Abstract
Background
Several studies have demonstrated an association between chronic pain and impairment of cognitive capabilities. Since the number sense is one of the cognitive ability involved in the evaluation of pain intensity using some pain measurement tools, impairment of number sense may impact pain assessment. Therefore, the validity of number-based pain assessment tools should be re-evaluated.
Objectives
This study aimed to determine whether number sense is altered in chronic and acute pain patients compared to healthy subjects.
Methods
Overall, 150 participants were recruited and divided into the three groups of controls, chronic and acute pain patients. Pain intensity was evaluated using numeric and verbal rating scales as pain assessment tools. Number sense was assessed using number naming, number marking, and line bisection tasks. Deviation from correct answers was measured for each task.
Results
Patients with chronic pain (migraine headache) had higher pain intensity scores than acute pain subjects. Chronic pain patients showed significant deviation from the expected responses compared to controls in the line bisection task.
Conclusions
Chronic pain patients may have impaired number sense and may differently use number-based pain assessment tools in comparison with healthy individuals.
Keywords: Pain, Headache, Migraine, Visual Analog Scale
1. Background
The prevalence of chronic pain has been estimated to be about 38% of the world population (1), and chronic pain can be costly to the patient and society (2-6). It is important to measure pain intensity through valid and reliable instruments, which are verbal rating (VRS), numerical rating (NRS), and visual analog scales (VAS), which are all dependent on spatial cognition (7). Some researchers have demonstrated that cognitive skills such as memory and attention are impaired in chronic pain patients (8, 9).
Number sense (NS) is an intuitive skill that helps us measure numerical and scalar magnitudes and probably is relied on the mental and spatial representation of numbers in the brain. Number sense is a cognitive ability essential for spatial-numerical processing, such as the assessment of numerical value and measurements of scale sizes (10). Therefore, the integrity and soundness of the NS are important when using VAS or NRS (11, 12).
Some reports demonstrate NS may be impaired in chronic pain patients (10, 12). As NRS and VAS are highly dependent on the integrity of NS, the appropriateness of the use of VAS and NRS in chronic pain is questioned. However, there are some concerns about these reports as their subjects had different types of chronic and acute pain conditions. Chronic pain disorders have different biological natures; for example, we cannot compare the NS in a patient with diabetic polyneuropathy with a patient who has thalamic pain. Moreover, findings are not consistent across different studies.
2. Objectives
We investigated the impact of chronic and acute pain on the NS in a more uniform population of patients allocated to the three groups of chronic pain (MH) and acute pain (post-op orthopedic) cases and controls.
3. Methods
Experiments were carried out following the last revision of the Statement of Helsinki, 1964. All the subjects consented to participate in this study, and the Ethics Committee of the university approved the study protocol (no.: IR.TUMS.VCR.REC.1395.1523). We evaluated pain intensity by NRS and VRS. NRS was an 11-point scale with 0 and 10 indicating no pain and worst pain imaginable, respectively. VRS had four pain descriptors, including none, mild, moderate, and severe. We registered basal pain intensity (pain at rest) for all the participants.
3.1. Participants
We considered three groups, including chronic pain (MH) patients, acute pain (orthopedic) cases, and controls. Patients’ characteristics, including age, male/female ratio, education, and handedness (right or left) were registered for every participant. Since the mental number line is affected by reading and writing directions, all subjects were recruited from Persian-speaking people who were fluent in Farsi.
The inclusion criteria were: (A) chronic pain patients with MH according to ICHD-II diagnostic criteria for at least 12 months, who were referred to our pain clinic by the neurology service of the hospital; (B) acute pain patients who had orthopedic surgery within the last 24 hours; (C) clear mental status, Ramsay sedation scale, level 2; (D) patients with ASA classification I-III; (E) fluency in Farsi; and (F) patients aged 18 - 70 years old. The healthy control group were hospital staff. The exclusion criteria were: (A) history of any type of persistent pain for the acute pain or control groups; (B) history of any type of chronic pain for MH group other than MH; (C) illiterate subjects or anybody who could not perform the study; and (D) unwilling to participate in the study.
3.2. Experiments
Two experiments were designed to assess number line tasks, including number marking, number naming, and line bisection tasks. Experiment 1 was for number marking and number naming tasks. It was designed to evaluate subjects’ abilities to transform abstract numbers into spatial representations on a direct line. This ability is similar to what subjects do when they use VAS. Experiment 2 (Line-bisection task) was designed to measure the participants’ ability to accurately recognize spatial-numerical processes. In these tasks, the participants were evaluated individually.
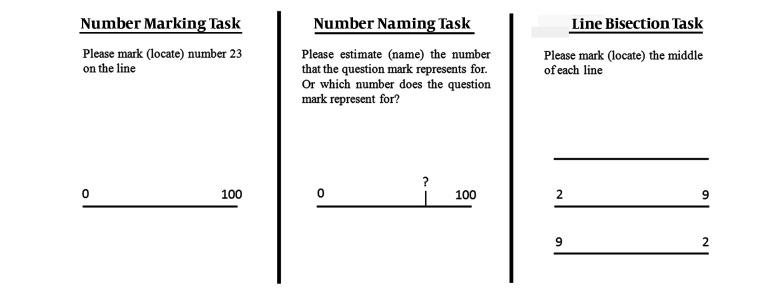
For the number marking task, a 23-cm long horizontal line with two numerical anchors including 0 and 100 at each end of the line was displayed at the center of an A4 paper (Figure 1). The line was anchored with “0” on the left and “100” on the right side. The participants were presented with eight papers, each having a separate line and a randomly chosen number from the following ones (6, 17, 29, 43, 52, 61, 84, and 96). On each paper, they were asked to locate (mark) one of the eight numbers on each line, which they estimated would be the best position for that number. The distance between 0 and their answers was measured. To measure the final number values, the measured distances were divided by 0.23 and to evaluate the “deviation from correct response”, the final number values were subtracted from the correct numbers.
Figure 1. Number marking, number naming, and line bisection tasks.
Since the parietal cortex is involved in motor function (13), the number naming task was designed to eliminate the possible effect of the dysfunction of the parietal cortex on patients’ responses. Subjects were exposed to eight separate papers in random order. On each paper, there was a 23 cm long horizontal line, with numerical anchors at each end of the line, “0” and “100” on the left and right sides, respectively (Figure 1). Each line had a vertical line representing a number between 0 to 100. The subjects were asked to estimate the number each mark indicated. Deviation from the correct number was calculated by subtracting the correct values from the subjects’ responses.
The prefrontal and parietal cortex are complex regions that are critical for spatial-numerical comprehension (14). Since spatial neglect may occur in pain patients because of the prefrontal and parietal cortex dysfunction, the line-bisection task was conducted. For this task, subjects were shown three separate lines with a length of 8 cm on an A4 paper (Figure 1). The first line had no numbers on any end; the second had “2” on the left and “9” on the right end. The third line had “9” on the left and “2” on the right end. We asked the participants to locate the midpoint of the lines based on their estimation. To measure the “deviation from the correct answer”, the distance between the left end and the marked point was measured. The correct midpoint value (4 cm) was subtracted from the response value. The results of experiments 1 and 2 were determined as the “mean absolute deviation from the expected (correct) response” (MADER). We checked the results of the line bisection task simultaneously by the direction of the presented line and subject groups.
3.3. Statistics
Data were analyzed using SPSS version 25 (IBM, New York, NY, USA). To compare continuous variables, we used analysis of variance (ANOVA) test. Post-hoc test was performed by LSD. We used Generalized Linear Models, to adjust the effect of covariates (e.g., education level and gender). Chi-Square or Fisher’s exact tests were performed to evaluate the relationship among categorical variables and between groups when appropriate. Continuous variables were presented as mean ± S.D. The significance level was set at P ≤ 0.05. Based on data from previous studies, when considering α = 0.016 and power = 0.9, then the sample size was calculated to be about 50 subjects in each group.
4. Results
One hundred and fifty subjects were enrolled in the study and equally distributed in three groups. Patients’ characteristics and basal pain intensity are demonstrated in Table 1. There was no significant difference between the three groups in the variables of age and handedness. However, education level, male/female ratio, and pain intensity were significantly different between the groups.
Table 1. Patients’ Characteristics and Basal Pain Intensity in the Three Groups of Studya.
| Orthopedic (N = 50) | Migraine (N = 50) | Healthy Controls (N = 50) | P Value | |
|---|---|---|---|---|
| Gender | 0.020 | |||
| Male | 23 | 10 | 19 | |
| Female | 27 | 40 | 31 | |
| Age, year (mean ± SD) | 30.9 ± 13.6 | 36.2 ± 11.1 | 31.8 ± 11.8 | 0.113 |
| Education | 0.001 | |||
| Under-diploma | 19 | 11 | 5 | |
| Diploma | 23 | 19 | 13 | |
| Bachelor | 3 | 13 | 22 | |
| Higher education | 5 | 7 | 10 | |
| Handedness | 0.345 | |||
| Right | 47 | 49 | 48 | |
| Left | 3 | 1 | 2 | |
| Pain intensity, NRS (median (interquartile range)) | 3 (0 - 6) | 8 (5.75 - 10) | - | < 0.001 |
Abbreviation: NRS, Numeric Rating scale.
aP < 0.05, significant difference.
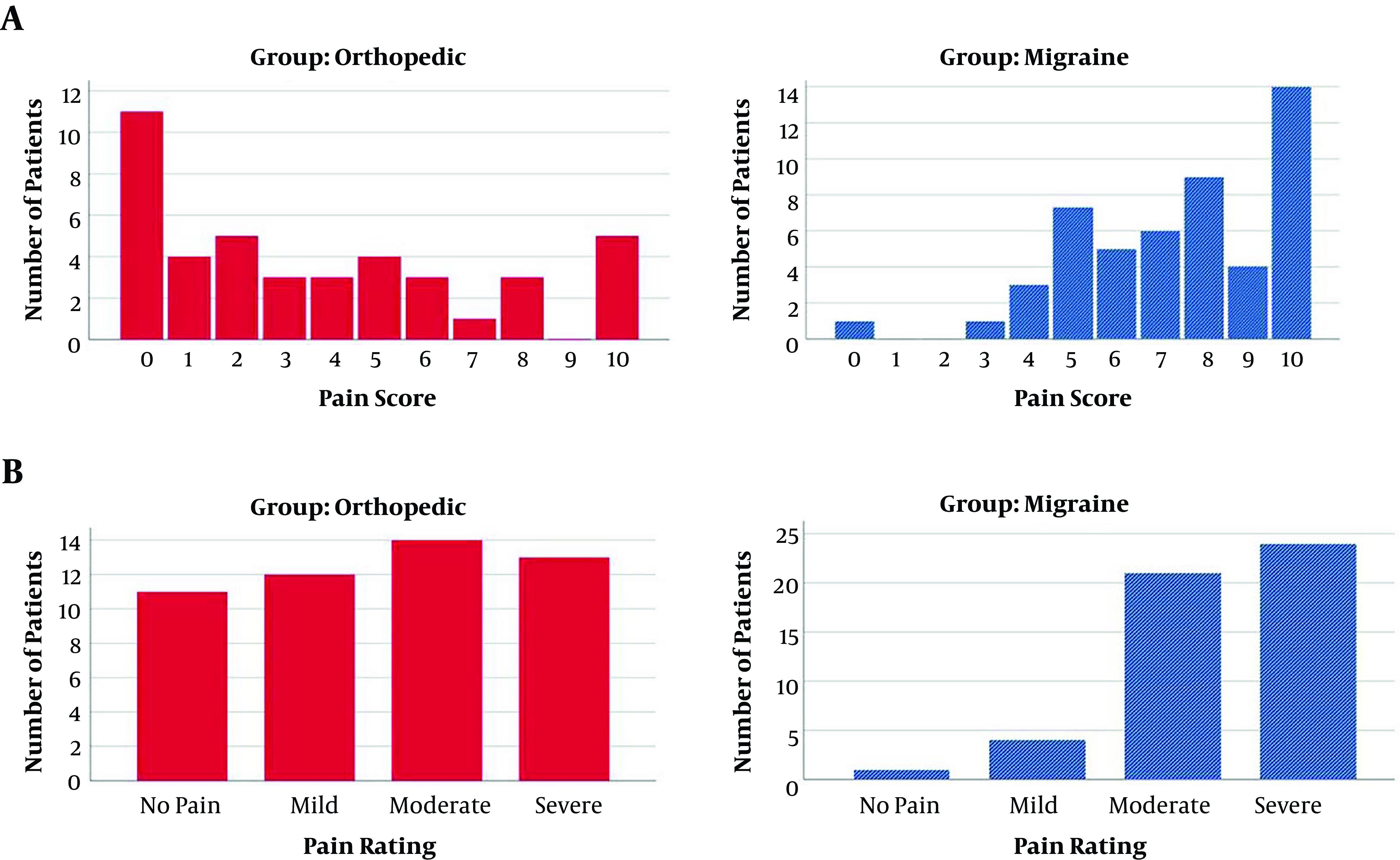
The pain intensity assessed by NRS showed that 18% in the orthopedic group (n = 9) and 66% of patients in the migraine group (n = 31) selected a number equal to or greater than 7 (Figure 2A). The pain intensity evaluated by VRS revealed that 54% of orthopedic patients (n = 27) and 90% of migraine patients (n = 45) described their pain as moderate or severe (Figure 2B). The migraine group reported higher pain intensity scores (P = 0.001).
Figure 2. Distribution of the patients with different pain intensity scores assessed by A, numeric rating and B, verbal rating scales in orthopedic and migraine groups.
The MADERs for each of the tasks in the three groups are demonstrated in Table 2. Statistical analysis showed significant differences in the line bisection task between the migraine and control groups (P = 0.001). The MADER of migraine group for line bisection task was significantly higher than that in the control and orthopedic groups. The MADERs for the number marking and naming tasks were not significantly different between the groups.
Table 2. MADER for Number Marking, Number Naming, and Line Bisection Tasks in Each of the Three Study Groupsa, b.
| Groups | Tasks | |||||
|---|---|---|---|---|---|---|
| Number Marking | P Value | Number Naming | P Value | Line Bisection | P Value | |
| Control | -2.68 ± 11.38 | 0.14 ± 2.22 | 0.410d | 0.15 ± 0.60 | ||
| Migraine | -0.39 ± 6.64 | 0.187c | 0.45 ± 2.55 | 0.410d | 0.51 ± 0.44 | 0.001c |
| Orthopedic | -4.87 ± 6.94 | 0.206c | 0.81 ± 2.59 | 0.410d | 0.30 ± 0.46 | 0.148c |
aMADER, mean absolute deviation from the expected (correct) response.
bValues are expressed as mean ± SD.
cP value, comparison with control group (Post Hoc test, LSD).
dP value, comparison between groups (ANOVA). P < 0.05, significant difference.
Adjusting the effects of male/female ratio, education level, and pain intensity by using Generalized Linear Models and ANCOVA analysis showed that the results obtained from MADER of number marking, number naming, and line bisection tasks were not related to the effect of these covariates (P > 0.05). The distribution of other factors like age and handedness was not significantly different between the groups.
We also examined the results of the line bisection task simultaneously by the direction of the presented line and subject groups (Table 3). When we considered the different locations of “2” and “9” on the two ends of the presented lines, the Bonferroni analysis showed that there was no significant difference in MADER between the migraine and control groups and between the orthopedic and control groups.
Table 3. The Number of Subjects Selected the Correct, Left Side and Right Side of the Middle in Each Group for the Three Lines in Line Bisection Taska, b.
| Group | Statistical Index | Line | ||
|---|---|---|---|---|
| _______ | 2_______9 | 9_______2 | ||
| Control | Correct point | 14 (28) | 8 (16) | 12 (24) |
| Left-sided deviation | 14 (28) | 20 (40) | 17 (34) | |
| Right-sided deviation | 22 (44) | 22 (44) | 21 (42) | |
| Migraine | Correct point | 17 (34) | 6 (12) | 8 (16.3) |
| Left-sided deviation | 2 (4) | 7 (14) | 4 (8.2) | |
| Right-sided deviation | 31 (62) | 37 (74) | 37 (74.5) | |
| Orthopedic | Correct point | 17 (34) | 13 (26) | 13 (26) |
| Left-sided deviation | 10 (20) | 10 (20) | 14 (28) | |
| Right-sided deviation | 23 (46) | 27(54) | 23 (46) | |
aValues are expressed as No. (%).
bP value > 0.05.
5. Discussion
We evaluated the NS by line bisection, number marking, and number naming tasks in MH, acute pain, and control groups. MH patients had higher pain intensity scores than acute pain patients. The line bisection task was significantly impaired in the MH group. However, number naming or number marking was not significantly altered in MH patients.
Patients with MH had higher pain intensity scores than acute pain patients in our study. This finding was in line with the results of previous studies (10, 12). It may have two reasons. First, chronic pain patients usually consult pain clinics when their pain problem interferes with their lives, or their pain intensity should be at least severe enough to urge them to seek treatment. Second, the available analgesics for acute pain might be more effective than chronic pain management modalities because multimodal and preventive analgesia are well indicated and administered in acute post-op pain settings (15). Consequently, acute pain management could be more effective. Nevertheless, we demonstrated that the difference in pain intensity could not affect the results of our study in NS and number line tasks.
Chronic pain patients use number-based assessment tools differently from acute pain patients and healthy individuals (10, 12). Wolrich et al. (12) showed that number marking and number naming were impaired in chronic pain patients. Spindler et al. (10) reported number naming was altered in chronic pain patients. Our data were in agreement with previous studies and showed that the line bisection task was impaired in MH patients. Ultimately, the common point between these reports is that NS may be at least partially impaired in chronic pain patients.
NRS and VAS are dependent on spatial cognition and require correct spatial comprehension and intact NS (16). There are some functional and structural changes in some brain regions of chronic pain patients that are involved in cognitive and motor functions (6, 17). The health of NS, which is related to intact spatial cognition, is necessary for the correct result of these pain assessment tools. Moreover, MRI studies have demonstrated widespread functional and structural alternations in several brain regions, such as the thalamus, cingulate cortex, insula, prefrontal and parietal cortices in almost all chronic pain patients (14, 17, 18). Since these areas are involved in cognitive functions, including spatial perception, distance comprehension, and measurement (19, 20), it has been inferred that NS is impaired in chronic pain patients. Consequently, chronic pain patients cannot accomplish number line tasks similar to healthy individuals. These results may question the appropriateness of the VAS or NRS to evaluate pain intensity for chronic pain patients (10, 12). More studies are needed to evaluate the accuracy of the number-based pain assessment tools in chronic pain patients. Until then, verbal-based assessment tools like VRS should be more widely used.
In line bisection task, the right-sided deviation was more in migraine patients than in both the orthopedic and control groups for all the three lines, while the results are nearly the same for the orthopedic and control groups. The interesting point is that participants with right-sided deviations make the largest subgroups, a result similar to what was observed in previous studies (12).
The line bisection task is used to assess the effects of prefrontal and parietal cortex dysfunction on spatial neglect-like symptoms (10, 12). In our patients, the dysfunction in migraine patients was more than in control and orthopedic groups. Some reports, however, have stated cognitive decline and even decreased volume of gray matter in the parietal and frontal lobes of migraine patients (21), which can explain our results. Foti et al. (22) indicated a discrepancy among multiple studies about the presence of cognitive impairment in migraineurs.
Number line tasks showed inconsistent results across different studies (10, 12). The enrolled patients in these reports had different pain disorders that might have diverse biological natures. Therefore, they might have a different status of NS integrity or cognitive health. NS could be impaired to different degrees in these different types of chronic pain patients. The advantage of our study was that our patients were recruited from one type of chronic pain disorder (MH). Our acute pain patients were also homogenous and were recruited from one entity of acute pain. Moreover, it has been demonstrated that impaired NS only existed in one-third of chronic pain patients (12). Spindler et al. (10) showed that despite the structural and functional changes in the brain of chronic pain patients, their cognitive function was not always affected. The intact cognitive function could be compensated, and they might be able to improve their accuracy in the number line tasks (10). Besides, there is a report about a higher rate of obsessive/compulsive trait in MH patients (23) compared to the general population, which brings to mind the possibility of higher accuracy of these patients in numerical abilities. It may explain why the number line tasks are not consistent in all studies. MH patients may be able to compensate and improve their NS-related function.
Our results could add to the present literature about the validity of pain assessment tools in addition to the data about the numerical-spatial abilities of patients suffering from acute and chronic pain.
5.1. Conclusions
This study revealed that MH patients may have impaired NS, at least in some aspects, and may use number-based pain assessment tools differently in comparison with patients or healthy individuals.
Footnotes
Authors' Contribution: Hossein Majedi directed and designed the study, devised the main conceptual ideas, data analysis, interpretation, and writing the manuscript. Mahsa Mohammadi did data collection. Abbas Tafakhori designed the study and reviewed the manuscript. Zahra Khazaeipour did data analysis. All authors read and confirmed the final manuscript.
Conflict of Interests: There was no conflict of interest in this study.
Ethical Approval: This study was approved by the Ethics Committee of Tehran University of Medical Sciences (code: IR.TUMS.VCR.REC.1395.1523).
Funding/Support: There was no funding or support for this study.
Informed Consent: All patients in this study provided informed consent. All experiments were performed in compliance with the relevant laws and institutional guidelines.
Contributor Information
Hossein Majedi, Email: hossein_majedi@yahoo.com, hmajedi@tums.ac.ir.
Mahsa Mohammadi, Email: mohammadig1380@gmail.com.
Abbas Tafakhori, Email: abbas.tafakhori@gmail.com.
Zahra Khazaeipour, Email: khazaeipour@tums.ac.ir.
References
- 1.Tsang A, Von Korff M, Lee S, Alonso J, Karam E, Angermeyer MC, et al. Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain. 2008;9(10):883–91. doi: 10.1016/j.jpain.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 2.Majedi H, Safdarian M, Hajiaghababaei M, Vaccaro AR, Rahimi-Movaghar V. Characteristics of neuropathic pain in individuals with chronic spinal cord injury. Neurosciences (Riyadh). 2018;23(4):292–300. doi: 10.17712/nsj.2018.4.20180223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Majedi H, Amini MH, Yousefshahi F, Khazaeipour Z, Majedi M, Rahimi M, et al. Predicting Factors of Pain Duration in Patients with Chronic Pain: A Large Population-based Study. Anesth Pain Med. 2020;10(1):e95776. doi: 10.5812/aapm.95776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Majedi H, Dehghani SS, Soleyman-Jahi S, Tafakhori A, Emami SA, Mireskandari M, et al. Assessment of Factors Predicting Inadequate Pain Management in Chronic Pain Patients. Anesth Pain Med. 2019;9(6):e97229. doi: 10.5812/aapm.97229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walk D, Poliak-Tunis M. Chronic Pain Management: An Overview of Taxonomy, Conditions Commonly Encountered, and Assessment. Med Clin North Am. 2016;100(1):1–16. doi: 10.1016/j.mcna.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 6.Imani F, Patel VB. Therapeutic Challenges for Knee Osteoarthritis. Anesth Pain Med. 2019;9(3):e95377. doi: 10.5812/aapm.95377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, et al. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41(6):1073–93. doi: 10.1016/j.jpainsymman.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 8.Moriarty O, Ruane N, O'Gorman D, Maharaj CH, Mitchell C, Sarma KM, et al. Cognitive Impairment in Patients with Chronic Neuropathic or Radicular Pain: An Interaction of Pain and Age. Front Behav Neurosci. 2017;11:100. doi: 10.3389/fnbeh.2017.00100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tamburin S, Maier A, Schiff S, Lauriola MF, Di Rosa E, Zanette G, et al. Cognition and emotional decision-making in chronic low back pain: an ERPs study during Iowa gambling task. Front Psychol. 2014;5:1350. doi: 10.3389/fpsyg.2014.01350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spindler M, Koch K, Borisov E, Ozyurt J, Soros P, Thiel C, et al. The Influence of Chronic Pain and Cognitive Function on Spatial-Numerical Processing. Front Behav Neurosci. 2018;12:165. doi: 10.3389/fnbeh.2018.00165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lichtner V, Dowding D, Closs SJ. The relative meaning of absolute numbers: the case of pain intensity scores as decision support systems for pain management of patients with dementia. BMC Med Inform Decis Mak. 2015;15:111. doi: 10.1186/s12911-015-0233-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wolrich J, Poots AJ, Kuehler BM, Rice AS, Rahman A, Bantel C. Is number sense impaired in chronic pain patients? Br J Anaesth. 2014;113(6):1024–31. doi: 10.1093/bja/aeu255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rathelot JA, Dum RP, Strick PL. Posterior parietal cortex contains a command apparatus for hand movements. Proc Natl Acad Sci U S A. 2017;114(16):4255–60. doi: 10.1073/pnas.1608132114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ruscheweyh R, Deppe M, Lohmann H, Stehling C, Floel A, Ringelstein EB, et al. Pain is associated with regional grey matter reduction in the general population. Pain. 2011;152(4):904–11. doi: 10.1016/j.pain.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 15.Imani F, Varrassi G. Ketamine as Adjuvant for Acute Pain Management. Anesth Pain Med. 2019;9(6):e100178. doi: 10.5812/aapm.100178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Herr KA, Spratt K, Mobily PR, Richardson G. Pain intensity assessment in older adults: use of experimental pain to compare psychometric properties and usability of selected pain scales with younger adults. Clin J Pain. 2004;20(4):207–19. doi: 10.1097/00002508-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Geha PY, Baliki MN, Harden RN, Bauer WR, Parrish TB, Apkarian AV. The brain in chronic CRPS pain: abnormal gray-white matter interactions in emotional and autonomic regions. Neuron. 2008;60(4):570–81. doi: 10.1016/j.neuron.2008.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Malik KM, Beckerly R, Imani F. Musculoskeletal Disorders a Universal Source of Pain and Disability Misunderstood and Mismanaged: A Critical Analysis Based on the U.S. Model of Care. Anesth Pain Med. 2018;8(6):e85532. doi: 10.5812/aapm.85532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jacob SN, Nieder A. Tuning to non-symbolic proportions in the human frontoparietal cortex. Eur J Neurosci. 2009;30(7):1432–42. doi: 10.1111/j.1460-9568.2009.06932.x. [DOI] [PubMed] [Google Scholar]
- 20.Khan TW, Imani F. The management of chronic pain; caught between a rock and a hard place: The Case for a renewed focus on provider, patient, and payer education. Anesthesiology and pain medicine. 2017;7(1) doi: 10.5812/aapm.40951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schmitz N, Arkink EB, Mulder M, Rubia K, Admiraal-Behloul F, Schoonman GG, et al. Frontal lobe structure and executive function in migraine patients. Neurosci Lett. 2008;440(2):92–6. doi: 10.1016/j.neulet.2008.05.033. [DOI] [PubMed] [Google Scholar]
- 22.Foti M, Lo Buono V, Corallo F, Palmeri R, Bramanti P, Marino S. Neuropsychological assessment in migraine patients: a descriptive review on cognitive implications. Neurol Sci. 2017;38(4):553–62. doi: 10.1007/s10072-017-2814-z. [DOI] [PubMed] [Google Scholar]
- 23.Cupini LM, De Murtas M, Costa C, Mancini M, Eusebi P, Sarchielli P, et al. Obsessive-Compulsive Disorder and Migraine With Medication-Overuse Headache. Headache: The Journal of Head and Face Pain. 2009;49(7):1005–13. doi: 10.1111/j.1526-4610.2009.01457.x. [DOI] [PubMed] [Google Scholar]