Abstract
Malnutrition in hospitalized patients remains a significant problem. Protected Mealtimes is a complex, inter-professional ward-based intervention that was first introduced in the United Kingdom to address this issue. Now implemented internationally, the approach still remains in key policy documents including the National Health Service Essence of Care. This review aims to synthesize the nutrition, satisfaction and quality of life patient/resident outcomes that arise from the implementation of Protected Mealtimes in hospitals and residential aged care facilities and to consider fidelity issues that have been reported in previous research. A defined search strategy was implemented in seven databases to identify full text papers of original research that evaluated Protected Mealtimes implementation. After screening, data were extracted from eight studies (7 quantitative and 1 qualitative study) that were conducted in hospitals. There was no research identified from the aged care sector. There were few positive outcomes that resulted from Protected Mealtimes implementation, many fidelity issues with the intervention were reported. It is apparent that Protected Mealtimes provide few, if any, benefits for hospitalized patients. It is a complex, multi-pronged initiative that has limited fidelity and limited outcomes. As such, we recommend that disinvestment by policy makers for hospitals should be considered, with the implementation of other evidence based mealtime initiatives. We provide no recommendation for disinvestment in the aged care sector, since the approach has not been evaluated against any of the eligible outcomes of this review.
Keywords: disinvestment, hospitals, policy, Protected Mealtimes
Background
The challenge of managing malnutrition in hospital and residential aged care settings is well known. With documented prevalence rates of >30% in hospitals1 and within a range of 10–62% in residential aged care facilities (RACFs),2 different foodservice strategies have been implemented in an effort to improve the nutritional status of patients and residents.3–6 The reality of delivering mealtime care and implementing changes to foodservice systems in complex environments is not as straightforward as it may seem.7,8 Tensions exist between delivering patient centred care and the system in which this care is delivered, attributable to factors including awareness and attitudes, the environment, leadership and time pressures.7
Protected Mealtimes is one approach that has been implemented in many hospitals and RACFs in an attempt to improve the nutritional status of patients and residents. Aiming to facilitate mealtimes that are free from unnecessary interruptions, Protected Mealtimes is a suite of interventions that influence the ward environment. First developed in the United Kingdom (UK), the original policy9 included 12 principles to be considered during mealtimes by clinical and support staff, including foodservice staff. These principles include changes to mealtime practices at the environmental (eg, closing the ward to visitors during mealtimes), staffing (eg, nursing staff will make food a priority during mealtimes; staff breaks to be organised to maximise mealtime staffing), and patient (patients needing assistance will be identified; patients will have an opportunity to wash their hands prior to meal service) levels. Acknowledging that the policy encouraged tailoring to the local context, Protected Mealtime policies have since extended to countries including Australia,10 Denmark11 and Canada.12 The origins of the policy in the UK are found in the implementation of complex inter-professional strategies within the Essence of Care framework and the Productive Ward.13 The current Essence of Care documents14 recommend strategies that are consistent with the original Hospital Caterers Association policy including:
“d. inappropriate activity at meal times, such as cleaning and routine activities, are curtailed, for example, as in the ‘protected meal times’ initiative” (p15), and
“n. People’s meal times are protected from unnecessary interruptions” (p20)
But what is the current evidence for implementing Protected Mealtimes policies in hospitals and RACFs? A previous review15 was limited to studies in hospital settings only where nutritional intake data that arose from the implementation of Protected Mealtimes were reported. This review identified that the impact of the intervention on nutritional intake was limited, however suggested that other potential benefits may arise from implementing this approach. Satisfaction of patients/residents as well as their overall experience are essential considerations of contemporary health systems,16 and the Protected Mealtime experience may benefit patients/residents in ways other than through influencing their nutritional intake.
The current review aims to update and extend the previous review of Protected Mealtimes to provide direction for policy makers and health service/RACF managers. With implementation rates of 40% of health services in the UK17 and 5% in Australian and New Zealand hospitals,10 an evidence based view of the outcomes of the initiative is essential to inform future practice. Specifically, this review aims to synthesize the patient/resident nutrition, satisfaction and quality of life outcomes that arise from the implementation of Protected Mealtimes in hospitals and RACFs. Issues of fidelity with the implementation of Protected Mealtimes will also be explored, as this is known to have been problematic in evaluations conducted early in the UK implementation.17
Methods
We sought full-text papers evaluating the nutrition, satisfaction and quality of life outcomes from the implementation of Protected Mealtimes in hospitals and residential aged care facilities (RACFs). The intervention of interest was the suite of practices that together are described as Protected Mealtimes, with comparison made to usual practice (ie, no Protected Mealtimes intervention implemented). Primary outcomes were patient (hospital)/resident (RACF) outcomes, including nutrition (eg, food intake was observed enabling nutritional intake to be estimated), satisfaction (eg, evaluation using validated patient foodservice satisfaction tools) and quality of life (eg evaluation using validated quality of life tools) outcomes. Research limited to describing barriers and enablers to implementation and descriptions of fidelity to the different aspects of the intervention were not considered. Research undertaken in settings other than hospitals and RACFs was ineligible. Full-text papers were eligible whilst conference abstracts and other non-full text reports were ineligible. No language or date restrictions were applied.
Replicating the searches utilised in the previous review of this topic,15 the keyword search terms protect* AND (mealtime* OR “meal time*”) were used for all database searches. This expansive search strategy was developed to ensure that all relevant papers were captured. Seven databases were searched to identify relevant publications: Ovid MEDLINE, Embase via Ovid, CINAHL Plus, PsycINFO, Scopus, Cochrane Library (including NHS economic evaluations), and the NICE evidence database. Searches were run from database inception until January 2020.
Database searches were exported to Endnote X818 where duplicates were removed. Both authors screened titles/abstracts against the inclusion criteria using Covidence.19 Then, full texts were assessed against the same eligibility criteria to identify studies for inclusion. Any conflicts between authors were resolved through consensus discussion. In addition, reference lists of included studies were hand searched to identify any additional papers that were not included in the database search.
A data extraction template was developed to facilitate comparison between studies. Data extraction was undertaken of author/year/study design, setting/location, participants, description of intervention and control, outcomes (nutritional outcomes, satisfaction and quality of life), and any reported fidelity issues. Results were synthesized narratively due to the heterogeneous study designs, outcomes, and implementation fidelity.
Results
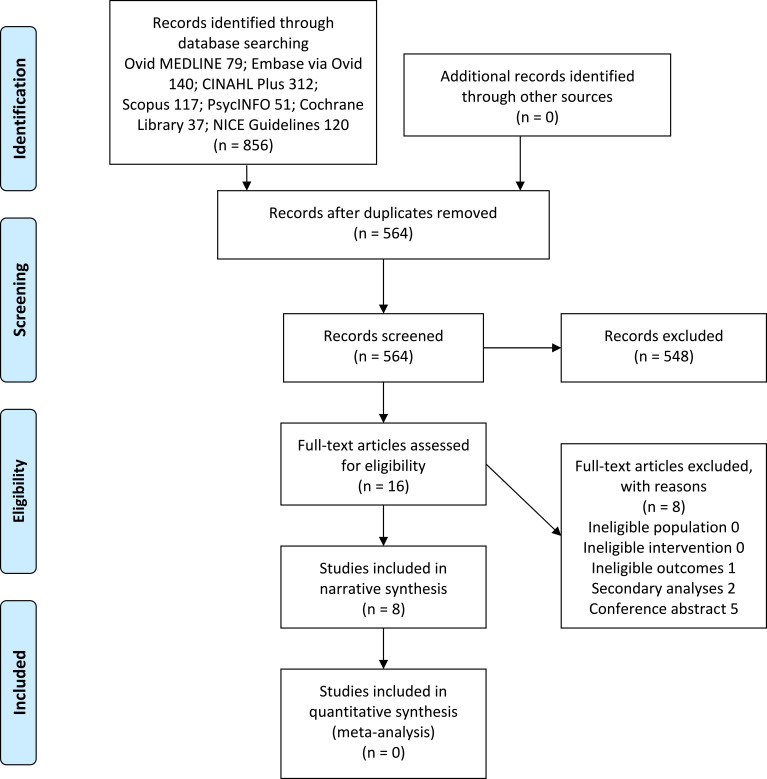
A flowchart highlighting the identification of studies in the database search through to the final library is shown in Figure 1. Many studies were excluded at title/abstract review due to not meeting the inclusion criteria. Broad search terms with few limits or filters were applied during database searching to ensure that all relevant studies were captured, hence a large proportion of irrelevant records were identified. The majority of exclusions at full text review were due to the removal of conference abstracts. Eight studies that sought to evaluate the implementation of Protected Mealtimes using either nutritional or patient satisfaction or outcomes were included. No studies utilised quality of life outcomes to evaluate Protected Mealtimes. The sample size of contributing studies varied considerably from n=13 in the qualitative study20 to larger quantitative studies21–27 including observations of 799 meals pre- and 833 meals post-implementation of Protected Mealtimes in the study of Huxtable & Palmer.23 These studies were from Denmark,20 Canada,20 England22,25 and Australia.23,24,26,27 All were conducted in hospitals, there were no studies identified that evaluated Protected Mealtimes implementation in RACFs.
Figure 1.
Flow diagram of study selection from database searching through to final library of included studies.
Guided by the original Protected Mealtimes policy, implementation varied between aiming to implement all of the aspects of the original policy, through to tailoring implementation to the local context. For example, whilst the study of Huxtable & Palmer23 included the provision of additional staffing (volunteers introduced to provide mealtime assistance), other studies reported (or did not report) no staffing changes.
The focus of the body of Protected Mealtimes research was on understanding change in nutritional intake. Five of the included studies21–23,26,27 were quantitative studies with estimates of energy and protein intake conducted pre- and post-implementation of the intervention. An increase in daily energy and protein intake was reported in the study of n=33 participants in Canada,21 however the only statistically significant change across all included studies was in breakfast protein consumption.23 No other studies reported significant changes in nutritional intake.
Some studies sought to understand other outcomes that may arise from Protected Mealtimes implementation. The study of Ng et al25 evaluated blood glucose levels in patients admitted to a specialist diabetes unit. No changes to blood glucose levels, hypoglycaemia incidence or length of stay occurred as a result of the introduction of Protected Mealtimes. Jefferies et al24 explored Protected Mealtimes implementation through the measurement of patient food satisfaction. Some improvements were reported (amount of food received and meal tray appearance), however it was unclear if there were changes to these practices as part of the introduction of Protected Mealtimes.
The only study that used a qualitative method was that of Beck et al20 who conducted semi-structured interviews with 13 patients on a neurological ward. Participants responded positively to Protected Mealtimes, with the pre-meal bell enabling them to be prepared for the meal. They appreciated the calmness and aesthetics that arose from Protected Mealtimes implementation. Participants also viewed the mealtime intervention with a level of trust, and felt frustrated and/or distrustful when their mealtimes were interrupted. No studies reported on patient satisfaction with the intervention using quantitative methods.
All studies where fidelity with Protected Mealtimes was evaluated reported implementation challenges. In several studies where mealtime practices were observed there were notable increases in the number and length of positive mealtime interruptions, and reductions in unnecessary interruptions, consistent with the intent of the intervention. Increased provision of mealtime assistance did not always occur as intended.23 Ward based practices, eg, meal signs displayed and ward entry doors closed, were more frequently reported post-Protected Mealtimes implementation.
Discussion
The present review aimed to synthesize the patient/resident nutrition, satisfaction and quality of life outcomes that arise from the implementation of Protected Mealtimes, and to explore issues of implementation fidelity, in hospitals and RACFs. This review builds on the previous review which concluded that there was “insufficient evidence for widespread implementation of Protected Mealtimes in hospitals”15(p62). The searches for the previous review were run four years prior to the present review, with the setting of interest extended this time to include RACFs and additional other clinical outcomes, patient satisfaction and quality of life, as well as an extended search timeframe. As such, five of the eight included studies in the current review were either not published or were ineligible for the previous review. The studies that overlap between the previous and current review are those of Hickson et al22 Huxtable and Palmer,23 and Young et al.27
This review has identified consistent findings across the body of evidence for Protected Mealtimes. Unlike evidence translation in many aspects of healthcare (including nutritional care)28 which can progress very slowly, Protected Mealtimes have been implemented internationally with an insufficient evidence base to warrant the many changes that it brings to the hospital ward routine. Although this hurried adoption of a practice in the absence of studies that show significant improvements to patient outcome is not new, Protected Mealtimes is another example of translation into policy of a practice that had never been evaluated in the clinical context.29
Based on the findings of this review it is apparent that Protected Mealtimes provides few, if any, nutritional benefits for hospitalized patients. The fidelity data extracted in Table 1 facilitates a greater understanding of why this policy has not delivered the anticipated changes in nutritional intake. To this point the policy has not had the staffing support to implement it well. Since the redistribution of staff roles to manage mealtime care within pre-existing staff models is insufficient, the outcomes may have been different with substantial increases in staff numbers/availability to support mealtimes. If implemented, the effect of staffing changes on the outcomes evaluated within this review would require evaluation, including cost-effectiveness.30
Table 1.
Study Characteristics and Outcomes of Included Studies
| Author; Year; Study Design | Setting, Location | Participants | Description of Intervention | Description of Control | Outcomes | Fidelity Issues Reported |
|---|---|---|---|---|---|---|
| Beck et al;20 2017; Semi-structured interviews with patients post-intervention | 2 neurological wards, Denmark | n=13 patients | Intervention “Quiet Please” developed based on PM tailored to the local context. | Not applicable | 3 themes emerged: the importance of the bell prior to mealtimes; calmness and aesthetics; a trust-bearing agreement | Not measured quantitatively. Patients described feeling disappointed when the mealtime intervention was not implemented by staff. Where this occurred patients reported feeling frustrated and some distrust of staff. |
| Goarley et al;21 2019; Quantitative pre-post study | 1 non-acute hospital unit, Canada | n=33 adults Observations were made for 4 days before and after PM implementation |
PM implementation focused specifically on interruptions and mealtime assistance | Pre-intervention ward conditions not reported | Mean energy per person/day increased 6715kJ to 7096kJ (increase 5.4%); mean protein intake per person/day increased from 60.1g to 64.7g (increase 7.2%) | Number and length of interruptions decreased (46.6% and 25.2%), average length of assistance increased (26.4%) |
| Hickson et al;22 2011a; Quantitative pre-post study | 40 pre- and 34 post-intervention wards across 2 acute hospitals, England | Pre-intervention: n=253 patients observed for patient mealtime experience; post-intervention: n=237 patients observed for patient mealtime experience | PM introduced through guideline document, Hospital staff dissemination, Intranet messages, large PM signage at mealtimes | Pre-intervention ward conditions not reported | Mean±SD: Energy intake meal pre-intervention: 1281 ±1017 kJ/per meal, post-intervention: 1093±1068 kJ/per meal; protein intake pre-intervention 15.0±11.6 g/meal, post- intervention 10.6±11.2 g/meal. |
Mealtime environment observations (ward level): no statistically significant improvements (at p≥0.05) but improvements reported in some observations. Statistically significant improvements in some patient-level observations, eg patients offered opportunity to wash hands, table clean and clutter free. |
| Huxtable et al;23 2013; Quantitative pre-post study | 6 acute hospital wards, Australia | n=799 meals pre- and n=833 meals post-intervention | Range of PM strategies implemented; volunteers also introduced to provide mealtime assistance. | Pre-intervention ward conditions not reported | All meals (mean± SD): energy intake: pre-intervention 1466±660 kJ, post-intervention 1467±635 kJ (p = 0.979); protein intake: pre- intervention 15±7 g, post-intervention 15± 7g (p = 0.482). Protein (breakfast): pre-intervention 10±5 g, post-intervention 12±6 g (p = 0.025). |
Patients receiving mealtime assistance was unchanged (p=0.928); feeding assistance increased from 15–29% (p=0.002); interruptions were less likely to occur pre-PM. |
| Jefferies et al;24 2015; Quantitative pre-post study | 14 pre- and 20 post intervention wards across 3 hospitals, Australia | n=435 (pre) and n=422 patients (post) observed at mealtimes; n=226 (pre) and n=240 patients (post) completed a food satisfaction survey | Locally developed policy based on UK PM model | Pre-intervention ward conditions not specifically reported, volunteers were available | Patient satisfaction was reported using the locally developed Patient Food Satisfaction Survey. Significant improvements noted in statements relating to amount of food received and meal tray appearance, but no other statements. | No statistically significant difference in the mealtime assistance required, most patients required limited or no assistance. Where feeding assistance was required, most patients received adequate levels of assistance: pre-PM 82.7%, post-PM 883% (p-0.058). Use of bedside signage and nursing notes improved significantly, as did use of carers for provision of mealtime assistance. No statistically significant differences in other mealtime observations reported. |
| Ng et al;25 2010; Quantitative pre-post study | 1 specialist diabetes unit, England | n=136 pre- and n=158 post- PM implementation | PM based on Hospital Caterers Association; 1 hour was allocated for PM at each of 3 meal periods. Except for emergencies, staff were refrained from interrupting patients during this period, including the administration of anti-diabetes therapy. | Pre-intervention ward conditions not reported | Mean blood glucose (mmol/L [±SE]) pre-PM 10.7±0.33, post-PM 10.6±0.32, p=0.79; incidence of hypoglycaemia (CG <3.5 mmol/L) pre-PM 20.4%, post-PM 25.2%, p= 0.36; mean length of stay (days) pre-PM 3.7, post-PM 4, p=0.11 |
Not reported |
| Porter et al;26 2017; Stepped wedge cluster randomised controlled trial | 3 subacute wards in 3 hospitals, Australia | n=149 participants, with n=210 24 hour meal observations made in control period, n=206 meal observations made in observation period | Intervention designed according to the British Hospital Caterers Association PM reference policy and by principles of implementation science. | Patients continued to receive usual mealtime care which did not include PM. | Energy intake (kJ/day) (mean±SD): control 6532 ± 2328, intervention 6479 ± 2486, p=0.876; Protein intake (g/day) (mean±SD): control 67.0 ± 25.2, intervention 68.6 ± 26.0, p=0.860 | Fidelity was variable. Between control and intervention the number of positive interruptions increased in number and length, number of negative interruptions decreased; ward entry doors were closed more (9 control vs 23 PM), meal sign displayed (13 control vs 31 PM); other changes were limited. |
| Young et al;27 2013; Quantitative pre-post study | 1 acute hospital, Australia | Pre-intervention: n=115 patients 79.4±7.9 years; post-intervention: n=39 patients 82.8±7.7 years | No changes to staffing; strategies negotiated with clinicians and support staff for PM introduction including: - limit non-urgent activities and interruptions at mealtimes - re-prioritise clinical tasks to focus on meals at mealtimes - clinical staff to encourage and assist patients with nutritional intake |
Established malnutrition screening and nutrition support policies implemented. No mealtime procedures with mealtime assistance provided by nursing staff in an unstructured manner | Mean±SD: 24hr energy intake: pre-intervention 5011±1774 kJ, post-intervention 4957±2237 kJ; protein intake: pre-intervention 47±19g, post-intervention 43±21g. Intake (mean per kg): Energy: pre-intervention 75kJ/kg, post-intervention 76kJ/kg; protein: pre-intervention 0.7g/kg, post-intervention 0.7g/kg. |
Mealtime assistance increased from 30% pre-PM to 80% post-PM; mealtime interruptions decreased from pre-PM 38% to 33%; reduction in non-clinical nursing tasks during mealtimes from pre-PM 66% to 27% post-PM. |
Notes: aUnpublished nutritional intake data (mean ±SD) provided previously by authors for 39 patients pre- and 60 patients post-intervention. 1 kilocalorie= 4.18 kilojoules.
Abbreviation: PM, Protected Mealtimes.
Our synthesis of the current evidence for Protected Mealtimes is that it is a complex, multi-pronged initiative that has limited fidelity and limited known outcomes. As such, we recommend that future research should be conducted to explore the intervention from the perspectives of patients (eg, through measurement of satisfaction and quality of life). Alternatively, disinvestment by policy makers for hospitals through substituting this intervention with another evidence based approach may be considered. We provide no recommendation for disinvestment in the RACF sector, since the approach has not been evaluated against any of the eligible outcomes of this review. Rather, future research evaluating implementation of Protected Mealtimes in this setting is required.
There is an increasingly large body of evidence associated with disinvestment in health-care processes where high-value outcomes are unlikely to result. Hundreds of clinical interventions have been identified for potential disinvestment,31,32 for example, reducing inappropriate referrals and reducing the number of funded IVF cycles. Disinvestment also applies at a policy level, and on the findings of this review, we encourage policy makers at a national and hospital/trust level to remove the recommendation that staff protect mealtimes. Indeed, disinvestment is occurring within other aspects of dietetic care as a result of workload management and staff capabilities.33 Nutrition-related strategies that are evidence based, such as the introduction of volunteer mealtime assistance for specific patients,6 are warranted. Our recommendation is for substitution rather than full withdrawal, restriction or retraction disinvestment models of mealtime care.34
This is not to say that aspects of Protected Mealtimes are not clinically valuable, or desirable from the perspective of patients.20 A secondary analysis of the Huxtable et al23 research included in this review identified that some specific factors of the Protected Mealtimes initiative resulted in statistically significant changes. These included that the need for mealtime assistance was identified and documented, patients were appropriately positioned, and volunteers were introduced to the ward.35 The broader literature suggests that mealtime assistance programs can be implemented as a standalone strategy and are therefore evidence based.6 A mealtime assistance program requires far less organizational change both in implementation and evaluation cycles than the more complex Protected Mealtimes program. The provision of mealtime assistance is embedded within the broader suite of Protected Mealtimes principles where staff should be able “to deliver and assist patients/clients with food” and “patients requiring assistance with food will be identified to the ward/unit team prior to the service of meals”9 and its use as a standalone strategy has yielded positive findings.
Strengths of this review include a wide ranging search strategy across seven databases with no language or date restrictions applied. We acknowledge that different approaches were considered in the design of this review. A content analysis of available policies would have enabled synthesis of differences between Protected Mealtimes policies and implementation strategies within NHS Trusts and internationally. A limitation of this approach is that many policies exist behind network intranet sites, and those available widely on the internet may not be a representative sample. Removal of restrictions applied to the pool of literature such as the requirement for full text papers may have increased the size of the final library. However, authors applied this restriction after consideration of the previous published Protected Mealtimes review15 where all non-full text papers rated as negative during the quality assessment. It is also acknowledged that the mealtime principles incorporated within the Protected Mealtimes approach may have been implemented and evaluated without being named as such. The search strategy was dependent on the term “Protected Mealtimes” to identify papers for inclusion; where this term was not included then relevant studies may have been overlooked.
Conclusion
There are limited positive findings for the implementation of Protected Mealtimes across the body of evidence identified and synthesized within this review. Issues of fidelity are also consistently noted across the evidence base. Findings support the disinvestment of Protected Mealtimes from hospital policy documents in the UK and elsewhere.
Author Contributions
All authors contributed towards data analysis, drafting and critically revising the paper, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Agarwal E, Ferguson M, Banks M, et al. Malnutrition and poor food intake are associated with prolonged hospital stay, frequent readmissions, and greater in-hospital mortality: results from the Nutrition Care Day Survey 2010. Clin Nutr. 2013;32(5):737–745. doi: 10.1016/j.clnu.2012.11.021 [DOI] [PubMed] [Google Scholar]
- 2.Bell CL, Tamura BK, Masaki KH, et al. Prevalence and measures of nutritional compromise among nursing home patients: weight loss, low body mass index, malnutrition, and feeding dependency, a systematic review of the literature. J Am Med Dir Assoc. 2013;14(2):94–100. doi: 10.1016/j.jamda.2012.10.012 [DOI] [PubMed] [Google Scholar]
- 3.Dijxhoorn DN, Mortier MJMJ, van den Berg MGA, Wanten GJA. The currently available literature on inpatient foodservices: systematic review and critical appraisal. J Acad Nutr Diet. 2019;119(7):1118–1141.e36. doi: 10.1016/j.jand.2019.01.018 [DOI] [PubMed] [Google Scholar]
- 4.MacKenzie-Shalders K, Maunder K, So D, Norris R, McCray S. Impact of electronic bedside meal ordering systems on dietary intake, patient satisfaction, plate waste and costs: a systematic literature review. Nutr Diet. 2020;77(1):103–111. doi: 10.1111/1747-0080.12600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ottrey E, Porter J. Hospital menu interventions: a systematic review of research. Int J Health Care Qual Assur. 2016;29(1):62–74. doi: 10.1108/IJHCQA-04-2015-0051 [DOI] [PubMed] [Google Scholar]
- 6.Tassone E, Tovey J, Paciepnik J, et al. Should we implement mealtime assistance in the hospital setting? A systematic literature review with meta-analyses of current research. J Clin Nurs. 2015;24(19–20):2710–2721. doi: 10.1111/jocn.12913 [DOI] [PubMed] [Google Scholar]
- 7.Ottrey E, Porter J, Huggins C, Palermo C. “Meal realities” An ethnographic exploration of hospital mealtime environment and practice. J Adv Nurs. 2018;74(3):603–613. doi: 10.1111/jan.13477 [DOI] [PubMed] [Google Scholar]
- 8.Ottrey E, Palermo C, Huggins CE, Porter J. A longitudinal ethnographic study of hospital staff attitudes and experiences of change in nutrition care. J Hum Nutr Diet. 2020. doi: 10.1111/jhn.12734 [DOI] [PubMed] [Google Scholar]
- 9.Hospital Caterers Association. Protected mealtimes policy; 2004. Available from: http://www.hospitalcaterers.org/media/1817/pmd.pdf. Accessed February3, 2020.
- 10.Agarwal E, Ferguson M, Banks M, Bauer J, Capra S, Isenring E. Nutritional status and dietary intake of acute care patients: results from the Nutrition Care Day Survey 2010. Clin Nutr. 2012;31(1):41–47. doi: 10.1016/j.clnu.2011.08.002 [DOI] [PubMed] [Google Scholar]
- 11.Beck M, Martinsen B, Birkelund R, Poulsen I. Raising a beautiful swan: a phenomenological hermeneutic interpretation of health professionals’ experiences of participating in a mealtime intervention inspired by protected mealtimes. Int J Qual Stud Health Well-being. 2017;12(1):1. doi: 10.1080/17482631.2017.1360699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chan J, Carpenter C. An evaluation of a pilot protected mealtime program in a Canadian hospital. Can J Diet Pract Res. 2015;76(2):81–85. doi: 10.3148/cjdpr-2014-035 [DOI] [PubMed] [Google Scholar]
- 13.Robert G, Sarre S, Maben J, Griffiths P, Chable R. Exploring the sustainability of quality improvement interventions in healthcare organisations: a multiple methods study of the 10-year impact of the ‘Productive Ward: releasing Time to Care’ programme in English acute hospitals. BMJ Qual Saf. 2020;29(1):31–40. doi: 10.1136/bmjqs-2019-009457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Department of Health. Essence of care; 2010. Available from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216691/dh_119978.pdf. Accessed February3, 2020.
- 15.Porter J, Ottrey E, Huggins CE. Protected mealtimes in hospitals and nutritional intake: systematic review and meta-analyses. Int J Nurs Stud. 2017;65:62–69. doi: 10.1016/j.ijnurstu.2016.11.002 [DOI] [PubMed] [Google Scholar]
- 16.Porter J. The perspectives of patients and their families remain largely unheard in mealtime assistance research. Evid Based Nurs. 2017;20(3):95–96. doi: 10.1136/eb-2017-102682 [DOI] [PubMed] [Google Scholar]
- 17.National Health Service. Protected mealtimes review –Findings and recommendations report –V1; 2007. National Patient Safety Agency. Available from: https://webarchive.nationalarchives.gov.uk/20180501172657/http://www.nrls.npsa.nhs.uk/resources/search-by-audience/hospital-doctor/?entryid45=59806&p=2. Accessed February3, 2020.
- 18.Endnote X8; Clarivate Analytics. Philadelphia, PA, USA; 2017. [Google Scholar]
- 19.Covidence Systematic Review Software. Melbourne, Australia: Veritas Health Innovation; 2018. [Google Scholar]
- 20.Beck M, Birkelund R, Poulsen I, Martinsen B. Supporting existential care with protected mealtimes: patients’ experiences of a mealtime intervention in a neurological ward. J Adv Nurs. 2017;73(8):1947–1957. doi: 10.1111/jan.13278 [DOI] [PubMed] [Google Scholar]
- 21.Goarley A, Abou El Hassan D, Ahmadi L. Effect of a protected mealtime pilot on energy and protein intake in a Canadian hospital. Can J Diet Pract Res. 2019;81:1–3. [DOI] [PubMed] [Google Scholar]
- 22.Hickson M, Connolly A, Whelan K. Impact of protected mealtimes on ward mealtime environment, patient experience and nutrient intake in hospitalised patients. J Hum Nutr Diet. 2011;24(4):370–374. doi: 10.1111/j.1365-277X.2011.01167.x [DOI] [PubMed] [Google Scholar]
- 23.Huxtable S, Palmer M. The efficacy of protected mealtimes in reducing mealtime interruptions and improving mealtime assistance in adult inpatients in an Australian hospital. Eur J Clin Nutr. 2013;67(9):904–910. doi: 10.1038/ejcn.2013.126 [DOI] [PubMed] [Google Scholar]
- 24.Jefferies D, Johnson M, Langdon R. Rekindling the role of nurses in patients’ oral nutrition. Int J Nurs Pract. 2015;21(3):286–296. doi: 10.1111/ijn.12269 [DOI] [PubMed] [Google Scholar]
- 25.Ng JM, Mellor DD, Narayanan D, et al. Do protected mealtimes improve inpatient glycaemic control? J Diabetes Nurs. 2010;14(6):234–238. [Google Scholar]
- 26.Porter J, Haines T, Truby H. The efficacy of Protected Mealtimes in hospitalised patients: a stepped wedge cluster randomised controlled trial. BMC Med. 2017;15(1):25. doi: 10.1186/s12916-017-0780-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Young AM, Mudge AM, Banks M, et al. Encouraging, assisting and time to EAT: improved nutritional intake for older medical patients receiving Protected Mealtimes and/or additional nursing feeding assistances. Clin Nutr. 2013;32(4):543–549. doi: 10.1016/j.clnu.2012.11.009 [DOI] [PubMed] [Google Scholar]
- 28.Thirsk J. Editorial: knowledge translation. Nutr Diet. 2018;75(4):341–344. doi: 10.1111/1747-0080.12466 [DOI] [PubMed] [Google Scholar]
- 29.Balas EA, Chapman WW. Road map for diffusion of innovation in health care. Health Aff. 2018;37(2):198–204. doi: 10.1377/hlthaff.2017.1155 [DOI] [PubMed] [Google Scholar]
- 30.Mitchell H, Porter J. The cost-effectiveness of identifying and treating malnutrition - a systematic review. J Hum Nutr Diet. 2016;29(2):156–164. doi: 10.1111/jhn.12308 [DOI] [PubMed] [Google Scholar]
- 31.Garner S, Littlejohns P. Disinvestment from low value clinical interventions: NICEly done? BMJ. 2011;343(jul27 2):d4519. doi: 10.1136/bmj.d4519 [DOI] [PubMed] [Google Scholar]
- 32.Daniels T, Williams I, Robinson S, Spence K. Tackling disinvestment in health care services. The views of resource allocators in the English NHS. J Health Organ Manag. 2013;27(6):762–780. doi: 10.1108/JHOM-11-2012-0225 [DOI] [PubMed] [Google Scholar]
- 33.Bell JJ, Young A, Hill J, et al. Rationale and developmental methodology for the SIMPLE approach: a systematised, interdisciplinary malnutrition pathway for implementation and evaluation in hospitals. Nutr Diet. 2018;75(2):226–234. doi: 10.1111/1747-0080.12406 [DOI] [PubMed] [Google Scholar]
- 34.Daniels T, Williams I, Robinson S, Spence K. Tackling disinvestment in health care services. J Health Organ Manag. 2013;27(6):762–780. [DOI] [PubMed] [Google Scholar]
- 35.Palmer M, Huxtable S. Aspects of protected mealtimes are associated with improved mealtime energy and protein intakes in hospitalized adult patients on medical and surgical wards over 2 years. Eur J Clin Nutr. 2015;69(8):961–965. doi: 10.1038/ejcn.2015.87 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Hospital Caterers Association. Protected mealtimes policy; 2004. Available from: http://www.hospitalcaterers.org/media/1817/pmd.pdf. Accessed February3, 2020.
- Department of Health. Essence of care; 2010. Available from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216691/dh_119978.pdf. Accessed February3, 2020.
- National Health Service. Protected mealtimes review –Findings and recommendations report –V1; 2007. National Patient Safety Agency. Available from: https://webarchive.nationalarchives.gov.uk/20180501172657/http://www.nrls.npsa.nhs.uk/resources/search-by-audience/hospital-doctor/?entryid45=59806&p=2. Accessed February3, 2020.