Abstract
Background
The COVID-19 pandemic had a huge impact on national and regional health systems. The impact of SARS-CoV-2 on the quality of care for patients with liver disease is still unknown.
Aims
The Italian Association for the Study of the Liver (AISF) conducted a survey to assess the impact of SARS-CoV-2 on hepatology units activities in Italy.
Methods
A prospective web-based survey was proposed to all AISF active members. The survey was available online from April 8 2020, to May 3 2020, (lockdown phase in Italy).
Results
194 AISF members answered the questionnaire, most of whom were specialists in Gastroenterology (41%) or Internal Medicine (28%), and worked in Northern Italy (51%). 26% of hepatology wards had been converted into COVID-19 wards, and 33% had bed reductions. All hepatological activities, including the management of patients with decompensated liver disease, liver transplant and HCC had been significantly reduced/stopped. The number of physicians answering that their practices had not been modified ranged between 0.6% (for chronic hepatitis) to 47% (for the execution of paracentesis). The recorded answers were consistent among different regions, and did not show any north-south gradient
Conclusion
COVID-19 outbreak significantly impacted on hepatological clinical activity. This survey can serve as a basis to compare the impact of future measures aimed at delivering an acceptable level of liver care during a national pandemic or crisis.
Keywords: Hepatology, Covid-19, SARS COV-2
1. Introduction
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection, and its clinical manifestations (coronavirus disease 2019, COVID-19) was declared a pandemic by the World Health Organization (WHO) on March 11th 2020 [1]. SARS-CoV-2 has infected millions of people worldwide, causing more than 400.000 deaths. SARS-CoV-2 pandemic has reshaped the clinical activity in hospitals all over the world with a huge impact on national and regional health systems, requiring increased capacity in the Intensive Care Units as well as dedicated COVID-19 wards [2,3]. Health care professionals have been reallocated to manage COVID-19 patients, thus modifying the care for those with other chronic diseases. The enforcement of lock-down rules and the perceived risk of in hospital SARS-CoV-2 spread has further reduced the number of patients presenting to the ER and the number of outpatients appointment [4]. A recent study from Italy reported that the mortality from acute heart attacks almost tripled during the COVID-19 outbreak because of late referral [5]. The impact of SARS-CoV-2 on the quality of care for patients with liver disease is still unknown. However, given that hepatologists (internal medicine, gastroenterologists or infectious disease specialists) were likely to be involved in the management of COVID-19 wards and that most recommendations advised to postpone non-urgent outpatient reviews and investigations, it is important to understand how clinical care for patients with chronic liver diseases was affected [6,7]. For this reason, the Italian Association for the Study of the Liver (AISF), which represents Italian hepatologists of varying backgrounds, conducted a survey to assess the impact of SARS-CoV-2 on hepatology units in Italy.
2. Materials and methods
The study was performed by means of a web-based survey proposed to all AISF active members (n = 668). A questionnaire made of 30 multiple-choice questions, some allowing for multiple answers, was designed by the AISF governing board (supplementary material). The questionnaire was proposed to all AISF members via a weblink sent by email, which could only be accessed/answered once through an interactive web-based platform; completion could be stopped and resumed on each question. The survey was available online from April 8 2020, to May 3 2020, (lockdown phase in Italy). On May 4, all answers were collected and analyzed using IBM SPSS Statistics for Macintosh, Version 26.0 (IBM Corp. Armonk, NY). The survey was aimed at addressing the impact of the COVID-19 emergency on the most relevant activities carried out for purposes of diagnosis, follow-up and treatment of patients with chronic liver disease. The impact was measured by assessing the quantitative and qualitative changes of such activities during the lock-down period, compared to pre-pandemic routines. Information on the professional position/qualification of the responders was also collected.
3. Results
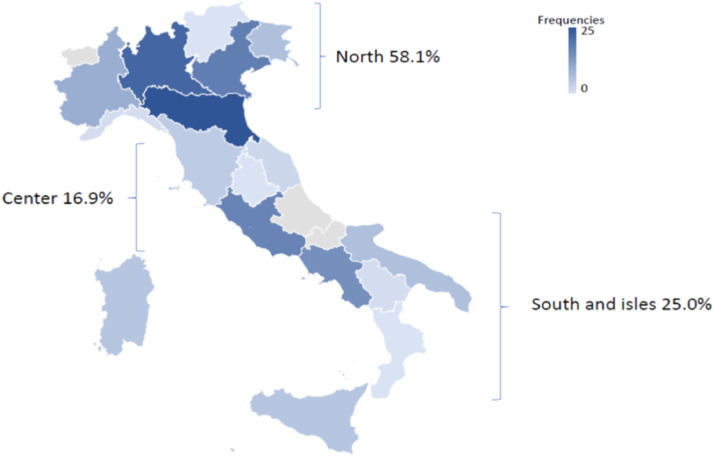
Overall, 194 AISF members answered the questionnaire, most of whom were specialists in Gastroenterology (41%) or Internal Medicine (28%), and worked in Northern Italy (51%) (Fig. 1 ).
Fig. 1.
Geographic distribution of the Survey Participants.
The questionnaire was structured into two specific sections, evaluating 1) how the COVID-19 pandemic changed the organization of the hepatology Units and 2) how the specific management of liver diseases was affected.
3.1. Impact of COVID-19 on the activity of the Hepatology units
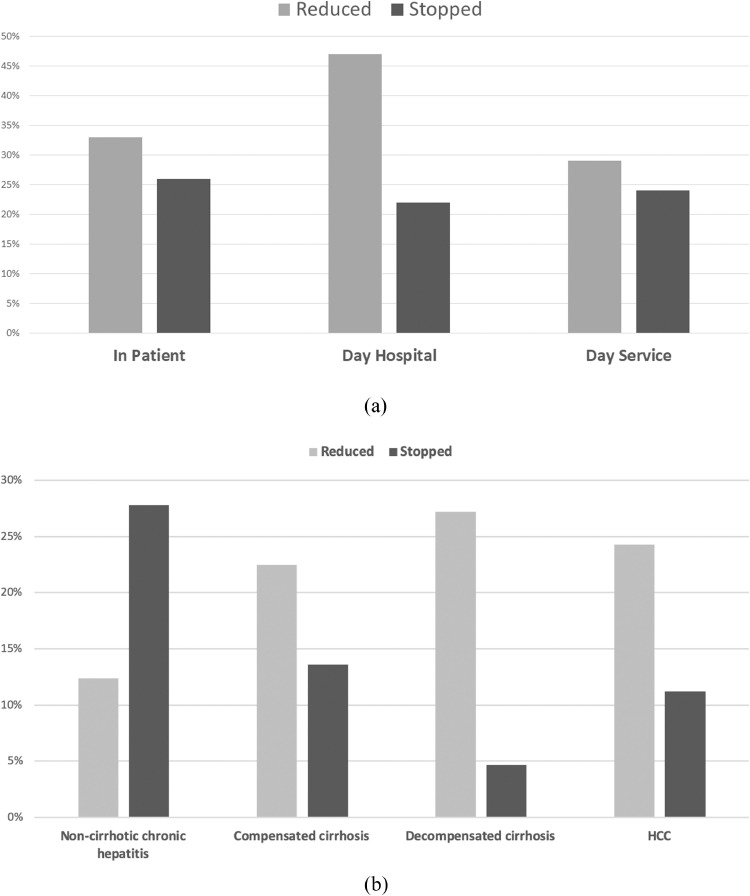
Only 20% of responders reported no relevant change in the activity of hepatology wards. Interestingly, in over a quarter of cases (26%) the wards of the responders had been converted into COVID-19 wards, while in a third (33%) the number of beds had been reduced, as a consequence of the need to manage the huge number of hospitalized COVID-19 patients (Fig. 2 A). Similarly, a reduction or even a complete interruption of day hospital (47% and 22%) and/or day service (29% and 24%) activity had occurred (Fig. 2A).
Fig. 2.
(A) Variations in the activity of hepatology in patients units, day services and day hospitals. (B) Variations in outpatient activities according to the severity of liver disease.
When analysing outpatient activity, the magnitude of the reduction in the number of daily reviews was directly linked to the severity of the underlying liver disease. Indeed, no change in the outpatient activity was reported in 0.6% for chronic hepatitis and compensated cirrhosis, 18% for hepatocellular carcinoma (HCC), and 32% for decompensated cirrhosis (Fig. 2B).
A switch to remote (e-mail or phone) contact had occurred in 40% of cases for chronic hepatitis, 44% for compensated cirrhosis, 25% for HCC, and 17% for decompensated cirrhosis.
3.2. Impact of COVID-19 on the management of liver diseases
3.2.1. Viral hepatitis
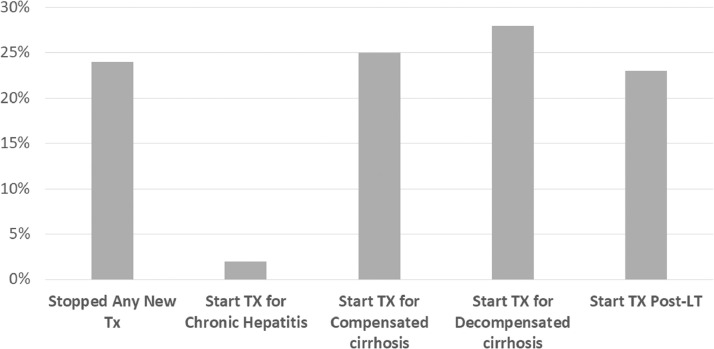
Overall, initiation of hepatitis B (HBV) or C (HCV) antiviral treatment was postponed in 23% of the centres. Even in patients considered at high risk of rapid clinical deterioration (e.g. those with extra-hepatic hepatitis C manifestations, those with compensated or decompensated cirrhosis) treatment had been started in only 20–28% of cases (Fig. 3 ).
Fig. 3.
Policy for starting antiviral treatments for viral hepatitis.
3.2.2. Cirrhosis
Management of cirrhosis and its complications was also severely affected, with screening for oesophageal varices being reduced or suspended in 46% and 20% of the centres, respectively. Endoscopic band-ligation for primary or secondary prophylaxis of variceal hemorrage had been reduced in 33% of the centres and suspended in 12%. Therapeutic paracenteses had been reduced in 7% of centres and switched from day hospital to inpatient procedures in 18% of the cases.
3.2.3. Liver cancer
As for the management of HCC, in almost half (45%) of the centres, surveillance and follow-up were limited. Both surgical and nonsurgical loco-regional treatment procedures had been reduced (44% and 34%, respectively) or suspended (44% and 8%, respectively). Similar figures were observed when analysing medical treatment for HCC, with 27% of responders reporting reductions in the number of patients starting treatment, 4% stopping the initiation systemic therapies and 34% reporting no major change in their activity.
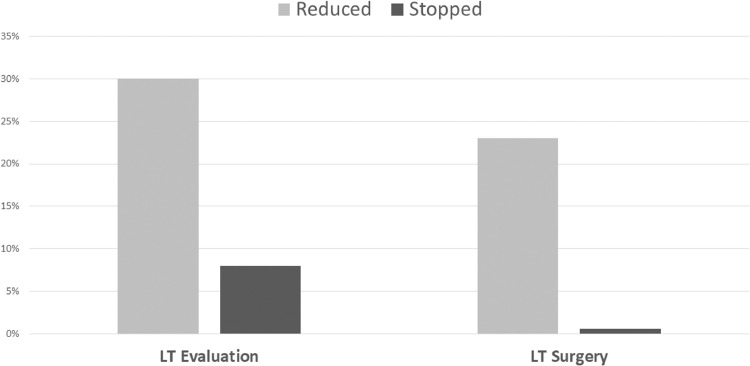
3.2.4. Liver transplant
COVID-19 also heavily affected the activity of liver transplant centres: 30% reported a reduction in the number of pre-transplant assessments, while in 44% of cases post-transplant reviews were postponed (Fig. 4 ). Interestingly, although less than 1% of responders reported a temporary interruption of transplant activity, in 23% of cases a reduction in the number of performed liver transplants was reported (Fig. 4).
Fig. 4.
Management of Liver transplantation.
4. Discussion
The COVID-19 pandemic has taken a heavy toll on worldwide mortality, with nearly 400.000 patients dying of COVID-19 related complications. These figures do not include the number of deaths caused by other diseases at the time of massive and urgent reorganization of a health system which was overwhelmed by the pandemic. While several articles have shown that cardiac diseases and elective and non-elective surgery have been dramatically impacted by COVID-19 [8,9], our survey shows that management of liver diseases in Italy has been severely impacted by the COVID-19 too. Indeed, the number of physicians answering that their practice had not been modified ranged between 0.6% (for chronic hepatitis) to 47% (for the execution of paracentesis). This highlights that most centers reorganized their clinical activity to maintain, where possible, the procedures or evaluations which were considered urgent. Still, when looking at the management of patients with decompensated liver disease, liver transplant or HCC, the number of physicians who reported that they had to halt their clinical activity was 4.7%, 0.6% and 11%, respectively. Interestingly, although the incidence of COVID-19 was higher in Northern Italy, the recorded answers did not differ significantly between regions, suggesting that hepatological activity had been modified regardless of the local prevalence of COVID-19 (supplementary figures).
While our survey cannot determine the exact reasons for reduced output of hepatology units in Italy, we can hypothesize that several causes might have played a role. Firstly, hepatologists were involved in the management of COVID-19 patients due to their solid internal medicine background. Secondly, hepatology wards often admit patients with other medical conditions and could have been reconverted to COVID-19 wards more rapidly. Lastly, most liver diseases are chronic and relatively benign and slow in their evolution (viral hepatitis, non-alcoholic fatty liver disease) over short periods of time. While the last point is certainly true, our survey surprisingly showed that even high risk complications such as HCC and ascites, or the prevention of gastrointestinal bleeding, suffered a steep reduction in monitoring/management during COVID-19 pandemic. While we cannot quantify the clinical impact of the reduced level of care that was offered to patients with liver disease in Italy over the past 3–4 months, an increase in liver related mortality is probably to be expected [10]. Similarly, we cannot exactly evaluate the consequences of the pandemic on the national hepatitis elimination program, but it is reasonable to assume that the reduction in treated patients with HCV (1000 between February and May 2020) as compared to the 12,000 who received treatment during the same period in 2019 is likely to impinge on the 2030 hepatitis elimination goal. Indeed, modeling studies indicate that 41,000 patients need to be treated annually in Italy to achieve HCV elimination [11]. Our results underline the need to introduce specific measures to guarantee a consistent access to care for patients with chronic liver diseases in case of a second wave of COVID-19 cases or a different, future pandemic. These should include dedicated hospitals/wards, day hospitals and teams of health care professionals. For outpatients, the implementation of telemedicine to manage benign/stable conditions as well as a stronger liaison with general practitioners would probably avoid unnecessary admittance to hospitals whilst guaranteeing an acceptable level of care.
We think our survey should thus be seen as a tool to re-discuss the organization of hepatological activities and to proactively reshape them in case of another national emergency, whilst also providing the basis to compare the impact of future measures aimed at delivering an acceptable level of care in hepatology centers during a national pandemic.
Declaration of Competing Interest
All Authors report no relevant conflicts of interests
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.dld.2020.07.008.
Appendix. Supplementary materials
References
- 1.WHOTimeline - COVID-19 [Internet]. [cited2020 May 20]. Available from:https://www.who.int/news-room/detail/27-04-2020-who-timeline-covid-19)
- 2.Fagiuoli S., Lorini F.L. Remuzzi G; Covid-19 Bergamo Hospital Crisis UnitAdaptations and Lessons in the Province of Bergamo. N Engl J Med. 2020 May 21;382(21):e71. doi: 10.1056/NEJMc2011599. Epub 2020 May 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grasselli G., Pesenti A., Cecconi M. Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: early Experience and Forecast During an Emergency Response. JAMA. 2020 Mar 13 doi: 10.1001/jama.2020.4031. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 4.Viganò M., Voza A., Harari S., Eusebio A., Ripoll Pons M., Bordonali M., Preti V., Rumi M.G., Badalamenti S., Aghemo A. Clinical Management of Nonrespiratory Diseases in the COVID-19 Pandemic: what Have We Done and What Needs to Be Done? Telemed J E Health. 2020 May 19 doi: 10.1089/tmj.2020.0148. [DOI] [PubMed] [Google Scholar]
- 5.Cosentino N., Assanelli E., Merlino L. An in-hospital pathway for acute coronary syndrome patients during the COVID-19 outbreak: initial experience under real-world suboptimal conditions. Canadian J Cardiol. 2020 Apr 17 doi: 10.1016/j.cjca.2020.04.011. in presshttps://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boettler T., Newsome P.N., Mondelli M.U., Maticic M., Cordero E., Cornberg M. Berg Care of patients with liver disease during the COVID-19 pandemic: EASL-ESCMID position paper. JHEP Rep. Jun 2020;2(3) doi: 10.1016/j.jhepr.2020.100113. Epub 2020 Apr 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sun J., Aghemo A., Forner A., Valenti L. COVID-19 and liver disease. Liver Int. 2020 Apr 6 doi: 10.1111/liv.14470. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 8.Torzilli G., Vigano L., Galvanin J., Castoro C., Quagliuolo V., Spinelli A., Zerbi A., Donadon M., Montorsi M. COVID-SURGE-ITA group.a snapshot of elective oncological surgery in Italy during COVID-19 emergency: pearls, pitfalls, and perspectives. Ann Surg. 2020 May 21 doi: 10.1097/SLA.0000000000004081. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Filippo O., D'Ascenzo F., Angelini F., Bocchino P.P., Conrotto F., Saglietto A. Reduced Rate of Hospital Admissions for ACS During Covid-19 Outbreak in Northern Italy. N Engl J Med. 2020 Apr 28 doi: 10.1056/NEJMc2009166. NEJMc2009166Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kondili L.A., Marcellusi A., Ryder S. Craxì AWill the COVID-19 pandemic affect HCV disease burden? Dig Liver Dis. 2020 May 29 doi: 10.1016/j.dld.2020.05.040. S1590-8658(20)30245-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Razavi H., Sanchez Gonzalez Y., Yuen C., Cornberg M. Global timing of hepatitis C virus elimination in high-income countries. Liver Int. Mar 2020;40(3):522–529. doi: 10.1111/liv.14324. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.