Summary
Background
COVID-19 is an ongoing global pandemic. Changes in haematological characteristics in patients with COVID-19 are emerging as important features of the disease. We aimed to explore the haematological characteristics and related risk factors in patients with COVID-19.
Methods
This retrospective cohort study included patients with COVID-19 admitted to three designated sites of Wuhan Union Hospital (Wuhan, China). Demographic, clinical, laboratory, treatment, and outcome data were extracted from electronic medical records and compared between patients with moderate, severe, and critical disease (defined according to the diagnosis and treatment protocol for novel coronavirus pneumonia, trial version 7, published by the National Health Commission of China). We assessed the risk factors associated with critical illness and poor prognosis. Dynamic haematological and coagulation parameters were investigated with a linear mixed model, and coagulopathy screening with sepsis-induced coagulopathy and International Society of Thrombosis and Hemostasis overt disseminated intravascular coagulation scoring systems was applied.
Findings
Of 466 patients admitted to hospital from Jan 23 to Feb 23, 2020, 380 patients with COVID-19 were included in our study. The incidence of thrombocytopenia (platelet count <100 × 109 cells per L) in patients with critical disease (42 [49%] of 86) was significantly higher than in those with severe (20 [14%] of 145) or moderate (nine [6%] of 149) disease (p<0·0001). The numbers of lymphocytes and eosinophils were significantly lower in patients with critical disease than those with severe or moderate disease (p<0·0001), and prothrombin time, D-dimer, and fibrin degradation products significantly increased with increasing disease severity (p<0·0001). In multivariate analyses, death was associated with increased neutrophil to lymphocyte ratio (≥9·13; odds ratio [OR] 5·39 [95% CI 1·70–17·13], p=0·0042), thrombocytopenia (platelet count <100 × 109 per L; OR 8·33 [2·56–27·15], p=0·00045), prolonged prothrombin time (>16 s; OR 4·94 [1·50–16·25], p=0·0094), and increased D-dimer (>2 mg/L; OR 4·41 [1·06–18·30], p=0·041). Thrombotic and haemorrhagic events were common complications in patients who died (19 [35%] of 55). Sepsis-induced coagulopathy and International Society of Thrombosis and Hemostasis overt disseminated intravascular coagulation scores (assessed in 12 patients who survived and eight patients who died) increased over time in patients who died. The onset of sepsis-induced coagulopathy was typically before overt disseminated intravascular coagulation.
Interpretation
Rapid blood tests, including platelet count, prothrombin time, D-dimer, and neutrophil to lymphocyte ratio can help clinicians to assess severity and prognosis of patients with COVID-19. The sepsis-induced coagulopathy scoring system can be used for early assessment and management of patients with critical disease.
Funding
National Key Research and Development Program of China.
Introduction
In December, 2019, an outbreak of COVID-19 caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) occurred in Wuhan, China,1 and has rapidly infected people across the world. COVID-19 presents as complicated clinical manifestations, from flu-like symptoms to multiple organ failure and death.1 Nearly 20% of patients with COVID-19 become critically ill, with a high mortality ranging from 8·1% to 33%.1, 2, 3 According to the diagnosis and treatment protocol for novel coronavirus pneumonia (trial version 7)4 published by the National Health Commission of China, there are four severity levels of COVID-19 based on the clinical manifestations: mild, moderate, severe, and critical disease. To some degree, differentiating severe patients from non-severe patients is helpful and can improve the cure rate of COVID-19. However, the criteria used for classification are respiratory factors such as respiratory rate, oxygen saturation, and lesion progression in pulmonary imaging.
Severe, especially critical, cases are usually complicated by other organ dysfunctions, including septic shock, heart failure, and disseminated intravascular coagulation (DIC).5, 6 In clinical practice, some thrombotic complications have been reported, including ischaemic limbs, strokes, and venous thromboembolism. Venous thromboembolism is common in patients with severe disease.7, 8, 9, 10, 11, 12 Although several studies reported that decreased platelet count and increased D-dimer were associated with severe COVID-19 and high mortality,5, 13, 14 few studies have systematically assessed haematological and coagulation parameters among patients with moderate, severe, and critical COVID-19. Coagulopathy is also common in patients with critical and fatal disease.6, 14 Therefore, finding efficient haematology and coagulation parameters for risk classifications and to predict prognosis is a priority.
Research in context.
Evidence before this study
We searched PubMed on March 20 and May 22, 2020, for articles that documented haematological factors and fatal outcomes of patients with COVID-19, resulting from infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), using the search terms (“novel coronavirus 2019” OR “SARS-CoV-2” OR “COVID-19”) AND (“death” OR “mortality” OR “hematology characteristics”) with no language or time restrictions. Most of the studies were focused on pneumology, gastroenterology, and neurology in patients with COVID-19. Several groups found that increased D-dimer and fibrin degradation products, as well as baseline platelet concentrations and changes, were associated with poor prognosis. Two studies from Italy found that patients with COVID-19 had severe hypercoagulability rather than hypocoagulability (ie, consumption coagulopathy). One study showed that anticoagulant therapy might improve prognosis of patients with severe COVID-19. Several teams reported that the incidence of thromboembolic complications in patients with severe disease and those who died (25–85%) was much higher than in those with non-severe disease and those who survived (8–15%). Furthermore, autopsies showed deep-vein thrombosis in seven (58%) of 12 patients in whom venous thromboembolism was not suspected before death, suggesting that the thrombosis risk was underestimated in COVID-19. One study showed that thromboprophylaxis halved the incidence of deep-vein thrombosis in patients with COVID-19 with a Padua prediction score of 4 or more. A small prospective observational study showed that preventive anticoagulation therapy might inhibit thrombosis by reversing the profile of hypercoagulability. However, few published studies have systematically assessed haematological characteristics in terms of disease severity and mortality in patients with COVID-19.
Added value of this study
This retrospective cohort study focuses on haematological and coagulation parameters in patients with moderate, severe, and critical COVID-19, along with specific analyses of coagulopathy in non-survivors. We found that some haematological indicators varied with disease severity. And the incidence of coagulopathy in non-survivors was high, with abnormalities in coagulation tests or typical signs, including thrombotic complications, bleeding, and unexplained organ failure. Furthermore, the combination of neutrophil to lymphocyte ratio, platelet count, D-dimer, and prothrombin time might provide clues for recognising poor prognosis.
Implications of all the available evidence
Dynamically monitoring haematological and coagulation parameters, such as neutrophil to lymphocyte ratio, platelet count, D-dimer, and prothrombin time might provide a reliable and convenient method for classifying and predicting the severity and outcomes of patients with COVID-19. Regularly assessing and screening the conditions of thrombosis and early disseminated intravascular coagulation among patients with severe or critical disease is necessary. Prophylactic strategies, including anticoagulation therapy, might potentially prevent patient deterioration and improve survival.
Here, we present a multicentre retrospective analysis to uncover the role of the haematological system in COVID-19 and explore the haematology and coagulation parameters for stratification and prognosis of critical cases of COVID-19.
Methods
Study design and participants
This retrospective cohort study included inpatients from three designated sites (the Main Campus, West Campus, and Cancer Centre) at the Wuhan Union Hospital (Wuhan, China).
Patients diagnosed with COVID-19 according to WHO interim guidance with positive SARS-CoV-2 RNA detection in throat swab specimens and moderate or worse disease were eligible. Exclusion criteria were missing haematology and coagulation data, transfer to other medical facilities with unknown outcomes, and age younger than 18 years.
The study was approved (number 20 200 080) by the research ethics commission of Wuhan Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, and the requirement for informed consent was waived by the ethics commission.
Definitions
According to the diagnosis and treatment protocol for novel coronavirus pneumonia (trial version 7)4 published by the National Health Commission, patients meeting any of the following criteria were classified as having critical disease: respiratory failure requiring mechanical ventilation; shock; or other organ failure that requires monitoring and treatment in an intensive care unit. Severe cases were defined as respiratory distress (≥30 breaths per min), oxygen saturation of 93% or less at rest, ratio of arterial partial pressure of oxygen to fractional concentration of oxygen in inspired air of 40 kPa or less, or more than 50% lesion progression over 24–48 h in pulmonary imaging. Moderate disease was defined as fever and respiratory symptoms with radiological findings of pneumonia but without the severe or critical features. Patients with mild disease, defined as mild clinical symptoms and no sign of pneumonia on imaging, did not require hospital admission so were not included in this study.
Procedures
Demographic, clinical, laboratory, treatment, and outcome data were extracted from electronic medical records. Laboratory tests were done at admission and then with some regularity according to the patients' condition during their hospital stay. For patients with generally stable vital signs, blood samples were taken every week; for severe or worsening patients, they were taken every 3 days or more frequently. Blood examinations involved measuring complete blood count, coagulation profile, serum biochemical tests, cytokines, and serum ferritin. Particularly, coagulation tests including prothrombin time, activated partial thromboplastin time (APTT), antithrombin III activity, fibrinogen, fibrin degradation products, and D-dimer were detected using a STA-R evolution coagulation analyser and original reagents (Diagnostica Stago, Saint-Denis, France). All laboratory tests were done in the core laboratory of Wuhan Union Hospital with standard procedures.
Acute respiratory distress syndrome (ARDS) was defined according to the Berlin definition.15 Septic shock was defined according to the 2016 third international consensus definition for septic shock.16 Coagulopathy was commonly referred to as haemorrhage or clotting disorder.17 Patients were screened by two scoring systems: sepsis-induced coagulopathy (SIC); and International Society of Thrombosis and Hemostasis (ISTH) overt DIC.18 The SIC system was proposed by the Scientific and Standardization Committee on DIC to identify an earlier phase of DIC and to facilitate early recognition and anticoagulant treatment in clinical practice.19 Critically ill patients were assessed for SIC (≥4 points) and ISTH overt DIC (≥5 points) retrospectively. Treatment of patients with low molecular weight heparin (LMWH) was recorded. Prophylactic anticoagulation treatment was not routinely given to patients with worse disease. Whether and when to implement treatment was judged by treating doctors. All data were checked electronically and classification of COVID-19 severity was taken as the worst classification during the patient's hospital stay. These assessments were done retrospectively by two physicians (FZ and DL), and a third researcher (HM) adjudicated any difference in interpretation between the two primary reviewers. Methods for laboratory confirmation of SARS-CoV-2 infection have been described elsewhere.1 Briefly, throat-swab specimens were obtained for SARS-CoV-2 detection by next-generation sequencing or real-time PCR methods. Discharged patients were followed up by telephone and appointments once every 2 weeks.
Statistical analysis
Continuous variables were expressed as mean and SD or median and IQR. For data with non-normal distribution, the Kruskal-Wallis test was used. The independent group t test was used to analyse normally distributed continuous variables, and the Mann-Whitney U test was used to analyse non-normally distributed continuous variables. Categorical variables were presented as frequency rates and percentages and analysed using χ2 test or Fisher's exact test as appropriate. We did multiple comparisons among groups using the Bonferroni adjustment method. To obtain a more accurate model, we included significant variables with an area under the curve greater than 0·6 in the multivariate logistic regression model using a stepwise selection procedure. A multivariable logistic regression model was fit to estimate the effect of indicators on inpatient mortality for severe and critical patients. We compared data from repeated measures using the linear mixed model. Groups (survivor vs non-survivor) and timepoints were fixed effects, and individuals were random effects. A two-sided p value of 0·05 or less was considered statistically significant. We did statistical analyses using SPSS software (version 23.0) unless otherwise indicated.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. YH and HM had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Between Jan 23 and Feb 23, 2020, 466 patients were admitted to Wuhan Union Hospital. 86 patients were excluded from the study because they did not have haematology and coagulation data (28 patients), they were transferred to other medical facilities with unknown outcomes (55 patients), or they were younger than 18 years (three patients). Data from 380 patients admitted to hospital with confirmed COVID-19 were analysed in our study (table 1 ). The patients with severe and critical disease were older than those with moderate disease. Men had more severe disease than women. 182 (48%) of 380 patients had comorbidities, with hypertension being the most common, followed by diabetes, coronary heart disease, and carcinoma. Of the 86 patients with critical illness, 19 (22%) patients received high-flow nasal cannula oxygen therapy, 31 (36%) received non-invasive mechanical ventilation, and 47 (55%) received invasive mechanical ventilation. 32 (37%) patients received vasopressors and five (6%) patients received kidney replacement therapy. Clinical outcomes were monitored up to March 20, 2020.
Table 1.
Demographic characteristics of the cohort
| Total (n=380) | Moderate disease (n=149) | Severe disease (n=145) | Critical disease (n=86) |
p value |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Overall | Moderate vs severe | Moderate vs critical | Severe vs critical | ||||||
| Age, years | 64·0 (53·0–73·0) | 56·0 (41·5–67·5) | 67·0 (58·0–76·0) | 68·0 (61·0–78·0) | <0·0001 | <0·0001 | <0·0001 | 1·0 | |
| Sex | |||||||||
| Female | 174 (46%) | 80 (54%) | 69 (48%) | 25 (29%) | 0·0011* | 0·89 | <0·0001 | 0·017 | |
| Male | 206 (54%) | 69 (46%) | 76 (52%) | 61 (71%) | .. | .. | .. | .. | |
| Comorbidity | |||||||||
| Any | 182 (48%) | 60 (40%) | 74 (51%) | 48 (56%) | 0·045* | 0·19 | 0·064 | 1·0 | |
| Diabetes | 61 (16%) | 14 (9%) | 30 (21%) | 17 (20%) | 0·017* | 0·020 | 0·071 | 1·0 | |
| Hypertension | 114 (30%) | 37 (25%) | 49 (34%) | 28 (33%) | 0·21* | .. | .. | .. | |
| Coronary heart disease | 22 (6%) | 11 (7%) | 3 (2%) | 8 (9%) | 0·030† | 0·097 | 1·0 | 0·064 | |
| Carcinoma | 20 (5%) | 4 (3%) | 8 (6%) | 8 (9%) | 0·085† | .. | .. | .. | |
| Other | 77 (20%) | 21 (14%) | 24 (17%) | 32 (37%) | <0·0001* | 1·0 | 0·00013 | 0·0012 | |
| Death | 55 (14%) | 0 | 2 (1%) | 53 (62%) | <0·0001† | 0·73 | <0·0001 | <0·0001 | |
Data are median (IQR) or n (%). For variables with overall p values graeter than 0·05, we did not perform group comparisons. Categorical variables were analysed using
χ2 test or
Fisher's exact test.
Of the haematological and coagulation parameters (table 2 ), neutrophil count, lymphocyte count, neutrophil to lymphocyte ratio, prothrombin time, D-dimer, fibrin degradation products, C-reactive protein, and lactate dehydrogenase (all p<0·0001), and white blood cell count, IL-10, and serum ferritin (p<0·05), were significantly different across all comparisons. Counts of eosinophils and platelets were significantly lower in patients with critical disease than those with severe disease (p<0·0001). Thrombocytopenia (platelet count <100 × 109 cells per L) was recorded in 42 (49%) of 86 patients with critical disease, which is a significantly higher frequency than in patients with severe (20 [14%] of 145) and moderate (nine [6%] of 149) disease (both p<0·0001).
Table 2.
Laboratory findings of the patients on admission
| Missing data | Total (n=380) | Moderate disease (n=149) | Severe disease (n=145) | Critical disease (n=86) |
p value |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Moderate vs Severe | Moderate vs Critical | Severe vs Critical | |||||||
| White blood cell count, 109 cells per L | 0 | 5·89 (4·40–8·27) | 5·05 (3·98–6·26) | 5·89 (4·36–8·28) | 9·33 (6·65–13·40) | <0·0001 | 0·00053 | <0·0001 | <0·0001 | |
| Neutrophil count, 109 cells per L | 0 | 4·19 (2·71–6·37) | 3·22 (2·37–4·39) | 4·19 (2·97–6·33) | 8·08 (5·30–12·12) | <0·0001 | <0·0001 | <0·0001 | <0·0001 | |
| Lymphocyte count, 109 cells per L | 0 | 0·95 (0·59–1·47) | 1·2 (0·90–1·59) | 0·89 (0·59–1·36) | 0·54 (0·30–0·91) | <0·0001 | <0·0001 | <0·0001 | <0·0001 | |
| Neutrophil to lymphocyte ratio | 0 | 4·14 (2·25–9·08) | 2·67 (1·69–4·08) | 4·71 (2·62–7·78) | 16·02 (6·49–24·79) | <0·0001 | <0·0001 | <0·0001 | <0·0001 | |
| Monocyte count, 109 cells per L | 44 | 0·47 (0·30–0·62) | 0·46 (0·35–0·61) | 0·52 (0·32–0·64) | 0·38 (0·20–0·54) | 0·0020 | 1·0 | 0·014 | 0·0020 | |
| Eosinophil count, 109 cells per L | 0 | 0·03 (0·01–0·09) | 0·04 (0·01–0·10) | 0·05 (0·01–0·11) | 0·01 (0–0·03) | <0·0001 | 1·0 | <0·0001 | <0·0001 | |
| Basophil count, 109 cells per L | 44 | 0·01 (0·01–0·03) | 0·01 (0·01–0·03) | 0·01 (0·01–0·03) | 0·03 (0·01–0·03) | 0·39 | .. | .. | .. | |
| Haemoglobin, g/dL | 0 | 119·00 (107·25–131·00) | 122·00 (111·00–133·00) | 118·00 (108·50–129·50) | 115·00 (92·75–127·25) | 0·0012 | 0·11 | 0·0014 | 0·22 | |
| Platelet count, 109 cells per L | 0 | 189·50 (121·50–271·00) | 198·00 (145·50–249·50) | 227·00 (142·50–328·00) | 105·00 (55·75–200·75) | <0·0001 | 0·23 | <0·0001 | <0·0001 | |
| <100 | .. | 71/380 (19%) | 9/149 (6%) | 20/145 (14%) | 42/86 (49%) | <0·0001* | 0·077 | <0·0001 | <0·0001 | |
| ≥100 | .. | 309/380 (81%) | 140/149 (94%) | 125/145 (86%) | 44/86 (51%) | .. | .. | .. | .. | |
| Activated partial thromboplastin time, s | 30 | 37·40 (34·30–42·33) | 36·20 (33·38–39·70) | 37·60 (35·13–42·48) | 38·80 (34·23–48·15) | 0·0018 | 0·028 | 0·0021 | 0·85 | |
| ≤43·5 | .. | 274/350 (78%) | 116/130 (89%) | 106/136 (78%) | 52/84 (62%) | <0·0001* | 0·040 | <0·0001 | 0·031 | |
| >43·5 | .. | 76/350 (22%) | 14/130 (11%) | 30/136 (22%) | 32/84 (38%) | .. | .. | .. | .. | |
| Prothrombin time, s | 31 | 13·60 (12·80–14·80) | 13·00 (12·50–13·70) | 13·70 (12·90–14·55) | 16·60 (14·00–21·98) | <0·0001 | <0·0001 | <0·0001 | <0·0001 | |
| Fibrinogen, g/L | 75 | 4·37 (3·39–5·46) | 4·29 (3·42–5·23) | 4·80 (3·62–5·96) | 3·96 (2·60–5·14) | 0·00064 | 0·044 | 0·34 | 0·0014 | |
| <2 | .. | 18/305 (6%) | 1/135 (1%) | 0/86 | 17/84 (20%) | <0·0001† | 1·0 | <0·0001 | <0·0001 | |
| ≥2 | .. | 287/305 (94%) | 134/135 (99%) | 86/86 (100%) | 67/84 (80%) | .. | .. | .. | .. | |
| D-dimer, mg/L | 47 | 1·24 (0·47–4·58) | 0·42 (0·22–0·91) | 1·36 (0·65–3·06) | 7·24 (3·39–8·00) | <0·0001 | <0·0001 | <0·0001 | <0·0001 | |
| Fibrin degradation products, μg/mL | 132 | 3·20 (1·70–10·98) | 1·90 (1·23–3·18) | 4·20 (2·10–11·60) | 28·20 (6·00–113·15) | <0·0001* | <0·0001 | <0·0001 | <0·0001 | |
| Antithrombin III activity, % | 132 | 90·00 (79·00–97·00) | 92·00 (84·00–98·75) | 88·00 (78·00–95·00) | 85·00 (70·25–97·50) | 0·014 | 0·028 | 0·086 | 1·0 | |
| <80 | .. | 66/248 (27%) | 17/108 (16%) | 33/95 (35%) | 16/45 (36%) | 0·0030* | 0·0052 | 0·020 | 1·0 | |
| ≥80 | .. | 182/248 (73%) | 91/108 (84%) | 62/95 (65%) | 29/45 (64%) | .. | .. | .. | .. | |
| C-reactive protein, mg/L | 65 | 35·54 (7·41–84·43) | 10·15 (2·15–30·84) | 40·6 (10·49–83·20) | 92·79 (55·73–124·36) | <0·0001 | <0·0001 | <0·0001 | <0·0001 | |
| IL-6, pg/mL | 95 | 17·85 (5·26–46·73) | 14·13 (4·97–44·56) | 23·77 (10·10–49·03) | 37·4 (15·30–95·33) | <0·0001 | 0·053 | <0·0001 | 0·083 | |
| TNFα, ng/L | 128 | 2·45 (1·97–3·61) | 2·57 (2·00–3·93) | 2·45 (1·98–3·92) | 2·22 (1·92–2·90) | 0·082 | .. | .. | .. | |
| IL-4, ng/L | 128 | 2·10 (1·62–2·48) | 2·10 (1·58–2·42) | 2·10 (1·64–2·82) | 2·16 (1·66–2·62) | 0·42 | .. | .. | .. | |
| IL-2, ng/L | 128 | 2·56 (2·34–2·88) | 2·53 (2·34–2·79) | 2·56 (2·39–2·93) | 2·67 (2·34–2·95) | 0·14 | .. | .. | .. | |
| IL-10, ng/L | 121 | 4·04 (3·04–5·53) | 3·44 (2·67–4·49) | 4·43 (3·29–5·94) | 5·14 (4·15–8·50) | <0·0001 | 0·00031 | <0·0001 | 0·018 | |
| IFNγ, ng/L | 128 | 2·11 (1·70–2·62) | 2·09 (1·72–2·53) | 2·13 (1·67–2·83) | 2·11 (1·68–2·68) | 0·77 | .. | .. | .. | |
| Serum ferritin, μg/L | 302 | 530·45 (265·25–924·05) | 108·20 (57·55–310·20) | 539·19 (356·88–843·65) | 1146·20 (733·80–1749·10) | <0·0001 | <0·0001 | <0·0001 | 0·040 | |
| Lactate dehydrogenase, units per L | 102 | 283·00 (184·00–441·75) | 184·00 (166·00–234·00) | 302·00 (209·00–432·50) | 472·00 (353·00–610·00) | <0·0001 | <0·0001 | <0·0001 | <0·0001 | |
Data are median (IQR) or n/N (%) unless otherwise stated. For variables with overall p values greater than 0·05, we did not perform group comparisons. Categorical variables were analysed using
χ2 test or
Fisher's exact test.
Regarding coagulation parameters (table 2), APTT, prothrombin time, fibrinogen, D-dimer, fibrin degradation products, and antithrombin III activity were significantly different across severity levels (overall p<0·05). Prothrombin time (p<0·0001), D-dimer (p<0·0001), and fibrin degradation products (p<0·0001) were significantly higher in patients who were critically ill than in those with moderate and severe disease. The proportion of patients with prolonged APTT (ie, >43·5 s) was 14 (11%) of 130 patients with moderate disease compared with 32 (38%) of 84 with critical disease (p<0·0001). Fibrinogen concentration was significantly lower in patients with critical disease than in those with severe disease (p=0·0014). 17 (20%) of 84 patients with critical disease had low fibrinogen (<2 g/L); however, only one (1%) of 135 patients with moderate disease and none of the 86 with severe disease had low fibrinogen. The incidence of low antithrombin III activity (<80%) was higher in patients with severe (33 [35%] of 95, p=0·0052) and critical (16 [36%] of 45, p=0·020) disease than in those with moderate disease (17 [16%] of 108), but similar between patients with severe and critical disease (p=1·0).
55 in-hospital deaths occurred, most of which (53 patients [96%]) were in patients with critical disease, and two (4%) in patients with severe disease. ARDS (38 [69%] of 55) and septic shock (11 [20%]) were common complications in non-survivors, with thrombotic and haemorrhagic events (19 [35%]), including DIC (eight [15%]), venous thromboembolism (three [5%]), gastrointestinal bleeding (three [5%]), acute myocardial infarction (two [4%]), haematuresis (two [4%]), and acute cerebral infarction (one [2%]) also seen. Because all deaths were in patients with severe or critical disease, we compared variables between survivors (176 patients) and non-survivors (55 patients) who had severe or critical disease, aiming to identify risk factors for in-hospital deaths (appendix pp 1–4). Of the 55 patients who died, 40 (73%) were men and 15 (27%) were women. Concentrations of C-reactive protein, IL-6, IL-10, serum ferritin, and lactate dehydrogenase differed among survivors and non-survivors, similar to previous reports.5, 14 Although non-survivors had higher median IL-6 (61·53 pg/mL [IQR 16·45–122·08]) than survivors (24·91 pg/mL [11·02–54·36], p=0·026), the incidence of increased IL-6 (>10 pg/mL) did not differ between the two groups (101 [78%] of 129 survivors vs 29 [88%] of 33 non-survivors, p=0·22). The proportion of patients with leucocytosis, lymphopenia, thrombocytopenia, and anaemia, and values for neutrophil to lymphocyte ratio, APTT, prothrombin time, fibrinogen, and D-dimer, were significantly different between survivors and non-survivors (appendix pp 1–4).
Taking sensitivity and specificity into consideration, we chose the variables with more than 0·6 area under receiver operating characteristic curve in the multivariable logistic regression model. Increased neutrophil to lymphocyte ratio (≥9·13; odds ratio [OR] 5·39 [95% CI 1·70–17·13], p=0·0042), increased D-dimer (>2 mg/L; OR 4·41 [1·06–18·30], p=0·041), thrombocytopenia (platelet count <100 × 109 cells per L; OR 8·33 [2·56–27·15], p=0·00045), and prolonged prothrombin time (>16 s; OR 4·94 [1·50–16·25], p=0·0094) were associated with increased risk of death (appendix pp 1–3).
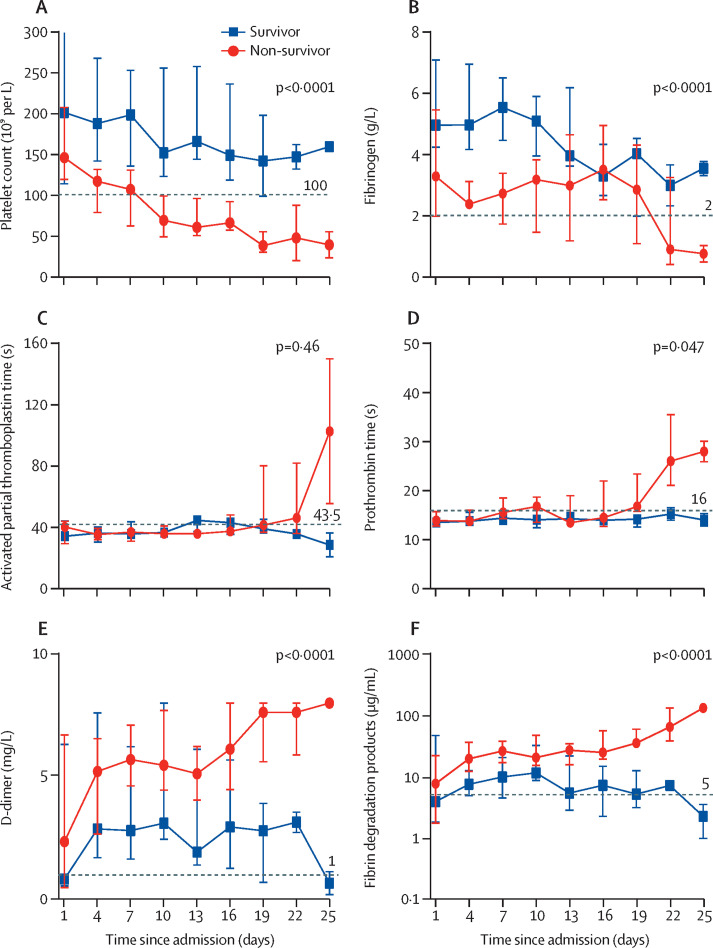
Eight non-survivors and 12 survivors had the dynamically monitored clinical and laboratory results needed for assessing SIC and overt DIC over the time period of their hospital stay, so the coagulation laboratory markers were compared between the two groups. Platelet count clearly decreased in non-survivors compared with survivors throughout the clinical course (figure ). Prothrombin time, D-dimer, and fibrin degradation products increased for non-survivors compared with survivors toward the end of the study period. Fibrinogen decreased for both non-survivors and survivors. We used two-step DIC diagnosis for sepsis-associated DIC recommended by ISTH; scores of SIC and ISTH overt DIC were recorded retrospectively. SIC and ISTH overt DIC both increased over time in the non-survivors (appendix p 5). The median SIC score reached diagnostic criteria (four points) on day 10, whereas the median ISTH overt DIC scores reached five after day 19. We investigated anticoagulation treatment, 4000 IU of LMWH once daily was most commonly used. Despite varied course of disease, onset of SIC typically preceded that of overt DIC (appendix p 5).
Figure.
Temporal changes of coagulation laboratory markers in critically ill patients with COVID-19
Platelet count (A), fibrinogen (B), activated partial thromboplastin time (C), prothrombin time (D), D-dimer (E), and fibrin degradation products (F) after admission of patients with COVID-19 who survived (n=12) and those who did not (n=8), who had these markers measured during their hospital stay. Data points are medians and error bars are IQRs. Horizontal dashed lines show the lower normal limits in A and B and upper normal limits in C–F.
Discussion
The results of this cohort study provide several important insights. Thrombotic and haemorrhagic events were common complications in non-survivors. An outcome of death was associated with thrombocytopenia, increased neutrophil to lymphocyte ratio, prolonged prothrombin time, and increased D-dimer. SIC and overt DIC scores also increased over time in the non-survivors.
The incidence of thrombocytopenia on admission was lower in patients with COVID-19 than in severe acute respiratory syndrome (SARS; 40–45%) and Middle East respiratory syndrome (MERS, 36%),20 but it increased with disease severity. Furthermore, platelet count decreased in patients with progressively severe illness. Decreased platelet count, reflecting their consumption and thrombin generation, is helpful in recognising the presence and severity of coagulopathy. Thrombocytopenia is common in viral infections, which might be explained by immunological platelet destruction, inappropriate platelet activation and consumption, and impaired megakaryopoiesis.21 However, whether mechanisms of thrombocytopenia differ between SARS-CoV-2 and other coronaviruses remains unknown. One possible reason might be the different types and concentrations of cytokines resulting in different degrees of coagulation disorders. Although patients infected with MERS-CoV were reported to have increased IFNγ,22 TNFα, IL-15, and IL-17, patients with severe COVID-19 had increased IL-1β, IL-6, IL-2, IL-2R, IL-7, IL-10, and TNFα.23
As knowledge of COVID-19 expands, inflammatory factors and lymphocyte function tests have been suggested for assessing severity of disease.4 However, not all tests can be easily accessed. Our results showed that high neutrophil to lymphocyte ratio, which might be a result of excessive inflammation and immune suppression in sepsis triggered by SARS-CoV-2 infection, can be useful for predicting severity and mortality. Routine blood tests are readily available and neutrophil to lymphocyte ratio can be calculated easily. In sepsis, neutrophils are hyperactivated with delayed apoptosis disorder, along with the depletion and exhaustion of CD4 and CD8 T cells as a result of apoptosis,24 which are common events in severe COVID-19.25 Partly due to T-cell apoptosis, lymphocytopenia is also common in SARS-CoV and MERS-CoV infection.20 Compared with less easily accessible tests, neutrophil to lymphocyte ratio appears to be an efficient and practical indicator for risk of COVID-19 mortality.
A large epidemiological study reported that about 50% of patients with COVID-19 have increased D-dimer during disease progression,3 and this proportion was as high as nearly 100% in patients who died,5, 6 which is consistent with our findings. Furthermore, we observed that non-survivors had progressively increasing D-dimer and fibrin degradation products, which reflect dissolution of thrombi, in accordance with previous studies.5, 6 The observation that fibrinogen gradually decreased over time in non-survivors but substantially increased during the early disease stages of COVID-19 might be explained by it being an acute reactive protein that is continuously consumed during disease progression. We also found that prothrombin time and APTT were within normal range in most patients at admission, perhaps because hypercoagulability occurs at the early stages of COVID-19.26 But long-lasting consumption of clotting factors might be the reason that prothrombin time progressively increased in non-survivors at the late stage of disease. Although the combination of thrombocytopenia, increased D-dimer, and prolonged prothrombin time is suggestive of DIC, previous studies have shown that incidence of DIC in overall and severe COVID-19 groups (0·6–2·7%) is much lower than in patients with septic shock (30–40%).3, 10, 14 However, the incidence of DIC in non-survivors in a previous study (15 [71%] of 21 patients) was much higher than in our study (eight [15%] of 55).6 Helms and colleagues10 showed that, compared with patients with non-COVID-19 ARDS, those with COVID‑19 ARDS had significantly higher prothrombin time, antithrombin, fibrinogen, and platelets, but lower APTT and D-dimer. Spiezia and colleagues26 confirmed that patients with COVID-19 and acute respiratory failure presented with a severe hypercoagulability rather than hypocoagulability (ie, consumption coagulopathy).26 These findings suggest that the pattern of coagulation differs between patients with severe COVID-19 and those with other severe diseases.
Given that DIC screening by itself might improve outcomes in patients with sepsis,27 coagulation parameters are important for the identification and intervention of coagulopathy as early as possible. In this study, we used the SIC and ISTH scoring systems for the diagnosis of DIC in patients with COVID-19. SIC is a newly proposed category delineated by a few global coagulation tests, which has been established as an early warning for DIC.19 Of note, eight non-survivors with coagulopathy had progression from SIC to ISTH overt DIC. Because of the retrospective nature of this study, we had little information about the use of LMWH in the cohort, partly because of inadequate awareness of routine thromboprophylaxis at the early stages of the pandemic. When and how to give such treatment was decided by treating doctors in different designated hospitals. In non-COVID-19 patients with sepsis and coagulopathy or DIC, large-scale randomised controlled trials reported that anticoagulant therapy resulted in a great reduction in mortality among patients with sepsis and coagulopathy or DIC.18 But those with advanced coagulopathy might have disease progression that is no longer amenable to benefit from anticoagulant therapy.18 Treatment with anticoagulants might postpone or even reverse the harmful procoagulant pattern. Tang and colleagues28 confirmed that the timely application of LMWH when patients met SIC criteria appeared to improve 28-day mortality. Fogarty and colleagues14 found that patients with COVID-19 on LMWH thromboprophylaxis rarely developed overt DIC. Further studies are needed to show whether early administration of anticoagulants can improve survival in patients with COVID-19.
Consistent with our results, accumulating evidence has shown that patients with severe and critical COVID-19 have a high risk of thrombosis (especially venous thromboembolism), even though LMWH prophylaxis was used.7, 8, 9, 10, 11, 12 Helms and colleagues10 showed that the incidence of thrombotic events (mainly pulmonary embolisms) in patients with COVID-19 ARDS were significantly higher than in non-COVID-19 patients with ARDS.10 Furthermore, Zhang and colleagues9 reported that the incidence of deep-vein thrombosis was 18 (34%) of 53 patients receiving venous thromboembolism prophylaxis whereas it was 19 (63%) of 30 in patients not receiving prophylaxis. We propose some possible mechanisms. First, refractory hypoxaemia in patients with severe COVID-19 might induce vasoconstriction resulting in reduced blood flow, promoting vascular occlusion.29 Second, because of excessive endothelial destruction, accompanied by diabetes, older age, and inevitable prolonged bed rest, patients with severe and critical COVID-19 are more susceptible to thrombotic events. Third, the fibrinolytic system might be further inhibited in COVID-19, making it more difficult to dissolve a thrombus, because patients with SARS have higher plasma plasminogen activator inhibitor-1 than both healthy controls and patients with other types of pneumonia.30 Thromboprophylaxis might decrease the incidence of thrombosis. Zhang and colleagues9 showed that thromboprophylaxis halved the incidence of deep-vein thrombosis in patients with COVID-19 with a Padua prediction score of 4 or more. On the basis of a multicentre prospective cohort study, Helms and colleagues10 suggest stronger anticoagulation strategies (eg, higher dose, higher frequency, or earlier intervention) for critically ill patients with COVID-19 than for critically ill patients without COVID-19. Therefore, we suggest that anticoagulation therapy should be considered for critical patients with COVID-19. Theoretically, the application of heparin sodium and LMWH inhibits blood coagulation, reduces inflammation, and inhibits platelet aggregation, thereby preventing thrombosis and delaying coagulopathy progression to DIC in high-risk patients. However, the timing, type, and dose of preventive anticoagulation therapy remains unclear and needs verification form high-quality randomised controlled trials.
Our study has some limitations. Some patients were excluded because of incomplete documentation of laboratory testing. Ideally, all critical patients would have had dynamic profiles of laboratory findings. In our retrospective analysis, we were able to find only eight non-survivors and 12 survivors who had the data that are needed for assessing SIC and overt DIC, such as platelet counts, coagulation parameters, serum biochemical indicators, and sequential organ failure assessment scores during hospital admission. In addition, LMWH was not given in a consistent way during the study period, so our analyses might be inaccurate. Further studies are needed to investigate the association between the early introduction of LMWH and outcomes of patients with critical disease.
In conclusion, coagulopathy is a non-negligible complication and potentially important cause of death in patients with critical COVID-19. Dynamically monitoring haematological and coagulation parameters, such as neutrophil to lymphocyte ratio, platelet count, D-dimer, and prothrombin time might provide a reliable and convenient method for classifying and predicting the severity and outcomes of patients with COVID-19. The SIC scoring system might be a useful tool for physicians to assess and manage critically ill patients.
Acknowledgments
Acknowledgments
This work is supported by the National Key Research and Development Program of China (nos 2020YFC0845700 and 2019YFC1316200).
Contributors
YH and HM designed the study. DL and FZ collected the data. DL, ZW, PY, FZ, and HM analysed the data. HM, DL, FZ, LL, and MX drafted the manuscript. YH, HW, JX, YG, LC, PY, ZW, YW, LT, and JD critically revised the manuscript. All authors gave final approval for the version to be published.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.Huang C, Wang Y, Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen N, Zhou M, Dong X. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan WJ, Ni ZY, Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Health Commission & National Administration of Traditional Chinese Medicine Diagnosis and treatment protocol for novel coronavirus pneumonia (trial version 7) Chin Med J. 2020;133:1087–1095. doi: 10.1097/CM9.0000000000000819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou F, Yu T, Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Llitjos JF, Leclerc M, Chochois C. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. 2020 doi: 10.1111/jth.14869. https://doi.org.10.1111/jth.14869 published online April 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.KlOK FA, Kruip MJHA, van der Meer NJM. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang L, Feng X, Zhang D. Deep vein thrombosis in hospitalized patients with coronavirus disease 2019 (COVID-19) in Wuhan. China: prevalence, risk factors, and outcome. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.046702. https://doi.org.10.1161/CIRCULATIONAHA.120.046702 published online May 18. [DOI] [PubMed] [Google Scholar]
- 10.Helms J, Tacquard C, Severac F. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lodigiani C, Iapichino G, Carenzo L. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18:1421–1424. doi: 10.1111/jth.14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang L, Yan X, Fan Q. D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19. J Thromb Haemost. 2020;18:1324–1329. doi: 10.1111/jth.14859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fogarty H, Townsend L, Ni Cheallaigh C. COVID19 coagulopathy in Caucasian patients. Br J Haematol. 2020;189:1044–1049. doi: 10.1111/bjh.16749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ranieri VM, Rubenfeld GD, Thompson BT. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 16.Singer M, Deutschman CS, Seymour CW. The third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zacharski LR, Engman CA. Coagulopathy. In: Schwab M, editor. Encyclopedia of Cancer. Springer; Berlin, Heidelberg: 2009. pp. 715–717. Berlin Heidelberg. [Google Scholar]
- 18.Iba T, Levy JH, Warkentin TE, Thachil J, van der Poll T, Levi M. Diagnosis and management of sepsis-induced coagulopathy and disseminated intravascular coagulation. J Thromb Haemost. 2019;17:1989–1994. doi: 10.1111/jth.14578. [DOI] [PubMed] [Google Scholar]
- 19.Iba T, Arakawa M, Di Nisio M. Newly proposed sepsis-induced coagulopathy precedes international society on thrombosis and haemostasis overt-disseminated intravascular coagulation and predicts high mortality. J Intensive Care Med. 2020;35:643–649. doi: 10.1177/0885066618773679. [DOI] [PubMed] [Google Scholar]
- 20.Bassetti M, Vena A, Giacobbe DR. The novel Chinese coronavirus (2019-nCoV) infections: challenges for fighting the storm. Eur J Clin Invest. 2020;50 doi: 10.1111/eci.13209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amgalan A, Othman M. Exploring possible mechanisms for COVID-19 induced thrombocytopenia: unanswered questions. J Thromb Haemost. 2020;18:1514–1516. doi: 10.1111/jth.14832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mahallawi WH, Khabour OF, Zhang Q, Makhdoum HM, Suliman BA. MERS-CoV infection in humans is associated with a pro-inflammatory Th1 and Th17 cytokine profile. Cytokine. 2018;104:8–13. doi: 10.1016/j.cyto.2018.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen G, Wu D, Guo W. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130:2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van der Poll T, van de Veerdonk FL, Scicluna BP, Netea MG. The immunopathology of sepsis and potential therapeutic targets. Nat Rev Immunol. 2017;17:407–420. doi: 10.1038/nri.2017.36. [DOI] [PubMed] [Google Scholar]
- 25.Zhou Y, Fu B, Zheng X. Pathogenic T-cells and inflammatory monocytes incite inflammatory storm in severe COVID-19 patients. Natl Sci Rev. 2020 doi: 10.1093/nsr/nwaa041. https://doi.org.10.1093/nsr/nwaa041 published online March 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spiezia L, Boscolo A, Poletto F. COVID-19-related severe hypercoagulability in patients admitted to intensive care unit for acute respiratory failure. Thromb Haemost. 2020;120:998–1000. doi: 10.1055/s-0040-1710018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Umemura Y, Yamakawa K, Hayakawa M, Hamasaki T, Fujimi S. Screening itself for disseminated intravascular coagulation may reduce mortality in sepsis: a nationwide multicenter registry in Japan. Thromb Res. 2018;161:60–66. doi: 10.1016/j.thromres.2017.11.023. [DOI] [PubMed] [Google Scholar]
- 28.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grimmer B, Kuebler WM. The endothelium in hypoxic pulmonary vasoconstriction. J Appl Physiol. 2017;123:1635–1646. doi: 10.1152/japplphysiol.00120.2017. [DOI] [PubMed] [Google Scholar]
- 30.Wu YP, Wei R, Liu ZH. Analysis of thrombotic factors in severe acute respiratory syndrome (SARS) patients. Thromb Haemost. 2006;96:100–101. doi: 10.1160/TH05-12-0827. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.