The COVID-19 pandemic has had a major impact on health care globally. More than 10·1 million cases of COVID-19 have been reported worldwide, with more than 502 000 deaths. The severity of COVID-19 varies considerably from asymptomatic to life threatening. In severe cases, the host response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) leads to sepsis or septic shock as defined by the international consensus definitions for sepsis and septic shock (sepsis-3), including life-threatening organ dysfunction.1 SARS-CoV-2 appears to enter host cells in the respiratory tract through the angiotensin-converting enzyme 2 receptor.2 In COVID-19-induced sepsis or septic shock, the respiratory manifestations such as severe dyspnoea and hypoxaemia are particularly obvious and pertinent and are also the basis for the grading of mild, moderate, severe, and critical COVID-19 infection, as suggested by the diagnosis and treatment protocol for novel coronavirus pneumonia published by National Health Commission in China.3 Further, COVID-19 infection is associated with coagulopathy of varying degrees, similar to the changes observed in sepsis induced coagulopathy (SIC) or disseminated intravascular coagulopathy (DIC).
The initial coagulopathy of COVID-19 has been characterised as increased D-dimer and fibrinogen or fibrin degradation products, but also abnormalities of prothrombin time, acute partial thromboplastin time, and platelet counts. Furthermore, severe COVID-19 infection might also lead to a cytokine storm similar to the cytokine profile present in secondary haemophagocytic lymphohistiocytosis, including increased ferritin level, IL-1, IL-2, IL-6, IL-7, granulocyte-colony stimulating factor, interferon-γ inducible protein 10, monocyte chemoattractant protein 1, macrophage inflammatory protein 1-α, and tumour necrosis factor-α.4, 5
In The Lancet Haematology, Danying Liao and colleagues6 present a retrospective observational cohort study, in which the coagulation profiles of 380 patients with COVID-19 admitted to hospital in Wuhan, China, are described (median age 64 years [53–73]; 174 [46%] women). The patients were classified as having moderate, severe, or critical COVID-19; notably, the severity of coagulopathy was associated with the severity of COVID-19. Thrombocytopenia, defined as platelet count less than 100 × 109 cells per L (odds ratio 8·33 [95% CI 2·56–27·15]), neutrophil to lymphocyte ratio of 9·13 or greater (5·39 [1·70–17·13]), prothrombin time longer than 16 s (4·94 [1·50–16·25]), and D-dimer more than 2 mg/L (4·41 [1·06–18·30]) were independently associated with increased mortality in a linear mixed model comparing survivors and non-survivors. The authors conclude that these routine coagulation tests can be used to help clinicians assess severity and prognosis of patients with COVID-19. The study is a valuable contribution to the knowledge of the coagulation profile of patients with COVID-19 and highlights the established role of routine coagulation tests as predictive variables for mortality and morbidity. However, the question of whether the observed changes in routine coagulation tests are just markers of the severity of illness or whether they show a significant and specific pathophysiology that drives morbidity and mortality in itself is still unanswered. Evidence exists to suggest that the observed coagulopaty is associated with an endotheliopathy that causes a thrombotic microangiopathy and microcirculatory impairment.7 This association is an interesting and plausible explanation for the observed post-mortem findings of microvascular platelet-rich thrombotic depositions in small vessels of the lungs and other organs of patients with COVID-19.8 SARS-CoV-2 uses the angiotensin-converting enzyme 2 receptor on endothelial cells for intracellular access to cells in the respiratory tract, with viral replication causing inflammation, endothelial cell apoptosis, and microvascular thrombosis. This pathophysiological course of events is consistent with the finding of microcirculatory clot formation and endothelial apoptosis in the post-mortems of patients with COVID-19,9 and it is a plausible explanation of sudden cerebrovascular complications, myocardial ischaemia, and the increasing reports of both microcirculatory and macrocirculatory thromboembolic complications in these patients.
Although the features of COVID-19-associated coagulopathy have been considered unique, with very high levels of D-dimer and only moderately decreased platelet counts, the similarities with SIC and DIC are clear. However, in patients with critical COVID-19 infection and a cytokine storm, an extreme hypercoagulable state rarely seen in regular DIC has been observed. The reason for this life-threatening condition is not known but might be driven by an uncontrolled hyperinflammatory response to a novel pathogen without previous immunity.7
Regardless, understanding of the effects of this new pathogen is improving, and the guidelines for optimisation of patient management, including thrombosis prophylaxis, are developing. Pending the results of several randomised controlled trials (NCT04345848, NCT04366960, NCT04367831 and NCT04372589), the opinion of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis on thrombosis prophylaxis is that “a change of anticoagulant regimen from prophylactic low molecular weight heparin or intermediate-dose to treatment-dose regimen can be considered in patients without established venous thromboembolism, but deteriorating pulmonary status or acute respiratory distress syndrome”.10
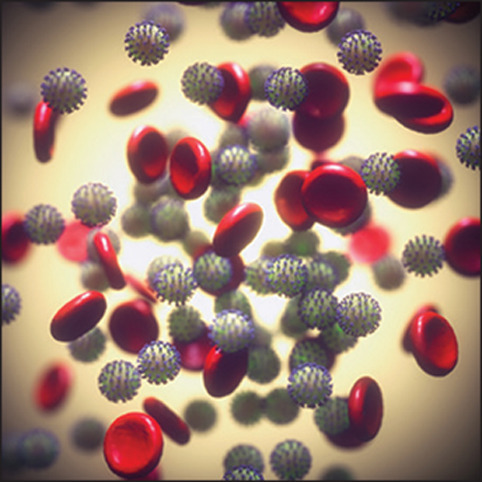
© 2020 KTSDESIGN/Science Photo Library
Acknowledgments
I declare no competing interests.
References
- 1.Singer M, Deutschman CS, Seymour CW. The third international consensus definitions for sepsis and septic shock (sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu R, Zhao X, Li J. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Health Commission & National Administration of Traditional Chinese Medicine Diagnosis and treatment protocol for novel coronavirus pneumonia (trial version 7) Chin Med J. 2020;133:1087–1095. doi: 10.1097/CM9.0000000000000819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta P, McAuley DF, Brown M. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang C, Wang Y, Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liao D, Zhou F, Luo L. Haematological characteristics and risk factors in the classification and prognosis evaluation of COVID-19: a retrospective cohort study. Lancet Haematol. 2020 doi: 10.1016/S2352-3026(20)30217-9. published online July 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135:2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levi M, Thachil J, Iba T, Levy JH. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020;7:e438–e440. doi: 10.1016/S2352-3026(20)30145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Varga Z, Flammer AJ, Steiger P. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spyropoulos AC, Levy JH, Ageno W. Scientific and Standardization Committee communication: clinical guidance on the diagnosis, prevention and treatment of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020 doi: 10.1111/jth.14929. https://doi.org.10.1111/jth.14929 published online May 27. [DOI] [PMC free article] [PubMed] [Google Scholar]


