On March 11, 2020, the World Health Organization declared the novel coronavirus disease 2019 (COVID-19) to be a global pandemic with millions affected and hundreds of thousands of deaths.1 , 2 Numerous restrictions have been enacted to mitigate disease transmission and ensure that the health care system has the ability to effectively respond to increased patient volume and acuity.3 In part, this has included the cancellation of many elective ambulatory clinic visits with the implementation of telehealth modalities in their place.4 To further encourage the use of telehealth, the Centers for Medicare and Medicaid Services increased payments for these encounters and permitted the use of audio-only technology.5
Telehealth, here used interchangeably with the term telemedicine, has been defined as the use of telecommunication modalities, such as telephone and real-time video, to connect patients with clinicians for the purpose of providing health care.6 Patients and providers alike have reported high levels of satisfaction with telehealth encounters as a result of its convenience and lower cost, and view the quality of care as comparable with traditional office visits.7, 8, 9, 10 Among the benefits of telehealth are improved outcomes, increased efficiency, and ease of use.11 , 12
Telehealth also may increase access to care by decreasing travel time and cost, limiting missed work days, and reducing the need to find alternative caregivers, especially among rural communities.8 , 11, 12, 13 During disasters, such as the COVID-19 pandemic, access to health care may be limited similarly for an even greater number of patients, and telehealth has been proposed as a useful and necessary modality in overcoming this challenge.14 , 15 Despite this, there have been limited studies on patient and provider experiences with telehealth services when they are used during disasters or other disruptions in the health care system.16 We determined the impact of the sudden increase in telehealth use during the COVID-19 pandemic on patient and provider satisfaction within community-based gastroenterology (GI) practices.
Measurement of Patient and Provider Satisfaction With Telehealth
We conducted a survey of GI patients’ and physicians’ satisfaction with telehealth during the COVID-19 pandemic. A total of 13,084 patients from 2 community-based GI practices in Michigan and the Washington, DC, region who participated in a telehealth visit from March to May 2020 were sent an online satisfaction survey by e-mail. Responses were received from 1492 patients as of June 17, 2020. The survey consisted of 2 prompts: “My GI provider was able to address my concerns during the telehealth visit,” and “I am willing to have more telehealth visits in the future.” Responses were recorded on a 5-point Likert scale (strongly agree, agree, neutral, disagree, or strongly disagree). Patients also were queried on the type of technology platform used with the following response options: smartphone/tablet, laptop/desktop, telephone (audio-only), or other. Sex, age group, and visit reason data also were collected.
Concurrently, a provider-based opinion survey was distributed to a medical association consisting of 95 independent GI practices with 2200 providers in 38 states who are members of the Digestive Health Physicians Association (DHPA).17 Seventy-one practices with 2017 providers opted to participate in the survey (74.7% practice response rate). Responses were received from 503 of these providers (22.9% overall response rate). The survey consisted of 4 prompts about telehealth services: (1) “Telemedicine is an acceptable care delivery model for a segment of GI patients,” (2) “Telemedicine allows me to get an accurate health history for my patients and formulate a satisfactory care plan,” (3) “Telemedicine allows me to provide timely testing and follow-through without interruption to patient care,” and (4) “I will continue using telemedicine in my practice to deliver patient care.” Responses were recorded on a 5-point Likert scale of strongly agree, agree, neutral, disagree, or strongly disagree. Providers also were asked to project what percentage of their future care would be delivered via telehealth: 0% to 25%, 26% to 50%, 51% to 75%, or 76% to 100%. The 95 practices in DHPA were asked to provide the number of telehealth visits conducted by all providers in the DHPA member medical group practices each month during a 3-month period from March to May 2020. Responses to this inquiry were received from 37 practices.
High satisfaction for all groups was defined as 80% approval or higher (responses of strongly agree and agree) to individual survey components. This threshold was selected based on customer satisfaction benchmarks for the telecommunication and health care sectors from the American Customer Service Index.18 Patient satisfaction was examined by age and reason for visit.
Patient Experience
Patient characteristics for the 1492 respondents are shown in Supplementary Table 1. Female patients accounted for 64.7% of respondents. Procedure-related visits, including preparatory and follow-up appointments, were the most common reason for a telehealth encounter. The most common platform used was a desktop or laptop (56.0%), with audio-only interactions making up 4.5% of the visits.
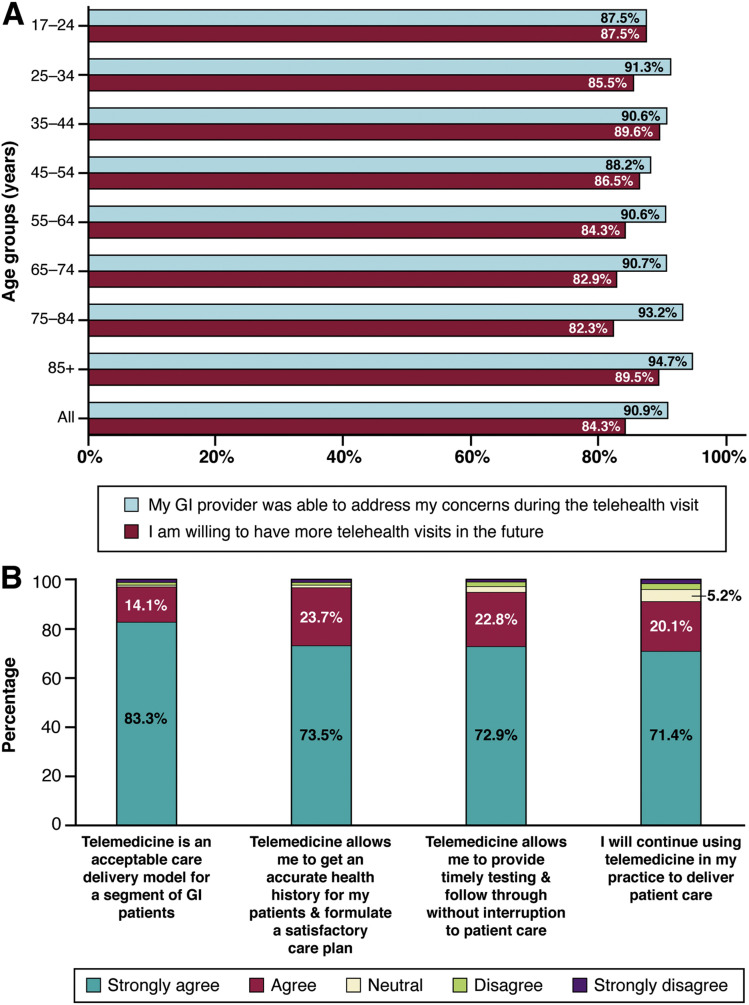
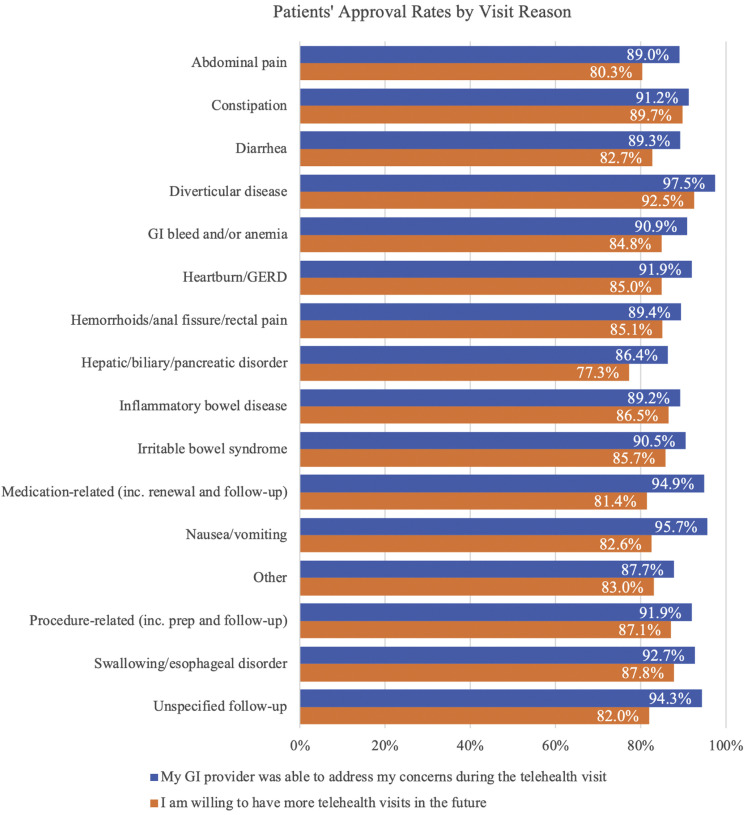
Overall, patients were highly satisfied with their telehealth visits; with greater than 80% indicating that the provider addressed their concern and that they were willing to participate in telehealth visits in the future. High satisfaction was observed in all age groups, with the highest rates in patients older than age 85 (Figure 1 A). Similarly, the vast majority of visit reasons were associated with high patient satisfaction (Supplementary Figure 1). Among the 86.4% of patients seen for hepatic, biliary, and pancreatic disorders who believed that the provider addressed their concern, 77.3% were willing to engage in a telehealth appointment in the future.
Figure 1.
(A) Patients’ approval rates to telehealth stratified by age groups. (B) Providers’ approval rates to telehealth. GI, gastrointestinal.
Supplementary Figure 1.
Patients’ approval rates stratified by visit reason. GERD, gastroesophageal reflux disease; GI, gastrointestinal.
Provider Experience
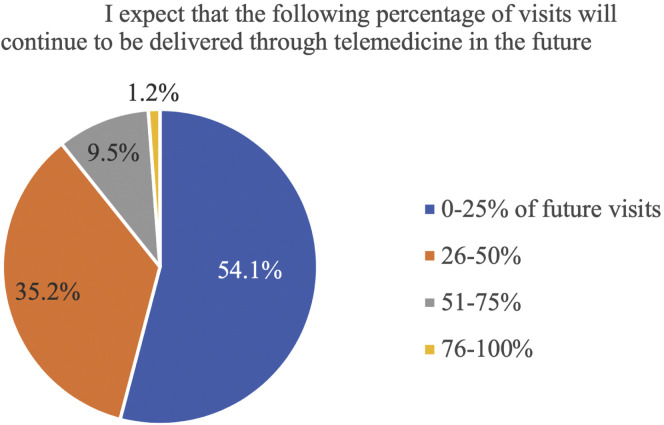
Practices were geographically diverse and ranged in size from 6 to 170 providers. Overall, we found a high level of satisfaction with telehealth services among providers, with greater than 90% of respondents approving (strongly agree or agree) of all 4 prompts (Figure 1 B). The majority (54.1%) expected that less than one quarter of their future care would be delivered via telehealth, with 10.7% projecting it to make up more than half of future encounters (Supplementary Figure 2).
Supplementary Figure 2.
Providers’ expectations of telehealth use in the future.
Telehealth visit volume data were obtained from 37 practices with a total of 899 providers. Collectively, these practice groups performed 51,187 telehealth visits in March, 90,084 in April, and 81,885 in May 2020.
Telehealth and the Triple Aim
In 2008, 3 distinct aims were proposed in an attempt to improve the health care system in the United States: (1) improve the care experience, (2) reduce cost, and (3) improve patient and population health outcomes.19 When viewed through the lens of these goals, telehealth is an effective care delivery modality and the results of this survey suggest that its expanded use would lead to system improvement. First, our findings show a high level of overall patient and provider satisfaction after telehealth appointments. Both groups perceived it to be an effective way to deliver gastroenterological care and expressed a willingness to participate in similar visits in the future. This is despite the abrupt nature of the transition to virtual visits, with little opportunity for practices to optimize processes and correct technology problems. In addition, patients had no option other than virtual visits because of the pandemic and, nonetheless, were highly satisfied with it and open to incorporating it into their care. It is reasonable to expect that patient and provider satisfaction would increase further when telehealth is implemented in a more stepwise manner. Although some studies found a less favorable view of telehealth among older patients, this survey showed a high level of satisfaction across all age groups. This is consistent with more recent literature, suggesting that older patients are becoming more accepting of telehealth as a care delivery model.11 This trend likely is owing to more frequent use of real-time video communication technologies in everyday life, less-cumbersome technology, and improved audio–video quality. The ability to use common platforms, such as FaceTime (Apple, Cupertino, CA) and Zoom (Zoom Video Communications, San Jose, CA), also likely made the prospect of a telehealth interaction with a provider less intimidating for patients.
Patients seen for a diverse array of reasons all showed high satisfaction with their care and were accepting of telehealth. Of those seen for hepatic, biliary, and pancreatic disorders, 77.3% expressed willingness to use telehealth in the future, which did not meet the high satisfaction threshold of 80%. However, 86.4% of these patients indicated that their concerns were addressed by the provider, and this is consistent with the findings of a recent study by Serper et al.20 Patients seen for follow-up care, medication-related issues, and preprocedural appointments were particularly satisfied with their virtual visits. In these groups, telehealth is particularly effective because it is much more convenient for the patient and thus improves the overall care experience. Among both patients and providers, the inability to perform a physical examination has been noted to be a potential barrier to telehealth.6 However, the vast majority of provider respondents believed they were able to formulate an acceptable care plan despite this limitation and were very willing to use telehealth in the future. The use of telehealth in GI care fulfills the first aim of health care improvement by enhancing the care experience for both patients and providers.
The second identified aim involves reducing health care costs through improved efficiency. Telehealth reduces the time and cost associated with a traditional office visit, including travel, missed work obligations, and childcare arrangements.11 From the patient perspective, convenience and decreased cost often are cited as major reasons for their satisfaction with telehealth. This is of particular importance to those with limited mobility, nontraditional work hours, and lower socioeconomic status. For patients who use public transportation or caregivers to travel to appointments, a short appointment may require hours of logistical planning and come at significant financial cost. Enabling these patients to interact with their providers from home would make accessing the health care system both less expensive and logistically less challenging.11 From the practice perspective, telehealth has the potential to be a cost-effective care delivery model by reducing personnel requirements and other expenditures.21 , 22 Continuing to permit the use of more accessible technologic platforms for telehealth will lead to further cost savings.
Telehealth also improves efficiency during times of disruptions to the health care system, such as the COVID-19 pandemic, when the resultant cost savings mean that resources can be invested in other critical needs. As such, telehealth serves as an innovative addition to the health care system’s response to natural disasters.14 The rapid implementation and utilization of telehealth during the COVID-19 pandemic represents large-scale use of this care delivery model in this setting. The transition to telehealth in place of most in-person encounters allowed patients to continue to receive care while reducing the risk of infection and maintaining high patient and provider satisfaction. This is of particular importance for elderly and immunocompromised patients and those with chronic health conditions, for whom an infection would significantly adversely affect their health and be more costly to the system as a whole. In addition, telehealth enabled practices to avoid the costly and complex task of contact tracing if a patient or employee were to be diagnosed with COVID-19. Given the current uncertainty regarding the possibility of re-infection and concerns of subsequent outbreaks, the continued use of telehealth services is critical for individual patient well being and the greater public health. Thus, telehealth improves efficiency and reduces cost for both patients and practice groups during times of routine care and, importantly, when the health care system is disrupted. The final aim, improved patient outcomes, is an area that requires additional study in GI patients, although better outcomes have been shown in other settings.11
Decrease in Regulatory Barriers
The COVID-19 pandemic required an unexpected, immediate expansion of telehealth use. To facilitate this, regulatory changes that addressed several well-documented barriers were instituted. These included increasing payments for telehealth encounters, permitting audio-only communications, and allowing for the use of everyday communication technology that is not specifically Health Insurance Portability and Accountability Act compliant.5 These changes allowed at least 37 community-based GI practices across the nation to conduct 51,187 telehealth encounters in March 2020 and 90,084 in April, an increase of 76.0%. This number likely represents only a very small percentage of the total telehealth visits conducted in the United States over the past several months. Preserving these regulatory flexibilities is critical to the expansion of telehealth and thus will contribute to overall health care system improvement.
Conclusions
During the COVID-19 pandemic, telehealth use increased dramatically to reduce disease transmission while ensuring continuity of care. This survey of community-based GI patients and providers showed high satisfaction and acceptance with virtual encounters. The results of our surveys are noteworthy for several reasons. Although previous studies have investigated provider and patient satisfaction in the provision of urology, dermatology, and urgent care, this survey evaluated provider and patient satisfaction it in the setting of community-based general GI practices.7 , 10 In addition, it shows that stakeholders experience high satisfaction with and acceptance of telehealth when it is implemented in response to a disruption of the health care system. Regulatory changes enacted by the Centers for Medicare and Medicaid Services and private payers in March 2020 enabled telehealth to fulfill 2 of the 3 aims of health care improvement by enhancing the care experience and improving cost effectiveness. Further research is needed to determine the effect of telehealth on patient outcomes.
Ziad F. Gellad, Section Editor
Footnotes
Conflicts of interest The authors disclose no conflicts.
Note: To access the supplementary material accompanying this article, visit the online version of Clinical Gastroenterology and Hepatology at www.cghjournal.org, and at https://doi.org/10.1016/j.cgh.2020.07.014.
Supplementary Material
Supplementary Table 1.
Patient Baseline Characteristics, Reason for Visit, and Technology Platform Used
| Patient characteristics | n = 1492 |
|---|---|
| Age, y | N (%) |
| 17–24 | 24 (1.6) |
| 25–34 | 69 (4.6) |
| 35–44 | 96 (6.4) |
| 45–54 | 170 (11.4) |
| 55–64 | 350 (23.5) |
| 65–74 | 496 (33.2) |
| 75–84 | 249 (16.7) |
| ≥85 | 38 (2.5) |
| Sex | |
| Female | 965 (64.7) |
| Visit reason | |
| Abdominal pain | 173 (11.6) |
| Constipation | 68 (4.6) |
| Diarrhea | 75 (5.0) |
| Diverticular disease | 40 (2.7) |
| GI bleed and/or anemia | 33 (2.2) |
| Heartburn/GERD | 173 (11.6) |
| Hemorrhoids/anal fissure/rectal pain | 47 (3.2) |
| Hepatic/biliary/pancreatic disorder | 66 (4.4) |
| Inflammatory bowel disease | 111 (7.4) |
| Irritable bowel syndrome | 42 (2.8) |
| Medication-related (including renewal and follow-up evaluation) | 59 (4.0) |
| Nausea/vomiting | 23 (1.5) |
| Procedure-related (including preparation and follow-up evaluation) | 248 (16.6) |
| Swallowing/esophageal disorder | 41 (2.7) |
| Other | 171 (11.5) |
| Unspecified follow-up evaluation | 122 (8.2) |
| Technology platform used | |
| Laptop/desktop | 836 (56.0) |
| Smartphone/tablet | 585 (39.2) |
| Telephone (audio-only) | 67 (4.5) |
| Unknown | 4 (0.3) |
GERD, gastroesophageal reflux disease; GI, gastrointestinal.
References
- 1.World Health Organization (WHO) WHO Director-General's opening remarks at the media briefing on COVID-19. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Available from: Published 11 Mar 2020. Accessed: April 21, 2020.
- 2.Centers for Disease Control and Prevention (CDC) Cases of coronavirus disease (COVID-19) in the U.S. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. April 20 Available from: 2020. Accessed: April 21, 2020.
- 3.CDC Social distancing, quarantine, and isolation. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html. April 4 Available from: 2020. Accessed: April 20, 2020.
- 4.CDC Outpatient and ambulatory care settings: responding to community transmission of COVID-19 in the United States. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ambulatory-care-settings.html Available from: 2020. Accessed: April 16, 2020.
- 5.Centers for Medicare and Medicaid Services (CMS) Trump administration issues second round of sweeping changes to support U.S. healthcare system during COVID-19 pandemic. https://www.cms.gov/newsroom/press-releases/trump-administration-issues-second-round-sweeping-changes-support-us-healthcare-system-during-covid. April 30 Available from: 2020. Accessed: May 12, 2020.
- 6.Dorsey E.R., Topol E.J. State of telehealth. N Engl J Med. 2016;375:154–161. doi: 10.1056/NEJMra1601705. [DOI] [PubMed] [Google Scholar]
- 7.Viers B.R., Pruthi S., Rivera M.E. Are patients willing to engage in telemedicine for their care: a survey of preuse perceptions and acceptance of remote video visits in a urological patient population. Urology. 2015;85:1233–1239. doi: 10.1016/j.urology.2014.12.064. [DOI] [PubMed] [Google Scholar]
- 8.Donelan K., Barreto E.A., Sossong S. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care. 2019;25:40–44. [PubMed] [Google Scholar]
- 9.Lee T., Kim L. Telemedicine in gastroenterology: a value-added service for patients. Clin Gastroenterol Hepatol. 2020;18:530–533. doi: 10.1016/j.cgh.2019.12.005. [DOI] [PubMed] [Google Scholar]
- 10.Polinski J.M., Barker T., Gagliano N. Patients' satisfaction with and preference for telehealth visits. J Gen Intern Med. 2016;31:269–275. doi: 10.1007/s11606-015-3489-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kruse C.S., Krowski N., Rodriguez B. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Totten A.M., US Agency for Healthcare Research and Quality, Oregon Health and Science University Pacific Northwest Evidence-based Practice Center, Effective Health Care Program. Telehealth: mapping the evidence for patient outcomes from systematic reviews. In: Technical brief 26. Rockville, MD: Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2016. https://www.ncbi.nlm.nih.gov/books/NBK379320/ Available from: Accessed May 25, 2020. [PubMed]
- 13.Orlando J.F., Beard M., Kumar S. Systematic review of patient and caregivers' satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients' health. PLoS One. 2019;14 doi: 10.1371/journal.pone.0221848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lurie N., Carr B.G. The role of telehealth in the medical response to disasters. JAMA Intern Med. 2018;178:745–746. doi: 10.1001/jamainternmed.2018.1314. [DOI] [PubMed] [Google Scholar]
- 15.Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382:1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 16.Latifi R., Tilley E.H. Telemedicine for disaster management: can it transform chaos into an organized, structured care from the distance? Am J Disaster Med. 2014;9:25–37. doi: 10.5055/ajdm.2014.0139. [DOI] [PubMed] [Google Scholar]
- 17.About Us Digestive Health Physicians Association. https://www.dhpassociation.org/about-us/ Available from:
- 18.Benchmarks by sector American Customer Service Index. https://www.theacsi.org/acsi-benchmarks/benchmarks-by-sector. 2020 Available from: Accessed June 19, 2020.
- 19.Berwick D.M., Nolan T.W., Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood) 2008;27:759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 20.Serper M., Cubell A.W., Deleener M.E. Telemedicine in liver disease and beyond: can the COVID-19 crisis lead to action? Hepatology. 2020 doi: 10.1002/hep.31276. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grustam A.S., Severens J.L., De Massari D. Cost-effectiveness analysis in telehealth: a comparison between home telemonitoring, nurse telephone support, and usual care in chronic heart failure management. Value Health. 2018;21:772–782. doi: 10.1016/j.jval.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 22.Kairy D., Lehoux P., Vincent C. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31:427–447. doi: 10.1080/09638280802062553. [DOI] [PubMed] [Google Scholar]