Abstract
Background
Despite recent growth in palliative care programs palliative care remains underutilized. Studies suggest that patients and providers commonly associate palliative care with end of life, often leading to misconceptions and late referrals.
Objective
To characterize self-reported palliative care knowledge and misconceptions about palliative care among US adults and demographic, health, and social role factors associated with knowledge and misconceptions.
Design
We conducted secondary data analysis of nationally representative, self-reported data from the 2018 Health Information National Trends Survey (HINTS) 5, Cycle 2. We examined associations between knowledge and misconceptions about palliative care together with demographics, health care access, health status, and social roles.
Participants
3504 US adults. 2594 included in the first analysis after omitting missing cases; 683 who reported knowing about palliative care were included in the second analysis.
Main Measures
Palliative care knowledge was self-reported in response to: “How would you describe your level of knowledge about palliative care?” Level of misconceptions was based on a series of factual and attitudinal statements about palliative care.
Key Results
Among US adults, 28.8% report knowing about palliative care, but only 12.6% report knowing what palliative care is and hold no misconceptions. Those most likely to report knowing about palliative care are female, college-educated, higher income, have a primary health care provider, or are a caregiver. Among those who report knowing about palliative care, misconceptions were common: 44.4% automatically think of death, 38.0% equate palliative care with hospice, 17.8% believe you must stop other treatments, and 15.9% see palliative care as giving up.
Conclusions
US adults who have some knowledge of palliative care are most likely to confuse it with hospice but are less likely to see it as requiring forgoing treatment or as giving up. Primary care clinicians should be encouraged to communicate about palliative care with patients.
KEY WORDS: palliative care, primary care, misconceptions
BACKGROUND
Palliative care is a health care specialty aimed at improving quality of life and relieving suffering for patients of any age or stage of disease. Specialty palliative care is provided by a team, including physicians, nurses, social workers, and chaplains to manage pain and symptoms associated with serious illness, promote illness understanding, enable treatment decisions aligned with goals of care, and to support care coordination across settings and specialties.1 Palliative care is appropriate no matter the age or stage of serious illness and is not associated with end of life or terminal illness.2 Evidence shows that patients living with serious illness, their family members, and the health care system can benefit from palliative care.1 Early integration of palliative care alongside disease-directed treatment can improve quality of life and reduce health care costs.2–6 Over the past decade, palliative care programs in hospital and community-based settings have grown dramatically.2 Still, despite increasing demand for services, palliative care remains underutilized and misunderstood.2, 7, 8
Inadequate knowledge and misconceptions lead to apprehension among patients and have been identified as barriers to the use of palliative care.7, 9, 10 Many wrongly believe palliative care is the same as hospice or associate it only with end of life.1, 10, 11 These misconceptions may also influence providers, who have reported that they worry recommending patients for palliative care could result in a loss of hope, or lead the patient to believe their provider is giving up on them.1, 9 Yet, research suggests that once consumers are aware of the benefits of palliative care, there is broad support for its value and role for patients with serious illness, no matter the age or stage.10
While qualitative studies and surveys in convenience samples have documented misconceptions related to palliative care,7, 9, 10 there are no national estimates for the magnitude of these misconceptions. Using a nationally representative sample of US adults, this study provides insight into the extent of these misconceptions and an examination of variability based on demographic and social characteristics.
OBJECTIVE
The objective of this study is to provide a robust baseline for palliative care knowledge and misconceptions in the general population and offer insights into the demographic, health care access, health status, and social role characteristics that are associated with greater knowledge and misconceptions. The purpose is to enable better targeting of public education strategies.
We hypothesize that a range of personal health status and social role characteristics (i.e., previous cancer diagnosis, poor health status, status as a widow, and status as a caregiver) would have a greater likelihood of exposing people to palliative care services and those respondents would report greater knowledge and fewer misconceptions.
METHODS
Data Source
This cross-sectional study uses data from the Health Information National Trends Survey (HINTS) 5, Cycle 2, conducted in 2018 (n = 3504) by the National Cancer Institute (NCI).12 The sample is nationally representative and the data are self-reported with the option of survey responses in English and Spanish.12 Post-collection weighting adjusted for household size and non-response.
Historically, NCI adds new questions based on trending topics and recent developments in communication and cancer care.12 In HINTS 5, Cycle 2, five questions about palliative care were added to Section F.12 The five questions about palliative care include the following: level of knowledge (F1), goals of palliative care (F2), where you would go first for information about palliative care (F3), most trusted source of information about palliative care (F4), and perceptions about palliative care (F5). We examined associations between knowledge and perceptions of palliative care together with demographics, health care access, health status, caregiver status, and previous cancer diagnosis.12
Sample Measures
Knowledge
The first of our two dependent variables was defined as “knowing about palliative care.” In question F1 of the survey instrument, respondents were asked: “How would you describe your level of knowledge about palliative care?” Three response items were provided, and we dichotomized “I know a little bit about palliative care” or “I know what palliative care is and could explain it to someone else” as “yes” and “I’ve never heard of it” as “no.”13
Misconceptions
The second dependent variable was the level of misconceptions about palliative care. In the administration of HINTS by NCI, questions about misconceptions were only asked of respondents who reported at least “know a little bit” in question F1 (and were coded as “yes” for knowing about palliative care in our analysis). Misconceptions were based on responses to four survey items in question F5.13 The items are consistent with palliative care definitions from the World Health Organization (WHO) and the National Consensus Project for Quality Palliative Care14, 15 and were administered as follows: “How much do you agree or disagree with the following statements about palliative care?” (1—Strongly Agree, 2—Somewhat Agree, 3—Somewhat Disagree, 4—Strongly Disagree, 5—Don’t Know) for the following four statements: “accepting palliative care means giving up,” “if you accept palliative care, you must stop other treatments,” “palliative care is the same as hospice care,” and “when I think of ‘palliative care,’ I automatically think of death.”13 All of these statements associate palliative care with end-of-life, hospice, or forgoing other treatments—common misconceptions reported in the literature.1, 2 Therefore, we categorized agreement (i.e., a response of 1 or 2) with these responses as misconception, disagreement (i.e., a response of 3 or 4) as accurate knowledge, and do not know (i.e., a response of 5) as missing. The resultant variables were treated in two ways: First, in data visualization, we preserved the distinctions between strongly and somewhat agree and disagree to capture how strongly held the misconception was. Second, in regression analysis, we modeled the response as total number of misconceptions (ranging from 0 to 4) as a count variable.
The HINTS survey included one more item related to palliative care in question F5, but we did not include it in our variable for misconceptions. The item is “it is a doctor’s obligation to inform all patients with cancer about the option of palliative care.” While agreement with this response focuses on greater integration of palliative care in cancer care, and would generally be aligned with greater upstream integration of palliative care, we excluded it since it relates more to a professional organizations assessment of appropriate referrals, rather than a broader understanding or misunderstanding of the field of palliative care.16
Statistical Analysis
We controlled for characteristics expected to increase the likelihood of a need for and/or the potential for greater interaction with palliative care. Drawing on the literature and expert knowledge, we compiled a causal framework focusing on four specific domains that we expected might impact an individual’s knowledge and perceptions about palliative care:17 demographics, health care access, health status, and social roles. Demographics includes age (in years), gender (“male,” “female”), race/ethnicity (“Non-Hispanic White,” “Non-Hispanic Black,” “Hispanic,” “Non-Hispanic Asian,” and “Non-Hispanic Other”), education (recoded to “Less than high school,” “High school to some college,” and “College or above”), and income (9-level categorical variable ranging from < US$9999 to $200,000 or more, in increments of $5000, $15,000, and $25,000). The second domain, health care access, includes the types of insurance by which the respondent was covered at the time of survey, and whether the respondent reports having a primary health care provider. The third domain highlights characteristics of respondents that would be more likely to have a need for palliative care, including health status (self-reported with a five-level Likert scale, recoded to fair/poor health status vs. excellent/very good/good health; and whether the person was ever diagnosed with cancer) and social roles (marital status, with an interest in widowed, and current status as a caregiver (i.e., whether they had performed any caregiving for someone with medical, behavioral, disability, or other condition)).
Descriptive statistics of the chosen variables and their unadjusted association with “knowing palliative care” were derived and tabulated. For regression analysis predicting “knowing palliative care,” we chose binary logistic regression which accommodates the dichotomous nature of the response variable.18 To assess the relationship between individual characteristics and number of misconceptions about palliative care, we conducted Poisson regression, which is fit for count outcomes such as the number of misconceptions.18 For both regression models, we first performed univariate models using each independent variable individually, followed by an adjusted model with all proposed factors included in the model. For continuous predictors, quadratic and cubic terms were also included initially to capture potential non-linear relationships. Non-significant quadratic and cubic terms were subsequently removed from the model. Based on this method, the quadratic term of age was retained in the adjusted logistic model. Statistical significance was determined based on p value < 0.05. For categorical variables, an overall log-likelihood ratio test was first performed, and we only interpreted the p values of the dummy variables if the overall test was statistically significant. All analyses used Stata 15 SE (StataCorp, College Station, TX, USA) and adjusted for the complex sampling weight feature of HINTS.
RESULTS
Less than one-third (28.8%) of the US adult population reports knowing about palliative care, with 17.9% knowing a little bit and 10.8% knowing well enough to explain to others. The multivariable logistic regression model (N = 2594) reveals that female gender and being college-educated are associated with a greater likelihood of knowing about palliative care. Age has an inverted u-shaped relationship, with people around 60 years old knowing more about palliative care. Income levels lower than $9999 (vs. $50,000 to $74,999) are associated with a lower likelihood of knowing about palliative care. Insurance status, health status, and cancer diagnosis were not associated with knowledge, but having a primary health care provider and being a caregiver were associated with a greater likelihood of knowing about palliative care (Table 1).
Table 1.
Descriptive Statistics and Logistic Regression, Knowing About Palliative Care
| Variable | Overall | Know about palliative care? (N = 3445)b | Multivariable logistic regression predicting the odds of knowing about palliative care (N = 2594) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Never heard of | A little/very well | |||||||||
| n | %a | n | %a | n | %a | p valuec | aOR | 95%CI | p value | |
| Never heard of palliative care | 2283 | 71.3% | 2.283 | – | 1162 | – | – | |||
| Age (years, mean, and 95%CI) | – | 49.0 (48.3, 49.7) | – | 47.6 (46.5, 48.7) | – | 54.8 (50.6, 53.0) | < 0.001 | 1.07 | 1.02, 1.13 | 0.012 |
| Age squared | – | – | – | – | – | 0.9994 | 0.9989, 0.9999 | 0.022 | ||
| Female | 2054 | 51.2% | 1205 | 45.8% | 806 | 64.0% | < 0.001 | 2.10 | 1.48, 2.97 | < 0.001 |
| Race/ethnicity | < 0.001 | 0.081d | ||||||||
| Non-Hispanic White | 1983 | 64.8% | 1165 | 60.6% | 796 | 75.8% | Ref. | – | – | |
| Non-Hispanic Black | 444 | 10.8% | 328 | 11.4% | 104 | 9.1% | 0.92 | 0.51, 1.67 | 0.786 | |
| Hispanic | 461 | 16.0% | 356 | 18.8% | 97 | 8.7% | 0.48 | 0.24, 0.94 | 0.032 | |
| Non-Hispanic Asian | 138 | 5.2% | 92 | 5.6% | 42 | 4.2% | 0.54 | 0.27, 1.06 | 0.071 | |
| Non-Hispanic Other | 125 | 3.3% | 83 | 3.7% | 40 | 2.2% | 0.80 | 0.39, 1.65 | 0.542 | |
| Education | < 0.001 | < 0.001d | ||||||||
| Less than HS | 275 | 9.0% | 240 | 11.2% | 23 | 2.5% | 0.54 | 0.17, 1.73 | 0.291 | |
| HS to some college | 1670 | 62.3% | 1215 | 66.8% | 424 | 51.0% | Ref. | – | – | |
| College or above | 1508 | 28.8% | 794 | 22.0% | 702 | 46.5% | 2.40 | 1.69, 3.40 | < 0.001 | |
| Income range, US$ | < 0.001 | 0.003d | ||||||||
| $0 to $9999 | 219 | 7.8% | 185 | 10.1% | 28 | 1.8% | 0.24 | 0.12, 0.48 | < 0.001 | |
| $10,000 to $14,999 | 183 | 5.2% | 138 | 5.8% | 42 | 3.6% | 0.66 | 0.22, 2.01 | 0.459 | |
| $15,000 to $19,999 | 177 | 4.7% | 137 | 5.1% | 35 | 3.6% | 0.97 | 0.46, 2.04 | 0.936 | |
| $20,000 to $34,999 | 428 | 11.9% | 294 | 12.4% | 126 | 10.3% | 0.92 | 0.51, 1.66 | 0.778 | |
| $35,000 to $49,999 | 404 | 13.5% | 283 | 15.0% | 115 | 9.4% | 0.60 | 0.35, 1.01 | 0.056 | |
| $50,000 to $74,999 | 567 | 17.8% | 380 | 18.5% | 184 | 16.6% | Ref. | – | – | |
| $75,000 to $99,999 | 364 | 12.6% | 212 | 11.4% | 149 | 15.6% | 1.49 | 0.76, 2.93 | 0.244 | |
| $100,000 to $199,999 | 548 | 19.4% | 288 | 16.5% | 252 | 26.4% | 1.29 | 0.77, 2.16 | 0.326 | |
| $200,000 or more | 197 | 7.2% | 83 | 5.1% | 112 | 12.7% | 1.81 | 0.97, 3.38 | 0.060 | |
| Insurance: Medicare | 1285 | 22.1% | 852 | 21.2% | 403 | 23.6% | 0.156 | 1.03 | 0.67, 1.59 | 0.885 |
| Insurance: Medicaid | 503 | 15.3% | 400 | 17.4% | 90 | 10.0% | < 0.001 | 0.98 | 0.47, 2.06 | 0.960 |
| Insurance: Private | 2225 | 66.0% | 1355 | 62.4% | 841 | 74.8% | < 0.001 | 0.72 | 0.42, 1.24 | 0.227 |
| Insurance: Other | 279 | 6.3% | 203 | 6.4% | 70 | 5.5% | 0.444 | 0.73 | 0.35, 1.51 | 0.388 |
| Insurance: Uninsured | 183 | 8.5% | 147 | 10.7% | 32 | 3.4% | < 0.001 | 0.44 | 0.16, 1.20 | 0.106 |
| Have a primary HC provider | 2470 | 65.5% | 1511 | 60.7% | 923 | 78.3% | < 0.001 | 1.50 | 1.05, 2.14 | 0.027 |
| Self-rated health as fair/poor | 554 | 14.8% | 408 | 16.6% | 134 | 10.0% | 0.003 | 0.84 | 0.49, 1.46 | 0.530 |
| Ever diagnosed w/cancer | 593 | 9.4% | 378 | 8.7% | 207 | 11.2% | 0.043 | 0.82 | 0.55, 1.23 | 0.331 |
| Marital status | < 0.001 | 0.364 d | ||||||||
| Married/living as married | 1747 | 52.5% | 1101 | 49.4% | 625 | 60.9% | Ref. | – | – | |
| Single | 605 | 30.4% | 430 | 34.0% | 165 | 21.5% | 0.96 | 0.60, 1.56 | 0.879 | |
| Divorced/separated | 668 | 11.9% | 431 | 11.9% | 225 | 11.5% | 1.33 | 0.89, 1.98 | 0.156 | |
| Widowed | 429 | 5.2% | 286 | 4.7% | 130 | 6.2% | 1.34 | 0.80, 2.24 | 0.267 | |
| Currently a caregiver | 484 | 14.9% | 262 | 12.0% | 210 | 21.2% | < 0.001 | 1.68 | 1.07, 2.64 | 0.024 |
Source/notes: Health Information National Trends Survey (HINTS) 5, Cycle 2, 2018. All results account for survey weights. Italicized numbers indicate aOR being statistically significant by itself (binary or continuous predictors) or as a group (categorical predictors). 95%CI: 95% confidence interval; aOR: adjusted odds ratio; HC: health care; HS: high school; Ref.: reference group
a: Frequencies are unweighted so they do not agree with the percentages; percentages, means and 95%CI, and ORs are weighted
b: Three choices are allowed for the question FI “How would you describe your level of knowledge about palliative care?” Answers “I know a little bit” and “I know what palliative care is and could explain it to someone else” were grouped together as “A little/very well”; answer “I’ve never heard of it” was listed as “Never heard of”
c: t test for age, χ2 test for others
d: p value of log likelihood ratio test of the whole categorical variable as a group. If this overall test is not statistically significant, the p values for the independent dummy variables inside the variable are not considered statistically significant
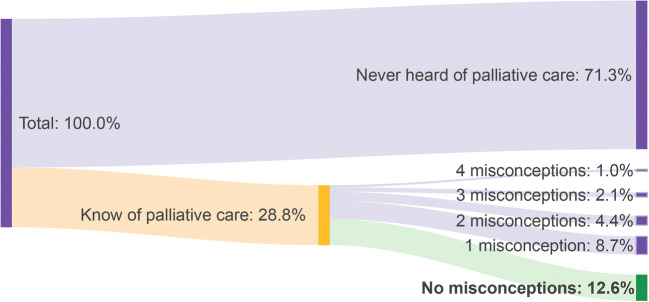
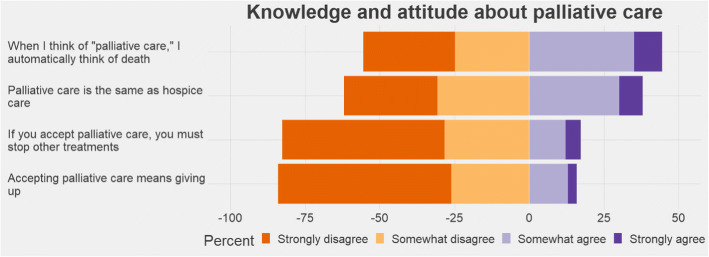
Only 12.6% of US adults have no misconceptions about palliative care (Fig. 1, N = 3445). Among respondents who reported knowing about palliative care, misconceptions were common. About 44.4% endorsed a statement that when they think of palliative care they automatically think of death, 38.0% responded that palliative care is the same as hospice care, 17.3% agreed that if you accept palliative care you must stop other treatments, and 15.9% suggested that accepting palliative care means giving up (Fig. 2). The multivariable Poisson regression (Subset N = 683) results suggest that among those who report knowing about palliative care, individuals who have less than a high school education, have private insurance, or are uninsured have a greater relative risk of holding a greater number of misconceptions. While income was overall a significant predictor (p = 0.0002), we do not observe a clear trend in the risk ratios along the income categories (Table 2).
Fig. 1.
Misconceptions about palliative care (N = 3445). Source/Notes: Source: Health Information National Trends Survey (HINTS) 5, Cycle 2, 2018. All results account for survey weights.
Fig. 2.
Knowledge and attitudes about palliative care, among people who report knowing about palliative care (N = 865). Source/Notes: Responses to question F5, Health Information National Trends Survey (HINTS) 5, Cycle 2, 2018. All results account for survey weights. Data on misconceptions about palliative care are only available for those who report knowing something about palliative care. The response “I don’t know” was omitted from this visualization.
Table 2.
Levels of Misconceptions About Palliative Care, Poisson Regression Results (N = 683)
| Variable | Multivariable Poisson regression predicting the numbers of misconceptions | ||
|---|---|---|---|
| aRR | 95%CI | p value | |
| Age (years, mean, and 95%CI) | 1.00 | 0.99, 1.01 | 0.462 |
| Female | 1.07 | 0.84, 1.36 | 0.575 |
| Race/ethnicity | 0.063 | ||
| Non-Hispanic White | Ref. | – | – |
| Non-Hispanic Black | 0.88 | 0.56, 1.39 | 0.586 |
| Hispanic | 0.97 | 0.49, 1.94 | 0.933 |
| Non-Hispanic Asian | 1.80 | 1.16, 2.79 | 0.010 |
| Non-Hispanic Other | 1.30 | 0.86, 1.96 | 0.205 |
| Education | 0.002 | ||
| Less than HS | 2.02 | 1.25, 3.25 | 0.005 |
| HS to some college | Ref. | – | – |
| College or above | 0.80 | 0.58, 1.10 | 0.171 |
| Income range, US$ | 0.033 | ||
| $0 to $9999 | 0.74 | 0.34, 1.59 | 0.435 |
| $10,000 to $14,999 | 1.08 | 0.61, 1.91 | 0.793 |
| $15,000 to $19,999 | 1.95 | 1.12, 3.39 | 0.019 |
| $20,000 to $34,999 | 1.13 | 0.78, 1.64 | 0.522 |
| $35,000 to $49,999 | 1.08 | 0.59, 1.95 | 0.807 |
| $50,000 to $74,999 | Ref. | – | – |
| $75,000 to $99,999 | 0.84 | 0.56, 1.26 | 0.388 |
| $100,000 to $199,999 | 1.08 | 0.76, 1.53 | 0.661 |
| $200,000 or more | 0.78 | 0.54, 1.12 | 0.174 |
| Insurance; Medicare | 1.00 | 0.69, 1.45 | 0.985 |
| Insurance: Medicaid | 1.46 | 0.75, 2.83 | 0.261 |
| Insurance: Private | 1.47 | 1.03, 2.11 | 0.036 |
| Insurance: Other | 0.98 | 0.58, 1.65 | 0.924 |
| Insurance: Uninsured | 2.78 | 1.57, 4.92 | 0.001 |
| Have a primary HC provider | 1.09 | 0.76, 1.57 | 0.639 |
| Self-rated health as fair/poor | 0.97 | 0.70, 1.35 | 0.849 |
| Ever diagnosed w/ cancer | 0.92 | 0.71, 1.20 | 0.544 |
| Marital status | 0.302 | ||
| Married/living as married | Ref. | – | – |
| Single | 0.87 | 0.57, 1.33 | 0.517 |
| Divorced/separated | 0.78 | 0.55, 1.11 | 0.167 |
| Widowed | 1.21 | 0.79, 1.84 | 0.376 |
| Currently a caregiver | 0.88 | 0.60, 1.30 | 0.519 |
Source/Notes: Health Information National Trends Survey (HINTS) 5, Cycle 2, 2018. All results account for survey weights. Italicized numbers indicate aRR being statistically significant by itself (binary or continuous predictors) or as a group (categorical predictors); a: p value of log likelihood ratio test of the whole categorical variable as a group. If this overall test is not statistically significant, the p values for the independent dummy variables inside the variable are not considered statistically significant; 95%CI: 95% confidence interval; aRR: adjusted rate ratio; HC: health care; HS: high school; Ref.: reference group
Limitations
This study is cross-sectional and therefore only captures one point in time with respect to knowledge and misconceptions about palliative care. Additionally, we are only able to assess the level of misconceptions among the population who report at least knowing a little bit about palliative care. The measure we use for caregiving is imperfect with respect to serious illness, as not all caregiving roles would indicate a need for palliative care (i.e., caregiving for a person with a developmental disability). Lastly, we have no way to capture how individuals have learned about palliative care, and whether primary care providers are the source of this information, despite associations between having a primary care provider and reporting greater knowledge of primary care.
DISCUSSION
These findings in this nationally representative sample provide insight into the public’s knowledge of palliative care. Palliative care is an important health care specialty that provides critical wraparound support for individuals with serious illness and their caregivers.11 Yet, most US adults report that they are not aware of palliative care, and those that report having some knowledge still have misconceptions.
This study further documents widespread lack of knowledge about palliative care. Lack of knowledge has already been shown to impede timely palliative care referrals, restrict informed decision-making based on robust communication and goals of care conversations, and undermine the prospect of truly patient-centered care.7, 11 However, among those reporting knowledge of palliative care, accurate perceptions were held more frequently than inaccurate ones. This suggests that current communications about palliative care are largely effective; however, they seem to be reaching very few US adults.
While this study documented the extent of misconceptions about palliative care among the public, prior research also noted the critical role of provider misconceptions in shaping patient access and referrals to palliative care.19 Studies suggest that providers often reserve palliative care referrals for care related to a terminal illness or symptom management, and assert that recommending patients for palliative care will result in a loss of hope, or lead the patient to believe their provider is giving up on them.1, 9, 19 The misconceptions assessed in this study directly address these fears. It is interesting to note that only 15% endorsed the statement that palliative care means giving up. Clinician training on communicating palliative care options should also dispel clinician misconceptions about patient reactions. Thus, strategies aimed at increasing awareness and countering broader public misconceptions must include efforts to address provider misconceptions.
Recent evidence suggests that we have a shortage of palliative care clinicians.2, 20 Thus, the finding that having a primary health care provider makes individuals more likely to know about palliative care suggests there is a valuable opportunity for enhancing education and training of non-palliative care providers in primary palliative care. To date, a range of medical student and provider education strategies have shown some promise for increasing knowledge of palliative care, as well as comfort with discussing complex pain and symptom management and advance care planning issues among patients with serious illness.19 Yet, there is little standardization across states for what these educational strategies should include,1 and many states still define palliative care within their hospice guidelines.21 Moreover, while a handful of states require primary care clinicians to provide information to patients about palliative care, these requirements are limited to patients with terminal illness.21 Together, these more limited strategies further the association between palliative care and end of life. Developing more robust, standardized education strategies together with state-level guidance for promoting earlier referrals could help to counter misconceptions about palliative care as end of life, better prepare primary care physicians to meet the needs of patients with serious illness, facilitate earlier referrals to specialty palliative care, and better prepare the non-palliative care workforce to deliver primary palliative care.
With the shift toward value-based health care, there are increasing opportunities to integrate palliative care earlier in the course of a serious illness in a way that creates aligned incentives for providers, payers, and patients.22 This integration should include further enhancement of primary palliative care competencies among primary care clinicians and specialists who see patients with serious illness and effective referral systems when specialty palliative care is warranted.23
Funding information
The Tufts Health Plan Professorship of Health Care Policy Research provided financial support for this analysis.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Prior Presentation This research was presented as a poster at the 2019 AcademyHealth Annual Research Meeting in Washington, DC.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Meier DE, Back AL, Berman A, Block SD, Corrigan JM, Morrison RS. A National Strategy For Palliative Care. Health Affairs. 2017;36(7):1265–73. doi: 10.1377/hlthaff.2017.0164. [DOI] [PubMed] [Google Scholar]
- 2.Aldridge MD, Hasselaar J, Garralda E, van der Eerden M, Stevenson D, McKendrick K, et al. Education, implementation, and policy barriers to greater integration of palliative care: A literature review. Palliat Med. 2016;30(3):224–39. doi: 10.1177/0269216315606645. [DOI] [PubMed] [Google Scholar]
- 3.Cunningham C, Travers K, Chapman R, Lawler E, Liu S, Pearson SD, et al. Palliative care in the outpatient setting: A comparative effectiveness report. Boston: Institute for Clinical and Economic Review; 2016. [Google Scholar]
- 4.Cassel JB. Palliative care's impact on utilization and costs: Implications for health services research and policy. In: Kelley AS, Meier DE, editors. Meeting the needs of older adults with serious illness: Challenges and opportunities in the age of health care reform. New York: Humana Press; 2014. pp. 109–26. [Google Scholar]
- 5.May P, Garrido MM, Cassel JB, Kelley AS, Meier DE, Normand C, et al. Palliative Care Teams’ Cost-Saving Effect Is Larger For Cancer Patients With Higher Numbers Of Comorbidities. Health Affairs. 2016;35(1):44–53. doi: 10.1377/hlthaff.2015.0752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.May P, Normand C, Cassel JB, Del Fabbro E, Fine RL, Menz R, et al. Economics of Palliative Care for Hospitalized Adults With Serious Illness: A Meta-analysis. JAMA Internal Medicine. 2018;178(6):820–9. doi: 10.1001/jamainternmed.2018.0750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schreibeis-Baum HC, Xenakis LE, Chen EK, Hanson M, Ahluwalia S, Ryan G, et al. A Qualitative Inquiry on Palliative and End-of-Life Care Policy Reform. Journal of palliative medicine. 2016;19(4):400–7. doi: 10.1089/jpm.2015.0296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Courtright KR, Cassel JB, Halpern SD. A Research Agenda for High-Value Palliative Care. Annals of Internal Medicine. 2018;168(1):71–2. doi: 10.7326/M17-2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ulrich Research Services . Palliative care key informant interviews. Boston, MA: Commonwealth of Massachusetts Department of Public Health; 2015. [Google Scholar]
- 10.Center to Advance Palliative Care . 2011 public opinion research on palliative care. New York: Center to Advance Palliative Care; 2011. [Google Scholar]
- 11.Kelley AS, Morrison RS. Palliative care for the seriously ill. New England Journal of Medicine. 2015;373(8):747–55. doi: 10.1056/NEJMra1404684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Westat . Health Information National Trends Survey 5 (HINTS 5): Cycle 2 Methodology Report. Bethesda, MD: National Cancer Institute; 2018. [Google Scholar]
- 13.Health Information National Trends Survey (HINTS): Annotated form cycle 2, English version. Washington, DC: National Institutes of Health, US Department of Health and Human Services. [Available from https://hints.cancer.gov/docs/Instruments/HINTS5_Cycle2_Annotated_Instrument_English.pdf].
- 14.World Health Organization. WHO Definition of Palliative Care 2019 [Available from: https://www.who.int/cancer/palliative/definition/en/]. Accessed 15 May 2019.
- 15.National Consensus Project for Quality Palliative Care . Clinical practice guidelines for quality palliative care. Richmond, VA: National Coalition for Hospice and Palliative Care; 2018. [Google Scholar]
- 16.Bickel KE, McNiff K, Buss MK, Kamal A, Lupu D, Abernethy AP, et al. Defining high-quality palliative care in oncology practice: An American Society of Clinical Oncology/American Academy of Hospice and Palliative Medicine Guidance Statement. Journal of Oncology Practice. 2016;12(9):e828–38. doi: 10.1200/JOP.2016.010686. [DOI] [PubMed] [Google Scholar]
- 17.Vittinghoff E, Glidden DV, Shiboski SC, McCullough CE. Regression methods in biostatistics: Linear, survival, and repeated measures models. 2. New York: Springer; 2012. [Google Scholar]
- 18.Ott RL, Longnecker M. An introduction to statistical methods and data analysis. 5. Duxbury: Pacific Grove, CA; 2001. [Google Scholar]
- 19.Roenn JHV, Voltz R, Serrie A. Barriers and Approaches to the Successful Integration of Palliative Care and Oncology Practice. 2013;11(suppl_1):S-11. [DOI] [PubMed]
- 20.Kamal AH, Wolf SP, Troy J, Leff V, Dahlin C, Rotella JD, et al. Policy Changes Key To Promoting Sustainability And Growth Of The Specialty Palliative Care Workforce. Health Aff. 2019;38(6):910–8. doi: 10.1377/hlthaff.2019.00018. [DOI] [PubMed] [Google Scholar]
- 21.Donlon R, Purington K, Williams N. Advancing palliative care for adults with serious illness: A national review of state palliative care policies and programs. Washington, DC: NASHP; 2018. [Google Scholar]
- 22.Bleser WK, Saunders RS, Winfield L, Japinga M, Smith N, Kaufman BG, et al. ACO Serious Illness Care: Survey And Case Studies Depict Current Challenges And Future Opportunities. 2019;38(6):1011–20. [DOI] [PubMed]
- 23.Carroll T, Weisbrod N, O'Connor A, Quill T. Primary Palliative Care Education: A Pilot Survey. The American journal of hospice & palliative care. 2018;35(4):565–9. doi: 10.1177/1049909117723618. [DOI] [PubMed] [Google Scholar]