Abstract
Food-dependent exercise-induced anaphylaxis (FDEIA) is a life-threatening but relatively rare disorder which occurs mainly in older children and young adults and manifests with symptoms of anaphylaxis upon exercise following ingestion of certain kinds of food. We herewith report 3 cases of soybean-induced FDEIA. We also highlight 2 types of soybean-induced FDEIA, one caused by storage protein components Gly m 5 and Gly m 6 and the other caused by pollen-related allergen components.
Keywords: FDEIA, Soybean, Component, Gly m 5, Gly m 6
Abbreviations: FDEIA, food-dependent exercise induced anaphylaxis; SAR, seasonal allergic rhinitis; JCP, Japanese cedar pollen; DAB, Diamino Benzidine; SDS-PAGE, Sodium Dodecyl Sulfate Poly-Acrylamide Gel Electrophoresis; SPT, Skin Prick Test; PTP, Prick to Prick test; ISU, ISAC Standardized Units; Gly m 4, Glycine max 4; Gly m 5, Glycine max 5; Gly m 6, Glycine max 6; Ara h 1, Arachis hypogaea 1; Ara h 2, Arachis hypogaea 2; Ara h 3, Arachis hypogaea 3; Jug r 1, Juglans regia 1
To the Editor:
Food-dependent exercise-induced anaphylaxis (FDEIA) is a life-threatening but relatively rare (estimated prevalence of 0.02%) disorder which occurs mainly in older children and young adults and manifests with symptoms of anaphylaxis upon exercise following ingestion of certain kinds of food.1,2 The most common foods implicated as a cause of FDEIA are wheat worldwide and crustaceans in the far east.2 We herewith present 3 cases of FDEIA due to tofu in children. Furthermore, we identified the causative allergen components in these patients. Details of these cases and investigational data are as shown in Table1.
Table 1.
Characteristics and investigational results of the 3 cases.
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Symptom onset (age) | 9 years | 10 years | 13 years |
| Gender | Male | Male | Female |
| Causative food | Tofu | Tofu | Tofu |
| Type of exercise | Running | Running | Running |
| Symptoms | Cough, itch, flush | Urticaria, nasal blockage, pallor, loss of activity | Skin rash, swelling of eyelids, wheeze |
| Co-morbid allergies | FA (Peanut), SAR | FA (Peanut, walnut) | SAR |
| Skin Prick Test | Not performed | Positive | Positive |
| OFC | Not performed | Positive | Positive |
| Immunoblotting | Positive | Positive | Not performed |
| Specific IgE to soybean, soybean components | 12.60 UA/ml, | 11.90 UA/ml | 0.64 UA/ml |
| Gly m 4 | 0.835 UA/ml | 3.3 (ISU) | 4.43 UA/ml |
| Gly m 5 | 4.37 UA/ml, | 0.3 (ISU) | <0.100 UA/ml |
| Gly m 6 | 17.6 UA/ml | 7.1 (ISU) | 0.133UA/ml |
FA: Food Allergy; SAR: Seasonal Allergic Rhinitis; OFC: Oral Food Challenge.
ISU: ISAC Standardized Units; Gly m 4: Glycine max 4; Gly m 5: Glycine max 5.
Gly m 6: Glycine max 6
Written informed consent was obtained from the parents of all 3 children.
Case 1
A 9-year-old boy presented with a history of symptoms of cough, itch, and flush upon exercise soon after eating his school lunch including tofu and other soybean products. He was severely allergic to peanuts with a history of dyspnea after ingestion of peanuts. There was no history of anaphylaxis to soybean until this episode. He also suffered from seasonal allergic rhinitis (SAR) to Japanese cedar pollen (JCP) and atopic dermatitis.
The specific IgE to soybean and peanuts measured by Immuno CAP (Thermo Fisher Scientific) were 12.60 and ≥ 100 UA/ml, respectively. Specific IgE to soybean component Glycine max 4, 5, 6 (Gly m 4, 5, 6) were 0.835, 4.37, and 17.6 UA/ml, respectively. Specific IgE to Arachis hypogaea 2 (Ara h 2) was 57.73 UA/ml, respectively, showing strong sensitization to peanut storage proteins.
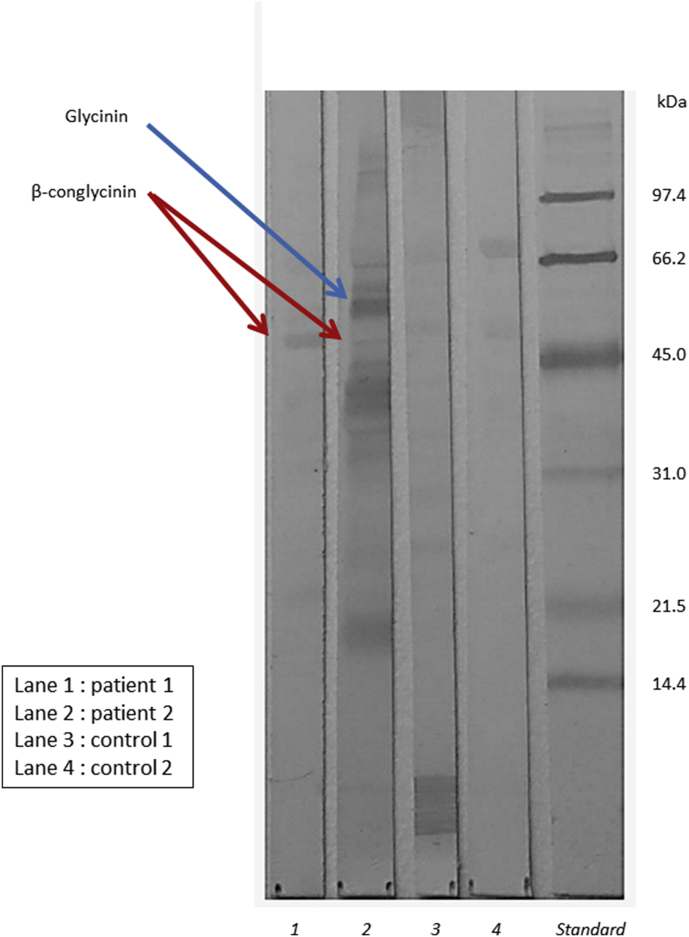
Immunoblotting for soybean was performed. The extract from soy flour (Kodama Health Foods) was subjected to SDS-PAGE on a 12% gel (Bio-Rad) and immunoblot analysis was performed using the patient's serum. The reaction was developed with Diamino benzidine (DAB). A positive band was detected between 50 and 70 kDa indicating the presence of specific IgE against storage proteins Gly m 5 (Fig. 1).
Fig. 1.
Immunoblot analysis of patients' serum and reaction to soybean protein. Diamino Benzidine staining of the soy flour extracts and immunoblotting using the patients' sera (Lane 1 and 2) and normal subjects' sera (Lane 3 and 4) (80 × dilution). Molecular weight markers were used as size standards. The patient's sera from Case 1 reacted to β-conglycinin (Gly m 5) (50–70kDa) (red arrow). The patient's sera from Case 2 reacted to both β-conglycinin (Gly m 5) and glycinin (Gly m 6) (50–60kDa) (blue arrow)
Case 2
A 10-year-old boy with food allergy to peanuts and walnuts manifested with symptoms of anaphylaxis including cough, nasal obstruction, and generalized urticaria followed by sudden feeling of weakness and cyanosis while running during his physical exercise class 30 min post lunch at school. The contents of his school lunch included fried tofu (soybean), rice, mandarin, and green vegetables. There was no history of an allergic reaction to tofu/soy products in the absence of exercise.
Skin prick test (SPT) using a commercial soybean extract (Torii Pharmaceuticals) was positive. Prick-to-prick (PTP) test for soybean products (tofu, fried tofu and soy milk) were also positive, but PTP to fermented soybean products and other foods eaten at lunch were negative. Specific IgE to soybean (Immuno CAP) was 11.90 UA/ml. Specific IgE to soybean and peanuts components were measured by ISAC (Thermo Fisher Scientific). Specific IgE (ISAC) to soybean allergen components Gly m 4, Gly m 5 and Gly m 6 were 3.3, 0.3, and 7.1 ISU, respectively. Specific IgE to peanut and walnut allergen components (storage proteins) Ara h 1, 2, 3 and Jug r 1 were 28.4, 39.9, 17.9 and 15.7 ISU, respectively.
Provocation tests to soybean were also performed. After ingestion of 100 gms of tofu, he underwent a treadmill ergometric stress test (Bruce protocol) 30 min later, which was negative. Provocation test was repeated the following day 30 min after taking 330 mg (10mg/kg) of aspirin and 100 gms of tofu according to the Japanese Guidelines of Oral Food Challenge 2009. Ten minutes after initiating the exercise, the patient manifested with symptoms of cough and wheeze indicating a positive provocation test. The immunoblot analysis using the patient's serum showed positive bands to storage protein β-conglycinin and Glycinin (Fig. 1), indicating sensitization to Gly m 5 and Gly m 6.
Case 3
A 13-year-old girl with SAR to JCP, mugwort, ragweed, and birch pollen had several episodes of urticaria and dyspnea when exercising shortly after lunch at school for the prior 3 years before visiting our clinic. Tofu was the common food item in the school lunch at all episodes.
SPT was positive only to soy milk and negative to soy extract and tofu. Specific IgE to crude soy extract and soybean allergen components Gly m 4, Gly m 5, and Gly m 6 were 0.64, 4.43, <0.100, and 0.133 UA/ml, respectively. She also had SAR to birch pollen. Specific IgE to JCP, mugwort, ragweed and birch were 2.89, 1.70, 3.33, and 14.10 UA/ml, respectively.
Provocation test done as described above after ingestion of 100 gms of tofu resulted in manifestation of skin rash and rhinorrhea 12 min after initiating the exercise, indicating a positive provocation test.
Soybean (Glycine max) contains various proteins. To date, at least 33 IgE-binding allergens are known and 8 are registered in the IUIS (International Union of Immunological Societies Allergen Nomenclature Sub-Committee).3, 4, 5 Sensitization to soy storage proteins indicates a high risk of having severe allergic reactions, according to Holzhauser et al.6 Nevertheless, in those places where birch pollinosis is common, Gly m 4 is known to cause severe symptoms in patients with birch pollinosis.7 Fukutomi et al reported that Japanese adult patients with soybean allergy had high levels of specific IgE to Gly m 4, alder, and birch pollens.8
Many patients with soybean allergy who are sensitized to Gly m 5 and Gly m 6 are reported to have peanut allergy.6,7 Here we present 3 cases of soybean related FDEIA. The FDEIA patient Case 1 had soybean and peanut allergy, and was sensitized to Gly m 4, Gly m 5 and Gly m 6. Case 2 had soybean, peanut, and walnut allergy and was sensitized to Gly m 5 and Gly m 6. Storage proteins are considered to be the cause of FDEIA. In contrast, in Case 3 who had SAR to birch pollen, the symptoms of FDEIA was thought to be caused by Bet v 1- related soybean protein, Gly m 4. Case 3 was thought to have been caused by a distinct protein type other than storage protein, namely PR-10. Case 3 had a positive SPT with soy milk but was negative to tofu. This difference in SPT result could probably be due to the fact that soy milk contains a higher amount of soy allergens including Gly m 4 as compared to tofu.
Food allergy to soybean products has been increasingly reported worldwide including several soybean products such as soybean sprouts, soy flour, or soy milk.7 Taramarcaz reported a case of FDEIA induced by a drink containing soybean protein.9 Adachi et al reported a case of FDEIA caused by tofu and analyzed the soybean allergens by pepsin digestion.10 They demonstrated that tofu, although not heated but gelatinized, contained more β-conglycinin (Gly m 5) as compared to soy milk and green soybean. Ito et al reported that the specific IgE to Gly m 5 and Gly m 6 were higher in children manifesting allergic symptoms to soybean than asymptomatic sensitized children.11
Food allergy is an increasing global health problem in both the developed and developing world.12,13 In many Asian countries as in Japan, soybean is commonly consumed daily in large quantities and is also a major cause of food allergies.11 FDEIA is mainly caused by foods, such as wheat and crustaceans. As reported here, more recently soybean is also a cause of FDEIA. We herewith conclude that there are 2 distinct types of soybean-induced FDEIA, one type related to storage proteins like Gly m 5 and 6 and the other type that is pollen associated FDEIA related to PR-10 like Gly m 4.
What we can learn from these three cases is important because it gives us new information on the disease pattern. When a patient experiences allergic symptoms after eating several kinds of foods combined with exercise, identification of the culprit food is crucial as soon as possible in order to avoid future episodes. If the meal contains soy products and the patient has a known peanut allergy, the clinician can assume the cause of the FDEIA to be the storage protein of soy. Likewise, one can consider the causative allergen as soy PR-10 when the patient does not have peanut allergy but has co-morbid seasonal allergic rhinitis to birch pollen. Although other confounding factors may also play a role, this difference in the components such as storage proteins versus labile proteins (such as PR-10) may suggest a difference in the risk of anaphylaxis.
Funding
Research funding for this work was received from the Pediatric Alumni Association of Nippon Medical School.
Availability of data and materials
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
Author contributions
Miyuki Hayashi and Ruby Pawankar contributed to the conceptualization and conduction of the study. Shingo Yamanishi and Yasuhiko Itoh have been involved in revising the manuscript.
Ethical approval
According to our hospital Institutional Review Board (IRB) which follows the Japanese National Clinical Guidelines IRB and ethical approval is not needed for case studies. Therefore, it is not subject to ethical approval.
Informed consent was obtained from legal parents of patients for reporting individual patient data and publishing this article.
Consent for publication
The authors read and approved the final version of the manuscript for publication.
Declaration of Competing interest
The authors declare that all the authors have no relevant conflicts of interest in relation to this work.
Acknowledgements
None.
Footnotes
Full list of author information is available at the end of the article.
References
- 1.Maulitz R.M., Pratt D.S., Schocket A.L. Exercise-induced anaphylactic reaction to shellfish. J Allergy Clin Immunol. 1979;63:433–434. doi: 10.1016/0091-6749(79)90218-5. [DOI] [PubMed] [Google Scholar]
- 2.Izadi N., Rabinovitch N. Food-dependent exercise-induced anaphylaxis to soybean. J Allergy Clin Immunol Pract. 2019;7:303–304. doi: 10.1016/j.jaip.2018.04.044. [DOI] [PubMed] [Google Scholar]
- 3.ALLERGOME. The Platform for Allergen Knowledge. http://www.allergome.org. Accessed 18 Jan 2020.
- 4.ALLERGEN NOMENCLATURE. WHO/IUIS Allergen Nomenclature Sub-committee. http://www.allergen.org. Accessed 18 Jan 2020.
- 5.Pomes A., Davies J.M., Gadermaier G. WHO/IUIS allergen nomenclature: providing a common language. Mol Immunol. 2018;100:3–13. doi: 10.1016/j.molimm.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holzhauser T., Wackermann O., Ballmer-Weber B.K. Soybean (Glycine max) allergy in Europe: Gly m 5 (beta-conglycinin) and Gly m 6 (glycinin) are potential diagnostic markers for severe allergic reactions to soy. J Allergy Clin Immunol. 2009;123:452–458. doi: 10.1016/j.jaci.2008.09.034. [DOI] [PubMed] [Google Scholar]
- 7.Ballmer-Weber B.K., Holzhauser T., Scibilia J. Clinical characteristics of soybean allergy in Europe: a double-blind, placebo-controlled food challenge study. J Allergy Clin Immunol. 2007;119:1489–1496. doi: 10.1016/j.jaci.2007.01.049. [DOI] [PubMed] [Google Scholar]
- 8.Fukutomi Y., Sjölander S., Nakazawa T. Clinical relevance of IgE to recombinant Gly m 4 in the diagnosis of adult soybean allergy. J Allergy Clin Immunol. 2012;129:860–863. doi: 10.1016/j.jaci.2012.01.031. e3. [DOI] [PubMed] [Google Scholar]
- 9.Taramarcaz P., Hauser C., Eigenmann P.A. Soy anaphylaxis. Allergy. 2001;56:792. doi: 10.1034/j.1398-9995.2001.00211.x. [DOI] [PubMed] [Google Scholar]
- 10.Adachi A., Horikawa T., Shimizu H. Soybean beta-conglycinin as the main allergen in a patient with food-dependent exercise-induced anaphylaxis by tofu: food processing alters pepsin resistance. Clin Exp Allergy. 2009;39:167–173. doi: 10.1111/j.1365-2222.2008.03148.x. [DOI] [PubMed] [Google Scholar]
- 11.Ito K., Sjölander S., Sato S. IgE to Gly m 5 and Gly m 6 is associated with severe allergic reactions to soybean in Japanese children. J Allergy Clin Immunol. 2011;128:673–675. doi: 10.1016/j.jaci.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 12.Prescott S.L., Pawankar R., Allen K.J. A global survey of changing patterns of food allergy burden in children. World Allergy Organ J. 2013 Dec 4;6(1):21. doi: 10.1186/1939-4551-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hossny E., Ebisawa M., El-Gamal Y. Challenges of managing food allergy in the developing world. World Allergy Organ J. 2019 Dec 2;12(11):100089. doi: 10.1016/j.waojou.2019.100089. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.