Abstract
Introduction
Exposure to disaster-related media may be a risk factor for mental distress, but this has not been examined in the context of the COVID-19 pandemic. This study assesses whether exposure to social and traditional media during the rise of the COVID-19 pandemic was associated with mental distress among U.S. adults.
Methods
Data came from the Understanding America Study, conducted with a cross-sectional, nationally representative sample of adults who completed surveys online. Participants included 6,329 adults surveyed between March 10 and March 31, 2020. Regression analyses examined the associations of (1) self-reported average time spent on social media in a day (hours) and (2) number of traditional media sources (radio, TV, and newspaper) consulted to learn about COVID-19 with self-reported mental distress (4-item Patient Health Questionnaire). Data were analyzed in April 2020.
Results
Participants responding at later survey dates reported more time spent on social media (β=0.02, 95% CI=0.01, 0.03), a greater number of traditional media sources consulted to learn about COVID-19 (β=0.01, 95% CI=0.01, 0.02), and greater mental distress (β=0.07, 95% CI=0.04, 0.09). Increased time spent on social media and consulting a greater number of traditional media sources to learn about COVID-19 were independently associated with increased mental distress, even after adjusting for potential confounders (social media: β=0.14, 95% CI=0.05, 0.23; traditional media: β=0.14, 95% CI=0.08, 0.20).
Conclusions
Exposure to a greater number of traditional media sources and more hours on social media was modestly associated with mental distress during the rise of the COVID-19 pandemic in the U.S.
INTRODUCTION
The rise of the coronavirus disease 2019 (COVID-19) pandemic has caused unprecedented changes to daily life in the U.S. Social distancing measures, including shelter-in-place or stay at home orders, are resulting in isolation from social contacts outside the home. In addition, the pandemic has had a severe impact on the economy, and unemployment rates are skyrocketing.1 In addition, fears about the risk for infection (both for oneself and for family and friends), financial hardship, and increased social isolation have tremendous potential to negatively impact mental health.2, 3, 4
On top of these stressors, mental health can also be affected by the enormous amounts of media coverage of the pandemic. During times of crisis, the public experiences an immediate and urgent need for information about health risks and personal safety.5 Individuals may be motivated to reduce confusion, develop a better understanding of the potential health threat, and act to reduce their level of risk by seeking information from the media.6 , 7 However, in the context of the current pandemic, some researchers have cautioned that pervasive media coverage of the COVID-19 pandemic may unnecessarily increase perceptions of fear and uncertainty.8
Numerous studies have investigated the association between media exposure and mental health in the context of public health crises.9, 10, 11, 12, 13 There is evidence that panic-inducing and sensationalized communication strategies on social media contributed to levels of anxiety in the U.S. during the 2003 severe acute respiratory syndrome outbreak and the 2014 Ebola crisis.5 , 14, 15, 16, 17 Self-reported time spent watching TV on the day of the September 11 attacks and the days after the attack were associated with symptoms of post-traumatic stress disorder in a nationally representative sample of U.S. adults.18 Mental distress has been conceptualized as a constellation of psychological symptoms, including anxiety, loneliness, hopelessness, and depression.19 Although mental distress can be considered a normal response to stressors, even mild symptoms can impair daily functioning.20 How exposure to media may be related to mental distress during a global pandemic, such as COVID-19, should be investigated to inform public health recommendations.
A recent survey from China reported that social media exposure to COVID-19‒related information was associated with depression and anxiety.21 A limitation of that study, however, was the use of a nonprobability sample. The unknown selection biases, coupled with a lack of information about the respondents’ mental health before the pandemic, limit the generalizability and certainty of findings. The objective of this analysis is to determine whether exposure to social and traditional (radio, TV, and newspaper) media during the rise of the COVID-19 pandemic was associated with mental distress among U.S. adults. Given the evidence that exposure to social and traditional media may have differential associations with mental distress,14 , 22 these sources are examined separately. In addition, because depressive symptoms have been associated with greater social media use,23 , 24 this study tests whether associations were moderated by prior depressive symptoms. Data are from the Understanding America Study (UAS) that were collected between March 10 and March 31, 2020. This period coincided with a number of key events in the rise of the COVID-19 pandemic, including the declaration of COVID-19 as a pandemic by the WHO, declaration of a national emergency by the president of the U.S., school and work closures, and implementation of social distancing directives in many U.S. states.25
METHODS
Study Sample
Participants were drawn from the UAS, a probability-based Internet panel of adults (aged ≥18 years) representing the U.S. This study used data from the UAS230 survey (March 2020 monthly survey), which was fielded between March 10, 2020, and March 31, 2020. Addresses used to sample participants came from the U.S. Postal Service Delivery Sequence file, prepared by the Marketing Systems Group to form a sampling frame of all household addresses in the U.S. After the initial mail-out recruitment, participants were surveyed through computer, mobile device, or tablet; Internet-connected tablets were provided to households that were not already online. Respondents were compensated with $20 for 30 minutes of survey time. Across the various UAS panels, the recruitment rate is about 14%. Additional details regarding the methodology of the UAS can be found at the UAS website (https://UASdata.usc.edu).
Of the 8,493 panel members eligible for the UAS230 survey, 1,561 (18.4%) did not start the survey (response rate of 81.6%). Of the remaining 6,932 participants, 48 (0.7%) started but did not complete the survey. The analytic sample comprised 6,329 participants (91.9%) who provided complete data on the variables of interest.
Measures
The outcome of interest was mental distress, measured with the 4-item Patient Health Questionnaire (PHQ-4).26 Participants were asked, in 4 prompts, for the frequency over the past 2 weeks with which they had been bothered by (1) feeling nervous, anxious, or on edge, (2) not being able to stop or control worrying, (3) feeling down, depressed, or hopeless, and (4) having little interest or pleasure in doing things. The response options were not at all (0), several days (1), more than half the days (2), and nearly every day (3). Total scores were generated by summing scores across the 4 items (range=0−12). The PHQ-4 has previously been validated and was found to be reliable in the general population.27
For social media exposure, participants were asked: How many minutes do you spend on social media in a day on average? A small proportion (0.5%) of participants reported implausible values for this question (i.e., <0 minutes or >480 minutes [8 hours] of social media use per day) and were excluded from analyses. Traditional media exposure was measured using responses to the question: Which of the following information sources have you used to learn about the coronavirus in the past 7 days? A total of 5 sources were considered traditional media sources: public TV or radio, national news sources (Fox News, CNN, MSNBC, NBC News, CBS News, or ABC News), national newspapers (New York Times, Washington Post, and USA Today), local newspapers, or local TV news sources. The authors generated an index that reflected the number of traditional media sources consulted (range=0−5).
A variety of covariates were included to account for potential confounding. Sociodemographic characteristics included age (years), sex (female or male), race/ethnicity (White, American Indian or Alaska Native, Asian, Black or African American, Hawaiian or Pacific Islander, Hispanic or Latino, or multiracial), education (high school degree or below, attended some college or received a 2-year degree, bachelor's degree, or Graduate degree), marital status (married, never married, separated or divorced, or widowed), household income (<$20,000, $20,000–$39,999, $40,000–$59,999, $60,000–$99,999, or ≥$100,000), and job status (has a job or does not have a job). In earlier waves of data collection for the UAS panel (June 2019, June 2017, or May 2015), participants had completed the 8-item version of the Center for Epidemiologic Studies–Depression Scale (range=0−8); this was used as an indicator of prior depressive symptoms.28 Participants had also previously answered the prompt: Have you ever had or has a doctor ever told you that you have any emotional, nervous, or psychiatric problems? (yes or no). This study also included 2 indicators of the perceived risk of coronavirus; higher perceived risk may lead individuals to consume more media and also be related to increased mental distress. Participants were asked to report: The chance that you will get the coronavirus in the next three months and the percent chance you will run out of money because of the coronavirus in the next three months, each on a scale from 0 to 100. In preliminary analyses, both indicators were significantly associated with exposure to social media (being infected: β=0.004, 95% CI=0.001, 0.006; running out of money: β=0.003, 95% CI=0.001, 0.005) and the number of traditional media sources consulted to learn about COVID-19 (being infected: β=0.001, 95% CI=0.001, 0.002; running out of money: β=0.001, 95% CI=0.0004, 0.002), supporting the decision to include these indicators as covariates.
Statistical Analysis
First, this study examined how patterns of use of social and traditional media as well as levels of mental distress differed by survey response date by estimating 3 linear regression models, with each type of media use and mental distress as the dependent variables and a continuous variable for the survey date (March 10–March 31) as an independent variable.
Second, multiple linear regression was used to estimate associations between media exposure and mental distress. The authors first estimated an unadjusted model that included (1) average time spent on social media in a day and (2) the number of traditional media sources consulted to learn about COVID-19 as independent variables. They then estimated an adjusted model with both independent variables and covariates, in addition to a continuous variable for survey date. Finally, they estimated 2 adjusted models that included an interaction with prior depressive symptoms and each of the independent variables.
In addition to being scored continuously, the PHQ-4 can also be scored using categories that indicate distress severity (normal [0–2], mild [3–5], moderate [6–8], or severe [9–12]).26 To test the sensitivity of the findings to the modeling of PHQ-4 scores, both the unadjusted and adjusted models were re-estimated using categorical PHQ-4 scores as the outcome using ordinal logistic regression.29
All analyses incorporated survey weights, calculated in 2 stages: (1) base weights accounting for probabilities of sample selection and survey nonresponse and (2) poststratification weights that bring the distributions in line with Current Population Survey benchmarks. Statistical significance was assessed at p<0.05 level. All analyses were conducted using Stata, version 16. Analyses were conducted from April 1 to April 10, 2020.
RESULTS
The mean time spent on social media in a day was 55.8 minutes or 0.93 hours (95% CI=0.89, 0.97), and the mean number of traditional media sources consulted was 2.50 sources (95% CI=2.45, 2.56). The mean PHQ-4 score was 1.92 (95% CI=1.83, 2.02) (Table 1 ). Having and using a Facebook, Instagram, or Twitter account was reported by 4,323 (68.1%), 2,256 (32.7%), and 1,230 (19.4%) participants, respectively. With respect to traditional media sources, 3,516 (55.0%) reported consulting public TV and radio, 4,468 (69.3%) reported consulting national news sources, 1,981 (31.2%) reported consulting local newspapers, 2,159 (31.5%) reported consulting national newspapers, and 3,983 (63.6%) reported consulting local TV news sources. The mean perceived chance of being infected with coronavirus in the next 3 months was 21.27% (95% CI=20.49, 22.05), and the mean perceived chance of having no money because of coronavirus in the next 3 months was 15.80% (95% CI=14.88, 16.73).
Table 1.
Descriptive Statistics of Sample Characteristics for U.S. Adults in the UAS230 Panel, March 10‒March 31, 2020 (n=6,329)
| Variable | n (%) |
|---|---|
| Age, yearsa | 48.8 (0.29) |
| Sex | |
| Male | 2,643 (49.0) |
| Female | 3,686 (51.0) |
| Race/ethnicity | |
| White | 4,211 (64.2) |
| American Indian/Alaska Native | 59 (0.4) |
| Asian | 307 (5.1) |
| Black/African American | 474 (11.2) |
| Hawaiian/Pacific Islander | 20 (0.1) |
| Hispanic/Latinx | 1,000 (16.0) |
| Multiracial | 258 (3.0) |
| Marital status | |
| Married | 3,525 (56.5) |
| Never married | 1,498 (24.3) |
| Separated or divorced | 1,014 (14.9) |
| Widowed | 292 (4.3) |
| Education | |
| Less than high school | 1,386 (38.0) |
| Some college/2-year degree | 2,362 (27.8) |
| Bachelor's | 1,536 (19.4) |
| Graduate | 1,045 (14.7) |
| Household income, $ | |
| <20,000 | 938 (16.7) |
| 20,000–39,999 | 1,178 (19.9) |
| 40,000–59,999 | 1,021 (16.9) |
| 60,000–99,999 | 1,552 (23.4) |
| ≥100,000 | 1,640 (23.1) |
| Currently have job | |
| No | 2,392 (38.4) |
| Yes | 3,937 (61.6) |
| Average time spent on social media per day, hoursa | 0.93 (0.02) |
| Number of traditional media sources consulteda | 2.50 (0.03) |
| Prior CES-D scorea | 1.65 (0.04) |
| Current PHQ-4 scorea | 1.92 (0.05) |
| Any prior emotional, nervous, or psychiatric conditions | |
| No | 4,553 (73.0) |
| Yes | 1,776 (27.0) |
| Perceived chance of being infected with coronavirus in the next 3 monthsa | 21.27 (0.40) |
| Perceived chance of having no money owing to coronavirusin the next 3 monthsa | 15.80 (0.47) |
Note: All means and percentages are weighted.
Reported as mean (SE).
CES-D, Center for Epidemiologic Studies–Depression Scale; PHQ-4, 4-item Patient Health Questionnaire; UAS, Understanding America Study.
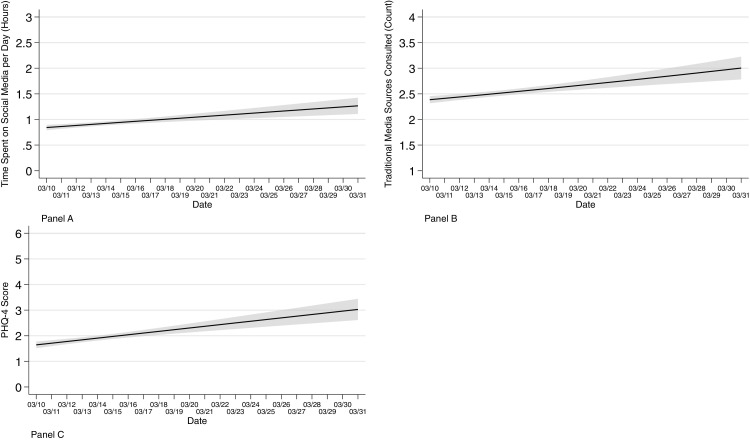
Exposure to forms of media (social media: β=0.02, 95% CI=0.01, 0.03; traditional media: β=0.03, 95% CI=0.02, 0.04) and mental distress (β=0.07, 95% CI=0.04, 0.09) were higher in participants who responded to the survey at later dates than in those responding sooner (Figure 1 ). Time spent on social media per day increased from a mean of 50.4 minutes or 0.84 hours (95% CI=0.79, 0.89) on the first day of the survey period to 76.2 minutes or 1.27 hours (95% CI=1.11, 1.42) on the last day of the survey period. The number of traditional media sources consulted increased from a mean of 2.38 sources (95% CI=2.31, 2.46) on the first day of the survey period to 3.00 sources (95% CI=2.78, 3.23) on the last day of the survey period. PHQ-4 scores increased from a mean of 1.64 (95% CI=1.51, 1.77) on the first day of the survey period to 3.03 (95% CI=2.61, 3.44) on the last day of the survey period.
Figure 1.
Linear predictions and 95% CIs for time spent on social media in a day (Panel A), the number of traditional media sources consulted to learn about COVID-19 (Panel B), and mental distress measured by the PHQ-4 (Panel C) by date of survey completion among U.S. adults in the UAS230 Panel, 2020 (n=6,329).
PHQ-4, 4-item Patient Health Questionnaire; UAS, Understanding America Study.
In unadjusted analyses, increased time spent on social media per day (β=0.34, 95% CI=0.24, 0.43) and consulting a greater number of traditional media sources to learn about COVID-19 (β=0.11, 95% CI=0.05, 0.18) were independently associated with increased mental distress (Table 2 ). These associations remained significant after adjusting for sociodemographic characteristics; prior depressive symptoms; any prior emotional, nervous, or psychiatric conditions; and perceived risk related to coronavirus (social media: β=0.14, 95% CI=0.05, 0.23; traditional media: β=0.14, 95% CI=0.08, 0.20). In other words, for both every 1-hour increase in time spent on social media and for every additional traditional media source consulted, there was a 0.14-point increase in mental distress. There was no significant interaction between either time spent on social media (p=0.699) or the number of traditional media sources consulted (p=0.945) and prior depressive symptoms, indicating that associations with mental distress did not vary by history of depressive symptoms. In the adjusted model, a later survey date; separated marital status; prior depressive symptoms; any prior emotional, nervous, or psychiatric conditions; perceived chance of being infected with coronavirus in the next 3 months; and perceived chance of having no money because of coronavirus in the next 3 months were associated with higher levels of mental distress. Older age, being an American Indian/Alaska Native, being Black/African American, and being a Hawaiian/Pacific Islander were associated with lower levels of mental distress.
Table 2.
Adjusted Associations Between Media Exposure and Mental Distress Among U.S. Adults in the UAS230 Panel, March 10–March 31, 2020 (n=6,329)
| Variable | Unadjusted | Adjusted |
|---|---|---|
| β (95% CI) | β (95% CI) | |
| Average time spent on social media per day, hours | 0.34 (0.24, 0.43) | 0.14 (0.05, 0.23) |
| Number of traditional media sources consulted | 0.11 (0.05, 0.18) | 0.14 (0.08, 0.20) |
| Days since March 10, 2020 | — | 0.03 (0.01, 0.05)⁎⁎ |
| Age, years | — | −0.01 (−0.02, −0.01)⁎⁎ |
| Sex | — | |
| Male | — | ref |
| Female | — | 0.12 (−0.06, 0.30) |
| Race/ethnicity | — | |
| White | — | ref |
| American Indian/Alaska Native | — | −1.44 (−2.17, −0.70)⁎⁎ |
| Asian | — | −0.31 (−0.69, 0.06) |
| Black/African American | — | −0.69 (−0.99, −0.38)⁎⁎ |
| Hawaiian/Pacific Islander | — | −1.35 (−2.33, −0.36)⁎⁎ |
| Hispanic/Latinx | — | −0.27 (−0.56, 0.02) |
| Multiracial | — | 0.05 (−0.52, 0.62) |
| Marital status | — | |
| Married | — | ref |
| Never married | — | 0.14 (−0.10, 0.38) |
| Separated or divorced | — | 0.27 (0.00, 0.53)* |
| Widowed | — | −0.10 (−0.44, 0.24) |
| Education | — | |
| Less than high school | — | ref |
| Some college/2-year degree | — | −0.09 (−0.31, 0.13) |
| Bachelor's | — | 0.17 (−0.06, 0.41) |
| Graduate | — | 0.13 (−0.12, 0.38) |
| Household income, $ | — | |
| <20,000 | — | ref |
| 20,000–39,999 | — | −0.15 (−0.49, 0.19) |
| 40,000–59,999 | — | −0.09 (−0.44, 0.26) |
| 60,000–99,999 | — | −0.26 (−0.58, 0.07) |
| ≥100,000 | — | −0.13 (−0.49, 0.22) |
| Currently have job | — | |
| No | — | ref |
| Yes | — | −0.21 (−0.43, 0.00) |
| Prior depressive symptoms | — | 0.42 (0.36, 0.47) |
| Any prior emotional, nervous, or psychiatric conditions | — | |
| No | — | ref |
| Yes | — | 0.81 (0.58, 1.04)⁎⁎ |
| Perceived chance of being infected with coronavirus in the next 3 months | — | 0.01 (0.01, 0.02)⁎⁎ |
| Perceived chance of having no money because of coronavirus in the next 3 months | — | 0.01 (0.01, 0.02)⁎⁎ |
Note: Boldface indicates statistical significance (*p<0.05, **p<0.01)
UAS, Understanding America Study.
In sensitivity analyses, on the basis of categorical PHQ-4 scores, 4,653 (71.2%) participants had no mental distress, 1,255 (17.6%) participants had mild mental distress, 458 participants (6.9%) had moderate mental distress, and 307 participants (4.4%) had severe mental distress. Results using categorical PHQ-4 scores as the outcome were similar to the results using continuous PHQ-4 scores (social media: OR=1.15, 95% CI=1.07, 1.24; traditional media: OR=1.17, 95% CI=1.11, 1.24), suggesting that the findings were not sensitive to PHQ-4‒modeling decisions (Appendix, available online, shows the results).
DISCUSSION
This study showed modest increases in social and traditional media exposure as well as mental distress among U.S. adults between March 10 and March 31, 2020—a time of critical societal change and acceleration of the COVID-19 pandemic. In addition, the analyses revealed that increased time spent on social media and the number of traditional media sources consulted to learn about coronavirus (TV, radio, and newspaper) were associated with levels of mental distress.
A global pandemic in the age of social media is unprecedented, which limits the ability to contextualize these findings. It is encouraging to note that most of the participants in this study reported either no or mild mental distress, indicating possible resilience, which has been commented on elsewhere.30 However, numerous previous studies suggest that heightened exposure to disaster-related media content may be associated with adverse stress reactions.9, 10, 11, 12, 13 , 16 The mechanisms underlying these associations may involve heightened perceptions of threat and altered hypothalamic–pituitary–adrenal axis functioning.9 Social learning theory also suggests that viewing the experiences of others through the media is involved in the acquisition of fear.31 In addition, the concept of relative risk appraisal posits that perceptions of risk are fundamentally shaped by affective judgments rather than rational decision making.32 This concept has been used to explain how sensationalized media content may lead to overestimations of perceived individual risk.32 In the context of the current pandemic, one study using data from adults in China demonstrated an association between social media exposure to COVID-19–related information and anxiety and depression.21 The results of the present study extend these findings by studying the exposure to both traditional and social media sources in a nationally representative sample of adults in the U.S. Moreover, this study was able to control for pre-existing depressive symptoms before the COVID-19 pandemic.
This study was cross-sectional and cannot be used to draw causal conclusions. However, previous longitudinal studies suggest that consumption of digital and social media can influence mental health symptomology.33, 34, 35, 36, 37 It may be tempting to suggest that individuals limit the scope of sources consulted or time spent consuming COVID-19–related media as a strategy to reduce mental distress; however, this must be carefully balanced with the need to maintain social connectedness through the media throughout periods of social distancing. In addition, public health authorities such as the WHO, the Centers for Disease Control and Prevention, and local and state governments continue to update recommendations related to maintaining personal safety and avoiding the spread of infection, which are primarily disseminated through the media. It is therefore infeasible and potentially harmful to recommend broad disengagement from the media at this time. In line with other available guidance,8 , 38 the authors instead recommend that the media be used for activities that could support mental health. Evidence suggests that positive social interactions on social media can support well-being23; therefore, individuals could engage with social support networks such as friends and family in lieu of in-person gatherings to foster social connectedness. In addition, information seeking regarding COVID-19 should be focused on public health authorities that offer up-to-date guidance in order to limit exposure to misinformation and sensationalized news headlines. Outside of the media, telehealth interventions for mental health also offer immense potential to support those with pre-existing and incident mental health conditions.39 , 40
Limitations
Some limitations of this study should be noted. First, the cross-sectional nature of the data limits the ability to study causal relationships. However, the authors were able to incorporate longitudinal data from prior waves of the UAS panel to adjust for prior mental health status, which increases confidence that the observed associations are not accounted for by pre-existing levels of mental distress. Second, the question about time spent on social media did not ask about exposure to COVID-19–related content; therefore, the authors did not have information about what type of content the individuals were exposed to on social media. Given the pervasiveness of media coverage of the COVID-19 pandemic, however, it is likely that those reporting more time on social media were also exposed to a greater extent to content related to COVID-19. Third, the timeframes referred to by the media exposure items were not specific to the date of the survey. The actual patterns of media use for a given survey date may, therefore, differ from those reported by respondents. Fourth, there may have been an overlap between social and traditional media (e.g., news reports viewed on Facebook) that these analyses were unable to account for. Fifth, this study measured mental distress with a short screening scale rather than a longer self-reported measure or diagnostic interview for mental disorders. Sixth, the UAS is a pre-existing survey that was not designed specifically to examine associations between media exposure and mental distress. Exposure to social and traditional media was assessed on different scales and reflected different constructs (i.e., number of media sources versus the amount of time exposed to media). Future studies with consistent, validated, and more detailed measures are needed to corroborate these findings. Finally, participants selected which date they completed the survey on. There may be differences in the participants who responded on earlier compared with those who reported on later survey dates, which may have biased the observed results.
Future studies may consider a variety of avenues. Previous studies have found a negative association between passive use of social media, characterized by observation and scrolling, and mental health.41 , 42 Studying the quality of social media use during the COVID-19 pandemic may allow for greater specificity of guidelines around responsible social media use. Previous studies have observed increased substance use after public health crises such as the September 11 attacks43; understanding associations between media exposure and substance use may inform prevention strategies. Finally, future studies should clarify specific aspects of media exposure associated with mental distress (e.g., perceptions of the individual delivering messages, conflicting messages from multiple sources, misinformation, confusion, sensationalized reports).44
CONCLUSIONS
Increased time spent on social media and consulting a greater number of traditional media sources to learn about COVID-19 were associated with mental distress among U.S. adults. Recommending that individuals give priority to media outlets that report information from public health authorities, such as the WHO and the Centers for Disease Control and Prevention, as well as engage in activities that emphasize social support may be an important prevention strategy.
ACKNOWLEDGMENTS
The project described in this paper relies on data from the survey(s) administered by the Understanding America Study, which is maintained by the Center for Economic and Social Research at the University of Southern California. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the University of Southern California or Understanding America Study. For any questions or more information about the Understanding America Study, contact Tania Gutsche, Project and Panel Manager, Center for Economic and Social Research, University of Southern California, at tgutsche@usc.edu.
The Understanding America Study is funded from several sources, including the Social Security Administration and the National Institute on Aging (5U01AG054580). The survey that collected the mental health and COVID-19–related data used in this paper was funded by the Center for Economic and Social Research at the University of Southern California. Work on this manuscript was in part supported by the National Institute of Child Health and Human Development (U54 HD079123). This work was also supported by a Rapid Response Research grant from the National Science Foundation (2028683). Dr. Veldhuis’ participation in this research was made possible through an NIH/National Institute on Alcohol Abuse and Alcoholism Ruth Kirschstein Postdoctoral Research Fellowship (F32AA025816). Ms. Riehm was supported by the National Institute of Mental Health Mental Health Services and Systems Training Program (5T32MH109436-03) and by a Doctoral Foreign Study Award from the Canadian Institutes of Health Research.
KER and JT conceptualized and designed the study, carried out data analyses, drafted the initial manuscript, and revised the manuscript. CH assisted with data analyses, drafting the initial manuscript, and reviewing the manuscript. DB, QJ, and AK designed and implemented the survey. LGK, DB, AK, QJ, CBV, RMJ, MDF, FK, and EAS assisted with interpreting results and reviewing the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
No financial disclosures were reported by the authors of this paper.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2020.06.008.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.Bureau of Labor Statistics, U.S. Department of Labor . Bureau of Labor Statistics, U.S. Department of Labor; Washington, DC: 2020. The employment situation—June 2020.https://www.bls.gov/news.release/pdf/empsit.pdf [Google Scholar]
- 2.Keeter S. People financially affected by COVID-19 outbreak are experiencing more psychological distress than others. Pew Research Center. March 30, 2020.https://www.pewresearch.org/fact-tank/2020/03/30/people-financially-affected-by-covid-19-outbreak-are-experiencing-more-psychological-distress-than-others/. Accessed June 28, 2020.
- 3.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. In press. Online April 13, 2020. 10.1056/NEJMp2008017. [DOI] [PubMed]
- 4.Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180(6):817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- 5.Fung IC-H, Tse ZTH, Cheung CN, Miu AS, Fu KW. Ebola and the social media. Lancet. 2014;384(9961):2207. doi: 10.1016/S0140-6736(14)62418-1. [DOI] [PubMed] [Google Scholar]
- 6.Thelwall M, Stuart D. RUOK? Blogging communication technologies during crises. J Comput Mediat Commun. 2007;12(2):523–548. doi: 10.1111/j.1083-6101.2007.00336.x. [DOI] [Google Scholar]
- 7.van der Meer TGLA, Jin Y. Seeking formula for misinformation treatment in public health crises: the effects of corrective information type and source. Health Commun. 2020;35(5):560–575. doi: 10.1080/10410236.2019.1573295. [DOI] [PubMed] [Google Scholar]
- 8.Garfin DR, Silver RC, Holman EA. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol. 2020;39(5):355–357. doi: 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lubens P, Holman EA. The unintended consequences of disaster-related media coverage. In: Raphael B, Fullerton CS, Weisaeth L, Ursano RJ, editors. Textbook of Disaster Psychiatry. 2nd ed. Cambridge University Press; Cambridge, UK: 2017. pp. 181–192. [DOI] [Google Scholar]
- 10.Lau JTF, Lau M, Kim JH, Tsui HY. Impacts of media coverage on the community stress level in Hong Kong after the tsunami on 26 December 2004. J Epidemiol Community Health. 2006;60(8):675–682. doi: 10.1136/jech.2005.041897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vasterman P, Yzermans CJ, Dirkzwager AJE. The role of the media and media hypes in the aftermath of disasters. Epidemiol Rev. 2005;27(1):107–114. doi: 10.1093/epirev/mxi002. [DOI] [PubMed] [Google Scholar]
- 12.Sugimoto A, Nomura S, Tsubokura M. The relationship between media consumption and health-related anxieties after the Fukushima Daiichi nuclear disaster. PLoS One. 2013;8(8):e65331. doi: 10.1371/journal.pone.0065331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pfefferbaum B, Newman E, Nelson SD, Nitiéma P, Pfefferbaum RL, Rahman A. Disaster media coverage and psychological outcomes: descriptive findings in the extant research. Curr Psychiatry Rep. 2014;16(9):464. doi: 10.1007/s11920-014-0464-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kilgo DK, Yoo J, Johnson TJ. Spreading Ebola panic: newspaper and social media coverage of the 2014 Ebola health crisis. Health Commun. 2019;34(8):811–817. doi: 10.1080/10410236.2018.1437524. [DOI] [PubMed] [Google Scholar]
- 15.Ihekweazu C. Ebola in prime time: a content analysis of sensationalism and efficacy information in U.S. nightly news coverage of the Ebola outbreaks. Health Commun. 2017;32(6):741–748. doi: 10.1080/10410236.2016.1172287. [DOI] [PubMed] [Google Scholar]
- 16.Thompson RR, Garfin DR, Holman EA, Silver RC. Distress, worry, and functioning following a global health crisis: a national study of Americans’ responses to Ebola. Clin Psychol Sci. 2017;5(3):513–521. doi: 10.1177/2167702617692030. [DOI] [Google Scholar]
- 17.Person B, Sy F, Holton K. Fear and stigma: the epidemic within the SARS outbreak. Emerg Infect Dis. 2004;10(2):358–363. doi: 10.3201/eid1002.030750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schlenger WE, Caddell JM, Ebert L. Psychological reactions to terrorist attacks: findings from the National Study of Americans’ Reactions to September 11. JAMA. 2002;288(5):581–588. doi: 10.1001/jama.288.5.581. [DOI] [PubMed] [Google Scholar]
- 19.Kessler RC, Andrews G, Colpe LJ. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 20.Horwitz AV. Distinguishing distress from disorder as psychological outcomes of stressful social arrangements. Health (London) 2007;11(3):273–289. doi: 10.1177/1363459307077541. [DOI] [PubMed] [Google Scholar]
- 21.Gao J, Zheng P, Jia Y. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4) doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goodwin R, Palgi Y, Hamama-Raz Y, Ben-Ezra M. In the eye of the storm or the bullseye of the media: social media use during Hurricane Sandy as a predictor of post-traumatic stress. J Psychiatr Res. 2013;47(8):1099–1100. doi: 10.1016/j.jpsychires.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 23.Seabrook EM, Kern ML, Rickard NS. Social networking sites, depression, and anxiety: a systematic review. JMIR Ment Health. 2016;3(4):e50. doi: 10.2196/mental.5842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marroquín B. Interpersonal emotion regulation as a mechanism of social support in depression. Clin Psychol Rev. 2011;31(8):1276–1290. doi: 10.1016/j.cpr.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 25.Mervosh S, Lu D, Swales V. See which states and cities have told residents to stay at home. New York Times. April 20, 2020.https://www.nytimes.com/interactive/2020/us/coronavirus-stay-at-home-order.html. Accessed April 7, 2020.
- 26.Kroenke K, Spitzer RL, Williams JBW, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 27.Löwe B, Wahl I, Rose M. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122(1–2):86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 28.Karim J, Weisz R, Bibi Z, ur Rehman S. Validation of the eight-item Center for Epidemiologic Studies Depression scale (CES-D) among older adults. Curr Psychol. 2015;34(4):681–692. doi: 10.1007/s12144-014-9281-y. [DOI] [Google Scholar]
- 29.Brant R. Assessing proportionality in the proportional odds model for ordinal logistic regression. Biometrics. 1990;46(4):1171–1178. doi: 10.2307/2532457. [DOI] [PubMed] [Google Scholar]
- 30.Polizzi C, Lynn SJ, Perry A. Stress and coping in the time of COVID-19: pathways to resilience and recovery. Clin Neuropsychiatr. 2020;17(2):59–62. doi: 10.36131/cn20200204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bandura A, Walters RH. Vol. 1. Prentice Hall; Englewood Cliffs, NJ: 1977. (Social Learning Theory). [Google Scholar]
- 32.Marshall RD, Bryant RA, Amsel L, Suh EJ, Cook JM, Neria Y. The psychology of ongoing threat: relative risk appraisal, the September 11 attacks, and terrorism-related fears. Ann Psychol. 2007;62(4):304–316. doi: 10.1037/0003-066X.62.4.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Riehm KE, Feder KA, Tormohlen KN. Associations between time spent using social media and internalizing and externalizing problems among U.S. youth. JAMA Psychiatry. 2019;76(12):1–9. doi: 10.1001/jamapsychiatry.2019.2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shakya HB, Christakis NA. Association of Facebook use with compromised well-being: a longitudinal study. Am J Epidemiol. 2017;185(3):203–211. doi: 10.1093/aje/kww189. [DOI] [PubMed] [Google Scholar]
- 35.Primack BA, Swanier B, Georgiopoulos AM, Land SR, Fine MJ. Association between media use in adolescence and depression in young adulthood: a longitudinal study. Arch Gen Psychiatry. 2009;66(2):181–188. doi: 10.1001/archgenpsychiatry.2008.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin LY, Sidani JE, Shensa A. Association between social media use and depression among U.S. young adults. Depress Anxiety. 2016;33(4):323–331. doi: 10.1002/da.22466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hunt MG, Marx R, Lipson C, Young J. No more FOMO: limiting social media decreases loneliness and depression. J Soc Clin Psychol. 2018;37(10):751–768. doi: 10.1521/jscp.2018.37.10.751. [DOI] [Google Scholar]
- 38.Depoux A, Martin S, Karafillakis E, Preet R, Wilder-Smith A, Larson H. The pandemic of social media panic travels faster than the COVID-19 outbreak. J Travel Med. 2020;27(3) doi: 10.1093/jtm/taaa031. taaa031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhou X, Snoswell CL, Harding LE. The role of telehealth in reducing the mental health burden from COVID-19. Telemed J E Health. 2020;26(4):377–379. doi: 10.1089/tmj.2020.0068. [DOI] [PubMed] [Google Scholar]
- 40.Smith AC, Thomas E, Snoswell CL. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19) J Telemed Telecare. 2020;26(5):309–313. doi: 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Escobar-Viera CG, Shensa A, Bowman ND. Passive and active social media use and depressive symptoms among United States adults. Cyberpsychol Behav Soc Netw. 2018;21(7):437–443. doi: 10.1089/cyber.2017.0668. [DOI] [PubMed] [Google Scholar]
- 42.Verduyn P, Lee DS, Park J. Passive Facebook usage undermines affective well-being: experimental and longitudinal evidence. J Exp Psychol Gen. 2015;144(2):480–488. doi: 10.1037/xge0000057. [DOI] [PubMed] [Google Scholar]
- 43.Perlman SE, Friedman S, Galea S. Short-term and medium-term health effects of 9/11. Lancet. 2011;378(9794):925–934. doi: 10.1016/S0140-6736(11)60967-7. [DOI] [PubMed] [Google Scholar]
- 44.Amsalem D, Dixon LB, Neria Y. The coronavirus disease 2019 (COVID-19) outbreak and mental health: current risks and recommended actions. JAMA Psychiatry. In press. Online June 24, 2020. 10.1001/jamapsychiatry.2020.1730. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.