Supplemental Digital Content is available in the text.
Abstract
Introduction:
Clinical event debriefing functions to identify optimal and suboptimal performance to improve future performance. “Cold” debriefing (CD), or debriefing performed more than 1 day after an event, was reported to improve patient survival in a single institution. We sought to describe the frequency and content of CD across multiple pediatric centers.
Methods:
Mixed-methods, a retrospective review of prospectively collected in-hospital cardiac arrest (IHCA) data, and a supplemental survey of 18 international institutions in the Pediatric Resuscitation Quality (pediRES-Q) collaborative. Data from 283 IHCA events reported between February 2016 and April 2018 were analyzed. We used a Plus/Delta framework to collect debriefing content and performed a qualitative analysis utilizing a modified Team Emergency Assessment Measurement Framework. Univariate and regression models were applied, accounting for clustering by site.
Results:
CD occurred in 33% (93/283) of IHCA events. Median time to debriefing was 26 days [IQR 11, 41] with a median duration of 60 minutes [20, 60]. Attendance was variable across sites (profession, number per debriefing): physicians 12 [IQR 4, 20], nurses 1 [1, 6], respiratory therapists 0 [0, 1], and administrators 1 [0, 1]. “Plus” comments reported per event were most commonly clinical standards 47% (44/93), cooperation 29% (27/93), and communication 17% (16/93). “Delta” comments were in similar categories: clinical standards 44% (41/93), cooperation 26% (24/93), and communication 14% (13/93).
Conclusions:
CDs were performed after 33% of cardiac arrests in this multicenter pediatric IHCA collaborative. The majority of plus and delta comments could be categorized as clinical standards, cooperation and communication.
INTRODUCTION
Clinical event debriefing adapts learnings from simulation debriefing to allow clinicians time to reflect and collectively learn after significant clinical events.1 Debriefing provides the opportunity to discuss interactions within the clinical environment to improve performance in the future.7–9 The American Heart Association, the International Liaison Committee on Resuscitation, and the National Academy of Sciences recommends clinical event debriefing as a tool to improve resuscitation team performance.10–12 Debriefings are categorized by time in relation to the initial event, with “hot” debriefings occurring in the minutes to hours following the event and “cold” debriefings occurring in the days to weeks following an incident.1,6 Hot debriefing utilizes facilitated participant discussion to reflect on events with the team present for the clinical event. This immediate review, while the event is fresh, is key to provide the opportunity for providers to share their emotional responses, address any questions related to clinical care, while concurrently building a culture of teamwork. CDs may include a broader audience, including nonparticipants in the clinical event, and provide the opportunity for a more comprehensive review of clinical decisions, teamwork, and quantitative data (eg, chest compression quality and time to medication).13
Debriefing after resuscitation attempts is associated with improved quality of chest compressions in simulated and clinical cardiac arrests.1,3,14,15 Rates of return of spontaneous circulation3 and survival to hospital discharge with good neurologic function improved after implementation of a CD program.1 Additionally, a comprehensive clinical event review in a pediatric cardiac center described issues with communication in 62% of events followed by environment/policy, then patient care concerns. These reviews led to either educational initiatives or modifications of existing policies.16 Little information exists to guide clinicians during the implementation of a CD program in terms of frequency of event review, expected participation, and common themes that may arise during a event review.
The purpose of this investigation was to characterize CD practices and session content occurring in an international, multicenter pediatric CPR quality collaborative following in-hospital cardiac arrest events.
METHODS
Design and Setting
We analyzed prospectively collected observational data on CDs performed as part of an international, multicenter Pediatric Resuscitation Quality Collaborative (pediRES-Q).17 At the time of data collection, 18 sites across the United States, England, Spain, the Netherlands, and Japan participated in the pediRES-Q collaborative. Site characteristics and bed volumes are available in Table 1, Supplemental Digital Content 1, http://links.lww.com/PQ9/A193. Local institutional review boards or research ethics committees approved participation before enrollment in the collaborative and approved data use agreements per local institutional regulations. This study met the criteria for waiver of consent per the United States Code of Federal Regulations 45 CFR 46.116(d) and 45 CFR 46.408(a). Compliance with the Health Insurance Portability and Accountability Act (HIPAA) was maintained.
Cardiac Arrest Events
We included all events in children less than 18 years old who suffered an in-hospital cardiac arrest and received at least 1 minute of chest compressions between February 1, 2016, and April 30, 2018, in the analysis.
Data Collection
Event data were entered into and managed using Research Electronic Data Capture tools coordinated and hosted at The Children’s Hospital of Philadelphia under an agreement with the software’s development consortium, led by Vanderbilt University.18 Data collected include patient demographics, illness category, event data, CPR performance metrics, postcardiac arrest care quality, and patient outcomes. Sites may choose to participate in quality improvement “bundles” including high-risk patient identification, just in time training, hot debriefing, and CD with subsequent data collection in each module.
The collaborative defined CD as a team-based discussion performed more than 24 hours after an IHCA event. Local hospital preferences determined CD practices without standardized training for debriefing facilitators Site facilitators implemented debriefing, and data were collected via a data collection tool organized by the plus-delta format. Facilitators addressed 2 additional questions: Could this event have been predicted (“event predictability”), and was there a delay in clinical care (“clinical delay”)? The CD steering committee added these as essential data that can be used by the site to improve future practice. The facilitator later recorded quantitative data regarding the timing of debriefing, number and type of participants, and length of the session. Additionally, open-ended questions enabled identification and description of the plus (“what went well”) and the delta (“what could be improved”) actions related to decision-making, teamwork, and other aspects of clinical care.
Participating sites received an additional survey in August 2018 to understand the organization of CD programs better. This survey included questions regarding the structure of CD sessions, notification practices for the debriefings, how sites use data within their debriefings, and identified barriers to CD.
Statistical Analysis
Descriptive statistics of CD participation and composition were performed for all events that reported CD in the database. Univariate associations were assessed with chi-square for proportions and Student’s t-test for continuous variables. To test the association between covariates and the likelihood of debriefing, we used a generalized linear mixed model. We accounted for clustering within hospital sites and included variables with a P value of <0.2 for univariate associations. Summative data were reported from the survey responses. Analyses were conducted using Statistical Analysis System (SAS) software version 9.4 (c SAS Institute Incorporated, Cary, N.C.). Results were considered statistically significant at a level of P <0.05.
We performed a qualitative content analysis on the open-ended comments collected in the pediRES-Q database from comments reported in the 4 categories: plus, delta, identification of clinical delay, and event predictability. The authors analyzed comments and categorized them using a modified Team Emergency Assessment Measure (TEAM) Framework.19 The TEAM framework consists of 10 categories: leadership, communication, cooperation, team climate, adaptability, situational awareness (SA), prioritization, clinical standards (CS) (eg, CPR quality), and other. Two study authors (A.S. and A.C.) independently reviewed and categorized comments into themes. They discussed discordant categorization results until a consensus was achieved. All comments reviewed were thematically sorted into existing categories with a small number of comments in the “other” category, and no novel categories were created. We calculated the overall proportions of responses by dividing the number of debriefings that contained a recorded response by the total number of CDs performed.
RESULTS
The pediRES-Q database contained 283 IHCA events between February 1, 2016, and April 30, 2018. Table 1 displays event-level information for cardiac arrest events. The median age of patients in this cohort was 2.1 years and 56% were male. The most frequent patient category was medical noncardiac (43%), followed by medical-cardiac (24%) and surgical-cardiac (22%). Sixty-six percent of patients survived to hospital discharge.
Table 1.
Event Characteristics

Of the 283 IHCA events, 33% (93/283) subsequently had a CD session performed. During the study period, 4/18 (22%) hospitals in this cohort performed 0 debriefing while 5/18 (28%) performed 1–4 debriefings; 6/18 (33%) performed 5–9, and 3/18 (17%) performed >10 debriefings. As a percentage of total arrests in a single site; 4/18 (22%) sites debriefed 0% of arrests; 4/18 (22%) sites debriefed 1%–25% of events; 2/18 (11%) sites debriefed 26%–50% of events, and 8/18 (44%) sites debriefed >50% of events.
The median time to CD session was 26 days [IQR 11, 41] with a median duration of 60 minutes [IQR 20, 60]. The median number of facilitators per event was 1 (IQR 1, 1; range 0–3). Facilitation and/or cofacilitation was performed by physicians 94% (87/93), nurses 18% (17/93), nurse practitioners 9% (8/93), or other (nonclinicians) 8% (7/93). Attendance varied across sites (profession, number per debriefing [IQR]): physicians (12 [4, 20]), nurses (1 [1, 6]), respiratory therapists (0 [0, 1]), and administrators (1 [0, 1]). Table 2, Supplemental Digital Content 2, http://links.lww.com/PQ9/A193, shows the univariate and multivariate analysis of debriefing by event characteristics. In the multivariate model controlling for clustering at the institution level, IHCA events that had CDs performed were longer than events that did not (22 min versus 14 min, P = 0.03).
Table 2 and Table 3, Supplemental Digital Content 3, http://links.lww.com/PQ9/A193 contain center responses and percentages of Plus and Delta comments. Plus comments were most commonly clinical standards 47% (44/93), cooperation 29% (27/93), and communication 17% (16/93); Delta comments were clinical standards 44% (41/93), cooperation 24% (24/93), and communication 14% (13/93). Tables 3 and 4 contain center responses and percentages of identification of clinical delay and event predictability, respectively. Comments about the identification of clinical delay were most commonly clinical standards 17% (16/93), cooperation 14% (13/93), and communication 14% (13/93). Comments about event predictability were situational awareness 30% (28/93) and clinical standards 13% (12/93).
Table 2.
Proportion of Debriefing Content Themes by Content Analysis of Debriefing Comments
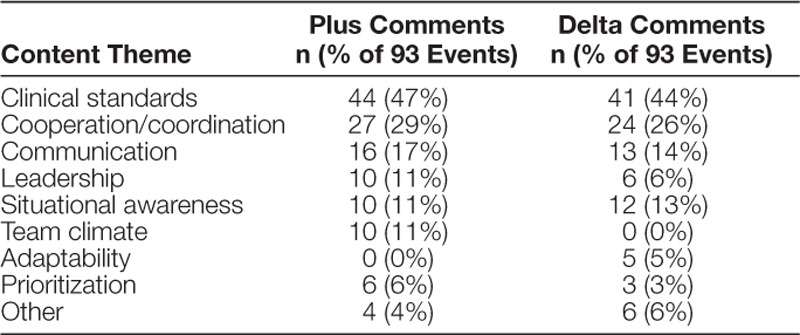
Table 3.
Proportion of “Delays” Debriefing Content Themes by Content Analysis of Debriefing Comments

Table 4.
Proportion “Predicted” Debriefing Content Themes by Content Analysis of Debriefing Comments

We sent the supplemental survey to the 18 participating centers with 17 responses (94%). Figure 1 and Table 4, Supplemental Digital Content 4, http://links.lww.com/PQ9/A193, summarize the survey responses. Eighty-eight percent of centers report performing CDs at the time of the survey. Centers reported that they chose events for CD based on significant learning points (47%). The next most common response was that some sites debrief all events (35%). The majority of debriefing sessions were scheduled as an additional conference (53%), followed by other (29%) with the majority (4/5) of “other” sessions cited as discussions as a part of a morbidity and mortality conference. Data reviewed during sessions included patient history (88%), resuscitation quality data (76%), prearrest clinical information (70%), and code sheet documentation (70%). Twenty-nine percent of facilitators had no training in debriefing facilitation, and 29% of facilitators have received limited training in debriefing facilitation. Twenty-four percent of facilitators received extensive training (older than 3 days). Time (24%) and lack of financial support to promote debriefings (24%) were the most commonly cited barriers to CD. Eighty-eight percent of centers stated that CD sessions have improved resuscitation care at their institutions. Table 5, Supplemental Digital Content 5 (http://links.lww.com/PQ9/A193) lists the survey result comment section regarding improvements in patient care related to CD programs.
Fig. 1.

Survey responses of providers performing cold debriefing. CS, code sheet; Hx, patient history; L of DS, lack of department/divison support; L or FE, lack of facilitator expertise; L of FS, lack of financial support; L of Int, lack of interest; L of T, lack of time; PAD, prearrest details.
DISCUSSION
In this study, we sought to characterize the frequency, processes, and content of CD sessions after IHCA in an international pediatric resuscitation collaborative. A majority of institutions (78%) reported performing CD sessions for 33% of the IHCA reported to the database. Longer duration IHCA events were more likely to have a CD.
The content of the CDs performed in this collaborative was qualitatively analyzed and sorted into themes based on the TEAM Framework. “Plus/what went well,” “Delta/what could be improved,” and identification of clinical delay themes most frequently pertained to clinical standards, cooperation, and communication during events. Not surprisingly, event predictability themes featured situational awareness and clinical standards. Whether an event could have been predicted is challenging due to hindsight bias; however, if a team has keen situational awareness, they may be able to recognize clinical patterns that predate a cardiac arrest event. In a similar study of hot debriefing in the same collaborative, cooperation and communication were the most frequent themes, followed by clinical standards.20 This finding suggests that regardless of the debriefing timing when a team discusses “what went well” or “what could be improved,” teams tend to focus on clinical and teamwork issues that are central to patient outcomes. In comparison to the previous analysis of hot debriefing, this study of CD differs slightly in that displaying and reviewing objective data collected from the event is likely to trigger particular discussion related to the objective data (eg, quality of chest compressions and peri-shock pause duration are likely discussed when CPR data are displayed). Event predictability themes were similar between hot and CD sessions, with comments focusing on the team’s situational awareness.20 These differences in content between hot and CD sessions reflect the timing and focus of the different sessions.
Our data suggest that multidisciplinary teams of physicians, nurses, and respiratory therapists attend CD sessions; however, physicians made up a majority of the participants. This finding is not surprising as nurses and respiratory therapists often find it difficult to leave the bedside during clinical care, and are usually not reimbursed for attending meetings. The sessions occurred approximately a month after an IHCA occurred, and the median length was 1 hour. Approximately, a third of IHCA events had CDs performed, whereas 57% of events from the same collaborative had hot debriefings performed.20 Both the decision to hold a CD (eg, if the units debrief all, some, or no events), as well as the timing of the debriefing relative to the cardiac arrest event likely influence debriefing attendance. A variety of reasons may contribute to the effect of timing of the debriefing, including but not limited to: (1) availability of providers (more likely to available on the day of the event); (2) relevance and interest (perhaps higher immediately after the event); (3) emotional engagement (likely higher immediately after the event); and (4) scheduling priorities and resources (not all sites have resources to perform facilitated CDs). More study is required to define ways of engaging more participation in both hot and CDs. In light of this evidence that nursing and respiratory therapists are represented in lower numbers during debriefings, facilitators must make extra effort to feedback the key take-home points from the session to everyone that works in the unit.
CDs were performed on IHCA events of all lengths; however, it is clear from survey results and data that more prolonged and complicated events are more likely to have a cold debrief performed. These events likely had more learning points that were felt by debriefing leaders to benefit discussion among a larger group of participants. Although this finding may seem logical, we would argue that debriefing is essential for all types of cardiac arrest events—regardless of duration and/or outcome—as there is much to be learned from both positive and negative patient outcomes and team experiences.
CD practices within the collaborative showed significant variability. Only 44% of sites debriefed more than 50% of the cardiac arrests that occurred at their site. A closer look at the qualitative survey responses in combination with quantitative results from the database suggests that 3 types of debriefing structures emerge. “Dedicated CDs” are an hour-long, monthly review of a salient event and all staff that work in a unit are invited to attend as described in a report by Zebuhr et al.13 “Code Review Committees” seem to be sessions that occur bi-weekly or monthly, accompanied by a diverse audience and may review data from multiple events within the hour session, similar to work described by Blankenship et al.16 The third type of event review could be described as “Within another conference.” These sessions add a review of qualitative CPR data and cardiac arrest issues nested into either a morbidity and mortality conference or case conference, attended by a broad audience of clinicians. There may be benefits and drawbacks to this “within another conference” subtype. For instance, in programs with a robust M&M conference with multidisciplinary attendance, the addition of CPR quality data and resuscitation best practices may bring this data to a wider audience. However, many topics may need to be addressed during an M&M session, so the relative amount of time discussing CPR quality and resuscitation performance may be limited. All of the subtypes of CD occur in an interdisciplinary manner and bring discussions of rare events to audiences more extensive than the immediate response team. No literature exists to support one type of presentation as more effective at communicating needs for resuscitation gaps to improve performance at future events. Similarly, we lack evidence to support a prescribed frequency of debriefing. However, our collaborative has defined successful “implementation” of CD as debriefing >50% of events if a center has less than 10 IHCA a year and >10 CD sessions/year if the center has more than 10 IHCA. Further studies about the structure and frequency of CD may identify what makes this intervention most effective.
The most common barriers to performing CDs were time and lack of financial support to promote the conference. Centers that plan to start a CD program should anticipate these barriers and create a plan to address these issues directly during the implementation of debriefings. CD programs that discuss and follow up on the implementation of identified solutions from these sessions may fulfill Part 4 maintenance of certification through the American Board of Pediatrics. Despite these barriers, the majority of centers in this collaboration have been able to institute some degree of CD in their institutions. A majority (88%) report that they believe that this work has improved resuscitation care in their institution.
Dedicated facilitator training for debriefing was variable across institutions. Twenty-nine percent of facilitators had no training in debriefing facilitation, and 29% of facilitators have received limited training in debriefing facilitation, and 24% have received extensive training (>3 d). Prior facilitator training was most likely in the context of simulation-based education. In our study, we chose not to provide standardized facilitator training across sites, primarily for logistical reasons. Instead, we decided to use a standardized debriefing tool, providing a general outline while still permitting the facilitator to structure their follow-up and probing questions. Lack of a standardized approach to debriefing represents a limitation of our study. For the most part, we have no way of determining how questions were asked, who was engaged in the discussion, if relevant performance gaps were addressed, and if the facilitator took the time to explore underlying frames. The potential variability in the debriefing approach may have influenced learning outcomes and take-home messages. Future research should explore the impact of standardized facilitator training on the effectiveness of clinical debriefing programs.
There are several other limitations to this study. First, these data describe centers that have voluntarily joined a pediatric resuscitation quality improvement collaborative and are likely not generalizable to all pediatric hospitals. These centers may be more interested or better resourced to focus on resuscitation practices, thus more committed to performing CD. Second, these data rely on clinician recall of discussions during a CD session. Facilitators recorded 2 or 3 points per session, so while the most salient topics were likely reported, this is not a comprehensive representation of discussions during CDs. Third, we do not know if the debriefing facilitator or site PI (could be the same or different clinicians) completed the survey. If the facilitator completed the survey, this could be a conflict as they may have different attitudes toward debriefing. Finally, there was a conflict between the survey responses and the reviewed data, which is likely because the survey was completed months after data collection ended.
CONCLUSIONS
In this multicenter, international resuscitation quality improvement collaborative, CDs occurred in 33% of all IHCA events, and 78% of sites reported performing at least one CD during the study period. Clinical issues raised were the most common themes of clinical standards, communication, and cooperation. Further study is required to understand how the facilitation and structure of CDs impact functions of teams and patient outcomes after in-hospital cardiac arrest.
DISCLOSURE
Dr. Wolfe, Ms. Niles, Dr. Nadkarni, and Dr. Duval-Arnould disclosed that The Children’s Hospital of Philadelphia receives support from an unrestricted research grant from ZOLL Medical. Dr. Wolfe has received research funding for NHLBI (funds to institution), as well as speaking honoraria from Zoll Medical. Dr. Sutton has received research grants from NHLBI and NICHD to study pediatric in-hospital cardiopulmonary resuscitation (funds to institution), Pediatric Advanced Life Support authorship via the American Heart Association, membership on the Emergency Cardiovascular Care Committee and past speaking honoraria for Zoll Medical. The authors have no financial interest to declare in relation to the content of this article.
ACKNOWLEDGMENTS
The resuscitation clinical learning laboratory collaboration would not have been possible without the generous and unrestricted educational grant support of Laerdal Medical (2006–2013) and ZOLL Medical (2014–2018).
Supplementary Material
Footnotes
Published online 8 July 2020
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
For a list of the pediRES-Q Investigators, please visit http://links.lww.com/PQ9/A205.
To cite: Wolfe HA, Wenger J, Sutton R, Seshadri R, Niles DE, Nadkarni V, Duval-Arnould J, Sen AI, Cheng A; on behalf of the pediRES-Q Investigator. Cold Debriefings after In-hospital Cardiac Arrest in an International Pediatric Resuscitation Quality Improvement Collaborative Pediatr Qual Saf 2020;4:e319.
REFERENCES
- 1.Wolfe H, Zebuhr C, Topjian AA, et al. Interdisciplinary ICU cardiac arrest debriefing improves survival outcomes*. Crit Care Med. 2014; 42:1688–1695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reeder RW, Girling A, Wolfe H, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network (CPCCRN). Improving outcomes after pediatric cardiac arrest - the ICU-Resuscitation Project: study protocol for a randomized controlled trial. Trials. 2018; 19:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edelson DP, Litzinger B, Arora V, et al. Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med. 2008; 168:1063–1069 [DOI] [PubMed] [Google Scholar]
- 4.Kessler DO, Cheng A, Mullan PC. Debriefing in the emergency department after clinical events: a practical guide. Ann Emerg Med. 2015; 65:690–698 [DOI] [PubMed] [Google Scholar]
- 5.Sawyer T, Eppich W, Brett-Fleegler M, et al. More than one way to debrief: a critical review of healthcare simulation debriefing methods. Simul Healthc. 2016; 11:209–217 [DOI] [PubMed] [Google Scholar]
- 6.Mullan PC, Wuestner E, Kerr TD, et al. Implementation of an in situ qualitative debriefing tool for resuscitations. Resuscitation. 2013; 84:946–951 [DOI] [PubMed] [Google Scholar]
- 7.Cheng A, Nadkarni VM, Mancini MB, et al. ; American Heart Association Education Science Investigators; and on behalf of the American Heart Association Education Science and Programs Committee, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Council on Cardiovascular and Stroke Nursing; and Council on Quality of Care and Outcomes Research. Resuscitation education science: educational strategies to improve outcomes from cardiac arrest: a scientific statement from the American Heart Association. Circulation. 2018; 138:e82–e122 [DOI] [PubMed] [Google Scholar]
- 8.Cheng A, Eppich W, Grant V, et al. Debriefing for technology-enhanced simulation: a systematic review and meta-analysis. Med Educ. 2014; 48:657–666 [DOI] [PubMed] [Google Scholar]
- 9.Eppich WJ, Mullan PC, Brett-Fleegler M, et al. “Let’s Talk About It”: translating lessons from health care simulation to clinical event debriefings and coaching conversations. Clin Pediatr Emerg Med. 2016; 17:200–211 [Google Scholar]
- 10.Meaney PA, Bobrow BJ, Mancini ME, et al. ; CPR Quality Summit Investigators, the American Heart Association Emergency Cardiovascular Care Committee, and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013; 128:417–435 [DOI] [PubMed] [Google Scholar]
- 11.Monsieurs KG, Nolan JP, Bossaert LL, et al. ; ERC Guidelines 2015 Writing Group. European resuscitation council guidelines for resuscitation 2015: section 1. Executive summary. Resuscitation. 2015; 95:1–80 [DOI] [PubMed] [Google Scholar]
- 12.Graham R, McCoy MA, Schultz AM; Institute of Medicine (IOM) In: Strategies to Improve Cardiac Arrest Survival: A Time to Act. 2015Washington, DC: The National Academy Press; [PubMed] [Google Scholar]
- 13.Zebuhr C, Sutton RM, Morrison W, et al. Evaluation of quantitative debriefing after pediatric cardiac arrest. Resuscitation. 2012; 83:1124–1128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hunt EA, Jeffers J, McNamara L, et al. Improved cardiopulmonary resuscitation performance with CODE ACES2: a resuscitation quality bundle. J Am Heart Assoc. 2018; 7:e009860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dine CJ, Gersh RE, Leary M, et al. Improving cardiopulmonary resuscitation quality and resuscitation training by combining audiovisual feedback and debriefing. Crit Care Med. 2008; 36:2817–2822 [DOI] [PubMed] [Google Scholar]
- 16.Blankenship AC, Fernandez RP, Joy BF, et al. Multidisciplinary review of code events in a Heart Center. Am J Crit Care. 2016; 25:e90–e97 [DOI] [PubMed] [Google Scholar]
- 17.Niles DE, Duval-Arnould J, Skellett S, et al. Characterization of pediatric in-hospital cardiopulmonary resuscitation quality metrics across an International Resuscitation Collaborative. Pediatr Crit Care Med. 2018; 19:421–432 [DOI] [PubMed] [Google Scholar]
- 18.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cooper S, Cant R, Porter J, et al. Rating medical emergency teamwork performance: development of the Team Emergency Assessment Measure (TEAM). Resuscitation. 2010; 81:446–452 [DOI] [PubMed] [Google Scholar]
- 20.Sweberg T, Sen AI, Mullan PC, et al. ; Pediatric Resuscitation Quality (pediRES-Q) Collaborative Investigators. Description of hot debriefings after in-hospital cardiac arrests in an international pediatric quality improvement collaborative. Resuscitation. 2018; 128:181–187 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


