Abstract
Physical inactivity is a key risk factor for a range of chronic diseases and conditions, yet, approximately 50% of U.S. adults fall below recommended levels of regular aerobic physical activity (PA). This is particularly true for ethnic minority populations such as Latino adults for whom few culturally adapted programs have been developed and tested. Text messaging (SMS) represents a convenient and accessible communication channel for delivering targeted PA information and support, but has not been rigorously evaluated against standard telehealth advising programs. The objective of the On The Move randomized controlled trial is to test the effectiveness of a linguistically and culturally targeted SMS PA intervention (SMS PA Advisor) versus two comparison conditions: a) a standard, staff-delivered phone PA intervention (Telephone PA Advisor) and b) an attention-control arm consisting of a culturally targeted SMS intervention to promote a healthy diet (SMS Nutrition Advisor). The study sample (N = 350) consists of generally healthy, insufficiently active Latino adults ages 35 years and older living in five northern California counties. Study assessments occur at baseline, 6, and 12 months, with a subset of participants completing 18-month assessments. The primary outcome is 12-month change in walking, and secondary outcomes include other forms of PA, assessed via validated self-report measures and supported by accelerometry, and physical function and well-being variables. Potential mediators and moderators of intervention success will be explored to better determine which subgroups do best with which type of intervention. Here we present the study design and methods, including recruitment strategies and yields.
Trial Registration: clinicaltrial.gov Identifier = NCT02385591
Keywords: Aging, Physical activity, Latino, Text-messaging, Digital health, mHealth
1. Introduction
Regular physical activity has been found to positively impact many of the most common chronic diseases in the U.S., yet approximately half of Americans engage in levels of aerobic physical activity that are insufficient for achieving many of these benefits [1]. This is particularly true for older, low-income, and Latino adults [2], who have elevated rates of obesity, Type 2 diabetes, and other chronic conditions [3], and often more limited access to appropriate health promotion programs [4].
The growth of tele-health programs to promote regular physical activity and other health behaviors provides a potentially convenient and accessible communication channel for delivering evidence-based physical activity advice and support to the American public [5]. This is particularly the case for Latino and other underserved groups, the majority of whom own mobile phones [6] and also report time and logistical constraints that may make it difficult to attend in-person classes or programs [4,7,8].
Short message service (SMS), also known as text messaging, is an especially prevalent and convenient form of communication that can be delivered via simple cell phone devices as well as smartphones to populations with a range of educational levels. The small number of mobile phone interventions to date that have included or focused primarily on text messaging generally have reported significant positive effects, relative to controls, on physical activity levels [5,9]. However, few such interventions have been based on relevant behavioral theory or customized specifically for Latino adults, and most interventions have been less than 6 months in duration [9,10].
The On The Move Trial represents among the first studies to systematically compare the effects of a culturally customized physical activity SMS advising program to a standard, staff-delivered physical activity phone advising program in Latino adults. A second comparison arm—a culturally customized SMS intervention to promote a healthy diet—was also included to investigate any nonspecific effects of the innovative SMS delivery platform itself on physical activity levels. Given the relative lack of community-based clinical trials in the health promotion area that have specifically targeted midlife and older Latino adults [8], the On The Move Trial also provides an opportunity to evaluate different recruitment channels of particular relevance to Latino adults.
Phone-based interventions may be particularly suitable for midlife and older adults given their convenience (e.g., participants are not required to travel to a program location), customizability, and the fact that the majority of adults in this age group (i.e., 94% or higher in adults through age 64 years and 85% of adults ages 65 and older) use mobile phones [6]. The study design and procedures, including recruitment, intervention, and assessment procedures, constitute the major focus of this paper.
2. Methods and procedures
The trial was conducted by the Healthy Aging Research and Technology Solutions (HARTS) laboratory at Stanford University School of Medicine. The Stanford University School of Medicine Institutional Review Board approved the study protocol for this trial. Study materials, including informed consent and recruitment, intervention, and assessment forms, were produced in English and underwent thorough translation into Spanish by certified translators (see below). Participants provided written consent upon reviewing the consent form with a bilingual staff member. The trial was registered at Clinicaltrials.gov (#NCT02385591).
2.1. Study design
The major objective of this randomized controlled trial (RCT) is to compare two different communication modalities (human phone advising vs. interactive SMS advising) for delivering a theoretically derived PA program. The specific primary aim is to test whether a culturally appropriate 12-month physical activity intervention delivered via an interactive SMS platform is similar in effectiveness to a standard human telephone advisor intervention. The primary focus of the PA interventions is on walking—a convenient and popular form of physical activity, especially for insufficiently active adults [5]. An additional aim is to evaluate whether the interactive SMS platform is superior to an SMS attention-control arm in increasing physical activity levels. The study employs a single-blind, parallel randomized controlled design. Outcome assessors are blinded to intervention assignment and masked to prior assessment data for each participant. As part of the interventions, participants learn behavioral adoption and maintenance strategies throughout the year to foster increased autonomy, prevent relapse, and promote personal, proactive problem-solving around future challenges.
In addition, to explore the potential for sustained maintenance of physical activity behaviors beyond the end of the 12-month intervention period, those participants beginning their study participation in the early stage of the trial period (N = 167) complete an additional study assessment at 18 months. During this 12- to 18-month maintenance period, participants do not receive text messages or phone counseling sessions, but have the opportunity to reach out to study staff with any questions.
2.2. Study location and participants
The study has recruited eligible participants from five counties located in the greater San Francisco Bay Area, CA. Approximately 26% of the general population across these five counties report being of Latino or Hispanic ethnicity [11]. Latino residents in the western U.S. come largely from Mexico and Central America [12]. Of those born outside the US, approximately 50% have lived here for 15 or more years.
The following study eligibility criteria have been used to enroll study participants: (a) ages 35 years and older; (b) insufficiently active [13], i.e., engaged in less than 125 min/week of moderate intensity activity such as brisk walking over the past six months, based on initial study physical activity screening items (see below), followed by a final baseline physical activity determination using the Community Healthy Activities Model Program for Seniors (CHAMPS) questionnaire [14], described further below; (c) able to safely engage in moderate forms of physical activities such as walking based on the Physical Activity Readiness Questionnaire (PAR-Q) [15]; (d) able to read and understand English or Spanish sufficiently to provide informed consent and participate in all study procedures; e) planning to live in the area for the next twelve months; f) self-reported body mass index (BMI) ≥25 and ≤ 46 kg/m2, which was based on self-reported height and weight; g) willing to modify diet by increasing vegetables, fruits, and whole grains and reducing sugars and fats; h) not pregnant, planning to become pregnant in the next year or had a newborn in the past year; and i) self-identified as Latino or Hispanic. Individuals were deemed ineligible if they answered “yes” to any of the PAR-Q screening items, to ensure participant safety given that all interventions were being delivered remotely in the community.
The study screen to determine physical activity status includes the following questions: 1) In the last three months have you regularly participated (at least two times per week) in any physical activity that has increased your breathing, such as aerobics, brisk walking, dancing, swimming, or playing sports? If the participants answered “yes”, they were asked to describe how many days per week and minutes per day they regularly exercised. These numbers are multiplied to calculate the total number of minutes per week. If the total number is 125 min or more, the individual is deemed ineligible. If the total number of minutes per week is reported as less than 125, then individuals are asked to report, in a typical or normal week over the past four weeks, the total number of minutes per week they engaged in dance, walking or hiking uphill, walking fast or briskly for exercise, and water exercises other than swimming. Individuals are deemed eligible if participation in the above exercises totals less than 125 min per week. A final determination of study eligibility based on physical activity status occurs at baseline using the full 27-item CHAMPS questionnaire to ensure that individuals' physical activity levels were commensurate with study eligibility criteria.
2.3. Study participant recruitment methods
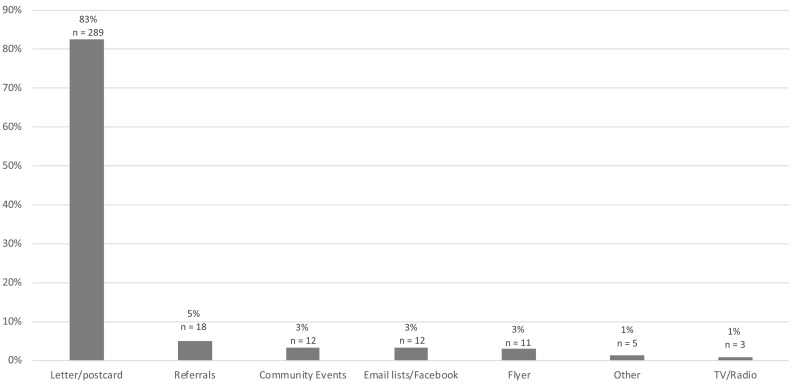
To increase external validity, three complementary recruitment methods have been employed: geographically defined targeted mass mailings, cultural media-based promotion, and community outreach [[16], [17], [18]]. For the geographically defined targeted mass mailings, mailing addresses of residents in geographically defined Census block groups in the five target counties were accessed via a private mail service company and selected based on age and Latino ethnicity. Introductory bilingual letters describing the study and business reply cards were sent to households, along with a toll-free number to call and study website link to obtain further study information and undergo initial screening for study eligibility. The media promotional methods included university and other community email lists serving primarily Latino adults, social network platforms such as Facebook, and study announcements placed in local Latino newspapers and on local Spanish television and radio stations. As part of community outreach activities, study information was placed at local community centers and was made available at local stakeholder events attended by bilingual study staff, such as health and resource fairs, back to school nights, Parent Teacher Association (PTA) meetings, local school council events, and parent group meetings, as well as local libraries, churches, local health clinics serving Latino adults, and local grocery stores [19]. Study participants and others who expressed interest in the study also were encouraged to refer others or share study information with others. The subject yield, with respect to the number of individuals who were enrolled in the trial by the different recruitment strategies across the 22-month study recruitment period, is summarized in Fig. 2 in the Results section.
Fig. 2.
Recruitment methods and study enrollment yield, by method.
2.4. Study participant screening methods
Interested individuals could complete the eligibility screen, which took approximately 15 min to complete, via study website or phone call with study staff. If eligible based on the online screen, a staff member contacted the individual to verify eligibility and schedule an orientation session. Approximately 40% of participants completed the screen online.
Those individuals judged to be initially eligible based on the telephone or web-based screen were invited to attend, depending upon where they lived, a group study orientation session at either Stanford University or a designated community center or similar location in their area. During the study orientation the study objectives and procedures were explained in further detail, all questions were answered, and interested individuals were consented and scheduled for an individual baseline assessment visit held at the same location. Participants were given multiple options for attending the initial study orientation session, including holding an individual session for them if needed. If they did not show sufficient interest to attend that important initial session, they were not able to continue in the study given that informed consent was obtained in that session.
Following the baseline assessment, those individuals found to be eligible and willing to enroll in the study were randomized to receive one of the three study interventions, followed by an initial introductory session (lasting about 30 min) for their designated intervention, typically in person but occasionally conducted by phone with research staff when an in-person meeting was unable to be scheduled.
2.5. Study participant retention methods
To promote full study understanding and sustained levels of participant retention across the 12-month intervention and assessment period, initial group-based study orientation sessions were employed following the telephone screening process and prior to baseline assessment to ensure that all individuals considering study participation were fully informed about the study objectives and expectations. This type of interactive pre-enrollment educational session has been linked with high levels of study retention in health behavior change trials lasting through 18 months [20].
2.6. Development and delivery of study interventions: conceptual overview
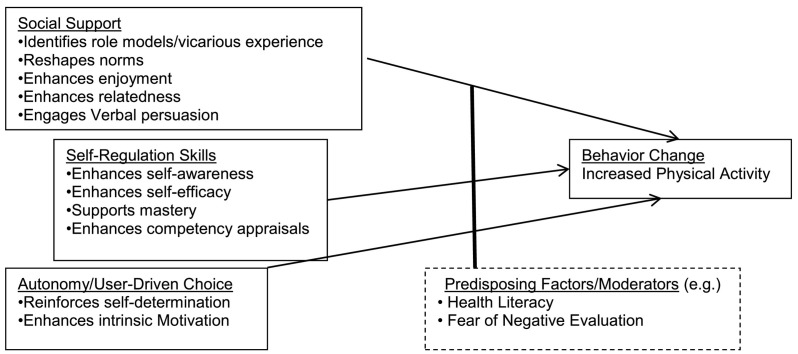
The two physical activity interventions and nutrition-control intervention are based on theoretically derived cognitive-behavioral advice and support strategies used in the evidence-based Active Choices physical activity counseling program and similar behaviorally based, evidence-supported interventions in the field [[21], [22], [23], [24]]. They are grounded specifically in Social Cognitive Theory and Self-Determination Theory (See Fig. 1 ), which emphasize individually-tailored self-management and self-regulation skill building, personalized advice and feedback, cultivation of social support, and user-driven choice/decision-making to promote feelings of autonomy and sustained behavior change [25]. Both Social Cognitive and Self-Determination Theories have explanatory power for individual-level behavior change, and have intra-individual elements that are modifiable through communication and counseling [26,27]. Substantial evidence supports these theories, which often have been found to have moderate or greater effect sizes for improving PA levels [5,28,29].
Fig. 1.
Social cognitive theory and self-determination theory elements that can increase physical activity.
As part of Social Cognitive Theory, self-regulation and social support are frequently recommended for physical activity and other health promotion interventions [26]. Self-regulation is theorized to stimulate and reinforce behavior change through the primary tools of goal setting, self-monitoring, and obtaining personalized feedback on one's performance [30]. In both Human and SMS physical activity advisor programs, participants receive simple tools (e.g., pedometers, paper tracking logs) to self-monitor physical activity. Participants assigned to the nutrition SMS intervention receive simple tools to self-monitor their food choices. Participants are asked to set physical activity goals using the FITT principle (Frequency, Intensity, Time, and Type) [31]. They are coached to compare their goals with their performance using personalized feedback from self-monitoring; this guides them to self-correct towards goal attainment.
Integral to Social Cognitive Theory, social support stimulates behavior change through vicarious experience/observation (i.e., learning by watching others do the desired behavior), verbal persuasion and encouragement from important others, and reshaping of social norms to accommodate new patterns. Participants are encouraged to name an important other who can facilitate their activity (e.g., exercise together, give reminders and words of encouragement). They also are asked to identify an inspiring role model. Participants are asked to reflect on their social and familial norms (e.g., “what does your family say about exercise?”), and reflect on how these norms can be reconciled with an active lifestyle. Derived from Self-Determination Theory, autonomous motivation has been identified as a potentially critical factor for mediating physical activity adoption [32]. According to this theory, autonomy is a core human need; satisfaction of this need facilitates development of intrinsic motivation, which is important for sustained behavior change [27]. Prior studies suggest that critical factors to increase autonomous motivation include giving people choices, empowering people to determine their own goals and intentions, and acknowledging personal difficulties encountered [33,34]. Intervention content for the three arms is summarized in Table 1 .
Table 1.
Intervention content for the three study arms.
| Table 1. Intervention Content | Human PA telephone advisor | Interactive SMS PA advisor | Interactive SMS nutrition advisor (control arm) |
|---|---|---|---|
| Program contact |
|
|
|
Self regulation:
|
|
|
|
Social support:
|
|
|
|
Autonomous motivation:
|
|
|
|
2.7. Development of the physical activity and nutrition-control SMS interventions
The two SMS interventions were developed in collaboration with CareMessage, a not-for-profit organization that builds mobile health solutions for underserved populations [[35], [36], [37], [38]]. Their patented, text message-based coaching technology enables providers to interact with patients/users through automated messages. CareMessage has content streams for physical activity and nutrition that are customizable to deliver specific messages, and, for the purposes of this study, can be varied with respect to the frequency and timing of delivery. Messages are interactive in that they ask the message receiver for answers to specific questions about goals (e.g., “Do you prefer to exercise in the morning or evening?”).
To ensure that text messages were at an appropriate reading level (i.e., 3rd-5th grade), CareMessage and HARTS lab project personnel created a database of messages for which the word count was calculated automatically. Once the optimal word count was obtained, text messages were assessed for readability by inputting the text to readable.com online software to obtain the Flesch-Kincaid grade level [39]. Messages were revised until the optimal grade level threshold or lower was achieved.
To ensure that all three interventions reflected local Latino cultural norms and values, the majority of project staff were members of the Latino community and/or had extensive experience in developing and testing communication messages and information for local Latino adults. They provided specific input during the study start-up phase to ensure that cultural norms and values were adequately reflected in all interventions (e.g., “familismo”, i.e., importance of the family in all aspects of Latino culture). Prior to program finalization, multiple focus groups at local community centers with members of the target population also were conducted to obtain feedback on study information and messages, which were incorporated into the interventions. Study materials were translated using certified medical interpreters, and pre-tested with members of the target population to ensure participant understanding.
Prior to formally initiating the On The Move Trial, a pilot study was conducted with CareMessage to test the feasibility and acceptability of SMS message content with 30 inactive Latino adults (67% women, 15 sedentary, 15 physically active; Mean age = 60.5 years; mean BMI = 31.2 kg/m2; 25% were novice text message users; 60% preferred messages in Spanish). Flesch-Kincaid grade level for the messages [39,40] averaged 3.8 (range 1.2–5.8), which indicated that average readability was between third and fourth grade education levels. With 21 texts scheduled for automated delivery over 6 weeks, 100% of messages were delivered successfully, and participants responded to 63% of the interactive messages. Response was highest (≥ 80%) for messages about social support, goal setting, and tips to avoid injury. On a scale of 1 (low) to 7 (high), participants gave average ratings of 5.7 for helpfulness and 6.4 for satisfaction. Eighty-eight percent reported that they would recommend the SMS Advisor to friends and family. The main difficulties found were texting on older phones with numeric keypads or wanting to respond free-form to multiple choice or True/False questions. These issues were readily addressed with training from study staff concerning how to utilize SMS. Baseline to post-test assessments indicated that all but one of the participants increased physical activity over the 6-week period. These data indicated the acceptability of text messaging with this target population.
2.8. Intervention fidelity and quality assurance
To maintain intervention fidelity and quality assurance in the Human PA Telephone Advisor arm, trained staff members conduct regular quality control checks and activities as has been standard with the Active Choices telephone advising program [41,42]. These activities include periodic review by senior intervention staff of Telephone Advisor logs and notes completed after each Advisor-participant session, review of the audiotapes that are collected (with participant consent) for all advising sessions, and random check-ins by study staff with study participants.
Quality assurance for the two SMS Advisor arms includes regular monitoring of system performance and backup, participant response rates, and ongoing availability of a study helpline for participants to call for assistance in correcting any problems. A designated Stanford staff member has been in regular contact (twice a month or more frequently as needed) with the CareMessage Product team to ensure that any problems that occur could be resolved in a timely manner.
The intervention staff involved in all of the study interventions have met on a weekly basis throughout the study period to engage in mutual sharing and problem-solving of their experiences and challenges with their participants of relevance to ongoing intervention engagement and study retention.
2.9. Assessment: primary outcome measure
The primary outcome is change in total weekly walking minutes across the 12-month intervention period—which represents the most appealing and easy to do physical activity in this age group [5]. For all participants, physical activity is assessed at three time points: baseline, an interim assessment at six months, and at 12 months, with the 12 -month assessment considered the primary endpoint. To provide specific information on physical activity types, the validated Community Healthy Activities Model Program for Seniors (CHAMPS) questionnaire for midlife and older adults (interview format) [14,43], available in English and Spanish, is used to assess usual weekly minutes of different types and intensities of PA over the previous 4 weeks. Such validated self-report instruments represent the most direct and reliable means for assessing the specific types of PA typically being targeted in interventions, given that device-based assessment tools (pedometers, accelerometers) capture more general movement levels beyond such purposeful PA behavior [44,45]. CHAMPS variables have been consistently associated with device-based physical activity measures in prior studies [46,47], and the CHAMPS is the only PA instrument for older adults that correlates with both doubly-labeled water-measured PA energy expenditure and accelerometers [48]. It also has been shown to be sensitive to change with moderate-intensity PA programs such as Active Choices in a variety of community samples, including Latino adults [8,22,23,42]. The proportion of each study arm meeting the national physical activity recommendations of at least 150 min/week of moderate-to-vigorous physical activity will also be evaluated [49].
2.10. Secondary outcome measures
Secondary physical activity outcomes of interest from the CHAMPS include moderate-to-vigorous physical activity (MVPA) and total physical activity levels. Physical activity measurement using the CHAMPS is accompanied by the validated Actigraph® accelerometer (model wGT3X) as a secondary activity measure at the three major assessment time points [50]. The accelerometer provides device-based information related to overall physical activity amounts and intensity (though not the types of activities in which people engage). The accelerometry protocol from a large study of 860 older adults is being applied [44]. The activity monitor is worn on the hip during waking hours for seven consecutive days at each time point, ensuring a sufficient number of days of physical activity data (at least four days is considered as complete data) commensurate with current physical activity studies in older adults [51]. Participants are instructed to wear the accelerometer for at least eight hours per day during their waking hours, commensurate with other studies aimed at expanding data inclusivity, including in underserved populations [52,53].
Wear-time validity is determined through applying the wear and non-wear time analysis and classification algorithms reported by Choi et al. [54], and analysis and interpretation of the accelerometry data is based on our prior investigations and those of other aging adult populations [55], including Copeland et al. [56].
Other secondary outcome variables of particular importance to aging Latino populations include the following: sedentary/inactive recreation behaviors, measured using a validated one-week recall survey responsive to change in older adults [57]; body mass index (BMI), derived using standard clinical assessment protocols for height and weight [43]; abdominal adiposity through waist circumference; resting blood pressure and heart rate, using standard protocols [43]; physical function, assessed with the validated two-minute step test from the Senior Fitness Test protocol [58]; and quality of life and well-being, which is being measured with two questionnaires. The first of these questionnaires is the 26-item World Health Organization (WHO) Quality of Life and self-rated health questionnaire (brief version) [59,60] which assesses perceived health and well-being related to four domains–physical health, psychological health, social relationships, and the environment. The second quality of life and well-being measure is the 76-item Stanford WELL for Life Scale, which assesses ten well-being domains, including physical health, stress and resilience, financial stability, spirituality and religiosity, purpose and meaning, sense of self, experience of positive and negative emotions, social connectedness, lifestyle behaviors, and exploration/creativity [61,62].
In addition to the above outcomes, program safety and adverse events are tracked in all three intervention arms with standardized forms and protocols used in prior physical activity and other health promotion intervention trials [23,42]. Also, overall participant acceptability ratings of the novel SMS interventions are assessed at the end of the major 12-month intervention period via the Working Alliance Inventory's 12-item bonding subscale [8,63].
2.11. Baseline moderators of intervention effects
In our prior CHAT intervention trial, which compared human vs. computerized phone advice for PA [22,64], we found that while both PA programs produced comparable average increases in PA, different factors predicted which participants responded better to the different programs [65]. Based on the human-computer literature and our own work [8,64], we evaluate key baseline moderators relevant to the human versus SMS Advisor comparison and social aspects of Latino culture, including the following: 1) Fear of Negative Evaluation: Drawn from Interpersonal Theory, persons with greater interpersonal discomfort and anxiety have been shown to perform better with computers than humans in real time [66,67] and show preference for texting over voice communication [68]. We assess this construct via Fenigstein et al.'s self-consciousness scale [69]. 2) Health Literacy and Acculturation: While both SMS and human advisor programs have been developed with accessibility by low-literate populations in mind, it is important to capture users' initial health literacy level and determine if it moderates greater or lesser success in the assigned interventions. We use the Rapid Estimates of Adult Literacy in Medicine (REALM) [70] for those who prefer English, or the Short Assessment of Health Literacy for Spanish Adults (SAHLSA-50) [71], validated based on the REALM, for those who prefer Spanish. Additionally, given that baseline levels of acculturation may impact subsequent engagement with the different interventions [[70], [71], [72]], this construct is assessed at baseline through self-reported number of years in the U.S., country of birth, and primary language spoken at home, which can be combined to reflect levels of acculturation [73]. 3) Perceived neighborhood built environments and neighborhood cohesion: In addition to the psychosocial characteristics described above, the nature of the neighborhood environments in which physical activity typically occurs can affect physical activity levels [44]. For older Latino adults, living in neighborhoods that enhance walkability as well as social contact and cohesion has been associated with greater physical activity and physical function [74,75]. It follows that those with higher neighborhood walkability as well as social cohesion may do well irrespective of program assignment, whereas those lower in walkability and social cohesion might require the additional personalized “touch” possible with the Human Telephone Advisor. These constructs are measured at baseline with the Neighborhood Environment Walkability Scale (NEWS) [76] and the Neighborhood Social Cohesion scale [77].
2.12. Potential mediators of intervention effects
To evaluate the potential mechanisms through which the interventions may exert their effects, putative mediators of intervention success are being collected at major measurement time points. They include self-efficacy for physical activity, social support, autonomous motivation (e.g., “I would exercise regularly because I feel that I want to take responsibility for my health”) and other forms of motivational self-regulation drawn from Self-Determination Theory [78], including external regulation (e.g., “I would exercise regularly because I feel pressure from other to do so”), introjected regulation (e.g., “I would exercise regularly because I would feel guilty or ashamed of myself if I did not do so”), and amotivation (e.g., “I really don't think about it”) [79]. We posit that both PA interventions will positively influence these domains and improve PA as a result. Success using self-regulatory skills is being assessed with the Exercise Goal-Setting Scale, which captures goal-setting, self-monitoring, and problem-solving, along with the Exercise Planning and Scheduling Scale [80,81]. Increased perceived support from family, friends, and the study advisor (human or SMS) is being assessed with the adapted Social Support for Exercise scale [82]. Autonomous motivation is being assessed with the Treatment Self-Regulation Questionnaire-Exercise [79].
2.13. Process evaluation measures
To assess program use, the SMS Advisor in both SMS arms automatically quantifies, for each participant, the number of texts sent, number of texts with failed delivery, and number of texts with interactive components that did/did not receive a response. The Human Advisors track and record the number of calls attempted, number of calls successfully completed, and total length of calls for each participant. These metrics will be used to assess the rate of engagement with the respective advisor. To assess program acceptance, participants complete attitudinal measures including the bonding subscale of the Working Alliance Inventory, a 12-item computer program acceptability measure [63]. To assess safety, potential adverse events are captured using a standard form from our prior work [22].
2.14. Randomization of participants to study arms
Following stratification by gender, participants have been randomly assigned, using a computerized version of the Efron procedure [83] to one of the three study arms (Human PA Telephone Advisor, interactive SMS PA Advisor, interactive SMS Nutrition Advisor). Allocation concealment was in place during the randomization process to minimize selection and similar types of allocation bias. Assessment staff members are blinded to randomization assignment and masked to prior assessment data.
2.15. Sample size calculation and data analysis plan
Sample size estimates have been developed to test the study's primary question related to whether the automated SMS Physical Activity Advisor intervention results in 12-month weekly walking increases that are similar to those achieved in the Human Physical Activity Advisor intervention. Using a two-tailed 95% confidence interval on the effect size (Cohen's d), we will evaluate how the estimated true effect size compares with a critical effect size magnitude, set a priori, reflecting the threshold of clinical significance between the two treatments, ∆. Adequate power for clinical equivalence typically requires a sample size such that there is better than 90% probability that both upper and lower bounds of the confidence interval lie within a distance of ∆ from zero when the true effect size has magnitude greater than ∆. Powering the study for clinical equivalence typically provides sufficient power to test for superiority and noninferiority as well [84].
The effect size (Cohen's d) is the standardized difference between the rates of change in total walking minutes/week over the 12-month period. The critical value of Δ is based on a clinically meaningful difference between arms of 30 min of total walking minutes per week [5] and a within-arm standard deviation of 100 (i.e., ∆ = 0.3). By enrolling approximately 140 subjects per physical activity arm and adjusting for potential attrition of 15%, a final sample size of 119 subjects per physical activity arm was determined to provide greater than 80% power to determine 12-month equivalency, as well as superiority and non-inferiority, between the two physical activity arms. Because standard imputation methods will be used for missing data in this intent-to-treat trial [85], all enrolled participants will in actuality contribute to the study analyses. Multiple imputations will be performed by replacing missing 12-month values with a set of plausible values using the option of imputation by fully conditional specification methods (ten imputations will be done). Imputation results will then be combined [85,86]. All reported outcomes will use intent-to-treat (ITT) methods. The data will be analyzed using mixed-effects linear regression models. Mixed-effects linear regression effectively addresses both missing data and early dropout in “intent-to-treat” analysis [87,88]. Similar mixed-effects linear regression techniques will be used to address the secondary outcomes of interest, e.g., intervention impacts on clinical measures, physical function, and rated quality of life and well-being variables.
We also hypothesize, as a secondary comparison, that both physical activity arms will produce significant increases from baseline to 12 months in physical activity relative to the attention-control (nutrition SMS) arm. Given that detecting a significant difference between physical activity arms and Control typically requires a smaller sample size than equivalency testing between the two physical activity arms, we have enrolled a smaller number of attention-control subjects (N = 70).
2.16. Comparative cost analysis of the two PA programs
Given the lack of cost analyses for health promotion programs generally, and particularly with respect to e-Health programs in comparison to human advisor programs, collecting such information is strongly recommended [89,90]. Planned analysis procedures to explore relative costs of the two programs are informed by cost evaluations employed by other investigators in the physical activity field as well as our prior work [[91], [92], [93]]. Program costs will be compared to outcomes (e.g., weekly walking minutes) to determine a dollar value of the program relative to the desired outcome [94]. This allows us to determine if the intervention that produces an equivalent or better outcome is less expensive to administer or, if not, to obtain estimates of the value of additional money spent (e.g., average number of dollars spent to obtain each additional minute of exercise per week). The economic trade-offs between the interventions are unclear and warrant a deeper investigation. Examination of people-related costs, scalability, and impact of the delivery channels will help inform the cost analysis. We view such analyses as preliminary, and will use them to evaluate the need for more detailed studies of the cost-effectiveness of these types of PA programs [89,92]. Based on prior literature [91,92,95], relevant costs that are tracked in each arm include the initial costs of developing/refining each intervention, and the costs of administering and participating in the programs. Tracked participation costs include frequency and length of the program advising communications and any related contacts. The time participants spend engaging in physical activity is an outcome and will not be counted among program costs.
With respect to statistical power, cost analysis studies involving phone and automated physical activity advisors are lacking. A prior center-based physical activity study that was able to compare the cost-effectiveness of two active physical activity programs had a combined sample size for the two active intervention arms (n = 235) that was smaller than the sample size in the current study [92]. Similar mixed-effects linear regression methods will be employed as described earlier.
2.17. Baseline moderator analysis
In addition to the above analyses, we plan to conduct exploratory moderator analyses following the procedures described by Kraemer et al. [96] and using mixed-effects linear regression models. The previously described moderator variables of interest (e.g., fear of negative evaluation, health literacy) will be centered and an interaction term calculated between the moderator variable and study arm assignment. Alpha will be set at 0.05 using a two-tailed test of significance for all interactions. Effect sizes will be calculated for moderation effects using Cohen's d formula [97]. Results from these analyses will inform future studies aimed specifically at a priori testing of specific moderators in this population to improve intervention response for non-responder groups [93].
2.18. Exploratory mediator analysis
As per our prior mediation work [98,99], mediator analysis will follow the general procedures first described by Baron and Kenny [100] and informed by MacKinnon [101]. After confirming intervention success in changing physical activity, mixed effects linear regression will be used to evaluate if the interventions produced significant changes in the proposed mediators, described earlier, and if the proposed mediators were associated with significant increases in physical activity. Variables meeting these criteria will be included in formal tests of mediation, which will employ mixed effects linear regression modeling to assess whether treatment effect was attenuated after accounting for its indirect effects via the mediators. Complete mediation occurs when the direct effect of treatment in achieving improvements in physical activity vanishes when controlling for the putative mediator. The single mediator approach can be generalized to multiple-mediation scenarios provided that in step two of the Baron and Kenny approach, the putative mediators are regressed simultaneously on intervention group via a multivariate normal regression model, as per Preacher and Hayes [102].
3. Results
3.1. Study participants enrolled and recruitment sources
Participant study enrollment occurred between November 2015 and September 2017. A total of 350 participants are enrolled in the trial (Human Telephone PA Advisor arm: n = 139; SMS PA Advisor arm: n = 141; SMS Nutrition Advisor Control arm: n = 70. Study participants range in age from 35 to 79 years (mean age [SD] = 52 [9] years), and 73% are women. Given that decreases in adult physical activity levels begin to emerge in the middle of the 4th decade of life for Latinos and other populations [103,104], 35 years was chosen as an appropriate lower age to begin recruiting insufficiently active midlife and older Latino individuals.
Recruitment sources for the total enrolled participant sample are shown in Fig. 2 . The highest enrollment yield (83% of enrolled participants) came from the geographically defined and demographically targeted bilingual mass mailings in the five greater San Francisco Bay Area counties being targeted (San Mateo, Santa Clara, Alameda, Santa Cruz, and Monterey counties). These letters and postcards described the study and invited persons to contact the study team by phone or online. The total number of targeted mailings sent was 342,296. The total cost of the targeted mailings recruitment strategy was approximately $165,778.
4. Discussion
The On The Move Trial is among the first studies to systematically compare the effectiveness of physical activity advice delivered by human phone advisors versus SMS messaging in underactive Latino adults. Insufficiently active Latino adults are at elevated risk for a variety of chronic diseases and conditions, yet have rarely been targeted for tailored physical activity advice and support using communication sources (i.e., human phone advisors, SMS advisors) that have heightened potential for population reach and sustainability. The inclusion of a relevant SMS attention-control arm provides further opportunities to gain insights concerning the efficacy of the two physical activity interventions in increasing 12-month physical activity levels. Additional study strengths include a suitably large sample size of approximately 140 participants in each of the two experimental arms, which should allow for the statistical evaluation of equivalence, as well as superiority and noninferiority, between these two arms; a one-year intervention period that allows for evaluation of intervention success both in the short term and longer term; measurement of an array of selected constructs of relevance as potential baseline moderators and mediators of intervention success for this understudied population; and a multi-component recruitment plan spanning five northern California counties which facilitates enrollment of a more heterogeneous and potentially generalizable study sample. As described, the especially high yield of the targeted mass mailings—a less frequently used recruitment strategy in community-based research studies—suggests that this type of recruitment strategy may be particularly useful for Latino populations. A randomized controlled physical activity trial of Latino adults of an older age than the present sample found the same superiority of the targeted mass mailing approach relative to other recruitment strategies [93]. Similarly, at least one study has shown that personalized direct mailings can increase response rates for Latino adults relative to non-targeted approaches [17]. The planned comparative cost analysis affords additional information concerning the potential implementation and translatability of the two physical activity interventions in real-world contexts.
5. Conclusion
The On The Move Trial provides a rigorous comparison of two remotely-delivered physical activity interventions that represent readily accessible, convenient, and potentially lower-cost alternatives to more standard in-person programs currently being offered in many U.S. communities. The increasing use and reach of mobile phones across the population, including lower income and underserved population segments, provides an excellent opportunity to leverage their use for physical activity promotion. Doing so may help to reduce the health disparities gap [105] while presenting a safe alternative to in-person programs in response to the COVID-19 pandemic and similar public health outbreaks. The phone-delivered interventions under study, if successful, can significantly expand the evidence-based choices that can be offered to Latino populations as well as other community members.
Authors contributions
AK: Developed, with CCS, the study investigation and design, obtained funding to support the research, provided general study oversight, including study methods development and implementation, contributed to analysis and interpretation of results, and took the lead in writing the manuscript.
IC: Contributed to study methods development and implementation, data collection, project management and quality assurance, study-related community outreach, data management and interpretation of results, edited the manuscript and approved the final version of the manuscript.
JS: Contributed to study methods development and implementation, study-related community outreach and recruitment, data collection and interpretation of results, edited the manuscript and approved the final version of the manuscript.
CCS: Developed, with AK, the study investigation and design, collaborated in obtaining funding to support the research, contributed to study methods development, management, and implementation, edited the manuscript and approved final version of the manuscript.
PRE: Contributed, with DA, to study data cleaning and data analysis and interpretation, provided edits to the manuscript, and approved the final version of the manuscript.
DG: Contributed to study methods development, implementation, data collection and quality control, edited the manuscript and approved the final version of the manuscript.
MH: Contributed to study methods implementation and data collection, including medical oversight, and approved the final version of the manuscript.
MD: Contributed to study methods implementation and data collection, and approved the final version of the manuscript.
MLP: Contributed to study data interpretation and visualization of study data, provided edits to the manuscript, and approved the final version of the manuscript.
NMP: Contributed to the build of the SMS interventions, design of the underlying technology, and edited and approved the final version of the manuscript.
CC: Contributed to the build of the SMS interventions, design of the underlying technology, and edited and approved the final version of the manuscript.
DA: Data management, statistical analysis and interpretation, and approved the final manuscript.
Declaration of Competing Interest
The authors report no competing or conflicts of interest.
Acknowledgments
This investigation was supported by US Public Health Service Grant R01DK102016 from the National Institute of Diabetes and Digestive and Kidney Diseases awarded to Dr. King. Dr. King also received partial support from US Public Health Service Grants R01CA211048 and P20CA217199 from the National Cancer Institute, R01HL11644804 from the National Heart, Lung, and Blood Institute, a grant from the Discovery Innovation Fund in Basic Biomedical Sciences from Stanford University, and US Public Health Service Grant 1U54EB020405 supporting the National Center for Mobility Data Integration and Insight (PI: S Delp). Drs. Hauser, Espinosa and Patel received support from National Institutes of Health training grant T32HL007034 (PI: C. Gardner).
We gratefully acknowledge the assistance and support of the following individuals in project activities or methods input: Jose Diaz, German Blanco, Ana Cortes, Aldo Chazaro, Isela Blanco-Velasquez, Michele Escobar, Betsy Barrera, Gustavo Chavez, Darlyne Esparza, Lidya Esparza-Rivera, Martha Gabaray, Ruby Gonzalez, John Ioannidis, MD, PhD, Alan Moreno, Cain Murguía, Randall Stafford, MD, PhD, Selene Virgen, and Sandra Winter, PhD from the Stanford University School of Medicine. We also gratefully acknowledge Ms. Ana Rosa and Rosalinda Cortez's contributions to development of the SMS interventions.
The above funding sources had no involvement in the described research, including research development, execution, analysis, interpretation of results, and write-up and submission of this paper's content and results.
Contributor Information
Abby C. King, Email: king@stanford.edu.
Ines Campero, Email: icampero@stanford.edu.
Jylana L. Sheats, Email: JSheats@tulane.edu.
Cynthia M. Castro Sweet, Email: cynthia@omadahealth.com.
Patricia Rodriguez Espinosa, Email: prespinosa@stanford.edu.
Dulce Garcia, Email: dgarcia3@stanford.edu.
Michelle Hauser, Email: mehauser@stanford.edu.
Monica Done, Email: mdone@stanford.edu.
Michele L. Patel, Email: michele.patel@stanford.edu.
Nina M. Parikh, Email: nparikh@caremessage.org.
Cecilia Corral, Email: ccorral@caremessage.org.
David K. Ahn, Email: dahn@stanford.edu.
References
- 1.U.S. Department of Health & Human Services . 2nd ed. Department of Health & Human Services; Washington, DC: U.S: 2018. Physical Activity Guidelines for Americans. [Google Scholar]
- 2.Pleis J.R., Ward B.W., Lucas J.W. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. In: Statistics NCfH, editor. Vital Health Stat. vol. 10(249) CDC; Atlanta, CA: 2010. [PubMed] [Google Scholar]
- 3.Livingston G., Minushkin S., Cohn D. Pew Hispanic Center. 2008. Hispanics and health care in the United States: Access, information and knowledge. [Google Scholar]
- 4.Silvia C.A. Barriers to physical activity in the Hispanic community. J. Public Health Policy. 2003;24(1):41–58. [PubMed] [Google Scholar]
- 5.Physical Activity Guidelines Advisory Committee . Department of Health and Human Services; Washington, DC: U.S: 2018. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. [Google Scholar]
- 6.Pew Research Center Mobile Fact Sheet. 2019. https://www.pewinternet.org/fact-sheet/mobile/;
- 7.Marquez D.X., Hoyem R., Fogg L., Bustamante E.E., Staffileno B., Wilbur J. Physical activity of urban community-dwelling older Latino adults. J. Phys. Act. Health. 2011;8(Suppl. 2):S161–S170. [PubMed] [Google Scholar]
- 8.King A.C., Bickmore T.W., Campero M.I., Pruitt L.A., Yin J.L. Employing “virtual advisors” in preventive care for underserved communities: results from the COMPASS study. J. Health Commun. Int. Perspect. 2013;18(12):1449–1464. doi: 10.1080/10810730.2013.798374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buchholz S.W., Wilbur J., Ingram D., Fogg L. Physical activity text messaging interventions in adults: a systematic review. Worldviews on Evid. Based Nurs. Sigma Theta Tau Int. Honor Soc. Nurs. 2013;10(3):163–173. doi: 10.1111/wvn.12002. [DOI] [PubMed] [Google Scholar]
- 10.Head K.J., Noar S.M., Iannarino N.T., Grant H.N. Efficacy ot text messaging-based interventions for health promotion: a meta-analysis. Soc. Sci. Med. 2013;97:41–48. doi: 10.1016/j.socscimed.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 11.U.S. Census Bureau . U.S. Census Bureau; Washington, DC: 2015. 2015 American Community Survey. In. [Google Scholar]
- 12.U.S Census Data. 2010. http://2010.census.gov/2010census/data/
- 13.Physical Activity Guidelines Advisory Committee . Department of Health and Human Services; Washington, DC: U.S: 2008. Report of the Physical Activity Guidelines Advisory Committee, 2008. [Google Scholar]
- 14.Stewart A.L., Mills K.M., King A.C., Haskell W.L., Gillis D., Ritter P.L. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med. Sci. Sports Exerc. 2001;33(7):1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Thomas S., Reading J., Shephard R.J. Revision of the physical activity readiness questionnaire (PAR-Q) Canadian J. Sports Sci. 1992;17:338–345. [PubMed] [Google Scholar]
- 16.King A.C., Harris R.B., Haskell W.L. Effect of recruitment strategy on types of subjects entered into a primary prevention clinical trial. Ann. Epidemiol. 1994;4:312–320. doi: 10.1016/1047-2797(94)90087-6. [DOI] [PubMed] [Google Scholar]
- 17.Kiernan M., Phillips K., Fair J.M., King A.C. Using direct mail to recruit Hispanic adults into a dietary intervention: an experimental study. Ann. Behav. Med. 2000;22(1):89–93. doi: 10.1007/BF02895172. [DOI] [PubMed] [Google Scholar]
- 18.Brown S.D., Lee K., Schoffman D.E., King A.C., Crawley L.M., Kiernan M. Minority recruitment into clinical trials: experimental findings and practical implications. Contemp. Clin. Trials. 2012;33(4):620–623. doi: 10.1016/j.cct.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Soto J., Campero M.I., Castro C.M., King A.C. Society of Behavioral Medicine 33rd Annual Meeting and Scientific Sessions: Rapid Communications. vol. 33. Society of Behavioral Medicine; New Orleans, LA: 2012. Lessons from recruiting Latino older adults into the LIFE trial; p. 56. [Google Scholar]
- 20.Goldberg J.H., Kiernan M. Innovative techniques to address retention in a behavioral weight-loss trial. Health Educ. Res. 2005;20(4):439–447. doi: 10.1093/her/cyg139. [DOI] [PubMed] [Google Scholar]
- 21.King A.C., Haskell W.L., Taylor C.B., Kraemer H.C., DeBusk R.F. Group- vs home-based exercise training in healthy older men and women. A community-based clinical trial. JAMA. 1991;266(11):1535–1542. [PubMed] [Google Scholar]
- 22.King A.C., Friedman R.M., Marcus B.H., Castro C., Napolitano M., Ahn D., Baker L. Ongoing physical activity advice by humans versus computers: the community health advice by telephone (CHAT) trial. Health Psychol. 2007;26:718–727. doi: 10.1037/0278-6133.26.6.718. [DOI] [PubMed] [Google Scholar]
- 23.King A.C., Castro C.M., Buman M.P., Hekler E.B., Urizar G., Ahn D.G. Behavioral impacts of sequentially versus simultaneously delivered dietary plus physical activity interventions: the CALM Trial. Ann. Behav. Med. 2013;46(2):157–168. doi: 10.1007/s12160-013-9501-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilcox S., Dowda M., Leviton L.C., Bartlett-Prescott J., Bazzarre T., Campbell-Voytal K., Carpenter R.A., Castro C.M., Dowdy D., Dunn A.L. Active for life: final results from the translation of two physical activity programs. Am. J. Prev. Med. 2008;35(4):340–351. doi: 10.1016/j.amepre.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 25.Castro C.M., King A.C. Telephone-assisted counseling for physical activity. Exerc. Sport Sci. Rev. 2002;30(2):64–68. doi: 10.1097/00003677-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Bandura A. Health promotion by social cognitive means. Health Educ. Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 27.Ryan R.M., Deci E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 28.Greaves C.J., Sheppard K.E., Abraham C., Hardeman W., Roden M., Evans P.H., Schwarz P., Group TIS Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 2011;11:119–130. doi: 10.1186/1471-2458-11-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Teixeira P.J., Carraca E.V., Markland D., Silva M.N., Ryan R.M. Exercise, physical activity, and self-determination theory: a systematic review. Int. J. Behav. Nutr. Phys. Act. 2012;9:78–107. doi: 10.1186/1479-5868-9-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bandura A. Englewood Cliffs, NJ; Prentice Hall: 1986. Social Foundations of Thought and Action: A Social Cognitive Theory. [Google Scholar]
- 31.Pescatello L.S., Arena R., Riebe D., Thompson P.D. 9th ed. Lippincott Williams and Wilkins; Baltimore: 2013. ACSM’s Guidelines for Exercise Testing and Prescription. [DOI] [PubMed] [Google Scholar]
- 32.Ryan R.M., Frederick C.M., Lepes D., Rubio N., Sheldon K.M. Intrinsic motivation and exercise adherence. Int. J. Sport Psychol. 1997;28:335–354. [Google Scholar]
- 33.Chatzisarantis N.L., Hagger M.S. Effects of an intervention based on self-determination theory on self-reported leisure-time physical activity participation. Psychol. Health. 2009;24(1):29–48. doi: 10.1080/08870440701809533. [DOI] [PubMed] [Google Scholar]
- 34.Chatzisarantis N.L., Hagger M.S., Kamarova S., Kawabata M. When effects of the universal psychological need for autonomy on health behaviour extend to a large proportion of individuals: a field experiment. Br. J. Health Psychol. 2012;17(4):785–797. doi: 10.1111/j.2044-8287.2012.02073.x. [DOI] [PubMed] [Google Scholar]
- 35.Watterson J.L., Rodriguez H.P., Shortell S.M., Aguilera A. Improved diabetes care management through a text-message intervention for low-income patients: mixed-methods pilot study. JMIR Diabet. 2018;3(4) doi: 10.2196/diabetes.8645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Axley P., Kodali S., Kuo Y.F., Ravi S., Seay T., Parikh N.M., Singal A.K. Text messaging approach improves weight loss in patients with nonalcoholic fatty liver disease: a randomized study. Liver Int. 2018;38(5):924–931. doi: 10.1111/liv.13622. [DOI] [PubMed] [Google Scholar]
- 37.Weiss C., Ammerman S.D. Designing, implementing and assessing a novel text-messaging intervention for an adolescent mobile health clinic: a collaborative approach. J. Child. Adolesc. Behav. 2016;4:299. [Google Scholar]
- 38.Cheyne K., Smith M., Felter E.M., Orozco M., Steiner E.A., Park Y., Gary-Webb T.L. Food Bank-based diabetes prevention intervention to address food security, dietary intake, and physical activity in a food-insecure cohort at high risk for diabetes. Prev. Chronic Dis. 2020;17 doi: 10.5888/pcd17.190210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cotugna N., Vickery C.E., Carpenter-Haefele K.M. Evaluation of literacy level of patient education pages in health-related journals. J. Community Health. 2005;30(3):213–219. doi: 10.1007/s10900-004-1959-x. [DOI] [PubMed] [Google Scholar]
- 40.Williamson J.M., Martin A.G. Analysis of patient information leaflets provided by a district general hospital by the Flesch and Flesch-Kincaid method. Int. J. Clin. Pract. 2010;64(13):1824–1831. doi: 10.1111/j.1742-1241.2010.02408.x. [DOI] [PubMed] [Google Scholar]
- 41.King A.C., Sallis J.F., Dunn A.L., Simons-Morton D.G., Albright C.A., Cohen S., Rejeski J., Marcus B.H., Coday M.C. For the activity counseling trial research group: overview of the activity counseling trial (ACT) intervention for promoting physical activity in primary care settings. Med. Sci. Sports Exerc. 1998;30:1086–1096. doi: 10.1097/00005768-199807000-00011. [DOI] [PubMed] [Google Scholar]
- 42.Castro C.M., Pruitt L.A., Buman M.P., King A.C. Physical activity program delivery by professionals versus volunteers: the TEAM randomized trial. Health Psychol. 2011;30(3):285–294. doi: 10.1037/a0021980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pahor M., Guralnik J.M., Ambrosius W.T., Blair S., Bonds D.E., Church T.S., Espeland M.A., Fielding R.A., Gill T.M., Groessl E.J. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014;311(23):2387–2396. doi: 10.1001/jama.2014.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.King A.C., Sallis J.F., Frank L.D., Saelens B.E., Cain K., Conway T.L., Chapman J.E., Ahn D.K., Kerr J. Aging in neighborhoods differing in walkability and income: associations with physical activity and obesity in older adults. Soc. Sci. Med. 2011;73:1525–1533. doi: 10.1016/j.socscimed.2011.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Troiano R.P., McClain J.J., Brychta R.J., Chen K.Y. Evolution of accelerometer methods for physical activity research. Br. J. Sports Med. 2014;48(13):1019–1023. doi: 10.1136/bjsports-2014-093546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Harada N.D., Chiu V., King A.C., Stewart A.L. An evaluation of three self-report physical activity instruments for older adults. Med. Sci. Sports Exerc. 2001;33:962–970. doi: 10.1097/00005768-200106000-00016. [DOI] [PubMed] [Google Scholar]
- 47.Hekler E.B., Buman M.P., Haskell W.L., Conway T.L., Cain K.L., Sallis J.F., Saelens B.E., Frank L.D., Kerr J., King A.C. Reliability and validity of CHAMPS self-reported sedentary to vigorous intensity physical activity in older adults. J. Phys. Act. Health. 2012;9:225–236. doi: 10.1123/jpah.9.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Colbert L.H., Matthews C.E., Havighurst T.C., Kim K., Schoeller D.A. Comparative validity of physical activity measures in older adults. Med. Sci. Sports Exerc. 2011;43(5):867–876. doi: 10.1249/MSS.0b013e3181fc7162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Piercy K.L., Troiano R.P., Ballard R.M., Carlson S.A., Fulton J.E., Galuska D.A., George S.M., Olson R.D. The physical activity guidelines for Americans. JAMA. 2018;320:2020–2028. doi: 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Feito Y., Bassett D.R., Thompson D.L. Evaluation of activity monitors in controlled and free-living environments. Med. Sci. Sports Exerc. 2011;44(4):733–741. doi: 10.1249/MSS.0b013e3182351913. [DOI] [PubMed] [Google Scholar]
- 51.Hart T.L., Swartz A.M., Cashin S.E., Strath S.J. How many days of monitoring predict physical activity and sedentary behaviour in older adults? Int. J. Behav. Nutr. Phys. Act. 2011;8:62–68. doi: 10.1186/1479-5868-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Evenson K.R., Wen F., Metzger J.S., Herring A.H. Physical activity and sedentary behavior patterns using accelerometry from a national sample of United States adults. Int. J. Behav. Nutr. Phys. Act. 2015;12:20. doi: 10.1186/s12966-015-0183-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Evenson K.R., Wen F., Herring A.H. Associations of accelerometry-assessed and self-reported physical activity and sedentary behavior with all-cause and cardiovascular mortality among US adults. Am. J. Epidemiol. 2016;184(9):621–632. doi: 10.1093/aje/kww070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Choi L., Liu Z., Matthews C.E., Buchowski M.S. Validation of accelerometer wear and nonwear time classification algorithm. Med. Sci. Sports Exerc. 2011;43(2):357–364. doi: 10.1249/MSS.0b013e3181ed61a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rejeski W.J., Marsh A.P., Brubaker P.H., Buman M., Fielding R.A., Hire D., Manini T., Rego A., Miller M.E., Investigators L.S. Analysis and interpretation of accelerometry data in older adults: the LIFE study. J. Gerontol. A Biol. Sci. Med. Sci. 2016;71(4):521–528. doi: 10.1093/gerona/glv204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Copeland J.L., Esliger D.W. Accelerometer assessment of physical activity in active, healthy older adults. J. Aging Phys. Act. 2009;17(1):17–30. doi: 10.1123/japa.17.1.17. [DOI] [PubMed] [Google Scholar]
- 57.Gardiner P.A., Clark B.K., Healy G.N., Eakin E.G., Winkler E.A.H., Owen N. Measuring older adults’ sedentary time: reliability, validity, and responsiveness. Med. Sci. Sports Exerc. 2011;43(11):2127–2133. doi: 10.1249/MSS.0b013e31821b94f7. [DOI] [PubMed] [Google Scholar]
- 58.Rikli R.E., Jones C.J. Development and validation of a functional fitness test for community-residing older adults. J. Aging Phys. Act. 1999;7:129–161. [Google Scholar]
- 59.World Health Organization Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL group. Psychol. Med. 1998;28(3):551–558. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 60.Skevington S.M., Lotfy M., O’Connell K.A., Group. W The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual. Life Res. 2004;13(2):299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 61.Chrisinger B.W., Gustafson J.A., King A.C., Winter S.J. Understanding where we are well: neighborhood-level social and environmental correlates of well-being in the stanford well for life study. Int. J. Environ. Res. Public Health. 2019:16(10). doi: 10.3390/ijerph16101786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Heaney C.A., Avery E.C., Rich T., Ahuja N.J., Winter S.J. Stanford WELL for life: learning what it means to be well. Am. J. Health Promot. 2017;31:449. [Google Scholar]
- 63.Horvath A., Greenberg L. Development and validation of the working alliance inventory. J. Couns. Psychol. 1989;36(2):223–233. [Google Scholar]
- 64.King A.C., Hekler E.B., Castro C.M., Buman M.P., Marcus B.H., Friedman R.H., Napolitano M.A. Exercise advice by humans versus computers: maintenance effects at 18 months. Health Psychol. 2013;33:192–196. doi: 10.1037/a0030646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hekler E.B., Buman M.P., Otten J., Castro C.M., Grieco L., Marcus B., Friedman R.H., Napolitano M.A., King A.C. Determining who responds better to a computer- vs. human-delivered physical activity intervention: results from the community health advice by telephone (CHAT) trial. Int. J. Behav. Nutr. Phys. Act. 2013;10:109–118. doi: 10.1186/1479-5868-10-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Caplan S.E. Relations samong loneliness, social anxiety, and problematic internet use. CyberPsychol. Behav. 2007;10(2):234–242. doi: 10.1089/cpb.2006.9963. [DOI] [PubMed] [Google Scholar]
- 67.HIgh A.C., Caplan S.E. Social anxiety and computer-mediated communication during initial interactions: implications for the hyperpersonal perspective. Comput. Hum. Behav. 2009;25(2):475–482. [Google Scholar]
- 68.Reid D.J., Reid F.J. Text or talk? Social anxiety, loneliness, and divergent preferences for cell phone use. CyberPsychol. Behav. 2007;10(3):424–435. doi: 10.1089/cpb.2006.9936. [DOI] [PubMed] [Google Scholar]
- 69.Fenigstein A., Scheier M.F., Buss A.H. Public and private self-consciousness: assessment and theory. J. Consult. Clin. Psychol. 1975;43:522–527. [Google Scholar]
- 70.Davis T.C., Long S.W., Jackson R.H., Mayeayx E.J., George R.B., Murphy P.W., Crouch M.A. Rapid estimate of adult literacy in medicine:a shortened screening instrument. Fam. Med. 1993;25(6):391–395. [PubMed] [Google Scholar]
- 71.Lee S.Y.D., Bender D.E., Ruiz R.E., Choi Y.I. Development of an easy-to-use Spanish health literacy test. Health Serv. Res. 2006;41:1392–1412. doi: 10.1111/j.1475-6773.2006.00532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Marin G., Sabogal F., Marin B., Otero-Sabogal R., Perez-Stable E. Development of a short acculturation scale for Hispanics. Hisp. J. Behav. Sci. 1987;9:183–205. [Google Scholar]
- 73.Sundquist J., Winkleby M. Country of birth, acculturation status and abdominal obesity in a national sample of Mexican-American women and men. Int. J. Epidemiol. 2000;29(3):470–477. [PubMed] [Google Scholar]
- 74.Brown S.C., Mason C.A., Perrino T., Lombard J.L., Martinez F., Plater-Zyberk E., Spokane A.R., Szapocznik J. Built environment and physical functioning in Hispanic elders: the role of “eyes on the street”. Environ. Health Perspect. 2008;116:1300–1307. doi: 10.1289/ehp.11160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Martinez S.M., Ayala G.X., Patrick K., Arredondo E.M., Roesch S., Elder J. Associated pathways between neighborhood environment, community resource factors, and leisure-time physical activity among Mexican-American adults in San Diego, California. Am. J. Health Promot. 2012;26(5):281–288. doi: 10.4278/ajhp.100722-QUAN-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Adams M.A., Ryan S., Kerr J., Sallis J.F., Patrick K., Frank L.D., Norman G.J. Validation of the neighborhood environment walkability scale (NEWS) items using geographic information systems. J. Phys. Act. Health. 2009;6(s1):S113–S123. doi: 10.1123/jpah.6.s1.s113. [DOI] [PubMed] [Google Scholar]
- 77.Sampson R.J., Raudenbush S.W., Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 78.Deci E.L., Ryan R.M. The support of autonomy and the control of behavior. J. Pers. Soc. Psychol. 1987;53(6):1024–1037. doi: 10.1037//0022-3514.53.6.1024. [DOI] [PubMed] [Google Scholar]
- 79.Levesque C.S., Williams G.C., Elliot D., Pickering M.A., Bodenhamer B., Finley P.J. Validating the theoretical structure of the treatment self-regulation questionnaire (TSRQ) across three different health behaviors. Health Educ. Res. 2007;22(5):691–702. doi: 10.1093/her/cyl148. [DOI] [PubMed] [Google Scholar]
- 80.Anderson E.S., Wojcik J.R., Winett R.A., Williams D.M. Social-cognitive determinants of physical activity: the influence of social support, self-efficacy, outcome expectations, and self-regulation among participants in a church-based health promotion study. Health Psychol. 2006;25(4):510–520. doi: 10.1037/0278-6133.25.4.510. [DOI] [PubMed] [Google Scholar]
- 81.Anderson E.S., Winett R.A., Wojcik J.R., Williams D.M. Social cognitive mediators of change in a group randomized nutrition and physical activity intervention: social support, self-efficacy, outcome expectations and self-regulation in the guide-to-health trial. J. Health Psychol. 2010;15(1):21–32. doi: 10.1177/1359105309342297. [DOI] [PubMed] [Google Scholar]
- 82.Sallis J.F., Grossman R.M., Pinski R.B., Patterson T.L., Nader P.R. The development of scales to measure social support for diet and exercise behaviors. Prev. Med. 1987;16:825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 83.Efron B. Forcing a sequential experiment to be balanced. Biometrika. 1971;58:403–417. [Google Scholar]
- 84.Kraemer H.C., Blasey C. 2nd ed. Sage Publications, Inc.; Los Angeles: 2016. How Many Subjects? Statistical Power Analysis in Research. [Google Scholar]
- 85.Little R.J.A., Rubin D.B. Second ed. John Wiley & Sons; New York: 2002. Statistical Analysis with Missing Data. [Google Scholar]
- 86.SAS Institute Inc . second ed. SAS Institute Inc.; Cary, NC: 2009. SAS/STAT 9.2 User's Guide. [Google Scholar]
- 87.Gibbons R.D., Hedeker D., Waternaux C., Kraemer H.C., Greenhouse J.B. Some conceptual and statistical issues in the analysis of longitudinal psychiatric data. Arch. Gen. Psychiatry. 1993;50:739–750. doi: 10.1001/archpsyc.1993.01820210073009. [DOI] [PubMed] [Google Scholar]
- 88.Laird N., Lange N., Stram D. Maximum likelihood computations with repeated measures: application. J. Am. Stat. Assoc. 1987;82:97–105. [Google Scholar]
- 89.Tate D.F., Finkelstein E.A., Khavjou O., Gustafson A. Cost effectiveness of internet interventions: review and recommendations. Ann. Behav. Med. 2009;38:40–45. doi: 10.1007/s12160-009-9131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.U.S. Department of Health and Human Services . USDHHS; Washington, DC: 2011. HHS Action plan to Reduce Racial and Ethnic Disparities: A Nation Free of Disparities in Health and Health Care. [Google Scholar]
- 91.Roux L., Pratt M., Tengs TO, Yore M.M., Yanagawa T.L., Van Den Bos J., Rutt C., Brownson R.C., Powell K.E., Heath G. Cost effectiveness of community-based physical activity interventions. Am. J. Prev. Med. 2008;35(6):578–588. doi: 10.1016/j.amepre.2008.06.040. [DOI] [PubMed] [Google Scholar]
- 92.Sevick M.A., Dunn A.L., Morrow M.S., Marcus B.H., Chen G.J., Blair S.N. Cost-effectiveness of lifestyle and structured exercise interventions in sedentary adults: results of project ACTIVE. Am. J. Prev. Med. 2000;19(1):1–8. doi: 10.1016/s0749-3797(00)00154-9. [DOI] [PubMed] [Google Scholar]
- 93.King A.C., Campero I., Sheats J.L., Castro Sweet C.M., Garcia D., Chazaro A., Blanco G., Hauser M., Fierros F., Ahn D.K. Testing the comparative effects of physical activity advice by humans vs. computers in underserved populations: the COMPASS trial design, methods, and baseline characteristics. Contemp. Clin. Trials. 2017;61(October):115–125. doi: 10.1016/j.cct.2017.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Warner K.E., Luce B.R. Health Administration Press; Ann Arbor: 1982. Cost-Benefit and Cost-Effectiveness Analyses in Health Care: Principles, Practice, and Potential. [Google Scholar]
- 95.Thomas K.S., Miller P., Doherty M., Muir K.R., Jones A.C., O’Reilly S.C. Cost-effectiveness of a two-year home exercise program for the treatment of knee pain. Arthritis Rheum. 2005;53(3):388–394. doi: 10.1002/art.21173. [DOI] [PubMed] [Google Scholar]
- 96.Kraemer H.C., Wilson G.T., Fairburn C.G., Agras W.S. Mediators and moderators of treatment effects in randomized clinical trials. Arch. Gen. Psychiatry. 2002;59 doi: 10.1001/archpsyc.59.10.877. (887–883) [DOI] [PubMed] [Google Scholar]
- 97.Rosenthal R., Rosnow R.L. 2nd ed. McGraw-Hill; New York: 1991. Essentials of Behavioral Research: Methods and Data Analysis. [Google Scholar]
- 98.Napolitano M.A., Papandonatos G.D., Lewis B.A., Whiteley J.A., Williams D.M., King A.C., Bock B.C., Pinto B., Marcus B.H. Mediators of physical activity behavior change: a multivariate approach. Health Psychol. 2008;27(4):409–418. doi: 10.1037/0278-6133.27.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Buman M.P., Hekler E.B., Bliwise D.L., King A.C. Moderators and mediators of exercise-induced objective sleep improvements in midlife and older adults with sleep complaints. Health Psychol. 2011;30(5):579–587. doi: 10.1037/a0024293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Baron R.M., Kenny D.A. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 101.MacKinnon D.P., Fairchild A.J., Fritz M.S. Mediation analysis. Annu. Rev. Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Preacher K., Hayes A. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 103.Fan J.X., Kowaleski-Jones L., Wen M. Walking or dancing: patterns of physical activity by cross-sectional age among U.S. women. J. Aging Health. 2013;25(7):1182–1203. doi: 10.1177/0898264313495561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Arredondo E.M., Sotres-Alvarez D., Stoutenberg M., Davis S.M., Crespo N.C., Carnethon M.R., Castaneda S.F., Isasi C.R., Espinoza R.A., Daviglus M.L. Physical activity levels in U.S. Latino/Hispanic adults: results from the Hispanic community health study/study of Latinos. Am. J. Prev. Med. 2016;50(4):500–508. doi: 10.1016/j.amepre.2015.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Munoz R.F. Using evidence-based internet interventions to reduce health disparities worldwide. J. Med. Internet Res. 2010;12(5) doi: 10.2196/jmir.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]