan-Level Racial Residential Segregation and Black-White Disparities in Hypertension. American Journal Of Epidemiology, 174(5), 537–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovalchik SA, Slaughter ME, Miles J, Friedman EM, & Shih RA (2015). Neighbourhood racial/ethnic composition and segregation and trajectories of cognitive decline among US older adults. Journal Of Epidemiology And Community Health, 69(10), 978–984. [DOI] [PubMed] [Google Scholar]
- Kramer MR, Cooper HL, Drews-Botsch CD, Waller LA, & Hogue CR (2010). Metropolitan isolation segregation and Black–White disparities in very preterm birth: A test of mediating pathways and variance explained. Social Science & Medicine, 71(12), 2108–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer MR, & Hogue CR (2009). Is segregation bad for your health? Epidemiologic reviews, 31(1), 178–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Waterman PD, Batra N, Murphy JS, Dooley DP, & Shah SN (2017). Measures of local segregation for monitoring health inequities by local health departments. American Journal of Public Health, 107(6), 903–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krivo L, Bryon R, Calder C, & Kwan M (2007). Patterns of local segregation: Do they matter for crime? Paper presented at the Population Association of America Annual Meeting, New York. [Google Scholar]
- Kwate NOA (2008). Fried chicken and fresh apples: racial segregation as a fundamental cause of fast food density in black neighborhoods. Health & Place, 14(1), 32–44. [DOI] [PubMed] [Google Scholar]
- LaVeist TA (2005). Minority populations and health. In: San Francisco, CA: Jossey-Bass. [Google Scholar]
- LeClere FB, Rogers RG, & Peters KD (1997). Ethnicity and mortality in the United States: individual and community correlates. Social forces, 76(1), 169–198. [Google Scholar]
- Lee B, Martin M, Matthews S, & Farrell C (2017). State-level changes in US racial and ethnic diversity, 1980 to 2015: A universal trend? Demographic Research, 37, 1031–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee BA, Iceland J, & Farrell CR (2014). Is ethnoracial residential integration on the rise? Evidence for metropolitan and micropolitan America since 1980. Diversity and disparities: America enters a new century. New York: Russell Sage Foundation. [Google Scholar]
- Lee M-A (2009). Neighborhood residential segregation and mental health: A multilevel analysis on Hispanic Americans in Chicago. Social Science & Medicine, 68(11), 1975–1984. [DOI] [PubMed] [Google Scholar]
- Lee M-A, & Ferraro KF (2007). Neighborhood residential segregation and physical health among Hispanic Americans: good, bad, or benign? Journal Of Health And Social Behavior, 48(2), 131–148. [DOI] [PubMed] [Google Scholar]
- Levac D, Colquhoun H, & O’Brien KK (2010). Scoping studies: advancing the methodology. Implementation science, 5(1), 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichter DT, Parisi D, Taquino MC, & Grice SM (2010). Residential segregation in new Hispanic destinations: Cities, suburbs, and rural communities compared. Social science research, 39(2), 215–230. [Google Scholar]
- Logan JR (1978). Growth, politics, and the stratification of places. American Journal of Sociology, 404–416. [Google Scholar]
- Logan JR, Zhang W, & Alba RD (2002). Immigrant enclaves and ethnic communities in New York and Los Angeles. American sociological review, 299–322. [Google Scholar]
- Lopez R (2005). Black-white residential segregation and physical activity. Ethnicity & Disease, 16(2), 495–502. [PubMed] [Google Scholar]
- Lutfi K, Trepka MJ, Fennie KP, Ibañez G, & Gladwin H (2018). Racial residential segregation and STI diagnosis among non-Hispanic blacks, 2006–2010. Journal of immigrant and minority health, 20(3), 577–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutfi K, Trepka MJ, Fennie KP, Ibanez G, & Gladwin H (2015). Racial residential segregation and risky sexual behavior among non-Hispanic blacks, 2006–2010. Social Science & Medicine, 140, 95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey D (1985). Ethnic residential segregation: A theoretical synthesis and empirical review. Sociology and Social Research, 69(3), 315–350. [Google Scholar]
- Massey DS (2004). Segregation and stratification: a biosocial perspective. Du Bois Review, 1(01), 7–25. [Google Scholar]
- Massey DS, & Denton NA (1988). The dimensions of residential segregation. Social forces, 67(2), 281–315. [Google Scholar]
- Massey DS, & Denton NA (1993). American apartheid: Segregation and the making of the underclass: Harvard University Press. [Google Scholar]
- Mayne SL, Yellayi D, Pool LR, Grobman WA, & Kershaw KN (2018). Racial Residential Segregation and Hypertensive Disorder of Pregnancy Among Women in Chicago: Analysis of Electronic Health Record Data. American journal of hypertension, 31(11), 1221–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire TG, & Miranda J (2008). New evidence regarding racial and ethnic disparities in mental health: Policy implications. Health Affairs, 27(2), 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellerson J, Landrine H, Hao Y, Corral I, Zhao L, & Cooper DL (2010). Residential segregation and exercise among a national sample of Hispanic adults. Health & Place, 16(3), 613–615. [DOI] [PubMed] [Google Scholar]
- Mendez DD, Hogan VK, & Culhane JF (2013). Institutional racism, neighborhood factors, stress, and preterm birth. Ethnicity & Health. [DOI] [PMC free article] [PubMed]
- Mobley LR, Kuo T-M, Scott L, Rutherford Y, & Bose S (2017). Modeling geospatial patterns of late-stage diagnosis of breast cancer in the US. International journal of environmental research and public health, 14(5), 484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mobley LR, Root ED, Finkelstein EA, Khavjou O, Farris RP, & Will JC (2006). Environment, obesity, and cardiovascular disease risk in low-income women. American journal of preventive medicine, 30(4), 327–332. e321. [DOI] [PubMed] [Google Scholar]
- Mobley LR, Scott L, Rutherford Y, & Kuo T-M (2017). Using residential segregation to predict colorectal cancer stage at diagnosis: Two different approaches. Annals of epidemiology, 27(1), 10–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mobley LR, Subramanian S, Tangka FK, Hoover S, Wang J, Hall IJ, & Singh SD (2017). Breast cancer screening among women with Medicaid, 2006–2008: a multilevel analysis. Journal of racial and ethnic health disparities, 4(3), 446–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCHS. (2013). Health, United States, 2012: With Special Feature on Emergency Care. Hyattsville, MD. [PubMed] [Google Scholar]
- Nelson KA (2013). Does residential segregation help or hurt? Exploring differences in the relationship between segregation and health among US Hispanics by nativity and ethnic subgroup. The Social Science Journal, 50(4), 646–657. [Google Scholar]
- Noah AJ, Yang T-C, & Wang W.-l. (2018). The black-white disparity in sexually transmitted diseases during pregnancy: how do racial segregation and income inequality matter? Sexually transmitted diseases, 45(5), 301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nobles CJ, Valentine SE, Zepeda ED, Wang Y, Ahles EM, Shtasel DL, & Marques L (2017). Residential segregation and mental health among Latinos in a nationally representative survey. J Epidemiol Community Health, 71(4), 318–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojinnaka CO, Luo W, Ory MG, McMaughan D, & Bolin JN (2017). Disparities in surgical treatment of early-stage breast cancer among female residents of Texas: The role of racial residential segregation. Clinical breast cancer, 17(2), e43–e52. [DOI] [PubMed] [Google Scholar]
- Osypuk TL, & Acevedo-Garcia D (2008). Are racial disparities in preterm birth larger in hypersegregated areas? American Journal Of Epidemiology, 167(11), 1295–1304. [DOI] [PubMed] [Google Scholar]
- Osypuk TL, Bates LM, & Acevedo-Garcia D (2010). Another Mexican birthweight paradox? The role of residential enclaves and neighborhood poverty in the birthweight of Mexican-origin infants. Social Science & Medicine, 70(4), 550–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennap D, Burcu M, Safer DJ, & Zito JM (2017). Hispanic residential isolation, ADHD diagnosis and stimulant treatment among Medicaid-insured youth. Ethnicity & Disease, 27(2), 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett KE, & Wilkinson RG (2008). People like us: ethnic group density effects on health. Ethnicity & Health, 13(4), 321–334. [DOI] [PubMed] [Google Scholar]
- Piontak JR, & Schulman MD (2016). School context matters: the impacts of concentrated poverty and racial segregation on childhood obesity. Journal of School Health, 86(12), 864–872. [DOI] [PubMed] [Google Scholar]
- Plascak JJ, Llanos AA, Pennell ML, Weier RC, & Paskett ED (2014). Neighborhood factors associated with time to resolution following an abnormal breast or cervical cancer screening test. Cancer Epidemiology and Prevention Biomarkers, 23(12), 2819–2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plascak JJ, Molina Y, Wu-Georges S, Idris A, & Thompson B (2016). Latino residential segregation and self-rated health among Latinos: Washington State Behavioral Risk Factor Surveillance System, 2012–2014. Social Science & Medicine, 159, 38–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon SF, & Firebaugh G (2002). Measures of multigroup segregation. Sociological methodology, 32(1), 33–67. [Google Scholar]
- Reardon SF, Matthews SA, O’Sullivan D, Lee BA, Firebaugh G, Farrell CR, & Bischoff K (2008). The geographic scale of metropolitan racial segregation. Demography, 45(3), 489–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon SF, & O’Sullivan D (2004). Measures of spatial segregation. Sociological methodology, 34(1), 121–162. [Google Scholar]
- Robert SA, & Ruel E (2006). Racial Segregation and Health Disparities Between Black and White Older Adults. Journals of Gerontology Series B: Psychological Sciences & Social Sciences, 61B(4), S203–S211. [DOI] [PubMed] [Google Scholar]
- Rothstein R (2017). The color of law: A forgotten history of how our government segregated America. New York, New York: Liveright Publishing. [Google Scholar]
- Russell EF, Kramer MR, Cooper HLF, Gabram-Mendola S, Senior-Crosby D, & Jacob Arriola KR (2012). Metropolitan area racial residential segregation, neighborhood racial composition, and breast cancer mortality. Cancer Causes & Control: CCC, 23(9), 1519–1527. [DOI] [PubMed] [Google Scholar]
- Salow AD, Pool LR, Grobman WA, & Kershaw KN (2018). Associations of neighborhood-level racial residential segregation with adverse pregnancy outcomes. American journal of obstetrics and gynecology, 218(3), 351. e351–351. e357. [DOI] [PubMed] [Google Scholar]
- Schnake-Mahl AS, Jahn JL, Subramanian S, Waters MC, & Arcaya M (2020). Gentrification, Neighborhood Change, and Population Health: a Systematic Review. Journal of Urban Health, 97(1), 1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz AJ, Zenk SN, Israel BA, Mentz G, Stokes C, & Galea S (2008). Do neighborhood economic characteristics, racial composition, and residential stability predict perceptions of stress associated with the physical and social environment? Findings from a multilevel analysis in Detroit. Journal of Urban Health, 85(5), 642–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith N (2010). A short history of gentrification. The Gentrification Debates: A Reader, 31–36. [Google Scholar]
- Song L, & Lin N (2009). Social capital and health inequality: evidence from Taiwan. Journal Of Health And Social Behavior, 50(2), 149–163. [DOI] [PubMed] [Google Scholar]
- Subramanian SV, Acevedo-Garcia D, & Osypuk TL (2005). Racial residential segregation and geographic heterogeneity in black/white disparity in poor self-rated health in the US: a multilevel statistical analysis. Social Science & Medicine, 60(8), 1667–1679. [DOI] [PubMed] [Google Scholar]
- Sun M, & Wong DW (2010). Incorporating data quality information in mapping American Community Survey data. Cartography and Geographic Information Science, 37(4), 285–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempalski B, Cooper HL, Kelley ME, Linton SL, Wolfe ME, Chen Y-T, … Williams LD (2019). Identifying which place characteristics are associated with the odds of recent HIV testing in a large sample of people who inject drugs in 19 US metropolitan areas. AIDS and Behavior, 23(2), 318–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas-Hawkins C, Flynn L, Zha P, & Savage B (2019). Associations among race, residential segregation, community income, and emergency department use by adults with end-stage renal disease. Public Health Nursing, 36(5), 645–652. [DOI] [PubMed] [Google Scholar]
- Walton E (2009). Residential segregation and birth weight among racial and ethnic minorities in the United States. Journal Of Health And Social Behavior, 50(4), 427–442. [DOI] [PubMed] [Google Scholar]
- Wei R, Tong D, & Phillips JM (2017). An integrated classification scheme for mapping estimates and errors of estimation from the American Community Survey. Computers, Environment and Urban Systems, 63, 95–103. [Google Scholar]
- White K, & Borrell LN (2011). Racial/ethnic residential segregation: Framing the context of health risk and health disparities. Health & Place, 17(2), 438–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitley R, Prince M, McKenzie K, & Stewart R (2006). Exploring the ethnic density effect: a qualitative study of a London electoral ward. International journal of social psychiatry, 52(4), 376–391. [DOI] [PubMed] [Google Scholar]
- Wilkes R, & Iceland J (2004). Hypersegregation in the twenty-first century. Demography, 41(1), 23–36. [DOI] [PubMed] [Google Scholar]
- Williams AD, Wallace M, Nobles C, & Mendola P (2018). Racial residential segregation and racial disparities in stillbirth in the United States. Health & Place, 51, 208–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Collins C (2001). Racial residential segregation: a fundamental cause of racial disparities in health. Public health reports, 116(5), 404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong DW (2002). Modeling local segregation: a spatial interaction approach. Geographical and Environmental Modelling, 6(1), 81–97. [Google Scholar]
- Wong DW, & Sun M (2013). Handling data quality information of survey data in GIS: A case of using the American Community Survey data. Spatial demography, 1(1), 3–16. [Google Scholar]
- Yang T-C, Shoff C, Noah AJ, Black N, & Sparks CS (2014). Racial segregation and maternal smoking during pregnancy: A multilevel analysis using the racial segregation interaction index. Social Science & Medicine, 107, 26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang T-C, Zhao Y, & Song Q (2017). Residential segregation and racial disparities in self-rated health: How do dimensions of residential segregation matter? Social science research, 61, 29–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang TC, Jensen L, & Haran M (2011). Social Capital and Human Mortality: Explaining the Rural Paradox with County-Level Mortality Data. Rural Sociology, 76(3), 347–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi SS, Ruff RR, Jung M, & Waddell EN (2014). Racial/ethnic residential segregation, neighborhood poverty and urinary biomarkers of diet in New York City adults. Social Science & Medicine, 122, 122–129. [DOI] [PubMed] [Google Scholar]
- Yu C-Y, Woo A, Hawkins C, & Iman S (2018). The Impacts of Residential Segregation on Obesity. Journal of Physical Activity and Health, 15(11), 834–839. [DOI] [PubMed] [Google Scholar]