Abstract
Introduction
The ongoing coronavirus disease 2019 (COVID-19) outbreak impacts the mental health of patients, health workers, and the public. The level of impact on the mental health of orthodontic patients in treatment is unknown. The objective of the study was to evaluate the mental health of orthodontic patients in China during the early stage of the pandemic.
Methods
An online survey was conducted on a convenience sample of anonymous participants. The questionnaire, in Chinese (Mandarin), comprised 5 sections. Sections 1-3 included demographic, epidemical, and orthodontic status of the patients. Section 4 assessed mental health-related to orthodontics. Section 5 was the Kessler-10 Mental Distress Scale. A total of 48 orthodontists were invited to distribute the questionnaires to their patients. Descriptive statistics, principal component analysis, K-means cluster analysis, and bivariate logistics regression analysis were performed with significance set at P <0.05.
Results
Questionnaires were collected from 558 patients (104 males, 354 females; mean age 24.78 ± 6.33 years). The prevalence of mental distress was 38% (174/458). Higher odds ratios were associated with female participants, missed appointments, and Hubei residence. The type of orthodontic appliance was associated with the anxiety of prolonged treatment duration. The manner of communication with patients regarding the postponement of appointments was associated with patients' concerns of prolonged treatment duration. The frequency of contact from dentists was associated with patients' independence.
Conclusions
Over one-third of orthodontic patients experienced mental distress during the pandemic. Multiple factors affected the level of anxiety of orthodontic patients, such as the type of orthodontic appliance, time since last dental visit, manner of communication with the orthodontist, and the localities of the pandemic progression.
Highlights
-
•
Thirty-eight percent of patients had orthodontic-related mental distress during the pandemic.
-
•
Orthodontic patients in the epicenter revealed higher odds of mental distress.
-
•
Orthodontists who contact patients personally might relieve their anxiety.
-
•
Patients with invisible appliances felt less anxiety about the duration of treatment.
-
•
The results could guide orthodontists from other countries with similar situations.
Coronavirus disease 2019 (COVID-19) was first reported in Wuhan, Hubei Province, China, in December 2019. With stunning speed, now it is sweeping across the whole world, causing a global health emergency of international concern. On March 11, 2020, the World Health Organization declared COVID-19 a global pandemic. By May 28, 2020, the disease has been reported in over 210 countries and territories with increasing confirmed patients in Italy, United States, Brazil, Russia, and Spain. With the ongoing outbreak, the mental health of COVID-19 patients, health workers, and the public has become of great concern.1
During the pandemic, all the provinces in China, as well as many cities in other countries such as Italy, have raised highest-level health emergency. Cities were locked down with residents staying at home to avoid disease transmission. Because of the prolonged lockdown, subjects are suffering from a feeling of isolation from society, which could further develop into depression and anxiety.2 Among these subjects, a particular focus should be on dental patients.
In a dental clinic setting, the patients, dentists, and dental assistants are exposed to the aerosol mist of saliva or blood droplets generated from high-speed handpiece or ultrasonic instruments to the surroundings. The delivery of orthodontic treatment involves close contact with patients. It was found that droplet and close contact transmission were the main transmission route for COVID-19.3 It has been previously reported that 9 dental practitioners were infected by the coronavirus in the School and Hospital of Stomatology, Wuhan University.4 Therefore, many dental hospitals and clinics were advised to provide treatment for dental emergencies only with the shutdown of all other dental departments, especially in the Hubei Province, since January 23, 2020. Thus, routine follow-up visits of orthodontic treatment had been interrupted by the pandemic. Furthermore, some patients suffered from orthodontic emergencies, such as loose brackets and protruding wire, but were unable to get timely and effective help from the specialists. After February 25, 2020, some hospitals and clinics were allowed to open with extra-protective measures such as epidemiologic record evaluation, temperature check, and upgraded personal protective measures during the dental treatment.4, 5, 6 All these factors might lead to an increase in the mental stress of the patients.
The objectives of the present study were to evaluate the mental distress of orthodontic patients and to investigate the level of their anxiety on treatment duration and outcome during the early stage of the pandemic.
Material and methods
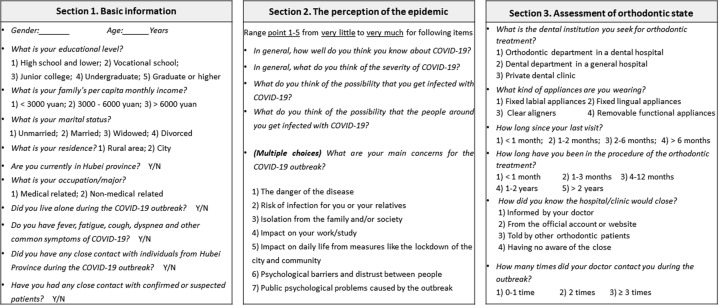
The study protocol was approved by the West China Hospital of Stomatology (Approval no. WCHSIRB-D-2020-218). Because the investigator could reach the participants only by telephone or the Internet, an anonymous online questionnaire consisting of 5 sections (Figs 1 and 2 ) was developed in Mandarin Chinese via www.wjx.cn.
Fig 1.
Sections 1-3 of the questionnaire. Y/N, yes or no.
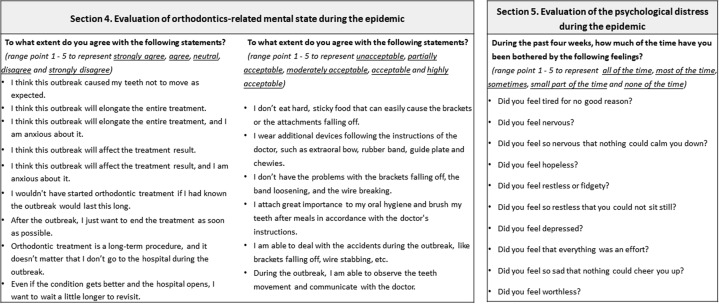
Fig 2.
Sections 4 and 5 of the questionnaire.
A total of 48 orthodontists were invited to distribute the questionnaire to be completed by their patients. The inclusion criteria were as follows: (1) in the process of orthodontic treatment, (2) able to read Mandarin online, (3) had informed consent for the use of the data recorded, and (4) completed all the items in the questionnaire within a reasonable time. The questionnaire was available online from February 20 to February 22, which was during the early stage of the pandemic.
Section 1 assessed demographic and COVID-19-related epidemical information, such as sex, age, education level, residence, family income, marital status, profession and employment status, history of COVID-19–related symptoms, close contact with subjects from Hubei Province, and close contact with confirmed or suspected patients.
Section 2 focused on the perception of the pandemic, which included the knowledge and severity of the pandemic, the risk of infection for themselves and the people around them, and the main concerns about the pandemic.
Section 3 focused on the orthodontic state of the patients, including the type of their dental institutions and orthodontic appliances, the time since their last dental visit, the duration since treatment began, the way they received the suspension notice, and frequency of contacts from their orthodontist.
Section 4 assessed the orthodontic-related mental state. There are 15 items in this section with a 5-point scale ranging in score from 1 to 5 for each item. The 15 items aimed to evaluate the patients' anxiety about treatment duration and outcome, their compliance, patience, and independence. Specifically, compliance is defined as the ability to perform the home instructions such as elastics use, sequential change of aligners, and oral hygiene maintenance. Independence refers to the ability to deal with orthodontic accidents and the initiative to communicate with the dentist. Patience is defined as the willingness to wait for the appointment until the pandemic was under control. Sections 1-4 were developed by a proficient orthodontist (J.W.) who has more than 20 years of experience with the help of 2 junior orthodontists (X.X. and X.F.). All these items were validated preliminarily.
Section 5 focused on the Kessler-10 Psychological Distress Scale, which included 10 items to evaluate the mental distress of patients over the past 4 weeks.7 The 5-point scale for each item ranged from a score of 1 (none of the time) to a score of 5 (all of the time), with a total score range of 10-50. The Chinese version of the scale was shown to have highly acceptable validity and reliability (Cronbach α ranged from 0.80-0.87) in previous studies.8, 9, 10 A total score of 10-19 was considered normal, whereas a score of 20-50 was indicative of mental distress.
After data collection, the internal consistency of items in Sections 4 and 5 was evaluated by calculating Cronbach α coefficients.11 The items in Section 4 were selected for subsequent principal component analysis (PCA).12 Sampling adequacy was tested using the Kaiser-Meyer-Olkin test.13 Then K-means cluster analysis was performed using each principal component (PC) to classify the study samples into 2 categories on the basis of the characteristics of each PC. The mental distress and the classifications of PC, which were binary variables, were considered as dependent variables in bivariate logistic regression analysis to assess the association with their independent variables. The strength of the relationship was interpreted using odds ratios (ORs) with 95% confidence intervals (CIs). The model adequacy in bivariate logistic regression was approved with Hosmer and Lemeshow14 goodness of fit test. All statistical tests were 2-sided and were performed by IBM SPSS Statistics (version 24; IBM Corp, Armonk, NY) with a significance level of 0.05.
Results
A total of 458 valid questionnaires were collected by February 22, 2020. The mean age of the participants was 24.78 years, with a standard deviation of 6.33 years. Descriptive statistics of the sample are reported in Table I, Table II, Table III, Table IV . For categorical data, the frequency and percentage of each category are reported. There were 354 females (77.29%) and 104 males (22.71%). For residence, 22 (5.68%) patients were in Hubei Province, and 432 patients were not (Table I).
Table I.
Basic information of orthodontic patients (n = 458)
| Independent variables | Category | Frequency, n | Percentage, % |
|---|---|---|---|
| Age | ≤24 y | 244 | 53.28 |
| >24 y | 214 | 46.72 | |
| Sex | Male | 104 | 22.71 |
| Female | 354 | 77.29 | |
| Educational level | High school and lower | 68 | 14.85 |
| Vocational school | 28 | 6.11 | |
| Junior college | 72 | 15.72 | |
| Undergraduate | 229 | 50.00 | |
| Graduate or higher | 61 | 13.32 | |
| Monthly income | <3000 yuan | 56 | 12.23 |
| 3000 ≤ income < 6000 yuan | 201 | 43.89 | |
| 6000 yuan or more | 201 | 43.89 | |
| Marital status | Unmarried | 351 | 76.64 |
| Married | 98 | 21.40 | |
| Widowed | 1 | 0.22 | |
| Separated or divorced | 8 | 1.75 | |
| Residence | Rural area | 89 | 19.43 |
| City | 369 | 80.57 | |
| Currently in Hubei Province | Yes | 26 | 5.68 |
| No | 432 | 94.32 | |
| Occupation and/or major | Medical-related | 93 | 20.31 |
| Nonmedical-related | 365 | 79.69 | |
| Live alone | Yes | 79 | 17.25 |
| No | 379 | 82.75 | |
| COVID symptoms | Yes | 4 | 0.87 |
| No | 454 | 99.13 | |
| Close contact with subjects from Hubei Province | Yes | 24 | 5.24 |
| No | 434 | 94.76 | |
| Close contact with confirmed or suspected patients | Yes | 2 | 0.44 |
| No | 456 | 99.56 |
Table II.
Patients' perception of the pandemic (n = 458)
| Independent variables | Category | Frequency, n | Percentage, % |
|---|---|---|---|
| Knowledge | 1 | 2 | 0.44 |
| 2 | 2 | 0.44 | |
| 3 | 55 | 12.01 | |
| 4 | 292 | 63.76 | |
| 5 | 107 | 23.36 | |
| Severity | 1 | 0 | 0.00 |
| 2 | 2 | 0.44 | |
| 3 | 9 | 1.97 | |
| 4 | 143 | 31.22 | |
| 5 | 304 | 66.38 | |
| Infection possibility | 1 | 127 | 27.73 |
| 2 | 137 | 29.91 | |
| 3 | 145 | 31.66 | |
| 4 | 29 | 6.33 | |
| 5 | 20 | 4.37 | |
| Infection possibility of people around | 1 | 105 | 22.93 |
| 2 | 153 | 33.41 | |
| 3 | 153 | 33.41 | |
| 4 | 39 | 8.52 | |
| 5 | 8 | 1.75 |
Note. The “Category” column ranges from 1 being “very little” to 5 being “very much.”
Table III.
Patients' main concerns about COVID-19 (n = 458)
| Independent variables | Category | Frequency, n | Percentage, % |
|---|---|---|---|
| Danger of the disease | Yes | 332 | 72.49 |
| No | 126 | 27.51 | |
| Risk of infection | Yes | 372 | 81.22 |
| No | 86 | 18.78 | |
| Isolation | Yes | 210 | 45.85 |
| No | 248 | 54.15 | |
| Impact on work and/or study | Yes | 289 | 63.10 |
| No | 169 | 36.90 | |
| Impact on daily life | Yes | 245 | 53.49 |
| No | 213 | 46.51 | |
| Psychological barriers and distrust | Yes | 149 | 32.53 |
| No | 309 | 67.47 | |
| Public psychological problems | Yes | 268 | 58.52 |
| No | 190 | 41.48 |
Table IV.
Assessment of patients' orthodontic status (n = 458)
| Independent variables | Category | Frequency, n | Percentage, % |
|---|---|---|---|
| Medical institution | Orthodontic department in dental hospital | 264 | 57.64 |
| Dental department in general hospital | 81 | 17.69 | |
| Private dental clinic | 113 | 24.67 | |
| Type of appliances | Fixed labial appliances | 309 | 67.47 |
| Fixed lingual appliances | 35 | 7.64 | |
| Clear aligners | 94 | 20.52 | |
| Functional appliances | 20 | 4.37 | |
| Duration from the last appointment | Within 1 mo | 44 | 9.61 |
| 1-2 mo | 350 | 76.42 | |
| 2-6 mo | 48 | 10.48 | |
| More than 6 mo | 16 | 3.49 | |
| Duration since the beginning | Within 1 mo | 10 | 2.18 |
| 1-3 mo | 63 | 13.76 | |
| 4-12 mo | 152 | 33.19 | |
| 1-2 y | 147 | 32.10 | |
| More than 2 y | 86 | 18.78 | |
| Way to get the suspension | Informed by doctor | 242 | 52.84 |
| From the official account or Web site | 181 | 39.52 | |
| Told by other patients | 16 | 3.49 | |
| Not aware | 19 | 4.15 | |
| Frequency of contact from dentist | 0-1 time | 283 | 61.79 |
| 2 times | 105 | 22.93 | |
| 3 times and more | 70 | 15.28 |
For the patients' perception of the pandemic, 292 (63.76%) respondents thought they knew much about COVID-19, and 107 (23.36%) thought they knew very much. Three hundred four respondents considered this disease as very severe (Table II). For patients' main concerns about COVID-19, 72.49% (332/458) and 81.22% (372/458) were concerned about the danger of the disease and the risk of infection, respectively, whereas 45.85% (210/458) were concerned about the isolation from the family or society (Table III).
For the patients' orthodontic status, 264 (57.64%) patients were registered in orthodontic departments in dental hospitals. Fixed labial appliances were worn by 309 (67.47%) patients, whereas 94 (20.52%) wore clear aligners, and 35 (7.64%) wore fixed lingual appliances. Only 9.61% (44/458) of the patients had visited the orthodontist within a month. For the suspension notice, 242 (52.84%) patients were informed by the doctor. For the frequency of contact from the dentist, 283 (61.79%) patients had contacted the dentist 0-1 time, whereas 70 (15.28%) patients had contacted the dentist 3 times or more (Table IV).
The Cronbach α value for the 15 items in Section 4 was 0.700. The PCA derived 5 components with 66.26% of cumulative explanation (Tables V and VI ). The Kaiser-Meyer-Olkin value was 0.787. PC1 and PC2 depicted the anxiety about treatment duration and treatment outcome. The compliance, independence, and patience of the patients were described in the PC3, PC4, and PC5, respectively (Table VI). The classifications of K-means cluster analysis based on each PC were shown in Table VI.
Table V.
Principal component analysis after varimax rotation
| Item | PCA1 | PCA2 | PCA3 | PCA4 | PCA5 |
|---|---|---|---|---|---|
| I think this outbreak will elongate the entire treatment | 0.838 | 0.082 | −0.019 | 0.131 | 0.020 |
| I think this outbreak caused my teeth not to move as expected | 0.770 | 0.082 | 0.050 | 0.075 | −0.080 |
| I think the outbreak will elongate the entire treatment, and I am anxious about it | 0.704 | 0.486 | −0.018 | 0.060 | −0.125 |
| I wouldn't have started orthodontic treatment if I had known the outbreak would last this long | −0.058 | 0.817 | 0.003 | 0.001 | −0.024 |
| I think this outbreak will affect the treatment result, and I am anxious about it | 0.529 | 0.692 | 0.041 | 0.000 | −0.161 |
| After the outbreak, I just want to end the treatment as soon as possible | 0.235 | 0.677 | −0.005 | 0.084 | −0.039 |
| I think this outbreak will affect the treatment result | 0.574 | 0.625 | 0.067 | 0.046 | −0.095 |
| I don't eat hard, sticky food that can easily cause the brackets or the attachments falling off | −0.019 | −0.058 | 0.808 | −0.053 | −0.033 |
| I wear additional devices following the instructions of the doctor, such as extraoral bow, rubber band, guide plate, and chewies | −0.125 | 0.144 | 0.708 | 0.198 | 0.087 |
| I attach great importance to my oral hygiene and brush my teeth after meals in accordance with the doctor's instructions | −0.016 | 0.033 | 0.667 | 0.246 | 0.066 |
| I don't have the problems with the brackets falling off, the band loosening, and the wire breaking | 0.207 | −0.053 | 0.660 | 0.042 | −0.060 |
| I am able to deal with the accidents during the outbreak, such as brackets falling off, wire stabbing, etc. | 0.055 | 0.010 | 0.141 | 0.859 | −0.072 |
| During the outbreak, I am able to observe the teeth movement and communicate with the doctor | 0.177 | 0.080 | 0.181 | 0.801 | −0.053 |
| Even if the condition gets better and the hospital opens, I want to wait a little longer to revisit | −0.096 | 0.073 | 0.021 | −0.050 | 0.842 |
| Orthodontic treatment is a long-term procedure, and it doesn't matter that I don't go to the hospital during the outbreak | −0.043 | −0.278 | 0.019 | −0.066 | 0.773 |
Table VI.
The first 5 principal components, their variance explained (%), cumulative percentage (%), and K-means cluster analysis results based on each principal component
| Principal components | Meaning of the principal component | Variance explained, % | Cumulative percentage, % | Category | Frequency, n | Percentage, % |
|---|---|---|---|---|---|---|
| PC1 | Anxiety about the treatment duration | 27.090 | 27.090 | High | 213 | 46.51 |
| Low | 245 | 53.49 | ||||
| PC2 | Anxiety about the treatment outcome | 15.594 | 42.683 | High | 184 | 40.17 |
| Low | 274 | 59.83 | ||||
| PC3 | Compliance | 8.711 | 51.394 | High | 248 | 54.15 |
| Low | 210 | 45.85 | ||||
| PC4 | Independence | 8.033 | 59.427 | High | 243 | 53.06 |
| Low | 215 | 46.94 | ||||
| PC5 | Patience | 6.837 | 66.264 | High | 266 | 58.08 |
| Low | 192 | 41.92 |
Cronbach α value (internal consistency) for the 10 items in Section 5 was 0.938. The mean ± standard deviation for the Chinese version of the scale was 18.38 ± 7.21. The prevalence of mental distress among the participants was 38.00% (174/458), with a 95% CI of 33.50-42.50.
As shown in Table VII , the results of multivariable regression showed that female patients (OR, 1.77; 95% CI, 1.07-2.93), concern about isolation from the family or society (OR, 1.54; 95% CI, 1.04-2.30), time intervals of more than 6 months since last visit (OR, 5.02; 95% CI, 1.45-17.38), and Hubei residence (OR, 5.69; 95% CI, 2.30-14.12) had higher odds of mental distress.
Table VII.
Regressive analysis of mental distress (Kessler-10 Psychological Distress Scale)
| Independent variables | Category | OR | 95% CI | P |
|---|---|---|---|---|
| Sex | Male | Reference | Reference | 0.027∗ |
| Female | 1.77 | 1.07-2.93 | ||
| Concern about isolation | No | Reference | Reference | 0.033∗ |
| Yes | 1.54 | 1.04-2.30 | ||
| Duration from the last appointment | Within 1 mo | Reference | Reference | 0.042∗ |
| 1-2 mo | 1.35 | 0.66-2.74 | 0.414 | |
| 2-6 mo | 2.01 | 0.82-4.92 | 0.127 | |
| More than 6 mo | 5.02 | 1.45-17.38 | 0.011∗ | |
| Currently in Hubei Province | No | Reference | Reference | <0.001∗∗ |
| Yes | 5.69 | 2.30-14.12 |
∗P <0.05; ∗∗P <0.001.
Fixed lingual appliance (OR, 0.36; 95% CI, 0.17-0.78) and clear aligners (OR, 0.57; 95% CI, 0.35-0.93) were less associated with high anxiety about treatment duration (PC1) compared with the fixed labial appliance. In addition, 1-2 months (OR, 2.18; 95% CI, 1.12-4.22) and 2-6 months (OR, 2.89; 95% CI, 1.20-6.95) since the last visit were more associated with high anxiety about treatment duration compared with within 1 month since the last visit. Knowing about suspension from official accounts (OR, 1.72; 95% CI, 1.14-2.59) and told by other patients (OR, 3.96; 95% CI, 1.14-13.76) were more associated with high anxiety about treatment duration than those informed by their doctors (Table VIII ).
Table VIII.
Regressive analysis of the principal components
| Principal component | Independent variables | Category | OR | 95% CI | P |
|---|---|---|---|---|---|
| PC1, anxiety about treatment duration | Type of appliances | Fixed labial appliance | Reference | Reference | 0.008∗∗ |
| Fixed lingual appliance | 0.36 | 0.17-0.78 | 0.009∗∗ | ||
| Clear aligners | 0.57 | 0.35-0.93 | 0.024∗ | ||
| Functional appliances | 0.42 | 0.15-1.20 | 0.107 | ||
| Time since the last appointment | Within 1 mo | Reference | Reference | 0.003∗∗ | |
| 1-2 mo | 2.18 | 1.12-4.22 | 0.021∗ | ||
| 2-6 mo | 2.89 | 1.20-6.95 | 0.018∗ | ||
| More than 6 mo | 0.24 | 0.05-1.27 | 0.093 | ||
| Way to get the suspension | Informed by doctor | Reference | Reference | 0.019∗ | |
| From the official account or Web site | 1.72 | 1.14-2.59 | 0.010∗ | ||
| Told by other patients | 3.96 | 1.14-13.76 | 0.030∗ | ||
| Not aware | 1.47 | 0.52-4.15 | 0.470 | ||
| PC2, anxiety about treatment outcome | Residence | Rural area | Reference | Reference | 0.009∗∗ |
| City | 0.53 | 0.33-0.86 | |||
| Concern about isolation | No | Reference | Reference | <0.001∗∗∗ | |
| Yes | 2.02 | 1.37-2.97 | |||
| Time interval since last appointment | Within 1 mo | Reference | Reference | 0.022∗ | |
| 1-2 mo | 1.42 | 0.71-2.81 | 0.320 | ||
| 2-6 mo | 1.87 | 0.78-4.48 | 0.158 | ||
| More than 6 mo | 7.44 | 1.97-28.11 | 0.003∗∗ | ||
| PC3, compliance | None | – | – | – | – |
| PC4, independence | Medical institution | Private dental clinic | Reference | Reference | 0.020∗ |
| Orthodontic department in dental hospital | 1.51 | 0.92-2.49 | 0.104 | ||
| Dental department in general hospital | 2.61 | 1.33-5.12 | 0.005∗∗ | ||
| Occupation and/or major | Medical-related | Reference | Reference | <0.001∗∗∗ | |
| Nonmedical-related | 0.35 | 0.20-0.60 | |||
| Close contact with subjects from Hubei Province | Yes | Reference | Reference | 0.005∗∗ | |
| No | 25.95 | 2.63-256.51 | |||
| Concern about public psychological problems | No | Reference | Reference | 0.035∗ | |
| Yes | 1.56 | 1.03-2.35 | |||
| Type of appliances | Fixed labial appliance | Reference | Reference | 0.016∗ | |
| Fixed lingual appliance | 0.92 | 0.41-2.03 | 0.828 | ||
| Clear aligners | 2.25 | 1.34-3.80 | 0.002∗∗ | ||
| Functional appliances | 1.68 | 0.63-4.49 | 0.301 | ||
| Frequency of contact from dentists | 0-1 time | Reference | Reference | 0.002∗∗ | |
| 2 times | 2.21 | 1.35-3.62 | 0.002∗∗ | ||
| 3 times and more | 2.06 | 1.15-3.69 | 0.015∗ | ||
| PC5, patience | Medical institution | Orthodontic department in dental hospital | Reference | Reference | 0.037∗ |
| Dental department in general hospital | 1.75 | 1.11-2.76 | 0.017∗ | ||
| Private dental clinic | 1.88 | 1.01-3.48 | 0.046∗ | ||
| Occupation and/or major | Medical-related | Reference | Reference | 0.034∗ | |
| Nonmedical-related | 0.57 | 0.34-0.96 | |||
| Concern about infection | No | Reference | Reference | 0.011∗ | |
| Yes | 1.91 | 1.16-3.14 | |||
| Concern about work and/or study | No | Reference | Reference | 0.048∗ | |
| Yes | 1.53 | 1.00-2.33 | |||
| Concern about daily life | No | Reference | Reference | 0.001∗∗ | |
| Yes | 0.49 | 0.32-0.74 |
∗P <0.05; ∗∗P <0.01; ∗∗∗P <0.001.
Residing in an urban area (OR, 0.53; 95% CI, 0.33-0.86), concern about isolation (OR, 2.02; 95% CI, 1.37-2.97), and more than 6 months since last visit (OR, 7.44; 95% CI, 1.97-28.11) were more associated with high anxiety about treatment outcome (PC2; Table VIII). No independent variable was found to be associated with high compliance (PC3, P >0.05).
General dental departments (OR, 2.61; 95% CI, 1.97-28.11; compared with dental clinics) and clear aligners (OR, 2.25; 95% CI, 1.34-3.80) showed a higher association with high independence (PC4). Nonmedical-related occupations showed less association with high independence. Dentist contact of 2 times (OR, 2.21; 95% CI, 1.35-3.62) and ≥3 times (OR, 2.06; 95% CI, 1.15-3.69) were more associated with high independence compared with 0-1 time (Table VIII).
Receiving treatment in dental clinics (OR, 1.88; 95% CI, 1.01-3.48) and general dental departments (OR, 1.75; 95% CI, 1.11-2.76) were more associated with high patience (PC5). Patients with nonmedical-related occupations (OR, 0.57; 95% CI, 0.34-0.96) had lower odds of high patience (Table VIII).
Discussion
Our study revealed that 38% (174/458) of the participants had mental distress, which was relatively worse compared with previous studies.7 , 15 The mean value of this study (18.38) was relatively higher than the mean value (16.66) of 3091 residents with 6 weeks of smoke exposure from an open-cut coalmine fire,16 which indicated the severely adverse effects of this pandemic on mental health.
The number of female patients was 3 times greater than that of male patients, which was consistent with the trend that females are more likely to seek orthodontic treatment.17 , 18 Half of the patients were undergraduates, and 61 (13.32%) patients had a higher education level than undergraduate. The reason might be that patients with higher educational level were familiar with online technology and were more willing to fill the online questionnaires.19 Another reason might be that some patients in primary or high schools were not allowed to use the smartphones by their parents.
The results of the questionnaires showed that the majority of the respondents considered COVID-19 a serious disease and showed great concern, although this study was conducted at a relatively early stage of the pandemic. The majority of the patients (90.39%) were unable to visit the orthodontists for over 1 month amid the outbreak, and the interval tends to extend as some hospitals and clinics remain closed. Over half of the patients seldom got contact with the orthodontist, because some orthodontists might not share their contact details with the patients.
In PCA, items with larger factor loadings (>0.60; Table V) were considered to be more critical in the meaning of the PCs.20 Thus, the meaning of each PC was interpreted on the basis of the content of the items. The results of the K-means cluster analysis indicated that the majority of the patients hold relatively positive attitudes toward the pandemic. Over half of them had a low level of anxiety about the treatment duration and outcome, but the anxiety might increase as the suspension goes on.
Many factors were found to be associated with orthodontic patients' mental health. In this study, we found that female patients were more likely to have mental distress, which might be attributed to the biologic nature of their responses to stressors and risk factors,21 as well as their lower quality of life in orthodontic treatment.22 In addition, patients currently in Hubei Province had significantly higher odds of mental distress as they might suffer more from the fear of the virus and endure longer isolation from society.
Patients living in rural areas were more prone to develop anxiety about treatment outcomes. The reasons might be that they had lower incomes than urban residents (P <0.001; Supplementary Table) and might be more vulnerable to the economic impact brought by the pandemic. In addition, they might endure more transportation difficulties when revisiting their orthodontists, as most dental clinics and hospitals were located in cities. Patients worried about isolation from the family or society might feel hopeless and being cut off from the society. Therefore, they were apt to have mental distress and anxiety about treatment outcomes. Additional attention could be given to these patients.
The time interval from the last dental visit was shown to be an associated factor. Disruption of routine appointments led to higher odds of mental distress and anxiety about treatment duration and outcome. Beckwith et al23 reported that each missed appointment added 1.09 months to treatment time, and 64.63% of the patients held the view that the pandemic would extend the entire treatment. It could infer that a prolonged delay during a lockdown could potentially lead to a further increase in the severity and number of patients who developed anxiety and mental distress, although the delivery of orthodontic treatment is considered to be elective and regarded as nonessential dental service when compared with dental emergencies. Orthodontists should work on relieving patients' anxiety because a 2-month delay does not affect much in the overall 2 years of treatment. In addition, the prolonged delay might have an impact on the gingival health and white spot lesion development when the lockdown period is extensive, because not every orthodontic patient develops good home care oral hygiene practices during treatment. This factor has implications on treatment outcome. Future research could investigate the longer-term impact.
The type of appliances was associated with anxiety about treatment duration. Treatment duration of both labial and lingual fixed appliances could be affected by replaced brackets and/or bands and missed appointments.24 The treatment duration of lingual appliances is similar to buccal appliances,25 but with the invisible characteristics of lingual appliances, patients seem to be less worried about the treatment duration. Another consideration is that lingual appliance wearers had higher incomes than buccal appliance wearers (P <0.001; Supplementary Table), and patients with better financial conditions might be less anxious amid this pandemic. However, the explanations to substantiate this finding would require future investigation. The esthetics of clear aligners is better than labial appliances as well,26 and clear aligners are less affected by orthodontic emergencies and missed appointments if the patients have got enough sets of aligners from the orthodontist. Therefore, patients with clear aligners also tend to be less anxious about the treatment duration.
The type of dental institution was shown to play an important role in the mental behavior of orthodontic patients. Patients registered in dental clinics showed the lowest independence to deal with orthodontic accidents, whereas patients receiving treatment at orthodontic departments in dental hospitals wanted to revisit their dentists more urgently after the pandemic. These findings might be related to the differences of dental institutions, both in practitioners and infrastructures. In the mainland of China, practitioners in public hospitals might provide patients with more official instructions,27 contributing to their high independence. The infrastructures in general dental departments and dental clinics might not be as comprehensive as the orthodontic departments in dental hospitals,28 and that would increase patients' concern with nosocomial infection, causing further delay in their revisit.
In this particular period, “teledentistry” is of great value.29 The manner of communication with patients was associated with anxiety about treatment duration. Patients who got the suspension notice directly from the doctor showed less anxiety compared with patients who got the notices from official accounts, Web sites, or other patients, suggesting effective contact was important for patients whose appointments have been interrupted. Because the pandemic is not totally under control, orthodontists should personally contact the patients regularly, especially patients from the “hotspot” areas, and give them instructions about oral health maintenance and emergency handling. In this way, the patients might express less mental distress and could maintain better orthodontic conditions by themselves.
On the basis of the results, we want to provide the following recommendations to the practitioners: (1) Routinely and directly communicate with the patients during a lockdown, (2) give priority to communication with females and patients in the epicenter and rural areas, (3) give instructions to patients on home care oral hygiene practices and emergency handling via telephones or Internet, (4) apply aligners instead of labial fixed appliances and distribute enough sets of aligners during the early stage of a lockdown, and (5) further research could be conducted to explore the exact reasons for the lingual appliances' positive impact on mental health, and to evaluate the longer-term impact of a lockdown on the mental and oral health of orthodontic patients.
This study had some limitations. In the regression analysis, several factors were found to have ORs with large CIs. For instance, Hubei residence was associated with mental distress (OR, 5.69; 95% CI, 2.30-14.12). The large CI might be due to the uneven distribution of residence, with 26 participants residing in Hubei, whereas 432 participants were from outside the province. In addition, the large CI could impair the accuracy of the estimated effect; however, the direction (damage or protect) would not be affected if the P value were significant (<0.05). In future research, an even distribution of residence might help to assess the accurate strength of the effect of Hubei residence.
Another limitation was that the 5 principal components accounted for 66% of the variance. The response scale for each item was a 5-point scale. Compared with continuous variables, this 5-point scale could impair the explained variance. Although the cumulative percentage reached over 60% in our study, which was acceptable for questionnaire studies,30 it could be improved by implementing response scales with more points. In addition, no independent variable was found to be associated with PC3 (compliance), whereas personal characteristics, pain, inconvenience, and specific dental knowledge were reported to be correlated with compliance in previous studies.31 Items related to the associated factors regarding compliance could be added into Section 1 in future questionnaires.
Conclusions
Over one-third of the orthodontic patients experienced mental distress during the early stage of the COVID-19 pandemic. Multiple factors affected the level of mental distress of orthodontic patients, such as the type of orthodontic appliance, interval from the last dental visit, manner of communication with the orthodontist, and the localities of the pandemic progression.
Footnotes
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and none were reported.
This research was supported by the National Natural Science Foundation of China to Jun Wang (grant numbers 81771114 and 81970967).
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.ajodo.2020.07.005.
Appendix
Supplementary Table.
Differences of incomes between different types of appliances and residence (n = 458)
| Independent variables | Category | <3000 yuan (n = 56) | 3000 ≤ income < 6000 yuan (n = 201) | 6000 yuan or more (n = 201) | P |
|---|---|---|---|---|---|
| Type of appliances | Fixed labial appliances | 44 | 149 | 116 | <0.001∗∗∗ |
| Fixed lingual appliances | 1 | 9 | 25 | ||
| Clear aligners | 3 | 37 | 54 | ||
| Functional appliances | 8 | 6 | 6 | ||
| Residence | Rural area | 31 | 41 | 17 | <0.001∗∗∗ |
| City | 25 | 160 | 184 |
∗∗∗P <0.001.
References
- 1.Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7:300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sone T., Nakaya N., Sugawara Y., Tomata Y., Watanabe T., Tsuji I. Longitudinal association between time-varying social isolation and psychological distress after the Great East Japan Earthquake. Soc Sci Med. 2016;152:96–101. doi: 10.1016/j.socscimed.2016.01.037. [DOI] [PubMed] [Google Scholar]
- 3.Lu C.W., Liu X.F., Jia Z.F. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395:e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meng L., Hua F., Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pitak-Arnnop P., Schubert S., Dhanuthai K., Sappayatosok K., Bauer U., Ngamwannagul P. Swine-origin H1N1 influenza A virus and dental practice: a critical review. Clin Oral Investig. 2010;14:11–17. doi: 10.1007/s00784-009-0373-2. [DOI] [PubMed] [Google Scholar]
- 7.Andrews G., Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10) Aust N Z J Public Health. 2001;25:494–497. doi: 10.1111/j.1467-842x.2001.tb00310.x. [DOI] [PubMed] [Google Scholar]
- 8.Feng D., Kong W., Zhao W., Li Z., Wang L. The mediating role of perceived prejudice in the relationship between self-esteem and psychological distress among Chinese male nursing students. J Prof Nurs. 2019;35:505–511. doi: 10.1016/j.profnurs.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Bu X.Q., You L.M., Li Y., Liu K., Zheng J., Yan T.B. Psychometric properties of the Kessler 10 Scale in Chinese parents of children with cancer. Cancer Nurs. 2017;40:297–304. doi: 10.1097/NCC.0000000000000392. [DOI] [PubMed] [Google Scholar]
- 10.Huang J.P., Xia W., Sun C.H., Zhang H.Y., Wu L.J. Psychological distress and its correlates in Chinese adolescents. Aust N Z J Psychiatry. 2009;43:674–680. doi: 10.1080/00048670902970817. quiz 681. [DOI] [PubMed] [Google Scholar]
- 11.Şimşek G.G., Noyan F. McDonald's ωt, Cronbach's α, and generalized θ for composite reliability of common factors structures. Commun Stat Simul Comput. 2013;42:2008–2025. [Google Scholar]
- 12.Scullin M.K., Harrison T.L., Factor S.A., Bliwise D.L. A neurodegenerative disease sleep questionnaire: principal component analysis in Parkinson's disease. J Neurol Sci. 2014;336:243–246. doi: 10.1016/j.jns.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goni M.D., Naing N.N., Hasan H., Wan-Arfah N., Deris Z.Z., Arifin W.N. Development and validation of knowledge, attitude and practice questionnaire for prevention of respiratory tract infections among Malaysian Hajj pilgrims. BMC Public Health. 2020;20:189. doi: 10.1186/s12889-020-8269-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hosmer D.W., Hosmer T., Le Cessie S., Lemeshow S. A comparison of goodness-of-fit tests for the logistic regression model. Stat Med. 1997;16:965–980. doi: 10.1002/(sici)1097-0258(19970515)16:9<965::aid-sim509>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 15.Zenebe Y., Necho M. Socio-demographic and substance-related factors associated with mental distress among Wollo University students: institution-based cross-sectional study. Ann Gen Psychiatry. 2019;18:28. doi: 10.1186/s12991-019-0252-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maybery D., Jones R., Dipnall J.F., Berger E., Campbell T., McFarlane A. A mixed-methods study of psychological distress following an environmental catastrophe: the case of the Hazelwood open-cut coalmine fire in Australia. Anxiety Stress Coping. 2020;33:216–230. doi: 10.1080/10615806.2019.1695523. [DOI] [PubMed] [Google Scholar]
- 17.Agou S., Locker D., Streiner D.L., Tompson B. Impact of self-esteem on the oral-health-related quality of life of children with malocclusion. Am J Orthod Dentofacial Orthop. 2008;134:484–489. doi: 10.1016/j.ajodo.2006.11.021. [DOI] [PubMed] [Google Scholar]
- 18.Krey K.F., Hirsch C. Frequency of orthodontic treatment in German children and adolescents: influence of age, gender, and socio-economic status. Eur J Orthod. 2012;34:152–157. doi: 10.1093/ejo/cjq155. [DOI] [PubMed] [Google Scholar]
- 19.Park K., Park N., Heo W., Gustafson K. What prompts college students to participate in online surveys? Int Educ Stud. 2019;12:69–79. [Google Scholar]
- 20.Henson R.K., Roberts J.K. Use of exploratory factor analysis in published research: common errors and some comment on improved practice. Educ Psychol Meas. 2006;66:393–416. [Google Scholar]
- 21.Tesfahunegn T.B., Gebremariam E.H. Mental distress and associated factors among Aksum University students, Ethiopia: a cross-sectional study. BMC Psychiatry. 2019;19:71. doi: 10.1186/s12888-019-2051-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paes da Silva S., Pitchika V., Baumert U., Wehrbein H., Schwestka-Polly R., Drescher D. Oral health-related quality of life in orthodontics: a cross-sectional multicentre study on patients in orthodontic treatment. Eur J Orthod. 2020;42:270–280. doi: 10.1093/ejo/cjz064. [DOI] [PubMed] [Google Scholar]
- 23.Beckwith F.R., Ackerman R.J., Jr., Cobb C.M., Tira D.E. An evaluation of factors affecting duration of orthodontic treatment. Am J Orthod Dentofacial Orthop. 1999;115:439–447. doi: 10.1016/s0889-5406(99)70265-9. [DOI] [PubMed] [Google Scholar]
- 24.Mavreas D., Athanasiou A.E. Factors affecting the duration of orthodontic treatment: a systematic review. Eur J Orthod. 2008;30:386–395. doi: 10.1093/ejo/cjn018. [DOI] [PubMed] [Google Scholar]
- 25.Knösel M., Klang E., Helms H.J., Wiechmann D. Lingual orthodontic treatment duration: performance of two different completely customized multi-bracket appliances (Incognito and WIN) in groups with different treatment complexities. Head Face Med. 2014;10:46. doi: 10.1186/1746-160X-10-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ke Y., Zhu Y., Zhu M. A comparison of treatment effectiveness between clear aligner and fixed appliance therapies. BMC Oral Health. 2019;19:24. doi: 10.1186/s12903-018-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li X., Xu Z.R., Tang N., Ye C., Zhu X.L., Zhou T. Effect of intervention using a messaging app on compliance and duration of treatment in orthodontic patients. Clin Oral Investig. 2016;20:1849–1859. doi: 10.1007/s00784-015-1662-6. [DOI] [PubMed] [Google Scholar]
- 28.Tang H.S., Yao Z.Q., Wang W.M. Emergency management of prevention and control of the novel coronavirus infection in departments of stomatologyZhonghua Kou Qiang Yi Xue Za Zhi. 2020;55:246–248. doi: 10.3760/cma.j.cn112144-20200205-00037. Chinese. [DOI] [PubMed] [Google Scholar]
- 29.Kravitz N.D., Burris B., Butler D., Dabney C.W. Teledentistry, do-it-yourself orthodontics, and remote treatment monitoring. J Clin Orthod. 2016;50:718–726. [PubMed] [Google Scholar]
- 30.Hair J.F., Black W.C., Babin B.J., Anderson R.E. 8th ed. Cengage Learning, EMEA; Hampshire, United Kingdom: 2019. Multivariate data analysis; pp. 195–215. [Google Scholar]
- 31.Egolf R.J., BeGole E.A., Upshaw H.S. Factors associated with orthodontic patient compliance with intraoral elastic and headgear wear. Am J Orthod Dentofacial Orthop. 1990;97:336–348. doi: 10.1016/0889-5406(90)70106-M. [DOI] [PubMed] [Google Scholar]