Abstract
Severe hypertriglyceridaemia is associated with pancreatitis and chronic pancreatitis-induced diabetes. Familial chylomicronaemia syndrome (FCS) is a rare autosomal recessive disorder of lipid metabolism characterised by high levels of triglycerides (TGs) due to failure of chylomicron clearance. It causes repeated episodes of severe abdominal pain, fatigue and attacks of acute pancreatitis. There are few current options for its long-term management. The only universal long-term therapy is restriction of total dietary fat intake to <10-15% of daily calories (15 to 20g per day). Many patients have been treated with fibrates and statins with a variable response, but many remain susceptible to pancreatitis. Other genetic syndromes associated with hypertriglyceridaemia include familial partial lipodystrophy (FPLD). Targeting apolipoprotein C3 (apoC3) offers the ability to increase clearance of chylomicrons and other triglyceride-rich lipoproteins. Volanesorsen is an antisense oligonucleotide (ASO) inhibitor of apoC3, which reduces TG levels by 70–80% which has been shown also to reduce rates of pancreatitis and improve well-being in FCS and reduce TGs and improve insulin resistance in FPLD. It is now undergoing licensing and payer reviews. Further developments of antisense technology including small interfering RNA therapy to apoC3 as well as other approaches to modulating triglycerides are in development for this rare disorder.
Keywords: triglyceride, pancreatitis, familial chylomicronaemia syndrome, lipoprotein lipase, chylomicron, lipodystrophy, familial partial lipodystrophy, volanesorsen
Plain Language Summary
High levels of blood fats (triglycerides) are linked to higher rates of hospital admission for stomach (abdominal) aches and especially for inflammation of the pancreas (pancreatitis). In some rare people, high levels of triglycerides are caused by defects in the genes coding for enzymes that digest large fat particles (chylomicrons) in the bloodstream or by defects that mean that fats cannot be stored in fat tissue. These fat particles contain a protein (apoC3) that controls their rate of degradation. Volanesorsen is a member of a new class of drugs that stop proteins being made and specifically blocks the making of apoC3. In clinical studies, volanesorsen has been shown to reduce blood fat levels and to reduce the severity of abdominal pain and admissions for pancreatitis.
Introduction
Hypertriglyceridaemia
Significant hypertriglyceridaemia occurs in 11% while severe hypertriglyceridaemia (Fredrickson type 5 or type 1) has an incidence of 1 in 1000.1,2 The differential diagnosis includes new uncontrolled diabetes, excess alcohol intake, and some drug therapies but many cases have a genetic component.2 Most cases of moderate (200–1000mg/dl; ≈2-10mmol/l) and severe hypertriglyceridaemia (>1000mg/dl; ≈10mmol/L) are polygenic in origin.3,4 Extreme hypertriglyceridemia requiring emergency assessment is defined as >2000mg/dl (≈20mmol/l). Monogenic conditions causing severe hypertriglyceridaemia include familial chylomicronaemia syndrome (FCS) and familial partial lipodystrophy (FPL). Any form of hypertriglyceridaemia is associated with exponentially increasing risk for developing pancreatitis rather than coronary heart disease.2 The risk of pancreatitis and CVD is significantly increased in subjects with non-fasting TG concentrations >443mg/dl (5mmol/L).5 An extreme TG group (>2000mg/dl; ~20mmol/L) has been suggested to have a 25-fold increase risk of pancreatitis6 though many cases seem to present at >3000mg/dl (35mmol/L).7
Clinical Features of Chylomicronaemia Syndrome
Familial chylomicronaemia syndrome (FCS) is a rare autosomal recessive disorder with an estimated prevalence of 1 in 1000,000.8,9 It may be more frequent as milder cases have not been genetically diagnosed.1 FCS can present in childhood or early adulthood. The presence of pancreatitis, recurrent episodes of abdominal pain, lipemia retinalis (visible intraarterial hypertriglyceridemia) or eruptive xanthomata are often considered pathognomonic for a chylomicronaemia syndrome.10 A few cases that cause a phenocopy of FCS are caused by autoimmune reactions to components of the LPL pathway.11,12
FCS has profound consequences having an increased risk of mortality and complications secondary to pancreatitis as shown in a series of 221 patients with triglyceride-induced pancreatitis13 and also on quality of life as documented in a study of 166 patients with FCS.14 The median age of FCS patients was 33 years with a median age at diagnosis of 9 years. Hospital admissions were frequent with 40% being admitted in the past year often involving stays on intensive care. Pancreatitis had occurred in 40% with a lifetime mean of 13 episodes per patient and 53% remained symptomatic for abdominal pain despite being on a strict diet. Thus, having FCS has profound effects on employment status, emotional/mental well-being, and social relationship.14,15
Lipid Biochemistry
Chylomicronaemia syndromes are caused by defects in the lipoprotein lipase (LPL) pathway for metabolism (catabolism) of triglyceride-rich lipoproteins (TGRL). LPL is required for the hydrolysis of triglycerides (TGs) in chylomicrons (CMs) and very-low-density lipoprotein (VLDL) particles. Chylomicrons contain a shortened form of apolipoprotein B (B48) made specifically in gut enterocytes while liver-synthesised VLDL contains full-length apoB (apoB100). Chylomicrons in contrast to VLDL particles seem to be pro-inflammatory in the general circulation.16,17 In patients with chylomicronaemia syndrome, the fasting plasma is turbid and if left undisturbed for several hours, CM float to the top and form a creamy supernatant layer.18 Fasting TG levels are almost invariably >1500 mg/dL (≈15mmol/L) and not infrequently rising as high as 10,000 mg/dL (≈100mmol/L) or more.4 Parallel but lesser elevations occur in cholesterol levels. While chylomicronaemia predominates, patients often have elevated plasma levels of CM remnants and some VLDL as well.19 Lipoprotein electrophoresis demonstrates a type 1 (CM) or type 5 (excess VLDL) pattern. Lipid ultracentrifugation is considered the optimal diagnostic method for chylomicronaemia and shows significant excess triglyceride in CM and/or VLDL density fractions but is not widely available. The simpler biochemical phenotype in the lipid profile is of a disproportionally raised triglyceride level compared to the apolipoprotein B100 concentration, given the relative lack of VLDL, and is used as the basis of diagnostic algorithm.20 This is caused by an excess of apolipoprotein B48 containing CM particles as opposed to apoB100 containing VLDL. Measurements used to be made of LPL activity, but these are difficult to perform and standardise so genetic diagnosis is now preferred.
Genetics of Familial Chyomicronaemia Syndrome
FCS is an inherited autosomal recessive disease caused by mutations in LPL (lipoprotein lipase) and in other genes encoding proteins required for LPL activity, such as apolipoprotein (apo) C2, apoA5, lipase maturation factor-1 (LMF-1) and glycosylphosphatidylinositol-anchored high-density lipoprotein–binding protein 1 (GPIHBP1).3 The most common cause of FCS involves mutations in the LPL gene.21 Heterozygotes with LPL variants often have moderate elevations in plasma TG levels and increased risk for CHD.22,23 ApoC2 is a required cofactor for LPL activation.24 ApoC2 deficiency results in functional lack of LPL activity and chylomicronaemia but with a less severe in phenotype than LPL mutations.25 ApoA5 facilitates the association of VLDL and chylomicrons with LPL and promotes hydrolysis of the TGs.26 GPIHBP1 is required for transport and tethering of LPL to the endothelial luminal surface and acts as an endothelial binding ligand for CMs.27
Current Treatment of FCS
Treatment for FCS involves management of both acute exacerbations of chylomicronaemia as well as chronic management to reduce the probability of destabilisation.
Acute treatment for FCS involves fasting to reduce CM production and increase natural clearance plus management of any hyperglycaemia in addition to supportive treatment for any underlying pancreatitis.28,30 Lipoprotein removal through plasmapheresis removes triglyceride-rich lipoproteins (TGRLs) acutely and is preferred to apheresis.31 Clinical algorithms for acute management of TG-related pancreatitis are available.30,31
The only universal current long-term therapy is restriction of total fat intake to less than 10–15% of daily calories (15 to 20g per day).32 This is challenging and found difficult by 90% of patients.14 It can also be ineffective in preventing chylomicronaemia and acute pancreatitis. Medium-chain triglycerides are also used in patients with FCS as these are not incorporated into CMs though are a substrate for energy metabolism.33,34 Some patients have been treated with fibrates,31,35 omega-3 fatty acids33,36 and statins37 with reasonable clinical response31 but this approach is more typically useful in multifactorial chylomicronaemia syndrome (MCS).29,38,39 This data is consistent with lipoprotein kinetics studies. Though none have been performed in patients with FCS where LPL-related particle catabolism is significantly impaired, studies in patients with hypertriglyceridaemia (Fredrickson types 2B-5) show 20–30% reductions in apoB48 particle production rates with fibrates,40 omega-3 fatty acids41 and statins42 as well as the expected effects on fractional catabolic rates. Anecdotal reports exist of the response of patients with FCS to splenectomy43 or biliary-pancreatic diversion.44
Familial Partial Lipodystrophy
Lipodystrophy syndromes are rare and can be genetic or acquired. They are characterised by variable body fat loss and associated metabolic complications, including insulin resistance, dyslipidaemias especially hypertriglyceridaemia, hepatic steatosis and atherosclerotic cardiovascular disease (ASCVD).4,45 The four main types of lipodystrophy (excluding antiretroviral therapy-induced lipodystrophy in HIV-infected patient) are the genetic types congenital generalised lipodystrophy (CGL), and familial partial lipodystrophy (FPLD),46 while acquired generalised lipodystrophy (AGL) and acquired partial lipodystrophy (APL) may have an autoimmune component and can be metabolically severe.47 FPLD is caused by mutations in multiple genes including lamin or peroxisomal proliferator activator receptor-gamma (PPAR-γ) genes and is associated with moderate degrees of fat loss, extreme insulin resistance, type 2 diabetes and significant hypertriglyceridaemia in type 2 (Dunnigan) or type 1 (Kobberling) disease.4,48,49 Studies of apoC3 inhibition have only been proposed in FPL as both fibrates and thiazolidinediones have been used in the treatment of type 2 FPLD.4
Apolipoprotein C3 as a Drug Target
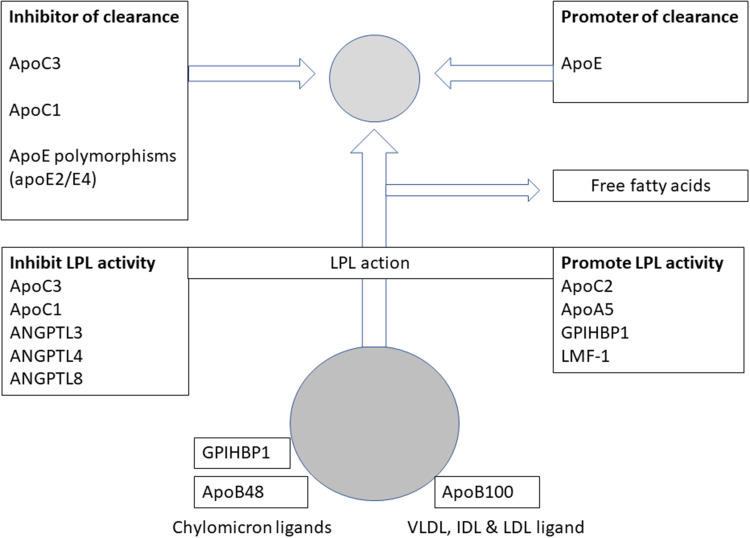
The clearance of TGRL is dependent on the activities of the LDL (apoB100/E), VLDL-receptor, LDL related protein-1 (LRP1) and apoE type 2 receptors50 and, possibly for CM in the gut, the SRB1 receptor.51 The binding of TGRL to these receptors is modulated by apoE and apoC with apoE increasing while apoC352,53 or apoC1 decreases clearance (Figure 1).
Figure 1.
Apolipoproteins and other proteins influencing the clearance of chylomicrons or very-low-density lipoprotein particles and affecting the activity of lipoprotein lipase.
Abbreviations: ANGPTL, angiopoietin-like protein; Apo, apolipoprotein; CM, chylomicron; GPIHBP1, glycosylphosphatidylinositol-anchored high-density lipoprotein-binding protein 1; LMF-1, lipase maturation factor-1.
In patients with excess triglycerides more CM and VLDL particles seem to be secreted containing apoC3 and with less apoE.54 ApoC3 may also directly regulate enterocyte metabolism of TGs.55 Deficiency of apoC3 in man is associated with hypolipoproteinaemia including reductions in triglycerides and these effects can be mimicked by antibodies to apoC3.56 Drugs such as fibrates,57,58 niacin59,60 and omega-3 fatty acids60 reduce apoC3 levels but have their principal effect on VLDL (apoB100) metabolism. Thus, reductions of apoC3 by these drugs may be secondary to VLDL turnover. ApoC3 may also directly inhibit LPL activity.61 Fibrates may also increase enterocyte apoA5 production.62 Other proteins promoting LPL activity such as LMF-1, GPIHBP-1 promote TGRL clearance while angiopoietin-like peptides (ANGPTL) retard TGRL clearance by inhibiting LPL activity.63 Thus, extensive animal, human and interventional data exist that apoC3 is a good pharmaceutical target for intervention to lower triglycerides. The evidence for the effects of apoC3 in chylomicron metabolism are less strong than for VLDL but sufficient to suggest that intervention would be efficacious in patients lacking LPL pathway function.
Chemistry and Pharmacodynamics
Volanesorsen (ISIS 304801; ISIS-ApoC-III Rx) is a second-generation 2ʹ-O-methoxyethyl (2ʹ-MOE) chimeric antisense therapeutic oligonucleotide (ASO).64 It selectively binds within the 3′ untranslated region (at base position 489–508) of apoC3 messenger ribonucleic acid (mRNA).65 This binding prevents the translation of the apoC3 mRNA and allows ribonuclease H1-mediated mRNA degradation, thereby promoting triglyceride clearance and the lowering of plasma triglyceride levels through LPL-independent pathways. These pathways include apoC3 inhibiting hepatic receptor-mediated pathways mediated by the LDLR and LRP1.65 Volanesorsen selectively reduced apoC3 mRNA in a concentration –dependent manner in human hepatoma cell line and primary human hepatocytes. As a result, administration of volanesorsen is associated with dose-dependent reductions in plasma apoC3 and a parallel reduction in triglycerides level.65
Pharmacokinetics
Volanesorsen is administered subcutaneously. In a Phase 1 clinical study on healthy volunteers, volanesorsen exhibits dose-dependent pharmacokinetics over the dose range of 50–400mg with respect to peak concentrations (Cmax) and the area under the time–concentration curve 24h after dosing (AUC0-24hr).65,66 Following subcutaneous injection across the 50–400mg dose range, peak plasma concentrations are typically reached in 2 to 4 hours and the absolute bioavailability of following a single subcutaneous administration is approximately 80% (most likely higher because an AUC of 0 to 24 hours was used and volanesorsen has a half-life of >2 weeks).67
Volanesorsen was rapidly and widely distributed to tissues from plasma with short mean residence times 6.4–8.1hrs65 and the plasma elimination half-life in the healthy volunteers receiving multiple doses of the drug ranged from 12 to 31 days with clearance primarily through urinary excretion of metabolites.68 Proof of concept with volanesorsen in FCS was demonstrated in 3 patients with FCS, following a dose of 285 mg once weekly or fortnightly, the estimated geometric mean (coefficient of variation as percentage of geometric mean) steady-state Cmax and AUC were similar while steady-state trough concentrations (Ctrough) were higher with once weekly dosing.69 The estimated steady-state volume of distribution in patients with FCS is 330L. It is highly bound to human plasma proteins (>98%) but the binding is concentration independent. It is not a substrate for cytochrome metabolism but is metabolised in tissues by endonucleases to form shorter oligonucleotides that are then degraded by exonucleases.68
Clinical Efficacy
Several clinical trials have documented the efficacy of volanesorsen in the treatment of FCS and elevated TGs.
Early Phase Clinical Trials
The phase 1 proof of concept first in human study (CS1) was conducted in 33 healthy subjects. Volanesorsen was administered on alternate days during the first week (Days 1, 3 and 5) and then once-weekly for the next 3 weeks (Days 8, 15 and 22). Treatment resulted in dose-dependent substantial reductions in apoC3 of 20%, 17%, 71%, and 78% on Day 29, 1 week after the last dose, at doses of 50, 100, 200, and 400 mg, respectively, which was associated with dose-dependent reductions in TGs of 20%, 25%, 43%, and 44%.65
Changes in triglycerides correlated with change in apoC3 (r=0.89) and 2 out of 3 subjects showed suppression of apoC3 production at the 400mg dose.
In Phase 2, randomized, double-blind, placebo-controlled, dose-response study (CS2) volanesorsen was administered weekly subcutaneously for 13 weeks in 57 subjects with severe or uncontrolled hypertriglyceridemia (randomised 41:16) and 28 on fibrate therapy (randomised 20:8)70 (Table 1). Recruitment was by TG levels 350–2000mg/dl (4–23mmol/L) in the untreated group and TG 250–2000mg/dL (3–23mmol/l) for those on fibrate-statin therapy.70 Baseline triglyceride levels in the 2 cohorts were 581±291 mg/dL (6.6±3.3mmol/L) and 376±188 mg/dL (4.2±2.1 mmol/L). ApoC3 levels were reduced in a dose-proportional manner from 100–300mg compared to a rise on placebo (Table 2). These corresponded to 31–79% reductions in TG (least squares mean) compared to a 20% rise on placebo. Similarly, when volanesorsen was added to fibrate therapy apoC3 again decreased in a dose-proportional manner from 200 to 300mg, allied with concordant reductions of 52–65% were observed in triglycerides.70
Table 1.
Response of apoC3 and Triglyceride Levels to Volanesorsen Therapy in Patients with Hypertriglyceridaemia (Study CS2)70
| Placebo | 100mg | 200mg | 300mg | Fibrate-Placebo | Fibrate and 200mg | Fibrate and 300mg | |
|---|---|---|---|---|---|---|---|
| ApoC3 Baseline (mg/dL) | 22±8 | 22±8 | 23±5 | 23±6 | 19±6 | 16±4 | 18± 6 |
| ApoC3 Treated (mg/dl) | 22± 11 | 12± 5 | 8 ±4 | 4 ±2 | 18±4 | 6±3 | 5± 2 |
| Change (least- squares mean %) | 4±8 | −39±9 | −64±8 | −80±9 | −2± 6 | −61±6 | −72± 5 |
| Triglycerides baseline mg/dl) Median & IQR | 459(356–582) | 558(351–825) | 588(464–717) | 566(355–702) | 475(253–602) | 272(230–295) | 271(241–459) |
| Triglycerides baseline (mmol/L) median & IQR | 5.2(4.02–6.58) | 6.31(3.97–9.33) | 6.64(5.24–8.10) | 6.40(4.01–7.93) | 5.37(2.86–6.80) | 3.07(2.59–3.33) | 3.06(2.72–5.19) |
| Triglycerides treated (mg/dl) Median & IQR | 456(343–640) | 277(226–394) | 180(157–262) | 120(115–185) | 338(290–394) | 120(103–172) | 116(91–191) |
| Triglycerides treated (mmol/L) Median & IQR | 5.15(3.86–7.23) | 3.13(2.55–4.45) | 2.03(1.30–2.96) | 1.36(1.30–2.09) | 3.82(3.28–4.45) | 1.36(1.17–1.94) | 1.31(1.03–2.16) |
| Change (least- squares mean %) | 20±13 | −31±15 | −59±14 | −71±15 | −8±7 | −52±7 | −65±6 |
Table 2.
Key Phase 3 Clinical Trials of Volanesorsen
| Study/Study Population | Primary Objective | Study Design | Dose(mg) | Subjects | Parameters | Placebo Baseline mg/dl (mmol/L) | Placebo On-Treatment mg/dl (mmol/l) | Volanesorsen Baseline mg/dl (mmol/) | Volanesorsen On-Treatment mg/dl (mmol/L) |
Change(%) |
|---|---|---|---|---|---|---|---|---|---|---|
| ISIS304801-CS6 (APPROACH)72 Patients with FCS |
Efficacy Safety | Randomized, Double-Blind, Placebo Controlled, | 300 mg Once weekly for 52 weeks | Volanesorsen: 33 Placebo: 33 |
TG CM-TG ApoB48 ApoB100 ApoC3 |
2152±1153 (24.3±13.0) 1785±1149 (20.2±13.0) 9.3±6.0 69.4±19.8 28.9±13.1 |
2367±1315 (26.7±14.9) 1991±1279 (22.5±14.5) 9.9±6.9 70.4±22.7 30.7±16.1 |
2267±1259 (25.6±14.4) 1913±1216 (21.6±13.7) 11.2±7.1 64.7±19.5 31.4±15.3 |
590±497 (6.7±5.6) 436±480 (4.93±5.4) 2.6±2.4 75.9±27.1 4.6±2.8 |
18 vs.-77 29 vs −83 14 vs −76± 4 vs 20 6 vs −84 |
| ISIS 304801-CS7a (APPROACH OLE)76 Patients with FCS |
Safety | Open-Label Study. | 300 mg Once weekly for 52 weeks |
Volanesorsen: 67 50 naïve 14 CS6 continuing 3 CS16 continuing |
Naïve TG CS6 TG CS16 TG |
2317±1993 (26.1±22.5) 2641±1228 (29.8±13.9 2288±1524 (25.9± 17.2 |
979±683 (11.1±7.7) 1248±927 14.1±10.5) 1558±193 17.6±2.2) |
−47 –55 -39 |
||
| ISIS 304801-CS16b (COMPASS)76 Patients with Hypertriglyceridaemia |
Efficacy Safety |
Randomized, Double-Blind, Placebo Controlled, | 300 mg Once weekly for 26 weeksc |
Volanesorsen: 75 (5 FCS) Placebo: 38 (2 FCS) |
TG | 1414±1253 (16.0±14.2) |
1406±1409 (15.9±15.9) |
1183±759 (13.4±8.6) |
294±245 (3.3±2.8) |
−1 vs −71 |
Notes: aThis is an open-label extension (OLE) study in patients from CS6, CS16, or newly included patients. Data at 6 months. bIncluded patients with FCS. cFor CS16, the protocol was amended so that patients that had not already completed ≥5 months of dosing as of 27 May 2016 had dose frequency reduced to 300 mg every 2 weeks or dose reduced to 150 mg per week after 13 weeks of treatment. A total of 39 patients had their dose or frequency of dosing changed as a consequence of this amendment.
In a subgroup of the main phase 2 study, 3 patients with FCS and triglyceride levels ranging from 1406 to 2083 mg/dL (16–24 mmol/L) received volanesorsen for 13 weeks. Plasma apoC3 levels were reduced by 71–90% and TGs by 56–86% and all patients achieved a TG<500 mg/dL (5.7mmol/L).69
Phase 3 Clinical Trials
Approach (CS6)
The CS6 (APPROACH) phase 3 study evaluated the efficacy and safety of volanesorsen in 66 adult patients with TG>750mg/dl (8.48mmol/L) with clinical FCS from 130 patients screened and forms the key evidence for volanesorsen (Table 2). In the randomised cohort, 41 patients were homozygous or compound heterozygotes for 25 different inactivating mutations in LPL, and 11 patients had biallelic mutations in accessory proteins or were double heterozygous for LPL and APOA5 or LMF1 mutations while 14 patients did not have identifiable mutations. They were randomized 1:1 to 52 weeks of weekly subcutaneous volanesorsen (285mg) or placebo.71,72 Patients underwent a diet stabilization run-in period comprising <20g fat per day and mandatory alcohol restrictions before randomisation.
The final endpoint was met with a 94% reduction (1804mg/dl: 20.4mmol/L) in TG at 3 months. In the volanesorsen group, TG levels were reduced by 53% at 6 months and 40% at 12 months. The apparent decrease in efficacy was likely driven by dose adjustments and discontinued patients as continued TG measurements were required by the study protocol. Among patients with baseline TG>750mg/dL (8.48mmol/L), 77% vs 10% of patients were classified as responders by achieving this level on treatment. Over 12 months, this occurred in 60% of patients on weekly dosing and 46% of patients on fortnightly dosing schedules compared to 7% of patients on placebo. Adequate response defined as >40% reduction in TGs (based on the efficacy of fibrates) was achieved by 88 vs 9% patients (p < 0.0001). ApoC3 levels were reduced by 84% compared with a 6% increase on placebo at 3 months. In the treated group CM TGs were reduced by 83%, apoB48 by 76%, non–HDL-cholesterol (nHDL-C) by 46%, and very-low-density lipoprotein (VLDL)-cholesterol by 58% while HDL-C increased by 46%, and apoA1 by 14%. LDL-C increased by 136% and apoB by 20% indicating significant increased throughput in the apoB100 pathway. The effect of volanesorsen on TGs was independent of the genetic diagnosis as TG levels decreased by 65% in the 17 patients with mutations in LPL and 75% in 9 patients with non-LPL defects.
A composite endpoint for pancreatitis and pain was used for clinical efficacy. Adjudicated acute pancreatitis and abdominal pain occurred in 12 (36%) patients in the volanesorsen group and 13 (39%) patients on the placebo group comprising 2.73 vs 2.04 events/year (p=0.62). Pancreatitis was observed in 4 patients on placebo in the study and none on volanesorsen treatment though 1 patient had an attack 9 days after the last study dose. A post hoc analysis was conducted in patients with at least 2 episodes of pancreatitis in the previous 5 years. Prior rates of 24 events in 7 patients (volanesorsen) vs 17 events in 4 patients (placebo) changed to zero events on volanesorsen and 4 events in 3 patients on placebo (p=0.02). Self-reported abdominal pain intensity was reduced in the volanesorsen-treated patients (score −2.3 (n=7) vs.-1.3 (n=10); p=0.03).38
Compass (Cs16)
The COMPASS trial investigated the efficacy and safety of volanesorsen in 113 patients with hypertriglyceridemia defined as fasting TG>500mg/dl (5.65mmol/L).73 Recruitment TG levels were far higher at 1261±955mg/dl (14.3±10.8mmol/L). Patients were randomised to volanesorsen: (n= 75 including 5 FCS) or placebo (n=38; 2 FCS). All 114 participants (113 dosed) received volanesorsen 285 mg once per week (or less frequently) depending on safety or tolerability reasons. Preliminary results show that after 3 months of treatment TGs were reduced by 73±17% in the volanesorsen group compared with 2±53% on placebo corresponding to 1869md/dL (9.8mmol/l) reduction. The 7 patients with FCS had a baseline TG 2280±973mg/dL (25.8±11.0mmol/L) and achieved a similar 74±14% TG reduction. Pancreatitis events were reduced with volanesorsen therapy (0 vs 6; p=0.01) but 1 patient on volanesorsen had pancreatitis 3 months after the last dose.
Extension Study
An ongoing multi-centre phase 3 open-label extension (OLE) of treated subjects includes patients from the CS6 (APPROACH), CS16 (COMPASS index study) and a group of FCS patients who could have been potentially recruited (CS7) is ongoing.67 Combined data from COMPASS and APPROACH studies showed a reduction in pancreatitis events with 1 event on volanesorsen (1 patient) compared with 9 events (6 patients) on placebo (p=0.02).74 TG levels in the APPROACH and COMPASS were reduced by 49% and 65% at 3 months, 55% and 43% at 6 months, and 35% to 40% at 12 months of the OLE study compared to baseline values in the original studies. Reductions in TG (38% and 39%) were maintained up to 18 months. Patients not previously treated with volanesorsen achieved similar reductions in TG levels ranging from 60% to 32% from months 3 to 12.
A global retrospective study of a subset of patients from the APPROACH-OLE extension phase (ReFOCUS study; n=22) reported improvements in disease burden after volanesorsen therapy (median 222 days).75 More patients reported effective management of FCS symptoms after 3 months of treatment compared to before (19 vs 40%). Almost all reported that their symptoms were controlled with diet (90 vs 55%) after treatment. The number of FCS symptoms was reduced after 3 months of treatment with volanesorsen (median 6.5 vs 3.5; p<0.05). Reductions were seen in physical (47%, p=0.009), emotional (47%; p=0.007) and cognitive manifestations (46%; p=0.03) but not in pancreatitis admissions. Patients also reported improvements in their personal, social and professional lives with more patients reporting “no interference” (5% to 23%) and fewer patients reporting high levels of interference (59% to 37%).75 Overall this suggests an improvement in quality of life with treatment.
Safety and Tolerability
As is typical in phase 3 studies, many patients treated with volanesorsen experienced an adverse event (AE) across the programme.67 The most common were events related to local tolerability and decreases in platelet counts.76 In the APPROACH (CS6) study an injection site reaction (ISR) was reported by 61% of patients (12% of total drug injections) with volanesorsen compared with none on placebo. One patient withdrew due to an ISR.
The most common reason for discontinuation of volanesorsen treatment in APPROACH (CS6) was due to adverse events (9 patients, 27%) with 5 patients stopping due to platelet reductions and 4 for other reasons. Confirmed low platelet counts (<140 x109/L) were observed in 25 patients (76%) with volanesorsen and in 8 patients (24%) on placebo while levels <100 x 109/L were found in 16 patients (48%) on volanesorsen and none in patients who received placebo. Two patients developed severe thrombocytopaenia (<25 x 109/L) and discontinued treatment in mid-study. Neither had any bleeding. Platelet levels recovered after 23–33 days following steroid/immunoglobulin therapy. Investigators withdrew 3 other patients from the study for less severe thrombocytopaenia.
In the original CS6 protocol, treatment interruption followed by restarting at the original dose of study drug (300 mg/week) was the only permitted option for managing a platelet decline, other than discontinuing treatment. Patients withdrew from the study if they had a second decline in platelets. The platelet monitoring regime and dose adjustment were changed in mid-study. The rate of treatment discontinuations due to platelet reductions, and discontinuations for any reason, were higher before the change in the platelet monitoring and dose adjustment algorithm. No platelet counts <50 x 109/L were observed in CS6 after the protocol change. In the volanesorsen group, 30% of patients reduced their dosing to fortnightly (weeks 26 and 46) and 33% had dose interruptions because of adverse events or laboratory values mostly due to platelet reductions. Apart from ISRs and low platelets in CS6, the frequencies of nausea, weakness, myalgia or arthralgia, diarrhea, nose bleeds (epistaxis) and hyperglycaemia (diabetes) were higher in the volanesorsen-treated group.
Aggregated Safety Results
Across the studies, 75% of the AEs were mild in severity, with abdominal pain, nasopharyngitis, fatigue and headache being the most common (>15). Most volanesorsen-treated patients (82%) in the APPROACH and its OLE experienced ISRs persisting longer than 2 days with at least one symptom of pain, erythema, pruritus or local swelling. These typically occurred early in treatment with a median time to a diagnosed ISR of 4.3 weeks.76 In the COMPASS (CS16) study an ISR occurred with 24% of volanesorsen injections. No serious platelet reduction events were seen in the study though one potential SAE of serum sickness occurred 2 weeks after the last study dose.
Across all studies in FCS, in-study discontinuations were recorded by 10 patients receiving volanesorsen across the studies based on multiple AEs at the injection sites; discomfort, pruritus, rash, warmth (1 patient each), discolouration, oedema, (2 patients each), swelling (3 patients), erythema and pain (7 patients each).77
Serious Adverse Events in the Aggregated Studies
Serious adverse events (SAEs) were reported in 13% patients with volanesorsen treatment. Three SAEs in 3 (3%) patients were considered treatment-related and included 2 reports of thrombocytopenia (<25 x 109/L) (APPROACH) and a report of serum sickness (COMPASS). Several moderate severity SAEs were reported in APPROACH including abdominal pain (adjudicated as pancreatitis), cholangitis, drug-induced liver injury (following diclofenac), ankle fracture and dehydration. These were seen in one patient (3%) each. In the ongoing APPROACH-OLE, 13 patients (19%) (10 treatment naïve, and 3 previously treated) reported a serious adverse event (SAE).77 During these studies, 4 cases of pancreatitis and 1 case of proteinuria were observed. Events of juvenile idiopathic arthritis, reduced platelet count or severe thrombocytopenia and proteinuria were considered related to study drug.76 Treatment was discontinued due to severe thrombocytopaenia in 4 patients.
Anti-drug antibodies were reported positive in 16% and 30% of volanesorsen-treated patients in the APPROACH and COMPASS studies, respectively, but were not associated with safety concerns or reduced drug efficacy based on the limited data available.76
Familial Partial Lipodystrophy (BROADEN)
A study of the efficacy of volanesorsen was conducted in 15 patients with FPLD with moderate glycaemic control (HbA1c>7.5% (58mmol/mol)) and hypertriglyceridaemia (200–500mg/dl; 2.26–5.65mmol/L).78 Patients were randomized (2:1) to weekly subcutaneous treatment with 300 mg of volanesorsen or placebo for 13 weeks in a phase 2 study. Volanesorsen treatment decreased apoC3 by 88% and TG levels by 69% with an increase HDL-C of 42%. Insulin sensitivity improved by 50% and HbA1c decreased by 3.4 mmol/mol (0.44%) paralleling changes in fructosamine and glycated albumin. Changes in insulin resistance correlated with reductions in apoC3 (r =−0.61, p=0.03) and TGs (r = −0.68, p=0.01). The majority of adverse events reported were mild and no discontinuations occurred.
Discussion
Volanesorsen
The observational relationship between severe hypertriglyceridemia, particularly chylomicronaemia, and acute pancreatitis is well established. Patients with FCS have many documented complications from sustained chylomicronaemia, including commonly acute pancreatitis.4,20,28,39 This condition is an orphan disorder with a poor response to many current treatments. The clinical studies with volanesorsen have demonstrate a profound impact on the chosen surrogate outcomes of reductions in apoC3 and triglyceride levels (30–70%) which are maintained up to 18 months.72 These were accompanied by improvements in patient well-being75 and a reduction in the rate of pancreatitis events though none of the studies were powered for this endpoint and all comparisons made either involved short-term trial data or were with retrospective patient-matched case records.74
The volanesorsen studies have also shown a high rate of discontinuation (up to 30%), problems with injection site reactions. Platelet levels have also been a problem in these studies. In the CS6 APPROACH study, a number of patients had initially low platelet levels but this was not seen in the other volanesorsen trials. Furthermore, volanesorsen treatment was associated with an unpredictable poorly understood side-effect of thrombocytopaenia that has required dose interruption, change of administration schedules or drug discontinuation. The time course of thrombocytopaenia seemed to indicate a chronic effect possibly correlated with drug accumulation as it responded in many cases to dose interruption. Whether this is a compound or target (apoC3) specific effect is unclear. Cases of thrombocytopenia and bleeding have also been recorded with niacin which also reduces triglyceride and apoC3 levels79,80 but also with other ASOs with similar structural characteristics to volanesorsen such as inotersen (an ASO to transerythretin used to treat amyloidosis).81 The effect may be related to an underlying immune dysfunction.81
Protocols for volanesorsen administration have been modified after the initial phase 3 studies to include a reduction in dosing to fortnightly after an initial weekly administration loading phase and an additional mandatory requirement for long-term platelet monitoring. The recommended starting dosage is 285 mg once weekly for 3 months, followed by down-titration to a maintenance dosing schedule of once every 2 weeks. If a 25% reduction in TG levels is not achieved, or if TG remain >2000 md/dl (22.6 mmol/L) at 3 months, treatment should be stopped.
Regulatory authorities have taken differing views of the data available on 312 patients of whom 248 were treated with volanesorsen. This includes 86 patients with FCS. The US Food and Drug Administration (FDA) refused to approve volanesorsen for the treatment of patients with FCS based on safety issues of thrombocytopaenia and risks of bleeding (8/2018).82 In contrast, the European Medicines Agency (EMA) (02/2019) gave conditional marketing authorization of the drug for patients with confirmed FCS who are at high risk of pancreatitis in whom there is inadequate response to TG reduction therapy and diet provided that extra data were gathered in a registry study.76 All these bodies noted differences in the dose requested for approval compared to that used in the phase 3 studies and that randomised controlled trial data on the efficacy and safety data for the new lower proposed dose were lacking. Thus, they requested additional registry data on safety and efficacy is gathered on patients continuing on volanesorsen.
Among payer organisations, the National Institute for Health and Care Excellence (NICE) in the UK (1/2020) performed a systematic review of the evidence base for FCS, its consequences and the cost-effectiveness of volanesorsen.83 NICE noted that uncertainty existed about the relationship of the rate of recurrent acute pancreatitis in FCS with TG levels as some patients with FCS experience pancreatitis events at lower TG levels than those seen in patients with raised TGs from other causes. Hospital admissions data in FCS are also not completely reliable as many patients self-manage to avoid admission by fasting when they recognise symptoms of pancreatitis so admission events likely only represent the most serious events. The composite endpoint of pancreatitis admissions and abdominal pain attempted to compensate for this but adds a substantial subjective component- the use of days fasting (or nil by mouth on admission) might have been better. The design of the pivotal efficacy trial (APPROACH) allowed entry of patients who had previously received alipogene tiparvovec over 2 years before71 and 11% of patients recruited had previously received this gene therapy. Steroid, niacin or antipsychotic therapy were contra-indications to recruitment. The inclusion of alipogene-tiparvovec-treated patients may have reduced the rate of pancreatitis seen in the CS6 study thus understating its true effects.84
The long-term effectiveness of volanesorsen was also unclear as a diminution of response seen in APPROACH-OLE compared to the APPROACH study. This was further complicated by its design as a self-selected admixed sub-study compromised by high rates of drug discontinuation in the original study. The draft guidance from the highly specialised therapies (orphan diseases) did not recommend volanesorsen for use in the National Health Service in England for treating FCS at its suggested marketed price as its cost-effectiveness exceeded the £100,000/year quality-adjusted life year (QALY) threshold used by this committee. Further negotiations are underway about patient access schemes. Patients are already receiving volanesorsen in some countries based on compassionate use (USA) or early access to medicines schemes (UK).
The current programme for volanesorsen may be superseded by new developments. Tolerability has been noted to be a problem with ASOs and a new liver-targeted technology based on high first-pass liver extraction (through the asialoglycoprotein receptor) of modified small interfering RNA molecules may allow doses of active agents to be reduced while preserving efficacy and reducing adverse events.85 AKCEA-APO-CIII-LRx is a third-generation ligand-conjugated antisense (LICA) drug comprising an ASO to apoC3 with a N-acetylgalactosamine-containing adduct (GalNac) to increase first-pass hepatic clearance. The LICA technology may lower the risk of thrombocytopenia given its higher tissue selectivity and more flexible dosing possibilities including lower dose options due to its longer half-life.86 A dose-ranging study of 10, 30, 60, 90, or 120 mg of AKCEA-APOCIII-LRx in healthy volunteers showed reductions of 0, 42%, 73%, 81%, and 92% in apoC3, and 12%, 7%, 42%, 73%, and 77% in TGs after 14 days. In a multiple-dose study, patients received 15mg and 30mg weekly or 60mg every 4 weeks. Reductions of 66%, 84%, and 89% in apoC3, and 59%, 73%, and 66% in TGs were observed 1 week after the last dose had been administered. A placebo-controlled trial of IONIS-APO-CIII-LRx (ISIS 678354) for reduction of TGs in patients with hypertriglyceridaemia is underway. This modification may provide a solution to safety concerns about volanesorsen.
Therapeutic Competitors
A number of other therapeutic approaches have been taken to treat patients with FCS.
Gene therapy using an adeno-associated virus (AAV) vector and intra-muscular injection allied with short-term immunosuppressive therapy has been tried. Alipogene Tiparvovec (Glybera) had to dose at its maximum available dose and reduce total triglycerides transiently but had greater effects on new CM production. It showed up to a 50% reduction in pancreatitis events after 2 years.84,87 Its effectiveness was restricted to patients with LPL mutations and administration involved multi-point intra-muscular injections under general anaesthetic allied with temporary immunosuppressant therapy. It had a high front-end costs of 1,000,000 Euro per patient with a planned 5-year payment model.88,89 After 1 patient had been treated in Europe, this therapy was discontinued on commercial grounds.
As upregulation of apoC2 seems to inhibit the action of apoC3, a novel apolipoprotein-derived peptide therapeutic has been devised as an apoC2 mimetic (D6PV).90 This peptide reduced TG by 80% in both apoC2-deficient mice and human apoC3-transgenic mice. In hApoC3-Tg mice, D6PV reduced apoC3 by 80% and apoB by 65%. Whether this mimetic peptide is capable of use in man remains to be determined.
Previous studies have investigated therapies that interfere with cholesterol and triglyceride loading of CM and VLDL precursors. Lomitapide, a microsomal triglyceride transfer protein (MTP) inhibitor, is licensed for treatment of homozygous familial hypercholesterolaemia (HoFH) but is known to cause hepatic dysfunction.91 One patient with FCS was treated with lomitapide for 13 years achieving a 75% reduction in TGs, a reduction in pancreatitis admissions but unfortunately developed hepatic fibrosis.92 A different approach has been to inhibit intra-cellular triglyceride synthesis from diglyceride precursors which is a feature of CM and VLDL production. Pradigastat (LCQ908) is a diacyl-glycerol-acyl transferase-1 (DGAT-1) inhibitor. A phase 2 study of 6 patients with FCS using 10–40mg pradigastat showed that the 20mg and 40mg doses reduced TGs by 33% and 54%.93 This effect was driven by reductions in post-prandial TGs, CM production and apoB48 levels. No significant excess adverse events were seen over the 3-week study but this drug does not seem to have progressed in development.
Alternative drug targets in FCS include ANGPTL3 and ANGPTL4. ANGPTLs regulate triglyceride metabolism63 and loss of function variants and patients homozygous for ANGPTL3 deficiency are associated with lower TG levels and reduced rates of cardiovascular disease.94,95 Both ASO (AKCEA-ANGPTL3-LRx) and antibody interventions (evinacumab) have been developed with ASOs showing reductions of 33–60% in dose-ranging studies.96 Evinacumab, an anti-ANGPTL3 antibody, has been shown to reduce cholesterol in HoFH97 and is now in trial in patients with FCS as it reduced triglycerides by up to 76% in initial studies.94 In a dose-ranging study in patients with hypertriglyceridaemia evinacumab reduced TGs by 77% at 10mg/kg and 83% at 20mg/kg. Further studies are now underway with evinacumab. Other approaches to targeting ANGPTL include Clustered Regularly Interspaced Short Palindromic Repeats; CRISPR-associated protein-9 (CRISPR/Cas9) gene inactivation.98
In FPLD alternatives to volanesorsen treatment also exist. Some patients respond to new higher dose insulin formulations4,49 while specific adipocyte hormone therapies such as metreleptin which directly target the dysfunctional adipocytes may have a role.99
Conclusion
Familial chylomicronaemia syndrome is on orphan disorder where current treatment is inadequate and health burdens caused by pancreatitis are high. Inhibition of apoC3 using the ASO reduces triglyceride levels by up to 77% and rates of pancreatitis while improving well-being. Its adverse effect profile including a high rate of injection site reactions and especially its unpredictable adverse effect of causing thrombocytopaenia has led to modifications in its approved dosing schedule that have so far limited its approval outside of compassionate use. Further developments in ApoC3 inhibition may result in improved safety-efficacy profiles and other approaches to FCS are also in early trials. It is likely that FCS will become a treatable disorder in the near future.
Disclosure
Professor Wierzbicki has chaired lipid and other guideline groups at the National Institute for Health and Clinical Excellence (NICE) and was an external specialist adviser for the review of volanesorsen (ID1326). He was also an external specialist assessor of volanesorsen for the European Medicines Agency (EMA). The views expressed in this article are his own and do not represent those of NICE or the EMA. He is a site investigator for studies of volanesorsen and evinacumab in FCS. The authors report no other conflicts of interest in this work.
References
- 1.Christian JB, Bourgeois N, Snipes R, Lowe KA. Prevalence of severe (500 to 2000 mg/dl) hypertriglyceridemia in United States adults. Am J Cardiol. 2011;107(6):891–897. doi: 10.1016/j.amjcard.2010.11.008 [DOI] [PubMed] [Google Scholar]
- 2.Rashid N, Sharma PP, Scott RD, Lin KJ, Toth PP. Severe hypertriglyceridemia and factors associated with acute pancreatitis in an integrated health care system. J Clin Lipidol. 2016;10(4):880–890. doi: 10.1016/j.jacl.2016.02.019 [DOI] [PubMed] [Google Scholar]
- 3.Dron JS, Wang J, Cao H, et al. Severe hypertriglyceridemia is primarily polygenic. J Clin Lipidol. 2019;13(1):80–88. doi: 10.1016/j.jacl.2018.10.006 [DOI] [PubMed] [Google Scholar]
- 4.Chait A, Eckel RH. The chylomicronemia syndrome is most often multifactorial: a narrative review of causes and treatment. Ann Intern Med. 2019;170(9):626–634. doi: 10.7326/M19-0203 [DOI] [PubMed] [Google Scholar]
- 5.Pedersen SB, Langsted A, Nordestgaard BG. Nonfasting mild-to-moderate hypertriglyceridemia and risk of acute pancreatitis. JAMA Intern Med. 2016;176(12):1834–1842. doi: 10.1001/jamainternmed.2016.6875 [DOI] [PubMed] [Google Scholar]
- 6.Gaudet D, de Wal J, Tremblay K, et al. Review of the clinical development of alipogene tiparvovec gene therapy for lipoprotein lipase deficiency. AtherosclerSuppl. 2010;11(1):55–60. doi: 10.1016/j.atherosclerosissup.2010.03.004 [DOI] [PubMed] [Google Scholar]
- 7.Lloret Linares C, Pelletier AL, Czernichow S, et al. Acute pancreatitis in a cohort of 129 patients referred for severe hypertriglyceridemia. Pancreas. 2008;37(1):13. doi: 10.1097/MPA.0b013e31816074a1 [DOI] [PubMed] [Google Scholar]
- 8.Chyzhyk V, Kozmic S, Brown AS, et al. Extreme hypertriglyceridemia: genetic diversity, pancreatitis, pregnancy, and prevalence. J Clin Lipidol. 2019;13(1):89–99. [DOI] [PubMed] [Google Scholar]
- 9.Pallazola VA, Sajja A, Derenbecker R, et al. Prevalence of familial chylomicronemia syndrome in a quaternary care center. Eur J Prev Cardiol. 2019;2047487319888054. [DOI] [PubMed] [Google Scholar]
- 10.Brunzell JDBE, Bierman EL. Chylomicronemia syndrome. Interaction of genetic and acquired hypertriglyceridaemia. Med Clin North Am. 1982;66(2):455–468. doi: 10.1016/S0025-7125(16)31430-4 [DOI] [PubMed] [Google Scholar]
- 11.Beigneux AP, Miyashita K, Ploug M, et al. Autoantibodies against GPIHBP1 as a Cause of Hypertriglyceridemia. N Engl J Med. 2017;376(17):1647–1658. doi: 10.1056/NEJMoa1611930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brunzell JD, Miller NE, Alaupovic P, et al. Familial chylomicronemia due to a circulating inhibitor of lipoprotein lipase activity. J Lipid Res. 1983;24(1):12–19. [PubMed] [Google Scholar]
- 13.Vipperla K, Somerville C, Furlan A, et al. Clinical profile and natural course in a large cohort of patients with hypertriglyceridemia and pancreatitis. J Clin Gastroenterol. 2017;51(1):77–85. doi: 10.1097/MCG.0000000000000579 [DOI] [PubMed] [Google Scholar]
- 14.Davidson M, Stevenson M, Hsieh A, et al. The burden of familial chylomicronemia syndrome: results from the global IN-FOCUS study. J Clin Lipidol. 2018;12(4):898–907 e2. doi: 10.1016/j.jacl.2018.04.009 [DOI] [PubMed] [Google Scholar]
- 15.Chyzhyk VKS, Brown AS, Brown AS, et al. Extreme hyperglyceridemia: genetic diversity, pancreatitis, pregnancy and prevalence. J Clin Lipidol. 2019;13(1):89–99. doi: 10.1016/j.jacl.2018.09.007 [DOI] [PubMed] [Google Scholar]
- 16.Julve J, Martin-Campos JM, Escola-Gil JC, Blanco-Vaca F. Chylomicrons: advances in biology, pathology, laboratory testing, and therapeutics. Clin Chim Acta. 2016;455:134–148. doi: 10.1016/j.cca.2016.02.004 [DOI] [PubMed] [Google Scholar]
- 17.de Vries MA, Klop B, Alipour A, et al. In vivo evidence for chylomicrons as mediators of postprandial inflammation. Atherosclerosis. 2015;243(2):540–545. doi: 10.1016/j.atherosclerosis.2015.10.025 [DOI] [PubMed] [Google Scholar]
- 18.Tremblay K, Methot J, Brisson D, Gaudet D. Etiology and risk of lactescent plasma and severe hypertriglyceridemia. J Clin Lipidol. 2011;5(1):37–44. doi: 10.1016/j.jacl.2010.11.004 [DOI] [PubMed] [Google Scholar]
- 19.Bjornson E, Packard CJ, Adiels M, et al. Apolipoprotein B48 metabolism in chylomicrons and very low-density lipoproteins and its role in triglyceride transport in normo- and hypertriglyceridemic human subjects. J Intern Med. 2019;7:548. [DOI] [PubMed] [Google Scholar]
- 20.Stroes E, Moulin P, Parhofer KG, Rebours V, Lohr JM, Averna M. Diagnostic algorithm for familial chylomicronemia syndrome. Atheroscler Suppl. 2017;23:1–7. doi: 10.1016/j.atherosclerosissup.2016.10.002 [DOI] [PubMed] [Google Scholar]
- 21.D’Erasmo L, Di Costanzo A, Cassandra F, et al. Spectrum of mutations and long-term clinical outcomes in genetic chylomicronemia syndromes. Arterioscler Thromb Vasc Biol. 2019;39(12):2531–2541. doi: 10.1161/ATVBAHA.119.313401 [DOI] [PubMed] [Google Scholar]
- 22.Patel AP, Peloso GM, Pirruccello JP, et al. Targeted exonic sequencing of GWAS loci in the high extremes of the plasma lipids distribution. Atherosclerosis. 2016;250:63–68. doi: 10.1016/j.atherosclerosis.2016.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kanter JE, Shao B, Kramer F, et al. Increased apolipoprotein C3 drives cardiovascular risk in type 1 diabetes. J Clin Invest. 2019;130(10):4165–4179. doi: 10.1172/JCI127308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolska A, Reimund M, Remaley AT, Apolipoprotein C-I-I. The re-emergence of a forgotten factor. Curr Opin Lipidol. 2020;31(3):147–153. doi: 10.1097/MOL.0000000000000680 [DOI] [PubMed] [Google Scholar]
- 25.Santamarina-Fojo S. The familial chylomicronemia syndrome. Endocrinol Metab Clin North Am. 1998;27(3):551–567. doi: 10.1016/S0889-8529(05)70025-6 [DOI] [PubMed] [Google Scholar]
- 26.Nilsson SK, Heeren J, Olivecrona G, et al. Apolipoprotein A-V; a potent triglyceride reducer. Atherosclerosis. 2011;219(1):15–21. doi: 10.1016/j.atherosclerosis.2011.07.019 [DOI] [PubMed] [Google Scholar]
- 27.Beigneux AP, Fong LG, Bensadoun A, et al. GPIHBP1 missense mutations often cause multimerization of GPIHBP1 and thereby prevent lipoprotein lipase binding. Circ Res. 2015;116(4):624–632. doi: 10.1161/CIRCRESAHA.116.305085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Viljoen A, Wierzbicki AS. Diagnosis and treatment of severe hypertriglyceridemia. ExpertRevCardiovascTher. 2012;10(4):505–514. [DOI] [PubMed] [Google Scholar]
- 29.Moulin P, Dufour R, Averna M, et al. Identification and diagnosis of patients with familial chylomicronaemia syndrome (FCS): expert panel recommendations and proposal of an “FCS score”. Atherosclerosis. 2018;275:265–272. doi: 10.1016/j.atherosclerosis.2018.06.814 [DOI] [PubMed] [Google Scholar]
- 30.Garg R, Rustagi T. Management of Hypertriglyceridemia Induced Acute Pancreatitis. Biomed Res Int. 2018;2018:4721357. doi: 10.1155/2018/4721357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stefanutti C, Julius U. Treatment of primary hypertriglyceridemia states–General approach and the role of extracorporeal methods. Atheroscler Suppl. 2015;18:85–94. doi: 10.1016/j.atherosclerosissup.2015.02.017 [DOI] [PubMed] [Google Scholar]
- 32.Brown WV, Gaudet D, Goldberg I, Hegele R. Roundtable on etiology of familial chylomicronemia syndrome. J Clin Lipidol. 2018;12(1):5–11. doi: 10.1016/j.jacl.2017.12.015 [DOI] [PubMed] [Google Scholar]
- 33.Rouis M, Dugi KA, Previato L, et al. Therapeutic response to medium-chain triglycerides and omega-3 fatty acids in a patient with the familial chylomicronemia syndrome. Arterioscler Thromb Vasc Biol. 1997;17(7):1400–1406. doi: 10.1161/01.ATV.17.7.1400 [DOI] [PubMed] [Google Scholar]
- 34.Ahmad Z, Wilson DP. Familial chylomicronemia syndrome and response to medium-chain triglyceride therapy in an infant with novel mutations in GPIHBP1. J Clin Lipidol. 2014;8(6):635–639. doi: 10.1016/j.jacl.2014.08.010 [DOI] [PubMed] [Google Scholar]
- 35.Jung MK, Jin J, Kim HO, et al. A 1-month-old infant with chylomicronemia due to GPIHBP1 gene mutation treated by plasmapheresis. Ann Pediatr Endocrinol Metab. 2017;22(1):68–71. doi: 10.6065/apem.2017.22.1.68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oscarsson J, Hurt-Camejo E. Omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid and their mechanisms of action on apolipoprotein B-containing lipoproteins in humans: a review. Lipids Health Dis. 2017;16(1):149. doi: 10.1186/s12944-017-0541-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Preiss D, Tikkanen MJ, Welsh P, et al. Lipid-modifying therapies and risk of pancreatitis: a meta-analysis. JAMA. 2012;308(8):804–811. doi: 10.1001/jama.2012.8439 [DOI] [PubMed] [Google Scholar]
- 38.Chaudhry R, Viljoen A, Wierzbicki AS. Pharmacological treatment options for severe hypertriglyceridemia and familial chylomicronemia syndrome. Expert Rev Clin Pharmacol. 2018;11(6):589–598. doi: 10.1080/17512433.2018.1480368 [DOI] [PubMed] [Google Scholar]
- 39.Hegele RA, Berberich AJ, Ban MR, et al. Clinical and biochemical features of different molecular etiologies of familial chylomicronemia. J Clin Lipidol. 2018;12(4):920–927.e4. doi: 10.1016/j.jacl.2018.03.093 [DOI] [PubMed] [Google Scholar]
- 40.Hogue JC, Lamarche B, Deshaies Y, et al. Differential effect of fenofibrate and atorvastatin on in vivo kinetics of apolipoproteins B-100 and B-48 in subjects with type 2 diabetes mellitus with marked hypertriglyceridemia. Metabolism. 2008;57(2):246–254. doi: 10.1016/j.metabol.2007.09.008 [DOI] [PubMed] [Google Scholar]
- 41.Wong AT, Chan DC, Barrett PH, Adams LA, Watts GF. Effect of omega-3 fatty acid ethyl esters on apolipoprotein B-48 kinetics in obese subjects on a weight-loss diet: a new tracer kinetic study in the postprandial state. J Clin Endocrinol Metab. 2014;99(8):E1427–35. doi: 10.1210/jc.2013-4037 [DOI] [PubMed] [Google Scholar]
- 42.Lamon-Fava S, Diffenderfer MR, Barrett PH, et al. Effects of different doses of atorvastatin on human apolipoprotein B-100, B-48, and A-I metabolism. J Lipid Res. 2007;48(8):1746–1753. doi: 10.1194/jlr.M700067-JLR200 [DOI] [PubMed] [Google Scholar]
- 43.Marco-Benedi V, Lamiquiz-Moneo I, Alvarez-Sala LA, Civeira F. Disappearance of recurrent pancreatitis after splenectomy in familial chylomicronemia syndrome. Atherosclerosis. 2018;275:342–345. doi: 10.1016/j.atherosclerosis.2018.06.870 [DOI] [PubMed] [Google Scholar]
- 44.Castagneto M, De Gaetano A, Mingrone G, et al. A surgical option for familial chylomicronemia associated with insulin-resistant diabetes mellitus. Obes Surg. 1998;8(2):191–198. doi: 10.1381/096089298765554809 [DOI] [PubMed] [Google Scholar]
- 45.Hussain I, Garg A. Lipodystrophy Syndromes. Endocrinol Metab Clin North Am. 2016;45(4):783–797. doi: 10.1016/j.ecl.2016.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hussain I, Patni N, Garg A. Lipodystrophies, dyslipidaemias and atherosclerotic cardiovascular disease. Pathology. 2019;51(2):202–212. doi: 10.1016/j.pathol.2018.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ozgen Saydam B, Sonmez M, Simsir IY, et al. A subset of patients with acquired partial lipodystrophy developing severe metabolic abnormalities. Endocr Res. 2019;44(1–2):46–54. doi: 10.1080/07435800.2018.1513029 [DOI] [PubMed] [Google Scholar]
- 48.Brown RJ, Araujo-Vilar D, Cheung PT, et al. The Diagnosis and Management of Lipodystrophy Syndromes: A Multi-Society Practice Guideline. J Clin Endocrinol Metab. 2016;101(12):4500–4511. doi: 10.1210/jc.2016-2466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brown WV, Garg A, Gorden P, Shamburek R. JCL roundtable: diagnosis and clinical management of lipodystrophy. J Clin Lipidol. 2016;10(4):728–736. doi: 10.1016/j.jacl.2016.06.005 [DOI] [PubMed] [Google Scholar]
- 50.Actis Dato V, Chiabrando GA. The Role of Low-Density Lipoprotein Receptor-Related Protein 1 in Lipid Metabolism, Glucose Homeostasis and Inflammation. Int J Mol Sci. 2018;19(6):1780. doi: 10.3390/ijms19061780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lino M, Farr S, Baker C, Fuller M, Trigatti B, Adeli K. Intestinal scavenger receptor class B type I as a novel regulator of chylomicron production in healthy and diet-induced obese states. Am J Physiol Gastrointest Liver Physiol. 2015;309(5):G350–9. doi: 10.1152/ajpgi.00086.2015 [DOI] [PubMed] [Google Scholar]
- 52.Ramms B, Gordts P. Apolipoprotein C-III in triglyceride-rich lipoprotein metabolism. Curr Opin Lipidol. 2018;29(3):171–179. doi: 10.1097/MOL.0000000000000502 [DOI] [PubMed] [Google Scholar]
- 53.Sacks FM. The crucial roles of apolipoproteins E and C-III in apoB lipoprotein metabolism in normolipidemia and hypertriglyceridemia. Curr Opin Lipidol. 2015;26(1):56–63. doi: 10.1097/MOL.0000000000000146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mendivil CO, Zheng C, Furtado J, Lel J, Sacks FM. Metabolism of very-low-density lipoprotein and low-density lipoprotein containing apolipoprotein C-III and not other small apolipoproteins. Arterioscler Thromb Vasc Biol. 2010;30(2):239–245. doi: 10.1161/ATVBAHA.109.197830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li D, Rodia CN, Johnson ZK, et al. Intestinal basolateral lipid substrate transport is linked to chylomicron secretion and is regulated by apoC-III. J Lipid Res. 2019;60(9):1503–1515. doi: 10.1194/jlr.M092460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Khetarpal SA, Zeng X, Millar JS, et al. A human APOC3 missense variant and monoclonal antibody accelerate apoC-III clearance and lower triglyceride-rich lipoprotein levels. Nat Med. 2017;23(9):1086–1094. doi: 10.1038/nm.4390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sahebkar A, Simental-Mendia LE, Katsiki N, et al. Effect of fenofibrate on plasma apolipoprotein C-III levels: a systematic review and meta-analysis of randomised placebo-controlled trials. BMJ Open. 2019;8(11):e021508. doi: 10.1136/bmjopen-2018-021508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Andersson Y, Majd Z, Lefebvre AM, et al. Developmental and pharmacological regulation of apolipoprotein C-II gene expression. Comparison with apo C-I and apo C-III gene regulation. Arterioscler Thromb Vasc Biol. 1999;19(1):115–121. doi: 10.1161/01.ATV.19.1.115 [DOI] [PubMed] [Google Scholar]
- 59.Ooi EM, Watts GF, Chan DC, et al. Effects of extended-release niacin on the postprandial metabolism of Lp(a) and ApoB-100-containing lipoproteins in statin-treated men with type 2 diabetes mellitus. Arterioscler Thromb Vasc Biol. 2015;35(12):2686–2693. doi: 10.1161/ATVBAHA.115.306136 [DOI] [PubMed] [Google Scholar]
- 60.Savinova OV, Fillaus K, Harris WS, Shearer GC. Effects of niacin and omega-3 fatty acids on the apolipoproteins in overweight patients with elevated triglycerides and reduced HDL cholesterol. Atherosclerosis. 2015;240(2):520–525. doi: 10.1016/j.atherosclerosis.2015.04.793 [DOI] [PubMed] [Google Scholar]
- 61.Larsson M, Allan CM, Jung RS, et al. Apolipoprotein C-III inhibits triglyceride hydrolysis by GPIHBP1-bound LPL. J Lipid Res. 2017;58(9):1893–1902. doi: 10.1194/jlr.M078220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Guardiola M, Alvaro A, Vallve JC, et al. APOA5 gene expression in the human intestinal tissue and its response to in vitro exposure to fatty acid and fibrate. Nutr Metab Cardiovasc Dis. 2012;22(9):756–762. doi: 10.1016/j.numecd.2010.12.003 [DOI] [PubMed] [Google Scholar]
- 63.Zhang R. The ANGPTL3-4-8 model, a molecular mechanism for triglyceride trafficking. Open Biol. 2016;6(4):150272. doi: 10.1098/rsob.150272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wierzbicki AS, Viljoen A. Anti-sense oligonucleotide therapies for the treatment of hyperlipidaemia. Expert Opin Biol Ther. 2016;16(9):1125–1134. doi: 10.1080/14712598.2016.1196182 [DOI] [PubMed] [Google Scholar]
- 65.Graham MJ, Lee RG, Bell TA 3rd, et al. Antisense oligonucleotide inhibition of apolipoprotein C-III reduces plasma triglycerides in rodents, nonhuman primates, and humans. Circ Res. 2013;112(11):1479–1490. doi: 10.1161/CIRCRESAHA.111.300367 [DOI] [PubMed] [Google Scholar]
- 66.Julia Paik Sean D, Duggan S. Volanesorsen: first Global Approval. Drugs. 2019;79(12):1349–1354. [DOI] [PubMed] [Google Scholar]
- 67.European Medicines Agency. Volanesorsen: EU summary of product characteristics. Amsterdam, The Netherlands: European Medcines Agency; 2019Available from: https://www.waylivra.eu/wp-content/uploads/2019/05/WAYLIVRA-SmPC.pdf. Accessed June20, 2020.
- 68.Post N, Yu R, Greenlee S, et al. Metabolism and Disposition of Volanesorsen, a 2ʹ-O-(2 methoxyethyl) Antisense Oligonucleotide, Across Species. Drug Metab Dispos. 2019;47(10):1164–1173. doi: 10.1124/dmd.119.087395 [DOI] [PubMed] [Google Scholar]
- 69.Gaudet D, Brisson D, Tremblay K, et al. Targeting APOC3 in the familial chylomicronemia syndrome. N Engl J Med. 2014;371(23):2200–2206. doi: 10.1056/NEJMoa1400284 [DOI] [PubMed] [Google Scholar]
- 70.Gaudet D, Alexander VJ, Baker BF, et al. Antisense Inhibition of Apolipoprotein C-III in Patients with Hypertriglyceridemia. N Engl J Med. 2015;373(5):438–447. doi: 10.1056/NEJMoa1400283 [DOI] [PubMed] [Google Scholar]
- 71.Blom DJ, O’Dea L, Digenio A, et al. Characterizing familial chylomicronemia syndrome: baseline data of the APPROACH study. J Clin Lipidol. 2018;12(5):1234–43 e5. doi: 10.1016/j.jacl.2018.05.013 [DOI] [PubMed] [Google Scholar]
- 72.Witztum JL, Gaudet D, Freedman SD, et al. Volanesorsen and Triglyceride Levels in Familial Chylomicronemia Syndrome. N Engl J Med. 2019;381(6):531–542. doi: 10.1056/NEJMoa1715944 [DOI] [PubMed] [Google Scholar]
- 73.Gouni-Berthold I, Alexander V, Digenio A, et al. Apolipoprotein C-III inhibition with volanesorsen in patients with hypertriglyceridemia (COMPASS): A randomized, double-blind, placebo-controlled trial. Atheroscler Suppl. 2017;28:e1–e2. doi: 10.1016/j.atherosclerosissup.2017.08.003 [DOI] [Google Scholar]
- 74.Gelrud A, Digenio A, Alexander V, et al. Treatment with Volanesorsen (VLN) Reduced Triglycerides and Pancreatitis in Patients with FCS and sHTG vs Placebo: results of the APPROACH and COMPASS †. J Clin Lipidol. 2018;12(2):537. doi: 10.1016/j.jacl.2018.03.032 [DOI] [Google Scholar]
- 75.Arca M, Hsieh A, Soran H, Rosenblit P, O’Dea L, Stevenson M. The effect of volanesorsen treatment on the burden associated with familial chylomicronemia syndrome: the results of the ReFOCUS study. Expert Rev Cardiovasc Ther. 2018;16(7):537–546. doi: 10.1080/14779072.2018.1487290 [DOI] [PubMed] [Google Scholar]
- 76.European Medicines Agency. Volanesorsen (Waylivra): public assessment report Amsterdam, The Netherlands: European Medicines Agency; 2019. Available from: https;//www.ema.europa.eu/.
- 77.Paik J, Duggan S. Volanesorsen: first Global Approval. Drugs. 2019;79(12):1349–1354. doi: 10.1007/s40265-019-01168-z [DOI] [PubMed] [Google Scholar]
- 78.Digenio A, Dunbar RL, Alexander VJ, et al. Antisense-Mediated Lowering of Plasma Apolipoprotein C-III by Volanesorsen Improves Dyslipidemia and Insulin Sensitivity in Type 2 Diabetes. Diabetes Care. 2016;39(8):1408–1415. doi: 10.2337/dc16-0126 [DOI] [PubMed] [Google Scholar]
- 79.O’Connell C, Horwood K, Nadamuni M. Correction of refractory thrombocytopenia and anemia following withdrawal of extended release niacin. Am J Hematol. 2016;91(7):E318. doi: 10.1002/ajh.24371 [DOI] [PubMed] [Google Scholar]
- 80.Landray MJ, Haynes R, Hopewell JC, et al.; HPS THRIVE Collaborative Group. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371(3):203–212. [DOI] [PubMed] [Google Scholar]
- 81.Narayanan P, Curtis BR, Shen L, et al. Underlying Immune Disorder May Predispose Some Transthyretin Amyloidosis Subjects to Inotersen-Mediated Thrombocytopenia. Nucleic Acid Ther. 2020;30(2):94–103. doi: 10.1089/nat.2019.0829 [DOI] [PubMed] [Google Scholar]
- 82.Endocrinologic and Metabolic Drugs Advisory Committee Food and Drug Administration. FDA Briefing Document: EMDAC Meeting for Volanesorsen (Waylivra) Silver Spring. Maryland, USA: Food and Drug Adminstration; 2018. Available from:: www.fda.gov. Accessed June20, 2020. [Google Scholar]
- 83.National Institute for Health and Care Excellence (NICE). Volanesorsen for treating familial chylomicronemia syndrome (ID1326) London, United kingdom: national Institute for Health and Care Excellence; 2019Available from: https://www.nice.org.uk/guidance/indevelopment/gid-hst10015/documents. Accessed June20, 2020.
- 84.Gaudet D, Stroes ES, Methot J, et al. Long-Term Retrospective Analysis of Gene Therapy with Alipogene Tiparvovec and Its Effect on Lipoprotein Lipase Deficiency-Induced Pancreatitis. Hum Gene Ther. 2016;27(11):916–925. doi: 10.1089/hum.2015.158 [DOI] [PubMed] [Google Scholar]
- 85.Macchi C, Sirtori CR, Corsini A, Santos RD, Watts GF, Ruscica M. A new dawn for managing dyslipidemias: the era of RNA-based therapies. Pharmacol Res. 2019;150:104413. doi: 10.1016/j.phrs.2019.104413 [DOI] [PubMed] [Google Scholar]
- 86.Alexander VJ, Xia S, Hurh E, et al. N-acetyl galactosamine-conjugated antisense drug to APOC3 mRNA, triglycerides and atherogenic lipoprotein levels. Eur Heart J. 2019;40(33):2785–2796. doi: 10.1093/eurheartj/ehz209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gaudet D, Methot J, Dery S, et al. Efficacy and long-term safety of alipogene tiparvovec (AAV1-LPLS447X) gene therapy for lipoprotein lipase deficiency: an open-label trial. Gene Ther. 2013;20(4):361–369. doi: 10.1038/gt.2012.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Morrison C. $1-million price tag set for Glybera gene therapy. Nat Biotechnol. 2015;33(3):217–218. doi: 10.1038/nbt0315-217 [DOI] [PubMed] [Google Scholar]
- 89.Yla-Herttuala S. Glybera’s second act: the curtain rises on the high cost of therapy. Mol Ther. 2015;23(2):217–218. doi: 10.1038/mt.2014.248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wolska A, Lo L, Sviridov DO, et al. A dual apolipoprotein C-II mimetic-apolipoprotein C-III antagonist peptide lowers plasma triglycerides. Sci Transl Med. 2020;12(528):528. doi: 10.1126/scitranslmed.aaw7905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Alonso R, Cuevas A, Mata P. Lomitapide: a review of its clinical use, efficacy, and tolerability. Core Evid. 2019;14:19–30. doi: 10.2147/CE.S174169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sacks FM, Stanesa M, Hegele RA. Severe hypertriglyceridemia with pancreatitis: thirteen years’ treatment with lomitapide. JAMA Intern Med. 2014;174(3):443–447. doi: 10.1001/jamainternmed.2013.13309 [DOI] [PubMed] [Google Scholar]
- 93.Meyers CD, Tremblay K, Amer A, Chen J, Jiang L, Gaudet D. Effect of the DGAT1 inhibitor pradigastat on triglyceride and apoB48 levels in patients with familial chylomicronemia syndrome. Lipids Health Dis. 2015;14(1):8. doi: 10.1186/s12944-015-0006-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Dewey FE, Gusarova V, Dunbar RL, et al. Genetic and Pharmacologic Inactivation of ANGPTL3 and Cardiovascular Disease. N Engl J Med. 2017;377(3):211–221. doi: 10.1056/NEJMoa1612790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Minicocci I, Tikka A, Poggiogalle E, et al. Effects of angiopoietin-like protein 3 deficiency on postprandial lipid and lipoprotein metabolism. J Lipid Res. 2016;57(6):1097–1107. doi: 10.1194/jlr.P066183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Graham MJ, Lee RG, Brandt TA, et al. Cardiovascular and Metabolic Effects of ANGPTL3 Antisense Oligonucleotides. N Engl J Med. 2017;377(3):222–232. doi: 10.1056/NEJMoa1701329 [DOI] [PubMed] [Google Scholar]
- 97.Gaudet D, Gipe D, Hovingh K, et al. Safety and efficacy of evinacumab, a monoclonal antibody to ANGPTL3, in patients with homozygous familial hypercholesterolemia: a single-arm, open-label, proof-of-concept study. Atherosclerosis. 2017;263:e9. doi: 10.1016/j.atherosclerosis.2017.06.057 [DOI] [Google Scholar]
- 98.Chadwick AC, Evitt NH, Lv W, Musunuru K. Reduced Blood Lipid Levels With In Vivo CRISPR-Cas9 Base Editing of ANGPTL3. Circulation. 2018;137(9):975–977. doi: 10.1161/CIRCULATIONAHA.117.031335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Oral EA, Gorden P, Cochran E, et al. Long-term effectiveness and safety of metreleptin in the treatment of patients with partial lipodystrophy. Endocrine. 2019;64(3):500–511. doi: 10.1007/s12020-019-01862-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- European Medicines Agency. Volanesorsen: EU summary of product characteristics. Amsterdam, The Netherlands: European Medcines Agency; 2019Available from: https://www.waylivra.eu/wp-content/uploads/2019/05/WAYLIVRA-SmPC.pdf. Accessed June20, 2020.
- European Medicines Agency. Volanesorsen (Waylivra): public assessment report Amsterdam, The Netherlands: European Medicines Agency; 2019. Available from: https;//www.ema.europa.eu/.
- National Institute for Health and Care Excellence (NICE). Volanesorsen for treating familial chylomicronemia syndrome (ID1326) London, United kingdom: national Institute for Health and Care Excellence; 2019Available from: https://www.nice.org.uk/guidance/indevelopment/gid-hst10015/documents. Accessed June20, 2020.