Abstract
An oral vaccine against anthrax (Bacillus anthracis) is urgently needed to prevent annual anthrax outbreaks that are causing catastrophic losses in free-ranging livestock and wildlife worldwide. The Sterne vaccine, the current injectable livestock vaccine, is a suspension of live attenuated B. anthracis Sterne strain 34F2 spores (Sterne spores) in saponin. It is not effective when administered orally and individual subcutaneous injections are not a practical method of vaccination for wildlife. In this study, we report the development of a microencapsulated oral vaccine against anthrax. Evaluating Sterne spore stability at varying pH’s in vitro revealed that spore exposure to pH 2 results in spore death, confirming that protection from the gastric environment is of main concern when producing an oral vaccine. Therefore, Sterne spores were encapsulated in alginate and coated with a protein shell containing poly-L-lysine (PLL) and vitelline protein B (VpB), a non-immunogenic, proteolysis resistant protein isolated from Fasciola hepatica. Capsule exposure to pH 2 demonstrated enhanced acid gel character suggesting that alginate microcapsules provided the necessary protection for spores to survive the gastric environment. Post vaccination IgG levels in BALBc/J mouse serum samples indicated that encapsulated spores induced anti-anthrax specific responses in both the subcutaneous and the oral vaccination groups. Furthermore, the antibody responses from both vaccination routes were protective against anthrax lethal toxin in vitro, suggesting that further optimization of this vaccine formulation may result in a reliable oral vaccine that will conveniently and effectively prevent anthrax in wildlife populations.
Subject terms: Bacterial infection, Live attenuated vaccines, Live attenuated vaccines
Introduction
Anthrax infections have plagued humans and animals alike for millennia, possibly even causing the fifth and sixth plagues of Egypt1. The causative agent, Bacillus anthracis, has been studied since the beginning of microbiology but even after more than a century of scientific studies, the anthrax vaccination field has made little progress, especially with veterinary anthrax vaccines1,2. A recent study consolidated data from the last 20 years and found a worldwide distribution and suitability for anthrax in the environment with reports of the disease on every habitable continent, yet most animals remain unvaccinated3. While it may be prudent to mention that the incidence of human infection can be decreased with adequate livestock and wildlife vaccination policies, it should also be of great concern that free-ranging livestock and wildlife populations worldwide are unprotected against anthrax outbreaks that can cause catastrophic harm to sensitive wildlife conservation efforts3–6.
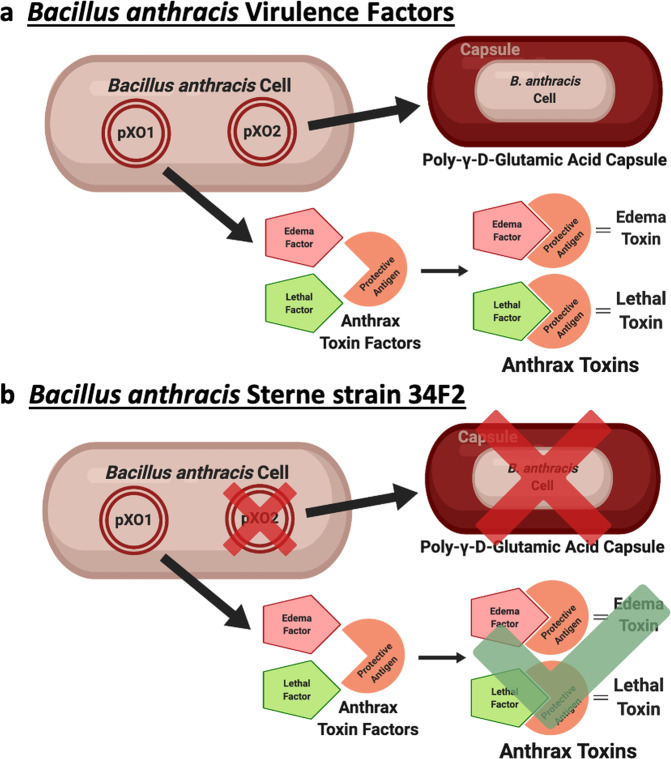
The current veterinary vaccine, historically referred to as the Sterne vaccine, uses B. anthracis Sterne strain 34F2 spores (Sterne spores) that have naturally lost the pXO2 plasmid and therefore can no longer produce the poly-γ-D-glutamic acid capsule, also known as the anti-phagocytic capsule (Fig. 1)6. The original formulation of the Sterne vaccine, which is still in use today, consists of Sterne spores suspended in saponin and has been used to vaccinate domesticated livestock against anthrax since its discovery in the late 1930’s1,7. Despite decades of successful protections, the Sterne vaccine is outdated, impractical, known to vary in its potency, and can cause adverse reactions, occasionally even death8. Logistically speaking, the Sterne vaccine is distributed as a subcutaneous injection which is a highly impractical method of vaccination for free-ranging livestock and wildlife1. Without a reasonable method of wildlife vaccination, yearly anthrax outbreaks in national parks and other wildlife areas worldwide pose economic, ecological and conservational burdens to wildlife and wildlife health professionals3,7,9,10. Even with these yearly outbreaks, the anthrax spore distribution in these areas is undetermined so it isn’t possible to vaccinate wildlife based on an estimated risk of exposure11. The most feasible way to protect wildlife in these areas would be via oral vaccination however, after results from a previous study demonstrated that the Sterne vaccine is incapable of eliciting an immune response following oral vaccination, the urgent need for an effective oral anthrax vaccine for wildlife has never been more evident12.
Fig. 1. Illustration of Bacillus anthracis plasmids.
a A fully virulent B. anthracis cell containing both the pXO1 and pXO2 plasmids. b B. anthracis Sterne strain 34F2 cell containing only the pXO1 plasmid. Created with BioRender.com.
Other research groups in the oral anthrax vaccination field have reported encouraging results from vaccines expressing a recombinant form of anthrax protective antigen in a variety of bacterial, viral or plant-based expression systems13–16. Any progress toward the development of an oral anthrax vaccine is a great achievement, but studies have suggested that anthrax spore associated antigens may also make important contributions to vaccine induced protection17,18. Since it is possible that exposure to a single recombinant antigen may not stimulate sufficient immune activity to protect against fully virulent exposure17, it may be advantageous to maintain the live attenuated format of the Sterne vaccine, but adapt it for oral use.
One method to accomplish this is through the exceptionally high flexibility of alginate encapsulation19–21. Alginate is naturally indigestible in mammalian systems which can be implemented as a natural controlled release vehicle22,23. In addition, the mild gelation conditions permit entrapment of the desired capsule load without significantly affecting the viability22. Post-gelation, the viability of the capsule load is maintained by stability of the microcapsule, particularly in gastric environments which has proven overwhelmingly beneficial for the development of probiotics20. Alginate has also demonstrated bio-adhesive properties when interacting with mucosal tissues. Combined with the depot effect of alginate capsules, these bio-adhesive properties ensure that the capsule load is repeatedly released in close proximity to target cells19.
The beneficial characteristics of alginate microcapsules can also be specifically tailored to each application by altering the capsule size, structure, load, layers, and many other aspects of each capsule formulation. When it comes to oral vaccine delivery incorporating stabilizing components, such as poly-L-lysine (PLL) and vitelline protein B (VpB), into the alginate microcapsule formulation can enhance the overall capsule stability. PLL is a common microcapsule coating that stabilizes alginate cross-linking24–26. VpB, a non-immunogenic, eggshell precursor protein isolated from the parasite Fasciola hepatica, is resistant to enzymatic and chemical degradation and can extend the already slow erosion of the alginate capsule27,28. Prior studies from our research group have applied a protein shell containing both of these components to microencapsulated Brucella spp. and reported stronger, extended immune responses that correlated with enhanced protection against wild-type challenge29–32.
In the current study, we evaluated the effect that this formulation had on the stability of microcapsules as enteric delivery vehicles. We also examined the immunogenicity of microencapsulated Sterne spores and observed a pronounced increase in the resulting antibody response from both subcutaneous and oral vaccination in mice. Moreover, an in vitro toxin challenge revealed that the observed antibody response was protective for the macrophage cell line following oral vaccination suggesting that with further optimization, microencapsulated Sterne spores can be developed into an alternative anthrax vaccine formulation capable of efficient and protective vaccination of free-ranging livestock and wildlife.
Results
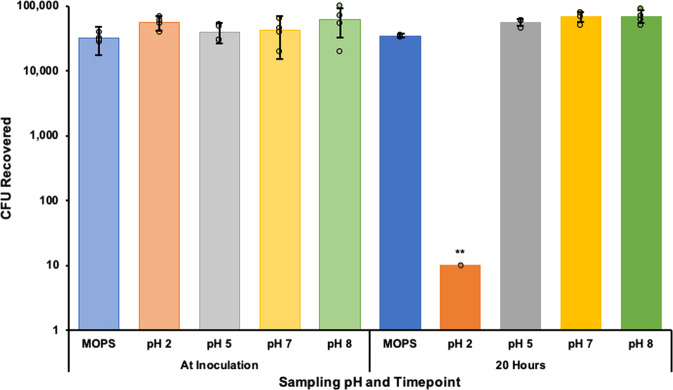
Sterne spore stability in simulated gastrointestinal environments
The unencapsulated Sterne spore response to simulated gastrointestinal fluids (GI fluids) was observed to better understand and account for impairments while in transit through the stomach and intestines. Simulated gastric (0.2% (w/v) NaCl, pH 2 and pH 5) and intestinal (0.68% (w/v) KH2PO4, pH 7 and 8) fluids33 were inoculated with 6.8 × 105 Bacillus anthracis Sterne strain 34F2 spores and incubated overnight at 37 °C with shaking. MOPS buffer (10 mM MOPS, 0.85% NaCl, [pH 7.4]) was also inoculated with 6.8 × 105 Sterne spores to serve as a negative control for encapsulated vaccine storage conditions. The unencapsulated Sterne spore titer was severely reduced as a result of exposure to 0.2% NaCl (w/v) pH 2 (p < 0.01) with no other significant responses observed from pH 5, 7 or 8 (Fig. 2).
Fig. 2. Sterne spore titer response to simulated gastrointestinal environments.
Simulated gastric (0.2% (w/v) NaCl, pH 2 and pH 5) and intestinal (0.68% (w/v) KH2PO4, pH 7 and 8) fluids were inoculated with 6.8 × 105 Bacillus anthracis Sterne strain 34F2 spores and incubated overnight at 37 °C with shaking. MOPS buffer (10 mM MOPS, 0.85% NaCl) was also inoculated with 6.8 × 105 Sterne spores to serve as a negative control for encapsulated vaccine storage conditions. The resulting viable bacterial titer in each solution was determined by plating serial dilutions. Differences between starting and resulting titers were determined by Student’s t-tests with **p < 0.01.
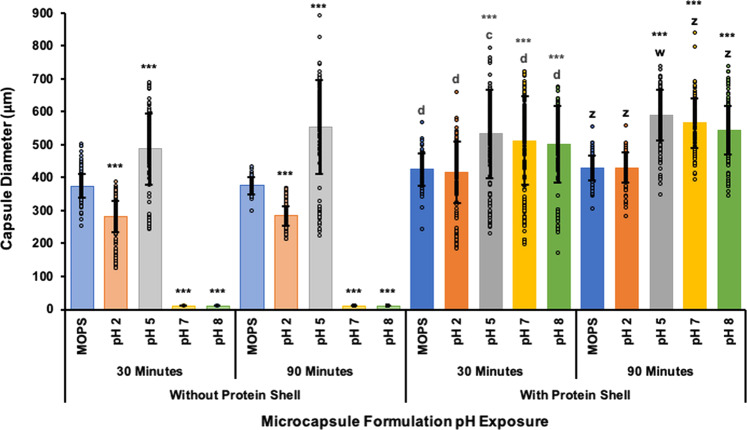
Comparison of microcapsule formulations in gastrointestinal environments
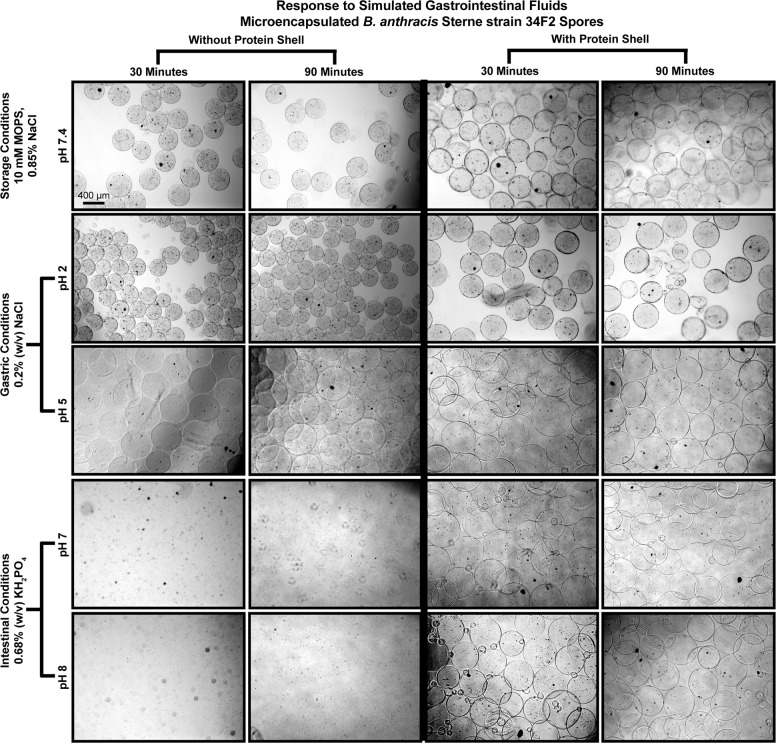
Microcapsules were also exposed to GI fluids to observe the relative stability in simulated gastrointestinal conditions33 with and without the PLL and VpB shell (protein shell). Microcapsule samples were suspended in MOPS buffer as a negative control and simulated GI fluids at pH 2, 5, 7, and 8 for 30 and 90 min at 37 °C with shaking. At pH 2, capsules that were not coated with the protein shell were shown to decrease in diameter compared to neutral storage conditions in MOPS, whereas at pH 5 capsules without the protein shell experienced significant swelling (Fig. 3). The most striking advantage of the protein shell was its capsule stabilization abilities at pH 7 and 8. Without the addition of this proteolysis resistant coating, the capsules completely disintegrated at neutral pHs (Fig. 4). These patterns were also observed in uncoated capsules after 90 min in GI fluids, simply to a higher degree as a result of the extended exposure. In comparison, capsules with the protein shell exhibited overall enhanced stability in all GI fluids by preventing shrinking at pH2 and complete capsule dissolution at pH 7 and 8 (Fig. 4).
Fig. 3. Microcapsule response to simulated gastrointestinal fluids.
Microcapsules with and without protein shell were suspended in simulated gastric (0.2% (w/v) NaCl, pH 2 and pH 5) and intestinal (0.68% (w/v) KH2PO4, pH 7 and 8) fluids for 30 and 90 min at 37 °C with shaking. Microcapsule samples were also suspended in MOPS buffer (10 mM MOPS, 0.85% NaCl) as a negative control for encapsulated vaccine storage conditions. The capsule diameters after exposure to simulated gastrointestinal fluids were observed in brightfield and measured in ImageJ. Data are reported as the average capsule diameter for the group in μm ± the standard deviation and changes were determined by one-way ANOVA followed by the Tukey–Kramer HSD test. Significant differences from pre-exposure diameters in MOPS within the same group are identified as ***p < 0.001. Differences between exposure diameters in microcapsules with and without the protein shell after the 30-min incubation are identified with c, p < 0.001 and d, p < 0.0001. Differences between exposure diameters in microcapsules with and without the protein shell after the 90-min incubation are identified with w, p < 0.05 and z, p < 0.0001.
Fig. 4. Microcapsule response with and without the protein shell to simulated gastrointestinal environments.
Representative brightfield images of microcapsule samples following exposure to simulated gastric (0.2% (w/v) NaCl, pH 2 and pH 5) and intestinal (0.68% (w/v) KH2PO4, pH 7 and 8) fluids for 30 and 90 min at 37 °C with shaking. Microcapsule samples were also suspended in MOPS buffer (10 mM MOPS, 0.85% NaCl) as a negative control for encapsulated vaccine storage conditions. The bottom two images of the two left columns portray the dissolution of capsules without the protein shell at pH 7 and pH 8. Bar represents 400 μm.
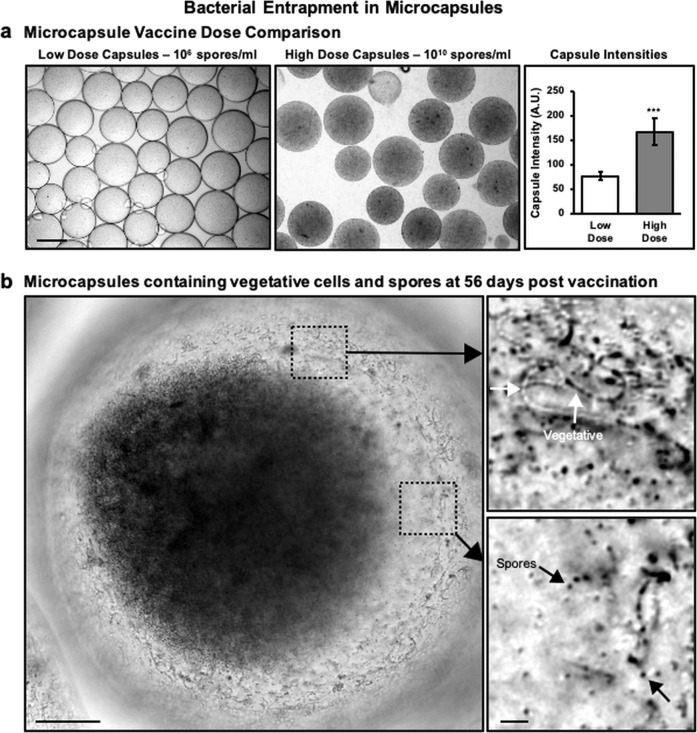
Evidence of bacterial entrapment and controlled release from microcapsules
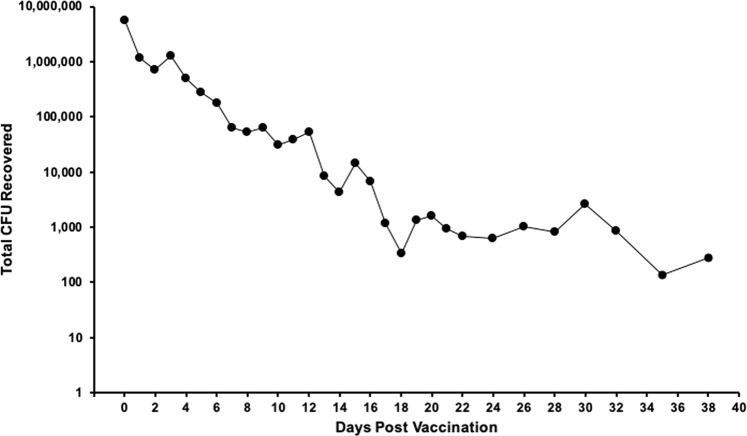
Microcapsules were imaged in the brightfield to confirm ideal capsule formation and bacterial entrapment. The drastic increase in the amount of encapsulated Sterne spores is visible when comparing the Low Dose Capsules with the High Dose Capsules in storage conditions which were made with 5 × 106 spores/ml and 4 × 1010 spores/ml, respectively (Fig. 5a, left and middle). This significant increase (p < 0.0001) is also evidenced by measuring the pixel intensity of the microcapsule images (Fig. 5a, right). An in vitro release experiment was conducted by collecting samples for 38 days to evaluate the timeframe of bacterial release from microcapsules coated with the protein shell. Microcapsules were suspended in 1 ml of MOPS buffer and incubated at 37 °C with shaking. The supernatant was removed and replaced at frequent intervals then serially diluted on LB agar to quantify the release rate. Results depicted in Fig. 6 confirm the sustained release abilities of microcapsules coated with the protein shell. Although the daily sample collection was stopped beyond 38 days, the full experiment was terminated at the same time as the mouse immunization experiment on day 56 when a final bacterial release sample and the remaining capsules were collected for imaging. After 56 days of shaking at 37 °C, the capsules still contained aggregations of viable Sterne spores and vegetative cells (Fig. 5b) suggesting that capsules would have been able to continue releasing viable bacteria for much longer.
Fig. 5. Sterne spore entrapment in microcapsules.
a Visual and pixel intensity comparison between Low and High Dose Capsules demonstrates the difference (***p < 0.0001) between the encapsulated doses as determined by Student’s t-tests. Bar represents 400 μm. b A considerable amount of aggregated Sterne cells are still entrapped within the microcapsules, as seen in this close up image of a single High Dose microcapsule 56 days after starting the in vitro release experiment. Bar represents 100 μm (left). Magnified images of vegetative cells (top right) and spores (bottom right) that remain entrapped within the High Dose microcapsule. Bar represents 10 μm.
Fig. 6. In vitro bacterial release from microcapsules.
A 1 ml sample of microcapsules with the protein shell was suspended in 10 ml MOPS at 37 °C with shaking. The MOPS buffer was completely removed and replaced each day. The collected supernatant was serially diluted and plated onto LB agar to quantify the CFU that had been released each day.
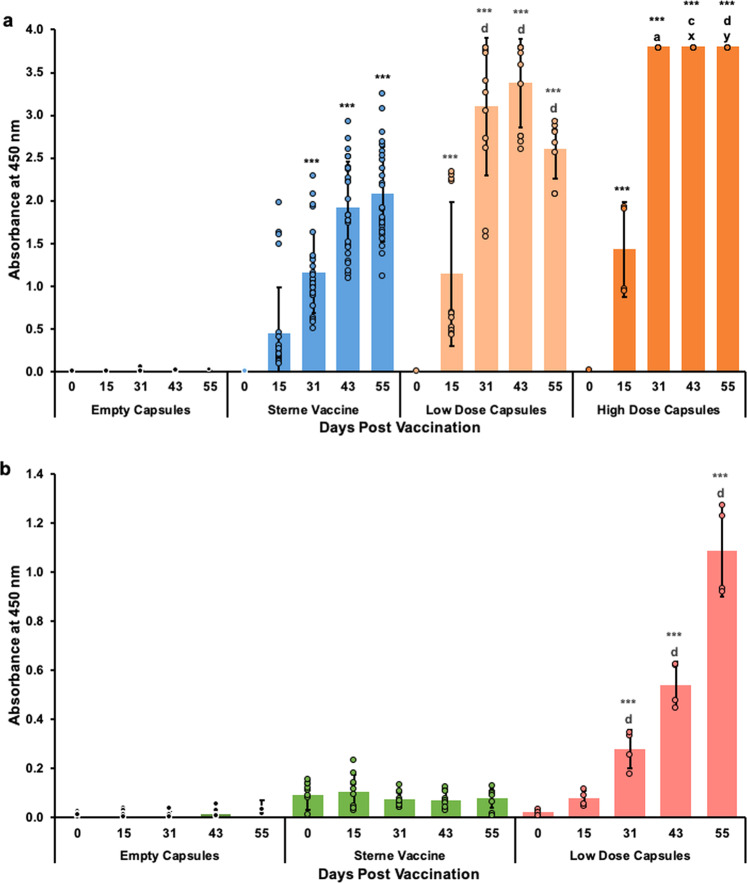
Microcapsule vaccines induce anthrax specific antibody responses
Antibody levels against anthrax protective antigen were measured by end point ELISA. All vaccines containing Sterne spores elicited strong antibody responses starting at 15 days post subcutaneous vaccination (Fig. 7a, Supplementary Figs. 1–3, Supplementary Table 1). Despite being inoculated with the same dose of spores (Table 1), the Low Dose Capsule group demonstrated a higher antibody response than the Sterne vaccine group on days 31 and 43 (Fig. 7a, Supplementary Figs 1 and 2, Supplementary Table 1). These antibody levels were even further increased in mice that were subcutaneously vaccinated with the High Dose Capsules which resulted in higher IgG titers at all time points (Fig. 7a, Supplementary Fig. 3, Supplementary Table 1). A similarly improved antibody response was also observed from the orally administered Low Dose Capsules starting at 31 days post vaccination and it continued to increase each week (Fig. 7b, Supplementary Fig. 4, Supplementary Table 1). Both orally administered vaccines contained the same dose of Sterne spores, but the oral Sterne vaccine did not induce any antibody response (Fig. 7b, Supplementary Fig. 5).
Fig. 7. IgG responses from subcutaneous and oral vaccination with Empty Capsules, Sterne vaccine, Low Dose Capsules and High Dose Capsules.
BALBc/J mice were either subcutaneously injected (a) or orally inoculated (b) with 106 unencapsulated B. anthracis Sterne strain 34F2 spores or 106 encapsulated Sterne spores in Low Dose Capsules. An additional group of mice were subcutaneously injected with 109 encapsulated Sterne spores in High Dose Capsules (a). All capsule vaccines were coated with the protein shell. The control groups received Empty Capsules. Serum samples were collected at 0, 15, 31, 43- and 55-days post vaccination and analyzed by ELISA. Antibody responses were analyzed by one-way ANOVA followed by the Tukey–Kramer HSD test and are shown as mean absorbances at 450 nm ± standard deviation from the 1:2000 dilution for subcutaneously inoculated mice and from the 1:125 dilution for orally inoculated mice. Significant differences from pre-vaccination (Day 0) within the same group are identified as ***p < 0.0001. Differences between responses to the Sterne vaccine and Low Dose Capsules at corresponding time points are identified with a, p < 0.05; c, p < 0.001 and d, p < 0.0001. Differences between responses to the Low Dose Capsules and High Dose Capsules at corresponding time points are identified with x, p < 0.01 and y, p < 0.0001.
Table 1.
Vaccination groups to assess the efficacy of microencapsulated Sterne spores as an oral vaccine.
| Route | Group (n = 5) | Inoculation volume | Spores/ml | Spores/mouse | Blood collection (days post-vaccination) |
|---|---|---|---|---|---|
| SC | Empty Capsules | 0.2 ml | – | – | 0, 15, 31, 43, 55 |
| SC | Sterne vaccine | 0.2 ml | 5 × 106 | 1 × 106 | 0, 15, 31, 43, 55 |
| SC | Low Dose Capsules | 0.2 ml | 5 × 106 | 1 × 106 | 0, 15, 31, 43, 55 |
| SC | High Dose Capsules | 0.2 ml | 4 × 1010 | 9 × 109 | 0, 15, 31, 43, 55 |
| Oral | Empty Capsules | 0.2 ml | – | – | 0, 15, 31, 43, 55 |
| Oral | Sterne vaccine | 0.2 ml | 5 × 106 | 1 × 106 | 0, 15, 31, 43, 55 |
| Oral | Low Dose Capsules | 0.2 ml | 5 × 106 | 1 × 106 | 0, 15, 31, 43, 55 |
SC subcutaneous, Empty capsules Microcapsules with PLL and VpB shell (no bacteria), Sterne vaccine B. anthracis Sterne strain 34F2 spores in saponin, Low Dose Capsules microcapsules with the protein shell and the standard dose of Sterne spores, High Dose Capsules microcapsules with the protein shell and a higher dose of Sterne spores.
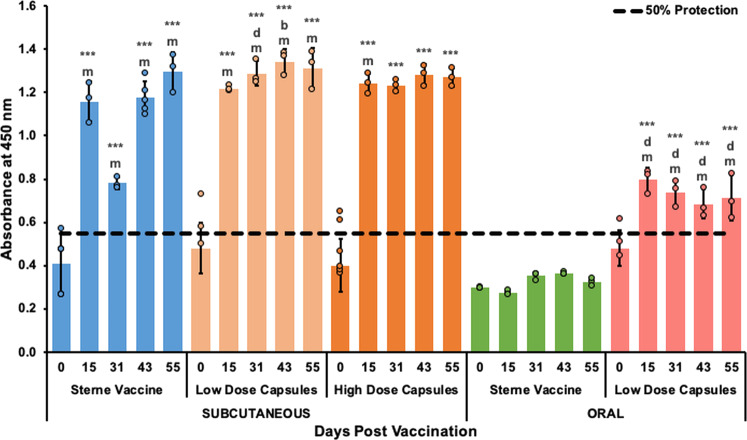
Microencapsulated Sterne spores induce toxin neutralizing antibodies
Lethal Toxin (LeTx) neutralization assays evaluated the ability for vaccination induced antibody responses to protect J774A.1 cells from LeTx mediated killing. The toxin neutralizing abilities of all vaccination groups are presented in Fig. 8 as mean absorbances at 595 nm ± the standard deviation at a single serum dilution of 1:50. Neutralizing antibody titers were estimated with serial dilutions and are reported in Supplementary Table 2. In agreement with the ELISA results, serum from all subcutaneously injected encapsulated vaccines containing Sterne spores appear to prevent ~100% of LeTx induced mortality in vitro at all measured time points (Fig. 8). The Low Dose Capsule vaccine exhibited enhanced LeTx neutralizing abilities at 31, 43, and 55-days post vaccination with stronger improvements induced by the High Dose Capsule vaccine (Supplementary Table 2). Strikingly, the orally administered Low Dose Capsule vaccine also resulted in partial toxin neutralizing effects at the same dilution as subcutaneously immunized mice (Fig. 8). Serum from mice immunized orally with the Sterne Vaccine did not provide any protection from LeTx challenge in vitro (Fig. 8, Supplementary Table 2).
Fig. 8. In vitro toxin neutralizing abilities of antibodies from subcutaneous and oral vaccination with the Sterne vaccine, Low Dose Capsules and High Dose Capsules.
Serum was collected from mice at 0, 15, 31, 43- and 55-days post subcutaneous or oral vaccination with 106 unencapsulated B. anthracis Sterne strain 34F2 spores, 106 encapsulated Sterne spores in Low Dose Capsules or 109 encapsulated Sterne spores in High Dose Capsules. Both Low and High capsule vaccines were coated with the protein shell. Control groups received Empty Capsules (results not included in this graph). Diluted serum samples were pre-incubated with LeTx then added to J774A.1 cells and the resulting cell viability was assessed with MTT dye. Data presented here represent the average absorbance at 595 nm ± standard deviations for each group at each time point at a 1:50 dilution with differences determined by one-way ANOVA followed by the Tukey–Kramer HSD test. Significant differences from pre-vaccination (Day 0) within the same group are identified as ***p < 0.0001. Differences between the Sterne Vaccine and Low Dose Capsules at corresponding time points are identified with b, p < 0.01 and d, p < 0.0001. Differences between subcutaneous and oral vaccination responses with the same vaccines at corresponding time points are identified with m, p < 0.0001. Differences between responses to the Low Dose Capsules and High Dose Capsules at corresponding time points were not significant.
Discussion
The benefits of oral vaccine delivery cannot be overstated, particularly when it comes to protecting free-ranging livestock and wildlife from current and emerging infectious diseases such as anthrax. Development of oral vaccines can allow for easy, wide-spread vaccination policies without needing to deal with the labor-intensive programs and painful injections associated with the majority of today’s human and animal vaccines. It is also possible that effective oral vaccines may be intrinsically more stable and have longer shelf-lives as a collateral benefit of the stability required for transit through the gastrointestinal tract. Furthermore, oral vaccines can lead to enhanced efficacy with less adverse effects due to mucosal immunity and oral delivery.
For all of these reasons and more, an alternative anthrax vaccine formulation specifically for oral administration is urgently needed to protect animals worldwide from potentially catastrophic anthrax outbreaks3,12. Many wildlife health professionals have demanded a new veterinary anthrax vaccine because individual hand-injections for each and every animal is not a practical method of vaccination for wildlife and a recent study demonstrated that oral vaccination with the Sterne vaccine is not effective1,12. Also, sustained protection from the Sterne vaccine can only be achieved with annual boosters which requires a yearly cycle of troublesome injections with the potential for adverse reactions1. To resolve the many issues associated with anthrax outbreaks and vaccination, we developed and evaluated an innovative anthrax vaccine formulation for oral vaccination. Results of our study demonstrate that subcutaneous and oral vaccination with microencapsulated B. anthracis Sterne strain 34F2 spores can induce antibody production in the murine model which can inactivate B. anthracis lethal toxin in vitro.
Oral vaccination is a common goal throughout the entire vaccinology field but there are still a limited number of oral vaccines approved for animal and human use because the main obstacle facing oral vaccination is, ironically, oral vaccination itself34–36. The principle of oral vaccination is completely dependent on getting sensitive antigens through the harsh, gastric environment that was evolutionarily designed specifically to prevent that exact thing from happening. In contrast, gastrointestinal pathogens, such as anthrax, have also evolved over thousands of years to survive the gastric environment for eventual uptake in the small intestine but these pathogen survival strategies aren’t typically conserved in live attenuated organisms, our most reliable vaccine format. Such is the case with B. anthracis Sterne strain 34F2. Upon exposure to a simulated gastric environment, there was a severe decrease in the viable Sterne spore titer (Fig. 2). Given that the majority of anthrax infections in wildlife are gastrointestinal, it can be reasoned that fully virulent anthrax spores are able to survive passage through a harsh acidic environment to establish infections following uptake in the small intestine. In comparison to the experiments performed here with the pXO2-negative Sterne strain, this suggests that fully virulent anthrax spores may be better equipped to survive the gastrointestinal environment due to retention of the pXO2 plasmid (Fig. 1). The details of this hypothesis were not investigated in this study but may be an important avenue to consider as we strive to understand and prevent infection with this pathogen. Sterne strain vulnerability to the simulated gastric environment also implies that development of an oral vaccine with the Sterne strain must involve some protection to ensure safe passage through the stomach. In the current study, we demonstrate that alginate encapsulation with a proteolysis resistant protein shell is able to shield Sterne spores enough through the gastric environment to induce an immune response following oral vaccination.
We assessed the stabilizing and shielding abilities of the microcapsules produced in this study by observing the microcapsule responses to simulated gastrointestinal environments. When alginate capsules are formed in a cross-linking solution, guluronate residues in the alginate cooperatively bind Ca2+ ions from the solution, thus cross-linking the alginate polymers to the “pre-gel” state21,24. Exposure of a calcium cross-linked pre-gel to nongelling cations, such as Na+, will reduce the mechanical stability of the alginate gel and possibly disintegrate the entire polymer matrix, as exhibited in Fig. 421,25. This can be prevented by adding additional cross-linked layers to the microcapsules, thus resulting in more stable capsules which we have demonstrated here by exposing uncoated and coated microcapsules to gastrointestinal environments37.
The added stability of these layers can be assessed through changes in microcapsule shrinking, swelling, and overall morphology. Changes in the alginate polymer network such as these can greatly affect the rate of diffusion through and the erosion of the network, thereby altering the antigen release rate22,38,39. Capsule shrinkage, as observed in uncoated capsules at pH 2 (Fig. 3), is indicative of increased acid-gel strength under higher proton concentrations33. Conversely, suspending uncoated capsules in pH 5 caused excessive swelling which implies increased pore size and therefore release of bacteria, whereas pH 7 and pH 8 resulted in complete disintegration of uncoated alginate capsules in the presence of nongelling ions (Fig. 4)21,25. Results of this study demonstrate the efficacy of using the PLL and VpB protein shell in this microcapsule formulation because it prevented most of the destabilizing affects observed in uncoated capsules. Specifically, the protein shell reduced the degree of swelling experienced by the capsules at pH 5, thereby avoiding drastic changes in the polymer network that could have led to premature bacterial release. Of most importance was that the protein shell maintained the capsule integrity at pH 7 and 8, whereas other studies have observed alginate disintegration at pH 7 and 840,41. By preventing complete capsule dissolution in neutral environments, the protein shell ensures that the capsule is stable enough to serve its controlled release purpose by stimulating mucosal immunity and uptake in the intestines. While it would have also been valuable to determine the surviving encapsulated spore titer following uncoated and coated capsule exposure to gastrointestinal pHs, this would have involved dissolving the coated capsules in trypsin which likely would have had its own effect on the viable Sterne spore recovery, therefore confounding any results that may have been acquired from the experiment.
A second challenge to oral vaccination, after having endured the harsh gastric environment, is to ensure antigen transport across the intestinal epithelia followed by antigen-presenting cell activation36. Advances in particulate vaccine delivery vehicles suggest that both issues can be resolved with microencapsulation. Prior studies have reported improved bacterial stability under acidic conditions due to microencapsulation in alginate20,21,42–44. In addition, alginate capsules can improve antigen uptake and processing by antigen-presenting cells through the depot effect45,46. These advantages proved beneficial in previous studies from our laboratory when microencapsulation of Brucella spp. in alginate microcapsules coated with the protein shell increased immune responses and reduced challenge organism recovery following oral vaccination29–32. Similar enhancements were observed in this study when we applied the same encapsulation method to B. anthracis Sterne strain 34F2 spores.
Subcutaneous vaccination with Low Dose Capsules enhanced the observed antibody response even though mice received the same dose of spores as those vaccinated with the Sterne vaccine (Fig. 7a, Supplementary Figs 1 and 2, Supplementary Table 1). Increasing the encapsulated spore dose also resulted in an even more robust antibody response following subcutaneous vaccination with High Dose Capsules (Fig. 7a). Excitingly, ELISA results also revealed a significant improvement in the amount of antibody produced following oral vaccination with the Low Dose Capsules when compared to the Sterne vaccine (Fig. 7b). Although this response is still lower than that of the subcutaneously injected vaccines, to our knowledge this is the first time a measurable antibody response has ever been recorded following oral vaccination with live attenuated Sterne spores. The single prior attempt we are aware of involved mixing Sterne spores with scarifying agents for oral vaccination by way of tiny lacerations in the gums, tongue, oropharynx, etc. and observed limited success47. In contrast, results presented here were obtained from mice vaccinated by oral gavage which completely bypassed the oral mucosa. This suggests that microencapsulation with the protein shell provides enough protection for Sterne spores to survive the gastric environment and progress into the small intestine to stimulate an immune response.
The advantages of this microcapsule formulation were also detected in results from toxin neutralization assays (Fig. 8) which are considered an additional marker and stronger correlate of protection13–15,48,49. Subcutaneous vaccination with Low Dose Capsules resulted in better protection for cultured macrophages at 31, 43, and 55-days post vaccination when compared to the unencapsulated Sterne vaccine (Supplementary Table 2). In addition, subcutaneous injection with ~9 × 109 Sterne spores per mouse in High Dose Capsules resulted in extraordinarily high serum IgG responses (Fig. 7a) that were fully protective in vitro by 15 days post vaccination (Fig. 8, Supplementary Table 2). This antibody response also may not yet have reached its peak prior to the end of the experiment. The in vitro release experiment demonstrated the controlled release abilities of this microcapsule formulation over the first 38 days (Fig. 6). However, images obtained from this experiment also showed that there was an excessive amount of Sterne spores and vegetative cells still entrapped within the high-dose capsules 56 days after vaccination suggesting that the controlled release could have continued for much longer (Fig. 5b).
According to previous work on mouse susceptibility to B. anthracis strains, the LD50 for BALB/cJ mice subcutaneously injected with the Sterne strain was 6.8 × 107 spores50. In this study, BALBc/J mice were subcutaneously injected with over 100-fold times more Sterne spores with only one death, implying that this microencapsulation method can allow for enhanced protection with higher Sterne spore doses and less reactogenicity. Inoculation with a higher dose of Sterne spores could also be critical for successful oral vaccination. Sterne spore exposure to acidic environments greatly reduces the viable spore titer (Fig. 2), so vaccinating with a higher dose of microencapsulated Sterne spores may account for any titer loss due to the gastric environment20.
Even more encouraging was the protection observed from the orally administered Low Dose Capsules. The antibody responses induced by oral vaccination depicted in Fig. 7b were produced from serum diluted 1:125 whereas the subcutaneous antibody responses depicted in Fig. 7a were produced from serum diluted 1:2000. Despite being much less concentrated according to the ELISA results, the antibody responses induced by oral vaccination with Low Dose Capsules were considered protective against LeTx challenge at the same serum dilution as subcutaneously vaccinated Low Dose Capsules (Fig. 8, Supplementary Table 2).
Similar to the response from the subcutaneously injected High Dose Capsules, it is also possible that the antibody response due to oral vaccination with Low Dose Capsules had not yet peaked prior to the end of the experiment. In fact, a significant antibody response wasn’t even detected until 31 days post vaccination (Fig. 7b). Given that the gastrointestinal emptying time for a mouse is <24 h51, the ELISA data suggest that coated capsules containing Sterne spores may be demonstrating the mucoadhesive properties of alginate by adhering to the intestinal lumen to gradually release their bacterial load22,52. This conclusion is also corroborated by the in vitro bacterial release experiment which demonstrated that significant amounts of Sterne spores were still entrapped within High Dose Capsules nearly two months after vaccination (Fig. 5). Continued exposure resulting from extended capsule stability acts as a self-contained booster effect and it is possible that oral vaccination with a higher dose of microencapsulated Sterne spores, or even a booster dose of the same vaccine may further enhance the orally induced immune response.
The findings of this study exemplify the advantages and efficacy of Sterne spore microencapsulation. We have demonstrated that the protein shell is essential for maintaining the controlled release aspects of alginate microcapsules. Our microcapsule formulation is also capable of sustaining Sterne spore viability in an acidic environment and of releasing viable Sterne cells for at least 56 days. Following a single vaccination dose in mice, microencapsulated Sterne spores generated a significant antibody response via subcutaneous, but more impressively, oral vaccination, both of which demonstrated partial to full protection during in vitro LeTx challenge. This immune response can be further enhanced by inoculating a higher bacterial dose with limited adverse effects.
While the results presented here reveal the great potential for this oral vaccine formulation, the majority of wildlife species affected by anthrax are ruminants and thus present further challenges to oral vaccination in the form of three additional stomachs and rumination53. Continued research is essential to optimize this vaccine for ruminant species. Future work will involve in vivo studies in a ruminant model to evaluate effective oral vaccination doses and the effect of vaccine boosters. It will also be critical to do an in vivo challenge experiment in a ruminant model to fully demonstrate the protective efficacy of this vaccine. Once the efficacy has been confirmed in a model more closely related to our target wildlife species, we will assess various methods to incorporate this vaccine into a wildlife bait to establish a practical wildlife vaccination method against anthrax. We will also fully explore the potential for environmental contamination with Sterne spores and ensure that no negative consequences will come of a vaccine-laden bait.
In summary, our study reports the achievement of an important first milestone toward the goal of oral vaccination against anthrax. We demonstrate the generation of protective antibody responses from oral vaccination with B. anthracis Sterne strain 34F2 spores and with further optimization, we believe this microcapsule formulation has the potential to adapt the Sterne spore for effective oral vaccination of free-ranging livestock and wildlife.
Methods
Preparation of Sterne spores
All bacteria used in this experiment were cultured from a vial of the Anthrax Spore Vaccine from Colorado Serum Company (Denver, CO, USA), the North American commercial producer of the Sterne vaccine. The Anthrax Spore Vaccine, which consists of live attenuated B. anthracis Sterne strain 34F2 spores in saponin, was used to inoculate a small volume of Luria Broth (LB) and cultured overnight at 37 °C with shaking12. The growth was pelleted by centrifugation at 3800 rpm for 15 min, resuspended in LB broth, then plated onto LB agar and incubated at 37 °C for 6 days to sporulate54–58. The full bacterial lawns were harvested from the plates and washed repeatedly with sterile water. Remaining vegetative cells were killed by heating at 68 °C for 1 h and removed by filtering through a 3.1 μm filter resulting in a suspension of pure Sterne spores. The final Sterne spore concentration was estimated by plating serial dilutions on LB agar.
Sterne spore response to simulated gastrointestinal environments
B. anthracis Sterne strain 34F2 spores were exposed to simulated gastric or intestinal fluids (GI fluids) to fully comprehend the obstacles to oral vaccination. Simulated gastric fluids consisted of 0.2% (w/v) NaCl and were adjusted to pH 2 and 5 with 1 M HCl to mimic the range of pHs in a non-fasted stomach33. Simulated intestinal fluids were 0.68% (w/v) K2HPO4 adjusted to pH 7 and 8 with 0.2 M NaOH33. The pH range convered by the prepared GI fluids was also representative of the environments throughout the ruminant digestive tract where the pH of the rumen is 6.5–7, the reticulum is ~6, the omasum is 4–5 and the abomasum is 2–453,59. A Sterne spore stock solution was prepared at an arbitrary concentration of 3.4 × 106 spores/ml. From this stock solution, 0.2 ml was used to inoculate 6.8 × 105 total Sterne spores into 5 ml of each GI fluid and MOPS Buffer (10 mM MOPS, 0.85% NaCl [pH 7.4]) as a control for future vaccine conditions. The starting spore titer of each inoculated GI fluid was determined by plating serial dilutions on LB agar, then the samples were placed on an orbital shaker at 37 °C. After an overnight incubation, the resulting spore concentration in the GI fluids was determined by plating serial dilutions. Data are reported as the average total recovered colony forming units (CFU) from each buffer.
Sterne vaccine preparation
The Anthrax Spore Vaccine is distributed by Colorado serum with a recommended 1 ml dose of between 4 × 106 and 6 × 106 viable Sterne spores in saponin for use in cattle, sheep, goats, swine, and horses12. This dosage range was simplified to 5 × 106 spores/ml for the purposes of this experiment and was used exactly as received from Colorado Serum Company.
Microencapsulation of B. anthracis Sterne strain 34F2 spores
Four different microcapsule vaccine formulations with and without the PLL and VpB coating (protein shell) were prepared for the experiments in this study: (i) microcapsules containing 5 × 106 spores/ml without the protein shell, (ii) empty microcapsules with the protein shell (Empty Capsules), (iii) microcapsules containing 5 × 106 spores/ml with the protein shell (Low Dose Capsules), and (iv) microcapsules containing 4 × 1010 spores/ml with the protein shell (High Dose Capsules) (Fig. 9).
Fig. 9. Illustration of microcapsules produced in this study.
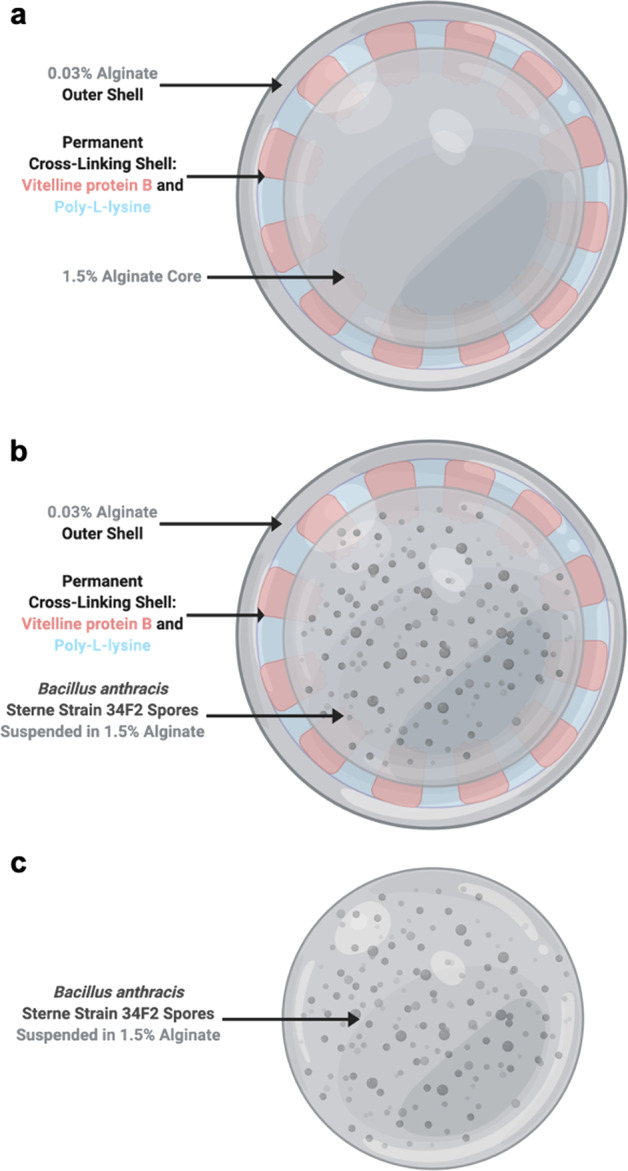
a Capsules without the protein shell loaded with Sterne spores, b Empty Capsules coated with the protein shell, c Low Dose Capsules loaded with Sterne spores and coated with protein shell. High Dose Capsules (not pictured) were also prepared like the Low Dose Capsules but with a higher amount of Sterne spores. Created with BioRender.com.
Microcapsules were prepared similar to previous studies31. Sodium alginate (NovaMatrix, Sandvika, Norway) was dissolved in MOPS buffer to a concentration of 1.5% (w/v) alginate. To make the low-dose capsules, 6 × 107 Sterne spores, as determined by the most recent stock titer results, were resuspended in 1 ml of MOPS buffer and then mixed with 5 ml of 1.5% (w/v) alginate solution. Microcapsules were formed using a Nisco Encapsulator VARV1 unit (Nisco Engineering AG, Zurich, Switzerland). The spore + alginate solution was extruded through a 170-μm nozzle, released directly into cross-linking solution (100 mM CaCl2, 10 mM MOPS) and stirred for 30 min. The capsules were thoroughly washed with MOPS and then coated with the protein shell by stirring for 30 min in 0.05% PLL and VpB in cross-linking solution. After another washing with MOPS, the capsules received an outer shell of 0.03% (w/v) alginate by mixing for 5 min. Final microcapsule vaccines (Fig. 9) were washed and resuspended 1:1 in MOPS for storage at 4 °C until use. Empty capsules were prepared as above but without any Sterne spores being added to the alginate and high-dose capsules were prepared with a higher amount of Sterne spores added to the alginate. The resulting dose of viable Sterne spores in the microcapsule vaccine was determined by dissolving 1 ml of capsules in 50 mM sodium citrate, 0.45% NaCl, 10 mM MOPS prior to permanent cross-linking with the protein shell31. All microcapsule batches were visualized in the brightfield and pixel intensities were measured in ImageJ.
Characterization of microcapsules in simulated gastrointestinal environments
Microcapsule morphology and bacterial presence within the alginate capsules were visualized with brightfield microscopy. Capsule responses, with and without the protein shell to simulated gastrointestinal fluids (GI fluids) were examined by suspending an aliquot of each capsule formulation in separate vials of the GI fluids. Vials were placed on a tube rocker at 37 °C and samples were collected at 30 and 90 min for imaging on an Olympus CKX41 microscope. Capsule diameters were measured in ImageJ.
Bacterial release from microcapsules
The bacterial release rates from the microcapsules were examined in vitro by suspending 1 ml of capsules in 9 ml of MOPS buffer and placing the tubes on a rocker at 37 °C31. At each sampling time point, the capsules were allowed to settle out of the buffer and then as much of the supernatant as possible was collected without disturbing the capsule pellet. The supernatant was plated on LB agar to estimate the bacterial release since the last time point. Capsules were resuspended in the same volume of MOPS buffer that had been removed and returned to the rocker at 37 °C. Samples were collected every day for 22 days, approximately every other day until day 38 and a final sample was collected at day 56 when the mouse study was terminated. Results are reported in terms of bacterial release per time point versus time.
Mouse immunizations
Female BALBc/J mice between four and six weeks of age were purchased from The Jackson Laboratory (Bar Harbor, ME, USA). Upon arrival at the animal facility, mice were randomly distributed into six groups of five mice each (Table 1) and allowed to acclimate for at least a week prior to any manipulation. All animal care and experimental procedures complied with all relevant ethical regulations for animal testing and research. The animal experiments conducted in this study received ethical approval from the Texas A&M University Institutional Animal Care and Use Committee (AUP # IACUC 2016-0112).
Mice were inoculated subcutaneously or by oral gavage with 0.2 ml of one of the four prepared vaccines: (i) Empty Capsules, (ii) Sterne vaccine, (iii) Low Dose Capsules, and (iv) High Dose Capsules (Table 1). All mice inoculated with either the Sterne vaccine or Low Dose Capsules received ~1 × 106 spores/mouse while mice inoculated with the High Dose Capsules received ~9 × 109 spores/mouse. The Empty Capsules served as the unvaccinated control. Antibody responses were evaluated in blood samples that were collected 3–7 days prior to vaccination and then every 10–14 days after vaccination for 8 weeks.
Detection of anthrax-specific antibody levels
Anthrax-specific antibody levels against protective antigen were measured by ELISA12. High binding ELISA plates were coated with 100 ng per well of anthrax protective antigen (List Biological Laboratories Inc., Campbell, CA, USA) in carbonate buffer, pH 9.6 and incubated at 37 °C for 1 h, then overnight at 4 °C. The plates were washed 3–5 times with phosphate buffered saline containing 0.5% Tween 20 (PBST). This washing step was repeated between each of the following steps. Next, the plates were blocked for 1 h at 37 °C with 100 μl per well of 1% (w/v) bovine serum albumin in PBST (1% BSA). Serial dilutions of all serum samples were prepared in 1% BSA, loaded 100 μl per well and incubated for 1 h at 37 °C. The secondary antibody, Anti-Mouse IgG (H + L) (SeraCare, Milford, MA, USA, Catalog # 074-1806) was diluted 1:5000 in 1% BSA and loaded 100 μl to a well with a 1 h incubation at 37 °C. TMB/E Substrate (Sigma-Aldrich, St. Louis, MO, USA) was added to each well and the reaction was stopped after 12 min with the addition of 100 μl of 0.5 M H2SO4. The optical density of all wells was read on a Tecan Infinite F50 Plate Reader at 450 nm. Samples (n = 5) from each time point, at each dilution were run in duplicate and experiments were repeated at least three times. Results are reported as average absorbance values for a single dilution for all vaccination groups at each time point. Also reported are the measured antibody titers as the reciprocal of the maximum dilution giving an absorbance greater than two standard deviations above the unvaccinated control.
Lethal toxin neutralization assays
Toxin neutralization assays were performed to determine the ability of collected serum samples to inhibit the cytotoxicity of anthrax lethal toxin (LeTx) in vitro14,15,48. J774A.1 macrophages (ATCC, Manassas, VA, USA, Catalog # TIB-67) were cultured in Dulbecco’s modified eagle medium (DMEM, HyClone) with 10% (w/v) fetal bovine serum (FBS) and 1% (w/v) penicillin. Upon reaching confluency, the cells were harvested and quantified using a hemocytometer, then brought to a final concentration of 5 × 104 cells/ml. Cells were added to a 96-well flat-bottom tissue culture plate at 200 μl/well and incubated overnight at 37 °C in 5% CO2. LeTx was prepared by adding lethal factor (List Biological Laboratories Inc., Campbell, CA, USA) and protective antigen (List Biological Laboratories Inc., Campbell, CA, USA) to DMEM containing 10% FBS and no antibiotic at concentrations of 0.25 and 0.1 μg/ml, respectively. The LeTx mixture was used to make serial dilutions of the collected mouse serum samples from each time point on a separate 96-well cell culture plate and then incubated for 1 h at 37 °C, 5% CO2. The media was removed from the prepared macrophage plate and replaced with 100 μl/well of the serum LeTx mixture in triplicate. After incubating for 4 h at 37 °C, 5% CO2, 10 μl of MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide; Roche, Basel, Switzerland) was added to each well and incubated for another 4 h at 37 °C, 5% CO2. Any remaining metabolically active cells reduced MTT, a yellow tetrazolium salt, to purple formazan crystals using NAD(P)H-dependent oxidoreductase enzymes. The insoluble formazan crystals were dissolved by adding 100 μl of solubilization solution (Roche, Basel, Switzerland) to each well and plates were incubated overnight at 37 °C, 5% CO2. The optical density of each well was read at 595 nm using a Tecan Infinite F50 Plate Reader. Cells that were exposed to only LeTx and no serum were used as a positive control. Cells that did not receive any LeTx or serum were used to determine 100% cell viability. The LeTx neutralizing abilities of collected serum samples are reported as average absorbance values for a single dilution for all vaccination groups at each time point from all repetitions of the experiment. Also included are the LeTx neutralizing antibody titers (NT50) reported as the maximum dilution that resulted in over 50% protection which were calculated as
Statistical analysis
Differences between starting and ending titers for Sterne spore responses to GI fluids, and the difference between microcapsule image pixel intensities were determined by two-sided Student’s t-tests with p < 0.05 considered significant. Across all other experiments, results are expressed as mean values ± standard deviations for all replicates at each time point for each group. Statistical analysis was performed using one-way ANOVA followed by the Tukey–Kramer HSD test with p < 0.05 considered significant.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Supplementary information
Acknowledgements
The authors thank Dr. Randall Berrier at Colorado Serum Company for generously providing multiple bottles of the Anthrax Spore Vaccine for use in this study. This work was supported by a faculty start-up grant from Texas A&M University to W.C., a Graduate Student Research Trainee Grant awarded to J.S.B. by Texas A&M University College of Veterinary Medicine and Biomedical Sciences and a Wild Animal Health Fund grant awarded to J.S.B. and W.C. from the American Association of Zoo Veterinarians.
Author contributions
All work done in this study was included in J.S.B.’s doctoral research project. J.S.B. designed and conducted all experiments, analyzed the data and wrote the article. S.P.C. assisted with designing and conducting all experiments, provided guidance for data analysis and approved the final paper. W.C., A.C.R-F., T.A.F., and Y.X. provided funding, equipment and guidance, and approved the final paper.
Data availability
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
Competing interests
A.C.R-.F. is a managing partner of NanoRelease Technologies LLC (NRT), a San Antonio-based company specializing in vaccine delivery platforms. The terms of this arrangement have been reviewed and approved by TXAgriLife Research and Texas A&M University in accordance with their conflict of interest policies.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
8/20/2021
A Correction to this paper has been published: 10.1038/s41541-021-00374-9
Supplementary information
Supplementary information is available for this paper at 10.1038/s41541-020-0208-3.
References
- 1.Hugh-Jones, M. E. & de Vos, V. Anthrax and wildlife. Rev. Sci. Tech.21, 359–383, 10.20506/rst.21.2.1336 (2002). [DOI] [PubMed]
- 2.Turnbull, P. C. B. & Shadomy, S. V. Anthrax from 5000 BC to AD 2010. In Bacillus anthracis and Anthrax (ed. Bergman, N. H.). 1–15 John Wiley & Sons, Inc., 10.1002/9780470891193 (2010).
- 3.Carlson CJ, et al. The global distribution of Bacillus anthracis and associated anthrax risk to humans, livestock and wildlife. Nat. Microbiol. 2019;4:1337–1343. doi: 10.1038/s41564-019-0435-4. [DOI] [PubMed] [Google Scholar]
- 4.Sterne M. Distribution and economic importance of anthrax. Fed. Proc. 1967;26:1493–1495. [PubMed] [Google Scholar]
- 5.Kracalik I, et al. Changing livestock vaccination policy alters the epidemiology of human anthrax, Georgia, 2000–2013. Vaccine. 2017;35:6283–6289. doi: 10.1016/j.vaccine.2017.09.081. [DOI] [PubMed] [Google Scholar]
- 6.Scorpio A, Blank TE, Day WA, Chabot DJ. Anthrax vaccines: pasteur to the present. Cell. Mol. Life Sci. 2006;63:2237–2248. doi: 10.1007/s00018-006-6312-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turnbull, P. (ed) Anthrax in Humans and Animals (World Health Organization and International Office of Epizootics, 2008).
- 8.Brossier F, Mock M, Sirard JC. Antigen delivery by attenuated Bacillus anthracis: new prospects in veterinary vaccines. J. Appl. Microbiol. 1999;87:298–302. doi: 10.1046/j.1365-2672.1999.00895.x. [DOI] [PubMed] [Google Scholar]
- 9.Hugh-Jones M, Blackburn J. The ecology of Bacillus anthracis. Mol. Asp. Med. 2009;30:356–367. doi: 10.1016/j.mam.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 10.Fasanella A, Galante D, Garofolo G, Jones MH. Anthrax undervalued zoonosis. Vet. Microbiol. 2010;140:318–331. doi: 10.1016/j.vetmic.2009.08.016. [DOI] [PubMed] [Google Scholar]
- 11.Hudson MJ, et al. Bacillus anthracis: balancing innocent research with dual-use potential. Int. J. Med. Microbiol. 2008;298:345–364. doi: 10.1016/j.ijmm.2007.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Benn Felix J, Chaki SP, Ficht TA, Rice-Ficht AC, Cook W. Bacillus anthracis Sterne Strain 34F2 vaccine antibody dose response by subcutaneous and oral administration. Poult. Fish. Wildl. Sci. 2019;7:206. [Google Scholar]
- 13.Aloni-Grinstein R, et al. Oral spore vaccine based on live attenuated nontoxinogenic Bacillus anthracis expressing recombinant mutant protective antigen. Infect. Immun. 2005;73:4043–4053. doi: 10.1128/IAI.73.7.4043-4053.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gorantala J, et al. A plant based protective antigen [PA(dIV)] vaccine expressed in chloroplasts demonstrates protective immunity in mice against anthrax. Vaccine. 2011;29:4521–4533. doi: 10.1016/j.vaccine.2011.03.082. [DOI] [PubMed] [Google Scholar]
- 15.Gorantala J, et al. Generation of protective immune response against anthrax by oral immunization with protective antigen plant-based vaccine. J. Biotechnol. 2014;176:1–10. doi: 10.1016/j.jbiotec.2014.01.033. [DOI] [PubMed] [Google Scholar]
- 16.Sim, B. K. L. et al. Protection against inhalation anthrax by immunization with Salmonella enterica serovar Typhi Ty21a stably producing protective antigen of Bacillus anthracis. npj Vaccines. 10.1038/s41541-017-0018-4 (2017). [DOI] [PMC free article] [PubMed]
- 17.Brossier F, Levy M, Mock M. Anthrax spores make an essential contribution to vaccine efficacy. Infect. Immun. 2002;70:661–664. doi: 10.1128/iai.70.2.661-664.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choo M-K, et al. TLR sensing of bacterial spore-associated RNA triggers host immune responses with detrimental effects. J. Exp. Med. 2017;214:1297–1311. doi: 10.1084/jem.20161141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rice-Ficht AC, Arenas-Gamboa AM, Kahl-McDonagh MM, Ficht TA. Polymeric particles in vaccine delivery. Curr. Opin. Microbiol. 2010;13:106–112. doi: 10.1016/j.mib.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 20.Cook MT, Tzortzis G, Charalampopoulos D, Khutoryanskiy VV. Microencapsulation of probiotics for gastrointestinal delivery. J. Control. Release. 2012;162:56–67. doi: 10.1016/j.jconrel.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Simó, G., Fernández-Fernández, E., Vila-Crespo, J., Ruipérez, V. & Rodríguez-Nogales, J. M. Research progress in coating techniques of alginate gel polymer for cell encapsulation. Carbohydr. Polym.10.1016/j.carbpol.2017.04.013 (2017). [DOI] [PubMed]
- 22.Gombotz WR, Wee SF. Protein release from alginate matrices. Adv. Drug Deliv. Rev. 2012;64:194–205. doi: 10.1016/s0169-409x(97)00124-5. [DOI] [PubMed] [Google Scholar]
- 23.Sundar S, Kundu J, Kundu SC. Biopolymeric nanoparticles. Sci. Technol. Adv. Mater. 2010;11:014104. doi: 10.1088/1468-6996/11/1/014104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De S, Robinson D. Polymer relationships during preparation of chitosan–alginate and poly-l-lysine–alginate nanospheres. J. Control. Release. 2003;89:101–112. doi: 10.1016/s0168-3659(03)00098-1. [DOI] [PubMed] [Google Scholar]
- 25.Martín MJ, Lara-Villoslada F, Ruiz MA, Morales ME. Microencapsulation of bacteria: a review of different technologies and their impact on the probiotic effects. Innov. Food Sci. Emerg. Technol. 2015;27:15–25. [Google Scholar]
- 26.Thu B, et al. Alginate polycation microcapsules: I. Interaction between alginate and polycation. Biomaterials. 1996;17:1031–1040. doi: 10.1016/0142-9612(96)84680-1. [DOI] [PubMed] [Google Scholar]
- 27.Herbert Waite J, Rice-Ficht AC. Eggshell precursor proteins of Fasciola hepatica, II. Microheterogeneity in vitelline protein B. Mol. Biochem. Parasitol. 1992;54:143–151. doi: 10.1016/0166-6851(92)90107-u. [DOI] [PubMed] [Google Scholar]
- 28.Rice-Ficht AC, Dusek KA, John Kochevar G, Herbert Waite J. Eggshell precursor proteins of Fasciola hepatica, I. Structure and expression of vitelline protein B. Mol. Biochem. Parasitol. 1992;54:129–141. doi: 10.1016/0166-6851(92)90106-t. [DOI] [PubMed] [Google Scholar]
- 29.Arenas-Gamboa AM, et al. Oral vaccination with microencapsuled Strain 19 vaccine confers enhanced protection against Brucella abortus strain 2308 challenge in Red deer (Cervus elaphus elaphus) J. Wildl. Dis. 2009;45:1021–1029. doi: 10.7589/0090-3558-45.4.1021. [DOI] [PubMed] [Google Scholar]
- 30.Arenas-Gamboa AM, Ficht TA, Kahl-McDonagh MM, Gomez G, Rice-Ficht AC. The Brucella abortus S19 ∆vjbR live vaccine candidate is safer than S19 and confers protection against wild-type challenge in BALB/c mice when delivered in a sustained-release vehicle. Infect. Immun. 2009;77:877–884. doi: 10.1128/IAI.01017-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arenas-Gamboa AM, Ficht TA, Kahl-McDonagh MM, Rice-Ficht AC. Immunization with a single dose of a microencapsulated Brucella melitensis mutant enhances protection against wild-type challenge. Infect. Immun. 2008;76:2448–2455. doi: 10.1128/IAI.00767-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arenas-Gamboa AM, et al. Enhanced immune response of red deer (Cervus elaphus) to live RB51 vaccine strain using composite microspheres. J. Wildl. Dis. 2009;45:165–173. doi: 10.7589/0090-3558-45.1.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cook MT, Tzortzis G, Charalampopoulos D, Khutoryanskiy VV. Production and evaluation of dry alginate-chitosan microcapsules as an enteric delivery vehicle for probiotic bacteria. Biomacromolecules. 2011;12:2834–2840. doi: 10.1021/bm200576h. [DOI] [PubMed] [Google Scholar]
- 34.Meeusen ENT, Walker J, Peters A, Pastoret PP, Jungersen G. Current status of veterinary vaccines. Clin. Microbiol. Rev. 2007;20:489–510. doi: 10.1128/CMR.00005-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.CDC & Ncird. U.S. Vaccines: Table 1 and Table 2.https://www.cdc.gov/vaccines/pubs/pinkbook/downloads/appendices/B/us-vaccines.pdf (2019).
- 36.Vela Ramirez, J. E., Sharpe, L. A. & Peppas, N. A. Current state and challenges in developing oral vaccines. Adv. Drug Delivery Rev.10.1016/j.addr.2017.04.008 (2017). [DOI] [PMC free article] [PubMed]
- 37.Gåserød O, Sannes A, Skjåk-Bræk G. Microcapsules of alginate-chitosan. II. A study of capsule stability and permeability. Biomaterials. 1999;20:773–783. doi: 10.1016/s0142-9612(98)00230-0. [DOI] [PubMed] [Google Scholar]
- 38.Thu B, et al. Alginate polycation microcapsules: II. Some functional properties. Biomaterials. 1996;17:1069–1079. doi: 10.1016/0142-9612(96)85907-2. [DOI] [PubMed] [Google Scholar]
- 39.Kuo CK, Ma PX. Maintaining dimensions and mechanical properties of ionically crosslinked alginate hydrogel scaffolds in vitro. J. Biomed. Mater. Res. - Part A. 2008 doi: 10.1002/jbm.a.31375. [DOI] [PubMed] [Google Scholar]
- 40.Chuang, J. J. et al. Effects of pH on the shape of alginate particles and its release behavior. Int. J. Polym. Sci. 2017, (2017).
- 41.Rasel, M. A. T. & Hasan, M. Formulation and evaluation of floating alginate beads of diclofenac sodium. Dhaka Univ. J. Pharm. Sci. 10.3329/dujps.v11i1.12484 (2012).
- 42.Iyer C, Kailasapathy K. Effect of co-encapsulation of probiotics with prebiotics on increasing the viability of encapsulated bacteria under in vitro acidic and bile salt conditions and in yogurt. J. Food Sci. 2005;70:M18–M23. [Google Scholar]
- 43.Li XY, et al. Preparation of alginate coated chitosan microparticles for vaccine delivery. BMC Biotechnol. 2008;8:1–11. doi: 10.1186/1472-6750-8-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Praepanitchai, O. A., Noomhorm, A., Anal, A. K. & Potes, M. E. Survival and behavior of encapsulated probiotics (Lactobacillus plantarum) in calcium-alginate-soy protein isolate-based hydrogel beads in different processing conditions (pH and temperature) and in pasteurized mango juice. Biomed Res. Int. 2019 (2019). [DOI] [PMC free article] [PubMed]
- 45.Storni, T., Kündig, T. M., Senti, G. & Johansen, P. Immunity in response to particulate antigen-delivery systems. Adv. Drug Delivery Rev.10.1016/j.addr.2004.09.008 (2005). [DOI] [PubMed]
- 46.Csaba, N. et al. Trimethyl chitosan nanoparticles encapsulated protective antigen Protects the mice against anthrax. Front. Immunol. 10.3389/fimmu.2018.00562 (2018). [DOI] [PMC free article] [PubMed]
- 47.Shakya KP, Hugh-Jones ME, Elzer PH. Evaluation of immune response to orally administered Sterne strain 34F2 anthrax vaccine. Vaccine. 2007;25:5374–5377. doi: 10.1016/j.vaccine.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 48.Hanson JF, Taft SC, Weiss AA. Neutralizing antibodies and persistence of immunity following anthrax vaccination. Clin. Vaccin. Immunol. 2006;13:208–213. doi: 10.1128/CVI.13.2.208-213.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reuveny S, et al. Search for correlates of protective immunity conferred by anthrax vaccine. Infect. Immun. 2001;69:2888–2893. doi: 10.1128/IAI.69.5.2888-2893.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Welkos SL, Keener TJ, Gibbs PH. Differences in susceptibility of inbred mice to Bacillus anthracis. Infect. Immun. 1986;51:795–800. doi: 10.1128/iai.51.3.795-800.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jang S-F, et al. Size discrimination in rat and mouse gastric emptying. Biopharm. Drug Dispos. 2013;34:107–124. doi: 10.1002/bdd.1828. [DOI] [PubMed] [Google Scholar]
- 52.McGhee JR, et al. The mucosal immune system: from fundamental concepts to vaccine development. Vaccine. 1992;10:75–88. doi: 10.1016/0264-410x(92)90021-b. [DOI] [PubMed] [Google Scholar]
- 53.Vandamme TF, Ellis KJ. Issues and challenges in developing ruminal drug delivery systems. Adv. Drug Deliv. Rev. 2004;56:1415–1436. doi: 10.1016/j.addr.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 54.Xu Y, Liang X, Chen Y, Koehler TM, Hook M. Identification and biochemical characterization of two novel collagen binding MSCRAMMs of Bacillus anthracis. J. Biol. Chem. 2004;279:51760–51768. doi: 10.1074/jbc.M406417200. [DOI] [PubMed] [Google Scholar]
- 55.Russell BH, Vasan R, Keene DR, Xu Y. Bacillus anthracis internalization by human fibroblasts and epithelial cells. Cell. Microbiol. 2007;9:1262–1274. doi: 10.1111/j.1462-5822.2006.00869.x. [DOI] [PubMed] [Google Scholar]
- 56.Russell BH, Vasan R, Keene DR, Koehler TM, Xu Y. Potential dissemination of Bacillus anthracis utilizing human lung epithelial cells. Cell. Microbiol. 2008;10:945–957. doi: 10.1111/j.1462-5822.2007.01098.x. [DOI] [PubMed] [Google Scholar]
- 57.Jenkins SA, Xu Y. Characterization of Bacillus anthracis persistence in vivo. PLoS ONE. 2013;8:1–9. doi: 10.1371/journal.pone.0066177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Basu S, et al. Role of Bacillus anthracis spore structures in macrophage cytokine responses. Infect. Immun. 2007;75:2351–2358. doi: 10.1128/IAI.01982-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Parish, J., Rivera, J. & Boland, H. Understanding the ruminant animal digestive system. Mississippi State University, Extension Service. 1–5. http://extension.msstate.edu/publications/publications/understanding-the-ruminant-animal-digestive-system#:~:text=True%20ruminants%2C%20such%20as%20cattle,significantly%20into%20the%20right%20side (2009).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article (and its supplementary information files).