Abstract
Signet ring cell adenocarcinomas (SRCCs) are a rare histological subtype of adenocarcinomas with a poor prognosis, typically due to advanced disease at diagnosis. A signet ring cell, mimicking its moniker, contains abundant intracytoplasmic mucin that pushes the nucleus to the periphery. In these cancers, this cell feature comprises more than 50% of the tumor. Despite predilection for the gastrointestinal tract, and in particular the stomach, primary SRCCs are also described in other sites, typically in case reports. This literature, however, lacks a standardized overview of the SRCC disease entity. Using a retrospective cohort approach, we summarize the clinicodemographic and mortality outcomes of SRCCs in thirteen primary sites, comprising 95% of all SRCCs in the Surveillance, Epidemiology, and End Results Program (SEER), a population-level cancer database covering nearly one-third of the United States population. SRCCs general trends compared to matching nonvariant adenocarcinomas are earlier age of onset, with initial presentation favoring higher rates of regional or distant disease presentation and poor tumor differentiation. After multivariable analysis, SRCCs typically have worse overall survivals, but substantial variances exist depending on tumor location. Identifying SRCCs at earlier disease stages is likely the single most important intervention to improving outcomes for these patients.
Keywords: diffuse type, CDH1, E-cadherin, histopathology, chemotherapy, radiotherapy, surgery, cancer
1. Introduction—Overview of Signet Ring Cell Adenocarcinomas
Signet ring cell adenocarcinomas (SRCCs) have been described in the literature since the 1950s, with most initial papers describing these cancers in the colon and urinary bladder [1,2]. Histologically, these cancers have the appearance of a signet ring. A signet ring has a flattened surface at the top of the ring with an engraved or raised symbol, historically used to stamp a seal into correspondence. Comparatively, these cells acquire a signet cell morphology due to accumulation of abundant mucin in cytoplasm, leading to nuclei dislocation to the periphery [3] (Figure 1). Formally, a cancer is labelled a SRCC if greater than 50% of tumor cells show prominent intracytoplasmic mucin and an eccentrically placed crescent-shaped nucleus [4], whereas adenocarcinomas with less than 50% signet ring cells are classified as “adenocarcinomas with a signet ring cell component” [5]. SRCCs are distinct from mucinous adenocarcinomas in that in the latter greater than 50% of the tumor consists of extracellular mucin [5].
Figure 1.
(a) Representative histological slide of poorly differentiated conventional gastric adenocarcinoma. (b) Representative histological slide of gastric signet adenocarcinoma, illustrating mucin-filled cytoplasm with nucleus pushed to the periphery. Figures sourced from Wikimedia Commons, public domain [6,7].
The systematic study of these cancers is limited due to the rarity of this histological diagnosis. For gastric cancers, the World Health Organization (WHO) classification lists SRCCs under the category of diffuse or poorly cohesive carcinomas, which is divided into SRCCs and other poorly cohesive carcinomas [5,8]. For colorectal cancers, SRCCs are a recognized histological subtype of adenocarcinomas if they meet the definition as described previously [2]. For other cancer sites, SRCCs are extremely rare (typically less than 0.5% of diagnoses). Hence for these sites, SRCCs are described as patterns rather than subtypes as there is limited evidence as to the clinical relevance [5]. Nevertheless, cancers with SRCC morphology are recognized by the International Classification of Diseases for Oncology (ICD)-0-3 classification as a unique entry (8490/3) under the larger umbrella of Cystic, Mucinous and Serous Neoplasms [9].
The ability to characterize rare cancers requires collective input of small numbers of cases from individual institutions into registries that cover large populations. With sufficient subsequent analytical power, this enables researchers to make meaningful conclusions beyond that provided in case reports or case series studies. Most of our knowledge about the demographics and prognosis of SRCCs comes from the summaries of population-level registries of gastric and colon cancers [10,11], with supplementation from case series on SRCCs from other sites. However, there is no study that systematically and robustly compares SRCCs by site to matching nonvariant cases.
The Surveillance, Epidemiology, and End Results (SEER) database is a population-based cancer registry managed by the National Cancer Institute, currently encompassing about one-third of the United States with near universal capture of cases as regional registries were added to the program since 1975 [12]. It has become an invaluable resource for enumerating histopathological data with survival and mortality data across all cancer sites, demographics, and time [13]. In this retrospective site-stratified analysis, we overcome the limitations imposed by the overall low incidence of SRCCs across tumor sites by investigating their clinicopathological characteristics and survival outcomes comparable to all other cancers by site, with subgroup analysis to major nonvariant types using the SEER database. These findings will provide a more through epidemiological description and quantification of this poorly characterized rare cancer entity with a historically poor prognosis.
2. Analysis of Signet Ring Cell Adenocarcinomas by Site
Subsections are presented in order of the percentage of SRCC cases relative to all cases of SRCC (Figure 2). First presented within each subsection is a demographics table with all included cases of cancers for that site, followed by the most common nonvariant histological type(s), and then SRCC cases. The second table presents both univariate and multivariable analyses for cause-specific mortality according the same demographic, histopathological, and treatment variables as the first table. Here, we present the hazard ratios for signet ring cell cancers compared to all other non-signet ring cell cancers within the site of interest. We then provide a sub-analysis of nonvariant histological type(s) to signet ring cell cancers to provide a representative comparator of risk to common cancer types within each site.
Figure 2.
(a) Distribution of signet ring cell tumors in SEER, 1975–2016, total of 41,847 cases. (b) Distribution of all solid (non-blood borne), non-signet ring cell tumors in SEER, 1975–2016, total of 9.56 million cases. In both plots data labels are percentages. Markers omitted if less than 1%.
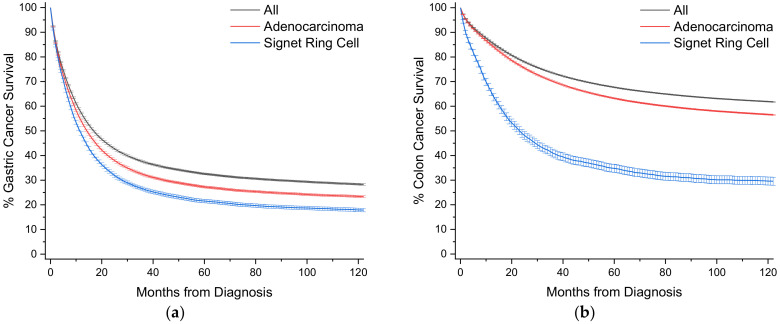
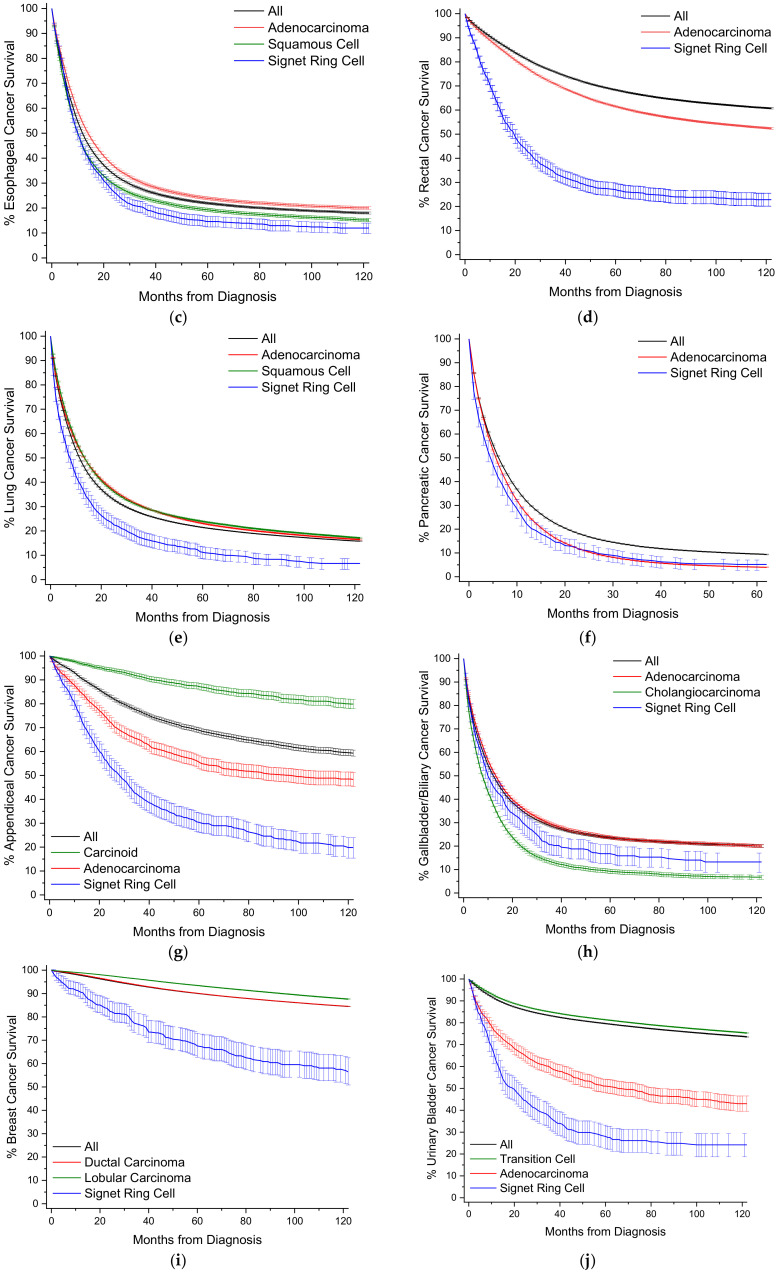
To provide a visual overview across all cancer sites, Kaplan-Meier survival curves with 95% confidence intervals are also presented (Figure 3).
Figure 3.
Kaplan-Meier survival curves. All survivor functions are shown with 95% confidence intervals. (a) Gastric cancer. (b) Colon cancer. (c) Esophageal cancer. (d) Rectal cancer. (e) Lung cancer. (f) Pancreatic cancer. (g) Appendiceal cancer. (h) Gallbladder/Biliary cancer. (i) Breast cancer. (j) Urinary Bladder cancer. (k) Small Bowel cancer. (l) Ovarian cancer. (m) Prostate cancer. In these curves, “All” represents the curves for all cancers within that site, with subtypes shown as labelled.
2.1. Gastric
SRCCs comprise 16.8% of all cases of gastric cancer, and nearly 57% of all SRCC cases (Table 1, Figure 2). When compared to nonvariant adenocarcinomas, SRCCs have an earlier mean age of onset of 6.6 years. The proportion of female cases increases from 34.4% to 48.0% for SRCCs compared to adenocarcinomas where two-thirds of cases occur in males. These cancers are most often detected at a distant or metastatic stage (43.0% vs. 37.3%) with a poor tumor grade (75.4% vs. 52.1%). Surgical and radiotherapy trends are similar in both groups, while SRCC patients are more often treated with chemotherapy (49.5% vs. 41.4%). Survival is significantly worse at all time points for SRCC patients, with 5- and 10-year survival at 19.2% vs. 25.8% and 16.0% vs. 22.1%, respectively (Figure 3a, Table 1). Median survival time is 10.2 months compared to 13.5 months for adenocarcinomas. When compared to all other gastric cancers, SRCCs have a hazard ratio (HR) of 1.23 (95% CI: 1.21–1.26), and 1.11 (95% CI: 1.08–1.13) to adenocarcinomas, after multivariate analyses (Table 2).
Table 1.
Baseline demographics and clinical characteristics by histology for gastric cancers.
| Gastric | All | Adenocarcinoma | Signet Ring |
|---|---|---|---|
| N (%) | 106,972 (100) | 65,218 (61.0) | 17,942 (16.8) |
| Age (Years) (%) | |||
| 0–14 | 38 (<0.1) | 3 (<0.1) | 4 (<0.1) |
| 15–29 | 858 (0.8) | 338 (0.5) | 283 (1.6) |
| 30–49 | 12,374 (11.6) | 5688 (8.7) | 3711 (20.7) |
| 50–69 | 43,379 (40.6) | 25,731 (39.5) | 7847 (43.7) |
| 70–85 | 39,088 (36.5) | 25,902 (39.7) | 4996 (27.8) |
| >85 | 11,235 (10.5) | 7556 (11.6) | 1101 (6.1) |
| Mean (SD) | 67.0 (14.4) | 68.6 (13.7) | 61.9 (15.3) |
| Gender (%) | |||
| Male | 64,729 (60.5) | 42,788 (65.6) | 9334 (52.0) |
| Female | 42,243 (39.5) | 22,430 (34.4) | 8608 (48.0) |
| Race (%) | |||
| White | 75,037 (70.1) | 45,689 (70.1) | 12,602 (70.2) |
| Black | 14,627 (13.7) | 8467 (13.0) | 2199 (12.3) |
| Other | 17,308 (16.2) | 11,062 (17.0) | 3141 (17.5) |
| Detection Stage (%) | |||
| In Situ | 1021 (1.0) | 475 (0.7) | 6 (<0.1) |
| Localized | 27,653 (25.9) | 14,922 (22.9) | 3256 (18.1) |
| Regional | 28,402 (26.6) | 18,989 (29.1) | 5586 (31.1) |
| Distant | 38,065 (35.6) | 24,333 (37.3) | 7707 (43.0) |
| Unstaged | 11,831 (11.1) | 6499 (10.0) | 1387 (7.7) |
| Grade Differentiation (%) | |||
| Well | 5762 (5.4) | 2903 (4.5) | 57 (0.3) |
| Moderate | 21,817 (20.4) | 18,465 (28.3) | 405 (2.3) |
| Poor | 52,910 (49.5) | 34,003 (52.1) | 13,531 (75.4) |
| Undifferentiated | 2524 (2.4) | 1015 (1.6) | 486 (2.7) |
| Unknown | 23,959 (22.4) | 8832 (13.5) | 3463 (19.3) |
| Surgery (%) | |||
| Yes | 56,058 (52.4) | 33,371 (51.2) * | 9088 (50.7) * |
| No | 50,914 (47.6) | 31,847 (48.8) * | 8854 (49.3) * |
| Radiotherapy (%) | |||
| Yes | 21,836 (20.4) | 15,520 (23.8) | 3949 (22.0) |
| No | 85,136 (79.6) | 49,698 (76.2) | 13,993 (78.0) |
| Chemotherapy (%) | |||
| Yes | 42,224 (39.5) | 26,979 (41.4) | 8896 (49.5) |
| No | 64,748 (60.5) | 38,239 (58.6) | 9056 (50.5) |
| Incidence Rate (95% CI) | |||
| All | 7.57 (7.53–7.62) | 4.50 (4.47–4.54) | 1.24 (1.22–1.26) |
| Male | 10.4 (10.3–10.5) | 6.79 (6.72–6.86) | 1.42 (1.39–1.45) |
| Female | 5.37 (5.32–5.43) | 2.71 (2.68–2.75) | 1.11 (1.08–1.13) |
| CSS % (95% CI) | |||
| 1-year | 55.7 (55.3–56.0) | 52.9 (52.4–53.3) | 45.8 (44.9–46.7) |
| 2-year | 41.7 (41.3–42.0) | 37.1 (36.7–37.6) | 30.0 (29.1–30.8) |
| 5-year | 31.1 (30.8–31.5) | 25.8 (25.4–26.2) | 19.2 (18.4–20.0) |
| 10-year | 27.0 (26.6–27.4) | 22.1 (21.6–22.5) | 16.0 (15.2–15.7) |
| Median (Months) | 15.6 | 13.5 | 10.2 |
| RS % (95% CI) | |||
| 1-year | 53.7 (53.4–54.1) | 51.0 (50.5–51.4) | 44.3 (43.2–45.2) |
| 2-year | 39.8 (39.4–40.1) | 35.3 (34.9–35.8) | 28.4 (27.6–29.2) |
| 5-year | 29.1 (28.7–29.5) | 24.0 (23.5–24.4) | 17.9 (17.1–18.6) |
| 10-year | 24.1 (23.6–24.6) | 19.3 (18.8–19.9) | 14.2 (13.3–15.1) |
| Median (Months) | 14.2 | 12.5 | 9.7 |
p < 0.05 for all comparisons between adenocarcinoma and signet ring cell comparisons, unless noted by * p ≥ 0.05. Incidence rates expressed per 100,000. CSS, cause-specific survival; RS, relative survival; CI, confidence interval.
Table 2.
Derived univariate and multivariable Cox-proportional hazard ratios (HR) of mortality for gastric cancers.
| Gastric | Signet Ring vs. Non-Signet Ring | Signet Ring vs. Adenocarcinoma | ||
|---|---|---|---|---|
| HR (95% CI) | Univariate | Multivariable | Univariate | Multivariable |
| Signet Ring Histology | 1.38 (1.36–1.41) | 1.23 (1.21–1.26) | 1.16 (1.14–1.19) | 1.11 (1.08–1.13) |
| Age (per 10 years) | 1.092 (1.085–1.098) | 1.142 (1.134–1.149) | 1.048 (1.041–1.054) | 1.095 (1.087–1.102) |
| Gender (Female) | 0.88 (0.87–0.90) | 0.91 (0.89–0.92) | 1.01 (0.99–1.03) * | 0.96 (0.95–0.98) |
| Race | ||||
| Black | 0.94 (0.92–0.96) | 1.01 (0.99–1.04) * | 0.99 (0.96–1.01) * | 1.01 (0.99–1.04) * |
| Other | 0.81 (0.79–0.83) | 0.86 (0.84–0.88) | 0.74 (0.72–0.76) | 0.82 (0.80–0.84) |
| Detection Stage | ||||
| In Situ | 0.40 (0.34–0.48) | 0.38 (0.32–0.46) | 0.36 (0.28–0.45) | 0.29 (0.23–0.37) |
| Regional | 2.79 (2.72–2.86) | 3.01 (2.93–3.09) | 2.13 (2.07–2.19) | 2.63 (2.56–2.72) |
| Distant | 7.13 (6.95–7.31) | 5.62 (5.46–5.78) | 5.75 (5.59–5.91) | 4.95 (4.80–5.12) |
| Unstaged | 3.68 (3.56–3.80) | 2.23 (2.15–2.31) | 3.69 (3.55–3.83) | 2.17 (2.09–2.26) |
| Grade Differentiation | ||||
| Moderate | 2.60 (2.46–2.75) | 1.86 (1.76–1.97) | 1.61 (1.51–1.71) | 1.28 (1.20–1.36) |
| Poor | 3.83 (3.64–4.04) | 2.44 (2.31–2.57) | 2.23 (2.11–2.36) | 1.69 (1.59–1.79) |
| Undifferentiated | 3.42 (3.19–3.68) | 2.40 (2.23–2.58) | 2.22 (2.04–2.41) | 1.80 (1.66–1.96) |
| Unknown | 2.47 (2.34–2.61) | 1.57 (1.49–1.66) | 2.55 (2.40–2.71) | 1.49 (1.40–1.58) |
| Surgery (Yes) | 0.316 (0.311–0.321) | 0.409 (0.401–0.418) | 0.315 (0.309–0.320) | 0.417 (0.408–0.427) |
| Radiotherapy (Yes) | 1.01 (0.99–1.03) * | 1.02 (1.00–1.04) * | 0.81 (0.80–0.83) | 0.98 (0.95–1.00) |
| Chemotherapy (Yes) | 1.26 (1.24–1.28) | 0.66 (0.65–0.68) | 1.05 (1.03–1.07) | 0.63 (0.61–0.64) |
p < 0.05 relative to reference unless noted by * p ≥ 0.05. Reference categories: Gender (Male), Race (White), Detection Stage (Localized), Grade differentiation (Well), Surgery (No), Radiotherapy (No), and Chemotherapy (No). CI, confidence interval.
2.2. Colon
Colon cancers are analyzed separately from cancers arising from the appendix and rectum (Section 2.4 and Section 2.7). Carcinoids rather than nonvariant adenocarcinomas are the most common cancer subtype in the appendix, and rectal cancer is heavily treated with radiotherapy, unlike colon cancers. SRCCs comprise 1.0% of all cases of colon cancer, and 15.3% of all SRCC cases (Table 3, Figure 2). When compared to nonvariant adenocarcinomas, SRCCs have an earlier mean age of onset of 3.5 years, compared to 6.6 years for gastric SRCCs. Unlike gastric SRCCs, there is no gender bias towards females, but like gastric SRCCs, these cancers are most often detected at a distant or metastatic stage (40.6% vs. 23.8%) with a poor tumor grade (68.5% vs. 18.5%). SRCC patients receive chemotherapy more often (47.4% vs. 33.6%), although chemotherapy uptake appears low despite most cancers presenting at stages regional and greater. Colon SRCC patients have worse overall survival relative to comparative nonvariant cancers, with 5- and 10-year survival at 33.6% vs. 61.8% and 28.6% vs. 55.0%, respectively (Figure 3b, Table 3). Median survival time is only 21.6 months compared to more than 10 years for adenocarcinomas. When compared to all other colon cancers, SRCCs have a HR of 1.45 (95% CI: 1.40–1.51), and 1.47 (95% CI: 1.41–1.53) to adenocarcinomas, after multivariate analyses (Table 4).
Table 3.
Baseline demographics and clinical characteristics by histology for colon cancers.
| Colon | All | Adenocarcinoma | Signet Ring |
|---|---|---|---|
| N | 448,221 (100) | 283,919 (63.3) | 4586 (1.0) |
| Age (Years) (%) | |||
| 0–14 | 32 (<0.1) | 6 (<0.1) | 10 (0.2) |
| 15–29 | 1930 (0.4) | 1066 (0.4) | 140 (3.1) |
| 30–49 | 38,386 (8.6) | 24,725 (8.7) | 649 (14.2) |
| 50–69 | 182,891 (40.8) | 113,023 (39.8) | 1730 (37.7) |
| 70–85 | 172,601 (38.5) | 111,469 (39.3) | 1582 (34.5) |
| >85 | 52,381 (11.7) | 33,630 (11.8) | 475 (10.4) |
| Mean (SD) | 68.4 (13.6) | 68.7 (13.6) | 65.2 (16.4) |
| Gender (%) | |||
| Male | 220,451 (49.2) | 138,746 (48.9) * | 2276 (49.6) * |
| Female | 227,770 (50.8) | 145,173 (51.1) * | 2310 (50.4) * |
| Race (%) | |||
| White | 356,033 (79.4) | 224,658 (79.1) | 3851 (84.0) |
| Black | 55,559 (12.4) | 34,885 (12.3) | 429 (9.4) |
| Other | 36,629 (8.2) | 24,376 (8.6) | 306 (6.7) |
| Detection Stage (%) | |||
| In Situ | 21,655 (4.8) | 1975 (0.7) | 1 (<0.1) |
| Localized | 159,954 (35.7) | 87,453 (30.8) | 544 (11.9) |
| Regional | 155,275 (34.6) | 117,946 (41.5) | 2078 (45.3) |
| Distant | 93,274 (20.8) | 67,485 (23.8) | 1864 (40.6) |
| Unstaged | 18,063 (4.0) | 9060 (3.2) | 99 (2.2) |
| Grade Differentiation (%) | |||
| Well | 38,192 (8.5) | 18,437 (6.5) | 25 (0.5) |
| Moderate | 254,481 (56.8) | 186,654 (65.7) | 246 (5.4) |
| Poor | 72,229 (16.1) | 52,503 (18.5) | 3143 (68.5) |
| Undifferentiated | 7970 (1.8) | 4397 (1.5) | 433 (9.4) |
| Unknown | 75,349 (16.8) | 21,928 (7.7) | 739 (16.1) |
| Surgery (%) | |||
| Yes | 394,923 (88.1) | 251,754 (88.7) | 3875 (84.5) |
| No | 53,298 (11.9) | 32,165 (11.3) | 711 (15.5) |
| Radiotherapy (%) | |||
| Yes | 9237 (2.1) | 6971 (2.5) | 166 (3.6) |
| No | 438,984 (97.9) | 276,948 (97.5) | 4420 (96.4) |
| Chemotherapy (%) | |||
| Yes | 125,723 (28.0) | 95,441 (33.6) | 2172 (47.4) |
| No | 322,498 (72.0) | 188,478 (66.4) | 2414 (52.6) |
| Incidence Rate (95% CI) | |||
| All | 31.2 (31.1–31.3) | 20.1 (20.0–20.2) | 3.5 (3.4–3.6) † |
| Male | 35.0 (34.9–35.2) | 22.6 (22.5–22.7) | 3.8 (3.7–4.0) † |
| Female | 28.1 (28.0–28.3) | 18.15 (18.06–18.24) | 3.1 (3.0–3.3) † |
| CSS % (95% CI) | |||
| 1-year | 83.5 (83.4–83.7) | 83.3 (83.2–83.5) | 64.0 (62.4–65.6) |
| 2-year | 75.9 (75.7–76.0) | 74.8 (74.6–74.9) | 47.5 (45.8–49.2) |
| 5-year | 64.6 (64.4–64.8) | 61.8 (61.6–62.0) | 33.6 (31.8–35.3) |
| 10-year | 58.5 (58.3–58.7) | 55.0 (54.7–55.2) | 28.6 (26.8–30.4) |
| Median (Months) | - | - | 21.6 |
| RS % (95% CI) | |||
| 1-year | 82.1 (82.0–82.2) | 81.9 (81.8–82.1) | 61.4 (59.7–63.0) |
| 2-year | 74.8 (74.7–75.0) | 73.8 (73.6–74.0) | 45.4 (43.6–47.1) |
| 5-year | 64.2 (64.0–64.4) | 61.7 (61.4–61.9) | 31.7 (29.9–33.6) |
| 10-year | 57.8 (57.5–58.1) | 54.7 (54.3–55.0) | 26.3 (24.0–28.7) |
| Median (Months) | - | - | 19.4 |
p < 0.05 for all comparisons between adenocarcinoma and signet ring cell comparisons, unless noted by * p ≥ 0.05. Incidence rates expressed per 100,000, except † (per 1 million). CSS, cause-specific survival; RS, relative survival; CI, confidence interval.
Table 4.
Derived univariate and multivariable Cox-proportional hazard ratios (HR) of mortality for colon cancers.
| Colon | Signet Ring vs. Non-Signet Ring | Signet Ring vs. Adenocarcinoma | ||
|---|---|---|---|---|
| HR (95% CI) | Univariate | Multivariable | Univariate | Multivariable |
| Signet Ring Histology | 2.69 (2.58–2.79) | 1.45 (1.40–1.51) | 2.31 (2.22–2.40) | 1.47 (1.41–1.53) |
| Age (per 10 years) | 1.149 (1.144–1.154) | 1.242 (1.237–1.248) | 1.089 (1.083–1.094) | 1.212 (1.205–1.218) |
| Gender (Female) | 1.03 (1.02–1.05) | 0.96 (0.95–0.97) | 0.98 (0.97–0.99) | 0.96 (0.95–0.97) |
| Race | ||||
| Black | 1.22 (1.20–1.24) | 1.21 (1.19–1.23) | 1.29 (1.26–1.31) | 1.23 (1.21–1.25) |
| Other | 0.91 (0.89–0.92) | 0.93 (0.92–0.95) | 0.92 (0.90–0.94) | 0.94 (0.92–0.96) |
| Detection Stage | ||||
| In Situ | 0.42 (0.39–0.44) | 0.39 (0.36–0.41) | 0.53 (0.45–0.62) | 0.43 (0.37–0.51) |
| Regional | 3.01 (2.96–3.07) | 3.13 (3.08–3.19) | 2.48 (2.43–2.53) | 2.70 (2.64–2.76) |
| Distant | 17.5 (17.2–17.8) | 16.6 (16.3–17.0) | 14.2 (13.9–14.5) | 14.4 (14.1–14.7) |
| Unstaged | 8.8 (8.5–9.0) | 4.32 (4.19–4.45) | 6.66 (6.42–6.91) | 3.40 (3.27–3.54) |
| Grade Differentiation | ||||
| Moderate | 1.73 (1.68–1.77) | 1.25 (1.22–1.28) | 1.37 (1.33–1.41) | 1.17 (1.13–1.20) |
| Poor | 3.18 (3.10–3.26) | 1.80 (1.75–1.85) | 2.34 (2.27–2.42) | 1.65 (1.60–1.71) |
| Undifferentiated | 3.19 (3.05–3.33) | 1.98 (1.89–2.06) | 2.37 (2.25–2.50) | 1.73 (1.64–1.83) |
| Unknown | 2.28 (2.22–2.35) | 1.39 (1.35–1.43) | 3.89 (3.75–4.03) | 1.41 (1.36–1.46) |
| Surgery (Yes) | 0.167 (0.165–0.170) | 0.39 (0.38–0.40) | 0.175 (0.172–0.178) | 0.40 (0.39–0.41) |
| Radiotherapy (Yes) | 2.14 (2.08–2.20) | 1.08 (1.05–1.11) | 1.83 (1.77–1.88) | 1.08 (1.05–1.12) |
| Chemotherapy (Yes) | 1.95 (1.93–1.98) | 0.86 (0.85–0.87) | 1.58 (1.56–1.60) | 0.81 (0.80–0.82) |
p < 0.05 relative to reference. Reference categories: Gender (Male), Race (White), Detection Stage (Localized), Grade differentiation (Well), Surgery (No), Radiotherapy (No), and Chemotherapy (No). CI, confidence interval.
2.3. Esophageal
SRCCs comprise 2.6% of all cases of esophageal cancer, and 4.7% of all SRCC cases (Table 5, Figure 2). When compared to nonvariant adenocarcinomas, there is no overt difference in age of onset, unlike gastric and colon SRCCs. There is also no gender bias, and SRCCs are more often detected regionally rather than distally, unlike the adenocarcinomas. However, consistent with the SRCCs the majority are of poor grade (77.8% compared to 42.1% for adenocarcinomas).
Table 5.
Baseline demographics and clinical characteristics by histology for esophageal cancers.
| Esophageal | All | Adenocarcinoma | Squamous Cell | Signet Ring |
|---|---|---|---|---|
| N | 59,989 (100) | 30,860 (51.4) | 20,634 (34.4) | 1549 (2.6) |
| Age (Years) (%) | ||||
| 0–14 | 3 (<0.1) | 0 (0) | 3 (<0.1) | 0 (0) |
| 15–29 | 109 (0.2) | 78 (0.3) | 11 (0.1) | 5 (0.3) |
| 30–49 | 4597 (7.7) | 2583 (8.4) | 1356 (6.6) | 133 (8.6) |
| 50–69 | 30,938 (51.6) | 16,299 (52.8) | 10,583 (51.3) | 816 (52.7) |
| 70–85 | 20,281 (33.8) | 10,002 (32.4) | 7333 (35.5) | 521 (33.6) |
| >85 | 4061 (6.8) | 1898 (6.2) | 1348 (6.5) | 74 (4.8) |
| Mean (SD) | 66.5 (12.0) | 65.9 (12.1) | 67.0 (11.6) | 65.8 (11.8) |
| Gender (%) | ||||
| Male | 46,488 (77.5) | 26,477 (85.8) | 13,442 (65.1) | 1346 (86.9) |
| Female | 13,501 (22.5) | 4383 (14.2) | 7192 (34.9) | 203 (13.1) |
| Race (%) | ||||
| White | 49,399 (82.3) | 29,242 (94.8) | 12,696 (61.5) | 1457 (94.1) |
| Black | 7273 (12.1) | 830 (2.7) | 5767 (27.9) | 45 (2.9) |
| Other | 3317 (5.5) | 788 (2.6) | 2171 (10.5) | 47 (3.0) |
| Detection Stage (%) | ||||
| In Situ | 906 (1.5) | 398 (1.3) | 256 (1.2) | 0 (0) |
| Localized | 12,352 (20.6) | 6673 (21.6) | 4332 (21.0) | 260 (16.8) |
| Regional | 18,347 (30.6) | 9326 (30.2) | 6954 (33.7) | 612 (39.5) |
| Distant | 20,768 (34.6) | 11,556 (37.4) | 6170 (29.9) | 542 (35.1) |
| Unstaged | 7616 (12.7) | 2907 (9.4) | 2922 (14.2) | 134 (8.7) |
| Grade Differentiation (%) | ||||
| Well | 2710 (4.5) | 1595 (5.2) | 961 (4.7) | 3 (0.2) |
| Moderate | 18,923 (31.5) | 10,368 (33.6) | 7985 (38.7) | 55 (3.6) |
| Poor | 24,233 (40.4) | 12,995 (42.1) | 7505 (36.4) | 1205 (77.8) |
| Undifferentiated | 1068 (1.8) | 392 (1.3) | 185 (0.9) | 41 (2.6) |
| Unknown | 13,055 (21.8) | 5510 (17.9) | 3998 (19.4) | 245 (15.8) |
| Surgery (%) | ||||
| Yes | 18,433 (30.7) | 11,160 (36.2) | 4995 (24.2) | 528 (34.1) |
| No | 41,556 (69.3) | 19,700 (63.8) | 15,639 (75.8) | 1021 (65.9) |
| Radiotherapy (%) | ||||
| Yes | 32,376 (54.0) | 15,984 (51.8) | 12,892 (62.5) | 914 (59.0) |
| No | 27,613 (46.0) | 14,876 (48.2) | 7742 (37.5) | 635 (41.0) |
| Chemotherapy (%) | ||||
| Yes | 34,006 (56.7) | 18,169 (58.9) | 11,887 (57.6) | 997 (64.4) |
| No | 25,983 (43.3) | 12,691 (41.1) | 8747 (42.4) | 552 (35.6) |
| Incidence Rate (95% CI) | ||||
| All | 4.40 (4.37–4.44) | 2.27 (2.24–2.29) | 1.47 (1.45–1.49) | 1.18 (1.13–1.24) † |
| Male | 7.58 (7.51–7.65) | 4.33 (4.28–4.38) | 2.10 (2.06–2.13) | 2.27 (2.15–2.39) † |
| Female | 1.82 (1.80–1.85) | 0.59 (0.58–0.61) | 0.96 (0.93–0.98) | 0.30 (0.26–0.34) † |
| CSS % (95% CI) | ||||
| 1-year | 48.2 (47.7–48.6) | 52.7 (52.0–53.3) | 43.8 (42.9–44.6) | 43.7 (41.0–46.5) |
| 2-year | 31.5 (31.0–31.9) | 34.8 (34.2–35.5) | 28.0 (27.2–28.8) | 25.5 (23.0–28.0) |
| 5-year | 20.0 (19.6–20.4) | 21.9 (21.3–22.5) | 18.3 (17.6–19.0) | 13.6 (11.6–15.8) |
| 10-year | 16.1 (15.7–16.6) | 17.8 (17.2–18.4) | 14.6 (13.8–15.3) | 11.4 (9.37–13.5) |
| Median (Months) | 11.3 | 13.2 | 9.7 | 9.8 |
| RS % (95% CI) | ||||
| 1-year | 46.1 (45.6–46.5) | 50.6 (50.0–51.2) | 41.6 (40.8–42.5) | 42.6 (39.9–45.3) |
| 2-year | 29.5 (29.1–30.0) | 33.0 (32.4–33.6) | 25.9 (25.2–26.7) | 24.2 (21.8–26.7) |
| 5-year | 17.8 (17.4–18.2) | 20.0 (19.4–20.6) | 15.8 (15.1–16.5) | 12.4 (10.4–14.6) |
| 10-year | 13.1 (12.7–13.6) | 15.0 (14.4–15.7) | 11.0 (10.2–11.8) | 10.0 (8.02–12.3) |
| Median (Months) | 10.5 | 12.3 | 9.1 | 9.5 |
p < 0.05 for all comparisons among adenocarcinoma, squamous cell, and signet ring cell comparisons. Incidence rates expressed per 100,000, except † (per 1 million). CSS, cause-specific survival; RS, relative survival; CI, confidence interval.
For comparative purposes, squamous cell cancers are also included, which have worse 5 and 10-year CSS to adenocarcinomas (18.3%, 14.6% vs. 21.9%, 17.8%). Compared to squamous cell, SRCCs have statistically significant worse survival (SRCC 5- and 10-year survival 13.6% and 11.4%, respectively) (Figure 3c, Table 5). Median survival time is 9.8 months for SRCCs, compared to 9.7 months and 13.2 months for squamous cell and adenocarcinomas, respectively. SRCCs have a HR of 1.15 (95% CI: 1.08–1.22) compared to all other cancers, 1.16 (95% CI: 1.09–1.24) to adenocarcinomas, and 1.09 (1.02–1.16) to squamous cell, after multivariate analyses (Table 6).
Table 6.
Derived univariate and multivariable Cox-proportional hazard ratios (HR) of mortality for esophageal cancers.
| Esophageal | Signet Ring vs Non-Signet Ring | Signet Ring vs Adenocarcinoma | Signet Ring vs Squamous Cell | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | Univariate | Multivariable | Univariate | Multivariable | Univariate | Multivariable |
| Signet Ring Histology | 1.19 (1.12–1.26) | 1.15 (1.08–1.22) | 1.30 (1.32–1.39) | 1.16 (1.09–1.24) | 1.06 (1.00–1.13) * | 1.09 (1.02–1.16) |
| Age (per 10 years) | 1.116 (1.106–1.126) | 1.098 (1.088–1.108) | 1.115 (1.102–1.129) | 1.100 (1.086–1.114) | 1.084 (1.069–1.100) | 1.064 (1.048–1.080) |
| Gender (Female) | 1.00 (0.97–1.02) * | 0.93 (0.90–0.95) | 1.07 (1.03–1.11) | 0.99 (0.95–1.03) * | 0.85 (0.82–0.88) | 0.85 (0.83–0.88) |
| Race | ||||||
| Black | 1.30 (1.26–1.34) | 1.21 (1.17–1.25) | 1.20 (1.11–1.31) | 1.07 (0.98–1.16) * | 1.21 (1.17–1.26) | 1.16 (1.11–1.20) |
| Other | 1.08 (1.04–1.13) | 1.00 (0.96–1.05) * | 1.07 (0.98–1.16) * | 0.92 (0.85–1.01) * | 1.00 (0.95–1.06) * | 0.97 (0.92–1.00) * |
| Detection Stage | ||||||
| In Situ | 0.29 (0.25–0.34) | 0.27 (0.23–0.32) | 0.29 (0.22–0.36) | 0.27 (0.21–0.34) | 0.35 (0.28–0.44) | 0.28 (0.22–0.35) |
| Regional | 1.59 (1.55–1.64) | 1.85 (1.79–1.91) | 1.91 (1.83–1.99) | 2.18 (2.08–2.29) | 1.23 (1.18–1.29) | 1.43 (1.36–1.49) |
| Distant | 3.46 (3.36–3.57) | 3.25 (3.14–3.36) | 4.52 (4.34–4.72) | 3.96 (3.78–4.16) | 2.36 (2.25–2.47) | 2.36 (2.25–2.48) |
| Unstaged | 2.30 (2.21–2.39) | 1.76 (1.70–1.83) | 2.91 (2.75–3.08) | 2.02 (1.90–2.14) | 1.64 (1.55–1.74) | 1.39 (1.31–1.47) |
| Grade Differentiation | ||||||
| Moderate | 1.49 (1.41–1.57) | 1.31 (1.24–1.39) | 1.55 (1.43–1.66) | 1.28 (1.19–1.38) | 1.33 (1.22–1.45) | 1.28 (1.18–1.40) |
| Poor | 1.93 (1.83–2.04) | 1.59 (1.51–1.68) | 2.20 (2.05–2.37) | 1.69 (1.57–1.82) | 1.49 (1.36–1.62) | 1.34 (1.23–1.47) |
| Undifferentiated | 1.90 (1.74–2.07) | 1.62 (1.48–1.77) | 1.98 (1.74–2.26) | 1.71 (1.50–1.95) | 1.39 (1.17–1.65) | 1.31 (1.10–1.56) |
| Unknown | 1.40 (1.32–1.48) | 1.18 (1.12–1.25) | 1.40 (1.30–1.52) | 1.18 (1.09–1.28) | 1.28 (1.17–1.40) | 1.19 (1.09–1.31) |
| Surgery (Yes) | 0.39 (0.38–0.40) | 0.49 (0.48–0.50) | 0.32 (0.31–0.33) | 0.44 (0.43–0.46) | 0.55 (0.53–0.57) | 0.58 (0.55–0.60) |
| Radiotherapy (Yes) | 0.90 (0.88–0.92) | 0.95 (0.92–0.97) | 1.00 (0.97–1.02) * | 1.02 (0.99–1.05) * | 0.68 (0.66–0.71) | 0.80 (0.77–0.84) |
| Chemotherapy (Yes) | 0.87 (0.85–0.89) | 0.59 (0.57–0.61) | 1.04 (1.01–1.07) | 0.59 (0.57–0.61) | 0.63 (0.61–0.65) | 0.57 (0.54–0.59) |
p < 0.05 relative to reference unless noted by * p ≥ 0.05. Reference categories: Gender (Male), Race (White), Detection Stage (Localized), Grade differentiation (Well), Surgery (No), Radiotherapy (No), and Chemotherapy (No). CI, confidence interval.
2.4. Rectal
SRCCs comprise 0.7% of all cases of rectal cancer, and 4.3% of all SRCC cases (Table 7, Figure 2). When compared to nonvariant adenocarcinomas, SRCCs have an earlier mean age of onset of 6.6 years like gastric SRCCs, compared to 3.5 years for colon SRCCs. Unlike gastric SRCCs, there a larger gender bias towards males compared to adenocarcinomas (65.3% vs. 58.6%). This bias is not present in colon SRCCs (Table 3). Similar to gastric and colon SRCCs, these cancers are most often detected at a distant or metastatic stage (33.0% vs. 20.1%) with a poor tumor grade (66.3% vs. 13.2%). SRCC patients receive both radiotherapy (55.6% vs. 46.4%) and chemotherapy more often (68.6% vs. 56.6%). Rectal SRCC patients have the worst overall survival relative to comparative nonvariant cancers of all the SRCCs, with 5- and 10-year survival at 24.9% vs. 59.8% and 19.8% vs. 50.7%, respectively (Figure 3d, Table 7).
Table 7.
Baseline demographics and clinical characteristics by histology for rectal cancers.
| Rectal | All | Adenocarcinoma | Signet Ring |
|---|---|---|---|
| N | 194,109 (100) | 119,273 (61.4) | 1295 (0.7) |
| Age (Years) (%) | |||
| 0–14 | 10 (<0.1) | 2 (<0.1) | 1 (0.1) |
| 15–29 | 1403 (0.7) | 636 (0.5) | 78 (6.0) |
| 30–49 | 27,051 (13.9) | 16,245 (13.6) | 323 (24.9) |
| 50–69 | 97,233 (50.1) | 57,992 (48.6) | 542 (41.9) |
| 70–85 | 55,826 (28.8) | 36,187 (30.3) | 296 (22.9) |
| >85 | 12,586 (6.5) | 8211 (6.9) | 55 (4.2) |
| Mean (SD) | 63.7 (13.7) | 64.4 (13.6) | 57.8 (16.9) |
| Gender (%) | |||
| Male | 110,203 (56.8) | 69,952 (58.6) | 845 (65.3) |
| Female | 83,906 (43.2) | 49,321 (41.4) | 450 (34.7) |
| Race (%) | |||
| White | 154,869 (79.8) | 96,639 (81.0) | 1002 (77.4) |
| Black | 19,448 (10.0) | 10,550 (8.8) | 130 (10.0) |
| Other | 19,792 (10.2) | 12,084 (10.1) | 163 (12.6) |
| Detection Stage (%) | |||
| In Situ | 9251 (4.8) | 730 (0.6) | 3 (0.2) |
| Localized | 78,378 (40.4) | 37,686 (31.6) | 156 (12.0) |
| Regional | 64,405 (33.2) | 50,775 (42.6) | 643 (49.7) |
| Distant | 30,903 (15.9) | 23,972 (20.1) | 427 (33.0) |
| Unstaged | 11,172 (5.8) | 6110 (5.1) | 66 (5.1) |
| Grade Differentiation (%) | |||
| Well | 17,774 (9.2) | 7599 (6.4) | 12 (0.9) |
| Moderate | 108,345 (55.8) | 82,503 (69.2) | 62 (4.8) |
| Poor | 22,844 (11.8) | 15,736 (13.2) | 859 (66.3) |
| Undifferentiated | 1999 (1.0) | 934 (0.8) | 90 (6.9) |
| Unknown | 43,147 (22.2) | 12,501 (10.5) | 272 (21.0) |
| Surgery (%) | |||
| Yes | 156,833 (80.8) | 94,549 (79.3) | 901 (69.6) |
| No | 37,276 (19.2) | 24,724 (20.7) | 394 (30.4) |
| Radiotherapy (%) | |||
| Yes | 71,720 (36.9) | 55,224 (46.3) | 720 (55.6) |
| No | 122,389 (63.1) | 64,049 (53.7) | 575 (44.4) |
| Chemotherapy (%) | |||
| Yes | 86,677 (44.7) | 67,533 (56.6) | 888 (68.6) |
| No | 107,432 (55.3) | 51,720 (43.4) | 407 (31.4) |
| Incidence Rate (95% CI) | |||
| All | 12.81 (12.75–12.87) | 8.02 (7.97–8.06) | 0.94 (0.89–0.99) † |
| Male | 16.11 (16.01–16.21) | 10.45 (10.37–10.53) | 1.33 (1.24–1.42) † |
| Female | 10.10 (10.03–10.17) | 6.02 (5.96–6.07) | 0.62 (0.57–0.68) † |
| CSS % (95% CI) | |||
| 1-year | 86.4 (86.2–86.5) | 85.3 (85.0–85.5) | 61.9 (58.5–65.2) |
| 2-year | 78.4 (78.2–78.7) | 76.0 (75.7–76.3) | 41.2 (37.7–44.6) |
| 5-year | 64.8 (64.5–65.0) | 59.8 (59.4–60.1) | 24.9 (21.8–28.2) |
| 10-year | 56.8 (56.5–57.2) | 50.7 (50.3–51.1) | 19.8 (16.6–23.1) |
| Median (Months) | - | - | 16.8 |
| RS % (95% CI) | |||
| 1-year | 85.2 (85.0–85.5) | 84.1 (83.9–84.4) | 59.8 (56.3–63.1) |
| 2-year | 77.6 (77.3–77.8) | 75.1 (74.8–75.4) | 39.4 (36.0–42.9) |
| 5-year | 64.5 (64.2–64.9) | 59.5 (59.1–59.9) | 23.2 (20.0–26.5) |
| 10-year | 56.5 (56.0–56.9) | 50.2 (49.6–50.8) | 18.5 (15.0–22.3) |
| Median (Months) | - | - | 16.0 |
p < 0.05 for all comparisons among adenocarcinoma and signet ring cell comparisons. Incidence rates expressed per 100,000, except † (per 1 million). CSS, cause-specific survival; RS, relative survival; CI, confidence interval.
Median survival time is 16.8 months compared to more than 10 years for adenocarcinomas. When compared to all rectal cancers, SRCCs have a HR of 2.14 (95% CI: 1.99–2.29), and 2.10 (95% CI: 1.95–2.25) to adenocarcinomas, after multivariate analyses (Table 8).
Table 8.
Derived univariate and multivariable Cox-proportional hazard ratios (HR) of mortality for rectal cancers.
| Rectal | Signet Ring vs. Non-Signet Ring | Signet Ring vs. Adenocarcinoma | ||
|---|---|---|---|---|
| HR (95% CI) | Univariate | Multivariable | Univariate | Multivariable |
| Signet Ring Histology | 3.42 (3.19–3.66) | 2.14 (1.99–2.29) | 2.70 (2.53–2.90) | 2.10 (1.95–2.25) |
| Age (per 10 years) | 1.242 (1.235–1.250) | 1.310 (1.301–1.319) | 1.178 (1.170–1.187) | 1.245 (1.236–1.255) |
| Gender (Female) | 0.94 (0.92–0.95) | 0.93 (0.91–0.94) | 0.97 (0.96–0.99) | 0.95 (0.93–0.97) |
| Race | ||||
| Black | 1.16 (1.13–1.19) | 1.19 (1.16–1.22) | 1.41 (1.36–1.45) | 1.29 (1.25–1.32) |
| Other | 0.88 (0.86–0.91) | 0.93 (0.90–0.95) | 0.96 (0.93–0.99) | 0.97 (0.94–1.00) * |
| Detection Stage | ||||
| In Situ | 0.37 (0.34–0.40) | 0.38 (0.35–0.41) | 0.46 (0.36–0.58) | 0.35 (0.28–0.45) |
| Regional | 2.80 (2.73–2.86) | 2.92 (2.85–2.99) | 2.00 (1.95–2.06) | 2.35 (2.28–2.42) |
| Distant | 14.6 (14.2–14.9) | 12.6 (12.2–12.9) | 10.5 (10.3–10.8) | 9.92 (9.62–10.2) |
| Unstaged | 4.53 (4.37–4.69) | 2.79 (2.69–2.90) | 4.61 (4.41–4.81) | 2.67 (2.55–2.80) |
| Grade Differentiation | ||||
| Moderate | 1.70 (1.64–1.76) | 1.24 (1.20–1.29) | 1.13 (1.09–1.18) | 1.06 (1.02–1.11) |
| Poor | 3.01 (2.89–3.13) | 1.82 (1.75–1.90) | 1.91 (1.83–2.00) | 1.58 (1.50–1.65) |
| Undifferentiated | 3.09 (2.87–3.33) | 2.10 (1.95–2.26) | 1.97 (1.78–2.18) | 1.65 (1.49–1.83) |
| Unknown | 1.26 (1.21–1.31) | 1.08 (1.04–1.13) | 2.00 (1.91–2.10) | 1.17 (1.11–1.23) |
| Surgery (Yes) | 0.228 (0.224–0.232) | 0.40 (0.39–0.41) | 0.220 (0.216–0.225) | 0.40 (0.39–0.41) |
| Radiotherapy (Yes) | 1.28 (1.26–1.30) | 1.10 (1.08–1.12) | 0.81 (0.80–0.83) | 1.04 (1.02–1.06) |
| Chemotherapy (Yes) | 1.75 (1.72–1.78) | 0.80 (0.78–0.82) | 1.07 (1.05–1.09) | 0.72 (0.70–0.73) |
p < 0.05 relative to reference unless noted by * p ≥ 0.05. Reference categories: Gender (Male), Race (White), Detection Stage (Localized), Grade differentiation (Well), Surgery (No), Radiotherapy (No), and Chemotherapy (No). CI, confidence interval.
2.5. Lung
SRCCs comprise 0.1% of all cases of lung cancer, and 3.1% of all SRCC cases (Table 9, Figure 2). When compared to nonvariant adenocarcinomas, SRCCs have an earlier mean age of onset of 3.9 years and 5.9 years relative to nonvariant adenocarcinomas and squamous cells, respectively. There is a gender bias towards males compared to adenocarcinomas (56.3% vs. 50.4%). Like most gastrointestinal tract SRCCs, relative to adenocarcinomas, lung SRCCs mainly present with distant/metastatic disease (73.7% vs. 58.4%) and poor grade (39.5% vs. 29.1%). Compared to both adenocarcinomas and squamous cells, SRCCs have much worse 5-year (9.7% vs. 21.6% vs. 22.5%) and 10-year (4.9% vs. 15.1% vs. 16.2%) survivals (Figure 3e, Table 9). Median survival time is 5.7 months for SRCCs, compared to about 12.5 months for both squamous cells and adenocarcinomas. SRCCs have a HR of 1.19 (95% CI: 1.10–1.28) compared to all other cancers, 1.24 (95% CI: 1.15–1.33) to adenocarcinomas, and 1.17 (1.09–1.26) to squamous cells, after multivariate analyses (Table 10).
Table 9.
Baseline demographics and clinical characteristics by histology for lung cancers.
| Lung | All | Adenocarcinoma | Squamous Cell | Signet Ring |
|---|---|---|---|---|
| N | 771,002 (100) | 236,024 (30.6) | 150,426 (19.5) | 1002 (0.1) |
| Age (Years) (%) | ||||
| 0–14 | 134 (<0.1) | 3 (<0.1) | 2 (<0.1) | 0 (0) |
| 15–29 | 1125 (0.1) | 191 (0.1) | 67 (<0.1) | 9 (0.9) |
| 30–49 | 41,482 (5.4) | 15,342 (6.5) | 4915 (3.3) | 122 (12.2) |
| 50–69 | 356,243 (46.2) | 116,978 (49.6) | 68,258 (45.4) | 536 (53.5) |
| 70–85 | 319,649 (41.5) | 90,680 (38.4) | 69,731 (46.4) | 299 (29.8) |
| >85 | 52,369 (6.8) | 12,830 (5.4) | 7453 (5.0) | 36 (3.6) |
| Mean (SD) | 68.3 (11.4) | 67.2 (11.4) | 69.2 (10.0) | 63.3 (12.8) |
| Gender (%) | ||||
| Male | 416,219 (54.0) | 118,856 (50.4) | 97,114 (64.6) | 564 (56.3) |
| Female | 354,783 (46.0) | 117,168 (49.6) | 53,312 (35.4) | 438 (43.7) |
| Race (%) | ||||
| White | 632,947 (82.1) | 187,596 (79.5) | 123,513 (82.1) | 811 (80.9) |
| Black | 87,586 (11.4) | 27,778 (11.8) | 19,123 (12.7) | 118 (11.8) |
| Other | 50,469 (6.5) | 20,650 (8.7) | 7790 (5.2) | 73 (7.3) |
| Detection Stage (%) | ||||
| In Situ | 781 (0.1) | 287 (0.1) | 321 (0.2) | 0 (0) |
| Localized | 130,847 (17.0) | 40,883 (17.3) | 33,020 (22.0) | 55 (5.5) |
| Regional | 185,572 (24.1) | 50,483 (21.4) | 53,745 (35.7) | 190 (19.0) |
| Distant | 409,261 (53.1) | 137,816 (58.4) | 57,379 (38.1) | 738 (73.7) |
| Unstaged | 44,541 (5.8) | 6555 (2.8) | 5961 (4.0) | 19 (1.9) |
| Grade Differentiation (%) | ||||
| Well | 31,217 (4.0) | 13,206 (5.6) | 3664 (2.4) | 6 (0.6) |
| Moderate | 102,756 (13.3) | 44,436 (18.8) | 40,323 (26.8) | 71 (7.1) |
| Poor | 187,802 (24.4) | 68,573 (29.1) | 53,169 (35.3) | 396 (39.5) |
| Undifferentiated | 48,057 (6.2) | 2123 (0.9) | 1539 (1.0) | 16 (1.6) |
| Unknown | 401,170 (52.0) | 107,686 (45.6) | 51,731 (34.4) | 513 (51.2) |
| Surgery (%) | ||||
| Yes | 189,192 (24.5) | 66,710 (28.3) | 46,764 (31.1) | 198 (19.8) |
| No | 581,810 (75.5) | 169,314 (71.7) | 103,662 (68.9) | 804 (80.2) |
| Radiotherapy (%) | ||||
| Yes | 297,248 (38.6) | 92,699 (39.3) | 70,553 (46.9) | 380 (37.9) |
| No | 473,754 (61.4) | 143,325 (60.7) | 79,873 (53.1) | 622 (62.1) |
| Chemotherapy (%) | ||||
| Yes | 311,134 (40.4) | 101,041 (42.8) | 56,174 (37.3) | 536 (53.5) |
| No | 459,868 (59.6) | 134,983 (57.2) | 94,252 (62.7) | 466 (46.5) |
| Incidence Rate (95% CI) | ||||
| All | 60.0 (59.9–60.1) | 18.4 (18.3–18.4) | 11.7 (11.6–11.7) | 7.1 (6.6–7.5) †† |
| Male | 72.7 (72.4–72.9) | 20.6 (20.5–20.7) | 16.8 (16.7–16.9) | 8.6 (7.9–9.4) †† |
| Female | 50.6 (50.4–50.8) | 16.8 (16.7–16.9) | 7.74 (7.67–7.80) | 5.9 (5.4–6.5) †† |
| CSS % (95% CI) | ||||
| 1-year | 46.6 (46.5–46.7) | 50.9 (50.7–51.2) | 51.2 (50.9–51.6) | 33.0 (29.8–36.2) |
| 2-year | 31.8 (31.7–32.0) | 36.0 (35.8–36.3) | 35.2 (34.8–35.5) | 20.5 (17.6–23.4) |
| 5-year | 20.2 (20.0–20.3) | 21.6 (21.4–21.8) | 22.5 (22.2–22.9) | 9.7 (7.5–12.1) |
| 10-year | 14.9 (14.8–15.0) | 15.1 (14.9–15.4) | 16.2 (15.9–16.5) | 4.9 (3.4–6.9) |
| Median (Months) | 10.5 | 12.5 | 12.6 | 5.7 |
| RS % (95% CI) | ||||
| 1-year | 44.5 (44.3–44.6) | 49.5 (49.2–49.7) | 48.8 (48.5–49.2) | 31.7 (28.5–34.9) |
| 2-year | 29.8 (29.7–29.9) | 34.6 (34.4–34.9) | 32.6 (32.3–32.9) | 19.8 (17.0–22.7) |
| 5-year | 18.1 (17.9–18.2) | 20.1 (19.9–20.3) | 19.5 (19.2–19.8) | 9.1 (7.0–11.5) |
| 10-year | 12.1 (11.9–12.2) | 13.0 (12.8–13.3) | 11.6 (11.3–12.0) | 4.3 (2.7–6.3) |
| Median (Months) | 9.6 | 11.7 | 11.5 | 5.4 |
p < 0.05 for all comparisons among adenocarcinoma, squamous cell, and signet ring cell comparisons. Incidence rates expressed per 100,000, except †† (per 10 million). CSS, cause-specific survival; RS, relative survival; CI, confidence interval.
Table 10.
Derived univariate and multivariable Cox-proportional hazard ratios (HR) of mortality for lung cancers.
| Lung | Signet Ring vs. Non-Signet Ring | Signet Ring vs. Adenocarcinoma | Signet Ring vs. Squamous Cell | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | Univariate | Multivariable | Univariate | Multivariable | Univariate | Multivariable |
| Signet Ring Histology | 1.37 (1.28–1.48) | 1.19 (1.10–1.28) | 1.48 (1.37–1.59) | 1.24 (1.15–1.33) | 1.51 (1.40–1.63) | 1.17 (1.09–1.26) |
| Age (per 10 years) | 1.114 (1.111–1.117) | 1.111 (1.108–1.114) | 1.070 (1.065–1.074) | 1.093 (1.088–1.098) | 1.089 (1.082–1.096) | 1.072 (1.065–1.079) |
| Gender (Female) | 0.827 (0.822–0.832) | 0.843 (0.838–0.847) | 0.804 (0.796–0.812) | 0.83 (0.82–0.84) | 0.89 (0.88–0.90) | 0.89 (0.87–0.90) |
| Race | ||||||
| Black | 1.09 (1.08–1.10) | 1.00 (0.99–1.01) * | 1.09 (1.07–1.11) | 1.00 (0.98–1.01) * | 1.17 (1.15–1.19) | 1.01 (0.99–1.03) * |
| Other | 0.94 (0.93–0.95) | 0.83 (0.82–0.84) | 0.92 (0.91–0.94) | 0.77 (0.75–0.78) | 1.12 (1.09–1.15) | 0.98 (0.95–1.01)* |
| Detection Stage | ||||||
| In Situ | 0.67 (0.57–0.77) | 0.59 (0.51–0.68) | 0.15 (0.08–0.27) | 0.16 (0.09–0.29) | 1.01 (0.85–1.20) * | 0.73 (0.62–0.87) |
| Regional | 2.28 (2.25–2.30) | 2.18 (2.16–2.20) | 2.21 (2.17–2.25) | 2.26 (2.22–2.31) | 2.00 (1.96–2.04) | 1.99 (1.95–2.03) |
| Distant | 5.74 (5.68–5.79) | 4.48 (4.33–4.53) | 6.51 (6.40–6.63) | 5.13 (5.03–5.24) | 4.91 (4.81–5.00) | 3.85 (3.77–3.93) |
| Unstaged | 3.68 (3.62–3.74) | 2.32 (2.28–2.35) | 3.75 (3.63–3.88) | 2.49 (2.41–2.58) | 2.89 (2.79–2.99) | 1.97 (1.91–2.05) |
| Grade Differentiation | ||||||
| Moderate | 1.62 (1.59–1.65) | 1.40 (1.37–1.42) | 1.38 (1.34–1.42) | 1.29 (1.25–1.33) | 0.90 (0.86–0.94) | 0.95 (0.91–0.99) |
| Poor | 2.71 (2.66–2.77) | 1.79 (1.76–1.83) | 2.37 (2.31–2.44) | 1.70 (1.65–1.75) | 1.06 (1.01–1.10) | 1.03 (0.99–1.08) * |
| Undifferentiated | 3.54 (3.46–3.61) | 2.02 (1.98–2.07) | 2.48 (2.34–2.63) | 1.74 (1.65–1.85) | 1.21 (1.12–1.30) | 1.18 (1.09–1.27) |
| Unknown | 3.61 (3.54–3.67) | 1.65 (1.62–1.69) | 3.50 (3.41–3.60) | 1.54 (1.50–1.59) | 1.59 (1.52–1.66) | 1.02 (0.98–1.07) * |
| Surgery (Yes) | 0.273 (0.271–0.276) | 0.453 (0.449–0.457) | 0.254 (0.251–0.257) | 0.463 (0.456–0.471) | 0.296 (0.292–0.301) | 0.392 (0.385–0.400) |
| Radiotherapy (Yes) | 1.335 (1.328–1.343) | 1.034 (1.027–1.040) | 1.51 (1.49–1.52) | 1.12 (1.10–1.13) | 1.43 (1.42–1.45) | 0.99 (0.98–1.00) * |
| Chemotherapy (Yes) | 1.197 (1.190–1.204) | 0.665 (0.660–0.669) | 1.25 (1.23–1.26) | 0.606 (0.599–0.613) | 1.13 (1.11–1.14) | 0.65 (0.64–0.66) |
p < 0.05 relative to reference unless noted by * p ≥ 0.05. Reference categories: Gender (Male), Race (White), Detection Stage (Localized), Grade differentiation (Well), Surgery (No), Radiotherapy (No), and Chemotherapy (No). CI, confidence interval.
2.6. Pancreatic
SRCCs comprise 0.4% of all cases of pancreatic cancer, and 2.1% of all SRCC cases (Table 11, Figure 2). The relative differences between SRCCs and nonvariant adenocarcinomas are not as large as in other cancer types, likely as pancreatic adenocarcinoma has among the worse survival outcomes of any cancer type. There is a slight gender bias towards males compared to adenocarcinomas (54.8% vs. 51.3%). Distant/metastatic disease and poor grade are the most common presentation for both SRCCs and adenocarcinomas. Treatment modalities are grossly similar in both groups. SRCC have slightly worse 1-year survival compared to adenocarcinomas (20.6% vs. 26.6%), but at 5-years, survival is slightly better, but not statistically significant (4.5% vs. 3.8%) (Table 11, Figure 3f). Median survival time is 3.5 months for SRCCs compared to 5.6 months for adenocarcinomas. When compared to all pancreatic cancers, SRCCs have a HR of 1.27 (95% CI: 1.16–1.40), and non-significantly 1.04 (95% CI: 0.95–1.14) to adenocarcinomas, after multivariate analyses (Table 12).
Table 11.
Baseline demographics and clinical characteristics by histology for pancreatic cancers.
| Pancreatic | All | Adenocarcinoma | Signet Ring |
|---|---|---|---|
| N | 160,539 (100) | 93,923 (58.5) | 640 (0.4) |
| Age (Years) (%) | |||
| 0–14 | 61 (<0.1) | 0 (0) | 0 (0) |
| 15–29 | 450 (0.3) | 66 (0.1) | 1 (0.2) |
| 30–49 | 10,797 (6.7) | 6062 (6.5) | 52 (8.1) |
| 50–69 | 68,769 (42.8) | 44,493 (47.4) | 316 (49.4) |
| 70–85 | 62,810 (39.1) | 36,664 (39.0) | 231 (36.1) |
| >85 | 17,652 (11.0) | 6638 (7.1) | 40 (6.3) |
| Mean (SD) | 68.9 (12.8) | 67.8 (11.7) | 66.7 (11.9) |
| Gender (%) | |||
| Male | 79,757 (49.7) | 48,192 (51.3) | 351 (54.8) |
| Female | 80,782 (50.3) | 45,731 (48.7) | 289 (45.2) |
| Race (%) | |||
| White | 128,028 (79.7) | 74,880 (79.7) | 529 (82.7) |
| Black | 19,779 (12.3) | 11,911 (12.7) | 63 (9.8) |
| Other | 12,732 (7.9) | 7132 (7.6) | 48 (7.5) |
| Detection Stage (%) | |||
| In Situ | 645 (0.4) | 41 (<0.1) | 0 (0) |
| Localized | 14,669 (9.1) | 6418 (6.8) | 17 (2.7) |
| Regional | 43,867 (27.3) | 27,826 (29.6) | 166 (25.9) |
| Distant | 84,626 (52.7) | 55,075 (58.6) | 437 (68.3) |
| Unstaged | 16,732 (10.4) | 4563 (4.9) | 20 (3.1) |
| Grade Differentiation (%) | |||
| Well | 8768 (5.5) | 3675 (3.9) | 1 (0.2) |
| Moderate | 21,250 (13.2) | 13,743 (14.6) | 32 (5.0) |
| Poor | 22,061 (13.7) | 14,872 (15.8) | 273 (42.7) |
| Undifferentiated | 1764 (1.1) | 582 (0.6) | 18 (2.8) |
| Unknown | 106,696 (66.5) | 61,051 (65.0) | 316 (49.4) |
| Surgery (%) | |||
| Yes | 32,963 (20.5) | 15,671 (16.7) | 134 (20.9) |
| No | 127,576 (79.5) | 78,252 (83.3) | 506 (79.1) |
| Radiotherapy (%) | |||
| Yes | 23,323 (14.5) | 16,224 (17.3) | 97 (15.2) |
| No | 137,216 (85.5) | 77,699 (82.7) | 543 (84.8) |
| Chemotherapy (%) | |||
| Yes | 66,287 (41.3) | 47,158 (50.2) | 275 (43.0) |
| No | 94,252 (58.7) | 46,765 (49.8) | 365 (57.0) |
| Incidence Rate (95% CI) | |||
| All | 12.23 (12.18–12.29) | 6.97 (6.93–7.02) | 4.6 (4.2–4.9) †† |
| Male | 13.89 (13.79–13.98) | 8.04 (7.97–8.11) | 5.7 (5.1–6.3) †† |
| Female | 10.87 (10.80–10.94) | 6.10 (6.04–6.15) | 3.7 (3.3–4.1) †† |
| CSS % (95% CI) | |||
| 1-year | 31.3 (31.0–31.6) | 26.6 (26.3–26.9) | 20.6 (17.2–24.2) |
| 2-year | 17.0 (16.8–17.2) | 10.7 (10.5–11.0) * | 8.9 (6.5–11.6) * |
| 5-year | 9.2 (9.0–9.4) | 3.8 (3.6–3.9) * | 4.5 (2.8–6.8) * |
| 10-year | 6.9 (6.7–7.1) | 2.5 (2.4–2.7) | 3.0 (1.5–5.3) ^ |
| Median (Months) | 5.9 | 5.6 | 3.5 |
| RS % (95% CI) | |||
| 1-year | 30.4 (30.2–30.7) | 25.9 (25.6–26.2) | 20.5 (17.1–24.0) |
| 2-year | 16.4 (16.1–16.6) | 10.3 (10.1–10.6) * | 8.9 (6.6–11.7) * |
| 5-year | 8.7 (8.5–8.9) | 3.6 (3.4–3.7) * | 4.3 (2.6–6.6) * |
| 10-year | 6.1 (5.9–6.3) | 2.2 (2.1–2.4) | 3.1 (1.6–5.5) ^ |
| Median (Months) | 5.7 | 5.4 | 3.4 |
p < 0.05 for all comparisons between adenocarcinoma and signet ring cell comparisons, unless noted by * p ≥ 0.05. Incidence rates expressed per 100,000, except †† (per 10 million); ^ (not age standardized). CSS, cause-specific survival; RS, relative survival; CI, confidence interval.
Table 12.
Derived univariate and multivariable Cox-proportional hazard ratios (HR) of mortality for pancreatic cancers.
| Pancreatic | Signet Ring vs. Non-Signet Ring | Signet Ring vs. Adenocarcinoma | ||
|---|---|---|---|---|
| HR (95% CI) | Univariate | Multivariable | Univariate | Multivariable |
| Signet Ring Histology | 1.27 (1.16–1.39) | 1.13 (1.03–1.24) | 1.08 (0.98–1.18) * | 1.04 (0.95–1.14) * |
| Age (per 10 years) | 1.215 (1.209–1.221) | 1.170 (1.164–1.176) | 1.121 (1.114–1.129) * | 1.090 (1.083–1.098) |
| Gender (Female) | 1.01 (0.99–1.02) * | 0.97 (0.96–0.98) | 0.98 (0.97–1.00) | 0.96 (0.95–0.97) |
| Race | ||||
| Black | 1.03 (1.01–1.05) | 1.05 (1.03–1.07) | 1.07 (1.05–1.10) | 1.07 (1.04–1.09) |
| Other | 0.93 (0.91–0.95) | 0.95 (0.93–0.97) | 1.00 (0.97–1.03) * | 0.96 (0.93–0.99) |
| Detection Stage | ||||
| In Situ | 0.11 (0.09–0.14) | 0.13 (0.10–0.17) | 0.13 (0.07–0.26) | 0.14 (0.07–0.27) |
| Regional | 1.55 (1.51–1.59) | 1.70 (1.66–1.74) | 1.07 (1.03–1.10) | 1.31 (1.27–1.36) |
| Distant | 3.01 (2.94–3.09) | 2.64 (2.57–2.70) | 2.16 (2.10–2.23) | 2.23 (2.16–2.30) |
| Unstaged | 2.46 (2.39–2.54) | 1.53 (1.49–1.58) | 1.57 (1.51–1.64) | 1.24 (1.19–1.30) |
| Grade Differentiation | ||||
| Moderate | 1.85 (1.79–1.92) | 1.86 (1.80–1.92) | 1.12 (1.07–1.16) | 1.25 (1.20–1.31) |
| Poor | 2.75 (2.66–2.85) | 2.42 (2.34–2.51) | 1.56 (1.49–1.62) | 1.59 (1.53–1.66) |
| Undifferentiated | 2.74 (2.57–2.92) | 2.26 (2.12–2.41) | 1.63 (1.47–1.80) | 1.52 (1.37–1.68) |
| Unknown | 3.11 (3.01–3.20) | 1.85 (1.80–1.91) | 1.79 (1.73–1.86) | 1.34 (1.29–1.39) |
| Surgery (Yes) | 0.343 (0.337–0.348) | 0.45 (0.44–0.46) | 0.42 (0.41–0.43) | 0.53 (0.51–0.54) |
| Radiotherapy (Yes) | 0.69 (0.68–0.70) | 0.99 (0.98–1.01) * | 0.58 (0.57–0.59) | 0.93 (0.91–0.95) |
| Chemotherapy (Yes) | 0.77 (0.76–0.78) | 0.67 (0.66–0.68) | 0.57 (0.56–0.58) | 0.54 (0.53–0.55) |
p < 0.05 relative to reference unless noted by * p ≥ 0.05. Reference categories: Gender (Male), Race (White), Detection Stage (Localized), Grade differentiation (Well), Surgery (No), Radiotherapy (No), and Chemotherapy (No). CI, confidence interval.
2.7. Appendiceal
SRCCs comprise 5.8% of all cases of appendiceal cancer, and 2.0% of all SRCC cases (Table 13, Figure 2). Data for carcinoid tumors is presented as this is the most common cancer subtype at 39.8% of cases. When compared to nonvariant adenocarcinomas, SRCCs have an earlier mean age of onset of 3.7 years. There is a large gender bias towards females compared to adenocarcinomas (62.5% vs. 47.1%), like as seen with gastric SRCCs. Typical among SRCCs, relative to adenocarcinomas, appendiceal SRCCs mainly present with distant/metastatic disease (62.2% vs. 29.9%) and poor grade (53.4% vs. 21.0%). SRCCs have worse 5-year (34.2% vs. 54.0%) and 10-year (24.1% vs. 47.2%) survivals relative to adenocarcinomas, with median survival times of 30 months and 82 months, respectively (Figure 3g, Table 9). Like colon and rectal cancers, SRCCs have a very high mortality HR of 3.50 (95% CI: 3.16–3.89) compared to all cancers, 8.29 (95% CI: 7.25–9.48) to carcinoids, and 2.00 (95% CI: 1.77–2.26) to adenocarcinomas, on univariate analysis. However, unlike colon and rectal cancers, after multivariable analysis, the HR of mortality for SRCCs compared to adenocarcinomas is equivalent (0.95 (95% CI: 0.82–1.09)) (Table 14).
Table 13.
Baseline demographics and clinical characteristics by histology for appendiceal cancers.
| Appendiceal | All | Carcinoid | Adenocarcinoma | Signet Ring |
|---|---|---|---|---|
| N | 11,456 (100) | 4562 (39.8) | 1761 (15.4) | 669 (5.8) |
| Age (Years) (%) | ||||
| 0–14 | 152 (1.3) | 151 (3.3) | 0 (0) | 0 (0) |
| 15–29 | 990 (8.6) | 871 (19.1) | 35 (2.0) | 4 (0.6) |
| 30–49 | 3052 (26.6) | 1457 (31.9) | 333 (18.9) | 195 (29.1) |
| 50–69 | 5114 (44.6) | 1680 (36.8) | 851 (48.3) | 345 (51.6) |
| 70–85 | 1867 (16.3) | 354 (7.8) | 455 (25.8) | 114 (17.0) |
| >85 | 281 (2.5) | 49 (1.1) | 87 (4.9) | 11 (1.6) |
| Mean (SD) | 53.9 (17.2) | 45.8 (18.0) | 61.4 (14.7) | 57.7 (12.7) |
| Gender (%) | ||||
| Male | 5230 (45.7) | 1999 (43.8) | 931 (52.9) | 251 (37.5) |
| Female | 6226 (54.3) | 2563 (56.2) | 830 (47.1) | 418 (62.5) |
| Race (%) | ||||
| White | 9608 (83.9) | 3983 (87.3) | 1394 (79.2) | 562 (84.0) |
| Black | 1093 (9.5) | 370 (8.1) | 241 (13.7) | 60 (9.0) |
| Other | 755 (6.6) | 209 (4.6) | 126 (7.2) | 47 (7.0) |
| Detection Stage (%) | ||||
| In Situ | 131 (1.1) | 1 (<0.1) | 20 (1.1) | 1 (0.1) |
| Localized | 4774 (41.7) | 2790 (61.2) | 661 (37.5) | 88 (13.2) |
| Regional | 2620 (22.9) | 1087 (23.8) | 513 (29.1) | 156 (23.3) |
| Distant | 3420 (29.9) | 381 (8.4) | 527 (29.9) | 416 (62.2) |
| Unstaged | 511 (4.5) | 303 (6.6) | 40 (2.3) | 8 (1.2) |
| Grade Differentiation (%) | ||||
| Well | 3514 (30.7) | 1873 (41.1) | 242 (13.7) | 12 (1.8) |
| Moderate | 2743 (23.9) | 427 (9.4) | 904 (51.3) | 40 (6.0) |
| Poor | 1408 (12.3) | 257 (5.6) | 370 (21.0) | 357 (53.4) |
| Undifferentiated | 176 (1.5) | 43 (0.9) | 16 (0.9) | 39 (5.8) |
| Unknown | 3615 (31.6) | 1962 (43.0) | 229 (13.0) | 221 (33.0) |
| Surgery (%) | ||||
| Yes | 10,772 (94.0) | 4481 (98.2) | 1639 (93.1) | 588 (87.9) |
| No | 684 (6.0) | 81 (1.8) | 122 (6.9) | 81 (12.1) |
| Radiotherapy (%) | ||||
| Yes | 228 (2.0) | 13 (0.3) | 73 (4.1) | 20 (3.0) |
| No | 11,228 (98.0) | 4549 (99.7) | 1688 (95.9) | 649 (97.0) |
| Chemotherapy (%) | ||||
| Yes | 3616 (31.6) | 453 (9.9) | 723 (41.1) | 446 (66.7) |
| No | 7840 (68.4) | 4109 (90.1) | 1038 (58.9) | 223 (33.3) |
| Incidence Rate (95% CI) | ||||
| All | 8.5 (8.3–8.6) † | 3.5 (3.4–3.6) † | 1.32 (1.26–1.38) † | 5.0 (4.6–5.4) †† |
| Male | 8.2 (8.0–8.4) † | 3.1 (2.9–3.2) † | 1.53 (1.43–1.63) † | 4.2 (3.8–4.8) †† |
| Female | 8.8 (8.6–9.1) † | 3.9 (3.7–4.0) † | 1.17 (1.09–1.24) † | 5.7 (5.2–6.3) †† |
| CSS % (95% CI) | ||||
| 1-year | 87.7 (86.7–88.5) | 92.1 (90.2–93.6) | 82.7 (80.4–84.7) | 74.8 (70.0–78.9) |
| 2-year | 78.7 (77.6–79.8) | 88.1 (85.9–90.0) | 70.7 (68.1–73.2) | 55.7 (50.3–60.7) |
| 5-year | 63.1 (61.7–64.5) | 78.3 (75.3–81.0) | 54.0 (50.9–57.0) | 34.2 (28.7–39.7) |
| 10-year | 53.1 (51.3–54.9) | 68.6 (63.2–73.4) | 47.2 (43.8–50.5) | 24.1 (18.1–30.6) |
| Median (Months) | - | - | 82.1 | 30.0 |
| RS % (95% CI) | ||||
| 1-year | 87.3 (86.2–88.2) | 91.1 (88.9–92.9) | 81.6 (79.2–83.8) | 74.0 (69.1–78.3) |
| 2-year | 78.9 (77.6–80.1) | 88.0 (85.3–90.2) | 70.6 (67.7–73.3) | 54.5 (48.9–59.7) |
| 5-year | 64.3 (62.5–66.0) | 78.8 (74.5–82.4) | 55.1 (51.4–58.6) | 34.2 (28.4–40.1) |
| 10-year | 54.3 (51.7–56.8) | 61.8 (54.2–68.5) | 48.8 (44.5–52.9) | 20.9 (14.4–28.3) |
| Median (Months) | - | - | 107 | 29.3 |
p < 0.05 for all comparisons among carcinoid, adenocarcinoma, and signet ring cell comparisons. Incidence rates expressed † (per 1 million) and †† (per 10 million). CSS, cause-specific survival; RS, relative survival; CI, confidence interval.
Table 14.
Derived univariate and multivariable Cox-proportional hazard ratios (HR) of mortality for appendiceal cancers.
| Appendiceal | Signet Ring vs. Non-Signet Ring | Signet Ring vs. Carcinoid | Signet Ring vs. Adenocarcinoma | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | Univariate | Multivariable | Univariate | Multivariable | Univariate | Multivariable |
| Signet Ring Histology | 3.50 (3.16–3.89) | 1.50 (1.33–1.68) | 8.29 (7.25–9.48) | 1.57 (1.33–1.86) | 2.00 (1.77–2.26) | 0.95 (0.82–1.09) * |
| Age (per 10 years) | 1.26 (1.23–1.29) | 1.25 (1.22–1.29) | 1.44 (1.38–1.50) | 1.33 (1.26–1.40) | 1.01 (0.97–1.05) * | 1.10 (1.05–1.15) |
| Gender (Female) | 1.02 (0.95–1.10) * | 0.91 (0.85–0.98) | 1.30 (1.14–1.49) | 1.11 (0.97–1.28) | 1.29 (1.15–1.45) | 1.06 (0.94–1.20) * |
| Race | ||||||
| Black | 1.29 (1.15–1.44) | 1.40 (1.25–1.56) | 1.36 (1.10–1.69) | 1.57 (1.27–1.95) | 1.03 (0.86–1.23) * | 1.20 (1.00–1.44) * |
| Other | 1.13 (0.98–1.30) * | 0.94 (0.81–1.08) * | 1.33 (1.00–1.79) * | 0.98 (0.73–1.32) * | 0.94 (0.74–1.20) * | 0.83 (0.65–1.06) * |
| Detection Stage | ||||||
| In Situ | 0.40 (0.17–0.97) | 0.32 (0.13–0.77) | - | - | 0.57 (0.14–2.30) * | 0.40 (0.10–1.62) * |
| Regional | 2.92 (2.58–3.30) | 2.31 (2.04–2.62) | 4.18 (3.31–5.29) | 3.31 (2.60–4.20) | 2.97 (2.40–3.66) | 2.83 (2.28–3.51) |
| Distant | 9.24 (8.31–10.3) | 6.30 (5.61–7.09) | 35.3 (28.6–43.5) | 14.7 (11.5–18.7) | 11.1 (9.14–13.4) | 9.24 (7.45–11.4) |
| Unstaged | 2.94 (2.31–3.75) | 2.37 (1.86–3.04) | 3.07 (1.76–5.36) | 2.55 (1.45–4.48) | 3.46 (2.11–5.6) | 2.64 (1.60–4.35) |
| Grade Differentiation | ||||||
| Moderate | 2.05 (1.82–2.31) | 1.76 (1.56–1.98) | 5.41 (3.26–8.98) | 2.18 (1.31–3.64) | 1.49 (1.13–1.96) | 1.43 (1.09–1.88) |
| Poor | 5.64 (5.01–6.36) | 3.44 (3.02–3.91) | 39.9 (26.2–60.9) | 4.92 (3.17–7.65) | 4.06 (3.11–5.30) | 2.34 (1.77–3.09) |
| Undifferentiated | 5.08 (4.00–6.45) | 2.84 (2.23–3.62) | 37.2 (22.2–62.3) | 5.34 (3.14–9.08) | 4.51 (2.97–6.86) | 2.34 (1.52–3.59) |
| Unknown | 1.83 (1.63–2.05) | 1.83 (1.63–2.05) | 7.84 (5.15–12.0) | 4.08 (2.67–6.23) | 3.55 (2.69–4.68) | 2.21 (1.65–2.97) |
| Surgery (Yes) | 0.25 (0.22–0.27) | 0.49 (0.44–0.55) | 0.16 (0.13–0.20) | 0.56 (0.45–0.71) | 0.25 (0.21–0.30) | 0.55 (0.45–0.67) |
| Radiotherapy (Yes) | 1.86 (1.56–2.22) | 1.19 (0.99–1.43) * | 6.11 (4.19–8.90) | 1.58 (1.07–2.33) | 1.25 (0.97–1.63) * | 1.04 (0.80–1.36) * |
| Chemotherapy (Yes) | 3.26 (3.03–3.50) | 1.37 (1.26–1.48) | 9.05 (7.89–10.4) | 1.62 (1.36–1.93) | 2.13 (1.89–2.41) | 0.92 (0.80–1.06) * |
p < 0.05 relative to reference unless noted by * p ≥ 0.05. Reference categories: Gender (Male), Race (White), Detection Stage (Localized), Grade differentiation (Well), Surgery (No), Radiotherapy (No), and Chemotherapy (No). CI, confidence interval.
2.8. Gallbladder/Biliary
SRCCs comprised 1.3% of all cases of gallbladder/biliary cancer, and 1.6% of all SRCC cases (Table 15, Figure 2). Similar to pancreatic cancers, the relative differences between SRCCs, nonvariant adenocarcinomas, and cholangiocarcinomas are not as large as in other cancer types, likely to their poor outcome. Mean age of onset is younger for SRCCs by about 4 years. The only clinically significant histopathological difference is that most SRCCs present with poor grade relative to adenocarcinomas and cholangiocarcinomas (71.6% vs. 25.9% vs. 12.2%). SRCC patients undergo surgery more often (70.1% vs. 60.8% vs. 20.3%). SRCC have slightly worse 5 year-survival compared to adenocarcinomas (16.2% vs. 22.1%) but better than cholangiocarcinomas (16.2% vs. 8.6%) (Figure 3h, Table 15). Median survival time is 10–12.5 months across the three subtypes. When compared to all gallbladder/biliary cancers, SRCCs have a HR of 1.12 (95% CI: 1.01–1.25), and non-significant HR of 1.10 (95% CI: 0.99–1.23) to adenocarcinomas, and 1.06 (0.94–1.20) to cholangiocarcinomas, after multivariate analyses (Table 16).
Table 15.
Baseline demographics and clinical characteristics by histology for gallbladder/biliary cancers.
| Gallbladder/Biliary | All | Adenocarcinoma | Cholangiocarcinoma | Signet Ring |
|---|---|---|---|---|
| N | 41,289 (100) | 23,923 (57.9) | 7483 (18.1) | 525 (1.3) |
| Age (Years) (%) | ||||
| 0–14 | 13 (<0.1) | 1 (<0.1) | 2 (<0.1) | 0 (0) |
| 15–29 | 120 (0.3) | 59 (0.2) | 17 (0.2) | 7 (1.3) |
| 30–49 | 2927 (7.1) | 1674 (7.0) | 477 (6.4) | 50 (9.5) |
| 50–69 | 16,142 (39.1) | 9637 (40.3) | 2962 (39.6) | 241 (45.9) |
| 70–85 | 16,720 (40.5) | 9867 (41.2) | 2989 (39.9) | 180 (34.3) |
| >85 | 5367 (13.0) | 2685 (11.2) | 1036 (13.8) | 47 (9.0) |
| Mean (SD) | 69.7 (13.2) | 69.4 (12.8) | 69.9 (13.1) | 66.5 (13.7) |
| Gender (%) | ||||
| Male | 17,677 (42.8) | 9858 (41.2) | 3766 (50.3) | 211 (40.2) |
| Female | 23,612 (57.2) | 14,065 (58.8) | 3717 (49.7) | 314 (59.8) |
| Race (%) | ||||
| White | 32,074 (77.7) | 18,724 (78.3) | 5757 (76.9) | 397 (75.6) |
| Black | 3980 (9.6) | 2335 (9.8) | 631 (8.4) | 65 (12.4) |
| Other | 5235 (12.7) | 2864 (12.0) | 1095 (14.6) | 63 (12.0) |
| Detection Stage (%) | ||||
| In Situ | 926 (2.2) | 389 (1.6) | 2 (<0.1) | 0 (0) |
| Localized | 8653 (21.0) | 5486 (22.9) | 986 (13.2) | 110 (21.0) |
| Regional | 13,856 (33.6) | 8713 (36.4) | 2281 (30.5) | 224 (42.7) |
| Distant | 13,012 (31.5) | 7539 (31.5) | 2756 (36.8) | 177 (33.7) |
| Unstaged | 4842 (11.7) | 1796 (7.5) | 1458 (19.5) | 14 (2.7) |
| Grade Differentiation (%) | ||||
| Well | 3503 (8.5) | 2341 (9.8) | 268 (3.6) | 4 (0.8) |
| Moderate | 10,297 (24.9) | 7690 (32.1) | 941 (12.6) | 25 (4.8) |
| Poor | 9102 (22.0) | 6190 (25.9) | 915 (12.2) | 376 (71.6) |
| Undifferentiated | 612 (1.5) | 210 (0.9) | 43 (0.6) | 12 (2.3) |
| Unknown | 17,775 (43.1) | 7492 (31.3) | 5316 (71.0) | 108 (20.6) |
| Surgery (%) | ||||
| Yes | 21,334 (51.7) | 14,545 (60.8) | 1516 (20.3) | 368 (70.1) |
| No | 19,955 (48.3) | 9378 (39.2) | 5967 (79.7) | 157 (29.9) |
| Radiotherapy (%) | ||||
| Yes | 6274 (15.2) | 3961 (16.6) | 1175 (15.7) | 104 (19.8) |
| No | 35,015 (84.8) | 19,962 (83.4) | 6308 (84.3) | 421 (80.2) |
| Chemotherapy (%) | ||||
| Yes | 12,898 (31.2) | 7965 (33.3) | 2711 (36.2) | 203 (38.7) |
| No | 28,391 (68.8) | 15,958 (66.7) | 4772 (63.8) | 322 (61.3) |
| Incidence Rate (95% CI) | ||||
| All | 2.99 (2.96–3.02) | 1.70 (1.67–1.72) | 6.2 (6.0–6.3) † | 3.9 (3.6–4.2) †† |
| Male | 3.09 (3.04–3.13) | 1.69 (1.65–1.72) | 7.3 (7.1–7.5) † | 3.4 (2.9–3.8) †† |
| Female | 2.94 (2.90–2.97) | 1.72 (1.69–1.75) | 5.3 (5.1–5.5) † | 4.3 (3.9–4.8) †† |
| CSS % (95% CI) | ||||
| 1-year | 47.9 (47.4–48.5) | 51.0 (50.3–51.8) | 37.0 (35.8–38.2) | 45.6 (40.7–50.4) |
| 2-year | 32.3 (31.7–32.8) | 34.7 (34.0–35.5) | 18.6 (17.5–19.6) | 31.2 (26.5–36.0) |
| 5-year | 20.7 (20.2–21.3) | 22.1 (21.4–22.8) | 8.6 (7.8–9.5) | 16.2 (12.3–20.5) |
| 10-year | 17.3 (16.7–17.8) | 18.4 (17.7–19.2) | 6.5 (5.7–7.4) | 12.6 (9.0–16.9) |
| Median (Months) | 11.0 | 12.5 | 7.2 | 10.2 |
| RS % (95% CI) | ||||
| 1-year | 45.9 (45.3–46.4) | 49.1 (48.3–49.8) | 35.1 (33.9–36.3) | 42.0 (37.3–46.6) |
| 2-year | 30.2 (29.7–30.8) | 32.6 (31.9–33.4) | 17.1 (16.1–18.1) | 27.6 (23.2–32.1) |
| 5-year | 18.5 (18.0–19.0) | 19.8 (19.2–20.6) | 7.4 (6.7–8.2) | 13.6 (10.1–17.5) |
| 10-year | 14.5 (13.9–15.1) | 15.5 (14.7–16.4) | 4.9 (4.1–5.7) | 10.1 (6.5–14.5) |
| Median (Months) | 10.1 | 11.6 | 6.6 | 9.2 |
p < 0.05 for all comparisons among adenocarcinoma, cholangiocarcinoma, and signet ring cell comparisons. Incidence rates expressed per 100,000, except † (per 1 million) and †† (per 10 million). CSS, cause-specific survival; RS, relative survival; CI, confidence interval.
Table 16.
Derived univariate and multivariable Cox-proportional hazard ratios (HR) of mortality for gallbladder/biliary cancers.
| Gallbladder/Biliary | Signet Ring vs. Non-Signet Ring | Signet Ring vs. Adenocarcinoma | Signet Ring vs. Cholangiocarcinoma | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | Univariate | Multivariable | Univariate | Multivariable | Univariate | Multivariable |
| Signet Ring Histology | 1.16 (1.05–1.30) | 1.12 (1.01–1.25) | 1.21 (1.09–1.35) | 1.10 (0.99–1.23) * | 0.78 (0.70–0.87) | 1.06 (0.94–1.20) * |
| Age (per 10 years) | 1.17 (1.16–1.18) | 1.15 (1.14–1.16) | 1.14 (1.13–1.16) | 1.15 (1.13–1.16) | 1.15 (1.12–1.17) | 1.11 (1.09–1.14) |
| Gender (Female) | 1.07 (1.04–1.09) | 1.05 (1.03–1.08) | 1.08 (1.05–1.12) | 1.07 (1.03–1.11) | 1.19 (1.13–1.25) | 1.05 (0.99–1.11) * |
| Race | ||||||
| Black | 1.04 (1.00–1.09) * | 1.05 (1.01–1.10) | 1.11 (1.05–1.17) | 1.09 (1.03–1.15) | 1.04 (0.94–1.15) * | 1.00 (0.90–1.10) * |
| Other | 0.92 (0.88–0.95) | 0.94 (0.91–0.98) | 0.92 (0.87–0.96) | 0.94 (0.90–0.99) | 0.93 (0.86–1.00) * | 0.92 (0.85–0.99) |
| Detection Stage | ||||||
| In Situ | 0.17 (0.14–0.20) | 0.17 (0.14–0.21) | 0.18 (0.13–0.24) | 0.17 (0.13–0.23) | 0.34 (0.05–2.45) * | 0.64 (0.09–4.56) |
| Regional | 1.59 (1.53–1.65) | 1.73 (1.66–1.80) | 1.56 (1.49–1.64) | 1.72 (1.63–1.80) | 0.91 (0.84–1.00) * | 1.32 (1.21–1.45) |
| Distant | 3.99 (3.84–4.14) | 3.28 (3.15–3.43) | 4.07 (3.88–4.27) | 3.48 (3.30–3.67) | 2.00 (1.84–2.18) | 2.25 (2.05–2.47) |
| Unstaged | 2.72 (2.59–2.86) | 1.45 (1.37–1.52) | 2.76 (2.58–2.97) | 1.47 (1.36–1.59) | 1.40 (1.26–1.55) | 1.10 (0.99–1.21) * |
| Grade Differentiation | ||||||
| Moderate | 1.41 (1.34–1.49) | 1.30 (1.23–1.38) | 1.33 (1.25–1.42) | 1.26 (1.18–1.35) | 1.08 (0.91–1.27) * | 1.08 (0.92–1.28) * |
| Poor | 2.32 (2.19–2.45) | 1.92 (1.81–2.03) | 2.15 (2.02–2.30) | 1.87 (1.75–2.00) | 1.49 (1.27–1.76) | 1.40 (1.19–1.66) |
| Undifferentiated | 2.25 (2.01–2.52) | 1.86 (1.66–2.08) | 2.09 (1.76–2.49) | 1.86 (1.56–2.22) | 1.61 (1.10–2.34) | 1.02 (0.69–1.48) * |
| Unknown | 2.76 (2.62–2.91) | 1.46 (1.38–1.55) | 2.77 (2.59–2.95) | 1.51 (1.41–1.62) | 2.10 (1.81–2.45) | 1.15 (0.98–1.35) * |
| Surgery (Yes) | 0.32 (0.31–0.33) | 0.43 (0.42–0.45) | 0.33 (0.32–0.34) | 0.45 (0.43–0.47) | 0.39 (0.36–0.41) | 0.44 (0.40–0.48) |
| Radiotherapy (Yes) | 0.82 (0.79–0.85) | 1.02 (0.98–1.06) * | 0.82 (0.78–0.85) | 1.03 (0.99–1.08) * | 0.63 (0.59–0.68) | 0.95 (0.88–1.03) * |
| Chemotherapy (Yes) | 1.05 (1.03–1.08) | 0.74 (0.72–0.76) | 1.05 (1.01–1.08) | 0.71 (0.69–0.74) | 0.73 (0.69–0.77) | 0.66 (0.62–0.71) |
p < 0.05 relative to reference unless noted by * p ≥ 0.05. Reference categories: Gender (Male), Race (White), Detection Stage (Localized), Grade differentiation (Well), Surgery (No), Radiotherapy (No), and Chemotherapy (No). CI, confidence interval.
2.9. Breast
SRCC comprise 0.03% of all cases of breast cancer, and 1.5% of all SRCC cases (Table 17, Figure 2). When compared to ductal and lobular cancers, SRCC have an older age of onset by about 7 years, unique among the SRCCs. Nearly a third of SRCCs are detected at distant/metastatic stage, whereas less than 5% of ductal and lobular cancers present at this stage. These patients are somewhat less likely to receive surgery (71.9% vs. ~94–95% for ductal and lobular cancers), likely due to increase likelihood of metastatic presentations. SRCCs have much worse 5-year (65.1% vs. ~90%) and 10-year (55.1% vs. ~82%) survivals relative to both ductal and lobular cancers (Figure 3i, Table 17). SRCCs have a very high mortality HR of 3.63 (95% CI: 3.09–4.27) and 4.65 (95% CI: 3.96–5.47) compared to breast and lobular cancers, respectively, on univariate analysis. However, after multivariable analysis, the HR of mortality for SRCCs compared to ductal cancers is equivalent (1.16 (95% CI: 0.98–1.36)), and marginally statistically increased for lobular cancers (1.19 (95% CI 1.01–1.40)) (Table 18).
Table 17.
Baseline demographics and clinical characteristics by histology for breast cancers.
| Breast | All | Ductal | Lobular | Signet Ring |
|---|---|---|---|---|
| N | 1,185,521 (100) | 813,140 (68.6) | 245,539 (20.7) | 384 (0.03) |
| Age (Years) (%) | ||||
| 0–14 | 17 (<0.1) | 6 (<0.1) | 0 (0) | 0 (0) |
| 15–29 | 6339 (0.5) | 4862 (0.6) | 508 (0.2) | 1 (0.3) |
| 30–49 | 283,566 (23.9) | 202,015 (25.0) | 55,048 (22.4) | 34 (8.9) |
| 50–69 | 581,741 (49.1) | 399,863 (49.0) | 124,886 (50.9) | 181 (47.1) |
| 70–85 | 265,451 (22.4) | 176,716 (21.8) | 55,945 (22.8) | 131 (34.1) |
| >85 | 48,407 (4.1) | 29,678 (3.7) | 9152 (3.7) | 37 (9.6) |
| Mean (SD) | 60.2 (13.7) | 59.7 (13.7) | 60.7 (13.1) | 67.2 (13.2) |
| Gender (%) | ||||
| Male | 7059 (0.6) | 5958 (0.7) | 541 (0.2) | 4 (1.0) |
| Female | 1,178,012 (99.4) | 807,182 (99.3) | 244,998 (99.8) | 380 (99.0) |
| Race (%) | ||||
| White | 956,313 (80.7) | 650,557 (80.0) | 205,120 (83.5) | 338 (88.0) |
| Black | 124,772 (10.5) | 88,018 (10.8) | 21,734 (8.9) | 27 (7.0) |
| Other | 104,436 (8.8) | 74,565 (9.2) | 18,685 (7.6) | 19 (4.9) |
| Detection Stage (%) | ||||
| In Situ | 231,711 (18.0) | 107,886 (13.3) | 75,431 (30.7) | 1 (0.3) |
| Localized | 589,407 (49.7) | 435,830 (53.6) | 100,852 (41.1) | 151 (39.3) |
| Regional | 301,018 (25.4) | 225,149 (27.7) | 58,965 (24.0) | 110 (28.6) |
| Distant | 63,128 (5.3) | 36,705 (4.5) | 8696 (3.5) | 114 (29.7) |
| Unstaged | 18,257 (1.5) | 7570 (0.9) | 1595 (0.6) | 8 (2.1) |
| Grade Differentiation (%) | ||||
| Well | 205,026 (17.3) | 133,481 (16.4) | 44,918 (18.3) | 14 (3.6) |
| Moderate | 436,567 (36.8) | 305,331 (37.5) | 102,616 (41.8) | 127 (33.1) |
| Poor | 357,949 (30.2) | 287,496 (35.4) | 42,394 (17.3) | 123 (32.0) |
| Undifferentiated | 28,401 (2.4) | 18,932 (2.3) | 5421 (2.2) | 15 (3.9) |
| Unknown | 157,578 (13.3) | 67,900 (8.4) | 50,190 (20.4) | 105 (27.3) |
| Surgery (%) | ||||
| Yes | 1,105,455 (93.2) | 768,601 (94.5) | 233,092 (94.9) | 276 (71.9) |
| No | 80,066 (6.8) | 44,539 (5.5) | 12,447 (5.1) | 108 (28.1) |
| Radiotherapy (%) | ||||
| Yes | 555,742 (46.9) | 399,316 (49.1) | 105,369 (42.9) | 144 (37.5) |
| No | 629,779 (53.1) | 413,824 (50.9) | 140,170 (57.1) | 240 (62.5) |
| Chemotherapy (%) | ||||
| Yes | 387,251 (32.7) | 297,100 (36.5) | 61,058 (24.9) | 138 (35.9) |
| No | 798,270 (67.3) | 516,040 (63.5) | 184,481 (75.1) | 246 (64.1) |
| Incidence Rate (95% CI) | ||||
| All | 68.1 (68.0–68.2) | 48.6 (48.5–48.7) | 12.69 (12.63–12.75) | 2.6 (2.3–2.9) †† |
| Male | 11.6 (11.3–11.9) † | 9.4 (9.2–9.7) † | 6.8 (6.1–7.4) †† | 7.5 (2.4–17.6) ††† |
| Female | 126.3 (126.0–126.5) | 90.4 (90.2–90.6) | 23.5 (23.4–23.6) | 4.6 (4.2–5.1) †† |
| CSS % (95% CI) | ||||
| 1-year | 96.35 (96.30–96.40) | 97.21 (97.16–97.26) | 97.96 (97.88–98.04) | 88.3 (83.7–91.6) |
| 2-year | 93.57 (93.51–93.64) | 94.5 (94.4–94.6) | 96.1 (96.0–96.2) | 80.2 (74.7–84.6) |
| 5-year | 87.0 (86.9–87.1) | 88.0 (87.9–88.1) | 90.1 (89.9–90.3) | 65.1 (58.6–70.9) |
| 10-year | 80.5 (80.3–80.6) | 81.7 (81.5–81.9) | 82.6 (82.3–82.8) | 55.1 (48.1–61.6) |
| Median (Months) | - | - | - | - |
| RS % (95% CI) | ||||
| 1-year | 96.93 (96.87–96.99) | 97.93 (97.86–98.00) | 98.9 (98.8–99.0) | 87.5 (82.5–91.2) |
| 2-year | 94.7 (94.6–94.8) | 95.8 (95.7–95.9) | 97.8 (97.7–98.0) | 80.3 (73.9–85.2) |
| 5-year | 89.2 (89.0–89.3) | 90.3 (90.2–90.5) | 93.3 (93.0–93.6) | 63.4 (55.6–70.2) |
| 10-year | 83.0 (82.8–83.3) | 84.5 (84.1–84.8) | 86.4 (85.8–87.0) | 51.6 (41.5–60.8) |
| Median (Months) | - | - | - | - |
p < 0.05 for all comparisons among ductal, lobular, and signet ring cell comparisons. Incidence rates expressed per 100,000, except † (per 1 million), †† (per 10 million), and ††† (per 1 billion). CSS, cause-specific survival; RS, relative survival; CI, confidence interval.
Table 18.
Derived univariate and multivariable Cox-proportional hazard ratios (HR) of mortality for breast cancers.
| Breast | Signet Ring vs. Non-Signet Ring | Signet Ring vs. Ductal | Signet Ring vs. Lobular | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | Univariate | Multivariable | Univariate | Multivariable | Univariate | Multivariable |
| Signet Ring Histology | 3.58 (3.04–4.20) | 1.13 (0.96–1.32) * | 3.63 (3.09–4.27) | 1.16 (0.98–1.36) * | 4.65 (3.96–5.47) | 1.19 (1.01–1.40) |
| Age (per 10 years) | 1.149 (1.145–1.154) | 1.218 (1.213–1.223) | 1.094 (1.089–1.099) | 1.196 (1.190–1.202) | 1.261 (1.248–1.274) | 1.274 (1.260–1.288) |
| Gender (Male) | 1.61 (1.52–1.70) | 1.08 (1.02–1.14) | 1.60 (1.51–1.71) | 1.11 (1.04–1.18) | 1.26 (0.96–1.65) * | 0.87 (0.66–1.15) * |
| Race | ||||||
| Black | 1.76 (1.73–1.78) | 1.46 (1.44–1.48) | 1.84 (1.81–1.87) | 1.49 (1.47–1.52) | 1.50 (1.44–1.56) | 1.50 (1.44–1.57) |
| Other | 0.80 (0.79–0.82) | 0.88 (0.86–0.89) | 0.84 (0.82–0.86) | 0.87 (0.85–0.89) | 0.71 (0.67–0.75) | 0.89 (0.84–0.95) |
| Detection Stage | ||||||
| In Situ | 0.25 (0.24–0.26) | 0.23 (0.22–0.24) | 0.29 (0.28–0.31) | 0.26 (0.25–0.27) | 0.22 (0.20–0.23) | 0.21 (0.19–0.23) |
| Regional | 3.43 (3.39–3.48) | 3.09 (3.05–3.13) | 3.31 (3.26–3.36) | 2.97 (2.92–3.02) | 3.75 (3.63–3.87) | 3.56 (3.44–3.68) |
| Distant | 22.3 (22.0–22.5) | 12.5 (12.3–12.7) | 21.0 (20.7–21.4) | 12.0 (11.8–12.3) | 28.3 (27.2–29.4) | 16.5 (15.8–17.3) |
| Unstaged | 8.62 (8.40–8.85) | 3.91 (3.81–4.03) | 6.37 (6.11–6.64) | 3.21 (3.07–3.35) | 7.52 (6.84–8.27) | 3.67 (3.33–4.06) |
| Grade Differentiation | ||||||
| Moderate | 2.31 (2.26–2.36) | 1.83 (1.79–1.87) | 2.56 (2.49–2.64) | 1.99 (1.94–2.05) | 1.63 (1.56–1.70) | 1.45 (1.39–1.52) |
| Poor | 4.68 (4.58–4.78) | 3.21 (3.13–3.28) | 5.13 (4.99–5.28) | 3.55 (3.44–3.65) | 2.55 (2.43–2.67) | 2.30 (2.20–2.41) |
| Undifferentiated | 2.48 (2.38–2.57) | 3.39 (3.26–3.52) | 2.65 (2.53–2.78) | 3.63 (3.46–3.81) | 0.94 (0.84–1.05) * | 2.20 (1.97–2.45) |
| Unknown | 3.70 (3.62–3.79) | 2.46 (2.40–2.52) | 2.93 (2.83–3.03) | 2.62 (2.53–2.71) | 1.58 (1.51–1.65) | 1.71 (1.63–1.80) |
| Surgery (Yes) | 0.118 (0.116–0.119) | 0.392 (0.385–0.398) | 0.129 (0.127–0.131) | 0.39 (0.38–0.40) | 0.136 (0.131–0.140) | 0.37 (0.35–0.39) |
| Radiotherapy (Yes) | 0.696 (0.689–0.703) | 0.805 (0.796–0.813) | 0.69 (0.68–0.70) | 0.79 (0.78–0.80) | 0.88 (0.86–0.91) | 0.85 (0.83–0.88) |
| Chemotherapy (Yes) | 2.22 (2.20–2.24) | 1.09 (1.08–1.10) | 2.13 (2.10–2.16) | 1.06 (1.04–1.08) | 2.63 (2.57–2.70) | 1.19 (1.16–1.23) |
p < 0.05 relative to reference unless noted by * p ≥ 0.05. Reference categories: Gender (Female), Race (White), Detection Stage (Localized), Grade differentiation (Well), Surgery (No), Radiotherapy (No), and Chemotherapy (No). CI, confidence interval.
2.10. Urinary Bladder
SRCCs comprised 0.2% of all cases of urinary bladder cancer, and 1.3% of all SRCC cases (Table 19, Figure 2). Transition cell carcinomas comprise 94% of all urinary bladder cases, and adenocarcinomas 0.5% of all cases. Mean age of onset is younger for SRCCs by 5.6 years and 3.5 years compared to transition cell and adenocarcinomas, respectively. SRCCs primarily present with localized and regional disease, predominantly with poor grade. SRCC have much worse 5 year-survival compared to transition cell and adenocarcinomas (28.3% vs. 49.4% vs. 82.0%), respectively. (Figure 3j, Table 19). Median survival time is 15.6 months for SRCCs, and 57.6 months for adenocarcinomas. When compared to all other urinary cancers, SRCCs have a HR of 4.83 (95% CI: 1.01–1.25) on univariate analysis, 1.56 (95% CI: 1.11–1.54), after multivariate analyses (Table 20).
Table 19.
Baseline demographics and clinical characteristics by histology for urinary bladder cancers.
| Urinary Bladder | All | Transition Cell | Adenocarcinoma | Signet Ring |
|---|---|---|---|---|
| N | 252,104 (100) | 237,005 (94.0) | 1330 (0.5) | 380 (0.2) |
| Age (Years) (%) | ||||
| 0–14 | 92 (<0.1) | 22 (<0.1) | 0 (0) | 0 (0) |
| 15–29 | 844 (0.3) | 767 (0.3) | 16 (1.2) | 1 (0.3) |
| 30–49 | 14,211 (5.6) | 13,146 (5.5) | 167 (12.6) | 52 (13.7) |
| 50–69 | 101,475 (40.3) | 96,290 (40.6) | 528 (39.7) | 187 (49.2) |
| 70–85 | 107,689 (42.7) | 101,623 (42.9) | 471 (35.4) | 122 (32.1) |
| >85 | 27,793 (11.0) | 25,157 (10.6) | 148 (11.1) | 18 (4.7) |
| Mean (SD) | 69.8 (12.5) | 69.7 (12.3) | 66.7 (15.1) | 64.1 (12.7) |
| Gender (%) | ||||
| Male | 189,668 (75.2) | 180,006 (76.0) | 846 (63.6) | 269 (70.8) |
| Female | 62,436 (24.8) | 56,999 (24.0) | 484 (36.4) | 111 (29.2) |
| Race (%) | ||||
| White | 226,912 (90.0) | 214,042 (90.3) | 1040 (78.2) | 316 (83.2) |
| Black | 13,717 (5.4) | 12,259 (5.2) | 194 (14.6) | 45 (11.8) |
| Other | 11,475 (4.6) | 10,704 (4.5) | 96 (7.2) | 19 (5.0) |
| Detection Stage (%) | ||||
| In Situ | 6454 (2.6) | 6386 (2.7) | 1 (0.1) | 0 (0) |
| Localized | 180,673 (71.7) | 176,458 (74.5) | 354 (26.6) | 52 (13.7) |
| Regional | 46,523 (18.5) | 41,382 (17.5) | 608 (45.7) | 203 (53.4) |
| Distant | 10,761 (4.3) | 8002 (3.4) | 294 (22.1) | 116 (30.5) |
| Unstaged | 7963 (3.1) | 4777 (2.0) | 73 (5.5) | 9 (2.4) |
| Grade Differentiation (%) | ||||
| Well | 32,449 (12.9) | 31,563 (13.3) | 64 (4.8) | 1 (0.3) |
| Moderate | 71,047 (28.2) | 68,936 (29.1) | 405 (30.5) | 7 (1.8) |
| Poor | 52,063 (20.7) | 48,571 (20.5) | 456 (34.3) | 228 (60.0) |
| Undifferentiated | 58,654 (23.3) | 56,559 (23.9) | 108 (8.1) | 66 (17.4) |
| Unknown | 37,891 (15.0) | 31,376 (13.2) | 297 (22.3) | 78 (20.5) |
| Surgery (%) | ||||
| Yes | 234,703 (93.1) | 224,146 (94.6) | 1137 (85.5) | 325 (85.5) |
| No | 17,401 (6.9) | 12,859 (5.4) | 193 (14.5) | 55 (14.5) |
| Radiotherapy (%) | ||||
| Yes | 11,546 (4.6) | 9787 (4.1) | 171 (12.9) | 78 (20.5) |
| No | 240,558 (95.4) | 227,218 (95.9) | 1159 (87.1) | 302 (79.5) |
| Chemotherapy (%) | ||||
| Yes | 42,371 (16.8) | 39,255 (16.6) | 307 (23.1) | 163 (42.9) |
| No | 209,733 (83.2) | 197,750 (83.4) | 1023 (76.9) | 217 (57.1) |
| Incidence Rate (95% CI) | ||||
| All | 20.45 (20.37–20.52) | 19.04 (18.97–19.12) | 1.07 (1.02–1.13) † | 3.0 (2.7–3.3) †† |
| Male | 36.1 (35.9–36.2) | 33.9 (33.7–34.0) | 1.62 (1.52–1.72) † | 4.8 (4.2–5.3) †† |
| Female | 8.82 (8.75–7.88) | 7.98 (7.92–8.05) | 0.67 (0.62–0.73) † | 1.5 (1.3–1.8) †† |
| CSS % (95% CI) | ||||
| 1-year | 91.0 (90.8–91.1) | 92.6 (92.5–92.7) | 73.5 (70.5–76.1) | 59.8 (54.0–65.1) |
| 2-year | 86.2 (86.0–86.3) | 88.1 (88.0–88.3) | 63.6 (60.4–66.6) | 42.0 (36.1–47.8) |
| 5-year | 80.0 (79.7–80.1) | 82.0 (81.9–82.2) | 49.4 (45.7–52.9) | 28.3 (22.7–34.1) |
| 10-year | 74.0 (73.8–74.3) | 76.1 (75.8–76.3) | 41.6 (37.4–45.7) | 22.2 (16.7–28.2) ^ |
| Median (Months) | - | - | 57.6 | 15.6 |
| RS % (95% CI) | ||||
| 1-year | 90.1 (90.0–90.2) | 92.0 (91.8–92.1) | 70.2 (67.2–73.0) | 57.1 (51.3–62.6) |
| 2-year | 85.2 (85.0–85.4) | 87.4 (87.2–87.6) | 59.4 (56.1–62.6) | 38.0 (32.2–43.9) |
| 5-year | 78.6 (78.4–78.9) | 81.0 (80.7–81.3) | 43.3 (39.4–47.1) | 24.3 (19.0–29.9) |
| 10-year | 71.4 (71.0–71.8) | 73.7 (73.3–74.1) | 36.5 (32.0–41.1) | 16.3 (11.2–22.4) ^ |
| Median (Months) | - | - | 42.9 | 14.4 |
p < 0.05 for all comparisons among transition cell, adenocarcinoma, and signet ring cell comparisons. Incidence rates expressed per 100,000, except † (per 1 million) and †† (per 10 million). CSS, cause-specific survival; RS, relative survival; ^ (not age standardized); CI, confidence interval.
Table 20.
Derived univariate and multivariable Cox-proportional hazard ratios (HR) of mortality for urinary bladder cancers.
| Urinary Bladder | Signet Ring vs. Non-Signet Ring | Signet Ring vs. Transition Cell | Signet Ring vs. Adenocarcinoma | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | Univariate | Multivariable | Univariate | Multivariable | Univariate | Multivariable |
| Signet Ring Histology | 4.83 (4.25–5.50) | 1.56 (1.37–1.78) | 5.43 (4.77–6.17) | 1.70 (1.49–1.93) | 1.74 (1.50–2.03) | 1.31 (1.11–1.54) |
| Age (per 10 years) | 1.49 (1.48–1.50) | 1.47 (1.46–1.48) | 1.52 (1.51–1.53) | 1.50 (1.48–1.51) | 1.15 (1.10–1.21) | 1.21 (1.14–1.27) |
| Gender (Female) | 1.27 (1.25–1.30) | 1.09 (1.07–1.11) | 1.19 (1.17–1.22) | 1.05 (1.03–1.07) | 1.26 (1.09–1.45) | 1.11 (0.96–1.29) * |
| Race | ||||||
| Black | 1.70 (1.65–1.75) | 1.42 (1.37–1.46) | 1.67 (1.61–1.73) | 1.44 (1.39–1.50) | 1.09 (0.89–1.32) * | 1.32 (1.09–1.62) |
| Other | 1.01 (0.96–1.05) * | 0.88 (0.84–0.91) | 1.00 (0.95–1.04) * | 0.88 (0.84–0.92) | 0.72 (0.52–0.99) | 0.88 (0.64–1.20) * |
| Detection Stage | ||||||
| In Situ | 0.23 (0.15–0.34) | 0.24 (0.16–0.36) | 0.26 (0.18–0.39) | 0.27 (0.18–0.40) | - | - |
| Regional | 6.56 (6.44–6.69) | 4.59 (4.50–4.70) | 6.66 (6.53–6.80) | 4.36 (4.27–4.47) | 2.38 (1.92–2.95) | 2.22 (1.77–2.80) |
| Distant | 26.9 (26.1–27.6) | 19.5 (18.9–20.1) | 28.6 (27.7–29.5) | 19.4 (18.8–20.1) | 8.64 (6.87–10.9) | 6.89 (5.34–8.89) |
| Unstaged | 4.17 (3.99–4.35) | 2.82 (2.69–2.95) | 2.99 (2.82–3.17) | 2.27 (2.13–2.42) | 2.17 (1.43–3.30) | 1.51 (0.98–2.32) * |
| Grade Differentiation | ||||||
| Moderate | 1.58 (1.51–1.65) | 1.42 (1.36–1.49) | 1.56 (1.49–1.64) | 1.43 (1.36–1.50) | 1.61 (0.96–2.70) * | 1.23 (0.73–2.08) * |
| Poor | 6.23 (5.97–6.50) | 2.68 (2.56–2.80) | 6.38 (6.10–6.67) | 2.84 (2.71–2.97) | 3.74 (2.27–6.16) | 2.28 (1.37–3.79) |
| Undifferentiated | 6.70 (6.42–7.00) | 2.63 (2.51–2.75) | 7.21 (6.89–7.54) | 2.86 (2.73–3.00) | 2.70 (1.58–4.61) | 1.93 (1.12–3.32) |
| Unknown | 3.47 (3.31–3.64) | 2.05 (1.95–2.15) | 2.76 (2.62–2.90) | 1.96 (1.86–2.06) | 2.47 (1.47–4.13) | 1.50 (0.89–2.52) * |
| Surgery (Yes) | 0.49 (0.48–0.51) | 0.64 (0.62–0.66) | 0.63 (0.61–0.65) | 0.68 (0.66–0.71) | 0.35 (0.29–0.42) | 0.55 (0.44–0.68) |
| Radiotherapy (Yes) | 5.32 (5.18–5.45) | 1.27 (1.24–1.31) | 5.80 (5.64–5.96) | 1.28 (1.25–1.32) | 1.88 (1.57–2.24) | 1.17 (0.97–1.41) * |
| Chemotherapy (Yes) | 2.19 (2.15–2.24) | 0.97 (0.94–0.99) | 2.26 (2.22–2.31) | 0.99 (0.96–1.01) * | 1.78 (1.54–2.05) | 0.93 (0.79–1.10) * |
p < 0.05 relative to reference unless noted by * p ≥ 0.05. Reference categories: Gender (Male), Race (White), Detection Stage (Localized), Grade differentiation (Well), Surgery (No), Radiotherapy (No), and Chemotherapy (No). CI, confidence interval.
2.11. Small Bowel
SRCCs comprise 1.1% of all cases of small bowel cancer, and 1.3% of all SRCC cases (Table 21, Figure 2). Data for carcinoid tumors is presented as this is the most common cancer subtype at 53.4% of cases. When compared to nonvariant adenocarcinomas, SRCCs have an earlier mean age of onset of 3.7 years like appendiceal cancers, but a near identical age compared to carcinoids. There is no overt gender bias. Relative to adenocarcinomas, appendiceal SRCCs present with slightly increased rates of regional and distant disease (~80% vs. ~70%) and poor grade (70.0% vs. 30.8%). SRCCs have worse 5-year survival relative to adenocarcinomas and carcinoids (13.8% vs. 23.1% vs. 74.7%), respectively (Figure 3k, Table 21). Median survival time is 14 months for SRCCs and 16.2 months for adenocarcinomas. When compared to all small bowel cancers, SRCCs have a HR of 1.64 (95% CI: 1.43–1.88), 4.47 (95% CI: 3.57–5.60) to carcinoids, and 1.23 (1.06–1.41) to adenocarcinomas, after multivariate analyses (Table 22).
Table 21.
Baseline demographics and clinical characteristics by histology for small bowel cancers.
| Small Bowel | All | Carcinoid | Adenocarcinoma | Signet Ring |
|---|---|---|---|---|
| N | 25,899 (100) | 13,837 (53.4) | 6111 (23.6) | 327 (1.3) |
| Age (Years) (%) | ||||
| 0–14 | 19 (0.1) | 4 (<0.1) | 0 (0) | 0 (0) |
| 15–29 | 248 (1.0) | 113 (0.8) | 42 (0.7) | 5 (1.5) |
| 30–49 | 3912 (15.1) | 2091 (15.1) | 794 (13.0) | 55 (16.8) |
| 50–69 | 12,530 (48.4) | 7337 (53.0) | 2533 (41.4) | 157 (48.0) |
| 70–85 | 7567 (29.2) | 3725 (26.9) | 2129 (34.8) | 90 (27.5) |
| >85 | 1623 (6.3) | 567 (4.2) | 613 (10.0) | 20 (6.1) |
| Mean (SD) | 63.6 (14.1) | 62.5 (13.1) | 66.4 (14.3) | 62.7 (14.3) |
| Gender (%) | ||||
| Male | 13,517 (52.2) | 7074 (51.1) | 3244 (53.1) | 185 (56.6) |
| Female | 12,382 (47.8) | 6763 (48.9) | 2867 (46.6) | 142 (43.4) |
| Race (%) | ||||
| White | 20,207 (78.0) | 11,066 (80.0) | 4521 (74.0) | 263 (80.4) |
| Black | 4180 (16.1) | 2305 (16.7) | 1136 (18.6) | 39 (11.9) |
| Other | 1512 (5.8) | 466 (3.4) | 454 (7.4) | 25 (7.6) |
| Detection Stage (%) | ||||
| In Situ | 188 (0.7) | 10 (0.1) | 32 (0.5) | 0 (0) |
| Localized | 8057 (31.1) | 4662 (33.7) | 1237 (20.2) | 33 (10.1) |
| Regional | 8590 (33.2) | 4980 (36.0) | 2100 (34.4) | 142 (43.4) |
| Distant | 7177 (27.7) | 3359 (24.3) | 2227 (36.4) | 132 (40.4) |
| Unstaged | 1887 (7.3) | 826 (6.0) | 515 (8.4) | 20 (6.1) |
| Grade Differentiation (%) | ||||
| Well | 6349 (24.5) | 5293 (38.3) | 453 (7.4) | 0 (0) |
| Moderate | 4867 (18.8) | 1235 (8.9) | 2559 (41.9) | 16 (4.9) |
| Poor | 3101 (12.0) | 185 (1.3) | 1880 (30.8) | 229 (70.0) |
| Undifferentiated | 515 (2.0) | 52 (0.4) | 62 (1.0) | 9 (2.8) |
| Unknown | 11,067 (42.7) | 7072 (51.1) | 1157 (18.9) | 73 (22.3) |
| Surgery (%) | ||||
| Yes | 20,068 (77.5) | 11,733 (84.8) | 3671 (60.1) | 219 (67.0) |
| No | 5831 (22.5) | 2104 (15.2) | 2440 (39.9) | 108 (33.0) |
| Radiotherapy (%) | ||||
| Yes | 993 (3.8) | 134 (1.0) | 604 (9.9) | 34 (10.4) |
| No | 24,906 (96.2) | 13,703 (99.0) | 5507 (90.1) | 293 (89.6) |
| Chemotherapy (%) | ||||
| Yes | 5280 (20.4) | 724 (5.2) | 2452 (40.1) | 160 (48.9) |
| No | 20,619 (79.6) | 13,113 (94.8) | 3659 (59.9) | 167 (51.1) |
| Incidence Rate (95% CI) | ||||
| All | 2.11 (2.08–2.13) | 1.12 (1.11–1.14) | 5.2 (5.1–5.4) † | 2.6 (2.4–2.9) †† |
| Male | 2.49 (2.45–2.53) | 1.29 (1.26–1.32) | 6.4 (6.2–6.6) † | 3.3 (2.9–3.8) †† |
| Female | 1.81 (1.78–1.84) | 0.99 (0.97–1.01) | 4.3 (4.1–4.4) † | 2.1 (1.8–2.4) †† |
| CSS % (95% CI) | ||||
| 1-year | 80.9 (80.4–81.5) | 94.9 (94.4–95.3) | 56.1 (54.7–57.5) | 54.2 (47.7–60.2) |
| 2-year | 74.5 (73.9–75.1) | 92.4 (91.8–92.9) | 41.8 (40.3–43.2) | 28.6 (22.8–34.8) |
| 5-year | 64.8 (64.1–65.5) | 85.0 (84.2–85.8) | 27.4 (26.0–28.9) | 15.5 (10.7–21.0) |
| 10-year | 56.1 (55.2–57.0) | 74.7 (73.3–75.9) | 23.1 (21.7–24.6) | 13.8 (9.2–19.3) |
| Median (Months) | - | - | 16.2 | 14 |
| RS % (95% CI) | ||||
| 1-year | 78.7 (78.1–79.3) | 93.2 (92.6–93.8) | 53.7 (52.3–55.1) | 50.8 (44.4–56.8) |
| 2-year | 72.5 (71.8–73.2) | 91.0 (90.2–91.7) | 39.6 (38.2–41.0) | 25.9 (20.4–31.7) |
| 5-year | 63.4 (62.5–64.2) | 84.3 (83.1–85.5) | 26.1 (24.6–27.5) | 13.8 (9.5–19.0) |
| 10-year | 53.2 (51.9–54.5) | 71.8 (69.5–73.9) | 21.4 (19.8–23.2) | 10.2 (6.3–15.2) |
| Median (Months) | - | - | 14.4 | 13 |
p < 0.05 for all comparisons among carcinoid, adenocarcinoma, and signet ring cell comparisons. Incidence rates expressed per 100,000, except † (per 1 million) and †† (per 10 million). CSS, cause-specific survival; RS, relative survival; CI, confidence interval.
Table 22.
Derived univariate and multivariable Cox-proportional hazard ratios (HR) of mortality for small bowel cancers.
| Small Bowel | Signet Ring vs non-Signet Ring | Signet Ring vs Carcinoid | Signet Ring vs Adenocarcinoma | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | Univariate | Multivariable | Univariate | Multivariable | Univariate | Multivariable |
| Signet Ring Histology | 4.10 (3.59–4.69) | 1.64 (1.43–1.88) | 12.9 (11.2–14.9) | 4.47 (3.57–5.60) | 1.35 (1.18–1.54) | 1.23 (1.06–1.41) |
| Age (per 10 years) | 1.31 (1.29–1.34) | 1.32 (1.30–1.35) | 1.36 (1.32–1.41) | 1.46 (1.41–1.51) | 1.20 (1.17–1.23) | 1.15 (1.12–1.18) |
| Gender (Female) | 0.97 (0.93-1.02) * | 0.94 (0.90–0.98) | 1.06 (0.98–1.15) | 0.99 (0.92–1.08) * | 1.02 (0.95–1.09) * | 1.00 (0.94–1.07) * |
| Race | ||||||
| Black | 1.02 (0.96-1.08) * | 1.10 (1.03–1.17) | 0.75 (0.66–0.85) | 1.00 (0.88-1.13) * | 1.01 (0.93–1.10) * | 1.02 (0.93–1.11) * |
| Other | 1.15 (1.05-1.27) | 0.99 (0.90–1.08) * | 0.71 (0.54–0.92) | 0.73 (0.56–0.96) | 0.97 (0.85–1.10) * | 0.88 (0.77–1.00) * |
| Detection Stage | ||||||
| In Situ | 1.09 (0.74-1.61) * | 0.91 (0.61–1.34) * | 1.94 (0.27-13.9) * | 1.41 (0.20-10.1) * | 0.88 (0.46–1.71) * | 0.69 (0.36–1.34) * |
| Regional | 2.20 (2.05–2.36) | 2.06 (1.91–2.21) | 2.78 (2.39–3.23) | 2.99 (2.57–3.49) | 1.79 (1.61–2.00) | 2.03 (1.81–2.27) |
| Distant | 5.91 (5.53–6.32) | 4.62 (4.31–4.96) | 9.64 (8.38–11.1) | 8.90 (7.71–10.3) | 5.10 (4.58–5.67) | 4.53 (4.03–5.09) |
| Unstaged | 3.35 (3.02–3.71) | 1.93 (1.73–2.15) | 2.94 (2.32–3.73) | 1.82 (1.42–2.32) | 3.72 (3.20–4.34) | 1.95 (1.66–2.28) |
| Grade Differentiation | ||||||
| Moderate | 3.96 (3.63–4.32) | 3.50 (3.20–3.82) | 1.70 (1.42–2.03) | 1.46 (1.22–1.75) | 1.22 (1.05–1.42) | 1.12 (0.96–1.30) * |
| Poor | 8.14 (7.46–8.88) | 5.58 (5.08–6.11) | 10.5 (8.95–12.3) | 2.94 (2.34–3.70) | 1.77 (1.52–2.06) | 1.50 (1.28–1.75) |
| Undifferentiated | 5.95 (5.17–6.85) | 5.11 (4.43–5.89) | 11.4 (8.2–15.8) | 4.64 (3.32–6.50) | 2.13 (1.55–2.92) | 2.23 (1.62–3.07) |
| Unknown | 2.07 (1.90–2.24) | 1.63 (1.50–1.77) | 1.54 (1.38–1.72) | 1.45 (1.29–1.62) | 2.54 (2.17–2.98) | 1.17 (0.99–1.37) * |
| Surgery (Yes) | 0.28 (0.26–0.29) | 0.36 (0.34–0.38) | 0.42 (0.38–0.46) | 0.47 (0.42–0.53) | 0.28 (0.26–0.30) | 0.40 (0.37–0.43) |
| Radiotherapy (Yes) | 2.93 (2.71–3.18) | 1.38 (1.27–1.50) | 4.42 (3.55–5.51) | 1.53 (1.22–1.92) | 1.07 (0.97–1.18) * | 1.10 (0.99–1.22) * |
| Chemotherapy (Yes) | 2.69 (2.57–2.82) | 1.31 (1.24–1.38) | 4.66 (4.20–5.17) | 1.73 (1.53–1.96) | 0.94 (0.88–1.01) * | 0.66 (0.62–0.71) |
p < 0.05 relative to reference unless noted by * p ≥ 0.05. Reference categories: Gender (Male), Race (White), Detection Stage (Localized), Grade differentiation (Well), Surgery (No), Radiotherapy (No), and Chemotherapy (No). CI, confidence interval.
2.12. Ovarian
SRCCs comprise 0.2% of all cases of ovarian cancer, and 0.6% of all SRCC cases (Table 23, Figure 2). Data for papillary serous cystoadenocarcinoma tumors is presented as this is the most common cancer subtype at 24.3% of cases. When compared to nonvariant adenocarcinomas, SRCCs have an earlier mean age of onset of 7 years like gastric cancers, but a later age of 1.7 years compared to the cystoadenocarcinomas. Consistent across all three subtypes, distant stage is the most common presentation. SRCCs have a comparable 5-year survival relative to adenocarcinomas, and much worse compared to cystoadenocarcinomas (10.8% vs. 19.2% vs. 38.2%), respectively (Figure 3l, Table 22). Median survival time is 7.9 months for SRCCs and 12.5 months for adenocarcinomas. When compared to all other ovarian cancers, SRCCs have a HR of 1.56 (95% CI: 1.31–1.86), 1.87 (95% CI: 1.56–2.23) to cystoadenocarcinomas, and 1.30 (1.09–1.56) to adenocarcinomas, after multivariate analyses (Table 24).
Table 23.
Baseline demographics and clinical characteristics by histology for ovarian cancers.
| Ovarian | All | Papillary Serous Cystadeno. | Adenocarcinoma | Signet |
|---|---|---|---|---|
| N | 104,705 (100) | 25,411 (24.3) | 11,844 (11.3) | 186 (0.2) |
| Age (Years) (%) | ||||
| 0–14 | 645 (0.6) | 6 (<0.1) | 2 (<0.1) | 0 (0) |
| 15–29 | 3906 (3.7) | 493 (1.9) | 58 (0.5) | 3 (1.6) |
| 30–49 | 20,498 (19.6) | 4802 (18.9) | 952 (8.1) | 34 (18.3) |
| 50–69 | 45,891 (43.8) | 12,533 (49.3) | 4351 (36.7) | 86 (46.2) |
| 70–85 | 27,087 (25.9) | 6782 (26.7) | 4903 (41.4) | 51 (27.4) |
| >85 | 6678 (6.4) | 795 (3.1) | 1578 (13.3) | 12 (6.5) |
| Mean (SD) | 60.7 (16.6) | 61.0 (14.0) | 69.7 (13.6) | 62.7 (14.7) |
| Race (%) | ||||
| White | 87,315 (83.4) | 22,197 (87.4) | 9846 (83.1) | 153 (82.3) |
| Black | 8499 (8.1) | 1674 (6.6) | 1265 (10.7) | 16 (8.6) |
| Other | 8891 (8.5) | 1540 (6.1) | 733 (6.2) | 17 (9.1) |
| Detection Stage (%) | ||||
| In Situ | 621 (0.6) | 14 (0.1) | 28 (0.2) | 0 (0) |
| Localized | 23,494 (22.4) | 2946 (11.6) | 444 (3.7) | 9 (4.8) |
| Regional | 9969 (9.5) | 1953 (7.7) | 611 (5.2) | 8 (4.3) |
| Distant | 64,289 (61.4) | 20,088 (79.1) | 9866 (83.3) | 161 (86.6) |
| Unstaged | 6332 (5.0) | 410 (1.6) | 895 (7.6) | 8 (4.3) |
| Grade Differentiation (%) | ||||
| Well | 7167 (6.8) | 1152 (4.6) | 162 (1.4) | 0 (0) |
| Moderate | 12,908 (12.3) | 3807 (15.0) | 569 (4.8) | 9 (4.8) |
| Poor | 30,025 (28.7) | 10,154 (40.0) | 3002 (25.3) | 68 (36.6) |
| Undifferentiated | 12,532 (12.0) | 3583 (14.1) | 322 (2.7) | 4 (2.2) |
| Unknown | 42,073 (40.2) | 6715 (26.4) | 7789 (65.8) | 105 (56.5) |
| Surgery (%) | ||||
| Yes | 82,018 (78.3) | 23,452 (92.3) | 4154 (35.1) | 97 (52.2) |
| No | 22,687 (21.7) | 1959 (7.7) | 7690 (64.9) | 89 (47.8) |
| Radiotherapy (%) | ||||
| Yes | 1567 (1.5) | 266 (1.0) | 200 (1.7) | 1 (0.5) |
| No | 103,138 (98.5) | 25,145 (99.0) | 11,644 (98.3) | 185 (99.5) |
| Chemotherapy (%) | ||||
| Yes | 63,158 (60.3) | 18,316 (72.1) | 7101 (60.0) | 114 (61.3) |
| No | 41,547 (39.7) | 7095 (27.9) | 4743 (40.0) | 72 (38.7) |
| Incidence Rate (95% CI) ^ | 12.5 (12.4–12.6) | 2.75 (2.71–2.79) | 1.40 (1.38–1.43) | 2.0 (1.7–2.4) †† |
| CSS % (95% CI) | ||||
| 1-year | 72.8 (72.5–73.2) | 83.0 (82.4–83.5) | 50.7 (49.6–51.7) | 41.7 (33.1–50.0) |
| 2-year | 70.0 (60.6–61.3) | 68.0 (67.3–68.7) | 36.9 (35.9–38.0) | 25.4 (18.1–33.5) |
| 5-year | 40.6 (40.1–40.9) | 38.2 (37.5–39.0) | 19.2 (18.3–20.2) | 10.8 (6.0–17.1) |
| 10-year | 30.4 (30.0–30.8) | 23.3 (22.6–24.1) | 12.9 (12.1–13.8) | 6.6 (2.9–12.4) |
| Median (Months) | 39.2 | 41.9 | 12.5 | 7.9 |
| RS % (95% CI) | ||||
| 1-year | 72.0 (71.7–72.3) | 83.1 (82.4–83.7) | 49.1 (48.1–50.2) | 40.1 (31.7–48.4) |
| 2-year | 60.6 (60.2–60.9) | 68.6 (67.8–69.4) | 35.8 (34.7–36.8) | 24.2 (16.9–32.1) |
| 5-year | 40.6 (40.2–41.0) | 39.3 (38.5–40.1) | 18.5 (17.6–19.4) | 9.9 (5.3–16.1) |
| 10-year | 30.7 (30.2–31.2) | 24.5 (23.6–25.4) | 12.3 (11.4–13.2) | 7.1 (3.1–13.4) |
| Median (Months) | 38.9 | 43.3 | 11.3 | 7.4 |
p < 0.05 for all comparisons among papillary serous cystoadenocarcinoma, adenocarcinoma, and signet ring cell comparisons. Incidence rates (^ indicates calculated among female population) expressed per 100,000 except †† (per 10 million). CSS, cause-specific survival; RS, relative survival; CI, confidence interval.
Table 24.
Derived univariate and multivariable Cox-proportional hazard ratios (HR) of mortality for ovarian cancers.
| Ovarian | Signet Ring vs. non-Signet Ring | Signet Ring vs. Papillary Serous Cystadenocarcinoma | Signet Ring vs. Adenocarcinoma | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | Univariate | Multivariable | Univariate | Multivariable | Univariate | Multivariable |
| Signet Ring Histology | 2.95 (2.47–3.51) | 1.56 (1.31–1.86) | 2.99 (2.51–3.56) | 1.87 (1.56–2.23) | 1.15 (0.96-1.37) * | 1.30 (1.09–1.56) |
| Age (per 10 years) | 1.52 (1.51–1.53) | 1.29 (1.28–1.30) | 1.38 (1.36–1.39) | 1.27 (1.26–1.29) | 1.34 (1.31–1.36) | 1.16 (1.13–1.18) |
| Race | ||||||
| Black | 1.17 (1.13–1.20) | 1.20 (1.16–1.24) | 1.08 (1.01–1.15) | 1.18 (1.11–1.26) | 1.24 (1.16–1.34) | 1.21 (1.13-1.31) |
| Other | 0.72 (0.70–0.75) | 0.94 (0.91–0.98) | 0.83 (0.77–0.89) | 0.94 (0.88–1.01) * | 0.86 (0.78–0.94) | 0.95 (0.86-1.04) * |
| Detection Stage | ||||||
| In Situ | 0.34 (0.22–0.54) | 0.35 (0.22–0.55) | - | - | - | - |
| Regional | 4.70 (4.45–4.97) | 3.70 (3.49–3.91) | 4.32 (3.79–4.91) | 3.31 (2.91–3.77) | 4.43 (3.49–5.62) | 4.00 (3.14–5.10) |
| Distant | 13.2 (12.6–13.7) | 9.01 (8.61–9.43) | 12.0 (10.8–13.3) | 8.90 (7.99–9.92) | 9.62 (7.79–11.9) | 7.56 (6.07–9.40) |
| Unstaged | 13.0 (12.3–13.7) | 5.17 (4.88–5.48) | 8.78 (7.45–10.3) | 5.56 (4.70–6.57) | 9.80 (7.59–11.9) | 5.34 (4.23–6.74) |
| Grade Differentiation | ||||||
| Moderate | 2.86 (2.69–3.05) | 1.76 (1.65–1.88) | 2.54 (2.28–2.82) | 1.99 (1.79–2.22) | 3.16 (2.33–4.30) | 1.47 (1.08–2.01) |
| Poor | 5.17 (4.87–5.49) | 2.08 (1.96–2.21) | 3.20 (2.89–3.53) | 2.14 (1.93–2.37) | 3.30 (2.46–4.42) | 1.35 (1.00–1.81) * |
| Undifferentiated | 4.69 (4.41–5.00) | 1.98 (1.86–2.11) | 2.99 (2.69–3.33) | 2.03 (1.83–2.26) | 3.22 (2.34–4.43) | 1.43 (1.03–1.97) |
| Unknown | 4.43 (4.17–4.70) | 1.81 (1.70–1.92) | 1.93 (1.74–2.14) | 1.75 (1.58–1.94) | 5.97 (4.47–7.99) | 1.46 (1.08–1.97) |
| Surgery (Yes) | 0.21 (0.20-0.22) | 0.36 (0.35-0.37) | 0.30 (0.28-0.31) | 0.38 (0.36-0.41) | 0.33 (0.31-0.35) | 0.47 (0.44-0.49) |
| Radiotherapy (Yes) | 1.34 (1.26-1.43) | 1.19 (1.12-1.27) | 1.11 (0.96-1.29) | 0.99 (0.85-1.15) * | 1.05 (0.90-1.23) * | 1.05 (0.89-1.22) * |
| Chemotherapy (Yes) | 1.64 (1.61-1.67) | 0.91 (0.89-0.93) | 1.98 (1.90-2.06) | 1.08 (1.04-1.13) | 0.67 (0.64-0.71) | 0.59 (0.56-0.62) |
p < 0.05 relative to reference unless noted by * p ≥ 0.05. Reference categories: Race (White), Detection Stage (Localized), Grade differentiation (Well), Surgery (No), Radiotherapy (No), and Chemotherapy (No). CI, confidence interval.
2.13. Prostate
SRCCs comprise 0.02% of all cases of prostate, and 0.4% of all SRCC cases (Table 25, Figure 2). Prostate cancer is predominantly nonvariant adenocarcinomas at 96.0% of all cases. When compared to nonvariant adenocarcinomas, SRCCs have an earlier mean age of onset of 1.7 years, but this is not statistically significant. SRCCs have a higher rate of detection at the distant/metastatic stage (13.2% vs. 4.2%), and most are poor grade differentiation (90.1% vs. 37.3%). There are no statistically significant differences among treatment modalities. SRCCs have worse 5-year survival relative to adenocarcinomas, (83.6% vs. 93.4%), respectively (Figure 3m, Table 25). When compared to all prostate cancers, SRCCs have a HR of 2.41 (95% CI: 1.71–3.39) and 2.63 (95% CI: 1.87–3.70) to adenocarcinomas, after univariate analyses. However, there are no significant differences after multivariable analyses (Table 26).
Table 25.
Baseline demographics and clinical characteristics by histology for prostate cancers.
| Prostate | All | Adenocarcinoma | Signet Ring |
|---|---|---|---|
| N | 999,669 (100) | 959,899 (96.0) | 152 (0.02) |
| Age (Years) (%) | |||
| 0–14 | 44 (<0.1) | 0 (0) * | 0 (0) * |
| 15–29 | 43 (<0.1) | 10 (<0.1) * | 0 (0) * |
| 30–49 | 27,207 (2.7) | 26,290 (2.7) * | 4 (2.6) * |
| 50–69 | 578,769 (57.9) | 563,449 (58.7) * | 83 (54.6) * |
| 70–85 | 356,646 (35.7) | 340,627 (35.5) * | 60 (39.5) * |
| >85 | 36,960 (3.7) | 29,523 (3.1) * | 5 (3.3) * |
| Mean (SD) | 67.1 (9.5) | 66.8 (9.3) * | 68.5 (9.8) * |
| Race (%) | |||
| White | 796,772 (79.7) | 764,998 (79.7) | 107 (70.4) |
| Black | 148,696 (14.9) | 143,025 (14.9) | 31 (0.4) |
| Other | 54,201 (5.4) | 51,876 (5.4) | 14 (9.2) |
| Detection Stage (%) | |||
| In Situ | 155 (<0.1) | 75 (<0.1) | 0 (0) |
| Localized/Regional | 840,596 (84.1) | 822,046 (85.6) | 114 (75.0) |
| Distant | 48,394 (4.8) | 40,274 (4.2) | 20 (13.2) |
| Unstaged | 110,524 (11.1) | 97,504 (10.2) | 18 (11.8) |
| Grade Differentiation (%) | |||
| Well | 67,068 (6.7) | 66,219 (6.9) | 0 (0) |
| Moderate | 503,255 (50.3) | 494,704 (51.5) | 11 (7.2) |
| Poor | 365,431 (36.6) | 358,221 (37.3) | 137 (90.1) |
| Undifferentiated | 2977 (0.3) | 2541 (0.3) | 1 (0.7) |
| Unknown | 60,938 (6.1) | 38,214 (4.0) | 3 (2.0) |
| Surgery (%) | |||
| Yes | 439,779 (44.0) | 426,321 (44.4) * | 71 (46.7) * |
| No | 559,890 (56.0) | 533,578 (55.6) * | 81 (53.3) * |
| Radiotherapy (%) | |||
| Yes | 343,522 (34.4) | 336,965 (35.1) * | 50 (32.9) * |
| No | 656,147 (65.6) | 622,934 (64.9) * | 102 (67.1) * |
| Chemotherapy (%) | |||
| Yes | 8234 (0.8) | 7086 (0.7) * | 3 (2.0) * |
| No | 991,435 (99.2) | 952,813 (99.3) * | 149 (98.0) * |
| Incidence Rate (95% CI) ^ | 141.2 (140.9–141.5) | 134.1 (133.8–134.3) | 2.0 (1.7–2.4) †† |
| CSS % (95% CI) | |||
| 1-year | 97.83 (97.79–97.86) | 98.49 (98.45–98.52) | 96.0 (90.7–98.3) |
| 2-year | 96.07 (96.03–96.12) | 96.92 (96.87–96.96) | 92.4 (84.0–96.5) |
| 5-year | 92.33 (92.26–92.39) | 93.35 (93.28–93.42) | 83.6 (72.5–90.5) |
| 10-year | 87.1 (87.0–87.2) | 88.1 (88.0–88.2) | 69.8 (56.4–79.8) |
| Median (Months) | - | - | - |
| RS (Months) (95% CI) | |||
| 1-year | 99.00 (98.95–99.04) | 99.70 (99.67–99.74) | 94.9 (88.1–97.8) |
| 2-year | 98.37 (98.30–98.43) | 99.35 (99.29–99.40) | 88.5 (76.0–94.7) |
| 5-year | 97.4 (97.3–97.5) | 98.7 (98.6–98.8) | 79.4 (64.1–88.7) |
| 10-year | 95.8 (95.1–96.0) | 97.2 (96.9–97.5) | 65.9 (46.8–79.5) |
| Median (Months) | - | - | - |
p < 0.05 for all comparisons between adenocarcinoma and signet ring cell comparisons, unless noted by * p ≥ 0.05. Incidence rates (^ indicates calculated among male population) expressed per 100,000 except †† (per 10 million). CSS, cause-specific survival; RS, relative survival; CI, confidence interval.
Table 26.
Derived univariate and multivariable Cox-proportional hazard ratios (HR) of mortality for prostate cancers.
| Prostate | Signet Ring vs. non-Signet Ring | Signet Ring vs. Adenocarcinoma | ||
|---|---|---|---|---|
| HR (95% CI) | Univariate | Multivariable | Univariate | Multivariable |
| Signet Ring Histology | 2.41 (1.71–3.39) | 1.17 (0.83–1.65) * | 2.63 (1.87–3.70) | 1.16 (0.83–1.63) * |
| Age (per 10 years) | 2.11 (2.09–2.12) | 1.67 (1.65–1.68) | 2.01 (1.99–2.02) | 1.67 (1.66–1.69) |
| Race | ||||
| Black | 1.27 (1.25–1.29) | 1.28 (1.26–1.31) | 1.30 (1.27–1.32) | 1.31 (1.29–1.33) |
| Other | 0.99 (0.97–1.02) * | 0.77 (0.75–0.79) | 0.98 (0.95–1.01) * | 0.76 (0.74–0.79) |
| Detection Stage | ||||
| In Situ | 1.21 (0.67–2.18) * | 0.56 (0.31–1.01) * | 1.17 (0.52–2.60) * | 0.60 (0.27–1.34) * |
| Distant | 27.4 (27.0–27.8) | 13.6 (13.3–13.8) | 26.7 (26.2–27.1) | 14.1 (13.9–14.4) |
| Unstaged | 3.02 (2.97–3.07) | 2.62 (2.57–2.66) | 2.66 (2.62–2.71) | 2.56 (2.51–2.60) |
| Grade Differentiation | ||||
| Moderate | 1.03 (0.99–1.08) * | 1.37 (1.31–1.42) | 1.04 (0.99–1.08) * | 1.35 (1.30–1.42) |
| Poor | 3.21 (3.09–3.34) | 3.39 (3.26–3.53) | 3.26 (3.14–3.39) | 3.38 (3.25–3.52) |
| Undifferentiated | 8.82 (8.22–9.47) | 5.94 (5.54–6.38) | 7.85 (7.27–8.47) | 5.28 (4.89–5.70) |
| Unknown | 8.87 (8.52–9.24) | 3.87 (3.72–4.04) | 6.50 (6.23–6.79) | 3.37 (3.22–3.52) |
| Surgery (Yes) | 0.486 (0.479–0.492) | 0.72 (0.71–0.73) | 0.524 (0.517–0.531) | 0.73 (0.72–0.74) |
| Radiotherapy (Yes) | 0.79 (0.78–0.80) | 0.84 (0.83–0.86) | 0.84 (0.83–0.85) | 0.85 (0.83–0.86) |
| Chemotherapy (Yes) | 7.21 (6.96–7.45) | 2.30 (2.22–2.38) | 6.99 (6.73–7.26) | 2.24 (2.15–2.33) |
p < 0.05 relative to reference unless noted by * p ≥ 0.05. Reference categories: Race (White), Detection Stage (Localized/Regional), Grade differentiation (Well), Surgery (No), Radiotherapy (No), and Chemotherapy (No). CI, confidence interval.
3. Discussion
To date, there has been no comparative analysis of SRCCs to site-matching nonvariant adenocarcinomas. Most of our knowledge about SRCCs is extrapolated from gastric cancers which comprise most SRCC cases. In this site, SRCCs are recognized as a distinct histological subtype, however, given the rarity of this disease entity in other sites, SRCCs are usually categorized instead as a pattern. This may have implications in patient management, as these patients and their families may benefit from more tailored screening or treatment regimens with the evolution of our understanding of SRCC tumor biology.
This analysis presents a quantification of the similarities among SRCCs across sites and points out some distinct differences. All sites have an earlier age of onset from 3–7 years for SRCCs, except for the breast and prostate cancer. Presentation at distant stages with poor differentiation are most common. Cancers of the large intestine have the worst survivals relative to nonvariant adenocarcinomas, whereas the mortality risk is not as largely increased for typically aggressive cancers sites (esophagus, pancreas, ovary). Even after adjusting for age, race, detection stage, grade, and treatment, the hazard risk for mortality relative to adenocarcinomas is most significant in the colon and rectum at 1.5–2.1. The risk for mortality remains significant after multivariate analysis in all sites except the pancreas, gallbladder, appendix, and prostate. This suggests that the primary tumor location may be an independent risk factor for cause-specific survival [14].
Conjectures regarding the inherit advanced disease pathology in SRCCs at presentation come from observations of the behavior of SRCCs in gastric cancer. The prototypical classification of gastric cancers is the Lauren classification from 1965 which divides them into intestinal and diffuse types [15]. As opposed to intestinal types, diffuse type cancers tend not to form macroscopic or fungating lesions. Diffuse type gastric cancers are defined by poorly-cohesive cells with no gland formation, and are predominately signet ring cell in nature [16]. This has evolved into the current dichotomy of diffuse gastric cancers: SRCCs and other poorly cohesive carcinomas. The two key pathogenic characteristics of SRCCs are their loss of cell-cell adhesion properties leading to their diffuse pattern of spread, and mucin accumulation [8]. It is not known if these two processes are connected.
In 1994, truncations in the protein E-cadherin, encoded by the gene CDH1, were first reported in diffuse gastric cancers [17]. Loss of E-cadherin expression is one on of the initiating steps in the epithelial-to-mesenchymal transition (EMT) process of metastasis, where loss of cell-cell contacts promotes a more plastic cellular cytoskeleton and anchorage-independent growth and survival during lymphatic and hematogenous spread of cells [18]. While this may be a mechanism behind gastric cancer SRCC aggressiveness, CDH1 mutations are believed instead to contribute to earlier in tumor initiation [19]. In 1998, this mutation was confirmed to exist as an autosomal dominant germline gene mutation responsible for the hereditary diffuse gastric cancer (HDGC) syndrome [20,21]. These patients have to an 70% cumulative lifetime risk of gastric cancer with onset typically around age 40, and a 42% lifetime risk of lobular breast cancer [21]. Patients testing positive for CDH1 mutations are recommended to undergo prophylactic gastrectomy by age 30 and high-risk breast cancer screening starting at age 35 [22,23]. The incidence of in situ signet ring cell lesions in prophylactic gastrectomy specimens is over 70% [24]. HDGC though comprises only 1–3% of all gastric cancers, whereas SRCCs comprise 10–18% of gastric cancers [24,25]. More widespread genetic testing is required to explore the genetic drivers of this entity. SRCCs is also the predominant histotype of linitis plastica, defined by thickened and rigid gastric walls caused by fibrous stroma reactions [26]. Linking CDH1 mutations to SRCC sites is difficult given their rarity [16], though a case of appendiceal SRCC occurring with a gastric SRCC is reported [27].
The particularly aggressive nature of SRCCs and its earlier onset in colorectal cancers has been highlighted in the literature [28,29]. These cancers have higher frequency of KRAS and BRAF mutations compared with conventional cancers [30], correlating to shorter overall survival [31]. Colorectal SRCCs more readily metastasize to the peritoneum rather than the lung and liver like conventional adenocarcinomas [32]. SRCC in the rectosigmoid has been associated with a history of ulcerative colitis [33], and methylation of the CDH1 promoter is seen in 93% of dysplastic biopsies compared to 6% of non-dysplastic biopsies in ulcerative colitis patients [34].
Several studies have looked at the effects of SRCC histology on therapeutic interventions. Neoadjuvant chemotherapy provided no survival benefit in patients with locally advanced gastric SRCC [35]. Esophageal SRCC predicts a poor response to preoperative chemoradiation, with no survival benefit from neoadjuvant treatment even if downstaging occurs [36]. This finding was further supported on systematic review [37]. SRCCs though with microsatellite instability-high (MSI-H tumors), are predominately in the right colon, and show good response to immune checkpoint therapy [38]. In prostate SRCCs, among the rarest SRCCs, with about 80 cases reported in the literature [39,40], a multimodal therapeutic approach is typically described, with hormonal treatment potentially adding longer-term benefit [41].
The presence of SRCCs outside of the gastrointestinal tract warrants careful immunohistochemical investigation to rule out metastasis, in addition to appropriate additional workup. This should include endoscopy with systematic random biopsies and narrow band imaging if gastric or colonic lesions are not seen macroscopically [42]. While estrogen receptor (ER) is most often positive in breast SRCCs, it can be negative in up to 20% of cases [43]. CK7 and CK20 expression patterns can often help in distinguishing from a gastric or colonic source [44]. The majority of ovarian SRCCs are metastatic from other primary lesions, typically of the gastrointestinal tract (Krukenberg tumors) [45]. In fact, the presence of SRCC histology carries a 98.4% positive predictive value for metastasis [46]. Consequently, any finding of ovarian SRCC warrants further investigation of an occult primary [47]. Predictors of a primary ovarian SRCC over a metastatic source include tumor unilaterality, younger age at diagnosis, and larger tumor size [46].
This study is not without limitations. This is a retrospective study and is therefore prone to selection bias. Our analysis is limited to binary treatment variables and does not take into consideration the temporal effects of advancements in therapeutic regimens over the course of the time period investigated. Stage and grade classifications have unique subtilities which are characteristic to the survival of individual cancer types, however, this study is focused on very broad definitions out of necessity. The rarity of SRCCs across most tumor sites does not allow for meaningful analysis outside of a population-level registry. Therefore, the primary strength of this work is our systematic analysis of one the largest cohorts of SRCC patients in a well-established population level cancer registry with rigorous quality improvement methodology [13].
4. Materials and Methods
4.1. Patient Selection
The National Cancer Institute’s SEER database was employed and included all amalgamated data from all 18 SEER cancer registries from 1975–2016, covering 28% of the United States population. Data release from the SEER database does not require informed patient consent. Permission to obtain the SEER database was obtained with the ID number 10095-Nov2018 via signed agreements [48].
The WHO formalized the definition of SRCCs as a histological subtype in gastric cancer in 1990 [8,25]. On the basis of jointpoint analysis (Jointpoint Trend Analysis Software, Version 4.8.0.1, Surveillance Research Program, National Cancer Institute, Calverton, MD, USA) completed on age-adjusted yearly incidence rates from 1975–2016, cases prior to 1992 were excluded assuming SRCCs were more likely to be diagnosed as adenocarcinomas prior to increased recognition of SRCCs as a distinct histological subtype in 1990 (Figure S1).
A complete outline of exclusion criteria and its effect on case numbers in presented in Table S1. A summary of the 18 SEER cancer registries and count of cancer cases within each registry is shown in Table S2. A complete definition of all variables and sites analyzed are presented in Tables S3 and S4.
4.2. Statistical Analysis
All data from the 18 SEER cancer registries was imported into Stata 15.1 (StataCorp LLC, College Station, TX, USA) for statistical analysis from SEER 1975–2016 Research Data in ASCII text format. A complete case analysis was completed after variable definition in Table S1. Baseline patient characteristics were compared with the t or χ2 test as appropriate. Univariate and multivariable Cox proportional hazard regression was used to determine the association of mortality with cancer histology type, after adjusting for age, gender, race, detection stage, grade differentiation, surgery, radiotherapy, and chemotherapy. All hazard ratios are calculated with 95% confidence intervals. Use of surgery, radiotherapy, and chemotherapy as treatment modalities are taken as binary variables. All p-values are two-sided, and the threshold of 0.05 was used to determine significance. Survival curves were plotted using the Kaplan-Meier method. Graphs are produced using Origin Pro 2020 (OriginLab Corporation, Northampton, MA, USA). Incidence rates are calculated with SEER*Stat 8.3.6 (Surveillance Research Program, National Cancer Institute, Calverton, MD, USA), using SEER 18 (2000–2016 data) and are age-adjusted to the 2000 United Sates standard population with the age variable recode <1 year olds. Cause-specific survival and relative survival are both age standardized to the International Cancer Survival Standard 1—Age 15+ variable via the actuarial method (and Ederer II cumulative expected method for relative survival), using SEER*Stat 8.3.6 and SEER 18 (2000–2016 data).
5. Conclusions
This study aims to provide a standardized and systematic characterization of the broad demographical and histopathological features of SRCCs across all major sites and compare them to nonvariant histological types. This resource should provide insight into the outcome characteristics of this otherwise rarely quantified cancer subtype for researchers and clinicians. Where applicable, SRCC patients need to be stratified in clinical trials as effective therapeutic interventions are largely lacking for this population. Whereas histology has been instrumental in identification of SRCCs and epidemiology in characterization of their prognosis, their effective surveillance and treatment will depend on future omics breakthroughs that underpin understanding of their unique pathogenesis.
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6694/12/6/1544/s1, Figure S1: Jointpoint analysis for gastric and colon cancers (1975–2016), Table S1: Exclusion criteria and counts of all cases and signet ring cell cases, Table S2. Count of all cases and signet cell cases by SEER cancer registry for all included cases. Table S3: Variables in analysis, Table S4: Breakdown of SRCC cases in SEER (1975–2016), both analyzed and not analyzed.
Author Contributions
M.G.K.B. conceptualized and analyzed the project and prepared the original draft. A.M. supervised this project and reviewed and edited this manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Laufman H., Saphir O. Primary linitis plastica type of carcinoma of the colon. AMA Arch. Surg. 1951;62:79–91. doi: 10.1001/archsurg.1951.01250030082009. [DOI] [PubMed] [Google Scholar]
- 2.Saphir O. Signet-ring cell carcinoma of the urinary bladder. Am. J. Pathol. 1955;31:223–231. [PMC free article] [PubMed] [Google Scholar]
- 3.El Hussein S., Khader S.N. Primary signet ring cell carcinoma of the pancreas: Cytopathology review of a rare entity. Diagn. Cytopathol. 2019;47:1314–1320. doi: 10.1002/dc.24324. [DOI] [PubMed] [Google Scholar]
- 4.Bosman F.T., Carneiro F., Hruban R.H., Theise N.D. WHO Classification of Tumours of the Digestive System. World Health Organization; Geneva, Switzerland: 2010. [Google Scholar]
- 5.WHO . Digestive System Tumours, WHO Classification of Tumours Series. 5th ed. International Agency for Research on Cancer; Lyon, France: 2019. [Google Scholar]
- 6.Adenocarcinoma Low Differentiated (Stomach) [(accessed on 14 April 2020)]; Available online: https://commons.wikimedia.org/wiki/File:Adenocarcinoma_low_differentiated_(stomach)_H%26E_magn_400x.jpg.
- 7.Poorly Cohesive Gastric Carcioma (Signet-Ring Cell Type) [(accessed on 14 April 2020)]; Available online: https://commons.wikimedia.org/wiki/File:Poorly_cohesive_gastric_carcioma_(signet-ring_cell_type).jpg.
- 8.Machlowska J., Puculek M., Sitarz M., Terlecki P., Maciejewski R., Sitarz R. State of the art for gastric signet ring cell carcinoma: From classification, prognosis, and genomic characteristics to specified treatments. Cancer Manag. Res. 2019;11:2151–2161. doi: 10.2147/CMAR.S188622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO . International Classification of Diseases for Oncology (ICD-O)–3rd Edition, 1st revision. World Health Organization; Geneva, Switzerland: 2013. [Google Scholar]
- 10.Huang B., Ni M., Chen C., Feng Y., Cai S. Younger Age Is Associated with Poorer Survival in Patients with Signet-Ring Cell Carcinoma of the Colon without Distant Metastasis. Gastroenterol. Res. Pract. 2016;2016:2913493. doi: 10.1155/2016/2913493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pokala S.K., Zhang C., Chen Z., Gamboa A.M., Cristofaro S.L., Keilin S.A., Cai Q., Willingham F.F. Incidence, Survival, and Predictors of Lymph Node Involvement in Early-Stage Gastric Signet Ring Cell Carcinoma in the US. J. Gastrointestinal Surg. Off. J Soc. Surg. Aliment. Tract. 2018;22:569–577. doi: 10.1007/s11605-017-3500-4. [DOI] [PubMed] [Google Scholar]
- 12.Park H.S., Lloyd S., Decker R.H., Wilson L.D., Yu J.B. Overview of the Surveillance, Epidemiology, and End Results Database: Evolution, Data Variables, and Quality Assurance. Curr. Prob. Cancer. 2012;36:183–190. doi: 10.1016/j.currproblcancer.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 13.Duggan M.A., Anderson W.F., Altekruse S., Penberthy L., Sherman M.E. The Surveillance, Epidemiology, and End Results (SEER) Program and Pathology: Toward Strengthening the Critical Relationship. Am. J. Surg. Pathol. 2016;40:e94–e102. doi: 10.1097/PAS.0000000000000749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu S.G., Chen X.T., Zhang W.W., Sun J.Y., Li F.Y., He Z.Y., Pei X.Q., Lin Q. Survival in signet ring cell carcinoma varies based on primary tumor location: A Surveillance, Epidemiology, and End Results database analysis. Exp. Rev. Gastroenterol. Hepatol. 2018;12:209–214. doi: 10.1080/17474124.2018.1416291. [DOI] [PubMed] [Google Scholar]
- 15.Lauren P. The two histological main types of gastric carcinoma: Diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol. Microbiol. Scand. 1965;64:31–49. doi: 10.1111/apm.1965.64.1.31. [DOI] [PubMed] [Google Scholar]
- 16.Luo W., Fedda F., Lynch P., Tan D. CDH1 Gene and Hereditary Diffuse Gastric Cancer Syndrome: Molecular and Histological Alterations and Implications for Diagnosis And Treatment. Front. Pharmacol. 2018;9:1421. doi: 10.3389/fphar.2018.01421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Becker K.F., Atkinson M.J., Reich U., Becker I., Nekarda H., Siewert J.R., Höfler H. E-cadherin gene mutations provide clues to diffuse type gastric carcinomas. Cancer Res. 1994;54:3845–3852. [PubMed] [Google Scholar]
- 18.Roche J. The Epithelial-to-Mesenchymal Transition in Cancer. Cancers. 2018;10:52. doi: 10.3390/cancers10020052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Humar B., Blair V., Charlton A., More H., Martin I., Guilford P. E-cadherin deficiency initiates gastric signet-ring cell carcinoma in mice and man. Cancer Res. 2009;69:2050–2056. doi: 10.1158/0008-5472.CAN-08-2457. [DOI] [PubMed] [Google Scholar]
- 20.Guilford P., Hopkins J., Harraway J., McLeod M., McLeod N., Harawira P., Taite H., Scoular R., Miller A., Reeve A.E. E-cadherin germline mutations in familial gastric cancer. Nature. 1998;392:402–405. doi: 10.1038/32918. [DOI] [PubMed] [Google Scholar]
- 21.Hansford S., Kaurah P., Li-Chang H., Woo M., Senz J., Pinheiro H., Schrader K.A., Schaeffer D.F., Shumansky K., Zogopoulos G., et al. Hereditary Diffuse Gastric Cancer Syndrome: CDH1 Mutations and Beyond. JAMA Oncol. 2015;1:23–32. doi: 10.1001/jamaoncol.2014.168. [DOI] [PubMed] [Google Scholar]
- 22.Van der Post R.S., Oliveira C., Guilford P., Carneiro F. Hereditary gastric cancer: What’s new? Update 2013–2018. Fam. Cancer. 2019;18:363–367. doi: 10.1007/s10689-019-00127-7. [DOI] [PubMed] [Google Scholar]
- 23.Van der Post R.S., Vogelaar I.P., Carneiro F., Guilford P., Huntsman D., Hoogerbrugge N., Caldas C., Schreiber K.E., Hardwick R.H., Ausems M.G., et al. Hereditary diffuse gastric cancer: Updated clinical guidelines with an emphasis on germline CDH1 mutation carriers. J. Med. Genet. 2015;52:361–374. doi: 10.1136/jmedgenet-2015-103094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaurah P., Talhouk A., MacMillan A., Lewis I., Chelcun-Schreiber K., Yoon S.S., Huntsman D. Hereditary diffuse gastric cancer: Cancer risk and the personal cost of preventive surgery. Fam. Cancer. 2019;18:429–438. doi: 10.1007/s10689-019-00133-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pernot S., Voron T., Perkins G., Lagorce-Pages C., Berger A., Taieb J. Signet-ring cell carcinoma of the stomach: Impact on prognosis and specific therapeutic challenge. World J. Gastroenterol. 2015;21:11428–11438. doi: 10.3748/wjg.v21.i40.11428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Piessen G., Messager M., Leteurtre E., Jean-Pierre T., Mariette C. Signet ring cell histology is an independent predictor of poor prognosis in gastric adenocarcinoma regardless of tumoral clinical presentation. Ann. Surg. 2009;250:878–887. doi: 10.1097/SLA.0b013e3181b21c7b. [DOI] [PubMed] [Google Scholar]
- 27.Hamilton L.E., Jones K., Church N., Medlicott S. Synchronous appendiceal and intramucosal gastric signet ring cell carcinomas in an individual with CDH1-associated hereditary diffuse gastric carcinoma: A case report of a novel association and review of the literature. BMC Gastroenterol. 2013;13:114. doi: 10.1186/1471-230X-13-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yeo H., Betel D., Abelson J.S., Zheng X.E., Yantiss R., Shah M.A. Early-onset Colorectal Cancer is Distinct From Traditional Colorectal Cancer. Clin. Colorectal Cancer. 2017;16:293–299.e296. doi: 10.1016/j.clcc.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 29.Chou C.L., Tseng C.J., Shiue Y.L. The impact of young age on the prognosis for colorectal cancer: A population-based study in Taiwan. JPN J. Clin. Oncol. 2017;47:1010–1018. doi: 10.1093/jjco/hyx110. [DOI] [PubMed] [Google Scholar]
- 30.Tajiri K., Sudou T., Fujita F., Hisaka T., Kinugasa T., Akagi Y. Clinicopathological and corresponding genetic features of colorectal signet ring cell carcinoma. Anticancer Res. 2017;37:3817–3823. doi: 10.21873/anticanres.11760. [DOI] [PubMed] [Google Scholar]
- 31.Remo A., Fassan M., Vanoli A., Bonetti L.R., Barresi V., Tatangelo F., Gafà R., Giordano G., Pancione M., Grillo F., et al. Morphology and Molecular Features of Rare Colorectal Carcinoma Histotypes. Cancers. 2019;11:1036. doi: 10.3390/cancers11071036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pande R., Sunga A., LeVea C., Wilding G.E., Bshara W., Reid M., Fakih M.G. Significance of Signet-Ring Cells in Patients with Colorectal Cancer. Diseases Colon. Rectum. 2008;51:50–55. doi: 10.1007/s10350-007-9073-7. [DOI] [PubMed] [Google Scholar]
- 33.Sugimoto S., Shimoda M., Iwao Y., Mutaguchi M., Nanki K., Mizuno S., Kameyama K., Ogata H., Naganuma M., Kanai T. Intramucosal poorly differentiated and signet-ring cell components in patients with ulcerative colitis-associated high-grade dysplasia. Dig. Endosc. 2019;31:706–711. doi: 10.1111/den.13482. [DOI] [PubMed] [Google Scholar]
- 34.Azarschab P., Porschen R., Gregor M., Blin N., Holzmann K. Epigenetic control of the E-cadherin gene (CDH1) by CpG methylation in colectomy samples of patients with ulcerative colitis. Genes Chromosomes Cancer. 2002;35:121–126. doi: 10.1002/gcc.10101. [DOI] [PubMed] [Google Scholar]
- 35.Li Y., Ma F.H., Xue L.Y., Tian Y.T. Neoadjuvant chemotherapy vs upfront surgery for gastric signet ring cell carcinoma: A retrospective, propensity score-matched study. World J. Gastroenterol. 2020;26:818–827. doi: 10.3748/wjg.v26.i8.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Patel V.R., Hofstetter W.L., Correa A.M., Agarwal A., Rashid A., Bhutani M.S., Lin S.H., Ajani J.A., Swisher S.G., Maru D.M. Signet ring cells in esophageal adenocarcinoma predict poor response to preoperative chemoradiation. Ann. Thorac. Surg. 2014;98:1064–1071. doi: 10.1016/j.athoracsur.2014.04.099. [DOI] [PubMed] [Google Scholar]
- 37.Bleaney C.W., Barrow M., Hayes S., Ang Y. The relevance and implications of signet-ring cell adenocarcinoma of the oesophagus. J. Clin. Pathol. 2018;71:201–206. doi: 10.1136/jclinpath-2017-204863. [DOI] [PubMed] [Google Scholar]
- 38.Alvi M.A., Loughrey M.B., Dunne P., McQuaid S., Turkington R., Fuchs M.A., McGready C., Bingham V., Pang B., Moore W., et al. Molecular profiling of signet ring cell colorectal cancer provides a strong rationale for genomic targeted and immune checkpoint inhibitor therapies. Br. J. Cancer. 2017;117:203–209. doi: 10.1038/bjc.2017.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Humphrey P.A. Histological variants of prostatic carcinoma and their significance. Histopathology. 2012;60:59–74. doi: 10.1111/j.1365-2559.2011.04039.x. [DOI] [PubMed] [Google Scholar]
- 40.Fujita K., Sugao H., Gotoh T., Yokomizo S., Itoh Y. Primary signet ring cell carcinoma of the prostate: Report and review of 42 cases. Int. J. Urol. 2004;11:178–181. doi: 10.1111/j.1442-2042.2003.00763.x. [DOI] [PubMed] [Google Scholar]
- 41.Tiwari D., Nayak B., Seth A. Good response of an aggressive rare variant of signet ring cell carcinoma of prostate with hormonal therapy. BMJ Case Rep. 2017;2017:bcr2016217567. doi: 10.1136/bcr-2016-217567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Phalanusitthepha C., Grimes K.L., Ikeda H., Sato H., Sato C., Hokierti C., Inoue H. Endoscopic features of early-stage signet-ring-cell carcinoma of the stomach. World J. Gastrointest. Endosc. 2015;7:741–746. doi: 10.4253/wjge.v7.i7.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tot T. The role of cytokeratins 20 and 7 and estrogen receptor analysis in separation of metastatic lobular carcinoma of the breast and metastatic signet ring cell carcinoma of the gastrointestinal tract. Apmis. 2000;108:467–472. doi: 10.1034/j.1600-0463.2000.d01-84.x. [DOI] [PubMed] [Google Scholar]
- 44.Li X., Feng Y.-F., Wei W.-D., Liu P., Xie Z.-M., Wang J., Xie X.-M. Signet-ring cell carcinoma of the breast: A case report. World J. Surg. Oncol. 2013;11:183. doi: 10.1186/1477-7819-11-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kim J.H., Cha H.J., Kim K.R., Kim K. Primary ovarian signet ring cell carcinoma: A rare case report. Mol. Clin. Oncol. 2018;9:211–214. doi: 10.3892/mco.2018.1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Simons M., Bolhuis T., De Haan A.F., Bruggink A.H., Bulten J., Massuger L.F., Nagtegaal I.D. A novel algorithm for better distinction of primary mucinous ovarian carcinomas and mucinous carcinomas metastatic to the ovary. Virchows Arch. 2019;474:289–296. doi: 10.1007/s00428-018-2504-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jaya Ganesh P., Vimal Chander R., Kanchana M.P. Primary ovarian mucinous carcinoma with signet ring cells—Report of a rare case. J. Clin. Diagn. Res. 2014;8:FD12–FD13. doi: 10.7860/JCDR/2014/8402.4473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Surveillance, Epidemiology, and End Results (SEER) Program Research Data (1975–2016), National Cancer Institute, DCCPS, Surveillance Research Program, Released April 2019, Based on the November 2018 Submission. [(accessed on 1 December 2019)]; Available online: www.seer.cancer.gov.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.