Highlights
-
•
Superior vena cava filter is safe and feasible.
-
•
Superior vena cava filter is rare.
-
•
We report a case of a superior vena cava filter through jugular access.
Keywords: superior vena cava filters, Upper extremity deep vein thrombosis, Vena cava filters
Abstract
Introduction
Venous thromboembolism is an important cause of morbidity and mortality in the world. Upper Extremity Deep Venous Thrombosis (UEDVT) may be a cause of pulmonary embolism. Anticoagulation is the treatment of choice for venous thromboembolism, which is associated with low hemorrhagic complications. However, there are situations that anticoagulation becomes contraindicated as gastrointestinal tract hemorrhages, stroke, progression of deep venous thrombosis in the presence of adequate anticoagulation, where the vena cava filter is recommended.
Case report
Patient 65 years old, female undergoing neurosurgical treatment of a mass suggestive of schwannoma with asymmetrical edema in the right upper limb, confirming the acute deep venous thrombosis by Doppler ultrassonogarphy. Anticoagulation was contraindicated by neurosurgery and after a multidisciplinary discussion, the superior vena cava filter was chosen.
Discussion
The Retrievable Celect™ Filter was implant in superior vena cava and may be considered as an alternative therapeutic method in cases where anticoagulation can not be performed.
Conclusion
Superior vena cava filter is controversial, but is safe, feasible and effective, in preventing symptomatic pulmonary embolisms in patients in whom anticoagulation is contraindicated.
1. Introduction
Pulmonary embolism (PE) is a fatal complication of venous thromboembolism that can be challenging to diagnose and manage [1]. The incidence of upper extremity deep venous thrombosis (UEDVT) ranges from 2 % to 4 % and the prevalence of venous thrombosis in this vascular segment has increased due to catheter implants in the deep venous system [2,3]. Oral or parenteral anticoagulation is the treatment of choice for pulmonary embolism in 4–28 % of patients [4].
The inferior vena cava filter is well established for prevention of pulmonary embolism in patients with deep venous thrombosis of the lower limbs with contraindication to anticoagulation only, based on the PREPIC trials [1,4]. In contrast, the placement of vena cava filters in the superior vena cava (SVC) to prevent PE from UEDVT is controversial, but can be an alternative, safe, feasible and effective, in preventing symptomatic pulmonary embolisms in patients in whom anticoagulation or thrombolysis has failed or is contraindicated [[5], [6], [7], [8]]. Filter placement in the SVC is technically more difficult than in the IVC because of the relatively small area for filter insertion and displacement. In this article, we present a case of SVC filter using the Celect™ Platinum Vena Cava Filter (Cook Medical, Bloomington, Indiana, US) in patients with UEDVT [9]. Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request
2. Case report
Patient 65 years old, female, with arterial hypertension, diabetes and submmited to renal transplantation 2 years ago sought medical assistance for the first time at the emergency room with complaints of mild headache, diplopia, dizziness and difficulty in walking. Brain scan was performed and an expansive lesion was observed in the right posterior fossa suggestive of Schwannoma. After initial evaluation, the patient was discharged from hospital with elective hospitalization schedule for surgical intervention.
The patient returned to the hospital 6 days later with urinary septic shock, generalized clonic tonic seizures and decreased level of consciousness. Computed tomography (CT) was performed with images of midline deviation, hydrocephalus and presence of expansive lesion in the right posterior fossa, causing intracranial hypertension. Due to its severity, we opted for decompressive craniectomy, resection of the lesion and external ventricular shunt. Fragment of the lesion was referred to pathological anatomy, confirming the diagnosis of diffuse large B-cell lymphoma. After surgical procedure patient maintains a reserved neurological condition, with orotracheal intubation, without sedation, but maintaining reflexes and respiratory drive. During recovery in the intensive care unit physical examination showed asymmetrical edema in the right upper limb, raising the hypothesis of deep vein thrombosis. Doppler ultrasonography of the right upper limb showed subclavian, axillary, subclavian and brachial veins non-compressible,dilated with intra-luminal echogenic material and no color flow, confirming the hypothesis of acute deep venous thrombosis in the upper limb. Subcutaneous enoxaparin at a dose of 1 mg / kg 12 / 12 h was started. After the next day of external ventricular bypass the cerebrospinal fluid drainage ceased. To try to unclog the ventricular shunt catheter, it was infused by the Actilyse® 3 mg catheter itself by the catheter itself. The patient was taken for multidisciplinary discussion regarding the indication of superior vena cava filter placement and informed consent was obtained. The vena cava filter is considered recoverable filter and family members are reported to be an off label procedure. The work was reported according to the Consensus Surgical CAse REport (SCARE) Guidelines, International Journal of Surgery 2018.
3. Technique
A Celect™ Platinum Vena Cava Filter (Cook Medical, Bloomington, Indiana, US) set was placed via the internal jugular vein approach to achieve correct orientation for deployment with the apex of the filter toward the right atrium and the base oriented toward and in line with the right internal jugular vein, using femoral kit via jugular access.The base of the filter was placed just below the brachiocephalic veins. The diameter of the superior vena cava was 22 mm in diameter and was within the manufacturer's recommendations. These procedures were conducted with the aid of phlebography through the introducer located the right internal jugular vein before and after insertion (Fig. 1, Fig. 2 ). On the basis of phlebography, the superior vena cava filter placement was successfully performed without complications (Fig. 2).
Fig. 1.
Phlebography before implantation of SVC filter. Yellow arrow, right brachiocephalic vein; blue arrow, left brachiocephalic vein; red arrow, cava superior vein.
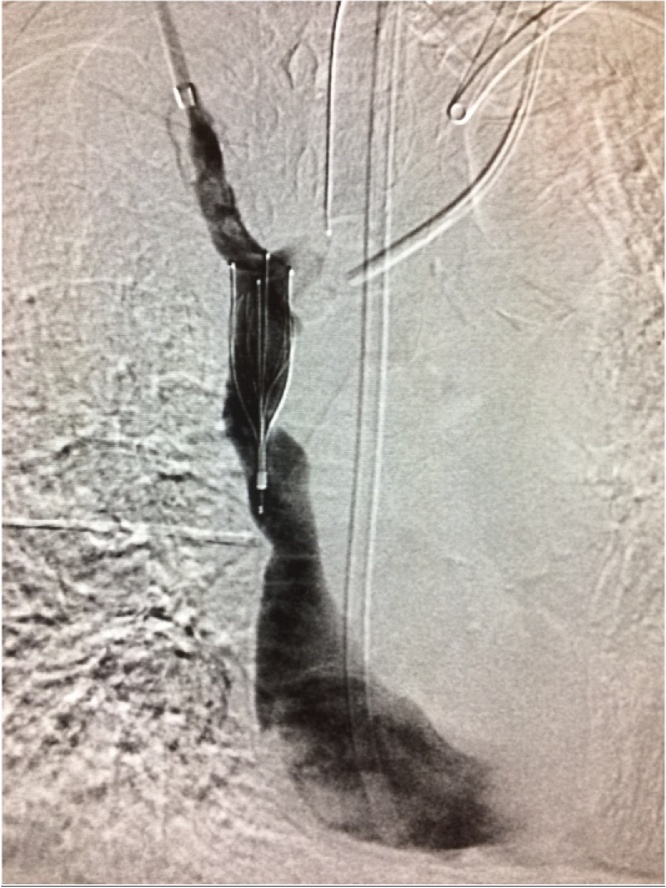
Fig. 2.
Control for SVC filter placement (inverted position).
The Celect™Platinum Vena Cava Filter (Cook Medical, Bloomington, Indiana, US) to be released into the superior vena cava by femoral access should first be released on the table, followed by reconnecting the filter to the delivery device. When the filter is released by jugular access the device is ready to be triggered. The right jugular access was guided by ultrasound and we can confirm that there was no thrombus at the site. Similarly, we can confirm with ultrasound that the left jugular vein was also patent.
Clinical status, mainly respiratory and cardiac status, worsened progressively, preventing any further interventional procedures. The patient suffered persistent hypoxemia and bradycardia throughout his time in hospital and died 15 days after the filter had been placed.
4. Discussion
There are data literature on the use, effectiveness and safety of SVC filters in patients with upper extremity deep venous thrombosis [7,13]. Indications for SVC filter placement are failure or contraindication to therapeutic anticoagulation or for presurgical prophylaxis.
SVC filter placement should begin with superior vena cavograms to exclude underlying venous stenosis, patency, diameter and length of the superior vena cava before filter deployment and no filter be deployed within an SVC with a diameter greater than 28 mm [10].
Ideal filter placement and positioning has been described with the filter hooks within the SVC at the confluence of the right and left brachiocephalic veins with the apex of the filter directed toward the right atrium. Placement in this location helps preventing the azygous vein from associated thromboembolic complications [10,6]. In addition, if possible, non-permanent filters, for exemple, temporary, convertible and retrievable, should be deployed in order to avoid associated complications of permanent filters as was used in our case a retrievable filter, Celect™ Platinum Vena Cava Filter (Cook Medical, Bloomington, Indiana, US). Owens et al., showed in a review of the literature that 67.5 % of patients that received a SVC filter died within 1 year after placement and that 64 % of these deaths occurred while still in hospital or within 1 month of filter placement [5,11].
It is not known is the true incidence of symptomatic and fatal PE originating from an upper-extremity source. Besides of,there is little debate that an upper extremity thrombus can embolize to the pulmonary artery and, if large enough, cause significant morbidity and/or mortality. In the study by Monreal et al., three of their five patients with UEDVT and PE were asymptomatic [12]. There are two major serie, Spence et al. who describe 41 patients and Usoh et al. 154 patients, both reported that of SVC filter placements is safe and effective with minimum complications. It is not possible to make a reasonable statement regarding the superiority of one filter versus another when comparing efficiency and/or safety [6,7].
Complications of SVC filter placement are rare, but potentially more severe compared with IVC filter placement. These complications included SVC perforation, cardiac tamponade, aortic perforation, SVC thrombosis, dislodgement and pneumothorax. In the case of strut perforation, there is little to no structure in the mediastinum equivalent to the retroperitoneal cavity to provide any barrier to protect surrounding organs. Whereas strut perforation in the IVC occurs often without consequence, perforation through the wall of the SVC may result in injury to the lung, aorta, pulmonar artery, heart, or pericardium [5].
5. Conclusion
In patients with a long life expectancy who are high risk for PE with contraindications to anticoagulation, placement of a retrievable SVC filter is an option. The filter should be easy to insert and retrieve. SVC filter placement is associated with a low incidence of complications with long-term follow-up. These data help to reaffirm the safety and effectiveness of SVC filter placement.
Declaration of Competing Interest
The author declare no conflict of interest in preparing this article.
Sources of funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical approval
Case reports are not required to be approved by the institution's ethics committee.
Consent
The document is attached.
Author contribution
TÚLIO FABIANO DE OLIVEIRA LEITE is a Vascular Surgeon from Faculdade Medicina de Botucatu (UNESP), Interventional Radiologist and Endovascular Surgeon from Universidade de São Paulo (USP). Research Member of the Research Group on Medical Sciences and Vascular Pathophysiology at Universidade Federal Fluminense (UFF / CAPES / CNPQ).
The study was carried out at the University of São Paulo.
-
1)
Conception and design of the study: TFOL
-
2)
Analysis and interpretation of data: TFOL
-
3)
Data collection: TFOL
-
4)
Writing of the article: TFOL
-
5)
Critical revision of the text: TFOL
-
6)
Final approval of the article *: TFOL
-
7)
Statistical analysis: TFOL
-
8)
General responsibility for the study: TFOL
-
9)
Financing information: There was no financing.
Registration of research studies
Not applicable.
Guarantor
Túlio Fabiano de Oliveira Leite.
Acknowledgement
None.
Biographies
Tulio Fabiano De Oliveira Leite é Cirurgião Vascular pela Faculdade Medicina de Botucatu (UNESP), Radiologista Intervencionista e Cirurgião Endovascular pela Universidade de São Paulo (USP). Membro Pesquisador do Grupo de Pesquisas em Ciências Médicas e Fisiopatologia Vascular na Universidade Federal Fluminense (UFF/CAPES/CNPQ).
Thiago Oliveira E. Silva é Cirurgião Vascular pela Faculdade Medicina do ABC, Radiologista Intervencionista e Cirurgião Endovascular pela Universidade de São Paulo (USP).
Osvaldo Ignacio Pereira é Doutor pela Universidade de São Paulo. Professor Assistente do Departamento de Radiologia Intervencionista e Cirurgia Endovascular da Universidade de São Paulo (FMUSP).
Francisco Cesar Carnevale é Doutor e Professor Livre Docente pela Universidade de São Paulo. Chefe do Serviço de Radiologia Intervencionista e Cirurgia Endovascular da Universidade de São Paulo (FMSUP).
Footnotes
O estudo foi realizado na Universidade de São Paulo.
Contributor Information
Tulio Fabiano De Oliveira Leite, Email: tuliofabiano@hotmail.com.
Thiago Oliveira E. Silva, Email: thiago_o_s@hotmail.com.
Osvaldo Ignacio Pereira, Email: oipereira@uol.com.br.
References
- 1.Giordano N.J., Jansson P.S., Young M.N., Hagan K.A., Kabrhel C. Epidemiology, pathophysiology, stratification, and natural history of pulmonary embolism. Tech. Vasc. Interv. Radiol. 2017;20(Sep. (3)):135–140. doi: 10.1053/j.tvir.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 2.Prandoni P., Bernardi E. Upper extremity deep vein thrombosis. Curr. Opin. Pulm. Med. 1999;5:222–226. doi: 10.1097/00063198-199907000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Saber W., Moua T., Williams E.C., Verso M., Agnelli G., Couban S., Young A., De Cicco M., Biffi R., Van Rooden C.J., Huisman M.V. Risk factors for catheter‐related thrombosis (CRT) in cancer patients: a patient‐level data (IPD) meta‐analysis of clinical trials and prospective studies. J. Thromb. Haemost. 2011;9(Feb. (2)):312–319. doi: 10.1111/j.1538-7836.2010.04126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hingorani A., Ascher E., Lorenson E., DePippo P., Salles-Cunha S., Scheinman M., Yorkovich W., Hanson J. Upper extremity deep venous thrombosis and its impact on morbidity and mortality rates in a hospital-based population. J. Vasc. Surg. 1997;26(Nov. (5)):853–860. doi: 10.1016/s0741-5214(97)70100-9. [DOI] [PubMed] [Google Scholar]
- 5.Owens C.A., Bui J.T., Knuttinen M.G., Gaba R.C., Carrillo T.C. Pulmonary embolism from upper extremity deep vein thrombosis and the role of superior vena cava filters: a review of the literature. J. Vasc. Interv. Radiol. 2010;21(Jun. (6)):779–787. doi: 10.1016/j.jvir.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 6.Spence L.D., Gironta M.G., Malde H.M., Mickolick C.T., Geisinger M.A., Dolmatch B.L. Acute upper extremity deep venous thrombosis: safety and effectiveness of superior vena caval filters. Radiology. 1999;210(Jan. (1)):53–58. doi: 10.1148/radiology.210.1.r99ja1353. [DOI] [PubMed] [Google Scholar]
- 7.Usoh F., Hingorani A., Ascher E., Shiferson A., Tran V., Marks N., Jacob T. Long-term follow-up for superior vena cava filter placement. Ann. Vasc. Surg. 2009;23(Jun. (3)):350–354. doi: 10.1016/j.avsg.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 8.Murphy K.D. Superior vena cava fi lters. Tech. Vasc. Interv. Radiol. 2004;7:105–109. doi: 10.1053/j.tvir.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A.J., Orgill D.P., Zhu H., Alsawadi A., Noureldin A., Rao A., Enam A. The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60(December):132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 10.Pais S.O., De Orchis D.F., Mirvis S.E. Superior vena caval placement of a Kimray-Greenfield filter. Radiology. 1987;165(Nov. (2)):385–386. doi: 10.1148/radiology.165.2.3659362. [DOI] [PubMed] [Google Scholar]
- 11.Bertanha M., Sobreira M.L., Moura R., Jaldin R.G., Mariuba J.V., Pinheiro Filho C.E., Rollo H.A., Yoshida W.B. Simultaneous placement of filters in inferior vena cava and superior vena cava. J. Vasc. Bras. 2013;12(Sep. (3)):226–229. [Google Scholar]
- 12.Monreal M., Raventos A., Lerma R. Pulmonary embolism in patients with upper extremity DVT associated to venous central lines: a prospective study. Thromb. Haemost. 1994;72:548–550. [PubMed] [Google Scholar]
- 13.Mir M.A. Superior vena cava filters: hindsight, insight and foresight. J. Thromb. Thrombolysis. 2008;26(Dec. (3)):257–261. doi: 10.1007/s11239-007-0186-6. [DOI] [PubMed] [Google Scholar]