Abstract
Introduction
For patients with brain metastases, palliative radiation therapy (RT) has long been a standard of care for improving quality of life and optimizing intracranial disease control. The duration of time between completion of palliative RT and patient death has rarely been evaluated.
Methods
A compilation of two prospective institutional databases encompassing April 2015 through December 2018 was used to identify patients who received palliative intracranial radiation therapy. A multivariate logistic regression model characterized patients adjusting for age, sex, admission status (inpatient versus outpatient), Karnofsky Performance Status (KPS), and radiation therapy indication.
Results
136 consecutive patients received intracranial palliative radiation therapy. Patients with baseline KPS <70 (OR = 2.2; 95%CI = 1.6–3.1; p < 0.0001) were significantly more likely to die within 30 days of treatment. Intracranial palliative radiation therapy was most commonly delivered to provide local control (66% of patients) or alleviate neurologic symptoms (32% of patients), and was most commonly delivered via whole brain radiation therapy in 10 fractions to 30 Gy (38% of patients). Of the 42 patients who died within 30 days of RT, 31 (74%) received at least 10 fractions.
Conclusions
Our findings indicate that baseline KPS <70 is independently predictive of death within 30 days of palliative intracranial RT, and that a large majority of patients who died within 30 days received at least 10 fractions. These results indicate that for poor performance status patients requiring palliative intracranial radiation, hypofractionated RT courses should be strongly considered.
Keywords: Metastatic brain disease, Radiation therapy, 30-day mortality, Fractionation, Palliative Care, Performance status
1. Introduction
Developing in approximately 30% of adults with cancer, brain metastases afflict more than 200,000 people annually in the United States with increasing incidence due to an aging population, improvements in systemic therapy, and the improved ability of imaging modalities to detect small lesions.1, 2, 3 Palliative radiation therapy (RT) for patients with brain metastases has long been a standard of care for improving quality of life and optimizing intracranial disease control.4, 5, 6 A recent analysis revealed that nearly half of patients prescribed standard fractionation (30 Gy in 10 fractions over two weeks) whole brain radiation therapy (WBRT) died before finishing treatment.7 The duration of time between completion of palliative RT for neurologic disease and patient death has rarely been evaluated; previous recursive partitioning analysis of Radiation Therapy Oncology Group (RTOG) brain metastases trials revealed the median survival of patients with Karnofsky Performance Status (KPS) <70 to be 2.3 months, compared to 7.1 months in patients with KPS >70 with isolated brain metastases, age <65 and primary controlled disease.8 We sought to assess factors associated with 30-day mortality following completion of palliative RT for metastatic brain disease.
2. Methods
A compilation of two prospective institutional review board (IRB)-approved databases encompassing April 2015 through December 2018 was used to identify patients who received palliative intracranial radiation therapy. Multivariate logistic regression models characterized patients adjusting for age, sex, admission status (inpatient versus outpatient), KPS, and radiation therapy indication. Functional independence was defined as KPS of at least 70; 30-day mortality was defined as death within 30 days immediately after final radiation treatment. Statistical analyses were performed in SPSS v.24 (IBM Corp., Armonk, NY). p < 0.05 was considered statistically significant.
3. Results
136 consecutive patients received intracranial palliative RT, which was most commonly delivered to provide local control (66% of patients) or alleviate neurologic symptoms (32% of patients). The most common intracranial palliative RT modality was WBRT in 10 fractions to 30 Gy (37.5% of patients). Thirty-seven patients (27.2%) received single-fraction stereotactic radiosurgery (SRS), 15 received Gamma Knife SRS and the remaining 22 received linear accelerator (LINAC) SRS. Multi-fraction SRS was performed in 28 patients (20.6%); one patient received three fractions and the other 27 received five fractions. In total, 70 patients (51.5%) received WBRT and 65 (47.8%) received SRS. The most common primary tumor sites were lung (57 patients; 41.9%), breast (24 patients; 17.6%), and melanoma (19 patients; 14.0%).
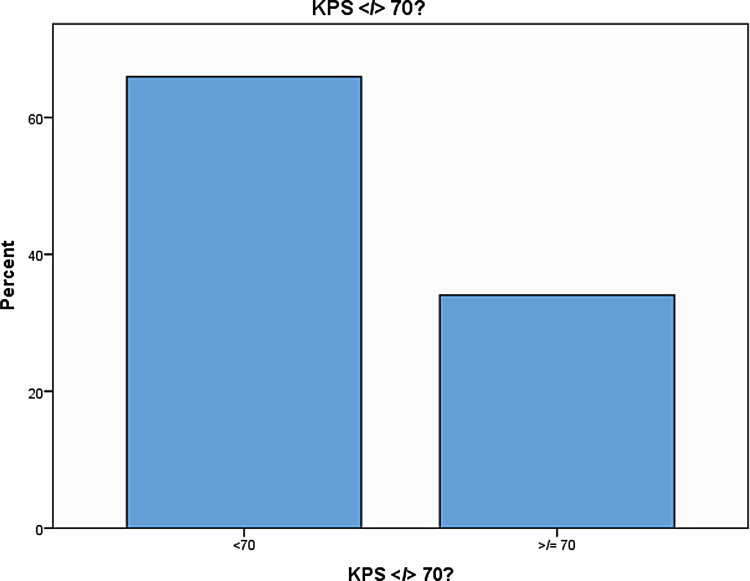
Forty-two patients (30.9%) died within 30 days of palliative RT. Of these, 31 (73.8%) received at least 10 fractions. Patients with baseline KPS <70 (odds ratio = 2.2; 95% confidence interval = 1.6–3.1; p < 0.0001) were significantly more likely to die within 30 days of treatment (Fig. 1). No other patient demographics were significantly associated with 30-day mortality post-RT. 64% of patients suffered extracranial metastatic disease at the time of palliative RT.
Fig. 1.
Depiction of the impact of pre-treatment Karnofsky Performance Status (KPS) on the proportion of patients with 30-day mortality following palliative intracranial radiation therapy. KPS <70 was significantly associated with increased 30-day mortality.
4. Discussion
Although the importance of functional independence (KPS >70) in metastatic brain disease has been well understood with regard to overall survival, the delineation of 30-day mortality in metastatic brain disease following radiation therapy has been examined in only one previous study.7,8 It has been well-established that the natural history of metastatic brain disease without treatment yields survival of one month, and that treatment with steroids alone adds an additional month of survival.3,9
Our findings indicate a high rate of 30-day mortality among patients undergoing palliative RT for brain metastases, and that KPS <70 independently predicts which patients are most likely to suffer 30-day mortality following palliative intracranial RT. The distribution of treatment between WBRT and SRS (and within SRS, between Gamma Knife and LINAC) indicates that our findings reflect treatment options consistent with the complete RT armamentarium for brain metastases currently available, as opposed to the limited armamentarium (paucity/absence of SRS) prevalent in many centers during the late 20th century when the majority of the Level I evidence palliative intracranial RT studies were conducted.5,6,8
The fact that nearly 1/3 of palliative intracranial RT patients do not live longer than one month after treatment should be a cause for sober reflection. Particularly when this work has demonstrated KPS as a useful tool for selecting which patients are most likely to suffer 30-day mortality post-RT, any patient with KPS < 70 with metastatic brain disease referred for RT should be strongly considered for hypofractionated regimens over regimens involving 10 or more fractions, as these longer regimens have failed to demonstrate a survival advantage in the WBRT literature over shorter regimens.5,6 It is also possible that many of these patients may not benefit from RT at all. For patients with increased 30-day mortality following palliative RT, any reduction of treatment time may manifest as a significant improvement in the quality of their remaining lifespan and should be heavily factored in RT management decision-making.
Limitations of this study include its retrospective nature and single-institution source of data, as well as the relatively small sample size (n = 136) compared with that across the three RTOG trials conducted between 1979 and 1993 (n = 1200).8 Furthermore, many centers may not have our institution’s access to the volume and range of SRS options; this may result in a proportion of WBRT among palliative intracranial RT cases being much higher than the 51% reported in our series. Another limitation is that given the relatively aggressive nature of our institution in using SRS for patients with up to 10 brain metastases, our WBRT population is likely enriched by patients who are going to have the worst outcomes. Finally, details regarding the number of brain metastases were absent, potentially limiting the applicability of our findings.
In conclusion, our findings indicate that baseline KPS <70 is independently predictive of death within 30 days of palliative intracranial RT. A large majority of patients suffering 30-day mortality received at least 10 fractions in our series, suggesting patient selection for full course versus hypofractionated RT should be improved, particularly for patients lacking functional independence.
Author contribution
Study concept and design: McClelland.
Acquisition, analysis, or interpretation of data: McClelland, Agrawal, Elbanna, Shiue, Bartlett, Lautenschlaeger, Watson, Ellsworth.
Drafting of the manuscript: McClelland.
Critical revision of the manuscript for important intellectual content: McClelland, Agrawal, Shiue, Bartlett, Lautenschlaeger, Zellars, Watson, Ellsworth.
Statistical analysis: Ellsworth.
Administrative, technical, or material support: McClelland, Agrawal, Shiue, Watson, Ellsworth.
Study supervision: Ellsworth, Watson, Zellars.
Conflict of interest
None declared.
Financial disclosure
None declared.
References
- 1.Pruitt A.A. Epidemiology, treatment, and complications of central nervous system metastases. Continuum (Minneap Minn) 2017;23:1580–1600. doi: 10.1212/CON.0000000000000551. [DOI] [PubMed] [Google Scholar]
- 2.Khuntia D., Brown P., Li J. Whole-brain radiotherapy in the management of brain metastasis. J Clin Oncol. 2006;24:1295–1304. doi: 10.1200/JCO.2005.04.6185. [DOI] [PubMed] [Google Scholar]
- 3.Sejpal S.V., Bhate A., Small W. Palliative radiation therapy in the management of brain metastases, spinal cord compression, and bone metastases. Semin Intervent Radiol. 2007;24:363–374. doi: 10.1055/s-2007-992324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chao J.H., Phillips R., Nickson J.J. Roengten-ray therapy of cerebral metastases. Cancer. 1954;7:682–689. doi: 10.1002/1097-0142(195407)7:4<682::aid-cncr2820070409>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 5.Borgelt B., Gelber R., Kramer S. The palliation of brain metastases: final results of the first two studies by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys. 1980;6:1–9. doi: 10.1016/0360-3016(80)90195-9. [DOI] [PubMed] [Google Scholar]
- 6.Borgelt B., Gelber R., Larson M. Ultra-rapid high dose irradiation schedules for the palliation of brain metastases: final results of the first two studies by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys. 1981;7:1633–1638. doi: 10.1016/0360-3016(81)90184-x. [DOI] [PubMed] [Google Scholar]
- 7.McClelland S., 3rd, Agrawal N., Shiue K. Nearly half of metastatic brain disease patients prescribed ten fractions of whole brain radiation therapy die without completing treatment. J Pain Symptom Manage. 2019 doi: 10.1016/j.jpainsymman.2019.04.022. Apr 25. pii: S0885-3924(19)30227-1. [DOI] [PubMed] [Google Scholar]
- 8.Gaspar L., Scott C., Rotman M. Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys. 1997;37:745–751. doi: 10.1016/s0360-3016(96)00619-0. [DOI] [PubMed] [Google Scholar]
- 9.Narayana A., Liebel S.A. Textbook of radiation oncology. In: Liebel S.A., Phillips T.L., editors. Primary and metastatic brain tumors. Elsevier; Philadelphia: 2004. pp. 463–495. [Google Scholar]