Abstract
The COVID-19 outbreak has infected millions of people across the world, caused hundreds of thousands of deaths, and collapsed national economies. Recognizing the importance of handwashing in preventing the spread of COVID-19, concerns have arisen about the condition of millions of Africans who lack access to hygiene facilities and clean water services. This paper compiles evidence from the WHO-UNICEF data to show the health disparities that limit the capacity of African countries to effectively address the COVID-19 disease along with recommendations for addressing the challenge.
Keywords: COVID-19, Coronavirus, Sub-Saharan Africa, Health inequality, Public health, Vulnerability
1. Introduction
Since January 2020, the novel coronavirus (COVID-19) outbreak has infected millions of people globally, caused hundreds of thousands of deaths, and collapsed national economies. COVID-19 is a respiratory disease transmitted human-to-human primarily through direct contact with an infected person or via respiratory droplets released as an infected person sneezes, coughs, or talks (Offord, 2020, World Health Organization, 2020). Viruses contained in these respiratory droplets can easily infect other people when they land on the nose, eyes, or mouth or are transferred there by people touching their faces with contaminated hands (Offord, 2020).
There are ongoing efforts to understand the pathological features of the disease and develop measures to prevent its community spread. So far, scientists have compiled evidence to explain the human-to-human transmission of COVID-19 (Paules et al., 2020) and how the disease spreads via asymptomatic carriers (Chan et al., 2020). Lu et al. (2020) have examined the potential route of COVID-19 transmission by studying the airflow inside an airconditioned restaurant in Guangzhou, China. The study traces the most likely cause of the outbreak to droplet transmission from airconditioned ventilation in which the key factor was the direction of airflow. Despite this evidence, “the mechanism by which asymptomatic carriers could acquire and transmit the coronavirus that causes COVID-19 requires further study” (Bai et al., 2020, p. 1407). Recognizing the importance of handwashing in preventing the spread of COVID-19, concerns have arisen about the condition of millions of Africans who lack access to hygiene facilities and clean water services.
The purpose of this paper is to show the health disparities that limit the capacity of Africans to effectively address the spread of the COVID-19 disease using evidence from the WHO-UNICEF household data. Our analysis reveals the challenging context of mitigating the spread of the COVID-19 pandemic in sub-Saharan Africa, given the disparities in health and the socioeconomic conditions in which they arise. We present three policy options for preventing the spread of the COVID-19 pandemic in sub-Saharan Africa.
2. The public health crisis in Sub-Saharan Africa
Various governments have developed policies to address health inequality and its social determinants (Owusu-Addo, Renzaho & Smith, 2020). Academics and practitioners have given considerable attention to efforts aimed at improving overall population health and reducing the burden of diseases as well as eliminating health disparities based on socioeconomic status, race, geography, gender and ethnicity (Arcaya et al., 2015, Balaj et al., 2017, Devaux, 2015, Graham and Kelly, 2004, Hu et al., 2016, Kilbourne et al., 2006, Whitehead, 2007). Omotoso and Koch (2018) contend, however, that despite significant efforts to address the socioeconomic issues that aggravate health inequalities, striking disparities in “health status still exists within and among countries” (p. 1).
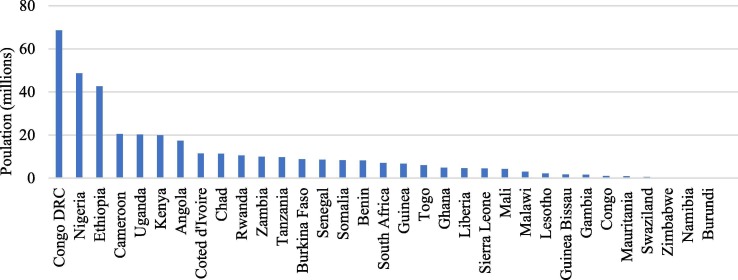
We cannot ignore the importance of making hygiene services accessible to vulnerable populations in sub-Saharan Africa. As the WHO-UNICEF data reveals, about 370 million Africans have no basic handwashing facility (see Fig. 1 ). In the Democratic Republic of Congo, over 68 million people, more than three-quarters of the country’s population, have no handwashing facilities. The situation in Nigeria, an oil-rich country where nearly 50 million people have no handwashing facilities, is unspeakable. Health disparities in Nigeria affect the distribution of water and hygiene services among poor populations, which can lead to a disproportionate impact on public health outcomes during a pandemic outbreak such as COVID-19. Ethiopia is another country where the health disparity is appalling, as 43 million people have no handwashing facility (see Fig. 1).
Fig. 1.
Population with no handwashing facility – Sub-Saharan Africa (2017). Source: WHO-UNICEF hygiene service levels household data (2017).
The health disparities in sub-Saharan Africa are prevalent in small countries such as Rwanda, Angola, Zambia, Togo, Senegal, Chad, Liberia, and Sierra Leone, where more than half the population lack handwashing facilities. For example, 10 million Rwandans, 17 million Angolans, 9.9 Zambian, 6 million Togolese, 4.6 million Liberians, 8.5 million Senegalese, and 4.4 million Sierra Leoneans have no handwashing facilities (see Fig. 1). In a small and low-income country like Liberia with a 5.1 million population, 4.6 million people, representing 90 percent of the country’s population, have no handwashing facilities. Equally important is a small country like Sao Tome and Principe with a population of 211,000 in which three quarters is urban, yet where about 92,000—nearly half of the country’s population—have no handwashing facilities.
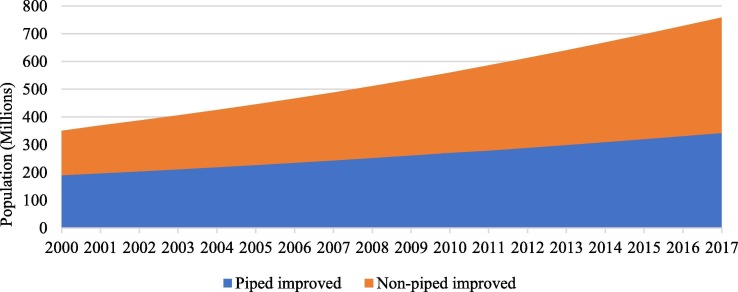
Water scarcity is another public health challenge in sub-Saharan Africa, where a staggering 495 million population had no access to piped drinking water between 2000 and 2017. In 2017 alone, about 416 million Africans did not have access to piped drinking water (Fig. 2 ). The disparity between the demand for drinking water and its availability has a disproportionate impact on the poor. Socioeconomic differences determine which populations have access to water and hygiene services or denied these services. The disparity in handwashing facility coverage across sub-Saharan Africa paints a disturbing picture of health inequality that reveals the vulnerability of the poor to the COVID-19 pandemic. As Abdullahi (2020) notes, poverty is rooted in the deprivation of people’s access to necessities such as healthcare and sanitation. Therefore, the impact of poverty in countries where existing health inequities may exacerbate the vulnerability of the poor to the COVID-19 pandemic remains a critical challenge.
Fig. 2.
Drinking water – Sub-Saharan Africa. Source: WHO-UNICEF data on population with piped and non-piped drinking water (2000–2017).
3. Socioeconomic conditions that increase vulnerability to COVID-19
In 2018, The Brookings Institution released the global poverty projections based on data from the World Poverty Clock, which shows that Africans account for two-thirds of the more than 643 million people across the world living in extreme poverty. The worst affected countries are Nigeria (87 million); Democratic Republic of Congo (60 million); Ethiopia (23.9 million); Tanzania (19.9 million); Mozambique (17.8 million); Kenya (14.7 million); and Uganda (14.2 million) (Adebayo, 2018, Kharas et al., 2018). The failure of an oil-rich country like Nigeria to translate its oil wealth into rising living standards for millions of its citizens weakens prospects for populations living in extreme poverty (Okoi, 2019). Under these conditions, poverty and economic inequality can increase the vulnerability of the poor to the COVID-19 pandemic.
As one of the world’s most unequal regions regarding income inequality (Gandhi, 2017), poverty in sub-Saharan Africa manifests in significant disparities in health status (Adeyanju et al., 2017, Boutayeb and Helmert, 2011, Braveman and Tarimo, 2002, Commission on Social Determinants of Health, 2008, Commission on Social Determinants of Health, 2008, Hakura et al., 2016, Kabudula et al., 2001, Marmot and Commission on Social Determinants of Health, 2007, Marmot, 2005, Orach and Garimoi, 2009, Wagstaff, 2000). Because elders are considered the most at-risk population due to pre-existing conditions, economic inequalities that manifest in significant health disparities can increase their vulnerability to COVID-19. Cloos (2010) found a positive relationship between health and the socioeconomic status of elders in Barbados. By implication, health inequalities correlate with the social determinants of health (Ataguba, Akazili & McIntyre, 2011), with elders being the most vulnerable. In African countries with severe health disparities arising from socioeconomic factors, the outbreak of COVID-19 can have a devastating impact on poor populations, especially elders.
The refugee crisis in Africa calls for concern. We cannot ignore the impact of COVID-19 on millions of Africans who have been displaced by conflict, terrorism, and persecution. In recent years, South Sudan has been the origin of most refugee cases on the continent, which often produce a spillover effect. The influx of South Sudanese refugees to neighbouring countries such as Uganda, Kenya, Ethiopia and the Democratic Republic of Congo (DRC) impose a humanitarian burden on these countries. The complex humanitarian challenge that displacement poses on the continent aggravates health disparities that render millions of displaced persons vulnerable to the COVID-19 disease. We argue, therefore, that the humanitarian challenge in sub-Saharan Africa is likely to increase the risk of the disease spreading more easily in refugee and displacement camps where millions of people are living in unhealthy conditions.
4. Conclusion
This paper examined the health inequities in sub-Saharan Africa that expose vulnerable populations to the COVID-19 pandemic. While COVID-19 is transforming our way of life, including our health, in unprecedented ways (Lichfield, 2020), containing the spread of the disease in societies with dysfunctional health systems raises critical concerns. Efforts to contain the spread of the disease would require developing and implementing public health interventions that take into consideration concerns about equity and social justice. The key challenge is how to translate research on the social determinants of health into public health practice (Tod & Hirst, 2014). The research agenda needs to move beyond documenting health inequalities to include efforts to support policy development to reduce inequality and improve healthy living conditions for the most vulnerable populations (Masseria, Hernández-Quevedo & Allin, 2010).
5. Policy options to prevent the spread of COVID-19
As the world awaits the development and availability of vaccines, several measures can be undertaken at the national and sub-national levels to prevent the worst effect of COVID-19 pandemic on poor communities across sub-Saharan Africa. We propose three policy options for addressing the challenge.
-
1.
Community-Based Health Promotion
The human-to-human spread of the COVID-19 disease is preventable by implementing measures that promote healthy behaviours at the population level in culturally appropriate ways. Health promotion must emphasize community-based interventions designed to achieve change in risk behaviour across a population **(Merzel & D’Afflitti, 2003). Such initiatives must focus on engaging with populations at risk to learn about their needs and the type of interventions required to support the population in practicing healthy behaviours such as physical distancing, handwashing, and the wearing of face mask in public. These measures must include organizing information sessions with local volunteers to assess threats and the capacity of community health institutions.
-
2.
Improving Access to Health Services
There are rising concerns about the lack of access to community health services to support hygienic behaviour. The government-imposed lockdown measures and the promotion of handwashing behaviour have been counterproductive in African communities where marginalized populations lack access to drinking water, handwashing facilities, and soap due to poverty. As Munodawafa, Sookram & Nganda (2013) noted, access to health services is key to addressing the prevalence of health inequalities in sub-Saharan Africa. Improving the living conditions of marginalized populations must include providing access to water, handwashing facility, and hand sanitizers. Governmental actors have responsibilities to prevent the spread of COVID-19 by making these services accessible to populations at risk.
-
3.
Using Pro-Poor Cash Transfers to Tackle the Structural Determinants of Health
Pro-poor strategies focused on improving living conditions are key to addressing health inequalities in sub-Saharan Africa (Munodawafa, Sookram, & Nganda, 2013). The implementation of cash transfer measures can mitigate the structural determinants of health, such as income poverty, that limit the capacity of marginalized populations to fight the COVID-19 pandemic. When people have the means to meet their basic needs for food and shelter, they will be encouraged to engage in healthy behaviours such as physical distancing and hygienic practices that will decrease their vulnerability to the COVID-19 disease.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Abdullahi, M. S. (2020). Three things Nigeria must do to end extreme poverty. World Economic Forum. Retrieved April 29, 2020, from https://www.weforum.org/agenda/2019/03/90-million-nigerians-live-in-extreme-poverty-here-are-3-ways-to-bring-them-out/.
- Adebayo, B. (2018, June 26). Nigeria overtakes India in extreme poverty ranking. CNN. https://www.cnn.com/2018/06/26/africa/nigeria-overtakes-india-extreme-poverty-intl/index.html.
- Adeyanju O., Tubeuf S., Ensor T. Socio-economic inequalities in access to maternal and child healthcare in Nigeria: Changes over time and decomposition analysis. Health Policy and Planning. 2017;32(8):1111–1118. doi: 10.1093/heapol/czx049. [DOI] [PubMed] [Google Scholar]
- Arcaya, M. C., Arcaya, A. L., & Subramanian, S. Inequalities in health: Definitions, concepts, and theories. Global Health Action, 8(1):27106. [DOI] [PMC free article] [PubMed]
- Ataguba J.E., Akazili J., McIntyre D. Socioeconomic-related health inequality in South Africa: Evidence from General Household Surveys. International Journal of Equity Health. 2011;10(48):1–10. doi: 10.1186/1475-9276-10-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai Y., Yao L., Wei T., Tian F., Jin D., Chen L., Wang M. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323(14):1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balaj M., McNamara C.L., Eikemo T.A., Bambra C. The social determinants of inequalities in self-reported health in Europe: Findings from the European social survey (2014) special module on the social determinants of health. European Journal of Public Health. 2017;27(1):107–114. doi: 10.1093/eurpub/ckw217. [DOI] [PubMed] [Google Scholar]
- Boutayeb A., Helmert U. Social inequalities, regional disparities and health inequity in North African countries. International Journal for Equity in Health. 2011;10(1):23. doi: 10.1186/1475-9276-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P., Tarimo E. Social inequalities in health within countries: Not only an issue for affluent nations. Social Science and Medicine. 2002;54(11):1621–1635. doi: 10.1016/s0277-9536(01)00331-8. [DOI] [PubMed] [Google Scholar]
- Chan J.F., Yuan S., Kok K.H. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloos P. Health inequalities in the Caribbean: Increasing opportunities and resources. Global Health Promotion. 2010;17(1):73–76. doi: 10.1177/1757975909356626. [DOI] [PubMed] [Google Scholar]
- Commission on Social Determinants of Health (2008). Closing the gap in a generation: health equity through action on the social determinants of health. Geneva: Geneva: World Health Organization. [DOI] [PubMed]
- Commission on Social Determinants of Health . World Health Organization; Geneva: 2008. Final report of the commission on social determinants of health. [Google Scholar]
- Devaux M. Income-related inequalities and inequities in health care services utilisation in 18 selected OECD countries. European Journal of Health Economics. 2015;16(1):21–33. doi: 10.1007/s10198-013-0546-4. [DOI] [PubMed] [Google Scholar]
- Gandhi, D. (2017, December 6). Figures of the week: Inequality in health and education outcomes in sub-Saharan Africa. Brookings Institution. https://www.brookings.edu/blog/africa-in-focus/2017/12/06/figures-of-the-week-inequality-in-health-and-education-outcomes-in-sub-saharan-africa/.
- Graham H., Kelly M.P. Health Development Agency; London: 2004. Health inequalities: Concepts, frameworks and policy. [Google Scholar]
- Hakura, M. D. S., Hussain, M. M., Newiak, M. M., Thakoor, V., & Yang, M. F (2016). Inequality, gender gaps and economic growth: Comparative evidence for sub-Saharan Africa. International Monetary Fund Working Paper, No 16/111.
- Hu Y., van Lenthe F.J., Borsboom G.J., Looman C.W., Bopp M., Burström B.…Mackenbach J.P. Trends in socioeconomic inequalities in self-assessed health in 17 European countries between 1990 and 2010. Journal of Epidemiology and Community Health. 2016;70(7):644–652. doi: 10.1136/jech-2015-206780. [DOI] [PubMed] [Google Scholar]
- Kabudula C.W., Houle B., Collinson M.A., Kahn K., Gómez-Olivé F.X., Tollman S., Clark S.J. Socioeconomic differences in mortality in the antiretroviral therapy era in Agincourt, rural South Africa, 2001–13: A population surveillance analysis. Lancet Global Health. 2001;5(9):924–935. doi: 10.1016/S2214-109X(17)30297-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kharas, H., Hamel, K., & Hofer, M. (2018, June 19). The start of a new poverty narrative. Brookings Institution. https://www.brookings.edu/blog/future-development/2018/06/19/the-start-of-a-new-poverty-narrative/.
- Kilbourne A.M., Switzer G., Hyman K., Crowley-Matoka M., Fine M.J. Advancing health disparities research within the health care system: A conceptual framework. American Journal of Public Health. 2006;96(12):2113–2121. doi: 10.2105/AJPH.2005.077628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichfield, G. (2020). We’re not going back to normal. MIT Technology Review. Retrieved April 9, 2020, from https://www.technologyreview.com/2020/03/17/905264/coronavirus-pandemic-social-distancing-18-months/.
- Lu J., Gul J., Li K., Xu C., Su W., Lai Z.…Yang Z. COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerging Infectious Diseases. 2020;26(7) doi: 10.3201/eid2607.200764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M., Commission on Social Determinants of Health Achieving health equity: From root causes to fair outcomes. Lancet. 2007;370(9593):1153–1163. doi: 10.1016/s0140-6736(07)61385-3. [DOI] [PubMed] [Google Scholar]
- Marmot M. Social determinants of health inequalities. Lancet. 2005;365(9464):1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- Masseria C., Hernández-Quevedo C., Allin S. Health inequality: What does it mean and how can we measure it? Expert Review of Pharmacoeconomics & Outcomes Research. 2010;10(2):177–186. doi: 10.1586/erp.10.14. [DOI] [PubMed] [Google Scholar]
- Munodawafa D., Sookram C., Nganda B. WHO, Regional Office for Africa; Brazzaville: 2013. A strategy for addressing the key determinants of health in the African region. [Google Scholar]
- Offord, C. (February 21, 2020). How COVID-19 is spread. TheScientist. Retrieved April 17, 2020, from https://www.the-scientist.com/news-opinion/how-covid-19-is-spread-67143?fbclid=iwar1jxbeooins_qkkfumihqoejf2zjst0dj6dof3dtd3otp8gpsxqfpyf68m.
- Okoi, O. (2019). The paradox of oil dependency in Nigeria. Africa Portal. Retrieved May 15, 2020, from https://www.africaportal.org/features/paradox-nigerias-oil-dependency/.
- Omotoso K., Koch S. Assessing changes in social determinants of health inequalities in South Africa: A decomposition analysis. International Journal for Equity in Health. 2018;17(1):181. doi: 10.1186/s12939-018-0885-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orach D., Garimoi C. Health equity: Challenges in low income countries. African Health Sciences. 2009;9(2):49–51. [PMC free article] [PubMed] [Google Scholar]
- Owusu-Addo, E., Renzaho, A.M.N., & Smith, B.J. (2020). The impact of cash transfers on social determinants of health and health inequalities in sub-Saharan Africa: a systematic review. Health Policy and Planning, 33(5), 675–696. https://doi-org.uml.idm.oclc.org/10.1093/heapol/czy020. [DOI] [PMC free article] [PubMed]
- Paules C.I., Marston H.D., Fauci A.S. Coronavirus infections—More than just the common cold. JAMA. 2020;323(8):707–708. doi: 10.1001/jama.2020.0757. [DOI] [PubMed] [Google Scholar]
- Tod A.M., Hirst J. Routledge; Abingdon, UK: 2014. Health and inequality: Applying public health research to policy and practice. [Google Scholar]
- Wagstaff A. World Bank; Washington, DC: 2000. Research on equity, poverty and health outcomes: Lessons for the developing World. [Google Scholar]
- Whitehead M. A typology of actions to tackle social inequalities in health. Journal of Epidemiology and Community Health. 2007;61(6):473–478. doi: 10.1136/jech.2005.037242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020). Water, sanitation, hygiene, and waste management for the COVID-19 virus. https://www.who.int/water_sanitation_health/news-events/wash-and-covid-19/en/.