Abstract
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing the coronavirus disease 2019 (COVID-19) has been declared a pandemic by the World Health Organization (WHO) on 11th March 2020. Bulk of research on this virus are carried out to unveil its multivariate pathology. Surprisingly, men are reportedly more vulnerable to COVID-19 even with higher fatality rate compared to women. Thus, it is crucial to determine whether SARS-CoV-2 infection can even affect male fertility as an immediate or long-term consequence of the disease. Among the discrete data available, an important finding is that angiotensin converting enzymes 2 (ACE2) receptor, that aids the SARS-CoV-2 entry into host cells, is profoundly expressed in testicular cells. In addition, the endogenous androgen milieu and its receptors are associated with ACE2 activation reflecting that enhanced testosterone levels may trigger the pathogenesis of COVID-19. In contrary, hypogonadism has also been reported in the acute phase of some COVID-19 cases. Moreover, SARS-CoV-2 infection-induced uncontrolled inflammatory responses may lead to systemic oxidative stress (OS), whose severe disruptive effects on testicular functions are well-documented. This article aims to precisely present the possible impact of COVID-19 on male reproductive functions, and to highlight the speculations that need in-depth research for the exact underlying mechanisms how COVID-19 is associated with men’s health and fertility.
Keywords: Androgen, Angiotensin-converting enzymes 2, COVID-19, Male infertility, Oxidative stress, SARS-CoV-2
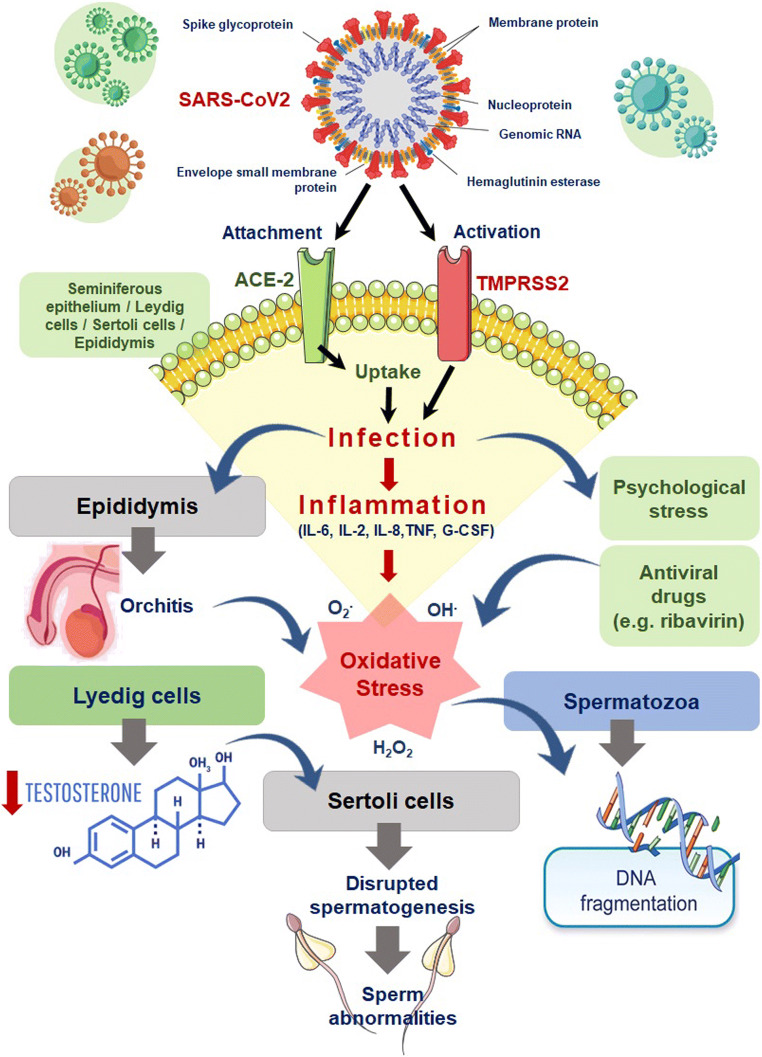
The corona virus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first identified in December 2019 in the Wuhan city in China causing several cases of pneumonia [1]. The virus has since spread globally, leading to acute respiratory distress syndrome (SARS) named as coronavirus disease 2019 (COVID-19) by the World Health Organization (WHO) [2]. On 11th March 2020, WHO has declared the disease as global pandemic [2]. However, the occurrence of COVID-19 shows gender differences and it is an unexplained phenomenon why men seem more susceptible to SARS-CoV-2 infection compared to women, with even higher fatality rate. Angiotensin-converting enzymes 2 (ACE2) receptor plays a key role in the COVID-19 pathogenesis aiding direct host cell damage. Binding of SARS-CoV-2 virus with the ACE2 receptors enables its cellular entry and replication [3]. Consequently, it may be perceived that cells with higher ACE2 expression are more susceptible to SAR-CoV2 infection [3]. Having considered these reports, it is a breakthrough revelation in male fertility research that testes show almost the highest ACE2 mRNA and protein expressions among the various body tissues [3]. The four main testicular cell types showing expression of ACE2 mRNA are the seminiferous duct cells, spermatogonia, Leydig cells, and Sertoli cells [3–5]. Moreover, distinctly high ACE2 expression in testicular cells, while comparatively low expression levels of ACE2 in ovarian cells [6, 7], may also support higher vulnerability of SARS-CoV-2-mediated impairment in male gonadal functions (Fig. 1).
Fig. 1.
Possible mechanisms of SARS-CoV-2 infection induced impairment in male reproductive functions
Research carried out following the outbreak of SARS-CoV in 2002 found that orchitis was one of its accepted health complication that may lead to disruption in spermatogenesis, germ cell apoptosis thereby affecting semen quality [8]. One study had showed that six male patients who succumbed to SARS-CoV infection in 2002 were suffering from orchitis as observed through testicular autopsy [8]. In this study, histopathological investigations revealed inflammatory infiltrates mainly in the seminiferous tubules [8]. Immunohistochemistry showed that IgG deposition was mainly present in seminiferous epithelium, interstitium, degenerated germ cells, and Sertoli cells [8]. Interestingly, in-situ hybridization of testicular tissue specimens does not recognize viral genomic materials [8]. Moreover, studies could not yet find viral trace in the seminal plasma [9, 10]. This indicates that inflammatory and immunologic reactions take pivotal role in the viral-mediated testicular damage.
Testicular expression of ACE2 has been shown to be age-related [5]. The highest expression in patients aged 30 and older than 20 has been reported, whereas those aged 60 have the lowest expression levels [5]. That could show that young male patients are more likely than older patients to experience testicular injury due to COVID-19. This also suggests the profound pathophysiological role of various hormonal milieu in SARS-CoV-2 infection in men. As reported, the first step needed of SARS-CoV-2 infectivity is the proteases-mediated priming of its spike proteins with host cell receptor, mainly via the transmembrane protease, serine 2 (TMPRSS2) [11]. TMPRSS2 have been suggested to cleave ACE2 receptor, aiding the entry of the virus into host cell [12]. Evidences through human studies claim that androgen receptor activation is needed to trigger TMPRSS2 gene transcription. Since, gene loci of androgen receptor and ACE2 are located in chromosome X, increased X-linked inheritance of genetic polymorphisms and consequently endogenous androgen actions may be a possible mechanism to explain male vulnerability to COVID-19 [13]. However, there are contradicting reports stating that SARS-CoV-2 infection in male leads to acute stage hypogonadism and it is suggested that reduction in androgenic action may lead to even fatal consequences. Several studies in human as well as in animals have linked hypogonadism with levels of increased pro-inflammatory cytokines, mainly IL-1β, IL-6, and TNF-α [14–16], which in turn are important inflammatory mediators in SARS-CoV-2 pathogenesis. Nevertheless, an acute critical inflammatory condition, as in the case of COVID-19, may suppress activity of hypothalamic–pituitary–testicular (HPT) axis, leading to reduced low luteinizing hormone (LH), follicle-stimulating hormone (FSH), and testosterone levels. But this theoretical perception does not correspond to a study conducted on 81 COVID-19 male patients, which reported lower serum testosterone levels, higher LH levels, and lower T:LH ratio in comparison to age-matched control subjects [17]. These findings may suggest direct effects of SARS-CoV-2 infection in testicular cells rather than via the HPT axis. Thus, the associations of SARS-CoV-2 infection and modulation of sex hormones in male are major missing links which await in-depth research interventions.
SAR-CoV2 can operate via multiple possible mechanisms which may lead to disruption of male reproductive functions. It is suggested that this virus activates oxidant-sensitive pathways via inflammatory responses, thereby inducing oxidative stress (OS), which presents a common pathological mechanism to disrupt several physiological functions via oxidative damage to host tissues. OS-mediated mechanisms of male infertility are widely documented, as OS can affect semen quality and disrupt sperm functions and morphology, intracellular oxidative damage to spermatozoa by lipid peroxidation of sperm membrane, sperm DNA damage, as well as inducing apoptotic pathways in spermatozoa [18, 19]. In SARS-CoV infections, the excessive production of reactive oxygen species (ROS) may trigger mainly the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB)-toll-like receptor (mainlyTLR-4) pathways [20]. This further stimulate release of cytokines causing exaggeration of the inflammatory responses [20]. As already discussed, this virus can potentially cause orchitis which also can lead to induction of OS. Moreover, SARS-CoV-2 infection causes psychological stress which is a major cause of systemic OS [21]. Besides the direct relation of SARS-CoV-2 infection and OS, treatment of COVID-19 include antiviral drugs like ribavirin which has been shown to be associated with induction of OS, reduced testosterone level, impaired spermatogenesis, and sperm abnormalities in animal studies [22, 23]. Moreover, ribavirin treatment showed reduced sperm count [24] and sperm DNA fragmentation (SDF) [25] up to 8 months following cessation of treatment [21, 26].
Based on these vital reports, it can be hypothesized that the testis could be a potential target for SARS-CoV-2 virus and testicular damage as well as subsequent infertility after COVID-19 infection can be theoretically explained. A direct invasion of SARS-CoV-2 virus is caused by ACE2 receptors likely causing direct testicular damage, or by affecting testicular functions by secondary immunological and inflammatory responses. This possibility needs to be investigated through follow-up studies of the reproductive functions of reclaimed male patients. Thus, it cannot be ruled out that COVID-19 could have immediate or delayed impacts on male fertility status. So far, no definitive data is obtained to track the reproductive functions in men recovered from COVID-19. Since male infertility is already showing a global declining trend which is a major threat to humankind, it is crucial to undertake thorough research to reveal the exact impact and mechanism by which the pandemic COVID-19 might affect the male fertility parameters.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS, China Medical Treatment Expert Group for Covid-19 Clinical characteristics of coronavirus disease 2019 in China. N Eng J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Naming the coronavirus disease (COVID-19) and the virus that causes it. 2020. [https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it]. Accessed 10 July 2020.
- 3.Fan C, Li K, Ding Y, Lu WL, Wang J. ACE2 expression in kidney and testis may cause kidney and testis damage after 2019-nCoV infection. MedRxiv. 2020. 10.1101/2020.02.12.20022418.
- 4.Wang Z, Xu X. scRNA-seq profiling of human testes reveals the presence of the ACE2 receptor, a target for SARS-CoV-2 infection in spermatogonia, Leydig and Sertoli cells. Cells. 2020;9(4):920. doi: 10.3390/cells9040920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shen Q, Xiao X, Aierken A, Liao M, Hua J. The ACE2 expression in Sertoli cells and germ cells may cause male reproductive disorder after SARS-CoV-2 infection. OSF Preprint. 2020. 10.31219/osf.io/fs5hd. [DOI] [PMC free article] [PubMed]
- 6.Shastri A, Wheat J, Agrawal S, Chaterjee N, Pradhan K, Goldfinger M, et al. Delayed clearance of SARS-CoV2 in male compared to female patients: High ACE2 expression in testes suggests possible existence of gender-specific viral reservoirs. medRxiv. 2020. 10.1101/2020.04.16.20060566.
- 7.Stanley KE, Thomas E, Leaver M, Wells D. Coronavirus disease (COVID-19) and fertility: viral host entry protein expression in male and female reproductive tissues. Fertil Steril. 2020;114:33–43. doi: 10.1016/j.fertnstert.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu J, Qi L, Chi X, Yang J, Wei X, Gong E, Peh S, Gu J. Orchitis: a complication of severe acute respiratory syndrome (SARS) Biol Reprod. 2006;74(2):410–416. doi: 10.1095/biolreprod.105.044776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pan F, Xiao X, Guo J, Song Y, Li H, Patel DP, Spivak AM, Alukal JP, Zhang X, Xiong C, Li PS, Hotaling JM. No evidence of SARS-CoV-2 in semen of males recovering from COVID-19. Fertil Steril. 2020;113:1135–1139. doi: 10.1016/j.fertnstert.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nora H, Philippos E, Marcel A, Cornelius D, Dunja B-B, Ortwin A, et al. Assessment of SARS-CoV-2 in human semen-a cohort study. Fertil Steril. 2020. 10.1016/j.fertnstert.2020.05.028. [DOI] [PMC free article] [PubMed]
- 11.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heurich A, Hofmann-Winkler H, Gierer S, Liepold T, Jahn O, Pöhlmann S. TMPRSS2 and ADAM17 cleave ACE2 differentially and only proteolysis by TMPRSS2 augments entry driven by the severe acute respiratory syndrome coronavirus spike protein. J Virol. 2014;88(2):1293–1307. doi: 10.1128/JVI.02202-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wambier CG, Goren A. SARS-COV-2 infection is likely to be androgen mediated. J Am Acad Dermatol. 2020;83:308–309. doi: 10.1016/j.jaad.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohamad N-V, Wong SK, Wan Hasan WN, Jolly JJ, Nur-Farhana MF, Ima-Nirwana S, Chin KY. The relationship between circulating testosterone and inflammatory cytokines in men. Aging Male. 2019;22(2):129–140. doi: 10.1080/13685538.2018.1482487. [DOI] [PubMed] [Google Scholar]
- 15.Maggio M, Basaria S, Ceda G, Ble A, Ling S, Bandinelli S, et al. The relationship between testosterone and molecular markers of inflammation in older men. J Endocrinol Investig. 2005;28(11 Suppl Proc):116–119. [PubMed] [Google Scholar]
- 16.Pozzilli P, Lenzi A. Testosterone, a key hormone in the context of COVID-19 pandemic. Metab Clin Exp. 2020;108:154252. doi: 10.1016/j.metabol.2020.154252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ma L, Xie W, Li D, Shi L, Mao Y, Xiong Y, et al. Effect of SARS-CoV-2 infection upon male gonadal function: a single center-based study. medRxiv. 2020. 10.1101/2020.03.21.20037267.
- 18.Dutta S, Majzoub A, Agarwal A. Oxidative stress and sperm function: a systematic review on evaluation and management. Arab J Urol. 2019;17(2):87–97. doi: 10.1080/2090598X.2019.1599624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sengupta P, Dutta S. Does SARS-CoV-2 infection cause sperm DNA fragmentation? Possible link with oxidative stress. Eur J Contracept Reprod Health Care. 2020. 10.1080/13625187.2020.1787376. [DOI] [PubMed]
- 20.Delgado-Roche L, Mesta F. Oxidative stress as key player in severe acute respiratory syndrome coronavirus (SARS-CoV) infection. Arch Med Res. 2020;51:384–387. doi: 10.1016/j.arcmed.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li R, Yin T, Fang F, Li Q, Chen J, Wang Y, Hao Y, Wu G, Duan P, Wang Y, Cheng D, Zhou Q, Zafar MI, Xiong C, Li H, Yang J, Qiao J. Potential risks of SARS-Cov-2 infection on reproductive health. Reprod BioMed Online. 2020;41:89–95. doi: 10.1016/j.rbmo.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Almasry SM, Hassan ZA, Elsaed WM, Elbastawisy YM. Structural evaluation of the peritubular sheath of rat’s testes after administration of ribavirin: a possible impact on the testicular function. Int J Immunopathol Pharmacol. 2017;30(3):282–296. doi: 10.1177/0394632017726261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Narayana K, D’Souza UJ, Rao KS. Ribavirin-induced sperm shape abnormalities in Wistar rat. Mutat Res. 2002;513(1–2):193–196. doi: 10.1016/S1383-5718(01)00308-4. [DOI] [PubMed] [Google Scholar]
- 24.Bukhari SA, Ahmed MM, Anjum F, Anwar H, Naqvi SAR, Zahra T, et al. Post interferon therapy decreases male fertility through gonadotoxic effect. Pak J Pharm Sci. 2018;31(4 Suppl):1565–1570. [PubMed] [Google Scholar]
- 25.Anifandis G, Messini CI, Daponte A, Messinis IE. COVID-19 and fertility: a virtual reality. Reprod BioMed Online. 2020;41:89–95. doi: 10.1016/j.rbmo.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pecou S, Moinard N, Walschaerts M, Pasquier C, Daudin M, Bujan L. Ribavirin and pegylated interferon treatment for hepatitis C was associated not only with semen alterations but also with sperm deoxyribonucleic acid fragmentation in humans. Fertil Steril. 2009;91(3):e17–e22. doi: 10.1016/j.fertnstert.2008.07.1755. [DOI] [PubMed] [Google Scholar]