Abstract
Background
With continued growth in the older adult population, US federal and state costs for long-term care services are projected to increase. Recent policy changes have shifted funding to home and community-based services (HCBS), but it remains unclear whether HCBS can prevent or delay long-term nursing home placement (NHP).
Methods
We searched MEDLINE (OVID), Sociological Abstracts, PsycINFO, CINAHL, and Embase (from inception through September 2018); and Cochrane Database of Systematic Reviews, Joanna Briggs Institute Database, AHRQ Evidence-based Practice Center, and VA Evidence Synthesis Program reports (from inception through November 2018) for English-language systematic reviews. We also sought expert referrals. Eligible reviews addressed HCBS for community-dwelling adults with, or at risk of developing, physical and/or cognitive impairments. Two individuals rated quality (using modified AMSTAR 2) and abstracted review characteristics, including definition of NHP and interventions. From a prioritized subset of the highest-quality and most recent reviews, we abstracted intervention effects and strength of evidence (as reported by review authors).
Results
Of 47 eligible reviews, most focused on caregiver support (n = 10), respite care and adult day programs (n = 9), case management (n = 8), and preventive home visits (n = 6). Among 20 prioritized reviews, 12 exclusively included randomized controlled trials, while the rest also included observational studies. Prioritized reviews found no overall benefit or inconsistent effects for caregiver support (n = 2), respite care and adult day programs (n = 3), case management (n = 4), and preventive home visits (n = 2). For caregiver support, case management, and preventive home visits, some reviews highlighted that a few studies of higher-intensity models reduced NHP. Reviews on other interventions (n = 9) generally found a lack of evidence examining NHP.
Discussion
Evidence indicated no benefit or inconsistent effects of HCBS in preventing or delaying NHP. Demonstration of substantial impacts on NHP may require longer-term studies of higher-intensity interventions that can be adapted for a variety of settings.
Registration
PROSPERO # CRD42018116198
Electronic supplementary material
The online version of this article (10.1007/s11606-019-05568-5) contains supplementary material, which is available to authorized users.
Key Words: long-term care services, home and community-based services, case management
INTRODUCTION
US federal and state programs fund the majority of long-term services and supports (LTSS), with Medicaid accounting for 71% of government expenditures.1 With continued growth in the older adult population, Medicaid spending on LTSS is projected to reach $154 billion by 2025 and more than $400 billion by 2050.1 In 2015, institutional LTSS, or long-term nursing home care, accounted for 47% of overall Medicaid expenditures on LTSS, a proportion that continues to decrease, in part due to national policies (e.g., Balancing Incentive Program) that aim to shift funds to home and community-based services (HCBS).2 However, there remains substantial uncertainty about the benefits of HCBS for community-dwelling adults with impairments, and concern that moving resources away from institutional LTSS may not lead to improved outcomes.3–6
Here, we present results from a larger review conducted by the Department of Veterans Affairs (VA) Evidence Synthesis Program (ESP),7 focusing on effects of HCBS in preventing or delaying long-term nursing home placement (NHP) for community-dwelling adults with physical and/or cognitive impairments. VA costs for LTSS for eligible veterans is projected to be $9.8 billion in fiscal year 2020, with over two thirds of these expenditures going to institutional care.8,9 VA policymakers are also interested in increasing use of HCBS to help veterans with impairments remain in community settings;10,11 thus, they sought evidence on whether HCBS can decrease the need for institutional care. To address a diverse set of interventions, and to provide summary effects for specific interventions, we conducted a systematic review of reviews.12 We prioritized the highest-quality and most recently completed reviews for detailed results on individual interventions. We provide qualitative syntheses of these results, highlight gaps in the evidence base, and offer recommendations for future research and policy.
METHODS
The review protocol was registered in PROSPERO (CRD42018116198).
Conceptual Model and Scope
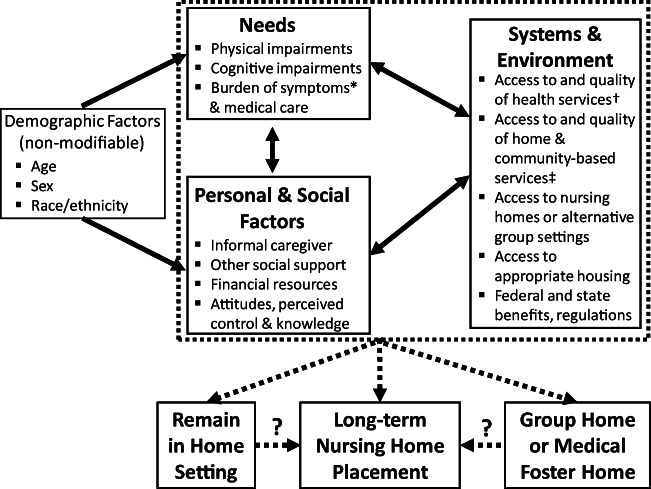
Collaboratively with VA stakeholders (representatives from VA Choose Home Initiative, Geriatrics and Extended Care, and Caregiver Support Program) and an advisory panel of experts in LTSS research, we developed a conceptual framework to organize the wide range of factors contributing to NHP and constituting the potential targets of interventions. We reviewed existing frameworks that have been applied in past research involving adults with impairments.13–16 Our framework (Fig. 1) included 3 categories of factors that may interact: (1) needs for care due to physical or cognitive impairment, symptoms, and/or medical treatments; (2) personal and social factors that are resources or barriers to meeting needs; and (3) systems and environmental factors including access and quality of healthcare services and HCBS.
Figure 1.
Conceptual model for long-term nursing home placement. *Due to mental health and physical health conditions.†Includes outpatient and inpatient care.‡Includes skilled health care at home (e.g., nursing, physical therapy) and personal assistance (e.g., home aides).
We applied our conceptual framework to formulate key questions, develop search terms, inform eligibility criteria, and determine elements of data abstraction. Given the complex array of factors that likely contribute to NHP for any given individual, we considered a broad range of HCBS, from interventions that sought to change modifiable risk factors (in community or outpatient settings) to programs that substituted services at home (for similar care provided at nursing facilities). Additionally, we considered that characteristics of adults with impairments (and often their caregivers) may impact effectiveness of various interventions.
Key Questions (KQ)
For adults with physical and/or cognitive impairments:
KQ1—What is the effectiveness of HCBS for preventing or delaying NHP?
KQ2—Which characteristics of participants moderate the effectiveness of interventions in preventing or delaying NHP?
Search Strategy
To balance a very broad scope of diverse interventions with determining effects of specific interventions, we focused on identifying relevant systematic reviews. We searched from inception: MEDLINE, Sociological Abstracts, PsycINFO, CINAHL, and Embase (through September 2018), and Cochrane Database of Systematic Reviews, Joanna Briggs Institute Database, Agency for Healthcare Research and Quality Evidence-based Practice Center reports, and VA ESP reports (through November 2018). Search terms included MeSH and free text for adults with impairments (or at high risk of developing impairments), range of HCBS, NHP, and systematic reviews (Appendix Table 1). Our expert advisory panel also provided referrals.
Screening and Selection of Eligible Reviews
Duplicate results were removed and abstracts screened by 2 individuals using DistillerSR (Evidence Partners, Ottawa, Canada). Prespecified eligibility criteria (Appendix Table 2) included systematic reviews on community-dwelling adults with existing, or at risk of developing, impairments; HCBS, such as case management, caregiver support, and respite care; and explicit inclusion of NHP (or similar terms such as “institutionalization”). A preliminary list of HCBS helped guide search strategies, but other relevant interventions emerged and were included during screening and selection. If a review defined “nursing home admissions” as including short-term stays for rehabilitation, it was excluded. Included abstracts underwent full-text review by 2 individuals; eligibility at full-text review required consensus.
Data Abstraction and Quality Assessment
All eligible reviews underwent independent data abstraction by 2 individuals for population characteristics (including country where study was conducted), dates of searches, number and characteristics of included primary studies, definition of NHP, and intervention characteristics.
Two reviewers independently assessed quality using criteria adapted from AMSTAR 217 (Appendix Fig. 1); overall quality was rated as high, medium, or low. Consensus on quality ratings was reached through discussion.
For specific effects on NHP, we selected the highest-quality and most recent eligible systematic reviews for each intervention. For example, we prioritized all 4 high-quality reviews on case management (2 conducted within the past 5 years and 2 published in 2013). From prioritized reviews, we further abstracted meta-analysis results (or qualitative summaries) of effects on NHP, moderation of effects by participant or intervention characteristics, ascertainment of NHP by included studies (abstracted directly from primary studies), quality ratings and strength of evidence (as reported by reviews), and total number of unique primary studies that examined NHP as an outcome.
Data Synthesis
Given heterogeneity in populations and interventions, we undertook a qualitative synthesis.18,19 First, we noted the number of eligible reviews addressing different interventions. To determine intervention categories, we primarily relied on review authors’ descriptions and classifications of interventions. However, we also applied our conceptual framework to highlight when interventions have overlapping targets or components (e.g., case management and caregiver-focused interventions). We then summarized intervention effects abstracted from the prioritized subset of higher-quality, more recent, eligible reviews. We also determined the quantity of evidence underlying prioritized reviews of different interventions (i.e., number of unique primary studies), and described the quality of underlying studies and strength of evidence (as rated by reviews). We addressed KQ2 by summarizing participant characteristics associated with effectiveness of interventions, whether this was determined via quantitative subgroup analyses or qualitative summaries.
RESULTS
Overview of Eligible and Prioritized Systematic Reviews
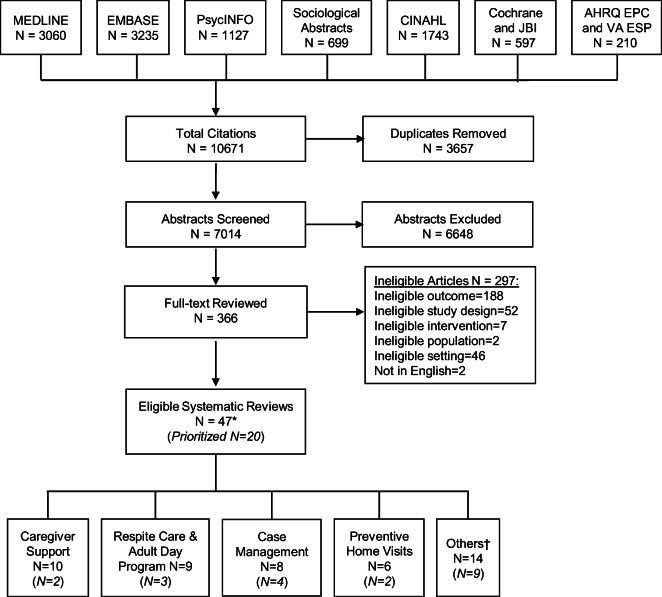
Of 7014 unique citations, 336 articles underwent full-text review and 47 eligible reviews on interventions were identified (Fig. 2). Most eligible reviews addressed older adults and/or those with dementia and evaluated caregiver support (n = 10),20–29 respite care and adult day programs (n = 9),30–38 case management (n = 8),39–46 or preventive home visits (n = 6)47–52 (see Text Box 1 for descriptions of main intervention categories). The remaining reviews53–66 were either very broad in scope (e.g., all nonpharmacologic interventions for dementia) or 1–2 reviews addressing an intervention (e.g., home-based primary care). Most eligible reviews included studies that were conducted in a variety of countries, including USA, Canada, Australia, and high-income countries in Europe and Asia.
Figure 2.
Search, selection, and prioritization of eligible systematic reviews. JBI = Johanna Briggs Institute; AHRQ EPC = Agency for Healthcare Research and Quality Evidence-Based Practice Centers; VA ESP = Department of Veterans Affairs Evidence Synthesis Program. *There were an additional 20 eligible reviews on risk factors for long-term nursing home placement; results on risk factors were described in the larger VA ESP report.†2 reviews—physical activity interventions; 2—home-based primary care; 2—any nonpharmacologic intervention for adults with dementia; 1—any intervention for falls prevention; 1—any intervention for patient or caregiver stress; 1—different settings for personal assistance; 1—in-home health care or personal assistance; 1—assistive technologies; 1—demonstration projects to integrate acute and long-term care in USA and Europe; 1—occupational therapy; and 1—light therapy.
Text Box 1. Major categories of interventions to prevent or delay long-term nursing home placement
|
Caregiver support—Interventions focused on education, training, and supportive counseling for caregivers. Cognitive reframing is a specific type of counseling that aims to change problematic cognitions (e.g., meaning of disruptive behavior displayed by those with dementia) to help caregivers adopt improved strategies for managing difficult situations. Respite care and adult day programs—Interventions that had a primary or major aim of relieving the burden of daily caregiving tasks. These involved providing a set of services, whether at home, in day clinics, or in residential settings, that partially or fully substituted for care provided by family and other social support. Case management—Interventions involved a variety of components, and some specifically described management of common geriatric syndromes. Case managers had variable professional backgrounds (most commonly nursing), and used a variety of modalities for contact with participants. Most interventions provided education on local resources and coordination of services. Often, interventions also included some caregiver counseling and support. Preventive home visits—In contrast to case management interventions, preventive home visits included older participants (e.g., from population registries) without known impairments or high-risk medical conditions. Interventions differed in number of visits (1 to 12). Nearly all included studies employed health professionals (nurses, physicians, and/or social workers) as visitors. |
For specific intervention effects, we prioritized a total of 20 eligible reviews, including all 15 high-quality reviews.21,27,30, 35,37,41,43,44,46,49,53,55,57,60,66 Characteristics of prioritized reviews are provided in Table 1 and intervention effects are summarized in Table 2 (see Appendix Table 3 for detailed quality ratings and Appendix 4 for detailed results). Overall, prioritized reviews found no benefit or inconsistent effects for caregiver support (2 reviews),21,27 respite care and adult day programs (3 reviews),30,35,37 case management (4 reviews),41,43,44,46 preventive home visits (2 reviews),49,51 and interventions to prevent falls (1 review).53 For caregiver support, case management, and preventive home visits, some reviews highlighted benefits in delaying NHP that were reported by a few studies of each intervention. Prioritized reviews on other interventions, including home-based primary care and physical activity programs, generally found a lack of studies examining NHP as an outcome.54,55,57,60,62–64,66 We provide more information below on effects of caregiver support, respite care and adult day programs, case management, and preventive home visits.
Table 1.
Characteristics of 20 Prioritized Systematic Reviews (SRs) on Interventions to Prevent or Delay Long-Term Nursing Home Placement (NHP)
| Interventions | # of SRs* | Recent† | Quality of SRs | SRs including | # of unique studies evaluating NHP§ | |||
|---|---|---|---|---|---|---|---|---|
| High | Medium | Only RCTs | Observational studies‡ | US studies | ||||
| Caregiver support | 2 | 1 | 2 | – | 2 | – | 1 | 7 |
| Respite care and day programs | 3 | 1 | 3 | – | 2 | 1 | 3 | 22 |
| Case management | 4 | 2 | 4 | – | 2 | 1 | 3 | 28 |
| Preventive home visits | 2 | – | 1 | 1 | 1 | 1 | 2 | 32 |
| Others|| | 9 | 6 | 5 | 3 | 5 | 4 | 6 | 11 |
RCTs randomized controlled trials, US United States
*SR prioritized based on higher quality and more recent searches
†Search conducted 2013 or later
‡May have also included RCTs in addition to observational studies
§For each intervention, the total number of unique primary studies identified by SR as evaluating NHP
||2 reviews—physical activity interventions; 1—home-based primary care; 1—interventions for falls prevention; 1—different settings for personal assistance; 1—assistive technologies; 1—demonstration projects to integrate acute and long-term care in the USA and Europe; 1—occupational therapy; and 1—light therapy
Table 2.
Summary of Results on Interventions to Delay or Prevent Long-Term Nursing Home Placement (NHP) from Prioritized Systematic Reviews
| Interventions (# of prioritized reviews) |
Effect on NHP | Description of results |
|---|---|---|
| 13 systematic reviews that limited inclusion to RCTs† | ||
| Caregiver support (2) | ↔/↓ | 1 high-quality review21,67 reported qualitative summaries, stating caregiver interventions “did not consistently improve…institutionalization for patients with memory-related disorders,” but also highlighted results from 2 studies that demonstrated delay in NHP |
| ? | 1 high-quality review on cognitive reframing for caregivers found no RCTs reporting NHP27 | |
| Respite care and day programs (2) | ↔ | 1 high-quality review reported quantitative meta-analysis for adult day programs and found no overall decrease in NHP (OR 0.84, 95% CI 0.58, 1.21) or when separated by type of comparator30 |
| ? | 1 high-quality review on all types of respite care identified only 1 RCT, which reported delay in combined outcome of NHP or death35 | |
| Case management (2) | ↔ | 2 high-quality reviews reported quantitative meta-analyses for adults with dementia—1 review found inconsistent results across different follow-up intervals (reduction in NHP at 6 and 18 months, but not at 10–12 and 24 months);43 1 review found no overall decrease in NHP (RR 0.94 [95% CI 0.85, 1.03]) or delay in timing (WMD 77.8 days [95% CI − 70.5, 226.1])44 |
| Preventive home visits (1) | ↔/↓ | 1 medium-quality review reported quantitative meta-analysis and found no effect overall (RR 0.91 [95% CI 0.76, 1.09]) but suggested more intensive interventions (> 9 visits) may decrease NHP51 |
| Other (5) | ? | 2 medium-quality reviews on physical activity interventions for frail or pre-frail older adults found no RCT reporting NHP63,64 |
| ↔ | 1 high-quality review on a variety of interventions for falls prevention reported qualitative summaries that multifactorial programs and exercise-focused interventions showed inconsistent effects53 | |
| ? | 1 high-quality review on light therapy for adults with dementia found no RCT reporting NHP55 | |
| ? | 1 high-quality review on assistive technologies for adults with dementia found no RCT reporting NHP60 | |
| 7 systematic reviews that included observational studies | ||
| Respite care and day programs (1) | ↑/↓ | 1 high-quality review reported quantitative meta-analysis of “quasi-experimental”‡ studies finding increased NHP (OR 1.79 [95% CI 1.02, 3.12]), but also provided qualitative summary of observational cohort studies, stating that there was “some support for the benefits of respite care…”37 |
| Case management (2) | ↔/↓ | 1 high-quality review reported qualitative summary for adults with dementia, stating that programs ≤ 2 years did not “confer clinically important delays in time to [NHP]” (moderate strength of evidence), but interventions for those with “in-home spouse caregivers and continued services for longer than 2 years” may be effective (low strength of evidence)46 |
| ↔ | 1 high-quality review reported qualitative summary for adults with frailty or multimorbidity, stating no effect on NHP (low strength of evidence)46 | |
| ? | 1 high-quality review on “reablement” interventions for older adults found only 1 study reporting NHP41 | |
| Preventive home visits (1) | ↔ | 1 high-quality review reported quantitative meta-analysis and found no effect overall (RR 1.02 [95% CI 0.88, 1.18]) or by different follow-up intervals49 |
| Other (4) | ? | 1 high-quality review on home-based primary care found no study reporting NHP66 |
| ? | 1 medium-quality review on occupational therapy found only 1 study reporting NHP54 | |
| ? | 1 high-quality review on different settings or models of personal assistance found no studies reporting NHP57 | |
| ↓ | 1 low-quality review reported qualitative summary of demonstration projects to better integrate acute and long-term care, stating decreased NHP occurred in 2 projects62 | |
↑ increased or accelerated NHP, ↔ no meaningful difference or effect, ↓ delayed or prevented NHP, ? reviews identified none or only 1 study, CI confidence interval, HR hazards ratio, OR odds ratio, RR relative risk ratio, RCT randomized controlled trial, WMD weighted mean difference
*Reviews selected based on highest quality and most recent search
†These reviews explicitly allowed only RCTs as included study designs
‡Review authors defined these as observational studies with a comparison group
Caregiver Support
Two high-quality prioritized reviews21,27 focused on caregiver interventions, included only RCTs, and collectively identified 7 studies that addressed NHP. One review27 specifically evaluated cognitive reframing for caregivers of adults with dementia, but was unable to identify trials that reported effects on NHP (despite aiming to examine NHP). The other review, conducted by VA ESP,21,67 evaluated diverse interventions for caregivers of adults with dementia or cancer, and found 7 trials which examined NHP.68–74 All studies focused on caregivers of adults with dementia, and review authors reported that these interventions “did not consistently improve…institutionalization for patients with memory-related disorders.”19 However, authors highlighted results from 2 studies that showed delays in NHP; both studies evaluated the same high-intensity model of caregiver support, including 6 tailored in-person counseling sessions over the first 4 months, and ad hoc contacts by counselors via different modalities throughout the follow-up period.70,74 Review authors rated low strength of evidence for all patient outcomes, including institutionalization.
Respite Care and Adult Day Programs
Three high-quality reviews28,33,35 examined respite care and/or adult day programs, and together identified 22 unique studies. The first review included only RCTs and focused on adult day programs for individuals with a variety of different medical conditions;30 quantitative meta-analysis using data from 13 trials75–87 found no overall benefit for decreasing institutionalization (pooled OR 0.84 [95% CI 0.58, 1.21]) or by different comparators (e.g., OR 0.91 [95% CI 0.70, 1.19] for day program vs. comprehensive geriatric care). Review authors reported “the quality of the body of evidence to be low for … death or institutional care…” The second review examined respite care for adults with dementia in any setting (e.g., at home or at day clinics) and identified only one RCT;35 this trial showed more days (i.e., a combined outcome of not experiencing institutionalization or death) for the intervention group.88 The third review included both RCTs and observational studies of respite care in any setting for adults with a variety of conditions.37 This review identified one RCT,89 4 “quasi-experimental” studies (nonrandomized prospective studies with any comparative control),90–93 and 3 observational cohort studies (without comparators)94–96 that evaluated NHP. Review authors conducted meta-analysis using data from 3 quasi-experimental studies,90–92 and found increased NHP in the respite care groups (OR 1.79 [95% CI 1.02, 3.12]). However, review authors reported that the 3 cohort studies94–96 showed “some support for the benefits of respite care…” Review authors did not indicate overall strength of evidence but noted the role of unmeasured confounders in contributing to these inconsistent results.
Case Management
Four prioritized high-quality reviews41,43,44,46 included 28 unique studies that evaluated effects of case management on NHP. Two reviews focused on adults with dementia,43,44 included only RCTs, and collectively identified 22 unique trials that reported NHP outcomes. One of these reviews43 conducted meta-analyses of data from 9 trials,97–105 stratifying by follow-up interval; there were lower odds of NHP with case management at 6 months (OR 0.82 [95% CI 0.69, 0.98]) and 18 months (OR 0.25 [95% CI 0.10, 0.60]), but not at 10–12 months (OR 0.95 [95% CI 0.83, 1.08]) or 24 months (OR 1.03 [95% CI 0.52, 2.03]). Review authors assessed the strength of evidence as low. The second review44 pooled data for NHP from 16 studies69,71–73,89,97,101,102,106–113 and reported “no statistically significant effect of dementia [case management] compared to usual care” (risk ratio [RR] 0.94 [95% CI 0.85, 1.03]). Additionally, meta-analysis using data on time to NHP from 5 studies69,73,89,110,111 found no statistically significant difference for case management compared with control (weighted mean difference 78.0 days [95% CI − 70.5, 226.1]). Review authors did not provide an assessment of overall strength of evidence.
Two additional reviews addressed older adults with various health conditions and included observational studies in addition to RCTs.41,46 One of these reviews46 found 10 studies that evaluated NHP for adults with dementia74,97,99–102,105,114–116 and 2 that focused on frailty or multimorbidity.117,118 Due to substantial heterogeneity of studies, review authors provided qualitative syntheses. For dementia, programs lasting 2 years or less did not “confer clinically important delays in time to nursing home placement…” (moderate strength of evidence), but those participants “who have in-home spouse caregivers and continue services for longer than 2 years” may benefit from delayed NHP (low strength of evidence). For adults with frailty or multimorbidity, case management did not decrease NHP (low strength of evidence). The other review41 addressed a high-intensity, time-limited case management intervention oriented towards optimizing function, termed “reablement,” for older adults. This review identified only one trial that reported NHP; this trial found no difference in NHP between intervention and control groups.119
Preventive Home Visits
Two prioritized reviews examined preventive home visits and collectively identified 32 unique studies evaluating NHP.49,51 A medium-quality review51 conducted quantitative meta-analysis using data from 13 RCTs120–132 and found overall “reduction in the risk of [NHP] was modest and nonsignificant” (RR 0.91 [95% CI 0.76, 1.09]). In stratified analyses by number of visits (over follow-up of 1–4 years for all studies), interventions with more than 9 visits123,125,127,131 showed an “estimated reduction [of NHP]… 34% (RR, 0.66; 95% CI, 0.48–0.92) and the typical risk difference was 2.3%.” Review authors did not report strength of evidence. The other review49 was high quality and included both RCTs and observational studies using “quasi-random methods that approximated the characteristics of randomization”. Quantitative meta-analysis using data from 26 studies117,121,122,124–128,131,133–149 showed no overall effect of home visits (RR 1.02 [95% CI 0.88, 1.18]). Stratified analyses found similar results across different follow-up intervals (e.g., RR 0.96 [95% CI 0.69, 1.33] for 8 studies with at least 3 years of follow-up).121,125,127,128,131,134,139,147 Review authors concluded there was “moderate quality evidence of no clinically important difference” between intervention and control.
DISCUSSION
We conducted a systematic review of reviews to examine evidence on interventions that may prevent or delay NHP for adults with, or at risk for, impairments. Caregiver support, respite care and adult day programs, case management, and preventive home visits showed inconsistent effects or no benefit for preventing or delaying NHP. Other interventions, such as home-based primary care and physical activity, had very limited to no evidence to address their effects on NHP.
Existing interventions to support adults with impairments often varied in targeted populations, from participants at earlier stages of chronic conditions to individuals with substantial impairments. While interventions addressing those with less impairments may be able to prevent progression of disability, such programs often require large-scale, long-term investments across a population to see appreciable benefits. In contrast, interventions for adults with substantial care needs will have limited ability to alter trajectories of decline. Current interventions for these individuals have largely sought to improve coordination of services and caregiver support, aiming to bolster informal support networks. However, some individuals with substantial needs do not have social support, and even for those who do, these resources can change quickly and dramatically (e.g., death of a spouse). Our results suggest that many existing interventions help meet the needs of adults with impairments only if there is adequate caregiver support.
Addressing NHP in the USA is made more difficult by fragmentation and complexity of the financial and regulatory environment for healthcare and LTSS. These larger environmental factors make early investment (to reap long-term benefits) not financially viable for many healthcare entities and community organizations. They also shape local access (or lack thereof) to services and limit the potential impact of individual interventions, such as case management, that must work with existing resources. Demonstration projects of new financial benefits or incentives150 must also operate within existing local barriers, including availability and quality of service providers. While changes in state and/or national policies may incentivize improved access and/or higher quality of HCBS,2,151 it will likely take time to change the landscape of local resources.
Evidence Gaps and Future Research
In addition to lack of evidence for certain types of interventions, there was great complexity and variability in multicomponent interventions, such as case management. Additionally, review authors noted that underlying primary studies ranged in participant characteristics and setting. These sources of heterogeneity contributed to challenges in categorizing studies and determining summary results across a body of evidence. In some cases, participants’ low risk for NHP contributed to concerns about inadequate power for detecting intervention effects.
To improve the design and evaluation of complex interventions for adults with impairments, future studies should employ strategies or frameworks that explicitly consider which intervention components may be most appropriate for whom and in which settings.152,153 Applying such strategies to inform selection of intervention components, and to describe whether those components were successfully implemented in particular settings, will facilitate future efforts to summarize and interpret results for complex interventions with similar goals. Therefore, we recommend the following:
Randomized evaluations of complex interventions that compare models which differ in only 1–2 key components or setting characteristics (e.g., similar types of services at home vs. in clinic)
Randomized evaluations with longer follow-up (likely > 2 years) and larger sample size, particularly for individuals at lower overall risk of NHP
Application of strategies and frameworks for selecting components and evaluating implementation of interventions, to inform interpretation of results of complex interventions
Implications for Policy
Due to wide variation in local availability of LTSS,154 coordinating care and services remains a key challenge for adults with impairments and their caregivers.155,156 Therefore, case management may offer other substantial benefits, despite our results suggesting the lack of effectiveness for delaying NHP. Successful case management interventions may need to have relatively high-frequency contacts that are initiated early in the course of chronic conditions (e.g., dementia) and extend for several years. Most US adults with impairments, including veterans, do not have access to this level of longitudinal support and care coordination. Implementing and sustaining such high-intensity case management will require better alignment of LTSS programs at state and federal levels.
Additionally, it remains unclear whether (and which) outcomes are improved with HCBS.5 Some have questioned whether the shift of funding to HCBS (and away from nursing homes) is wise, or if this will lead to worse outcomes for those with substantial needs that cannot be met in community settings.4,6 Our results support concerns that increased utilization of existing HCBS may not lead to appreciable changes in NHP, thus indicating the importance of understanding how HCBS may impact other outcomes. We agree with others who have encouraged policymakers to also consider the value of HCBS for improving patient and family-centered outcomes.3,5
Limitations
We focused on NHP and only included reviews that specified NHP as an outcome of interest. Reviews that exclusively addressed other outcomes, such as quality of life or caregiver burden, were ineligible. Therefore, our findings do not indicate that interventions were not effective for these other outcomes. We relied on review authors’ descriptions of interventions, quality ratings for studies included in reviews, and determination of overall strength of evidence. We also included subgroup analyses reported by reviews, some of which relied on observed characteristics of interventions (e.g., average number of follow-up visits), instead of study design elements. To determine how included studies assessed NHP, we examined primary studies included by prioritized reviews. We found that most studies used participant reports of NHP; few confirmed NHP with additional data sources, such as state or federal administrative data on LTSS utilization. No eligible reviews restricted included studies to only those conducted in the USA, and some studies were conducted > 20 years ago. It may be that evidence from outside the USA is less directly applicable to addressing needs of the US population, but we note that the primary difference between the USA and other high-income countries (that were locations of included studies) is funding of LTSS and not the general availability of various services, whether HCBS or long-term institutional care.157 Older studies may also be less applicable, due to changes in availability of HCBS and growth in assisted living facilities.158
Conclusions
Caregiver support, respite care and adult day programs, case management, and preventive home visits generally do not prevent or delay NHP for adults with (or at risk for) impairments, although a few studies suggested benefit for some higher-intensity models. Demonstration of substantial impacts on NHP may require longer-term studies of high-intensity interventions that can be adapted for a variety of settings.
Electronic supplementary material
(DOCX 959 kb)
Funding Information
This work was supported by VA Quality Enhancement Research Initiative (QUERI) funding for ESP (VA-ESP Project No. 09-009; 2019). The funder had no role in the study design, data collection, analysis and interpretation of the data, writing of the report, or decision to submit the article for publication.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Prior Presentations: Results from this evidence review were presented as a poster at the national meeting of the Society for General Internal Medicine in May 2019.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.U.S. Department of Health and Human Services Assistant Secretary for Planning and Evaluation Office of Disability. Aging and long-term care policy. 2018.
- 2.Medicaid. Balancing Long Term Services & Supports.
- 3.Grabowski DC. The cost-effectiveness of noninstitutional long-term care services: review and synthesis of the most recent evidence. Med Care Res Rev. 2006;63(1):3–28. doi: 10.1177/1077558705283120. [DOI] [PubMed] [Google Scholar]
- 4.Konetzka RT. The hidden costs of rebalancing long-term care. Health Serv Res. 2014;49(3):771–7. doi: 10.1111/1475-6773.12190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wysocki A, Butler M, Kane RL, Kane RA, Shippee T, Sainfort F. Long-term services and supports for older adults: a review of home and community-based services versus institutional care. J Aging Soc Policy. 2015;27(3):255–79. doi: 10.1080/08959420.2015.1024545. [DOI] [PubMed] [Google Scholar]
- 6.Wysocki A, Kane RL, Golberstein E, Dowd B, Lum T, Shippee T. The association between long-term care setting and potentially preventable hospitalizations among older dual eligibles. Health Serv Res. 2014;49(3):778–97. doi: 10.1111/1475-6773.12168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duan-Porter W, Ullman K, Rosebush C, McKenzie L, Ensrud KE, Ratner E, et al. Risk Factors and Interventions to Prevent or Delay Long-Term Nursing Home Placement for Adults with Impairments. VA ESP Project #09-009. 2019. [PubMed]
- 8.Colello K, SV. P. Congressional Research Service Report: Long-Term Care Services for Veterans. 2017.
- 9.Department of Veterans Affairs. Budget in brief. 2020.
- 10.Department of Veterans Affairs. Veterans’ families, caregivers, and survivors Federal Advisory Committee planning meeting minutes. October 23-24 2017.
- 11.Department of Veterans Affairs. VA Geriatrics and Gerontology Advisory Committee meeting minutes. October 23-24 2017.
- 12.Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11(1):15. doi: 10.1186/1471-2288-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995:1-10. [PubMed]
- 14.Flaskerud JH, Winslow BJ. Conceptualizing vulnerable populations health-related research. Nurs Res. 1998;47(2):69–78. doi: 10.1097/00006199-199803000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Lawton MP. Environment and other determinants of weil-being in older people. Gerontologist. 1983;23(4):349–57. doi: 10.1093/geront/23.4.349. [DOI] [PubMed] [Google Scholar]
- 16.Wahl HW, Iwarsson S, Oswald F. Aging well and the environment: toward an integrative model and research agenda for the future. Gerontologist. 2012;52(3):306–16. doi: 10.1093/geront/gnr154. [DOI] [PubMed] [Google Scholar]
- 17.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bearman M, Dawson P. Qualitative synthesis and systematic review in health professions education. Med Educ. 2013;47(3):252–60. doi: 10.1111/medu.12092. [DOI] [PubMed] [Google Scholar]
- 19.Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A. Synthesising qualitative and quantitative evidence: a review of possible methods. Journal of health services research & policy. 2005;10(1):45–53. doi: 10.1177/135581960501000110. [DOI] [PubMed] [Google Scholar]
- 20.Dickinson C, Dow J, Gibson G, Hayes L, Robalino S, Robinson L. Psychosocial intervention for carers of people with dementia: what components are most effective and when? A systematic review of systematic reviews. Int Psychogeriatr. 2017;29(1):31–43. doi: 10.1017/S1041610216001447. [DOI] [PubMed] [Google Scholar]
- 21.Griffin JM, Meis LA, Greer N, MacDonald R, Jensen A, Rutks I, et al. Effectiveness of caregiver interventions on patient outcomes in adults with dementia or Alzheimer’s disease: a systematic review. Gerontol Geriatr Med. 2015;1:1–17. doi: 10.1177/2333721415595789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jensen M, Agbata IN, Canavan M, McCarthy G. Effectiveness of educational interventions for informal caregivers of individuals with dementia residing in the community: systematic review and meta-analysis of randomised controlled trials. Int J Geriatr Psychiatry. 2015;30(2):130–43. doi: 10.1002/gps.4208. [DOI] [PubMed] [Google Scholar]
- 23.Pinquart M, Sorensen S. Helping caregivers of persons with dementia: which interventions work and how large are their effects? Int Psychogeriatr. 2006;18(4):577–95. doi: 10.1017/S1041610206003462. [DOI] [PubMed] [Google Scholar]
- 24.Smits CH, de Lange J, Droes RM, Meiland F, Vernooij-Dassen M, Pot AM. Effects of combined intervention programmes for people with dementia living at home and their caregivers: a systematic review. Int J Geriatr Psychiatry. 2007;22(12):1181–93. doi: 10.1002/gps.1805. [DOI] [PubMed] [Google Scholar]
- 25.Vandepitte S, Van Den Noortgate N, Putman K, Verhaeghe S, Faes K, Annemans L. Effectiveness of supporting informal caregivers of people with dementia: a systematic review. Value Health. 2015;18(7):A407–8. doi: 10.1016/j.jval.2015.09.961. [DOI] [PubMed] [Google Scholar]
- 26.Van't Leven N, Prick AE, Groenewoud JG, Roelofs PD, de Lange J, Pot AM. Dyadic interventions for community-dwelling people with dementia and their family caregivers: a systematic review. Int Psychogeriatr. 2013;25(10):1581–603. doi: 10.1017/S1041610213000860. [DOI] [PubMed] [Google Scholar]
- 27.Vernooij-Dassen M, Draskovic I, McCleery J, Downs M. Cognitive reframing for carers of people with dementia. Cochrane Database Syst Rev. 2011;11:CD005318. doi: 10.1002/14651858.CD005318.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goy E, Freeman, M., Kanasagara, D. A systematic evidence review of interventions for non-professional caregivers of individuals with dementia. VA ESP Project #05-225. 2010. [PubMed]
- 29.Parker D, Mills S, Abbey J. Effectiveness of interventions that assist caregivers to support people with dementia living in the community: a systematic review. International Journal of Evidence-Based Healthcare 2008. p. 137-72. [DOI] [PubMed]
- 30.Brown L, Forster A, Young J, Crocker T, Benham A, Langhorne P, et al. Medical day hospital care for older people versus alternative forms of care. Cochrane Database Syst Rev. 2015;6:CD001730. doi: 10.1002/14651858.CD001730.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Du Preez J, Millsteed J, Marquis R, Richmond J. The role of adult day services in supporting the occupational participation of people with dementia and their carers: an integrative review. Healthcare (Basel). 2018;6(2):08. doi: 10.3390/healthcare6020043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ellen MEMBAP, Demaio PBA, Lange AP, Wilson MGP. Adult day center programs and their associated outcomes on clients, caregivers, and the health system: a scoping review. Gerontologist. 2017;57(6). [DOI] [PubMed]
- 33.Fields NL, Anderson KA, Dabelko-Schoeny H. The effectiveness of adult day services for older adults: a review of the literature from 2000 to 2011. J Appl Gerontol. 2014;33(2):130–63. doi: 10.1177/0733464812443308. [DOI] [PubMed] [Google Scholar]
- 34.Brueckmann A, Seeliger C, Schlembach D, Schleussner E. PP048. Carotid intima-media-thickness in the first trimester as a predictor of preeclampsia. Pregnancy Hypertens. 2013;3(2):84. doi: 10.1016/j.preghy.2013.04.075. [DOI] [PubMed] [Google Scholar]
- 35.Lee H, Cameron MH. Respite care for people with dementia and their carers. Cochrane Database Syst Rev. 2014;1:CD004396. doi: 10.1002/14651858.CD004396.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al. A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers. Health Technol Assess. 2007;11(15):1–157. doi: 10.3310/hta11150. [DOI] [PubMed] [Google Scholar]
- 37.Shaw C, McNamara R, Abrams K, Cannings-John R, Hood K, Longo M, et al. Systematic review of respite care in the frail elderly. Health Technol Assess. 2009;13(20):1–224. doi: 10.3310/hta13200. [DOI] [PubMed] [Google Scholar]
- 38.Vandepitte S, Van Den Noortgate N, Putman K, Verhaeghe S, Verdonck C, Annemans L. Effectiveness of respite care in supporting informal caregivers of persons with dementia: a systematic review. Int J Geriatr Psychiatry. 2016;31(12):1277–88. doi: 10.1002/gps.4504. [DOI] [PubMed] [Google Scholar]
- 39.Beswick AD, Gooberman-Hill R, Smith A, Wylde V, Ebrahim S. Maintaining independence in older people. Rev Clin Gerontol. 2010;20(2):128–53. doi: 10.1017/s0959259810000079. [DOI] [Google Scholar]
- 40.Berthelsen CB, Kristensson J. The content, dissemination and effects of case management interventions for informal caregivers of older adults: a systematic review. Int J Nurs Stud. 2015;52(5):988–1002. doi: 10.1016/j.ijnurstu.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 41.Cochrane A, Furlong M, McGilloway S, Molloy DW, Stevenson M, Donnelly M. Time-limited home-care reablement services for maintaining and improving the functional independence of older adults. Cochrane Database Syst Rev. 2016;10:CD010825. doi: 10.1002/14651858.CD010825.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pimouguet C, Lavaud T, Dartigues JF, Helmer C. Dementia case management effectiveness on health care costs and resource utilization: a systematic review of randomized controlled trials. J Nutr Health Aging. 2010;14(8):669–76. doi: 10.1007/s12603-010-0314-4. [DOI] [PubMed] [Google Scholar]
- 43.Reilly S, Miranda-Castillo C, Malouf R, Hoe J, Toot S, Challis D, et al. Case management approaches to home support for people with dementia. Cochrane Database Syst Rev. 2015;1:CD008345. doi: 10.1002/14651858.CD008345.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tam-Tham H, Cepoiu-Martin M, Ronksley PE, Maxwell CJ, Hemmelgarn BR. Dementia case management and risk of long-term care placement: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2013;28(9):889–902. doi: 10.1002/gps.3906. [DOI] [PubMed] [Google Scholar]
- 45.You EC, Dunt DR, Doyle C. Case managed community aged care: what is the evidence for effects on service use and costs? J Aging Health. 2013;25(7):1204–42. doi: 10.1177/0898264313499931. [DOI] [PubMed] [Google Scholar]
- 46.Hickam DH, Weiss JW, Guise J-M, Buckley D, Motu'apuaka M, Graham E, et al. Outpatient case management for adults with medical illness and complex care needs. 2013(Prepared by the Oregon Evidence-based Practice Center under Contract No. 290-2007-10057-I.):AHRQ Publication No.13-EHC031-EF. Rockville, MD: Agency for Healthcare Research and Quality. [PubMed]
- 47.Elkan R, Kendrick D, Dewey M, Hewitt M, Robinson J, Blair M, et al. Effectiveness of home based support for older people: systematic review and meta-analysis. BMJ. 2001;323(7315):719–25. doi: 10.1136/bmj.323.7315.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Markle-Reid M, Browne G, Weir R, Gafni A, Roberts J, Henderson SR. The effectiveness and efficiency of home-based nursing health promotion for older people: a review of the literature. Med Care Res Rev. 2006;63(5):531–69. doi: 10.1177/1077558706290941. [DOI] [PubMed] [Google Scholar]
- 49.Mayo-Wilson E, Grant S, Burton J, Parsons A, Underhill K, Montgomery P. Preventive home visits for mortality, morbidity, and institutionalization in older adults: a systematic review and meta-analysis. PLoS ONE. 2014;9(3):e89257. doi: 10.1371/journal.pone.0089257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ploeg J, Feightner J, Hutchison B, Patterson C, Sigouin C, Gauld M. Effectiveness of preventive primary care outreach interventions aimed at older people: meta-analysis of randomized controlled trials. Can Fam Physician. 2005;51:1244–5. [PMC free article] [PubMed] [Google Scholar]
- 51.Stuck AE, Egger M, Hammer A, Minder CE, Beck JC. Home visits to prevent nursing home admission and functional decline in elderly people: systematic review and meta-regression analysis. JAMA. 2002;287(8):1022–8. doi: 10.1001/jama.287.8.1022. [DOI] [PubMed] [Google Scholar]
- 52.van Haastregt JC, Diederiks JP, van Rossum E, de Witte LP, Crebolder HF. Effects of preventive home visits to elderly people living in the community: systematic review. BMJ. 2000;320(7237):754–8. doi: 10.1136/bmj.320.7237.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, Beil TL. Interventions to prevent falls in older adults: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2018;319(16):1705–16. doi: 10.1001/jama.2017.21962. [DOI] [PubMed] [Google Scholar]
- 54.Steultjens EM, Dekker J, Bouter LM, Jellema S, Bakker EB, van den Ende CH. Occupational therapy for community dwelling elderly people: a systematic review. Age Ageing. 2004;33(5):453–60. doi: 10.1093/ageing/afh174. [DOI] [PubMed] [Google Scholar]
- 55.Forbes D, Blake CM, Thiessen EJ, Peacock S, Hawranik P. Light therapy for improving cognition, activities of daily living, sleep, challenging behaviour, and psychiatric disturbances in dementia. Cochrane Database Syst Rev. 2014;2:CD003946. doi: 10.1002/14651858.CD003946.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wulff KD, Cole DG, Clark RL, Dileonardo R, Leach J, Cooper J, et al. Aberration correction in holographic optical tweezers. Opt Express. 2006;14(9):4170–5. doi: 10.1364/oe.14.004170. [DOI] [PubMed] [Google Scholar]
- 57.Montgomery P, Mayo-Wilson E, Dennis J. Personal assistance for older adults (65+) without dementia. Cochrane Database Syst Rev. 2008;1:CD006855. doi: 10.1002/14651858.CD006855.pub2. [DOI] [PubMed] [Google Scholar]
- 58.Olazaran J, Reisberg B, Clare L, Cruz I, Pena-Casanova J, Del Ser T, et al. Nonpharmacological therapies in Alzheimer’s disease: a systematic review of efficacy. Dement Geriatr Cogn Disord. 2010;30(2):161–78. doi: 10.1159/000316119. [DOI] [PubMed] [Google Scholar]
- 59.Spijker A, Vernooij-Dassen M, Vasse E, Adang E, Wollersheim H, Grol R, et al. Effectiveness of nonpharmacological interventions in delaying the institutionalization of patients with dementia: a meta-analysis. J Am Geriatr Soc. 2008;56(6):1116–28. doi: 10.1111/j.1532-5415.2008.01705.x. [DOI] [PubMed] [Google Scholar]
- 60.Van der Roest HG, Wenborn J, Pastink C, Droes RM, Orrell M. Assistive technology for memory support in dementia. Cochrane Database Syst Rev. 2017;6:CD009627. doi: 10.1002/14651858.CD009627.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gilhooly KJ, Gilhooly ML, Sullivan MP, McIntyre A, Wilson L, Harding E, et al. A meta-review of stress, coping and interventions in dementia and dementia caregiving. BMC Geriatr. 2016;16:106. doi: 10.1186/s12877-016-0280-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Johri M, Beland F, Bergman H. International experiments in integrated care for the elderly: a synthesis of the evidence. Int J Geriatr Psychiatry. 2003;18(3):222–35. doi: 10.1002/gps.819. [DOI] [PubMed] [Google Scholar]
- 63.Frost R, Belk C, Jovicic A, Ricciardi F, Kharicha K, Gardner B, et al. Health promotion interventions for community-dwelling older people with mild or pre-frailty: a systematic review and meta-analysis. BMC Geriatr. 2017;17(1):157. doi: 10.1186/s12877-017-0547-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gine-Garriga M R-FM, Coll-Planas L, Sitja -Rabert M, & Salva A. Correction. Arch Phys Med Rehabil. 2018;99(1):211-2. 10.1016/j.apmr.2017.11.001
- 65.Stall N, Nowaczynski M, Sinha SK. Systematic review of outcomes from home-based primary care programs for homebound older adults. J Am Geriatr Soc. 2014;62(12):2243–51. doi: 10.1111/jgs.13088. [DOI] [PubMed] [Google Scholar]
- 66.Totten AM, White-Chu EF, Wasson N, Morgan E, Kansagara D, Davis-O'Reilly C, et al. Home-based primary care interventions. 2016(Prepared by the Pacific Northwest Evidence-based Practice Center under Contract No. 290-2012-00014-I.):AHRQ Publication No. 15(6)-EHC036-EF. Rockville, MD: Agency for Healthcare Research and Quality. [PubMed]
- 67.Griffin J, Meis L, Carlyle M, Greer N, Jensen A, MacDonald R, et al. Effectiveness of family and caregiver interventions on patient outcomes among adults with cancer or memory-related disorders: a systematic review. VA-ESP Project #09-009. 2013. [PubMed]
- 68.Belle SH, Burgio L, Burns R, Coon D, Czaja SJ, Gallagher-Thompson D, et al. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized, controlled trial. Ann Intern Med. 2006;145(10):727–38. doi: 10.7326/0003-4819-145-10-200611210-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Brodaty H, Mittelman M, Gibson L, Seeher K, Burns A. The effects of counseling spouse caregivers of people with Alzheimer disease taking donepezil and of country of residence on rates of admission to nursing homes and mortality. Am J Geriatr Psychiatry. 2009;17(9):734–43. doi: 10.1097/jgp.0b013e3181a65187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gaugler JE, Reese M, Mittelman MS. Effects of the NYU caregiver intervention-adult child on residential care placement. Gerontologist. 2013;53(6):985–97. doi: 10.1093/geront/gns193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Teri L, Gibbons LE, McCurry SM, Logsdon RG, Buchner DM, Barlow WE, et al. Exercise plus behavioral management in patients with Alzheimer disease: a randomized controlled trial. JAMA. 2003;290(15):2015–22. doi: 10.1001/jama.290.15.2015. [DOI] [PubMed] [Google Scholar]
- 72.Wray LO, Shulan MD, Toseland RW, Freeman KE, Vasquez BE, Gao J. The effect of telephone support groups on costs of care for veterans with dementia. Gerontologist. 2010;50(5):623–31. doi: 10.1093/geront/gnq040. [DOI] [PubMed] [Google Scholar]
- 73.Wright LK, Litaker M, Laraia MT, DeAndrade S. Continuum of care for Alzheimer’s disease: a nurse education and counseling program. Issues Ment Health Nurs. 2001;22(3):231–52. doi: 10.1080/01612840152053084. [DOI] [PubMed] [Google Scholar]
- 74.Mittelman MS, Haley WE, Clay OJ, Roth DL. Improving caregiver well-being delays nursing home placement of patients with Alzheimer disease. Neurology. 2006;67(9):1592–9. doi: 10.1212/01.wnl.0000242727.81172.91. [DOI] [PubMed] [Google Scholar]
- 75.Burch S, Longbottom J, McKay M, Borland C, Prevost T. A randomized controlled trial of day hospital and day centre therapy. Clin Rehabil. 1999;13(2):105–12. doi: 10.1191/026921599671803291. [DOI] [PubMed] [Google Scholar]
- 76.Crotty M, Giles LC, Halbert J, Harding J, Miller M. Home versus day rehabilitation: a randomised controlled trial. Age Ageing. 2008;37(6):628–33. doi: 10.1093/ageing/afn141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Eagle DJ, Guyatt GH, Patterson C, Turpie I, Sackett B, Singer J. Effectiveness of a geriatric day hospital. CMAJ. 1991;144(6):699–704. [PMC free article] [PubMed] [Google Scholar]
- 78.Gladman JR, Lincoln NB, Barer DH. A randomised controlled trial of domiciliary and hospital-based rehabilitation for stroke patients after discharge from hospital. J Neurol Neurosurg Psychiatry. 1993;56(9):960–6. doi: 10.1136/jnnp.56.9.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hedrick S, Branch L. Adult day health care evaluation study. Med Care. 1993;31:SS1–124. [PubMed] [Google Scholar]
- 80.Hui E, Lum CM, Woo J, Or KH, Kay RL. Outcomes of elderly stroke patients. Day hospital versus conventional medical management. Stroke. 1995;26(9):1616–9. doi: 10.1161/01.str.26.9.1616. [DOI] [PubMed] [Google Scholar]
- 81.Masud T, Coupland C, Drummond A, Gladman J, Kendrick D, Sach T, et al. Multifactorial day hospital intervention to reduce falls in high risk older people in primary care: a multi-centre randomised controlled trial [ISRCTN46584556] Trials. 2006;7(1):5. doi: 10.1186/1745-6215-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pitkälä K. The effectiveness of day hospital care on home care patients. J Am Geriatr Soc. 1998;46(9):1086–90. doi: 10.1111/j.1532-5415.1998.tb06645.x. [DOI] [PubMed] [Google Scholar]
- 83.Tucker MA, Davison JG, Ogle SJ. Day hospital rehabilitation--effectiveness and cost in the elderly: a randomised controlled trial. Br Med J (Clin Res Ed). 1984;289(6453):1209–12. doi: 10.1136/bmj.289.6453.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Vetter N, Smith A, Sastry D, Tinker G. Day hospital: pilot study report. St Davids Hospital, Department of Geriatrics: Research Team for the Care of Elderly People; 1989. [Google Scholar]
- 85.Weissert W, Wan T, Livieratos B, Katz S. Effects and costs of day-care services for the chronically ill: a randomized experiment. Med Care. 1980;18(6):567–84. doi: 10.1097/00005650-198006000-00001. [DOI] [PubMed] [Google Scholar]
- 86.Woodford-Williams E, Mc KJ, Trotter IS, Watson D, Bushby C. The day hospital in the community care of the elderly. Gerontol Clin (Basel). 1962;4(3):241–56. doi: 10.1159/000244750. [DOI] [PubMed] [Google Scholar]
- 87.Young JB, Forster A. The Bradford community stroke trial: results at six months. BMJ. 1992;304(6834):1085–9. doi: 10.1136/bmj.304.6834.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lawton MP, Brody EM, Saperstein AR. A controlled study of respite service for caregivers of Alzheimer’s patients. Gerontologist. 1989;29(1):8–16. doi: 10.1093/geront/29.1.8. [DOI] [PubMed] [Google Scholar]
- 89.Brodaty H, Gresham M, Luscombe G. THE PRINCE HENRY HOSPITAL DEMENTIA CAREGIVERS’TRAINING PROGRAMME. J International journal of geriatric psychiatry. 1997;12(2):183–92. doi: 10.1002/(sici)1099-1166(199702)12:2<183::aid-gps584>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 90.Conlin MM, Caranasos GJ, Davidson RA. Reduction of caregiver stress by respite care: a pilot study. South Med J. 1992;85(11):1096–100. doi: 10.1097/00007611-199211000-00010. [DOI] [PubMed] [Google Scholar]
- 91.Zarit SH, Stephens MAP, Townsend A, Greene R. Stress reduction for family caregivers: effects of adult day care use. J Gerontol B Psychol Sci Soc Sci. 1998;53(5):S267–S77. doi: 10.1093/geronb/53b.5.s267. [DOI] [PubMed] [Google Scholar]
- 92.Kosloski K, Montgomery RJ, Youngbauer JG. Utilization of respite services: a comparison of users, seekers, and nonseekers. J Appl Gerontol. 2001;20(1):111–32. [Google Scholar]
- 93.Riordan J, Bennett A. An evaluation of an augmented domiciliary service to older people with dementia and their carers. Aging and Mental Health. 1998;2(2):137–43. [Google Scholar]
- 94.Andrew T, Moriarty J, Levin E, Webb S. Outcome of referral to social services departments for people with cognitive impairment. Int J Geriatr Psychiatry. 2000;15(5):406–14. doi: 10.1002/(sici)1099-1166(200005)15:5<406::aid-gps122>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 95.Bond MJ, Clark MS. Predictors of the decision to yield care of a person with dementia. Australasian Journal on Ageing. 2002;21(2):86–91. [Google Scholar]
- 96.Gaugler JE, Kane RL, Kane RA, Clay T, Newcomer R. Caregiving and institutionalization of cognitively impaired older people: utilizing dynamic predictors of change. Gerontologist. 2003;43(2):219–29. doi: 10.1093/geront/43.2.219. [DOI] [PubMed] [Google Scholar]
- 97.Callahan CM, Boustani MA, Unverzagt FW, Austrom MG, Damush TM, Perkins AJ, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA. 2006;295(18):2148–57. doi: 10.1001/jama.295.18.2148. [DOI] [PubMed] [Google Scholar]
- 98.Chien WT, Lee IY. Randomized controlled trial of a dementia care programme for families of home-resided older people with dementia. J Adv Nurs. 2011;67(4):774–87. doi: 10.1111/j.1365-2648.2010.05537.x. [DOI] [PubMed] [Google Scholar]
- 99.Chien WT, Lee YM. A disease management program for families of persons in Hong Kong with dementia. Psychiatr Serv. 2008;59(4):433–6. doi: 10.1176/ps.2008.59.4.433. [DOI] [PubMed] [Google Scholar]
- 100.Chu P, Edwards J, Levin R, Thomson J. The use of clinical case management for early stage Alzheimer’s patients and their families. Am J Alzheimers Dis Other Demen. 2000;15(5):284–90. [Google Scholar]
- 101.Eloniemi-Sulkava U, Notkola IL, Hentinen M, Kivela SL, Sivenius J, Sulkava R. Effects of supporting community-living demented patients and their caregivers: a randomized trial. J Am Geriatr Soc. 2001;49(10):1282–7. doi: 10.1046/j.1532-5415.2001.49255.x. [DOI] [PubMed] [Google Scholar]
- 102.Eloniemi-Sulkava U, Saarenheimo M, Laakkonen ML, Pietila M, Savikko N, Kautiainen H, et al. Family care as collaboration: effectiveness of a multicomponent support program for elderly couples with dementia. Randomized controlled intervention study. J Am Geriatr Soc. 2009;57(12):2200–8. doi: 10.1111/j.1532-5415.2009.02564.x. [DOI] [PubMed] [Google Scholar]
- 103.Jansen AP, van Hout HP, Nijpels G, Rijmen F, Droes RM, Pot AM, et al. Effectiveness of case management among older adults with early symptoms of dementia and their primary informal caregivers: a randomized clinical trial. Int J Nurs Stud. 2011;48(8):933–43. doi: 10.1016/j.ijnurstu.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 104.Lam LC, Lee JS, Chung JC, Lau A, Woo J, Kwok TC. A randomized controlled trial to examine the effectiveness of case management model for community dwelling older persons with mild dementia in Hong Kong. Int J Geriatr Psychiatry. 2010;25(4):395–402. doi: 10.1002/gps.2352. [DOI] [PubMed] [Google Scholar]
- 105.Newcomer R, Yordi C, DuNah R, Fox P, Wilkinson A. Effects of the Medicare Alzheimer’s Disease Demonstration on caregiver burden and depression. Health Serv Res. 1999;34(3):669–89. [PMC free article] [PubMed] [Google Scholar]
- 106.Duru OK, Ettner SL, Vassar SD, Chodosh J, Vickrey BG. Cost evaluation of a coordinated care management intervention for dementia. Am J Manag Care. 2009;15(8):521–8. [PMC free article] [PubMed] [Google Scholar]
- 107.Fortinsky RH, Kulldorff M, Kleppinger A, Kenyon-Pesce L. Dementia care consultation for family caregivers: collaborative model linking an Alzheimer’s association chapter with primary care physicians. Aging Ment Health. 2009;13(2):162–70. doi: 10.1080/13607860902746160. [DOI] [PubMed] [Google Scholar]
- 108.Gaugler JE, Roth DL, Haley WE, Mittelman MS. Can counseling and support reduce burden and depressive symptoms in caregivers of people with Alzheimer’s disease during the transition to institutionalization? Results from the New York University caregiver intervention study. Journal of the American Geriatrics Society. 2008;56(3):421–8. doi: 10.1111/j.1532-5415.2007.01593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Miller R, Newcomer R, Fox P. Effects of the Medicare Alzheimer’s Disease Demonstration on nursing home entry. Health Serv Res. 1999;34(3):691–714. [PMC free article] [PubMed] [Google Scholar]
- 110.Mittelman MS, Ferris SH, Shulman E, Steinberg G, Levin B. A family intervention to delay nursing home placement of patients with Alzheimer disease. A randomized controlled trial. JAMA. 1996;276(21):1725–31. [PubMed] [Google Scholar]
- 111.Mohide EA, Pringle DM, Streiner DL, Gilbert JR, Muir G, Tew M. A randomized trial of family caregiver support in the home management of dementia. J Am Geriatr Soc. 1990;38(4):446–54. doi: 10.1111/j.1532-5415.1990.tb03544.x. [DOI] [PubMed] [Google Scholar]
- 112.Nobili A, Riva E, Tettamanti M, Lucca U, Liscio M, Petrucci B, et al. The effect of a structured intervention on caregivers of patients with dementia and problem behaviors: a randomized controlled pilot study. Alzheimer Dis Assoc Disord. 2004;18(2):75–82. doi: 10.1097/01.wad.0000126618.98867.fc. [DOI] [PubMed] [Google Scholar]
- 113.Vernooij-Dassen M. Dementia and Homecare: Determinants of the Sense of Competence of Primary Caregivers and the Effect of Professionally Guided Caregiver Support. Lisse, Netherlands: Swets & Zeitlinger; 1993. [Google Scholar]
- 114.Challis D, von Abendorff R, Brown P, Chesterman J, Hughes J. Care management, dementia care and specialist mental health services: an evaluation. Int J Geriatr Psychiatry. 2002;17(4):315–25. doi: 10.1002/gps.595. [DOI] [PubMed] [Google Scholar]
- 115.Eggert GM, Zimmer JG, Hall WJ, Friedman B. Case management: a randomized controlled study comparing a neighborhood team and a centralized individual model. Health Serv Res. 1991;26(4):471–507. [PMC free article] [PubMed] [Google Scholar]
- 116.Mittelman MS, Brodaty H, Wallen AS, Burns A. A three-country randomized controlled trial of a psychosocial intervention for caregivers combined with pharmacological treatment for patients with Alzheimer disease: effects on caregiver depression. Am J Geriatr Psychiatry. 2008;16(11):893–904. doi: 10.1097/JGP.0b013e3181898095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bernabei R, Landi F, Gambassi G, Sgadari A, Zuccala G, Mor V, et al. Randomised trial of impact of model of integrated care and case management for older people living in the community. BMJ. 1998;316(7141):1348–51. doi: 10.1136/bmj.316.7141.1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Boult C, Reider L, Leff B, Frick KD, Boyd CM, Wolff JL, et al. The effect of guided care teams on the use of health services: results from a cluster-randomized controlled trial. Arch Intern Med. 2011;171(5):460–6. doi: 10.1001/archinternmed.2010.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lewin G, De San MK, Knuiman M, Alan J, Boldy D, Hendrie D, et al. A randomised controlled trial of the Home Independence Program, an Australian restorative home-care programme for older adults. Health Soc Care Community. 2013;21(1):69–78. doi: 10.1111/j.1365-2524.2012.01088.x. [DOI] [PubMed] [Google Scholar]
- 120.Carpenter G, Demopoulos G. Screening the elderly in the community: controlled trial of dependency surveillance using a questionnaire administered by volunteers. BMJ. 1990;300(6734):1253–6. doi: 10.1136/bmj.300.6734.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Gunner-Svensson F, Ipsen J, Olsen J, Waldstrom B. Prevention of relocation of the aged in nursing homes. Scand J Prim Health Care. 1984;2(2):49–56. doi: 10.3109/02813438409017704. [DOI] [PubMed] [Google Scholar]
- 122.Hébert R, Dubois M-F, Wolfson C, Chambers L, Cohen C. Factors associated with long-term institutionalization of older people with dementia: data from the Canadian Study of Health and Aging. J Gerontol A Biol Sci Med Sci. 2001;56(11):M693–M9. doi: 10.1093/gerona/56.11.m693. [DOI] [PubMed] [Google Scholar]
- 123.Hendriksen C, Lund E, Strømgård E. Consequences of assessment and intervention among elderly people: a three year randomised controlled trial. Br Med J. 1984;289(6457):1522–4. doi: 10.1136/bmj.289.6457.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Newbury JW, Marley JE, Beilby JJ. A randomised controlled trial of the outcome of health assessment of people aged 75 years and over. Med J Aust. 2001;175(2):104–7. doi: 10.5694/j.1326-5377.2001.tb143541.x. [DOI] [PubMed] [Google Scholar]
- 125.Pathy MJ, Bayer A, Harding K, Dibble A. Randomised trial of case finding and surveillance of elderly people at home. The Lancet. 1992;340(8824):890–3. doi: 10.1016/0140-6736(92)93294-w. [DOI] [PubMed] [Google Scholar]
- 126.Sørensen K, Sivertsen J. Follow-up three years after intervention to relieve unmet medical and social needs of old people. Comprehensive gerontology. Section B, Behavioural, social, and applied sciences. 1988;2(2):85–91. [PubMed] [Google Scholar]
- 127.Stuck AE, Aronow HU, Steiner A, Alessi CA, Bula CJ, Gold MN, et al. A trial of annual in-home comprehensive geriatric assessments for elderly people living in the community. N Engl J Med. 1995;333(18):1184–9. doi: 10.1056/NEJM199511023331805. [DOI] [PubMed] [Google Scholar]
- 128.Stuck AE, Minder CE, Peter-Wüest I, Gillmann G, Egli C, Kesselring A, et al. A randomized trial of in-home visits for disability prevention in community-dwelling older people at low and high risk for nursing home admission. Arch Intern Med. 2000;160(7):977–86. doi: 10.1001/archinte.160.7.977. [DOI] [PubMed] [Google Scholar]
- 129.Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. New England Journal of Medicine. 1994;331(13):821–7. doi: 10.1056/NEJM199409293311301. [DOI] [PubMed] [Google Scholar]
- 130.van Haastregt JC, Diederiks JP, van Rossum E, de Witte LP, Voorhoeve PM, Crebolder HF. Effects of a programme of multifactorial home visits on falls and mobility impairments in elderly people at risk: randomised controlled trial. BMJ. 2000;321(7267):994–8. doi: 10.1136/bmj.321.7267.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.van Rossum E, Frederiks CM, Philipsen H, Portengen K, Wiskerke J, Knipschild P. Effects of preventive home visits to elderly people. BMJ. 1993;307(6895):27–32. doi: 10.1136/bmj.307.6895.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Vetter NJ, Lewis PA, Ford D. Can health visitors prevent fractures in elderly people? BMJ. 1992;304(6831):888–90. doi: 10.1136/bmj.304.6831.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bouman A, Van Rossum E, Ambergen T, Kempen G, Knipschild P. Effects of a home visiting program for older people with poor health status: a randomized, clinical trial in the Netherlands: (See editorial comments by Drs. Andreas Stuck and Robert Kane, pp 561–563) Journal of the American Geriatrics Society. 2008;56(3):397–404. doi: 10.1111/j.1532-5415.2007.01565.x. [DOI] [PubMed] [Google Scholar]
- 134.Byles JE, Tavener M, O'Connell RL, Nair BR, Higginbotham NH, Jackson CL, et al. Randomised controlled trial of health assessments for older Australian veterans and war widows. Med J Aust. 2004;181(4):186–90. doi: 10.5694/j.1326-5377.2004.tb06233.x. [DOI] [PubMed] [Google Scholar]
- 135.Caplan GA, Williams AJ, Daly B, Abraham K. A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department—the DEED II study. J Am Geriatr Soc. 2004;52(9):1417–23. doi: 10.1111/j.1532-5415.2004.52401.x. [DOI] [PubMed] [Google Scholar]
- 136.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet. 1999;353(9147):93–7. doi: 10.1016/S0140-6736(98)06119-4. [DOI] [PubMed] [Google Scholar]
- 137.Counsell SR, Callahan CM, Clark DO, Tu W, Buttar AB, Stump TE, et al. Geriatric care management for low-income seniors: a randomized controlled trial. JAMA. 2007;298(22):2623–33. doi: 10.1001/jama.298.22.2623. [DOI] [PubMed] [Google Scholar]
- 138.Dalby DM, Sellors JW, Fraser FD, Fraser C, van Ineveld C, Howard M. Effect of preventive home visits by a nurse on the outcomes of frail elderly people in the community: a randomized controlled trial. CMAJ. 2000;162(4):497–500. [PMC free article] [PubMed] [Google Scholar]
- 139.Hall N, De Beck P, Johnson D, Mackinnon K, Gutman G, Glick N. Randomized trial of a health promotion program for frail elders. Canadian Journal on Aging/La Revue Canadienne du vieillissement. 1992;11(1):72–91. [Google Scholar]
- 140.Hogan DB, MacDonald FA, Betts J, Bricker S, Ebly EM, Delarue B, et al. A randomized controlled trial of a community-based consultation service to prevent falls. CMAJ. 2001;165(5):537–43. [PMC free article] [PubMed] [Google Scholar]
- 141.Holland R, Lenaghan E, Harvey I, Smith R, Shepstone L, Lipp A, et al. Does home based medication review keep older people out of hospital? The HOMER randomised controlled trial. BMJ. 2005;330(7486):293. doi: 10.1136/bmj.38338.674583.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kono A, Kai I, Sakato C, Harker JO, Rubenstein LZ. Effect of preventive home visits for ambulatory housebound elders in Japan: a pilot study. Aging Clin Exp Res. 2004;16(4):293–9. doi: 10.1007/BF03324554. [DOI] [PubMed] [Google Scholar]
- 143.Kono A, Kanaya Y, Fujita T, Tsumura C, Kondo T, Kushiyama K, et al. Effects of a preventive home visit program in ambulatory frail older people: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2012;67(3):302–9. doi: 10.1093/gerona/glr176. [DOI] [PubMed] [Google Scholar]
- 144.Lenaghan E, Holland R, Brooks A. Home-based medication review in a high risk elderly population in primary care—the POLYMED randomised controlled trial. Age Ageing. 2007;36(3):292–7. doi: 10.1093/ageing/afm036. [DOI] [PubMed] [Google Scholar]
- 145.Shapiro A, Taylor M. Effects of a community-based early intervention program on the subjective well-being, institutionalization, and mortality of low-income elders. Gerontologist. 2002;42(3):334–41. doi: 10.1093/geront/42.3.334. [DOI] [PubMed] [Google Scholar]
- 146.Sommers LS, Marton KI, Barbaccia JC, Randolph J. Physician, nurse, and social worker collaboration in primary care for chronically ill seniors. Arch Intern Med. 2000;160(12):1825–33. doi: 10.1001/archinte.160.12.1825. [DOI] [PubMed] [Google Scholar]
- 147.Thomas R, Worrall G, Elgar F, Knight J. Can they keep going on their own? A four-year randomized trial of functional assessments of community residents. Canadian Journal on Aging/La Revue canadienne du vieillissement. 2007;26(4):379–89. doi: 10.3138/cja.26.4.379. [DOI] [PubMed] [Google Scholar]
- 148.van Hout HP, Jansen AP, van Marwijk HW, Pronk M, Frijters DF, Nijpels G. Prevention of adverse health trajectories in a vulnerable elderly population through nurse home visits: a randomized controlled trial [ISRCTN05358495] J Journals of Gerontology Series A: Biomedical Sciences Medical Sciences. 2010;65(7):734–42. doi: 10.1093/gerona/glq037. [DOI] [PubMed] [Google Scholar]
- 149.Yamada Y, Ikegami N. Preventive home visits for community-dwelling frail elderly people based on Minimum Data Set-Home Care: randomized controlled trial. Geriatrics and Gerontology International. 2003;3(4):236–42. [Google Scholar]
- 150.Kane RA. The noblest experiment of them all: learning from the national channeling evaluation. J Health Services Research. 1988;23(1):189. [PMC free article] [PubMed] [Google Scholar]
- 151.Medicaid. Money Follows the Person.
- 152.Collins LM, Murphy SA, Nair VN, Strecher VJ. A strategy for optimizing and evaluating behavioral interventions. Ann Behav Med. 2005;30(1):65–73. doi: 10.1207/s15324796abm3001_8. [DOI] [PubMed] [Google Scholar]
- 153.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Geriatrics and Gerontology Advisory Committee. Meeting minutes. September 27-28, 2018.
- 155.Veterans Experience Office. Choose home initiative line of action 1 report. June 2018.
- 156.Chapter 6-- Family Caregivers’ Interactions with Healthcare and Long-Term Services and Supports National Academies of Sciences, Engineering, and Medicine. In: Schulz R, Eden J, editors. Families Caring for an Aging America. Washington (DC): The National Academies Press; 2016. [PubMed]
- 157.Colombo F, Llena-Nozal A, Mercier J, Tjadens F. Help wanted? Providing and paying for long-term care. 2011. OECD Health Policy Studies, OECD Publishing; 2011.
- 158.Grabowski DC, Stevenson DG, Cornell PY. Assisted living expansion and the market for nursing home care. Health Serv Res. 2012;47(6):2296–315. doi: 10.1111/j.1475-6773.2012.01425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 959 kb)