Abstract
Transcription factors encoded by Homeobox (HOX) genes play numerous key functions during early embryonic development and differentiation. Multiple reports have shown that mis-regulation of HOX gene expression plays key roles in the development of cancers. Their expression levels in cancers tend to differ based on tissue and tumor type. Here, we performed a comprehensive analysis comparing HOX gene expression in different cancer types, obtained from The Cancer Genome Atlas (TCGA), with matched healthy tissues, obtained from Genotype-Tissue Expression (GTEx). We identified and quantified differential expression patterns that confirmed previously identified expression changes and highlighted new differential expression signatures. We discovered differential expression patterns that are in line with patient survival data. This comprehensive and quantitative analysis provides a global picture of HOX genes’ differential expression patterns in different cancer types.
Keywords: HOX genes, cancer, transcription factors, differential expression analysis, patient survival
1. Introduction
Homeobox (HOX) genes encode transcription factors that function as critical master regulators during embryogenesis in diverse processes, including apoptosis, receptor signaling, motility, and angiogenesis (reviewed in [1,2,3]). HOX genes have also been shown to function in adult stem cell differentiation [4,5,6].
The human HOX genes are organized in four genomic clusters marked by the letters A, B, C, and D, which are located on different chromosomes (7, 17, 12, and 2, respectively). The HOX genes of each cluster are numbered from 1 to 13. As some HOX genes in each locus were lost during evolution, there are a total of 39 HOX genes. HOX genes display spatial and temporal collinearity [7]. The HOX proteins are classified into 3 main groups—anterior (HOX1-3), central (HOX4-8), and posterior (HOX9-13), according to their expression along the anterior-posterior axis during development.
Multiple reports have demonstrated that mis-regulation of HOX genes expression plays key roles in the development of cancers. Only in the last five years have more than 50 reviews related to this subject been published; see, for example, References [4,8,9,10,11]. However, such studies were typically based on different technologies used in different labs and analyzed by different computational tools. Although some reviews summarized the findings of individual reports that analyzed the expression of distinct HOX genes in specific cancers (e.g., References [1,4]), a comprehensive quantitative comparison of HOX gene expression between cancer samples and samples obtained from healthy matched tissues is lacking.
Here, we present a thorough, standardized, uniform and systematic analysis performed using the most comprehensive data sources available to date: The Cancer Genome Atlas (TCGA) and the recently available Genotype-Tissue Expression (GTEx) resource [12]. Our standardized and systematic approach enabled us to perform rigorous comparisons between HOX gene expression data in different cancer types and matched healthy tissues, identify differential expression patterns that can confirm previously identified expression changes, and highlight new differential expression signatures, which we show are in line with patient survival data.
2. Results
2.1. Gene Expression Data Obtained from TCGA and GTEx Using Xena are Comparable
The TCGA database of cancer tissue expression levels does not include, by and large, samples of healthy tissues. Thus, our main strategy in this analysis is to compare expression data from cancer patients obtained from the TCGA database with healthy samples taken from the GTEx database. The developers of the UCSC Xena normalized the data to allow comparisons between these two data sources and indeed such a comparison was made in several studies (see, for example, References [13,14]). Nevertheless, in order to validate this approach, we first needed to establish that comparing data from these two sources is legitimate and does not introduce bias into the analysis.
For that purpose, we first analyzed gene expression either when both healthy and tumor data was obtained from TCGA, or when the tumor data was obtained from TCGA and the healthy data was obtained from GTEx. To this end, we used tissues that included at least 50 healthy samples in TCGA, namely breast invasive carcinoma (BRCA), liver hepatocellular carcinoma (LIHC), lung adenocarcinoma (LUAD), lung squamous cell carcinoma (LUSC), and thyroid carcinoma (THCA), which include 113, 50, 59, 50, and 59 TCGA healthy samples, respectively. To generate an empirical null distribution, we calculated the number of genes with differential expression between healthy and tumor breast tissue, for 1000 random sets of 39 genes (not specifically HOX genes). In each trial, we compared the lists of genes that were found to be differentially expressed in TCGA and GTEx. The calculation was done when both healthy and tumor data were obtained from TCGA and when the tumor data were taken from TCGA and healthy data were obtained from GTEx. The results demonstrate that the two data sources are comparable: the average difference in the number of differentially expressed genes is between 2 to 3 (Figure S1 and Table S1) and that HOX genes do not deviate differently from random sets of genes. When we specifically checked the number of HOX genes that were differentially expressed between tumor and healthy tissues using the healthy tissue from the two sources we found that for BRCA, LIHC, LUAD, LUSC & THCA the difference was 4, 4, 3, 3, and 7 genes, respectively (with empirical p-value 0.321, 0.221, 0.711, 0.49, and 0.004, respectively) (Figure S1 and Table S1). We assume that the large deviation for thyroid carcinoma stems from different relative abundance of the tumor subtypes: (papillary thyroid cancer, follicular thyroid cancer, anaplastic thyroid cancer, medullary thyroid cancer) in the two databases, but we did not have clinical documentation to analyzed this issue further.
These observations suggest that the comparison of gene expression data of tumor samples obtained from TCGA to gene expression data of healthy samples obtained from GTEx using Xena is valid.
2.2. Differential Expression of HOX Gene Clusters Can Discriminate Between Tumor Samples and Healthy Samples
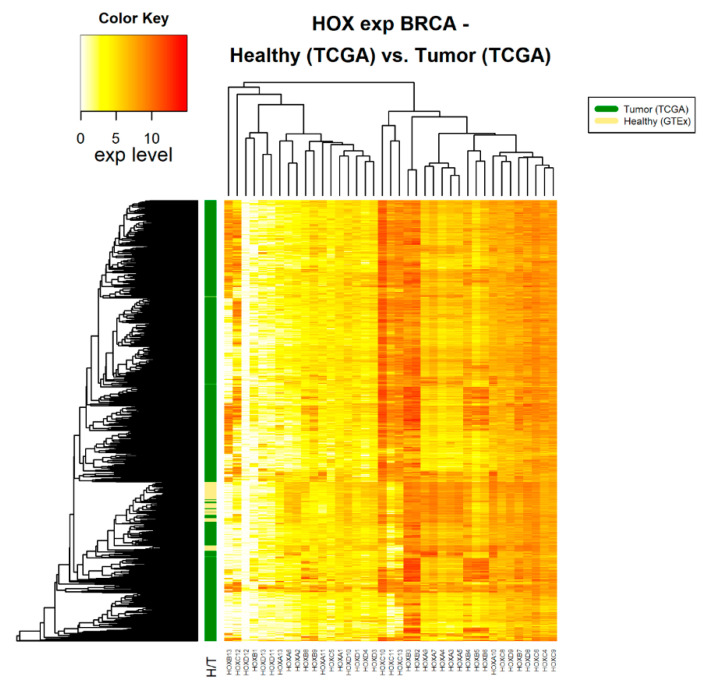
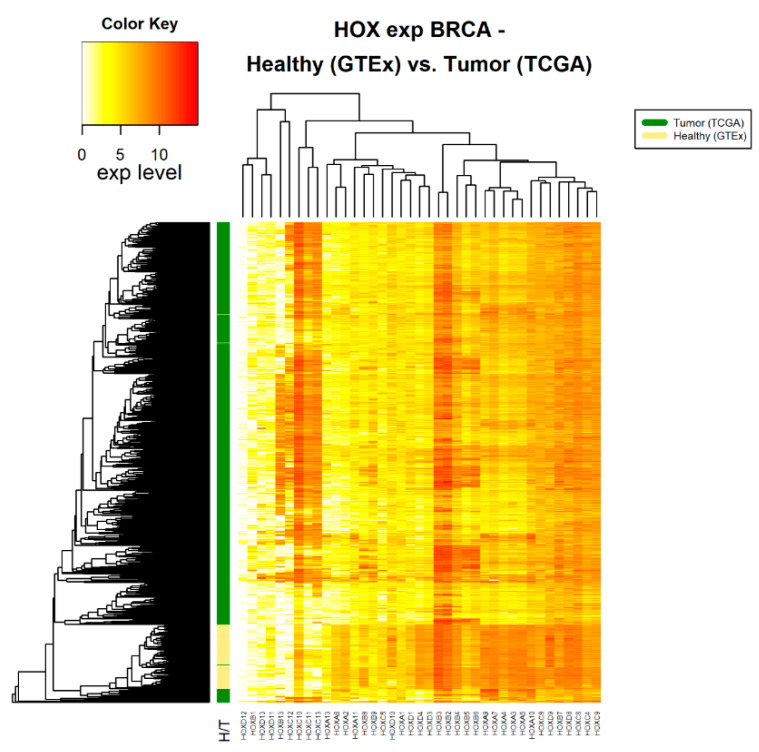
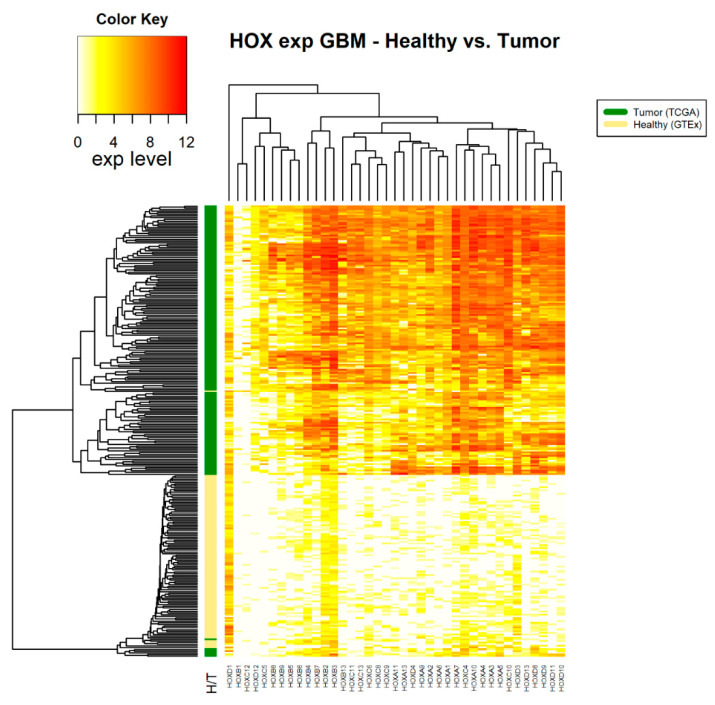
Following the assertion that GTEx data can be used as a source for healthy samples, we compared HOX gene clusters in tumor and healthy samples. Fourteen cancer types, for which there were at least 100 tumor samples (in TCGA) and at least 100 healthy samples (in GTEx), were included in this analysis (Table 1). For each of these 14 cancer types, namely cancers associated with the adrenal gland, brain, breast, colon, esophagus, blood cells (leukemia), liver, lung, pancreas, prostate, stomach, and thyroid, the normalized expression levels of 39 HOX genes were obtained. A hierarchical clustered heatmap was created based on the average Euclidean distance between healthy samples compared with the average Euclidean distance of tumor samples. As an example, we present 3 such heatmaps (Figure 1, Figure 2 and Figure 3). The other heatmaps can be found in the Figures S2–S13. The heatmaps demonstrate that, in all cancer types, differential expression of HOX gene clusters can separate tumor samples from healthy samples and that, for some of the HOX genes, the expression changes are higher than that of others (Figure 1, Figure 2 and Figure 3 and Figures S2–S13).
Table 1.
The number of Genotype-Tissue Expression (GTEx) and The Cancer Genome Atlas (TCGA) samples used in the study 1.
| Organ/Cancer Tissue Type | GTEX | TCGA | Total |
|---|---|---|---|
| Adrenal_Gland/PCPG | 128 | 185 | 313 |
| Brain/LGG | 105 | 527 | 632 |
| /GBM | 173 | 173 | |
| Breast/BRCA | 179 | 1253 | 1432 |
| Colon/COAD | 308 | 455 | 763 |
| Esophagus/ESCA | 273 | 195 | 468 |
| Leukemia/LAML | 337 | 173 | 510 |
| Liver/LIHC | 110 | 422 | 532 |
| Lung/LUAD | 288 | 598 | 886 |
| /LUSC | 551 | 551 | |
| Pancreas/PAAD | 167 | 183 | 350 |
| Prostate/PRAD | 100 | 556 | 656 |
| Stomach/STAD | 175 | 451 | 626 |
| Thyroid/THCA | 280 | 571 | 851 |
| Total | 2450 | 6293 | 8743 |
1 The number of healthy samples is listed under the GTEx column and the number of tumor samples is listed under TCGA column. Acronyms of cancer tissue types: BRCA = breast invasive carcinoma, COAD = colon adenocarcinoma, ESCA = esophageal carcinoma, GBM = glioblastoma multiforme, LAML = acute myeloid leukemia, LGG = brain lower grade glioma, LIHC = liver hepatocellular carcinoma, LUAD = lung adenocarcinoma, LUSC = lung squamous cell carcinoma, PAAD = pancreatic adenocarcinoma, PCPG = pheochromocytoma and paraganglioma, PRAD = prostate adenocarcinoma, STAD = stomach adenocarcinoma, and THCA = thyroid carcinoma.
Figure 1.
HOX gene expression in healthy and tumor breast tissue samples. The source of expression data of both healthy and tumor samples is TCGA.
Figure 2.
HOX gene expression in tumor and healthy breast tissue samples. The source of expression data of healthy and tumor samples is GTEx and TCGA, respectively.
Figure 3.
HOX gene expression in samples of healthy brain tissue and glioblastoma multiforme tumor tissue. The source of expression data of healthy and tumor samples is GTEX and TCGA, respectively.
2.3. Differential Expression of HOX Genes in 14 Different Cancer Types
To determine which HOX genes significantly change their expression levels in tumor tissues compared to healthy tissues, we performed the statistical Wilcoxon rank-sum test for every HOX gene and for every cancer type. A 2-fold differential expression cut-off was used for binary classification of differently expressed genes, i.e., HOX genes with expression in cancer samples statistically significant as higher than twice the expression in healthy samples, or lower than half the expression in healthy samples, were considered as “differentially expressed genes”.
In all 14 analyzed cancer types, there were multiple HOX genes with significant (p < 0.05 Bonferroni adjusted for n = 39) altered expression between healthy and tumor tissues (Figure 4).
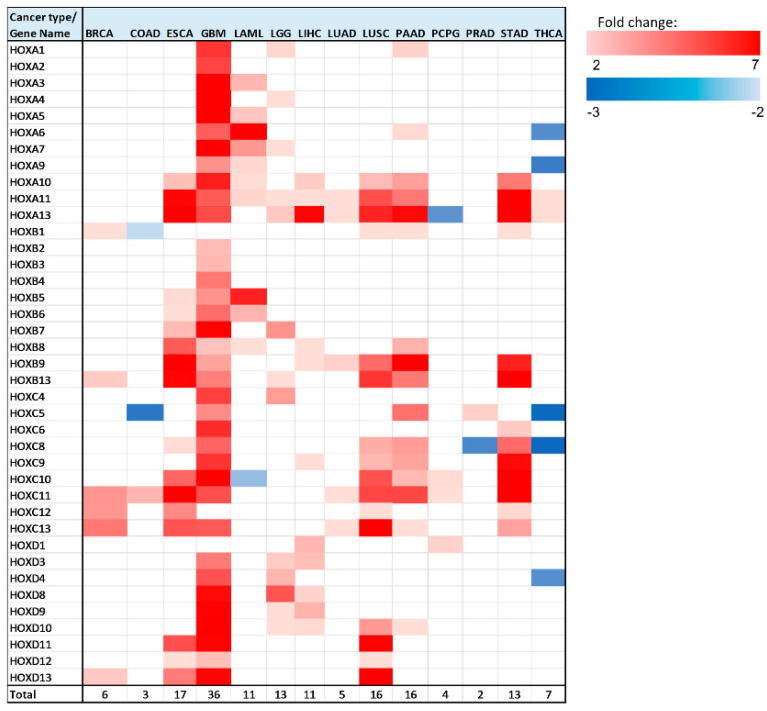
Figure 4.
Heatmap of differentially expressed HOX genes in different cancer types. Gene column includes list of all 39 HOX genes tested in this analysis. The rest of the columns represent the analyzed cancer types. Upregulated genes are marked in red color gradient (light red represents lower fold change), downregulated genes are marked in blue color gradient (light blue represents lower fold change).
Note that, in brain tumors, glioblastoma multiforme (GBM), a large number of HOX genes are differentially expressed between tumor and healthy samples (36 HOX genes). In the GTEx project design details, it was indicated that the majority of the brain and brainstem were left unfixed and shipped overnight on wet ice to a brain bank [15]. We ruled out the possibility that low expression of HOX genes in healthy samples of the brain is an artifact of the way that these samples were treated by showing that the expression level of other sets of random 39 genes were in the normal range. Notably, there were 6 HOX genes, namely HOXA2, HOXA4, HOXB2, HOXB3, HOXB4, and HOXC4, which changed expression only in brain cancer (either in GBM, brain lower grade glioma (LGG), or in both).
In addition to GBM, there were 5 cancer types for which a third or more of the HOX genes displayed altered gene expression, namely LGG, esophageal carcinoma (ESCA), LUSC, pancreatic adenocarcinoma (PAAD), and stomach adenocarcinoma (STAD). Intriguingly, 4 out of these 5 cancer type tissues are derived from endodermal organs that are located in the foregut.
As mentioned above, HOX genes are organized in 4 genomic clusters (HOXA, HOXB, HOXC, HOXD), and genes within each cluster can be grouped based on their expression in different developmental regions (anterior, central, or posterior). Table S2 provides the type of expression change (upregulation/downregulation/no change) for each analyzed cancer type, with HOX genes organized into clusters and groups. Interestingly, the majority of HOX genes (94 out of 160) that change expression belong to the posterior HOX group (HOX9-13) (Table S2). Notably, calculation and comparison of the mean expression level of 1000 randomly selected 16 HOX genes to the mean expression levels of the 16 posterior HOX revealed that many posterior HOX genes are expressed at low levels in multiple healthy tissues (empirical p-value = 0.013) (Figure S14), in line with PCR analysis of HOX gene expression in normal thyroid gland, performed by Takahashi et al. [16]. The “anterior HOX group” is the group with the least number of HOX genes with altered gene expression in cancer tissues—18 genes out of 160 differentially expressed genes (these 18 genes account for ~16% of the total number of anterior genes in 14 cancer). Most of the HOX genes (150 out of 160) with altered expression in the analyzed cancer tissues were upregulated. However, in colon adenocarcinoma (COAD), acute myeloid leukemia (LAML), pheochromocytoma and paraganglioma (PCPG), prostate adenocarcinoma (PRAD), and THCA, there were a total of 10 HOX genes that were downregulated (Figure 4, Table S2). HOXC is the HOX cluster with the highest number of HOX genes that change expression (48 genes). Most of the HOXC cluster genes display relatively low expression levels in the analyzed healthy tissues (Figure S14). In this analysis, HOXA11 and HOXA13 were identified as differentially expressed in the highest number of cancer types (10 out of 14).
We next focused on the genes that undergo the most significant changes (Table 2). We highlighted genes with at least a 3-fold expression change between healthy and tumor tissues, and with normalized gene expression levels in healthy tissues of at least 1 unit (RNA-seq by Expectation Maximization (RSEM) normalized count, log2(x + 1) transformed). This requirement was implemented in order to identify genes whose expression levels changed significantly, both in terms of fold change and in terms of absolute levels. HOX genes that met these criteria were found in 9 out of 14 analyzed cancer types: BRCA, ESCA, GBM, LAML, LGG, LIHC, LUSC, PAAD, and STAD. Seventeen out of 28 cases that met the above criteria for differentially expressed genes belong to the ‘posterior HOX group’, 10 belong to the ‘central HOX group’, and one gene belongs to the ‘anterior HOX group’. The highest expression fold change was observed for HOXC10 in STAD. Notably, there were 3 other HOX genes with a fold change greater than 4 in STAD: HOXA10, HOXB9, and HOXC8.
Table 2.
HOX genes with pronounced expression change between healthy and tumor tissues 1.
| Gene Name | Cancer Type | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| BRCA | ESCA | GBM | LAML | LGG | LIHC | LUSC | PAAD | STAD | |
| HOXA5 | 7.0 | ||||||||
| HOXA7 | 3.6 * | ||||||||
| HOXA9 | 3.7 | ||||||||
| HOXA10 | 6.2 | 3.4 | 4.3 | ||||||
| HOXB4 | 4.3 | ||||||||
| HOXB8 | 3.0 | ||||||||
| HOXB9 | 4.6 | 6.2 | |||||||
| HOXB13 | 6.8 | ||||||||
| HOXC4 | 5.5 | 3.5 * | |||||||
| HOXC6 | 5.9 | ||||||||
| HOXC8 | 3.2 | 3.5 | 4.6 | ||||||
| HOXC9 | 3.4 | ||||||||
| HOXC10 | 4.7 | 5.1 | 7.5 | ||||||
| HOXC11 | 3.7 | ||||||||
| HOXC13 | 4.3 | 5.1 | |||||||
| HOXD3 | 4.3 | ||||||||
| HOXD9 | 3.0 | ||||||||
| HOXD10 | 3.6 | ||||||||
| HOXD11 | 5.2 | ||||||||
1 The expression fold change of HOX genes with at least a 3-fold expression change between healthy and tumor tissues and with gene expression levels of at least 1 unit (RSEM normalized count, log2(x + 1) transformed) in healthy tissues. The cells marked * bold highlight the genes for which the Kaplan-Meier (KM) graph showed a significant correlation between gene expression and patients’ survival (analysis detailed below).
We noted that some differentially expressed HOX genes are expressed at very low levels in healthy tissues (less than 1 unit of normalized expression values; Xena) and have high expression fold-change. To identify the genes whose expression is significantly altered and their absolute expression levels in tumor tissues is not very low, we applied selection criteria to highlight the genes whose expression levels in tumor tissues were higher than 1 unit of normalized expression values and had at least a 3-fold expression change between healthy and tumor tissues (Table S3). The cancer types with the highest number of HOX gene that met the above criteria were in GBM (25 genes), while the highest expression changes were observed in STAD (Table S3). Notably, most of the HOX genes that met the above criteria belong to the posterior HOX group (38 out of 57 cases), and among them, HOXA13 stands-out as its expression changed in most cancer types (6 out of 14) (Table S3).
2.4. Kaplan-Meier Survival Analysis
The differentially expressed genes that most significantly changed (Table 2, Table S3) and also demonstrate correlation with patients’ survival may potentially serve as prognostic markers. To identify candidate genes that can serve as potential prognostic markers, a Kaplan-Meier (KM) survival analysis was performed for every differentially expressed gene in every cancer type (Table S4). Table 3 lists the genes for which the KM analysis results were statistically significant (p-value < 0.05 Bonferroni adjusted for n = 39).
Table 3.
HOX genes with statistically significant KM curve 1.
| Organ/Cancer Type | HOX Genes with a Significant KM Correlation |
|---|---|
| Brain-LGG | HOXA1, HOXA4, HOXA7, HOXA11 |
| HOXB13 | |
| HOXC4 | |
| HOXD3, HOXD4, HOXD8, HOXD9, HOXD10 | |
| Brain-GBM | HOXB2, HOXB9 |
| Leukemia-LAML | HOXA7 |
1 Differentially expressed HOX genes for which the KM analysis demonstrates a correlation between increased expression level and patients’ poor survival (p-value < 0.05 Bonferroni adjusted for n = 39).
In 14 out of the 160 cases in which a HOX gene was differentially expressed in one of the 14 analyzed cancer types, there was a significant correlation between increased expression levels and poor survival (p-value < 0.05 Bonferroni adjusted for n = 39) (Table S4).
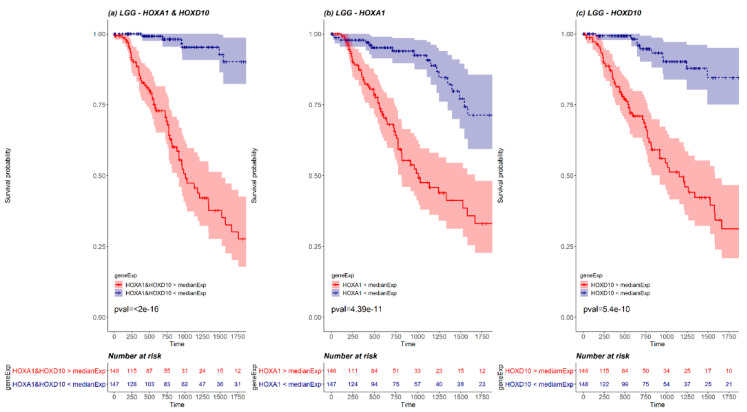
We next examined whether pairs of HOX genes could be used together as stronger prognosis markers. To this end, a KM survival analysis was performed for every cancer type, for every combination of HOX pair where both HOX genes were differentially expressed. The pairs that demonstrated significant results (p-value < 0.05 Bonferroni adjusted for n = 741), were compared with the KM survival analysis performed for each one of the paired genes separately (Supplementary Materials File 1 and Table S5). Such pairs were found in 2 cancer types, LGG and GBM (20 and 4 pairs, respectively). For example, LGG HOX pair HOXA1 and HOXD10 demonstrates a more statistically significant KM curve than the KM survival curve performed for each one of the paired genes separately (Figure 5). Details of significant pairs are included in Table S5. Importantly, each of these gene pairs could potentially serve as a prognostic marker.
Figure 5.
A KM plot of HOXA1 and HOXD10 pair (a) versus separate KM plots for each of HOXA1 (b) and HOXD10 (c) in LGG. The red line represents the survival of patients with expression higher than median expression, and the blue line represents the survival of patients with expression lower than median expression. The pink and the light blue background of the lines mark the confidence interval. Out of 527 LGG patients, there were 148 patients with both HOXA1 and HOXD10 expressed above LGG median expression (marked in red in the risk table below graph) and 147 patients with both HOXA1 and HOXD10 expressed below LGG median expression (marked in blue in the risk table below graph).
2.5. HOX Gene Pairs with Correlated Differential Expression
Genes that have combined effects or act in similar pathways may demonstrate an expression correlation. The expression analysis results included several cases in which in the same cancer type, there were a few genes that demonstrated a similar fold change between tumor and healthy tissue (Figure 4, Table 2). For example, in ESCA, HOXC13, and HOXD11 demonstrated~5-fold expression change, or in PAAD, HOXA10, HOXB8, HOXC8, and HOXC9 demonstrated~3-fold expression change (Table 2). Based on these findings, and following the results of the KM analysis, we next examined whether there are any HOX genes pairs that show correlated expression patterns within the same sample in both tumor and healthy tissues. To this end, a Pearson correlation was calculated for all possible 741 HOX gene pairs for each analyzed cancer type. The analysis was performed for gene pairs for which both tumor and healthy cohorts demonstrated normal distribution. These genes were identified by Kolmogorov–Smirnov normality test. The gene pairs that change expression between healthy and tumor samples and show moderate or strong correlation (i.e., either r > 0.4 or r < −0.4 [17]) in both tissue types were considered correlated. The resulting gene pairs were observed in 6 cancer types: ESCA, GBM, LAML, LIHC, LUSC, and STAD (Table 4, correlation graphs are included in Figures S15–S33). In 14 (out of 19) gene pairs, both pair members belong to the same cluster (Table 4, Figure S34). Notably, all resulting mixed clusters pairs include one gene from cluster A and one gene from another cluster (Table 4, Figure S34). Examination of the pair composition from the HOX group perspective indicates that only 9 (out of 19) pairs belong to the same HOX group (Figure S35).
Table 4.
HOX gene pairs with significant expression correlation categorized by cancer type 1.
| Cancer Type\Gene Name | HOX Pairs | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| HOXA5 | HOXA9 | HOXB3 | HOXB5 | HOXB6 | HOXB7 | HOXC8 | HOXC9 | HOXC10 | HOXD9 | Total | |
| ESCA | |||||||||||
| HOXA10 | ✓ | ✓ | 3 | ||||||||
| HOXB5 | ✓ | ✓ | 2 | ||||||||
| HOXB6 | ✓ | 1 | |||||||||
| HOXC10 | ✓ | 1 | |||||||||
| GBM | |||||||||||
| HOXA3 | ✓ | 1 | |||||||||
| HOXA10 | ✓ | 1 | |||||||||
| HOXB2 | ✓ | 1 | |||||||||
| HOXB4 | ✓ | 1 | |||||||||
| HOXB5 | ✓ | 1 | |||||||||
| LAML | |||||||||||
| HOXA3 | ✓ | 1 | |||||||||
| HOXA10 | ✓ | 1 | |||||||||
| LIHC | |||||||||||
| HOXD3 | ✓ | 1 | |||||||||
| HOXD8 | ✓ | 1 | |||||||||
| LUSC | |||||||||||
| HOXC8 | ✓ | 1 | |||||||||
| STAD | |||||||||||
| HOXC6 | ✓ | ✓ | 2 | ||||||||
1 The √ indicates HOX gene pair with significant expression correlation.
The expression correlation observed between HOXB5, HOXB6, and HOXB7 in ESCA, is in line with a previous report that showed that expression changes in the three “midcluster” HOXB genes, namely HOXB5, HOXB6, and HOXB7, can trigger changes in the transcriptional program of adult esophageal cells, with implications to the early stages of esophageal carcinogenesis [18]. It is possible that since these genes are neighboring genes they are regulated by the same factors and therefore manifest expression correlations.
Similarly, we wanted to check whether there are HOX gene pairs that show moderate or strong expression correlation in healthy tissue and lose it in tumor tissue, or vice versa. Out of 69 HOX gene pairs that show weak expression correlation (i.e., either r < 0.4 or 0 > r > −0.4) in healthy and moderate or strong correlation in tumor tissue, there were 21 pairs that showed strong correlation in tumor tissue (i.e., either r > 0.7 or r < −0.7). Moreover, 6 of these gene pairs were HOXA pairs observed in LAML with Pearson correlation coefficient r > = 0.89 (Figures S36–S56). Interestingly, there were only 7 HOX gene pairs that showed moderate expression correlation (0.4 < r < 0.7) in healthy tissue and did not show expression correlation in tumor tissue (either r < 0.4 or 0 > r > −0.4).
2.6. Comparison of HOX Genes Expression with Expression of House Keeping Genes
To validate that the differential expression pattern of HOX genes in tumor tissue is not a generic behavior of genes in tumor tissue, we examined the expression pattern of housekeeping (HK) genes in healthy and tumor tissue and compared it with HOX genes’ expression pattern. For every cancer type, a differential expression analysis was performed for a list of 3804 human HK genes compiled by Eisenberg et al. [19]. The vast majority of the HK genes are not differentially expressed between tumor and healthy samples. For every cancer type there were very few (10 or less out of 3804) HK genes that differentially expressed (Table S6). Moreover, in all analyzed cancer types, the expression levels of HK genes were higher (2-fold or more) than the expression level of HOX genes (empirical p-value = 0).
2.7. Comparison of HOX Genes Expression with Expression of Transcription Factors Enocoding Genes in Brain Healthy and Tumor Tissue
As cells from healthy brain tissue present virtually no proliferation, expression of a huge number of genes is activated in glioblastomas. Therefore, we performed a differential expression analysis between brain healthy tissue and GBM tumor tissue for other transcription factors (TF) and compared their expression pattern with HOX genes expression pattern. The analysis was performed on a list of human transcription factors compiled by Lambert SA et al. [20]. The HOX genes are a subgroup of the Homeodomain TF family. In GBM, most of the HOX genes (36 out of 39) are differentially expressed between tumor and healthy tissues, whereas a smaller fraction of the non-HOX Homeodomain genes (43 out of 187) is differentially expressed (Figures S57–S58, Table S7). Remarkably, in other TF gene families, such as bZIP and Nuclear Receptors, most of the genes are expressed in both healthy and tumor tissues and demonstrate little expression changes (Figures S59–S60 and Table S7).
2.8. Comparison of HOX Genes with Known Prognostic Markers
Many of the cancer-related prognostic markers used in medical clinics are not based on changes in gene expression level. In order to compare HOX gene expression patterns in cancer tissue with known cancer markers, we searched for prognostic markers that are known to undergo genetic alterations and protein level changes. We have compiled a list of 29 previously suggested prognostic markers genes for the 8 analyzed cancer types in which 11 or more (about a third) of the HOX genes were found to be differentially expressed (Table S8) [21,22,23,24,25,26,27,28,29,30,31,32]. For each marker, we examined whether it is differentially expressed between healthy and tumor tissue and performed a Kaplan-Meier (KM) survival analysis. The analysis demonstrated that only 6 of the previously suggested prognostic markers included in the list, namely ABCC3 in GBM, CDX2, KIT, and WT1 in LAML and CEACAM5 in LIHC and STAD, are differentially expressed between tumor and healthy tissue, and 3 of them (ABCC3, KIT, and WT1) demonstrate a significant correlation between increased expression levels and poor survival (p-value < 0.05) (Tables S8 and S9).
2.9. HOX Expression in BRCA HER2-Positive, BRCA HER2-Negative, and BRCA Triple-Negative Samples
Analysis of HOX genes expression in ‘BRCA Human Epidermal Growth Factor Receptor 2 (HER2)-positive’ tumor samples and ‘BRCA HER2-negative’ tumor samples, revealed significant differences in the expression levels of 8 HOX genes (Table S10). Interestingly, the expression level of HOXB13 in BRCA HER2-positive samples is~4-fold higher than its expression in HER2-negative samples.
A similar analysis performed for HOX genes expression in ‘BRCA Triple-negative’ tumor samples and ‘BRCA non-Triple-negative’ tumor samples revealed significant differences in the expression levels of 21 genes, yet all differences were less than 2-fold (Table S11).
3. Discussion
This work includes a comprehensive quantitative analysis of 14 cancer types providing an overview picture of HOX gene expression pattern in these cancers, using a consistent source of data (TCGA for tumor samples and GTEx for healthy samples). It includes at least 100 samples of every cancer type and highlights the expression differences between tumor and healthy samples.
The results show that differential expression of HOX gene clusters can discriminate between tumor samples and healthy samples (Figures S2–S13). In all analyzed cancer types, there were several HOX genes that demonstrated expression change of 2-fold or higher between healthy and tumor tissue. These results support the hypothesis raised by Bhatlekar et al. [1] that there may be HOX-related regulatory networks that become dysregulated during cancer development.
By and large, our findings agree with previous reports about the roles specific HOX genes play in cancers. However, we highlighted the involvement of HOX genes and gene pairs that were not previously implicated in cancer. There are also cases where our findings do not support previous reports, for example the involvement of several HOX genes in PRAD mentioned in [1], which we did not observe. It is clear that different studies (including ours) may have their own pitfalls and limitations, such as those discussed in a recently published study focusing on HOX and three amino acids loop extension (TALE) homeodomain transcription factors expression in cancer [33] that may stem from the amount of samples included in the analyses, the heterogeneity of the samples and the analyses methodology. However, our systematic and comprehensive analysis, implementing the same analysis method on all cancer types, provides a better global overview of the role of HOX gene expression in these cancers.
While the observed expression changes in HOX genes were both upregulation and downregulation, in the majority of cancer types the significant expression changes were towards upregulated expression. The analysis showed that in GBM, most of the HOX genes were differentially expressed. This can be attributed to the fact that HOX genes are hardly expressed in normal brain tissue (Figure S14). Thus, we suggest that in tumor tissues there is a change in a “master regulator pathway” that controls HOX genes expression and limits their expression in healthy tissues. The HOX genes belong to homeodomain TF group. Notably, in the comparison of their expression pattern to the expression pattern of other TF groups in GBM tumor tissue and healthy tissue, it was observed that unlike the HOX genes, most of the TF belonging to other TF groups, such as bZIP and Nuclear Receptors, are expressed in both tumor and healthy tissue to similar levels. We also observed that the expression level of HOX genes is higher in GBM samples than in LGG samples (Figure 3 and Figure 4, Figures S5 and S14). This observation could imply that in brain tissue, higher expression levels of HOX genes correlate with a more aggressive malignant tumor. Previous studies have shown that upregulation of different HOX genes can be used as gene signatures in glioblastoma [34,35,36]. However, it would be interesting to perform further analysis on samples from different Glioma stages, as additional supportive evidence could indicate that the expression levels of HOX genes may be used as a marker to determine the stage and progression of brain cancer.
Our analysis demonstrates that HOX genes are cooperatively involved in 6 different types of cancers. We showed which pairs of genes are co-up or -down regulated. The fact that in most of HOX gene pairs that demonstrate expression correlation both pair members belong to same cluster supports the hypothesis that they share a similar regulator. Yet, in order to better understand how HOX genes that are co-expressed influence tumor development, further mechanistic studies addressing their regulation are required.
HOX genes that undergo the most significant changes and also demonstrate significant correlations between gene expression and patients’ poor survival can be potential prognostic biomarkers. The genes marked in * bold in Table 2 and in Table S3 are those that met these 2 criteria. These genes were already suggested for consideration as prognostic biomarkers in previous studies (selected references are listed in Table S12 [34,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58]).
Interestingly, the comparison of the differential expression pattern of HOX genes between tumor and healthy tissue with some of the known prognostic markers that are also known to undergo genetic alterations and protein expression changes, showed that for most of these prognostic markers the expression change is less than 2-fold (the cutoff used in our analysis), and more than half of these genes do not demonstrate significant correlation between expression levels in tumor tissue and patients’ survival.
The importance of the cooperative effect of HOX genes is also demonstrated by our finding that specific pairs of HOX genes, whose expression levels are both high or low, can serve as better markers for survival than what can be predicted from each gene separately (Supplementary Materials File S1).
Most of the HOX genes that change expression in tumor tissues belong to the posterior HOX group. Since in most analyzed healthy tissues, the expression levels of posterior HOX genes are very low, one can speculate that posterior HOX genes have a bigger contribution to the development of cancer than anterior HOX genes.
Finally, apart from GBM, 4 of the cancer types for which a third or more of the HOX genes displayed altered gene expression (namely: ESCA, LUSC, PAAD, and STAD), originated from endodermally derived organs that are located in the foregut. Interestingly, these cancer types are known to be aggressive with low survival rates [50].
4. Materials and Methods
4.1. Data Downloads
The source of expression data files used in this analysis originated from UCSC Xena [59]. The analyzed data included gene expression data of tumor samples from the cancer genome atlas (TCGA) and gene expression data of healthy samples from Genotype-Tissue Expression (GTEx) downloaded from UCSC Xena data hubs [60]. Specifically, the data used in the analysis of differential HOX gene expression in different cancer types were obtained from the ‘UCSC Toil RNAseq Recompute’ data hub. Under this data hub, from “TCGA TARGET GTEx” cohort, the RSEM_norm_count file was downloaded from the “gene expression RNAseq” section, and the TCGA_GTEX_main_categories file was downloaded from the “phenotype” section. For the differential expression analysis of HOX genes, the samples from TCGA and GTEx were selected.
A separate analysis was performed in order to compare the expression of randomly selected genes in breast cancer patients. The expression data for this analysis included breast cancer samples from both tumor and healthy tissues obtained from the TCGA hub. The IlluminaHiSeq file was downloaded from the TCGA data hub, under the “TCGA Breast Cancer (BRCA)” cohort, and under the “gene expression RNAseq” section.
The list of housekeeping genes was downloaded from Reference [19].
The list of human transcription factor genes was downloaded from [20].
Clinical data for BRCA tumor samples was downloaded from the ‘Phenotypes TCGA hub’ located under UCSC Xena, ‘TCGA Breast Cancer (BRCA)’ cohort.
4.2. Association of Samples to Cancer Types
Each sample in the downloaded data was identified by a unique ID and categorized by tissue site and primary disease type in the case of tumor samples, or tissue site and tissue type in the case of healthy samples. The TCGA cohort included tumor samples belonging to 33 different cancer types and very few samples taken from healthy tissue. In this analysis only TCGA tumor samples were used, i.e., the few TCGA normal samples were removed. The GTEx cohort included samples from 54 different types of healthy tissues. The tissue categories in the TCGA cohort were slightly different from the tissue categories in the GTEx cohort. In order to compare gene expression from tumor samples with the expression in the corresponding healthy tissues, a joint category table was built. The joint category table matched the TCGA tumor tissue categories with their corresponding GTEx categories of healthy tissues (Table S13) and assigned them to a joint category. Every category in the table represents a cancer type. Based on this table, the samples were divided to 18 files. Importantly, the analysis was only performed on cancer types for which there were at least 100 tumor samples and at least 100 healthy samples. Fourteen out of the 18 files of different cancer types met these criteria. The expression data included in this analysis was associated with tissues from the following organs: adrenal gland, brain, breast, colon, esophagus, blood cells (leukemia), liver, lung, pancreas, prostate, stomach, and thyroid. Table 1 lists the organs, the total number of TCGA samples, and the total number of GTEx samples included in the analysis.
4.3. Heatmaps and Data Processing
Heatmaps and dendograms were constructed with R statistics version 3.4.3, using heatmap3 package standard settings [61]. Average linkage two ways hierarchical clustering with Euclidean distance were used for the construction of heatmaps. Other data processing was performed using scripts written in python 2.7 [62]. Code for the analysis of this study is available at https://github.com/OritAdato/HoxAnalysis.
4.4. Comparison of Expression of Randomly Selected Genes Between Cancer Tissue and Healthy Tissue
This analysis was performed on normalized RNA-seq expression data (RSEM normalized count, log2(x + 1) transformed) of tumor and healthy tissue downloaded from two different UCSC Xena data hubs: TCGA hub and “Toil RNAseq Recompute” hub. In the differential expression analysis of the tissue samples downloaded from the TCGA hub, both tumor and healthy samples were from TCGA, while in the differential expression analysis of the tissue samples downloaded from “Toil RNAseq Recompute” hub, the tumor samples were from TCGA, and the healthy samples were from GTEx [63]. This analysis was performed for five tumors types for which at least 50 healthy samples were available in TCGA (BRCA, LIHC, LUAD, LUSC, and THCA).
To generate a null distribution for HOX gene sets, we randomly picked sets of 39 genes. For 1000 randomly selected sets of 39 genes, we compared the changes in gene expression levels between tumor and healthy samples. Every comparison using a random set of 39 genes was performed twice: once for comparing a cohort of tumor samples from TCGA with healthy samples from TCGA, and a second time for comparing the same TCGA tumor samples with healthy samples from matching tissues in GTEx. For every gene expression comparison, Wilcoxon rank-sum test was run to check whether expression of healthy samples differs from expression of tumor samples. A two-fold cutoff was used to define differential expression. The list of differentially expressed genes from the comparison between tumor samples and TCGA healthy samples (p-value < 0.05 (Bonferroni adjusted to n = 39) and expression change >2-fold), was compared with the list of the differentially expressed genes resulting from the comparison between tumor samples and GTEx healthy samples. We compared the number of genes that were unique to either gene list (i.e., genes that were not included in the intersection between the two lists).
4.5. Calculating Euclidean Distance Between Healthy and Tumor Samples
Using R statistics version 3.4.3, the average intra Euclidean distance within the healthy samples was calculated and compared with the average inter Euclidean distance between healthy samples and tumor samples. The comparisons were performed on tumor and healthy samples using Wilcoxon rank-sum test.
4.6. Verifying the Observation that Posterior HOX Genes are Expressed at Low Levels in Multiple Healthy Tissues
For every HOX gene, across all 14 analyzed healthy tissues, the mean expression level was calculated. As there are a total of 16 posterior HOX genes (namely, HOXA9, HOXA10, HOXA11, HOXA13, HOXB9, HOXB13, HOXC9, HOXC10, HOXC11, HOXC12, HOXC13, HOXD9, HOXD10, HOXD11, HOXD12, and HOXD13), as an empirical null distribution, the mean expression level of 1000 randomly selected 16 HOX genes was calculated and compared to the mean expression level of the 16 posterior HOX genes.
4.7. Kaplan-Meier Survival Analysis Based on Expression of HOX Genes
To check whether HOX genes that change expression between tumor and healthy samples demonstrate a correlation with poor survival, a Kaplan-Meier (KM) survival plot was created for every differentially expressed gene in every cancer type indicated in Table 1. The KM plots were generated using UCSC Xena browser based on TCGA tumor samples’ survival data included in ‘TCGA TARGET GTEX’ study. The reported p-values were corrected using Bonferroni correction for multiple-hypothesis test. For every analyzed gene, tumor samples were first divided to 2 groups based on the median expression. If two group analysis result was not significant, then an additional analysis was performed on 3 groups of samples divides based on expression: the upper third, middle third, and lower third. Lastly, if 3 group analysis was not significant, then a KM analysis on upper quartile and lower quartile was performed.
4.8. KM Survival Analysis Based on Expression of HOX Gene Pairs
To search for pairs of HOX genes that can predict prognosis of cancer patients better than each HOX separately, a KM survival analysis was performed for all combinations of HOX gene pairs, in every cancer type. For every gene in a pair, the samples were divided to two groups: the group of samples in which the gene expression is higher than the median and a group in which the gene expression is lower than the median. The KM analysis of each gene pair compared 2 groups of samples: the group created by intersection of the 2 groups of samples with expression higher than the median expression of every gene (marked in red in KM plots and in the risk tables below the plots; group size denoted as N1), and the group created by intersection between the samples with expression lower than the median expression of every gene (marked in blue in KM plots and in the risk tables below the plots; group size denoted as N2). In addition, a KM survival analysis was performed for each gene separately. For this single gene analysis, we took the N1 samples with the highest expression and the N2 samples with the lowest expression. The survival analysis of the pair of genes was then compared with the survival analysis of every one of the genes separately. We focused on gene pairs with KM-based p-value < 0.05 (Bonferroni-corrected for multiple gene pairs) and a p-value smaller than the p-value of the survival analysis of each of the two genes separately.
4.9. Comparison of Expression of Randomly Selected Sets of 39 House Keeping Genes and HOX Genes
For every cancer type, 1000 sets of 39 HK genes were randomly selected. The GTEx median expression level and the TCGA median expression level was calculated for every set and compared with the GTEx median expression level and TCGA median expression of the 39 HOX genes, respectively.
4.10. Analysis of HOX Genes Expression in BRCA HER2-Positive, BRCA HER2-Negative and BRCA Triple-Negative Samples
The clinical data information regarding HER2 status, Progesterone status, and Estrogen status was correlated to every BRCA tumor sample based on sample ID. Tumor samples with status NA or status different than ‘negative’ or ‘positive’ were excluded from the analysis. For every HOX gene, the statistical Wilcoxon rank-sum test was performed to compare the expression between BRCA HER2-negative tumor samples and BRCA HER2-positive tumor samples.
Samples that had a negative status indication for HER2, Progesterone, and Estrogen were marked as triple-negative. The statistical Wilcoxon rank-sum test was performed to compare expression between triple-negative BRCA tumor samples and non-triple-negative BRCA tumor samples.
5. Conclusions
This comprehensive and quantitative analysis of HOX gene expression in healthy human tissues and 14 different cancer types, provides a global picture of the HOX genes expression patterns in the analyzed cancer tissues. Importantly, the quantitative characterization of specific differentially expressed HOX genes highlights specific HOX genes and HOX gene pairs, which can serve as novel biomarkers to discriminate between healthy and tumor tissues. Furthermore, the identification of specific HOX genes that are differentially co-expressed in distinct cancer types can serve as a basis for future mechanistic studies, which would contribute to the understanding of their regulation in health and disease.
Acknowledgments
We thank Jim Kadonaga, Doron Ginsberg, Diana Ideses, Hadar Krap and Anna Sloutskin for critical reading of the manuscript. We thank Guy Zehavi for advice on matching of pathological categories in initial stages of the study.
Abbreviations
| Acronyms | Definition |
| ACC | Adrenocortical carcinoma |
| BRCA | Breast invasive carcinoma |
| COAD | Colon adenocarcinoma |
| ESCA | Esophageal carcinoma |
| GBM | Glioblastoma multiforme |
| GTEx | Genotype-Tissue Expression |
| HER2 | Human Epidermal Growth Factor Receptor 2 |
| HK | Housekeeping |
| HOX | Homeobox |
| KM | Kaplan-Meier |
| LAML | Acute Myeloid Leukemia |
| LGG | Brain lower grade glioma |
| LIHC | Liver hepatocellular carcinoma |
| LUAD | Lung adenocarcinoma |
| LUSC | Lung squamous cell carcinoma |
| PAAD | Pancreatic adenocarcinoma |
| PCPG | Pheochromocytoma and paraganglioma |
| PRAD | Prostate adenocarcinoma |
| RSEM | RNA-seq by Expectation Maximization |
| STAD | Stomach adenocarcinoma |
| TALE | Three Amino Acids Loop Extension |
| TCGA | The Cancer Genome Atla |
| THCA | Thyroid carcinoma |
| TF | Transcription Factor |
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6694/12/6/1572/s1, Figure S1: Differences in the number of differentially expressed genes between tumor and healthy cancer tissue samples from TCGA:TCGA as compared to TCGA:GTEx for HOX genes and random sets of genes for five cancer types for which TCGA contains at least 50 healthy samples, Figure S2: HOX gene expression in samples of healthy colon tissue and colon adenocarcinoma (COAD) tumor tissue, Figure S3: HOX gene expression in samples of healthy esophagus and esophageal carcinoma (ESCA) tumor tissue, Figure S4: HOX gene expression in samples of healthy blood tissue and acute meloid leukemia (LAML) tumor tissue, Figure S5: HOX gene expression in samples of healthy brain cortex tissue and tumor lower grade glioma (LGG) tissue, Figure S6: HOX gene expression in samples of healthy liver and liver hepatocellular carcinoma (LIHC) tumor tissue, Figure S7: HOX gene expression in samples of healthy lung tissue and lung adenocarcinoma (LUAD) tumor tissue, Figure S8: HOX gene expression in samples of healthy lung tissue and lung a squamous cell carcinoma (LUSC) tumor tissue, Figure S9: HOX gene expression in samples of healthy pancreas tissue and pancreatic adenocarcinoma (PAAD) tumor tissue, Figure S10: HOX gene expression in samples of healthy adrenal gland tissue and pheochromocytoma and paraganglioma (PCPG) tumor tissue, Figure S11: HOX gene expression in samples of healthy prostate tissue and prostate adenocarcinoma (PRAD) tumor tissue, Figure S12: HOX gene expression in samples of healthy stomach tissue and stomach adenocarcinoma (STAAD) tumor tissue, Figure S13: HOX gene expression in samples of healthy thyroid tissue and tumor thyroid carcinoma (THCA), Figure S14: HOX genes median expression obtained from GTEx or TCGA, categorized by cancer type, Figure S15: Expression correlation between HOXA10 and HOXB5 in samples of healthy esophagus and samples of esophageal carcinoma (ESCA) tumor tissue, Figure S16: Expression correlation between HOXA10 and HOXB6 in samples of healthy esophagus and samples of esophageal carcinoma (ESCA) tumor tissue, Figure S17: Expression correlation between HOXA10 and HOXB7 in samples of healthy esophagus and samples of esophageal carcinoma (ESCA) tumor tissue, Figure S18: Expression correlation between HOXB5 and HOXB6 in samples of healthy esophagus and samples of esophageal carcinoma (ESCA) tumor tissue, Figure S19: Expression correlation between HOXB5 and HOXB7 in samples of healthy esophagus and samples of esophageal carcinoma (ESCA) tumor tissue, Figure S20: Expression correlation between HOXB6 and HOXB7 in samples of healthy esophagus and samples of esophageal carcinoma (ESCA) tumor tissue, Figure S21: Expression correlation between HOXC10 and HOXC8 in samples of healthy esophagus and samples of esophageal carcinoma (ESCA) tumor tissue, Figure S22: Expression correlation between HOXA3 and HOXC10 in samples of in samples of healthy brain tissue and glioblastoma multiforme (GBM) tumor tissue, Figure S23: Expression correlation between HOXA10 and HOXC10 in samples of in samples of healthy brain tissue and glioblastoma multiforme (GBM) tumor tissue, Figure S24: Expression correlation between HOXB2 and HOXB3 in samples of in samples of healthy brain tissue and glioblastoma multiforme (GBM) tumor tissue, Figure S25: Expression correlation between HOXB4 and HOXB5 in samples of in samples of healthy brain tissue and glioblastoma multiforme (GBM) tumor tissue, Figure S26: Expression correlation between HOXB5 and HOXB6 in samples of in samples of healthy brain tissue and glioblastoma multiforme (GBM) tumor tissue, Figure S27: Expression correlation between HOXA3 and HOXA5 in samples of healthy blood tissue and acute meloid leukemia (LAML) tumor tissue, Figure S28: Expression correlation between HOXA10 and HOXA9 in samples of healthy blood tissue and acute meloid leukemia (LAML) tumor tissue, Figure S29: Expression correlation between HOXD3 and HOXD9 in samples of healthy liver tissue and liver hepatocellular carcinoma (LIHC) tumor tissue, Figure S30: Expression correlation between HOXD8 and HOXD9 in samples of healthy liver tissue and liver hepatocellular carcinoma (LIHC) tumor tissue, Figure S31: Expression correlation between HOXC8 and HOXC9 in samples of healthy lung tissue and lung squamous cell carcinoma (LUSC) tumor tissue, Figure S32: Expression correlation between HOXC6 and HOXC8 in samples of healthy stomach tissue and stomach adenocarcinoma (STAD) tumor tissue, Figure S33: Expression correlation between HOXC6 and HOXC9 in samples of healthy stomach tissue and stomach adenocarcinoma (STAD) tumor tissue, Figure S34: Differentially expressed HOX genes pairs that show moderate expression correlation categorized by HOX cluster, Figure S35: Differentially expressed HOX gene pairs that demonstrate moderate expression correlation, categorized by HOX group, Figures S36–S56:Differentially expressed HOX pairs that do not demonstrate expression correlation in healthy tissue (Pearson correlation coefficient <0.4) and demonstrate high correlation in tumor tissue (Pearson correlation coefficient >0.7), Figure S57: Median expression level of Homeodomain transcription factors (not including HOX genes) in healthy brain tissue and GBM tumor tissue, Figure S58: Median expression level of HOX genes in healthy brain tissue and GBM tumor tissue, Figure S59: Median expression level of bZIP transcription factors in healthy brain tissue and GBM tumor tissue, Figure S60: Median expression level of Nuclear Receptors transcription factors in healthy brain tissue and GBM tumor tissue, Table S1: Differences in the number of differentially expressed genes between tumor and healthy tissue samples from TCGA:TCGA as compared to TCGA:GTEx, Table S2: Altered expression of HOX genes categorized by HOX cluster and group, Table S3: Lowly expressed HOX genes that undergo a significant expression increase in cancer, Table S4: Differentially expressed HOX genes for which the KM graph show significant correlation between gene expression and patient’s survival, Table S5: HOX gene pairs demonstrating more significant KM correlation between gene expression and patient’s survival compared to the KM of single gene, by cancer type, Table S6: Differentially expressed housekeeping genes by cancer type, Table S7: Transcription Factor expression in brain healthy tissue and GBM tumor tissue, Table S8: Differential expression status* of prognostic markers previously proposed in literature, Table S9: Kaplan-Meier (KM) survival graphs of genes used as prognostic markers, Table S10: HOX gene expression in BRCA tumor samples HER2 negative versus HER2 positive, Table S11: HOX gene expression in BRCA tumor samples Triple-negative versus non-Triple-negative, Table S12: HOX genes previously marked as potential cancer biomarkers, Table S13: TCGA & GTEx detailed tissue category list, File 1: KM plots of 24 differentially expressed HOX gene pairs that can serve as better markers for survival than what can be predicted from each gene separately.
Author Contributions
Conceptualization, O.A., T.J.-G. and R.U; Formal analysis, O.A.; Methodology, O.A., Y.O., J.K., T.J.-G. and R.U.; Software, O.A.; Supervision, T.J.-G. and R.U.; Writing—original draft, O.A.; Writing—review & editing, O.A., Y.O, J.K., T.J.-G. and R.U. All authors have read and agreed to the published version of the manuscript.
Funding
Orit Adato is partially supported by the Mina and Everard Goodman Faculty of Life Sciences, Bar-Ilan University.
Conflicts of Interest
The authors declare that they have no competing interests.
Software Source Code
The scripts used in the analysis of this study are available under: htps://github.com/OritAdato/HoxAnalysis.
References
- 1.Bhatlekar S., Fields J.Z., Boman B.M. HOX genes and their role in the development of human cancers. J. Mol. Med. (Berl.) 2014;92:811–823. doi: 10.1007/s00109-014-1181-y. [DOI] [PubMed] [Google Scholar]
- 2.Deschamps J., Duboule D. Embryonic timing, axial stem cells, chromatin dynamics, and the Hox clock. Genes Dev. 2017;31:1406–1416. doi: 10.1101/gad.303123.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah N., Sukumar S. The Hox genes and their roles in oncogenesis. Nat. Rev. Cancer. 2010;10:361–371. doi: 10.1038/nrc2826. [DOI] [PubMed] [Google Scholar]
- 4.Bhatlekar S., Fields J.Z., Boman B.M. Role of HOX Genes in Stem Cell Differentiation and Cancer. Stem. Cells Int. 2018;2018:3569493. doi: 10.1155/2018/3569493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kamkar F., Xaymardan M., Asli N.S. Hox-Mediated Spatial and Temporal Coding of Stem Cells in Homeostasis and Neoplasia. Stem. Cells Dev. 2016;25:1282–1289. doi: 10.1089/scd.2015.0352. [DOI] [PubMed] [Google Scholar]
- 6.Seifert A., Werheid D.F., Knapp S.M., Tobiasch E. Role of Hox genes in stem cell differentiation. World J. Stem. Cells. 2015;7:583–595. doi: 10.4252/wjsc.v7.i3.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iimura T., Pourquie O. Hox genes in time and space during vertebrate body formation. Dev. Growth Differ. 2007;49:265–275. doi: 10.1111/j.1440-169X.2007.00928.x. [DOI] [PubMed] [Google Scholar]
- 8.Li B., Huang Q., Wei G.H. The Role of HOX Transcription Factors in Cancer Predisposition and Progression. Cancers. 2019;11:528. doi: 10.3390/cancers11040528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li L., Zhang X., Liu Q., Yin H., Diao Y., Zhang Z., Wang Y., Gao Y., Ren X., Li J., et al. Emerging role of HOX genes and their related long noncoding RNAs in lung cancer. Crit. Rev. Oncol. Hematol. 2019;139:1–6. doi: 10.1016/j.critrevonc.2019.04.019. [DOI] [PubMed] [Google Scholar]
- 10.Primon M., Hunter K.D., Pandha H.S., Morgan R. Kinase Regulation of HOX Transcription Factors. Cancers. 2019;11:508. doi: 10.3390/cancers11040508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith J., Zyoud A., Allegrucci C. A Case of Identity: HOX Genes in Normal and Cancer Stem Cells. Cancers. 2019;11:512. doi: 10.3390/cancers11040512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carithers L.J., Ardlie K., Barcus M., Branton P.A., Britton A., Buia S.A., Compton C.C., DeLuca D.S., Peter-Demchok J., Gelfand E.T., et al. A Novel Approach to High-Quality Postmortem Tissue Procurement: The GTEx Project. Biopreserv. Biobank. 2015;13:311–319. doi: 10.1089/bio.2015.0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barger C.J., Branick C., Chee L., Karpf A.R. Pan-Cancer Analyses Reveal Genomic Features of FOXM1 Overexpression in Cancer. Cancers. 2019;11:251. doi: 10.3390/cancers11020251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frost F.G., Cherukuri P.F., Milanovich S., Boerkoel C.F. Pan-cancer RNA-seq data stratifies tumours by some hallmarks of cancer. J. Cell Mol. Med. 2020;24:418–430. doi: 10.1111/jcmm.14746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.GTEx Consortium The Genotype-Tissue Expression (GTEx) project. Nat. Genet. 2013;45:580–585. doi: 10.1038/ng.2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takahashi Y., Hamada J., Murakawa K., Takada M., Tada M., Nogami I., Hayashi N., Nakamori S., Monden M., Miyamoto M., et al. Expression profiles of 39 HOX genes in normal human adult organs and anaplastic thyroid cancer cell lines by quantitative real-time RT-PCR system. Exp. Cell Res. 2004;293:144–153. doi: 10.1016/j.yexcr.2003.09.024. [DOI] [PubMed] [Google Scholar]
- 17.Akoglu H. User’s guide to correlation coefficients. Turk. J. Emerg. Med. 2018;18:91–93. doi: 10.1016/j.tjem.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.di Pietro M., Lao-Sirieix P., Boyle S., Cassidy A., Castillo D., Saadi A., Eskeland R., Fitzgerald R.C. Evidence for a functional role of epigenetically regulated midcluster HOXB genes in the development of Barrett esophagus. Proc. Natl. Acad. Sci. USA. 2012;109:9077–9082. doi: 10.1073/pnas.1116933109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eisenberg E., Levanon E.Y. Human housekeeping genes, revisited. Trends Genet. TIG. 2013;29:569–574. doi: 10.1016/j.tig.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 20.Lambert S.A., Jolma A., Campitelli L.F., Das P.K., Yin Y., Albu M., Chen X., Taipale J., Hughes T.R., Weirauch M.T. The Human Transcription Factors. [(accessed on 26 May 2020)];Cell. 2018 175:598–599. doi: 10.1016/j.cell.2018.09.045. Available online: http://humantfs.ccbr.utoronto.ca/ [DOI] [PubMed] [Google Scholar]
- 21.Assmar M., Yeganeh S., Mansourghanaei F., Amirmozafari N. Combined Evaluation of AFP, CA15-3, CA125, CA19-9, and CEA Tumor Markers in Patients with Hepatitis B and C. Iran. J. Public Health. 2016;45:1645–1651. [PMC free article] [PubMed] [Google Scholar]
- 22.Battaglin F., Naseem M., Puccini A., Lenz H.J. Molecular biomarkers in gastro-esophageal cancer: Recent developments, current trends and future directions. Cancer Cell Int. 2018;18:99. doi: 10.1186/s12935-018-0594-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dong Q., Li Q., Wang M., Hu J., Dai J., Niu L., Yuan G., Pan Y. Elevated CD44 expression predicts poor prognosis in patients with low-grade glioma. Oncol. Lett. 2019;18:3698–3704. doi: 10.3892/ol.2019.10728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Handschuh L. Not Only Mutations Matter: Molecular Picture of Acute Myeloid Leukemia Emerging from Transcriptome Studies. J. Oncol. 2019;2019:7239206. doi: 10.1155/2019/7239206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang F.L., Yu S.J. Esophageal cancer: Risk factors, genetic association, and treatment. Asian J. Surg. 2018;41:210–215. doi: 10.1016/j.asjsur.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 26.Loosen S.H., Neumann U.P., Trautwein C., Roderburg C., Luedde T. Current and future biomarkers for pancreatic adenocarcinoma. Tumour Biol. J. Int. Soc. Oncodev. Med. 2017;39:1010428317692231. doi: 10.1177/1010428317692231. [DOI] [PubMed] [Google Scholar]
- 27.Man J., Zhang X., Dong H., Li S., Yu X., Meng L., Gu X., Yan H., Cui J., Lai Y. Screening and identification of key biomarkers in lung squamous cell carcinoma by bioinformatics analysis. Oncol. Lett. 2019;18:5185–5196. doi: 10.3892/ol.2019.10873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Menyhart O., Nagy A., Gyorffy B. Determining consistent prognostic biomarkers of overall survival and vascular invasion in hepatocellular carcinoma. R. Soc. Open Sci. 2018;5:181006. doi: 10.1098/rsos.181006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nwosu Z.C., Megger D.A., Hammad S., Sitek B., Roessler S., Ebert M.P., Meyer C., Dooley S. Identification of the Consistently Altered Metabolic Targets in Human Hepatocellular Carcinoma. Cell. Mol. Gastroenterol. Hepatol. 2017;4:303–323. doi: 10.1016/j.jcmgh.2017.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sasmita A.O., Wong Y.P., Ling A.P.K. Biomarkers and therapeutic advances in glioblastoma multiforme. Asia-Pac. J. Clin. Oncol. 2018;14:40–51. doi: 10.1111/ajco.12756. [DOI] [PubMed] [Google Scholar]
- 31.Virgilio E., Proietti A., D’Urso R., Cardelli P., Giarnieri E., Montagnini M., Giovagnoli M.R., Mercantini P., Balducci G., Cavallini M. Measuring Intragastric Tumor Markers in Gastric Cancer Patients: A Systematic Literature Review on Significance and Reliability. Anticancer Res. 2017;37:2817–2821. doi: 10.21873/anticanres.11632. [DOI] [PubMed] [Google Scholar]
- 32.Wang F., Zheng Z., Guan J., Qi D., Zhou S., Shen X., Wang F., Wenkert D., Kirmani B., Solouki T., et al. Identification of a panel of genes as a prognostic biomarker for glioblastoma. EBioMedicine. 2018;37:68–77. doi: 10.1016/j.ebiom.2018.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jia Y., Bleicher F., Merabet S. A systematic survey of HOX and TALE expression profiling in human cancers. Int. J. Dev. Biol. 2018;62:865–876. doi: 10.1387/ijdb.180286fb. [DOI] [PubMed] [Google Scholar]
- 34.Abdel-Fattah R., Xiao A., Bomgardner D., Pease C.S., Lopes M.B., Hussaini I.M. Differential expression of HOX genes in neoplastic and non-neoplastic human astrocytes. J. Pathol. 2006;209:15–24. doi: 10.1002/path.1939. [DOI] [PubMed] [Google Scholar]
- 35.Costa B.M., Smith J.S., Chen Y., Chen J., Phillips H.S., Aldape K.D., Zardo G., Nigro J., James C.D., Fridlyand J., et al. Reversing HOXA9 oncogene activation by PI3K inhibition: Epigenetic mechanism and prognostic significance in human glioblastoma. Cancer Res. 2010;70:453–462. doi: 10.1158/0008-5472.CAN-09-2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gallo M., Ho J., Coutinho F.J., Vanner R., Lee L., Head R., Ling E.K., Clarke I.D., Dirks P.B. A tumorigenic MLL-homeobox network in human glioblastoma stem cells. Cancer Res. 2013;73:417–427. doi: 10.1158/0008-5472.CAN-12-1881. [DOI] [PubMed] [Google Scholar]
- 37.Cai Y.D., Zhang S., Zhang Y.H., Pan X., Feng K., Chen L., Huang T., Kong X. Identification of the Gene Expression Rules That Define the Subtypes in Glioma. J. Clin. Med. 2018;7:350. doi: 10.3390/jcm7100350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cheng Y., Jutooru I., Chadalapaka G., Corton J.C., Safe S. The long non-coding RNA HOTTIP enhances pancreatic cancer cell proliferation, survival and migration. Oncotarget. 2015;6:10840–10852. doi: 10.18632/oncotarget.3450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Deng Y., He R., Zhang R., Gan B., Zhang Y., Chen G., Hu X. The expression of HOXA13 in lung adenocarcinoma and its clinical significance: A study based on The Cancer Genome Atlas, Oncomine and reverse transcription-quantitative polymerase chain reaction. Oncol. Lett. 2018;15:8556–8572. doi: 10.3892/ol.2018.8381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dong C.Y., Cui J., Li D.H., Li Q., Hong X.Y. HOXA10AS: A novel oncogenic long noncoding RNA in glioma. Oncol. Rep. 2018;40:2573–2583. doi: 10.3892/or.2018.6662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Drabkin H.A., Parsy C., Ferguson K., Guilhot F., Lacotte L., Roy L., Zeng C., Baron A., Hunger S.P., Varella-Garcia M., et al. Quantitative HOX expression in chromosomally defined subsets of acute myelogenous leukemia. Leukemia. 2002;16:186–195. doi: 10.1038/sj.leu.2402354. [DOI] [PubMed] [Google Scholar]
- 42.Duan R., Han L., Wang Q., Wei J., Chen L., Zhang J., Kang C., Wang L. HOXA13 is a potential GBM diagnostic marker and promotes glioma invasion by activating the Wnt and TGF-beta pathways. Oncotarget. 2015;6:27778–27793. doi: 10.18632/oncotarget.4813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eoh K.J., Kim H.J., Lee J.Y., Nam E.J., Kim S., Kim S.W., Kim Y.T. Upregulation of homeobox gene is correlated with poor survival outcomes in cervical cancer. Oncotarget. 2017;8:84396–84402. doi: 10.18632/oncotarget.21041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fischbach N.A., Rozenfeld S., Shen W., Fong S., Chrobak D., Ginzinger D., Kogan S.C., Radhakrishnan A., Le Beau M.M., Largman C., et al. HOXB6 overexpression in murine bone marrow immortalizes a myelomonocytic precursor in vitro and causes hematopoietic stem cell expansion and acute myeloid leukemia in vivo. Blood. 2005;105:1456–1466. doi: 10.1182/blood-2004-04-1583. [DOI] [PubMed] [Google Scholar]
- 45.Giampaolo A., Felli N., Diverio D., Morsilli O., Samoggia P., Breccia M., Lo Coco F., Peschle C., Testa U. Expression pattern of HOXB6 homeobox gene in myelomonocytic differentiation and acute myeloid leukemia. Leukemia. 2002;16:1293–1301. doi: 10.1038/sj.leu.2402532. [DOI] [PubMed] [Google Scholar]
- 46.Guo Y., Peng Y., Gao D., Zhang M., Yang W., Linghu E., Herman J.G., Fuks F., Dong G., Guo M. Silencing HOXD10 by promoter region hypermethylation activates ERK signaling in hepatocellular carcinoma. Clin. Epigenetics. 2017;9:116. doi: 10.1186/s13148-017-0412-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huo X.Y., Zhang X.Y., Yuan F., Zhao X.Y., You B.A. HOXB7 promotes proliferation and metastasis of glioma by regulating the Wnt/beta-catenin pathway. Eur. Rev. Med. Pharmacol. Sci. 2019;23:2476–2485. doi: 10.26355/eurrev_201903_17395. [DOI] [PubMed] [Google Scholar]
- 48.Kang J.U. Characterization of amplification patterns and target genes on the short arm of chromosome 7 in early-stage lung adenocarcinoma. Mol. Med. Rep. 2013;8:1373–1378. doi: 10.3892/mmr.2013.1686. [DOI] [PubMed] [Google Scholar]
- 49.Li B., McCrudden C.M., Yuen H.F., Xi X., Lyu P., Chan K.W., Zhang S.D., Kwok H.F. CD133 in brain tumor: The prognostic factor. Oncotarget. 2017;8:11144–11159. doi: 10.18632/oncotarget.14406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li Z., Zhao X., Zhou Y., Liu Y., Zhou Q., Ye H., Wang Y., Zeng J., Song Y., Gao W., et al. The long non-coding RNA HOTTIP promotes progression and gemcitabine resistance by regulating HOXA13 in pancreatic cancer. J. Transl. Med. 2015;13:84. doi: 10.1186/s12967-015-0442-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Long J., Zhang L., Wan X., Lin J., Bai Y., Xu W., Xiong J., Zhao H. A four-gene-based prognostic model predicts overall survival in patients with hepatocellular carcinoma. J. Cell Mol. Med. 2018;22:5928–5938. doi: 10.1111/jcmm.13863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shah N., Jin K., Cruz L.A., Park S., Sadik H., Cho S., Goswami C.P., Nakshatri H., Gupta R., Chang H.Y., et al. HOXB13 mediates tamoxifen resistance and invasiveness in human breast cancer by suppressing ERalpha and inducing IL-6 expression. Cancer Res. 2013;73:5449–5458. doi: 10.1158/0008-5472.CAN-13-1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Starkova J., Zamostna B., Mejstrikova E., Krejci R., Drabkin H.A., Trka J. HOX gene expression in phenotypic and genotypic subgroups and low HOXA gene expression as an adverse prognostic factor in pediatric ALL. Pediatr. Blood Cancer. 2010;55:1072–1082. doi: 10.1002/pbc.22749. [DOI] [PubMed] [Google Scholar]
- 54.Sui B.Q., Zhang C.D., Liu J.C., Wang L., Dai D.Q. HOXB13 expression and promoter methylation as a candidate biomarker in gastric cancer. Oncol. Lett. 2018;15:8833–8840. doi: 10.3892/ol.2018.8371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tang X.L., Ding B.X., Hua Y., Chen H., Wu T., Chen Z.Q., Yuan C.H. HOXC10 Promotes the Metastasis of Human Lung Adenocarcinoma and Indicates Poor Survival Outcome. Front. Physiol. 2017;8:557. doi: 10.3389/fphys.2017.00557. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 56.Zhan J., Wang P., Li S., Song J., He H., Wang Y., Liu Z., Wang F., Bai H., Fang W., et al. HOXB13 networking with ABCG1/EZH2/Slug mediates metastasis and confers resistance to cisplatin in lung adenocarcinoma patients. Theranostics. 2019;9:2084–2099. doi: 10.7150/thno.29463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhan J., Wang P., Niu M., Wang Y., Zhu X., Guo Y., Zhang H. High expression of transcriptional factor HoxB9 predicts poor prognosis in patients with lung adenocarcinoma. Histopathology. 2015;66:955–965. doi: 10.1111/his.12585. [DOI] [PubMed] [Google Scholar]
- 58.Lv X., Li L., Lv L., Qu X., Jin S., Li K., Deng X., Cheng L., He H., Dong L. HOXD9 promotes epithelial-mesenchymal transition and cancer metastasis by ZEB1 regulation in hepatocellular carcinoma. J. Exp. Clin. Cancer Res. 2015;34:133. doi: 10.1186/s13046-015-0245-3. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 59.Goldman M., Craft B., Hastie M., Repečka K., McDade F., Kamath A., Banerjee A., Luo Y., Rogers D., Brooks A.N., et al. The UCSC Xena platform for public and private cancer genomics data visualization and interpretation. [(accessed on 26 May 2020)];bioRxiv. 2019 :326470. doi: 10.1038/s41587-020-0546-8. Available online: https://xena.ucsc.edu/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vivian J., Rao A.A., Nothaft F.A., Ketchum C., Armstrong J., Novak A., Pfeil J., Narkizian J., Deran A.D., Musselman-Brown A., et al. Toil enables reproducible, open source, big biomedical data analyses. Nat. Biotechnol. 2017;35:314–316. doi: 10.1038/nbt.3772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhao S., Guo Y., Sheng Q., Shyr Y. Advanced heat map and clustering analysis using heatmap3. BioMed Res. Int. 2014;2014:986048. doi: 10.1155/2014/986048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.van Rossum G. Python Tutorial, Technical Report CS-R9526. Centrum voor Wiskunde en Informatica (CWI); Amsterdam, The Netherlands: 1995. [Google Scholar]
- 63.GTEx Consortium Human genomics. The Genotype-Tissue Expression (GTEx) pilot analysis: Multitissue gene regulation in humans. Science. 2015;348:648–660. doi: 10.1126/science.1262110. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.