Abstract
Background
Efforts to improve quality of end-of-life (EOL) care are increasingly focused on eliciting patients’ EOL preference through advance care planning (ACP). However, if patients’ EOL preference changes over time and their ACP documents are not updated, these documents may no longer be valid at the time EOL decisions are made.
Objectives
To assess extent and correlates of changes in stated preference for aggressive EOL care over time.
Design
Secondary analysis of data from a randomized controlled trial of a formal ACP program versus usual care in Singapore.
Patients
Two hundred eighty-two patients with heart failure (HF) and New York Heart Association Classification III and IV symptoms were recruited and interviewed every 4 months for up to 2 years to assess their preference for EOL care. Analytic sample included 200 patients interviewed at least twice.
Results
Nearly two thirds (64%) of patients changed their preferred type of EOL care at least once. Proportion of patients changing their stated preference for type of EOL care increased with time and the change was not unidirectional. Patients who understood their prognosis correctly were less likely to change their preference from non-aggressive to aggressive EOL care (OR 0.66, p value 0.07) or to prefer aggressive EOL care (OR 0.53; p value 0.001). On the other hand, patient-surrogate discussion of care preference was associated with a higher likelihood of change in patient preference from aggressive to non-aggressive EOL care (OR 1.83; p value 0.03).
Conclusion
The study provides evidence of instability in HF patients’ stated EOL care preference. This undermines the value of an ACP document recorded months before EOL decisions are made unless a strategy exists for easily updating this preference.
Trial Registration
ClinicalTrials.gov: NCT02299180
Electronic supplementary material
The online version of this article (10.1007/s11606-020-05740-2) contains supplementary material, which is available to authorized users.
KEY WORDS: advance care planning, heart failure, end-of-life care preference, decisional conflict, quality of life
INTRODUCTION
Quality end-of-life (EOL) care involves eliciting and respecting patient preference for care.1–3 Advance care planning (ACP) and advance directives (ADs) are vital tools for doing so.4–8 A key concern is that if patients’ stated preference for EOL care changes over time and their ACP or AD documents are not regularly updated, then the preference recorded months or years before may no longer be valid at the time EOL decisions are made.
In this context, a systematic review of studies reported that stated preference for type of EOL care was stable for more than 70% of patients included in the review.9 However, most studies included only a single follow-up conducted over a short duration, ranging from a few weeks to a few months,9–13 thus limiting their ability to assess changes in stated preference among patients diagnosed with an advanced serious illness and/or healthy adults expected to have a significantly long period of survival following the ACP documentation. This concern becomes very relevant as ACP and ADs are increasingly being targeted towards generally healthy populations and patients with serious illnesses not at risk of imminent mortality.14, 15
To address this gap in the literature, we aimed to estimate the extent and correlates of change in patients’ stated preference for type of EOL care over a period of 2 years, through follow-ups conducted every 4 months. We also assessed factors associated with patients’ stated preference for aggressive EOL care. We conducted this study among patients with moderate or severe heart failure (HF), a group characterized by long and unpredictable decline in physical function but who are likely to survive for several months or years following diagnosis.16, 17 With aging populations, the number of patients living with HF are likely to increase3, 4 making it a major cause of mortality among older adults.5
Based on previous literature,18–20 we hypothesized that patients who had undergone an ACP discussion will be less likely to prefer aggressive EOL care. As patients’ EOL decisions are known to be related to their quality of life,21–23 mental and financial well-being,19, 20, 24, 25 prognostic understanding,26, 27 self-efficacy to manage treatment,28 decisional conflict regarding EOL care,29, 30 and discussion of care preference with surrogate decision-maker,31 we also tested whether these time-varying factors were associated with change in patients’ preference for EOL care. Results will inform policy makers and physicians regarding the value of ACP and AD documents recorded some time back and on the need to continually update these documents.
METHODS
Study Design, Setting, and Participants
This study is a secondary analysis of a two-arm randomized controlled trial (RCT) of an ACP program versus usual care in Singapore. The trial was conducted between March 2015 and June 2018. The main results from this trial have been described in a separate manuscript. 32 We enrolled in-patients with HF and New York Heart Association Classification III and IV symptoms, 21 years and older, and able to give informed consent. We excluded those with psychiatric or cognitive disorders (n = 64) or with a previous ACP (n = 60). The study was performed at National Heart Centre Singapore and Department of Internal Medicine at Singapore General Hospital. It was approved by the SingHealth Institutional Review Board (2015/2781). Further details about the trial are described in the protocol paper.33
Following informed consent, 282 eligible patients completed a baseline survey and were randomized using block randomization to ACP (intervention) or control arm in a 1:2 ratio without stratification. Patients randomized to ACP received formal ACP by trained certified non-clinician facilitators based on the Respecting Choices Model, an internationally recognized evidence-based model of ACP that has been evaluated previously.4, 34 Subsequently, patients in both arms answered follow-up surveys every 4 months for 2 years (up to six follow-up surveys) (Supplementary Fig. 1). Thus, data from a total of seven time points were analyzed in our study. We administered all surveys face to face in patients’ preferred language (English, Mandarin, Malay, or Tamil) using a portable electronic device. Details of the study protocol such as sample size calculations have been reported previously.33 As change in stated preference for type of EOL care, our outcome of interest, can only be assessed for patients with at least two observations, we limited the current analyses to 200 patients who answered at least one follow-up survey.
Survey Questionnaire
At each time point, we asked patients regarding the type of EOL care they preferred (full treatment or limited additional treatment or comfort care). Full treatment, including intubation, mechanical ventilation, cardioversion, and transfer to intensive care, was defined as aggressive EOL care in this study. Non-aggressive EOL care included limited additional treatment (limited trial of treatment, oral or intravenous medications, non-invasive ventilation support, and transfer to hospital) or comfort care (medications, oxygen, and other measures used for comfort at the place where the patient lives). We explained all medical terms including “intubation,” “mechanical ventilation,” and “cardioversion” in simple language to ensure patients’ understanding of the care options.
We also assessed patients’ quality of life (Kansas City Cardiomyopathy Questionnaire (KCCQ) quality of life and clinical summary score)35; mental well-being (depression subscale of the Hospital Anxiety and Depression Scale)36, 37; financial well-being (by asking patients to what extent their choice for EOL treatment was influenced by financial constraints—very much/not very much/not at all); prognostic understanding (by asking patients if they thought that their current treatments would cure their heart condition—yes/no/not sure); self-efficacy (KCCQ self-efficacy score)35; decisional conflict regarding EOL care (low-literacy version of the decisional conflict scale)38; and whether they had discussed their care preference with their surrogate decision-maker (yes/no). Finally, we collected data on patients’ demographic characteristics including age, gender, ethnicity, marital status, education, number of children, and household income.
Statistical Analysis
We calculated at each time point the proportion of patients who changed their stated preference for type of EOL care in any direction from baseline, assuming no loss to follow-up, i.e., n = 200. We also assessed patients’ change in stated preference for type of EOL care based on their responses between two successive time points. For instance, we assessed change in patients’ preference from 4 to 8 months, but if data was missing at 4 months then we assessed change in preference from baseline to 8 months. We calculated change in preference from non-aggressive to aggressive care and vice versa. In separate models, we used mixed effects logistic regression method with patient ID as the random effect to assess correlates of change in preference from non-aggressive to aggressive care and from aggressive to non-aggressive care. Independent variables included ACP participation, patient baseline characteristics (age, gender, ethnicity, marital status, number of children, education), and patient time varying characteristics (financial constraint, correct prognostic understanding, decisional conflict, discussion of care preference with surrogate, self-efficacy, quality of life, and depression). Lastly, we assessed correlates of patients’ stated preference for aggressive EOL care at each time point using a mixed effects logistic regression model with patient ID as the random effect. Independent variables included were the same as above.
We used Stata version 15.1 for all analyses. For Figure 1, we used the R package longCatEDA39.
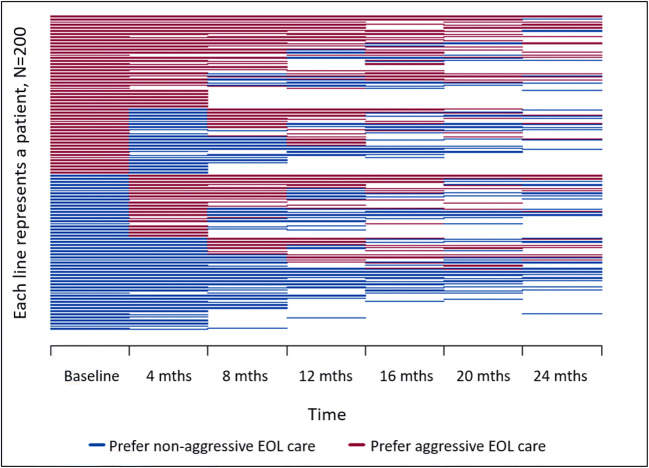
Fig. 1.
Individual patients’ preference for end-of-life (EOL) care across time.
RESULTS
Our patient sample (n = 200) was on average, 64 years of age, and mostly male (79%). About a quarter of them had participated in ACP discussions delivered as part of the RCT. Half of the patients preferred aggressive EOL care at baseline. Details of other baseline characteristics are in Table 1 and baseline characteristics by ACP participation are in Supplementary Table 1. We conducted 96% of the follow-up surveys within 1 month of the scheduled followed up time.
Table 1.
Patient Baseline Characteristics (N = 200)
| Characteristics | Frequency/mean | %/SD |
|---|---|---|
| Age (years)—range: 27–93 | 64.4 | 13.0 |
| Gender | ||
| Male | 158 | 79 |
| Female | 42 | 21 |
| Ethnicity | ||
| Chinese | 117 | 58.5 |
| Malay | 46 | 23.0 |
| Indian/others | 37 | 18.5 |
| Marital status | ||
| Married | 119 | 59.5 |
| Not married | 81 | 40.5 |
| Number of children—range: 0–10 | 2 | 2 |
| Education | ||
| Primary education or less | 90 | 45 |
| Secondary education or more | 110 | 55 |
| Household income | ||
| Less than $500 | 49 | 24.5 |
| $500—$2999 | 57 | 28.5 |
| $3000 and above | 41 | 20.5 |
| Do not know/refuse to answer | 53 | 26.5 |
| Participation in advance care planning | ||
| Yes | 49 | 24.5 |
| No | 151 | 75.5 |
| Stated preference for type of EOL care | ||
| Aggressive EOL care (full treatment) | 101 | 50.5 |
| Non-aggressive EOL care (limited additional treatment/comfort care) | 99 | 49.5 |
| KCCQ quality of life score—range: 0–100 | 47.6 | 29.6 |
| KCCQ clinical summary score—range: 0–97.5 | 56.6 | 21.6 |
| Depressive symptoms score—range: 0–19 | 5.7 | 4.2 |
| Financial constraints | ||
| Very much (high) | 71 | 35.5 |
| Not very much/not at all | 129 | 64.5 |
| Prognostic understanding | ||
| Treatment will not cure heart failure (correct) | 50 | 25 |
| Treatment will cure heart failure/unsure | 150 | 75 |
| KCCQ self-efficacy score—range: 0–100 | 82 | 22.7 |
| Decisional conflict score—range: 0–88.9 | 11.8 | 16.1 |
| Discussed care preference with surrogate decision-maker | ||
| Yes | 104 | 52 |
| No | 96 | 48 |
Freq., frequency; SD, standard deviation; IQR: interquartile range; EOL, end-of-life; KCCQ: Kansas City Cardiomyopathy Questionnaire
Change in Stated Preference for EOL Care
Overall, 64% (n = 128) of patients changed their stated preference for type of EOL care at least once through the study period. We used a horizontal line plot to visualize patients’ stated preference for type of EOL care over time (Fig. 1). In this plot, each horizontal line represents a patient. The first column of lines shows patient preference at baseline, the second column shows patient preference at 4 months, and so on. Many lines in this plot show a change in color, demonstrating instability in stated preference for type of EOL care for most patients during the study period.
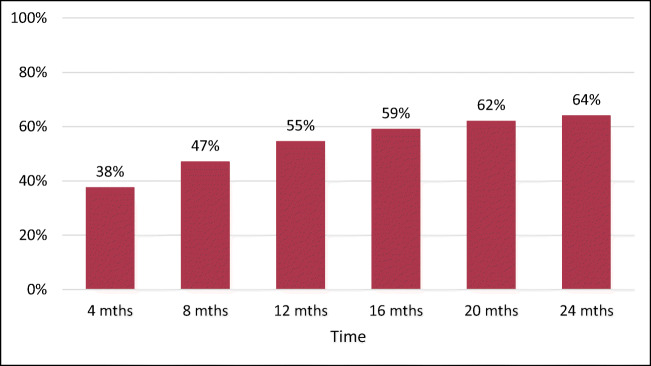
Assuming no loss to follow-up, i.e., n = 200 at each time point, we found that at 4 months at least one third of the patients could be expected to change their stated preference for type of EOL care relative to baseline. The proportion of patients expected to change their stated preference for type of EOL care relative to baseline increased at a decreasing rate over time, exceeding 50% at 1 year (Fig. 2).
Fig. 2.
Proportion of patients who changed end-of-life (EOL) care preference at least once since baseline.
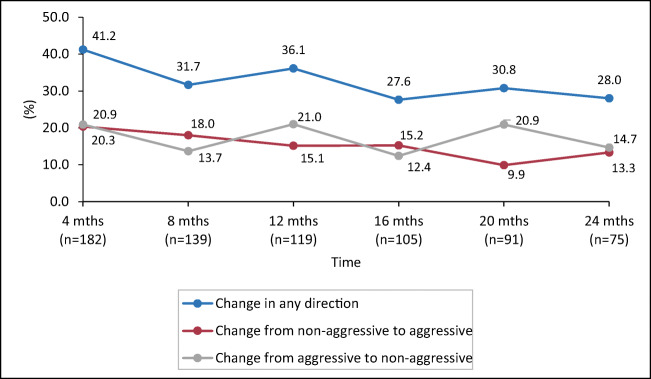
Among those surveyed at 4 months, we found that 41% changed their stated preference for type of EOL care relative to baseline, with an equal proportion changing their preferred care from aggressive to non-aggressive and vice-versa. The proportion of patients whose preferred care changed between two successive time points generally decreased over time. However, no specific trend was observed in the proportion of patients changing from aggressive to non-aggressive care or vice versa (Fig. 3).
Fig. 3.
Changes in patients’ preference for end-of-life (EOL) care over time.
The predictors of change in patients’ stated preference for type of EOL care at each time point are reported in Table 2. Patients who understood their prognosis correctly were less likely to have changed their preference from non-aggressive to aggressive EOL care (odds ratio (OR) 0.66, p value 0.07), while patients from Indian or other ethnic groups were more likely to change their preference to aggressive EOL care (OR 1.62; p value 0.09). On the other hand, patients who had discussed their care preference with their surrogates were more likely to have changed their preference from aggressive to non-aggressive EOL care (OR 1.81; p value 0.03).
Table 2.
Predictors of Change in Stated Preference for End-of-Life (EOL) Care
| Change in preference from non-aggressive to aggressive EOL care (N = 711) | Change in preference from aggressive to non-aggressive EOL care (N = 711) | |||
|---|---|---|---|---|
| Odds ratio | [95% CI] | Odds ratio | [95% CI] | |
| Received ACPa | 0.85 | [0.52, 1.38] | 0.87 | [0.54, 1.39] |
| Age | 1.01 | [0.99, 1.02] | 1.01 | [0.99, 1.03] |
| Malesa | 0.83 | [0.49, 1.43] | 1 | [0.61, 1.67] |
| Ethnicitya | ||||
| Malay | 1.2 | [0.67, 2.15] | 1.45 | [0.84, 2.48] |
| Indian/others | 1.62* | [0.92, 2.85] | 1.11 | [0.62, 1.99] |
| Marrieda | 1.11 | [0.7, 1.77] | 1.1 | [0.7, 1.73] |
| No. of children | 0.95 | [0.82, 1.09] | 0.98 | [0.86, 1.12] |
| Secondary education or more a | 0.81 | [0.49, 1.32] | 0.87 | [0.54, 1.4] |
| Household incomea | ||||
| $500—$2999 | 0.83 | [0.45, 1.52] | 1.04 | [0.58, 1.87] |
| $3000 and above | 1.12 | [0.53, 2.33] | 1.2 | [0.59, 2.45] |
| Do not know/refuse to answer | 0.97 | [0.52, 1.83] | 0.69 | [0.36, 1.29] |
| KCCQ quality-of-life score | 0.99 | [0.98, 1] | 1 | [0.98, 1.01] |
| KCCQ clinical summary score | 1 | [0.99, 1.01] | 1 | [0.99, 1.02] |
| Depressive symptoms score | 0.97 | [0.91, 1.04] | 0.97 | [0.91, 1.04] |
| High financial constraints a | 0.92 | [0.55, 1.53] | 1.34 | [0.82, 2.17] |
| Correct prognostic understandinga | 0.66* | [0.43, 1.03] | 0.92 | [0.61, 1.4] |
| KCCQ self-efficacy score | 0.99 | [0.98, 1.01] | 0.99 | [0.98, 1] |
| Decisional conflict score | 1 | [0.99, 1.01] | 1.01 | [1, 1.02] |
| Discussed care preference with surrogate decision-makera | 1.27 | [0.74, 2.16] | 1.81** | [1.05, 3.14] |
CI, confidence interval; ACP, advance care planning; No., number; EOL, end-of-life, KCCQ: Kansas City Cardiomyopathy Questionnaire
aReference categories for variables are as follows: did not participate in ACP, females, Chinese, not married, primary education or less at baseline, household income less than $500, low/no financial constraints, incorrect understanding of prognosis or being unsure of prognosis, did not discuss treatment preference with surrogate decision-maker
* and ** indicate a statistical significance level at 10% and 5% respectively
Preference for Aggressive EOL Care
Patient preference for aggressive EOL care was lower for older patients (OR 0.96, p value 0.00), those reporting that their preference was highly influenced by financial constraints (OR 0.61, p value 0.02), those with correct prognostic understanding (OR 0.53; p 0.001), and those with greater decisional conflict (OR 0.99; p value 0.02). On the other hand, patients with higher self-efficacy were more likely to prefer aggressive EOL care (OR 1.01, p value 0.09) (Table 3).
Table 3.
Predictors of Preference for Aggressive End-of-Life (EOL) Care (n = 911)
| Odds ratio | [95% CI] | |
|---|---|---|
| Received ACPa | 0.77 | [0.45, 1.32] |
| Age | 0.96** | [0.94, 0.98] |
| Malesa | 0.74 | [0.39, 1.41] |
| Ethnicitya | ||
| Malay | 1.21 | [0.63, 2.34] |
| Indian/others | 1.19 | [0.6, 2.35] |
| Marrieda | 1.37 | [0.79, 2.37] |
| No. of children | 0.89 | [0.76, 1.05] |
| Secondary education or morea | 1.12 | [0.63, 1.98] |
| Household incomea | ||
| $500—$2999 | 1.47 | [0.72, 3.02] |
| $3000 and above | 0.94 | [0.39, 2.25] |
| Do not know/refuse to answer | 0.97 | [0.46, 2.03] |
| KCCQ quality-of-life score | 1.01 | [1, 1.02] |
| KCCQ clinical summary score | 0.99 | [0.98, 1.01] |
| Depressive symptoms score | 1.02 | [0.97, 1.08] |
| High financial constraintsa | 0.61** | [0.4, 0.93] |
| Correct prognostic understandinga | 0.53** | [0.36, 0.77] |
| KCCQ self-efficacy score | 1.01* | [1, 1.02] |
| Decisional conflict score | 0.99** | [0.98, 1] |
| Discussed care preference with surrogate decision-makera | 0.82 | [0.54, 1.24] |
CI, confidence interval; ACP, advance care planning; No., number; EOL, end-of-life; KCCQ: Kansas City Cardiomyopathy Questionnaire
aDummy variables. Reference categories for variables are as follows: did not participate in ACP, females, Chinese, not married, primary education or less, household income less than $500, low/no influence of financial constraints, incorrect understanding of prognosis or being unsure of prognosis, did not discuss treatment preference with surrogate decision-maker
* and ** indicate a statistical significance level at 10% and 5% respectively
DISCUSSION
Our study highlights several challenges to the implementation of ACP programs among patients with HF. First, we found that nearly two thirds of HF patients changed their stated preference for type of EOL care over time and the change was not consistent in one direction. Second, our results showed that even at 4 months after baseline, the proportion of patients changing their stated preference for type of EOL care was high (38%) and that this proportion increased with time.
These findings highlight that if patient preference for type of EOL is documented at least 4 months ago and never updated, it will be challenging for physicians to determine whether or not the recorded preference is still valid at the time of making EOL treatment decisions. In fact, even at 4 months, there is a high likelihood that any ACP/AD document recording patient preference no longer accurately reflects patients’ current EOL care preference and if physicians unduly rely on such documents, they may deliver EOL care incongruent with patient’s preference at that point in time. This can amount to a serious medical error.40
A notable finding is that only a quarter of our patients correctly understood that the current treatments will not cure their heart condition irrespective of their participation in the ACP program. This is noteworthy considering the influence of prognostic understanding in HF patients’ treatment choices. Given that most HF patients are overly optimistic about their prognosis, it is possible that these patients may be stating a preference for aggressive EOL care without truly understanding the marginal survival benefits of such treatments. It is also possible that patients are experiencing an optimism bias—a phenomenon common among patients with life-limiting illnesses.41 This emphasizes the importance of specialized communication techniques to aid prognostic disclosure during ACP discussions so that patients can make informed decisions regarding their EOL treatment.
We also found that discussion of care preference between patients and surrogate decision-makers was associated with a change in patient preference from aggressive to non-aggressive EOL care. It could be that patients who changed their preference to non-aggressive EOL care may have been more inclined to discuss this change with their surrogate. Alternatively, discussion with a surrogate could have triggered this change. This suggests that surrogates are likely to be aware of a change in patient preference towards non-aggressive EOL care even if patients do not update their ACP/AD documents. Given the role of family in treatment decision-making in Asian settings,42, 43 physicians can further encourage patients and surrogates to frequently discuss patients’ care preference. This could enable surrogates and physicians to make EOL decisions consistent with patient last preference.
Our results show that higher financial constraints reduce patient preference for aggressive EOL care. Financial constraints are of special concern for patients in Singapore as approximately 55% of health expenditure in Singapore is out-of-pocket. This is a greater percentage than most other developed countries.43, 44 Physicians in Singapore should thus also assess patients’ financial constraints while eliciting their preference for type of EOL care.
We did not find that those of Chinese ethnicity differed from those of the minority ethnic groups in terms of their preference for type of EOL care. However, we found that patients of Indian or other ethnicity were more likely to change their preference to aggressive EOL care. Given the small number of individuals of minority ethnic groups in our study, ethnic differences in EOL care preference remains a topic for further investigation.
Based on our results, we recommend that patients should be given an opportunity to continually update their ACP documents as and when they change their preference. This entails finding strategies for patients to be able to easily update their ACP documents without needing to visit a health care provider. Easy-to-use decision aid tools and smart phone applications may be considered and tested in this regard. Physicians should also encourage patients to frequently discuss changes in care preference with their surrogates so that surrogates are aware of patients’ last stated preference.
The main strength of the study is the long duration of follow-up with patients involving frequent assessments of their stated preference for type of EOL care. The ACP, in this study, was delivered as part of the study trial by trained facilitators according to the Respecting Choices Model. Based on the results of the trial, there was no difference in patient baseline characteristics (age, gender, ethnicity, marital status, number of children, education, stated preference for type of EOL care, financial constraint, correct prognostic understanding, decisional conflict, discussion of care preference with surrogate, self-efficacy, quality of life, and depression) between those who received ACP and those who did not; this reduces the potential for a possible selection bias in ACP participation (Supplementary Table 1). The main limitation is attrition of patients during follow-up period due to death and loss to follow-up. However, the mixed effects regression method we used accounts for attrition and missing information. Another limitation of the study is the low participation rate of females. This could be due to higher rates of refusal by females. A similar issue has been reported by previous trials involving heart failure patients.45–47 Additionally, family member’s end-of-life preference may have influenced patient preference or their stability. We did not have data to assess this but it should be a topic of future research. Lastly, high non-response for household income may have limited our analysis and interpretation of its association with the outcomes examined.
CONCLUSION
This study provides evidence of instability in HF patients’ stated preference for type of EOL care. This undermines the value of documenting patient preference for EOL care even if these were done at least 4 months before EOL decisions are made. Future research should assess whether these findings apply to other settings and other illness groups, further explore the role of prognostic understanding of the illness in EOL care preference, and devise strategies for patients to continually update their ACP or AD documents in efforts to minimize the risk of inappropriate EOL treatments.
Electronic Supplementary Material
(DOCX 51 kb)
Acknowledgments
The authors would like to thank Dr. Nivedita Nadkarni for her helpful comments on statistical analysis.
Funding Information
This work was supported by the Lien Centre for Palliative Care of Duke-NUS Medical School (LCPC-IN14-0001) and the Ministry of Health - Health Services Research Grant (NMRC/HSRG/0053/2016).
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bruera E, Sweeney C, Calder K, Palmer L, Benisch-Tolley S. Patient preferences versus physician perceptions of treatment decisions in cancer care. J Clin Oncol Off J Am Soc Clin Oncol. 2001;19(11):2883–5. doi: 10.1200/JCO.2001.19.11.2883. [DOI] [PubMed] [Google Scholar]
- 2.Degner LF, Kristjanson LJ, Bowman D, Sloan JA, Carriere KC, O'Neil J, et al. Information Needs and Decisional Preferences in Women With Breast Cancer. JAMA. 1997;277(18):1485–92. [PubMed] [Google Scholar]
- 3.Pardon K, Deschepper R, Vander Stichele R, Bernheim J, Mortier F, Schallier D, et al. Are patients’ preferences for information and participation in medical decision-making being met? Interview study with lung cancer patients. Palliat Med. 2010;25(1):62–70. doi: 10.1177/0269216310373169. [DOI] [PubMed] [Google Scholar]
- 4.Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010; 340. [DOI] [PMC free article] [PubMed]
- 5.Briggs LA, Kirchhoff KT, Hammes BJ, Song M-K, Colvin ER. Patient-centered advance care planning in special patient populations: a pilot study. J Prof Nurs. 2004;20(1):47–58. doi: 10.1016/j.profnurs.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 6.El-Jawahri A, Paasche-Orlow MK, Matlock D, Stevenson LW, Lewis EF, Stewart G, et al. Randomized, Controlled Trial of an Advance Care Planning Video Decision Support Tool for Patients With Advanced Heart FailureClinical Perspective. Circulation. 2016;134(1):52–60. doi: 10.1161/CIRCULATIONAHA.116.021937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lyon ME, Jacobs S, Briggs L, Cheng Y, Wang J. Family-centered advance care planning for teens with cancer. JAMA Pediatr. 2013;167(5):460–7. doi: 10.1001/jamapediatrics.2013.943. [DOI] [PubMed] [Google Scholar]
- 8.Song M-K, Ward SE, Fine JP, Hanson LC, Lin F-C, Hladik GA, et al. Advance Care Planning and End-of-Life Decision Making in Dialysis: A Randomized Controlled Trial Targeting Patients and Their Surrogates. Am J Kidney Dis. 2015;66(5):813–22. doi: 10.1053/j.ajkd.2015.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Auriemma CL, Nguyen CA, Bronheim R, Kent S, Nadiger S, Pardo D, et al. Stability of End-of-Life Preferences: A Systematic Review of the EvidenceStability of End-of-Life PreferencesStability of End-of-Life Preferences. JAMA Intern Med. 2014;174(7):1085–92. doi: 10.1001/jamainternmed.2014.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McKim DA, King J, Walker K, Leblanc C, Timpson D, Wilson KG, et al. Formal ventilation patient education for ALS predicts real-life choices. Amyotroph Lateral Scler. 2012;13(1):59–65. doi: 10.3109/17482968.2011.626053. [DOI] [PubMed] [Google Scholar]
- 11.Sharman SJ. Current negative mood encourages changes in end-of-life treatment decisions and is associated with false memories. Cognit Emot. 2011;25(1):132–9. doi: 10.1080/02699931003612064. [DOI] [PubMed] [Google Scholar]
- 12.Eggar R, Spencer A, Anderson D, Hiller L. Views of elderly patients on cardiopulmonary resuscitation before and after treatment for depression. Int J Geriatr Psychiatry. 2002;17(2):170–4. doi: 10.1002/gps.523. [DOI] [PubMed] [Google Scholar]
- 13.Golin CE, Wenger NS, Liu H, Dawson NV. A prospective study of patient-physician communication about resuscitation. J Am Geriatr Soc. 2000;48(5):S52. doi: 10.1111/j.1532-5415.2000.tb03141.x. [DOI] [PubMed] [Google Scholar]
- 14.Malcomson H, Bisbee S. Perspectives of healthy elders on advance care planning. J Am Acad Nurse Pract. 2009;21(1):18–23. doi: 10.1111/j.1745-7599.2008.00369.x. [DOI] [PubMed] [Google Scholar]
- 15.Bravo G, Trottier L, Arcand M, Boire-Lavigne A-M, Blanchette D, Dubois M-F, et al. Promoting advance care planning among community-based older adults: A randomized controlled trial. Patient Educ Couns. 2016;99(11):1785–95. doi: 10.1016/j.pec.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 16.Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJV. More 'malignant' than cancer? Five-year survival following a first admission for heart failure. Eur J Heart Fail. 2001;3(3):315–22. doi: 10.1016/s1388-9842(00)00141-0. [DOI] [PubMed] [Google Scholar]
- 17.Askoxylakis V, Thieke C, Pleger ST, Most P, Tanner J, Lindel K, et al. Long-term survival of cancer patients compared to heart failure and stroke: A systematic review. BMC Cancer. 2010;10(1):105. doi: 10.1186/1471-2407-10-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Emanuel LL, Emanuel EJ, Stoeckle JD, Hummel LR, Barry MJ. Advance Directives: Stability of Patients' Treatment Choices. Arch Intern Med. 1994;154(2):209–17. doi: 10.1001/archinte.154.2.209. [DOI] [PubMed] [Google Scholar]
- 19.Danis M, Garrett J, Harris R, Patrick DL. Stability of Choices about Life-Sustaining Treatments. Ann Intern Med. 1994;120(7):567–73. doi: 10.7326/0003-4819-120-7-199404010-00006. [DOI] [PubMed] [Google Scholar]
- 20.Ditto PH, Smucker WD, Danks JH, Jacobson JA, Houts RM, Fagerlin A, et al. Stability of Older Adults' Preferences for Life-Sustaining Medical Treatment. Health Psychol. 2003;22(6):605–15. doi: 10.1037/0278-6133.22.6.605. [DOI] [PubMed] [Google Scholar]
- 21.Carmel S, Mutran E. Wishes regarding the use of life-sustaining treatments among elderly persons in Israel: An explanatory model. Soc Sci Med. 1997;45(11):1715–27. doi: 10.1016/s0277-9536(97)00104-4. [DOI] [PubMed] [Google Scholar]
- 22.Fried TR, Van Ness PH, Byers AL, Towle VR, O’Leary JR, Dubin JA. Changes in Preferences for Life-Sustaining Treatment Among Older Persons with Advanced Illness. J Gen Intern Med. 2007;22(4):495–501. doi: 10.1007/s11606-007-0104-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fried TR, O'Leary J, Van Ness P, Fraenkel L. Inconsistency Over Time in the Preferences of Older Persons with Advanced Illness for Life-Sustaining Treatment. J Am Geriatr Soc. 2007;55(7):1007–14. doi: 10.1111/j.1532-5415.2007.01232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosenfeld KE, Wenger NS, Phillips RS, Connors AF, Dawson NV, Layde P, et al. Factors Associated With Change in Resuscitation Preference of Seriously Ill Patients. Arch Intern Med. 1996;156(14):1558–64. [PubMed] [Google Scholar]
- 25.Janssen DJA, Spruit MA, Schols JMGA, Cox B, Nawrot TS, Curtis JR, et al. Predicting Changes in Preferences for Life-Sustaining Treatment Among Patients With Advanced Chronic Organ Failure. Chest. 2012;141(5):1251–9. doi: 10.1378/chest.11-1472. [DOI] [PubMed] [Google Scholar]
- 26.Weeks JC, Cook EF, O'Day SJ, Peterson LM, Wenger N, Reding D, et al. Relationship Between Cancer Patients' Predictions of Prognosis and Their Treatment Preferences. JAMA. 1998;279(21):1709–14. doi: 10.1001/jama.279.21.1709. [DOI] [PubMed] [Google Scholar]
- 27.Davison SN. End-of-Life Care Preferences and Needs: Perceptions of Patients with Chronic Kidney Disease. Clin J Am Soc Nephrol. 2010;5(2):195. doi: 10.2215/CJN.05960809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aiken LS, Butner J, Lockhart CA, Volk-Craft BE, Hamilton G, Williams FG. Outcome evaluation of a randomized trial of the PhoenixCare intervention: program of case management and coordinated care for the seriously chronically ill. J Palliat Med. 2006;9(1):111–26. doi: 10.1089/jpm.2006.9.111. [DOI] [PubMed] [Google Scholar]
- 29.Allen RS, Allen JY, Hilgeman MM, DeCoster J. End-of-Life Decision-Making, Decisional Conflict, and Enhanced Information: Race Effects. J Am Geriatr Soc. 2008;56(10):1904–9. doi: 10.1111/j.1532-5415.2008.01929.x. [DOI] [PubMed] [Google Scholar]
- 30.Heyland DK, Heyland R, Dodek P, You JJ, Sinuff T, Hiebert T, et al. Discordance between patients' stated values and treatment preferences for end-of-life care: results of a multicentre survey. BMJ Support Palliat Care. 2017;7(3):292. doi: 10.1136/bmjspcare-2015-001056. [DOI] [PubMed] [Google Scholar]
- 31.Song M-K, Ward SE, Hanson LC, Metzger M, Kim S. Determining Consistency of Surrogate Decisions and End-of-Life Care Received with Patient Goals-of-Care Preferences. J Palliat Med. 2016;19(6):610–6. doi: 10.1089/jpm.2015.0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Silveira MJ, Kim SYH, Langa KM. Advance Directives and Outcomes of Surrogate Decision Making before Death. N Engl J Med. 2010;362(13):1211–8. doi: 10.1056/NEJMsa0907901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Malhotra C, Sim D, Jaufeerally FR, et al. Impact of a formal advance care planning program on end-of-life care for patients with heart failure: Results from a randomized controlled trial. J Card Fail. 2020;S1071-9164(19)31494-0. 10.1016/j.cardfail.2020.01.015 [DOI] [PubMed]
- 34.Hammes BJ, Rooney BL, Gundrum JD. A Comparative, Retrospective, Observational Study of the Prevalence, Availability, and Specificity of Advance Care Plans in a County that Implemented an Advance Care Planning Microsystem. J Am Geriatr Soc. 2010;58(7):1249–55. doi: 10.1111/j.1532-5415.2010.02956.x. [DOI] [PubMed] [Google Scholar]
- 35.Green CP, Porter CB, Bresnahan DR, Spertus JA. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol. 2000;35(5):1245–55. doi: 10.1016/s0735-1097(00)00531-3. [DOI] [PubMed] [Google Scholar]
- 36.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 37.Herrmann C. International experiences with the Hospital Anxiety and Depression Scale--a review of validation data and clinical results. J Psychosom Res. 1997;42(1):17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 38.O'Connor AM. Validation of a decisional conflict scale. Med Decis Mak. 1995;15(1):25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 39.Tueller SJ, Van Dorn RA, Bobashev GV. Visualization of categorical longitudinal and times series data. Methods report (RTI Press). 2016; 2016. [DOI] [PMC free article] [PubMed]
- 40.Allison TA, Sudore RL. Disregard of Patients’ Preferences Is a Medical Error: Comment on “Failure to Engage Hospitalized Elderly Patients and Their Families in Advance Care Planning” Disregard of Patients’ Preferences. JAMA Intern Med. 2013;173(9):787. doi: 10.1001/jamainternmed.2013.203. [DOI] [PubMed] [Google Scholar]
- 41.Ozdemir S, Finkelstein EA. Cognitive Bias: The Downside of Shared Decision Making. JCO Clin Cancer Inform. 2018;2:1–10. doi: 10.1200/CCI.18.00011. [DOI] [PubMed] [Google Scholar]
- 42.Ozdemir S, Jafar TH, Choong LHL, Finkelstein EA. Family dynamics in a multi-ethnic Asian society: comparison of elderly CKD patients and their family caregivers experience with medical decision making for managing end stage kidney disease. BMC Nephrol. 2019;20(1):73. doi: 10.1186/s12882-019-1259-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lin M-L, Kan W-M, Chen C-H. Patients' Perceptions and Expectations of Family Participation in the Informed Consent Process of Elective Surgery in Taiwan. Asian Nurs Res. 2012;6(2):55–9. doi: 10.1016/j.anr.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 44.The World Bank. World Health Organization Global Health Expenditure database. 2018 [cited 2018 April 9]; Available from: https://data.worldbank.org/indicator/SH.XPD.OOPC.TO.ZS?locations=SG
- 45.Heiat A, Gross CP, Krumholz HM. Representation of the elderly, women, and minorities in heart failure clinical trials. Arch Intern Med. 2002;162(15):1682–8. doi: 10.1001/archinte.162.15.1682. [DOI] [PubMed] [Google Scholar]
- 46.Pilote L, Raparelli V. Participation of Women in Clinical Trials. J Am Coll Cardiol. 2018;71(18):1970. doi: 10.1016/j.jacc.2018.02.069. [DOI] [PubMed] [Google Scholar]
- 47.Melloni C, Berger Jeffrey S, Wang Tracy Y, Gunes F, Stebbins A, Pieper Karen S, et al. Representation of Women in Randomized Clinical Trials of Cardiovascular Disease Prevention. Circ Cardiovasc Qual Outcomes. 2010;3(2):135–42. doi: 10.1161/CIRCOUTCOMES.110.868307. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 51 kb)