Abstract
Bone problems in the population begin to be establish in childhood. The present study aims to assess the usual calcium, phosphorus, magnesium, and vitamin D intakes, along with the food sources of these nutrients, in Spanish children participating in the EsNuPI (Estudio Nutricional en Población Infantil Española) study. Two 24 h dietary recalls were applied to 1448 children (1 to <10 years) divided into two sub-samples: one reference sample (RS) of the general population [n = 707] and another sample which exclusively included children consuming enriched or fortified milks, here called “adapted milks” (AMS) [n = 741]. Estimation of the usual intake shows that nutrient intake increased with age for all nutrients except vitamin D. Using as reference the Dietary Reference Values from the European Food Safety Authority (EFSA), calcium and magnesium intakes were found to be below the average requirement (AR) and adequate intake (AI), respectively, in a considerable percentage of children. Furthermore, phosphorus exceeded the AI in 100% of individuals and vitamin D was lower than the AI in almost all children studied. The results were very similar when considering only plausible reporters. When analyzing the food sources of the nutrients studied, milk and dairy products contributed the most to calcium, phosphorus, magnesium, and vitamin D. Other sources of calcium were cereals and vegetables; for phosphorus: meat, meat products, and cereals; for magnesium: cereals and fruits; and, for vitamin D: fish and eggs. These results highlight the desirability of improving the intake concerning these nutrients, which are involved in bone and metabolic health in children. The AMS group appeared to contribute better to the adequacy of those nutrients than the RS group, but both still need further improvement. Of special interest are the results of vitamin D intakes, which were significantly higher in the AMS group (although still below the AI), independent of age.
Keywords: EsNuPI study, calcium, phosphorus, magnesium, vitamin D, pediatric nutrition, food sources, Spanish children, dairy products, infant formula
1. Introduction
Osteoporosis is a major global public health concern, the prevalence of which increases with the life expectancy of the population [1]. Although it develops in advanced stages of life, it originates in the pediatric age during childhood and adolescence. Therefore maximizing bone mineral mass during these vital stages can decrease the risk of osteoporotic fractures in later life [2,3,4].
Throughout childhood, genetic factors determine ~70–80% of growth and acquisition of bone mineral content, while lifestyle determines ~20–30% [5]; among these exogenous factors, which can be modified, food deserves attention [6,7].
Calcium, phosphorus, magnesium, and vitamin D, which are the nutrients object of attention in this study, play important roles in the growth and development of the bone mass, which is at its maximum in the pediatric stage [2,8,9] regardless of having many human biological roles in body homeostasis, physiological, and cellular functions [10,11]. During childhood and adolescence an adequate intake of these nutrients can contribute to achieving an optimal peak of bone mass, which may help to prevent the development of osteoporosis in later stages of life [6].
However, the intake of many of the nutrients involved in bone remodeling (i.e., calcium, magnesium, and vitamin D) has been shown to be insufficient in a high percentage of children in developed populations [2,12,13,14,15]. Indeed, the United States Department of Agriculture (USDA) [1] has pointed calcium and vitamin D as insufficient in the diet and of public health concern; therefore, knowing their intake in children has become a priority.
Studies in children under the age of 10 in Spain are scarce and heterogeneous in methodology [12,13,16,17,18]. The “Alimentando la Salud del Mañana” (ALSALMA) study (carried out in 2013) assessed only the nutritional patterns of children under three years of age [16]. The National Dietary Survey on the Child and Adolescent Population project in Spain (ENALIA) study analyzed nutrient intake in children from 6 months to 17 years old, but was carried out from 2012 to mid-2014 [13]. The Anthropometry, Intake and Energy Balance Study (ANIBES) analyzed energy and nutrient intake, but was carried out only in children from 9 to 12 years old [12]. The Identification and prevention of Dietary- and lifestyle-induced health EFfectsIn Children and infantS (IDEFICS) study analyzed the intake of European children from 2 to 9 years old; however, this research did not include a representative sample of the Spanish population [18]. Furthermore, it is necessary to carry out studies constantly, in order to know the evolution of these issues and the most current situation of each population.
As dietary habits and dietary patterns begin to establish in early childhood and persist during adulthood [19], knowledge of overall nutrient intake—specifically, those involved in bone growth remodeling—give us an opportunity for intervention aimed at reducing the risk of suffering from various diseases and, in particular, osteoporosis and fragility [20,21].
On the other hand, considering that children have a high need for nutrients, their consumption of nutrient-rich foods is essential [22]. Specifically, regular consumption of dairy products and milk formulas can be useful in children’s health, as they are foods of high nutritional value which provide high amounts of macro- and micro-nutrients, (mainly calcium, magnesium, phosphorus, vitamin D and high quality protein) that are important for bone health [23,24]. In fact, some authors have found higher quality diets in children with higher dairy consumption, compared to those with lower consumption [14,18,25]. Nevertheless, it is interesting to analyze whether the consumption of adapted, enriched, or fortified milk formulas (generally called “adapted milks” in the present study) has potential benefits or disadvantages in the diets of children.
Therefore, the EsNuPI (“Nutritional Study in Spanish Pediatric Population”) study (performed in Spanish children aged one to <10 years old), aims to analyze the usual intake and dietary sources of calcium, phosphorus, magnesium, and vitamin D in children as well as analyzing the differences between those who usually consume adapted milks and those consuming standard milk, along with the factors associated with their intake.
2. Materials and Methods
2.1. Study Design and Sample
The data used in this work are part of the EsNuPI study, which is a prospective, cross-sectional, observational study, conducted from October 2018 to January 2019. All details about the design, protocol, and methodology of the EsNuPI study have been already described in detail elsewhere [26].
The EsNuPI study was planned to determine the eating habits, energy and nutrient intake, physical activities, and sedentary behaviors of Spanish aged one to <10 years, which were non-vegan and living in urban areas with >50,000 inhabitants. Two sub-samples were selected, one including children taking standard milk (a representative sample of Spanish children; RS) and one of convenience, which included children taking adapted, enriched, or fortified milks, which we called the “adapted milk consumers sample” (AMS). In addition, considering the need for representation of all age and sex groups, the sample was stratified (50% boys, 50% girls, 1 to <3 years old, 3 to <6 years old, and 6 to <10 years old) [26,27].
The EsNuPI study was conducted under the Helsinki declaration and was approved by the Ethics Committee of the University of Granada (No. 659/CEIH/2018) and registered in ClinicalTrials.gov (Unique Protocol ID: FF01/2019).
2.2. Procedures and Data Collection
The study information was collected in an initial face to face interview and in a second telephone interview at least 7 days later. The data collected are described below.
2.2.1. Socio-Demographic and Anthropometric Information
In the first interview, a general questionnaire was applied to collect the following variables about children: place and date of birth, sex, academic level of parents or caregivers (elementary or less/secondary/university/higher education), place of residence, family income level, lifestyle, activity patterns, and sedentary behaviors of the child.
Height and weight data were declared by parents or caregivers, based on the child’s pediatric health card. Body mass index (BMI) was calculated and World Health Organization (WHO) reference standards were used to calculate BMI-Z scores [28,29]. BMI for age Z score was used to categorize children as ‘underweight’ (Z-BMI/age < −2 standard deviation (SD)), ‘normal BMI’ (Z-BMI/age −2 to +1 SD), or ‘overweight and obese’ (Z-BMI/age > +1 SD). Length/height for age Z score was used to categorize children as ‘stunting’ (Z-height/age < −2 SD), ‘normal height’ (Z-height/age −2 to +2 SD), or ‘high stature’ (Z-height/age > +2 SD).
2.2.2. Physical Activity and Sedentary Behavior Questionnaire
To assess physical activity and sedentary behaviors, a modification of a questionnaire previously validated in children <10 years old from Colombia, based on the memory of activities carried out in a seven-day period, was applied [30].
The activities carried out by the child in one day (24 h) during the last week (a seven-day record) were recorded, including information on sleep hours and screen time; data for weekdays and weekend days were recorded separately. For more detailed information, see Madrigal et al. [26,27].
2.2.3. Dietary Survey and Data Collection
Two 24 h dietary recalls (DR) were completed (one face-to-face and one by telephone) on non-consecutive days, including one weekday and one weekend day, using the parents or caregivers of the children to help determine the children’s food and drink consumption. Detailed information was requested on the dietary intake of the participants, indicating the ingredients, method of preparation, brands used for each dish consumed and the place of consumption (home or away). This information allowed us to code the products properly and to establish the weight consumed.
As supporting material for the correct completion of the dietary study, the interviewers used the “tables of common home measures, and habitual portion sizes for Spanish population” [31,32] and the “photo guide of common portions sizes of Spanish foods” [33], which was built using the “Pilot study for the Assessment of Nutrient intake and Food Consumption Among Kids in Europe” (PANCAKE) [34]. The photo guide included 12 food groups, 204 frequently consumed foods by Spanish children, and 944 photographs.
Furthermore, a software called “VD-FEN 2.1”, a Dietary Evaluation Program from the Spanish Nutrition Foundation (FEN) [33], was used to assess the reported intake of food, beverages, energy, and nutrients. This program uses Spanish food composition tables, with several expansions and updates [31].
In this paper, special attention was paid to the intake of nutrients most directly involved in bone remodeling to assess their reported intake and adequacy with respect to the European Food Safety Authority (EFSA) [35] recommendations. Furthermore, the calcium/phosphorus ratio was determined.
To determine the food sources of the nutrients under study, different food items were categorized into the following 18 food categories: “milk and dairy products”, “other dairy products”, “cereals”, “meat and meat products”, “oils and fats”, “bakery and pastry”, “fruits”, “vegetables”, “sugars and sweets”, “ready to cook/eat”, “beverages”, “legumes”, “eggs”, “fish and shellfish”, “appetizers”, “cereal-based baby foods and supplements”, “nuts”, and “sauces and condiments”. To clarify, “milk and dairy products” included yogurt, cheese, curd, and kefir; whereas “other dairy products” included dairy desserts, shakes, ice cream, cream, and condensed milk.
An analysis of the total amount of calcium, phosphorus, magnesium, and vitamin D provided by all the foods eaten by the population was performed. The population proportion method [36] was used to determine the contribution of each nutrient from the different food categories. Specifically, the calcium content specified in each food and beverage was added, according to its intake by everyone in the group. This calcium was compared to the total calcium consumed, which was obtained from the sum of the total calcium ingested by all participants during the two days. The percentage of calcium from each group was calculated as follows: (sum of calcium from food group (mg)/total sum of calcium from all foods (mg)) × 100 [36]. The same procedure was performed for the rest of nutrients studied (i.e., phosphorus, magnesium, and vitamin D).
2.3. Evaluation of Plausible Under- and Over-Reporters (Misreporting)
Intentional (as well as unintentional) misreporting, which comprises under- and over-reporting, are well-known problems in dietary assessments, which should be evaluated when conducting a dietary study [37]. Misreporting of energy intake for the EsNuPI study has been previously reported [27].
Subjects were identified as plausible under- or over-reporters of energy intake, considering the relationship between their energy intake (EI) and Basal metabolic rate (BMR), which was estimated using the equation of Schofield [38]. Given these criteria, under-reporters were identified as those with EI/BMR ratios up to 0.97–1.00, while over-reporters were identified by EI/BMR ratios above 2.45–2.58, depending on the subject’s age and sex.
It is important to assess misreporting; however, following the EFSA [39] recommendations, it is not appropriate to exclude potential misreports from the study. This is because the exclusion of misreports from the database can introduce bias into the research results. Therefore, they must be identified, but not excluded from the database.
2.4. Statistical Analysis
Once the dietary information was collected, the 746 foods reported by the children were grouped into 18 food groups and transformed into energy and nutrients for the analysis of the results.
As the average intake obtained by applying a 24 h dietary recall for only a small number of days (observed intakes) does not adequately represent the usual intake, it is necessary to apply a statistical model to eliminate the day-to-day variation in food consumption [40]. To this end, the method developed by Nusser et al. [41]—also known as the Iowa State University (ISU) method—was applied. This method consists of three steps: a transformation step, mapping the intake to a normal scale; an estimate of the usual intake by using a measurement error frame; and, finally, a retro-transformation step, to return the estimated usual intakes to their original scale.
The ISU method was implemented using the PC-SIDE software (version 1.0, 2003) (Iowa State University, Ames, IA, USA), which was designed for this purpose. This program estimates the percentiles of usual nutrient intake distributions and the percentages that remain above or below the dietary reference cut-off values. Whether the intake corresponded to the first 24 h DR performed in the initial interview or to the telephone interview was considered in the adjustment of dietary data, stratifying by sex, age group, and group membership (i.e., RS or AMS).
To assess nutrient adequacy, we used the Dietary Reference Values from EFSA [35], which includes reference values for calcium, phosphorus, magnesium, and vitamin D. The proportion of the population with usual intakes less than the average requirement (AR) provides an estimate for the proportion of the group whose intakes did not meet the nutrient requirements. For children aged 1 to <10 years, there are only established ARs for calcium, whereas for phosphorus, magnesium, and vitamin D, there are established adequate intakes (AIs). These AIs can be used to determine the proportion of individuals with adequate nutrient intake.
To describe the dietary intakes of the participants by sample group (RS and AMS), and by sex and age groups, the mean, standard deviation (SD), median, and 5th and 95th percentiles were used for continuous variables, and frequencies and percentages for categorical variables. For this analysis, the population was divided into those groups established by EFSA, according to age (calcium, phosphorus and vitamin D: 1 to <4 years, 4 to <6 years, and 6 to <10 years; magnesium: 1 to <3 years, 3 to <6 years, and 6 to <10 years) [35].
The Kolmogorov–Smirnoff normality test was used to check the normality of the distribution of the variables to decide between parametric or non-parametric analyses for comparisons. For variables that did not follow normality, appropriate non-parametric statistical tests were used for group comparisons.
Mann–Whitney U and Chi-squared tests were used to evaluate differences between the reference and adapted milk consumer samples (in the total sample and by age group). Variance analysis (ANOVA) with Bonferroni correction was used to make multiple comparisons or Kruskal–Wallis analysis to calculate differences between each age group within the established groups. Student’s t-test or Chi-squared test was used to evaluate adequacy differences between samples (RS and AMS) by sex and age groups. Kruskal–Wallis or Z-test with Bonferroni correction were used to perform multiple comparisons by age group between samples. Linear correlation and logistic regression analyses were also applied, in order to ascertain the influence of various variables on the intakes of the nutrients under study.
The level of significance was set at p < 0.05. Statistical analyses were performed using the statistical software package SPSS version 24.0 for Mac OS (IBM Corp., Armonk, NY, USA).
3. Results
3.1. Description of the Sample
The final EsNuPI sample included 1448 children (49.7% girls and 50.3% boys) between the ages of 1 and <10 years, whose parents or caregivers agreed to completed two 24 h DR. The RS group represented 48.8% of the sample studied and the AMS represented 51.2%.
Anthropometric, sociodemographic, and activity data are presented in Table 1, as well as data on consumption of supplements and number of feeding bottles or glasses of milk consumed per day.
Table 1.
General, anthropometric, and socioeconomic data by sex and age group in the Estudio Nutricional en Población Infantil Española (EsNuPI) population. Differences between reference sample and adapted milk consumer sample (n = 1448).
| Reference Sample | Adapted Milk Consumer Sample | |||||
|---|---|---|---|---|---|---|
| Total | Boys | Girls | Total | Boys | Girls | |
| n | 707 | 357 | 350 | 741 | 371 | 370 |
| Age group, n (%) | ||||||
| 1 to <3 years | 162 (22.9) * | 84 (23.5) * | 78 (22.3) * | 294 (39.7) * | 144 (38.8) * | 150 (40.5) * |
| 3 to <6 years | 244 (34.5) * | 122 (34.2) * | 122 (34.9) * | 262 (35.4) * | 128 (34.5) * | 134 (36.2) * |
| 6 to <10 years | 301 (42.6) * | 151 (42.3) * | 150 (42.9) * | 185 (25) * | 99 (26.7) * | 86 (23.2) * |
| Anthropometric characteristics, X ± SD | ||||||
| Weight (kg) # | 20.8 ± 8.4 * | 21.2 ± 8.5 * | 20.5 ± 8.2 | 17.4 ± 7.4 * | 17.9 ± 7.8 * | 16.9 ± 6.9 |
| Height (cm) # | 109.4 ± 20.1 * | 110.1 ± 20.2 * | 108.6 ± 20.0 | 100.5 ± 19.3 * | 101.7 ± 20.2 * | 99.2 ± 18.4 |
| BMI (kg/m2) # | 16.9 ± 2.9 | 16.9 ± 3.1 | 16.8 ± 2.7 | 16.8 ± 2.9 | 16.8 ± 2.6 | 16.8 ± 3.1 |
| Z-BMI/Age # | 0.59 ± 1.73 | 0.64 ± 1.97 | 0.54 ± 1.44 | 0.57 ± 1.72 | 0.52 ± 1.67 | 0.61 ± 1.77 |
| Z-Weight/Height # | 0.59 ± 1.79 | 0.61 ± 2.09 | 0.57 ± 1.42 | 0.62 ± 1.69 | 0.53 ± 1.61 | 0.71 ± 1.76 |
| Z-Height/Age # | −0.25 ± 1.7 * | −0.14 ± 1.82 * | −0.36 ± 1.57 | −0.54 ± 1.82 * | −0.52 ± 1.85 * | −0.55 ± 1.79 |
| Physical activity (PAL) (X ± SD) | ||||||
| 1 to <3 years | 1.56 ± 0.32 | 1.60 ± 0.32 | 1.53 ± 0.31 | 1.54 ± 0.30 a | 1.54 ± 0.29 a,b | 1.53 ± 0.30 |
| 3 to <6 years | 1.56 ± 0.22 | 1.59 ± 0.21 | 1.52 ± 0.23 | 1.52 ± 0.22 a | 1.53 ± 0.24 a | 1.52 ± 0.19 |
| 6 to <10 years | 1.58 ± 0.21 | 1.59 ± 0.22 | 1.57 ± 0.20 | 1.61 ± 0.21 b | 1.62 ± 0.21 b | 1.60 ± 0.21 |
| Size of the municipality n (%) | ||||||
| 50,001–300,000 people | 376 (53.2) | 193 (54.1) | 183 (52.3) | 406 (54.8) | 204 (55.0) | 202 (54.6) |
| >300,000 people | 331 (46.8) | 164 (45.9) | 167 (47.7) | 335 (45.2) | 167 (45.0) | 168 (45.4) |
| Highest level of education achieved by one of the parents, n (%) ¥ | ||||||
| ≤10 years of education | 22 (3.2) | 9 (2.6) | 13 (3.8) | 16 (2.2) | 8 (2.2) | 8 (2.2) |
| Secondary education | 428 (62.3) | 227 (65.4) | 201 (59.1) | 420 (57.9) | 210 (58.0) | 210 (57.7) |
| University studies | 237 (34.5) | 111 (32.0) | 126 (37.1) | 290 (39.9) | 144 (39.8) | 146 (40.1) |
| Family income, n (%) | ||||||
| ≤2000 €/month | 297 (42.0) | 146 (40.9) | 151 (43.1) | 297 (40.1) | 148 (39.9) | 149 (40.3) |
| >2000 €/month | 226 (32.0) | 123 (34.5) | 103 (29.4) | 238 (32.1) | 110 (29.6) | 128 (34.6) |
| Not known/no answer | 184 (26.0) | 88 (24.6) | 96 (27.4) | 206 (27.8) | 113 (30.5) | 93 (25.1) |
| Dietary supplements, n (%) | ||||||
| Vitamin D, n (%) | 3 (0.4) | 3 (0.8) | 0 (0.0) | 5 (0.7) | 4 (1.1) | 1 (0.3) |
| Multivitamins and Minerals or Vitamins, n (%) | 5 (0.7) | 2 (0.6) | 3 (0.9) | 5 (0.7) | 3 (0.8) | 2 (0.5) |
| Number of feeding bottles or glasses of milk per day, n (%) | ||||||
| Less than 2 | 222 (32.9) | 110 (32.0) | 115 (33.8) | 178 (24.1) | 92 (24.9) | 86 (23.3) |
| 2 or more | 459 (67.1) | 234 (68.0) | 225 (66.2) | 561 (75.9) | 278 (75.1) | 283 (76.7) |
# Variable that does not follow a normal distribution. ¥ Only information on 1413 children is available. SD: standard deviation; BMI: body mass index. Z-BMI/age: z-score for BMI for age. PAL: physical activity level. The PAL was calculated for individual and group level according to the European Food Safety Authority (EFSA) protocol, in order to assess misreporting (EFSA, 2013). * Significant differences between the reference sample and adapted milk consumer sample (in the total sample and by sex) are shown, applying the Chi-square and Mann–Whitney tests. Different superscript letters (a,b) indicate differences between age groups in the same column (same sex and same sample type: reference sample (RS) or adapted milks (AMS)), applying ANOVA tests. A p-Value < 0.05 was considered statistically significant.
In AMS, there was a higher percentage of children aged 1 to <6 years and, in RS, there were more children aged 6 years and older. This could explain why the weight and height of the AMS children were lower than those observed in RS (Table 1).
The consumption of dietary supplements very low, only 0.4% of RS and 0.7% of AMS took vitamin D supplements and 0.7% of RS and 0.7% of AMS took a polyvitamin with minerals or vitamin complexes (Table 1).
3.2. Usual Calcium, Phosphorus, Magnesium, and Vitamin D Intake in Children under Study
Table 2 presents the usual daily intake of calcium, phosphorus, magnesium, and vitamin D in the whole population and separately by age and sex groups, as well as differentiating between the RS and the AMS. Different age ranges were used for calcium, phosphorus, and vitamin D, as compared to Magnesium, according to the RI/AI marked by EFSA [35].
Table 2.
Daily calcium, phosphorus, magnesium, and vitamin D usual intake by sex and age group in the EsNuPI population. Differences between RS and AMS groups (n = 1448).
| Group by Age | AR | AI | Boys | Girls | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Median (P5–P95) | <AR (%) | >AI (%) | Mean | SD | Median (P5–P95) | <AR (%) | >AI (%) | |||
| Calcium (mg/day), RS # | ||||||||||||
| 1 to <4 years | 390 | 746 a * | 184 | 736 (462–1064) a * | 1.6 | 744 a | 149 | 740 (508–997) a | 0.5 | |||
| 4 to <6 years | 680 | 775 a,b * | 112 | 772 (597–964) a,b * | 20.0 | 743 a | 161 | 732 (499–1026) b | 37.0 | |||
| 6 to <10 years | 680 | 815 b * | 192 | 805 (517–1148) b * | 24.9 | 799 b * | 150 | 791 (566–1058) c * | 22.0 | |||
| Calcium (mg/day), AMS # | ||||||||||||
| 1 to <4 years | 390 | 702 a * | 131 | 697 (495–924) a * | 0.5 | 735 a | 146 | 727 (511–987) a | 0.4 | |||
| 4 to <6 years | 680 | 835 b * | 150 | 829 (600–1093) a * | 14.9 | 785 b | 132 | 780 (574–1009) b | 21.5 | |||
| 6 to <10 years | 680 | 903 c * | 131 | 897 (696–1127) b * | 3.7 | 846 c * | 171 | 833 (590–1147) c * | 18.6 | |||
| Phosphorus (mg/day), RS # | ||||||||||||
| 1 to <4 years | 250 | 943 a * | 215 | 942 (591–1298) a * | 100 | 939 a * | 196 | 940 (615–1260) a * | 100 | |||
| 4 to <6 years | 440 | 1103 b | 200 | 1102 (775–1434) b * | 100 | 1068 b | 175 | 1061 (792–1366) b | 100 | |||
| 6 to <10 years | 440 | 1179 c | 242 | 1164 (809–1600) c | 100 | 1143 c | 140 | 1138 (920–1381) c | 100 | |||
| Phosphorus (mg/day), AMS # | ||||||||||||
| 1 to <4 years | 250 | 826 a* | 191 | 822 (518–1146) a * | 100 | 870 a * | 213 | 861 (536–1235) a * | 100 | |||
| 4 to <6 years | 440 | 1116 b | 193 | 1108 (814–1446) b * | 100 | 1042 b | 160 | 1039 (784–1309) b | 100 | |||
| 6 to <10 years | 440 | 1182 c | 160 | 1175 (932–1456) c | 100 | 1130 c | 178 | 1124 (846–1432) c | 100 | |||
| Magnesium (mg/day), RS # | ||||||||||||
| 1 to <3 years | 170 | 173 a | 55 | 170 (86–257) a | 50.3 | 175 a | 35 | 173 (121–235) a | 54.0 | |||
| 3 to <6 years | 230 | 205 b * | 31 | 202 (159–258) b * | 19.6 | 200 b * | 33 | 198 (149–259) a,b * | 17.9 | |||
| 6 to <10 years | 230 | 220 c * | 46 | 218 (150–306) c * | 38.8 | 210 c * | 32 | 208 (162–266) b * | 24.5 | |||
| Magnesium (mg/day), AMS # | ||||||||||||
| 1 to <3 years | 170 | 178 a | 47 | 173 (111–263) a | 52.9 | 171 | 51 | 165 (100–265) a | 45.5 | |||
| 3 to <6 years | 230 | 185 a,b * | 29 | 183 (140–236) b * | 7.2 | 181 * | 30 | 180 (134–231) b * | 5.3 | |||
| 6 to <10 years | 230 | 192 b * | 27 | 191 (150–237) b * | 7.8 | 185 * | 45 | 183 (113–262) b * | 16.0 | |||
| Vitamin D (µg/day), RS # | ||||||||||||
| 1 to <4 years | 15 | 3.20 * | 2.84 | 2.43 (0.36–8.83) a,b * | 0.6 | 3.05 a * | 2.70 | 2.28 (0.34–8.55) * | 0.4 | |||
| 4 to <6 years | 15 | 2.77 * | 2.17 | 2.20 (0.45–7.04) a * | 0.1 | 3.14 b * | 2.12 | 2.63 (0.76–7.22) * | 0.1 | |||
| 6 to <10 years | 15 | 2.96 * | 0.96 | 2.85 (1.61–4.72) b * | 0.0 | 3.09 a,b * | 1.77 | 2.72 (0.97–6.52) * | 0.0 | |||
| Vitamin D (µg/day), AMS # | ||||||||||||
| 1 to <4 years | 15 | 6.80 * | 2.32 | 6.57 (3.42–10.95) * | 0.4 | 7.51 a * | 2.44 | 7.08 (4.30–12.10) a * | 0.9 | |||
| 4 to <6 years | 15 | 8.32 * | 3.44 | 7.88 (3.51–14.63) * | 4.3 | 7.02 a,b * | 2.50 | 6.73 (3.46–11.55) b * | 0.6 | |||
| 6 to <10 years | 15 | 7.47 * | 2.98 | 7.14 (3.18–12.86) * | 1.6 | 6.67 b * | 2.61 | 6.38 (2.92–11.4) b * | 0.5 | |||
Average requirement (AR) and adequate intakes (AI) (EFSA, 2017). RS: reference sample (n = 707). AMS: adapted milk consumers sample (n = 741). # Variable that does not follow a normal distribution Results are expressed as the mean, standard deviation, median, and P5–P95 (in brackets). The differences between the RS and AMS sample (in same sex and age group) are indicated by asterisks (*) applying T-student and Mann–Whitney tests. Different superscript letters (a,b,c) indicate differences between age groups in the same column (same sex and same sample type: reference sample (RS) or adapted milks (AMS)),applying the Kruskal–Wallis or ANOVA tests. Different letters indicate significant differences. A p-Value < 0.05 was considered statistically significant.
There were no sex differences in the intake of the nutrients studied, except for magnesium, for which boys (194 ± 45 mg/day) had a significantly higher intake than girls (188 ± 41 mg/day).
The intake of calcium (r = 0.283), phosphorus (r = 0.570), and magnesium (r = 0.316) increased with age (p < 0.001). However, vitamin D intake (r = −0.191) decreased with age (p < 0.001; Table 2).
3.2.1. Calcium
Calcium intake was lower than AR in a small percentage of children aged 1–3 years, but the percentage increased in children aged 6–10 and especially in those aged 4–6. As a result, the percentage of children aged 4 and over with calcium intake below AR was 24.5% in RS boys (compared to 26.7% in RS girls) and 8.1% in AMS boys (compared to 17.5% in AMS girls). It should be emphasized that the calcium intake was more adequate (significantly higher) in children aged 6 and over in the AMS group, compared to those in the RS group (Table 2).
Having a higher level of education in one parent or being underweight were factors in preventing calcium intake from being similar to or higher than the P50, in the RS group (Table 3), while taking two or more feeding bottles or glasses of milk per day was a factor that helped to achieve a calcium intake above the median both in the RS and AMS groups (Table 3 and Table 4).
Table 3.
Odds ratios and 95% confidence intervals for the presence of an intake similar to or greater than the median of calcium, phosphorus, magnesium, and vitamin D, relative to family and personal factors in the reference sample (RS) of the EsNuPI children population (n = 707).
| Calcium (mg/day) (≥P50) † | Phosphorus (mg/day) (≥P50) † | Magnesium (mg/day) (≥P50) † | Vitamin D (µg/day) (≥P50) † | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Factor | Subcategories | OR | IC | p | OR | IC | p | OR | IC | p | OR | IC | p |
| Sex | Boys | 1 | 1 | 1 | 1 | ||||||||
| Girls | 0.983 | 0.732–1.32 | 0.910 | 0.983 | 0.732–1.321 | 0.911 | 1.006 | 0.749–1.35 | 0.970 | 0.994 | 0.74–1.335 | 0.970 | |
| Age ¥ | 1 to <4 years | 1 | 1 | 1 | 1 | ||||||||
| 4 to <6 years | 1.075 | 0.716–1.612 | 0.728 | 1.042 | 0.695–1.564 | 0.842 | 1.000 | 0.672–1.488 | 1.000 | 1.042 | 0.695–1.564 | 0.842 | |
| 6-<10 years | 1.031 | 0.740–1.436 | 0.857 | 1.000 | 0.718–1.393 | 1.000 | 0.993 | 0.678–1.455 | 0.973 | 0.987 | 0.708–1.375 | 0.937 | |
| Number of feeding bottles or glasses of milk per day | Less than 2 | 1 | 1 | 1 | 1 | ||||||||
| 2 or more | 1.681 | 1.218–2.320 | 0.002 * | 1.252 | 0.910–1.723 | 0.168 | 1.127 | 0.819–1.551 | 0.463 | 1.167 | 0.848–1.605 | 0.344 | |
| Physical activity (PAL) | <P50 by sex and age | 1 | 1 | 1 | 1 | ||||||||
| ≥P50 by sex and age | 1.023 | 0.761–1.374 | 0.880 | 0.892 | 0.664–1.199 | 0.449 | 0.873 | 0.650–1.173 | 0.366 | 1.269 | 0.944–1.705 | 0.114 | |
| Size of the municipality | 50,001–300,000 people | 1 | 1 | 1 | 1 | ||||||||
| >300,0000 people | 1.277 | 0.950–1.716 | 0.106 | 1.25 | 0.930–1.68 | 0.140 | 1.336 | 0.994–1.797 | 0.055 | 1.449 | 1.077–1.949 | 0.014 * | |
| Family income | ≤2000 €/month | 1 | 1 | 1 | 1 | ||||||||
| >2000 €/month | 0.838 | 0.593–1.186 | 0.319 | 1.140 | 0.806–1.612 | 0.459 | 1.519 | 1.072–2.151 | 0.019 * | 1.071 | 0.757–1.514 | 0.699 | |
| Not known/no answer | 0.877 | 0.607–1.267 | 0.485 | 0.903 | 0.625–1.305 | 0.587 | 1.133 | 0.784–1.638 | 0.505 | 0.860 | 0.595–1.243 | 0.422 | |
| Highest level of education achieved by one of the parents | ≤10 years of education | 1 | 1 | 1 | 1 | ||||||||
| Secondary education | 0.297 | 0.108–0.819 | 0.019 * | 0.358 | 0.137–0.932 | 0.035 * | 0.810 | 0.343–1.915 | 0.632 | 0.402 | 0.161–1.005 | 0.051 | |
| University studies | 0.264 | 0.094–0.738 | 0.011 * | 0.391 | 0.148–1.034 | 0.058 | 0.899 | 0.374–2.161 | 0.812 | 0.539 | 0.212–1.369 | 0.194 | |
| BMI for age | Normal BMI | 1 | 1 | 1 | 1 | ||||||||
| Overweight and obese | 0.932 | 0.683–1.272 | 0.658 | 1.067 | 0.782–1.457 | 0.681 | 0.999 | 0.732–1.364 | 0.997 | 1.015 | 0.744–1.385 | 0.925 | |
| Underweight | 0.408 | 0.190–0.879 | 0.022 * | 0.647 | 0.314–1.335 | 0.238 | 0.558 | 0.268–1.163 | 0.120 | 0.558 | 0.268–1.163 | 0.120 | |
| Height for age | Normal height | 1 | 1 | 1 | 1 | ||||||||
| High stature | 1.246 | 0.744–2.087 | 0.404 | 1.549 | 0.918–2.612 | 0.101 | 1.538 | 0.911–2.594 | 0.107 | 1.080 | 0.646–1.804 | 0.769 | |
| Stunting | 0.836 | 0.519–1.349 | 0.463 | 1.006 | 0.625–1.619 | 0.981 | 0.854 | 0.53–1.378 | 0.518 | 1.472 | 0.909–2.385 | 0.116 | |
OR: odds ratio. PAL: physical activity level. † P50 or median was calculated in the reference group for each nutrient by sex and age group, and was used to categorize children according to whether they had a usual nutrient intake below the median or superior. ¥ Except for magnesium (1 to <3 years, 3 to <6 years, 6 to <10 years). Underweight was defined as Z-BMI/age < −2SD, normal BMI/age was defined as Z-BMI/age −2SD to +1SD and overweight and obese as Z-BMI/age > +1SD, as per WHO guidelines [28,29]. Stunting was defined as Z-height/age < −2SD, normal BMI/age was defined as Z-height/age −2SD to +2SD and high stature as Z-height/age > +2SD, as per WHO guidelines. * A p-Value < 0.05 was considered statistically significant.
Table 4.
Odds ratios and 95% confidence intervals for the presence of an intake similar to or greater than the median of calcium, phosphorus, magnesium, and vitamin D, relative to family and personal factors, in the adapted milk consumer sample (AMS) of the EsNuPI children population (n = 741).
| Calcium (mg/day) (≥P50) † | Phosphorus (mg/day) (≥P50) † | Magnesium (mg/day) (≥P50) † | Vitamin D (µg/day) (≥P50) † | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Factor | Subcategories | OR | IC | p | OR | IC | p | OR | IC | p | OR | IC | p |
| Sex | Boys | 1 | 1 | 1 | 1 | ||||||||
| Girls | 1.005 | 0.754–1.341 | 0.971 | 0.995 | 0.746–1.327 | 0.971 | 1.005 | 0.754–1.341 | 0.971 | 0.995 | 0.746–1.327 | 0.971 | |
| Age ¥ | 1 to <4 years | 1 | 1 | 1 | 1 | ||||||||
| 4 to <6 years | 1.029 | 0.703–1.506 | 0.885 | 1.000 | 0.683–1.464 | 1.000 | 1.000 | 0.717–1.395 | 1.000 | 1.000 | 0.683–1.464 | 1.000 | |
| 6 to <10 years | 1.011 | 0.715–1.430 | 0.951 | 1.011 | 0.715–1.430 | 0.951 | 0.989 | 0.685–1.429 | 0.954 | 1.011 | 0.715–1.430 | 0.951 | |
| Number of feeding bottles or glasses of milk per day | Less than 2 | 1 | 1 | 1 | 1 | ||||||||
| 2 or more | 2.206 | 1.556–3.129 | 0.000* | 1.302 | 0.928–1.826 | 0.127 | 0.961 | 0.686–1.346 | 0.815 | 2.352 | 1.655–3.342 | 0.000 * | |
| Physical activity (PAL) | <P50 by sex and age | 1 | 1 | 1 | 1 | ||||||||
| ≥P50 by sex and age | 0.797 | 0.597–1.063 | 0.123 | 0.968 | 0.726–1.291 | 0.825 | 0.763 | 0.571–1.018 | 0.066 | 1.067 | 0.800–1.423 | 0.659 | |
| Size of the municipality | 50,001–300,000 people | 1 | 1 | 1 | 1 | ||||||||
| >300,000 people | 0.874 | 0.654–1.167 | 0.362 | 1.427 | 1.067–1.908 | 0.016 * | 1.441 | 1.078–1.927 | 0.014 * | 0.709 | 0.530–0.948 | 0.020 * | |
| Family income | ≤2000 €/month | 1 | 1 | 1 | 1 | ||||||||
| >2000 €/month | 0.973 | 0.692–1.369 | 0.877 | 1.245 | 0.885–1.751 | 0.209 | 1.406 | 0.999–1.980 | 0.051 | 1.183 | 0.841–1.665 | 0.334 | |
| Not known/no answer | 0.854 | 0.598–1.219 | 0.385 | 1.128 | 0.790–1.61 | 0.507 | 1.489 | 1.042–2.129 | 0.029* | 0.938 | 0.658–1.339 | 0.726 | |
| Highest level of education achieved by one of the parents | ≤10 years of education | 1 | 1 | 1 | 1 | ||||||||
| Secondary education | 1.039 | 0.383–2.820 | 0.940 | 1.100 | 0.405–2.986 | 0.852 | 0.770 | 0.282–2.107 | 0.611 | 0.935 | 0.345–2.539 | 0.896 | |
| University studies | 0.933 | 0.341–2.554 | 0.893 | 0.883 | 0.323–2.417 | 0.809 | 0.789 | 0.286–2.174 | 0.646 | 1.071 | 0.392–2.932 | 0.893 | |
| BMI for age | Normal BMI | 1 | 1 | 1 | 1 | ||||||||
| Overweight and obese | 1.045 | 0.767–1.423 | 0.783 | 1.045 | 0.767–1.423 | 0.783 | 1.063 | 0.780–1.449 | 0.697 | 1.194 | 0.876–1.627 | 0.262 | |
| Underweight | 0.822 | 0.436–1.552 | 0.546 | 0.747 | 0.394–1.414 | 0.370 | 0.837 | 0.444–1.58 | 0.583 | 0.868 | 0.460–1.637 | 0.661 | |
| Height for age | Normal height | 1 | 1 | 1 | 1 | ||||||||
| High stature | 1.260 | 0.721–2.201 | 0.417 | 0.929 | 0.534–1.617 | 0.795 | 0.868 | 0.499–1.512 | 0.618 | 0.777 | 0.445–1.357 | 0.375 | |
| Stunting | 0.813 | 0.548–1.206 | 0.303 | 0.531 | 0.354–0.795 | 0.002 * | 0.863 | 0.582–1.278 | 0.462 | 1.165 | 0.786–1.727 | 0.447 | |
OR: odds ratio. PAL: physical activity level. † P50 or median was calculated in in the adapted milk consumer group for each nutrient by sex and age group, and was used to categorize children according to whether they had a usual nutrient intake below the median or superior. ¥ Except for magnesium (1 to <3 years, 3 to <6 years, 6 to <10 years). Underweight was defined as Z-BMI/age < −2SD, normal BMI/age was defined as Z-BMI/age −2SD to +1SD and overweight and obese as Z-BMI/age > +1SD, as per World Health Organization (WHO) guidelines [28,29]. Stunting was defined as Z-height/age < −2SD, normal BMI/age was defined as Z-height/age −2SD to +2SD and high stature as Z-height/age > +2SD, as per WHO guidelines. * A p-Value < 0.05 was considered statistically significant.
Usual calcium intake showed a weak positive (but significant) association with the height z-score in the total sample (r = 0.126; p = 0.000). By age, this positive correlation was found in children aged 4 to 5 years (r = 0.105; p = 0.018) and those 6 years and older (r = 0.134; p = 0.003).
3.2.2. Phosphorus
The intake of phosphorus in all cases exceeded AI, and was significantly lower in 1–3 years children of the AMS group, compared to those of the RS group (Table 2).
Having secondary education as highest level of education in one parent was associated with lower phosphorus intake in RS children. Those living in areas with larger populations (>300,000 people) were more likely to have intakes of phosphorus above the median (AMS), while having a delay in the height for age (or stunting) in AMS group was associated with a greater difficulty in achieving phosphorus intake similar to or greater than median (Table 3 and Table 4).
In the EsNuPI study, the ratio for calcium to phosphorus for the whole population was 0.78 ± 0.16 (RS: 0.74 ± 0.13 vs. AMS: 0.82 ± 0.16), which was very low compared to the recommendations. Specifically, 93.6% of the studied children had a calcium/phosphorus ratio below 1/1. This relationship decreased with age, but was significantly higher in the AMS group than in RS in all age categories considered (RS: 0.84 ± 0.18 vs. AMS: 0.90 ± 0.21 for children aged 1–3 years; RS: 0.72 ± 0.1 vs. AMS: 0.78 ± 0.11 in children aged 4–5 years; and RS: 0.69 ± 0.09 vs. AMS: 0.76 ± 0.09 for children aged 6 years and older).
3.2.3. Magnesium
Average and median magnesium intakes were close to the AI, although the percentage of children aged 3 to <6 years that exceeded the AI was low. Children aged 3 to <6 years and 6 to <10 years in the AMS group had significantly lower magnesium intakes than those in the RS group (Table 2).
Larger population size (>300,000 people) or undeclared income (Not known/no answer) were associated to have magnesium intake similar to or greater than median in AMS children (Table 4). Additionally, having higher incomes (>2000 €/month) was associated with higher magnesium intake in RS children (Table 3).
3.2.4. Vitamin D
The intake of vitamin D was significantly higher in AMS boys and girls, in all age groups, compared to RS children (Table 2). Only 0–0.6% of children in RS and 0.4–4.3% of children in AMS exceeded the AI.
Taking two or more feeding bottles or glasses of milk per day was a factor that helped to achieve vitamin D intake similar to or greater than median in AMS children (Table 4). Furthermore, those living in higher population areas (>300,000 people) were more likely to have intakes of vitamin D >P50 in RS children, while the same was associated with lower vitamin intake in AMS children.
3.2.5. Calcium, Phosphorus, Magnesium and Vitamin D in Plausible Reporters
The percentage of plausible energy reporters was high for both groups (84.7% in the RS group and 83.5% in the AMS group) [27]. Therefore, the data presented in the rest of this report have not been adjusted for misreporting.
Nevertheless, considering data of the usual daily intake of calcium, phosphorus, magnesium, and vitamin D of the plausible reporters only (Supplementary Table S1), very similar results were obtained to those found in the total sample.
Calcium intake was significantly higher in boys aged 6 and over in the AMS group, compared to those in the RS group; however, in plausible reporters, the difference was not significant in girls. The intake of phosphorus was significantly higher in males aged 1–3 years of the RS group, compared to those in the AMS group, and in boys and girls aged 4 to <6 years in the RS group, compared to the AMS group.
Regarding the calcium–phosphorus ratio, magnesium, and vitamin D, the situation was very similar to that obtained for the total sample.
3.3. Contribution of Food Sources to Calcium, Phosphorus, Magnesium and Vitamin D Reported Intakes
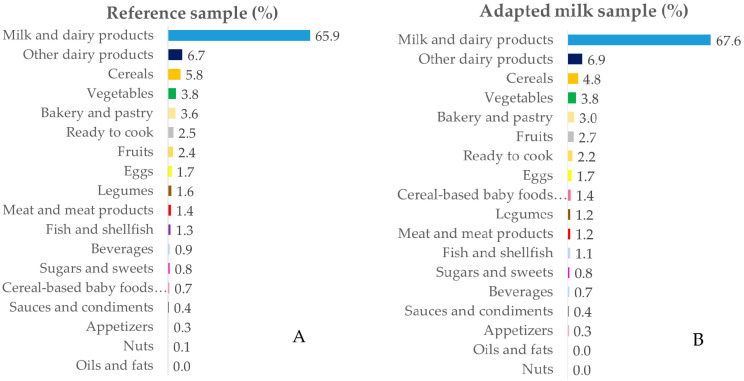
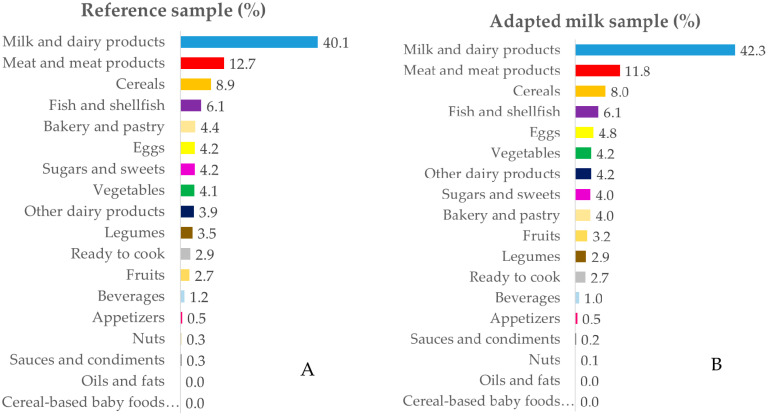
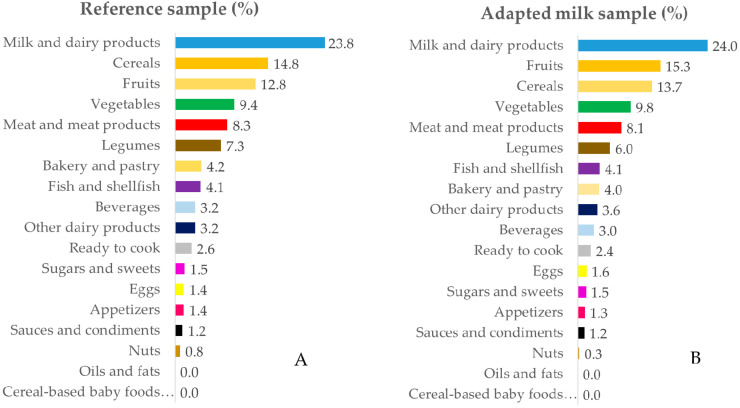
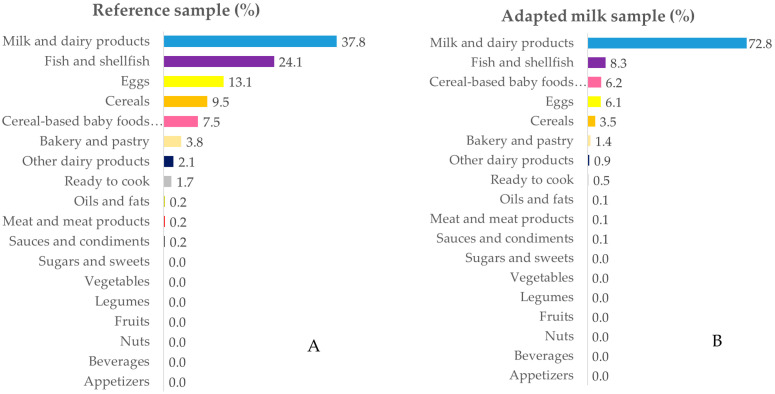
The intake data were grouped into 18 food groups for in-depth analysis. Figure 1, Figure 2, Figure 3 and Figure 4 represent the contribution (%) of food and beverage categories to the daily calcium, phosphorus, magnesium, and vitamin D reported intakes for the whole population. The data obtained for children in RS and AMS are summarized, and the food groups are presented in decreasing order of the amount of the nutrients they contribute to the daily intake.
Figure 1.
Percentage of the 18 food groups sources, in terms of the total calcium intake (%), among the reference sample (A) and the adapted milk consumer sample (B) of the Spanish Pediatric Population (EsNuPI) study.
Figure 2.
Percentage of the 18 food groups sources, in terms of the total phosphorus intake (%), among the reference sample (A) and the adapted milk consumer sample (B) of the Spanish Pediatric Population (EsNuPI) study.
Figure 3.
Percentage of the 18 food groups sources, in terms of the total magnesium intake (%), among the reference sample (A) and the adapted milk consumer sample (B) of the Spanish Pediatric Population (EsNuPI) study.
Figure 4.
Percentage of the 18 food groups sources, in terms of the total vitamin D intake (%), among the reference sample (A) and the adapted milk consumer sample (B) of the Spanish Pediatric Population (EsNuPI) study.
3.3.1. Calcium
The main sources of calcium for RS and AMS children were milk and dairy products, followed by other dairy products, cereals, vegetables, bakery and pastry, ready to cook/eat, fruits, and eggs. It can be noted that, in AMS children, cereal-based baby foods and supplements contributed 1.4% of the calcium; whereas, in RS children, they contributed 0.7% (Figure 1A,B). No major differences were observed when considering each age block separately (Supplementary Table S2).
3.3.2. Phosphorus
The largest source of phosphorus was milk and dairy products, followed (in both groups) by meat and meat products, cereals, fish, and shellfish. Foods that provided smaller amounts of phosphorus included bakery and pastry, eggs, sugars and sweets, and vegetables (Figure 2A,B). The above decreasing contribution order was maintained when considering different age groups (Supplementary Table S3).
3.3.3. Magnesium
Milk and dairy products were the main sources of magnesium for both RS and AMS groups, followed by cereals and fruits. Other relevant sources of magnesium were vegetables, meat and meat products, and legumes. The rest of the sources contributed less than 4.2% of the magnesium ingested (Figure 3A,B). The specific data characteristics of each age group are specified in Supplementary Table S4.
3.3.4. Vitamin D
The main source of vitamin D was milk and dairy products in both groups, followed by fish, eggs, cereals, cereal-based baby foods, supplements, and bakery and pastry (Figure 4A,B; see Supplementary Table S5 also).
4. Discussion
This paper provides recent estimates of the calcium, phosphorus, magnesium, and vitamin D intake, together with the food sources of these nutrients, in a representative sample of Spanish infants, toddlers, and children (1 to <10 years), as well as analyzing the differences between those who usually take adapted and fortified milk formulas versus standard milk. Furthermore, the influences of different factors (e.g., sociodemographic, anthropometric, parental educational level, and so on) on the intake of some of these nutrients were also analyzed.
The anthropometric, sociodemographic, and physical activity data of the children studied were similar to those found in other studies of Spanish children of a similar age [13,14,20,42,43,44].
Among the nutrients studied, calcium and vitamin D have been the most frequently analyzed, in relation to bone mass [4,12,14,20,45,46,47]. However, it is also important to pay attention to magnesium in relation to children’s bone health. Abrams et al. [9] in a sample of 63 healthy children aged 4 to 8 years found that magnesium intake but not calcium intake, was significantly associated with both total bone mineral content and density.
4.1. Calcium
Calcium intake in RS and AMS groups was similar to that found in Spain by Olza et al. [12], in children in the ANIBES study aged 9–12 years (872 ± 22 mg/day in boys and 759 ± 26 mg/day in girls), and also to those found by Dalmau et al. [20], in children in the ALSALMA study aged 1–2 years (795.1 mg/day) and 2–3 years (858.6 mg/day); by Ortega et al. [14], in children aged 7–11 years (859.9 ± 249.2 mg/day); by Chouraqui et al. [45] (770–792 mg/day in children of 12–23 months and 729–746 mg/day in children of 24–35 months) and by Jiménez-Aguilar et al. [46] (759.3 mg/day in children of 1–2 years and 859.9 mg/day in children of 3–4 years). However, it was slightly lower than that found in the ENALIA study [13] (928 ± 178.5 and 879 ± 161.9 mg/day in boys and girls of 1–3 years; 956 ± 159.1 and 903 ± 147.6 in boys and girls of 4–8 years; and 1025 ± 212.5 and 959 ± 167.7 mg/day in boys and girls of 9–13 years, respectively) and in the “Ingesta de calcio y densidad mineral ósea en escolares españoles” (CADO) study in children of 5–12 years (1227 ± 404 mg/day in boys and 1163 ± 401 mg/day in girls) [4]; it was also slightly lower than that found by other authors in other countries [19,22,48].
A review examining nutrient intake in nine European countries (i.e., Belgium, Denmark, France, Germany, the Netherlands, Poland, Serbia, Spain, and the UK) indicated that the intake of calcium in children aged 4–10 years ranges from 563 mg/day to 1106 mg/day [47], so the intake found in this paper was within the range observed by these authors.
Calcium intake increased with age, as has been found in other studies [13,46]; but as the AR also increases with age, the percentage of children with <AR intakes was higher in the older groups, especially in those of 4 to <6 years (Table 2 and Supplementary Table S1).
The percentage of inadequate calcium intake was similar to that observed in other studies in children of similar ages [20,22,45,49]. Calcium intake was significantly higher in children aged 6 and over in the AMS group, compared to those in the RS group (Table 2). Even though there is still controversy, several studies have analyzed the convenience of using products adapted to the higher nutrient needs of children [22,45]. Most of these studies have been conducted in young children (aged 1–3 years), in which authors such as Chouraqui et al. [45] have pointed out that the consumption of young-child formulas may help infants and children at risk of nutrient deficiencies to meet their nutritional requirements. These authors found that, at all ages studied, the children consuming young-child formula had higher intakes of several nutrients, especially vitamin D; although they also mentioned that vitamin D intake remained below the EFSA AI. Eussen et al. [22] also indicated that the replacement of habitual cow’s milk intake (in children 12–18 months) by a matching volume of 300 mL of young-child formula may lead to nutritional intakes close to recommendations in young children. The European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on Nutrition has suggested that, based on available evidence, there is no necessity for the routine use of young-child formula in children from 1 to 3 years of life, but that they can be used as part of a strategy to increase the intake of iron, vitamin D, and n-3 PUFA and decrease the intake of protein, compared with unfortified cow’s milk [50]. Coinciding with the benefit observed by Chouraqui et al. [45] associated with the consumption of young-child formula, a higher calcium intake was found in children aged 6–10 years taking AMS in this research, showing that membership to the AMS group was associated with a higher likelihood of having higher calcium intake than median.
Some authors [51] have suggested that socioeconomic status is a predictor of higher calcium and vitamin D intake, and that physical activity was also correlated to daily calcium and vitamin D intake; however, this type of influence was not observed in our study. However, higher income was a positive factor in achieving phosphorus and magnesium ≥P50 intakes. Considering the highest level of education achieved by one of the parents, it was observed that university education in one parent was a factor in preventing calcium intake from being similar to or higher than the P50 (Table 4). These results coincide with those of Tornaritis et al. [52], who also found no influence on the intake of these nutrients in children from 6 to 18 years of age, depending on the educational level of their mother.
We found a weak positive correlation between usual calcium intake and height z-score. This result was also observed by Rubio-López et al. [49].
4.2. Phosphorus
The results obtained for phosphorus intake were similar to those observed in other studies [12,20,22,45,48] and slightly lower than those obtained in other research [13,19] for children of a similar age (Table 2 and Supplementary Table S1).
Intake of phosphorus exceeded AI in 100% of the children studied and, as in other investigations [12,13], its contribution can be considered as sufficient and, in some age groups, even excessive [53].
4.3. Calcium–Phosphorus Ratio
Authors such as Loughrill et al. [54] have suggested that adequate intake of calcium and phosphorus should be in the appropriate ratio of 1–2:1. Poor calcium absorption can be magnified if the calcium–phosphorus ratio is inadequate [14,49,55,56,57].
As calcium intake was lower than AR in a variable percentage of children and phosphorus intake was higher than AI, this ratio was frequently lower than the recommended ratio, as has been found in other studies [14,49,55]. Specifically, 93.6% of the studied children had a calcium–phosphorus ratio below 1. Rubio-López et al. [49] also found that 99% of studied children had a calcium–phosphorus ratio below 1.
However, the calcium–phosphorus ratio was significantly higher in AMS than RS, a difference that remained in all age groups. This is a benefit for the AMS group, which has a higher calcium intake and higher calcium/phosphorus ratios in their diets; given that low calcium intake associated with high phosphorus intake may have an adverse effect on the use of calcium and maintenance of bone mass in children [49,54,55].
4.4. Magnesium
The magnesium intake found in the EsNuPI study was similar to that found by other authors [12,19,20,45], and somewhat inferior to that found by López-Sobaler et al. [13].
Taking into account the review of nutrient intake in nine European countries by Mensink et al. [47], for magnesium and considering children aged 1–3 years, the lowest mean intake was observed in the U.K. (154 mg/day) and the highest in Belgium (191 mg/day). For children aged 4–10 years, mean intakes ranged from 185 mg/day for girls in the U.K. to 290 mg/day for German boys [47]; therefore, the intake found in the EsNuPI study would be within the extremes mentioned by these authors.
The percentage of children aged 6 to <10 years who exceeded the AI was low. This situation was similar (although somewhat better) to that mentioned by Tornaritis et al. [52], who found a high prevalence of inadequacy in magnesium intake (85.0–89.9%) in children aged 9–13.9 years.
Higher income (i.e., a family income of >2000 €/month) was associated with higher magnesium intake, which coincides with studies which have indicated that children with a lower socioeconomic level have lower magnesium intakes [58,59].
4.5. Vitamin D
Intake of vitamin D was similar to or higher than that found in other studies [4,12,13,20,22,60], especially when we consider the AMS children. Chouraqui et al. [45] indicated that the intake was much higher in children (12–35 months) consuming young-child formula than in those not consuming such products. Similarly, in the present study, vitamin D intake was significantly higher in AMS children than in RS (Table 2), and membership to the AMS group was associated with a greater possibility of having a vitamin D intake that exceeded the median intake for this vitamin.
The intake of vitamin D in the present study, especially considering children in the AMS group, was higher than that found by Mensink et al. [47], who found intakes ranging from 1.3 µg/day (for Poland) to 2.3 µg/day (for Belgium) in children aged 1–3 years. For girls aged 4–10 years, mean intake ranged from 1.6 µg/day (for Spain and Germany) to 2.9 µg/day (for The Netherlands; age 7–10 years). For boys aged 4–10 years, mean intake ranged from 1.9 µg/day (for Spain, France, Germany and the UK) to 3.5 µg/day (for the Netherlands; age 7–10 years).
As indicated by other authors [4,12,13,20,22,47,61,62], the situation regarding vitamin D is very worrying, as almost all children did not achieve AI (Table 2). Vitamin D plays an important role in bone health and has been related to many other sanitary and functional benefits; thus improving its intake is a priority [63].
Whereas it is difficult to achieve AI for vitamin D, the use of fortified foods (i.e., dairy and cereals) may be helpful as, although vitamin D is synthesized in the skin by the action of ultraviolet light, data from across the world indicate that hypovitaminosis D is widespread and is considered a public health problem. Deficiency of vitamin D has been reported in some selected Spanish populations, due to insufficient intake, sedentary lifestyles with low sun exposure, and use of sunscreen lotions [47,64].
4.6. Nutrient Sources
In order to improve the situation of children, in relation to calcium, phosphorus, magnesium, and vitamin D intake, it is useful to know the food source of the nutrients under study.
Regarding the sources of nutrients in other studies, it should be noted that these differ from one study to another, reflecting the differences in the usual dietary patterns as well as the different fortification policies of each country. In addition, it should be noted that the classification of foods may be different in each study. All of these factors make it difficult to compare data from the different studies.
However, both in EsNuPI and in other studies, milk and dairy products were the main source of all the nutrients studied, especially for calcium [12,14,24,42,61,65,66,67,68]. In fact, it was found that drinking two or more feeding bottles or glasses of milk a day is a factor that helps to achieve calcium and vitamin D intake above the median. However, despite being the main source of various nutrients, the consumption of milk and dairy products has decreased in children in recent decades and in many countries, contributing to many children not complying with the AR/AI of various nutrients [24]. In the EsNuPI Study, the milk consumed in the AMS group includes fortified and adapted formulas whose composition is adapted, being usually enriched with vitamin D in contrast to standard milk. This was reflected in the intakes of vitamin D in AMS children that were higher than those in RS children, although the intakes remained below the AI in most children. Similarly, Chouraqui et al. [45] noted that the consumption of young-children formulas may help infants and children (1–3 years) which are at risk of nutrient deficiencies, in order to meet their nutritional requirements. Furthermore, Huybrechts et al. [65] concluded that the consumption of fortified (growth) milk in children could be recommended to increase children’s vitamin D intake.
As a source of calcium, dairy products were followed by other dairy products (including dairy desserts, flavored milk, ice cream, cream, and condensed milk). It is difficult to compare these results with those of other studies, as the foods are not always grouped the same. For example, sweetened milk drinks were the second dietary source of calcium in Flemish preschoolers [65], contributing 22.8% to calcium intake—almost as much as milk. According to ESPGHAN recommendations [69], the intake of free sugars should be reduced and minimized, with a desirable goal of <5% energy intake in children and adolescents aged from 2–18 years, and their intake should probably be even lower in infants and toddlers under 2 years.
In addition, cereals are an important source of magnesium and vitamin D. The importance of consumption of grains and enriched breakfast cereals with various nutrients has been associated with increased magnesium intake in children [70], and analyzing the average American diet, Hess et al. (2019) pointed out that grains were the least expensive source of magnesium [57]. In addition, fortified breakfast cereals are one of the main sources of vitamin D and other nutrients [61].
Taking these data into account, it is desirable to approximate the consumption of dairy products and cereals to the recommended consumption.
Finally, it is noteworthy that, in children who did not take adapted formulas (RS), fish and eggs were good sources of vitamin D. Both fish [65] and eggs [71] have been found to be good sources of vitamin D in children. Although these foods are the first source of vitamin D in the present study, it is possible that children may not be meeting the recommended amounts of these foods. Therefore, adequate consumption of these two food groups should be considered and improved as early as childhood. In addition, the consumption of enriched foods or beverages with vitamin D could improve the intake of this vitamin. In AMS children, the intake of vitamin D was higher than in the RS, due to the contribution of fortified dairy products; however, their intake situation has room for improvement.
4.7. Strengths and Limitations
One of the main strengths of this study is being representative of the sample of children aged 1 to <10 years, as this is a group that has been little studied. Furthermore, it provides very recent information and analyzes the differences between the intakes of the nutrients studied between children in the reference sample and in the adapted milk consumers’ sample. Although dietary surveys are prone to underestimating dietary intake, which influences the estimation of the percentage of inadequate nutrient intakes, we have analyzed the degree of misreporting of the population in our study, analyzing separately the data from those children with plausible reports. On the other hand, the use of only two dietary recalls does not adequately reflect an individual’s usual intake. In our study, the observed nutrient intakes were transformed into usual intakes using the Nusser method [41], which allowed for a better estimation of the distribution of nutrient intakes and of the percentage of intakes lower than AR.
As for the limitations of the EsNuPI study, it can be noted that it had a cross-sectional design, which allows to know the situation at that time without establishing a causal relationship between nutrient intake with the bone health of children; therefore, the deepening of this topic should be the subject of future research. Additionally, it analyzed only populations from urban areas, not considering rural areas.
5. Conclusions
The usual nutrient intakes in the EsNuPI study met or exceeded their requirements, except for those of vitamin D. It is worth considering the percentage of children who did not achieve AR for calcium and AI for magnesium, from which it can be said that the situation in nutrients involved in bone health and other health aspects is clearly improvable, with the situation in AMS children being more favorable than in RS; although the situation in AMS children should also still be improved, as it is far from optimal.
When analyzing the sources of calcium, magnesium, phosphorus, and vitamin D, milk and dairy products were the first sources, in all cases, in this representative sample of Spanish children from 1 to <10 years. However, despite being the main source of various nutrients, the consumption of milk and dairy products has decreased in children in recent decades and in many countries, contributing to many children not complying with the AR/AI of various nutrients [24]. Based on the present study, adapted milk could be an effective strategy for overcoming the deficiencies of micronutrients (especially vitamin D in children) which are involved in important biological roles in the body, especially in bone health [4,12,14,20,45,46,47,72].
Considering that the calcium and magnesium intakes were below the AR/AI in a significant percentage of children, that phosphorus exceeded the AI in 100% of individuals, and that vitamin D was found, in practically all those studied, to be below the AI, it seems appropriate to improve the situation of these nutrients, which are involved in bone health. The AMS group appears to be in somewhat better shape than the RS, but still needs further improvement. Of special interest are the results of vitamin D intakes: although still below the AI, they were significantly higher in the AMS group, independent of the age of children.
Acknowledgments
The authors would like to thank IPN for its support and technical advice.
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6643/12/6/1787/s1, Table S1: daily calcium, phosphorus, magnesium, and vitamin D usual intakes by sex and age group in the EsNuPI Study population. Results of plausible reporters. Table S2: percentage of the 18 food groups sources, in terms of the total calcium intake (in %), among Spanish Pediatric Population (EsNuPI) study by age group, in both the reference and the adapted milk consumer samples (n = 1448). Table S3: percentage of the 18 food groups sources, in terms of the total phosphorus intake (in %), among Spanish Pediatric Population (EsNuPI) study by age group, in both the reference and the adapted milk consumer samples (n = 1448). Table S4: percentage of the 18 food groups sources, in terms of the total magnesium intake (in %), among Spanish Pediatric Population (EsNuPI) study by age group, in both the reference and the adapted milk consumer samples (n = 1448). Table S5: percentage of the 18 food groups sources, in terms of the total Vitamin D intake (in %), among Spanish Pediatric Population (EsNuPI) study by age group, in both the reference and the adapted milk consumer samples (n = 1448).
Author Contributions
Methodology, M.J.S.-M., T.V., Á.H.-R., G.V.-M. and Á.G.; investigation, M.J.S.-M., T.V., Á.H.-R., G.V.-M. and Á.G.; writing—original draft preparation, E.C.-S., A.M.L.-S., A.I.J.-O., L.M.B., A.A.; R.M.O.; writing—review and editing, E.C.-S., A.M.L.-S., A.I.J.-O., A.A., L.M.B., R.M.O., M.J.S.-M., T.V., Á.H.-R., F.L.-V., R.L., J.M.M., E.M.d.V., M.D.R.-L., G.V.-M. and Á.G.; supervision, F.L.V., R.L., J.M.M., E.M.d.V., R.M.O., M.D.R.-L., G.V.-M. and Á.G.; project administration, G.V.-M. and Á.G.; funding acquisition, G.V.-M. and Á.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Instituto Puleva de Nutrición (IPN).
Conflicts of Interest
The funding sponsor had no role in the design of the study; in the collection, analyses, or interpretation of the data; in the writing of the manuscript, and in the decision to publish the results. The authors declare no conflicts of interest, with the exception of Federico Lara who is a member of the IPN
References
- 1.US Department of Health and Human Services and US Department of Agriculture 2015–2020 Dietary Guidelines for Americans. [(accessed on 14 June 2020)]; Available online: https://health.gov/dietaryguidelines/2015/guidelines/
- 2.Cashman K.D. Diet, Nutrition, and Bone Health. J. Nutr. 2007;137:2507S–2512S. doi: 10.1093/jn/137.11.2507S. [DOI] [PubMed] [Google Scholar]
- 3.Rizzoli R., Bianchi M.L., Garabédian M., McKay H.A., Moreno L.A. Maximizing bone mineral mass gain during growth for the prevention of fractures in the adolescents and the elderly. Bone. 2010;46:294–305. doi: 10.1016/j.bone.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Suárez Cortina L., Moreno Villares J.M., Martínez Suárez V., Aranceta Bartrina J., Dalmau Serra J., Gil Hernández A., Lama More R., Martín Mateos M.A., Pavón Belinchón P. Ingesta de calcio y densidad mineral ósea en una población de escolares españoles (estudio CADO) An. Pediatría. 2011;74:3–9. doi: 10.1016/j.anpedi.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Duren D.L., Sherwood R.J., Choh A.C., Czerwinski S.A., Cameron Chumlea W., Lee M., Sun S.S., Demerath E.W., Siervogel R.M., Towne B. Quantitative genetics of cortical bone mass in healthy 10-year-old children from the Fels Longitudinal Study. Bone. 2007;40:464–470. doi: 10.1016/j.bone.2006.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Julián-Almárcegui C., Gómez-Cabello A., Huybrechts I., González-Agüero A., Kaufman J.M., Casajús J.A., Vicente-Rodríguez G. Combined effects of interaction between physical activity and nutrition on bone health in children and adolescents: A systematic review. Nutr. Rev. 2015;73:127–139. doi: 10.1093/nutrit/nuu065. [DOI] [PubMed] [Google Scholar]
- 7.Moyer-Mileur L.J., Xie B., Ball S.D., Pratt T. Bone mass and density response to a 12-month trial of calcium and vitamin D supplement in preadolescent girls. J. Musculoskelet. Neuronal Interact. 2003;3:63–70. [PubMed] [Google Scholar]
- 8.de Lamas C., de Castro M.J., Gil-Campos M., Gil Á., Couce M.L., Leis R. Effects of Dairy Product Consumption on Height and Bone Mineral Content in Children: A Systematic Review of Controlled Trials. Adv. Nutr. 2019;10:S88–S96. doi: 10.1093/advances/nmy096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abrams S.A., Chen Z., Hawthorne K.M. Magnesium Metabolism in 4-Year-Old to 8-Year-Old Children. J. Bone Miner. Res. 2014;29:118–122. doi: 10.1002/jbmr.2021. [DOI] [PubMed] [Google Scholar]
- 10.Pérez-Llamas F., Zamora S. Calcio, fósforo, magnesio y flúor. In: Gil A., editor. Tratado de Nutrición, Vol. 1. Editorial Médica Panamericana; Madrid, Spain: 2017. pp. 481–507. [Google Scholar]
- 11.Gil Á., Plaza-Diaz J., Mesa M.D. Vitamin D: Classic and Novel Actions. Ann. Nutr. Metab. 2018;72:87–95. doi: 10.1159/000486536. [DOI] [PubMed] [Google Scholar]
- 12.Olza J., Aranceta-Bartrina J., González-Gross M., Ortega R., Serra-Majem L., Varela-Moreiras G., Gil Á. Reported Dietary Intake, Disparity between the Reported Consumption and the Level Needed for Adequacy and Food Sources of Calcium, Phosphorus, Magnesium and Vitamin D in the Spanish Population: Findings from the ANIBES Study †. Nutrients. 2017;9:168. doi: 10.3390/nu9020168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.López-Sobaler A.M., Aparicio A., González-Rodríguez L.G., Cuadrado-Soto E., Rubio J., Marcos V., Sanchidrián R., Santos S., Pérez-Farinós N., Dal Re M.Á., et al. Adequacy of Usual Vitamin and Mineral Intake in Spanish Children and Adolescents: ENALIA Study. Nutrients. 2017;9:131. doi: 10.3390/nu9020131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ortega R.M., López-Sobaler A.M., Jiménez Ortega A.I., Navia Lombán B., Ruiz-Roso Calvo de Mora B., Rodríguez-Rodríguez E., López Plaza B., Grupo de investigación no 920030 Food sources and average intake of calcium in a representative sample of Spanish schoolchildren. Nutr. Hosp. 2012;27:715–723. doi: 10.3305/nh.2012.27.3.5722. [DOI] [PubMed] [Google Scholar]
- 15.Partearroyo T., Samaniego-Vaesken M.d.L., Ruiz E., Varela-Moreiras G. Assessment of micronutrients intakes in the Spanish population: A review of the findings from the Anibes study. Nutr. Hosp. 2018;35:20–24. doi: 10.20960/nh.2282. [DOI] [PubMed] [Google Scholar]
- 16.Dalmau J., Peña-Quintana L., Moráis A., Martínez V., Varea V., Martínez M.J., Soler B. Quantitative analysis of nutrient intake in children under 3 years old. ALSALMA study. An. Pediatría. 2015;82:255–266. doi: 10.1016/j.anpedi.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 17.Huysentruyt K., Laire D., Van Avondt T., De Schepper J., Vandenplas Y. Energy and macronutrient intakes and adherence to dietary guidelines of infants and toddlers in Belgium. Eur. J. Nutr. 2016;55:1595–1604. doi: 10.1007/s00394-015-0978-y. [DOI] [PubMed] [Google Scholar]
- 18.Iglesia I., Intemann T., De Miguel-Etayo P., Pala V., Hebestreit A., Wolters M., Russo P., Veidebaum T., Papoutsou S., Nagy P., et al. Dairy Consumption at Snack Meal Occasions and the Overall Quality of Diet during Childhood. Prospective and Cross-Sectional Analyses from the IDEFICS/I.Family Cohort. Nutrients. 2020;12:642. doi: 10.3390/nu12030642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grimes C., Szymlek-Gay E., Campbell K., Nicklas T. Food Sources of Total Energy and Nutrients among U.S. Infants and Toddlers: National Health and Nutrition Examination Survey 2005–2012. Nutrients. 2015;7:6797–6836. doi: 10.3390/nu7085310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dalmau J., Moráis A., Martínez V., Peña-Quintana L., Varea V., Martínez M.J., Soler B. Evaluation of diet and nutrient intake in children under three years old. ALSALMA pilot study. An. Pediatría. 2014;81:22–31. doi: 10.1016/j.anpedi.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 21.Afshin A., Sur P.J., Fay K.A., Cornaby L., Ferrara G., Salama J.S., Mullany E.C., Abate K.H., Abbafati C., Abebe Z., et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393:1958–1972. doi: 10.1016/S0140-6736(19)30041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eussen S.R.B.M., Pean J., Olivier L., Delaere F., Lluch A. Theoretical Impact of Replacing Whole Cow’s Milk by Young-Child Formula on Nutrient Intakes of UK Young Children: Results of a Simulation Study. Ann. Nutr. Metab. 2015;67:247–256. doi: 10.1159/000440682. [DOI] [PubMed] [Google Scholar]
- 23.Srbely V., Janjua I., Buchholz A., Newton G. Interventions Aimed at Increasing Dairy and/or Calcium Consumption of Preschool-Aged Children: A Systematic Literature Review. Nutrients. 2019;11:714. doi: 10.3390/nu11040714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dror D.K., Allen L.H. Dairy product intake in children and adolescents in developed countries: Trends, nutritional contribution, and a review of association with health outcomes. Nutr. Rev. 2014;72:68–81. doi: 10.1111/nure.12078. [DOI] [PubMed] [Google Scholar]
- 25.Santaliestra-Pasías A.M., González-Gil E.M., Pala V., Intemann T., Hebestreit A., Russo P., Van Aart C., Rise P., Veidebaum T., Molnar D., et al. Predictive associations between lifestyle behaviours and dairy consumption: The IDEFICS study. Nutr. Metab. Cardiovasc. Dis. 2020;30:514–522. doi: 10.1016/j.numecd.2019.10.006. [DOI] [PubMed] [Google Scholar]
- 26.Madrigal C., Soto-Méndez M.J., Hernández-Ruiz Á., Ruiz E., Valero T., Ávila J.M., Lara-Villoslada F., Leis R., Martínez de Victoria E., Moreno J.M., et al. Dietary and Lifestyle Patterns in the Spanish Pediatric Population (One to <10 Years Old): Design, Protocol, and Methodology of the EsNuPI Study. Nutrients. 2019;11:3050. doi: 10.3390/nu11123050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Madrigal C., Soto-Méndez M.J., Hernández-Ruiz Á., Valero T., Ávila J.M., Ruiz E., Lara Villoslada F., Leis R., Martínez de Victoria E., Moreno J.M., et al. Energy Intake, Macronutrient Profile and Food Sources of Spanish Children Aged One to <10 Years—Results from the EsNuPI Study †. Nutrients. 2020;12:893. doi: 10.3390/nu12040893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization The WHO Child Growth Standards. [(accessed on 14 June 2020)]; Available online: http://www.who.int/childgrowth/en.
- 29.De Onis M. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007;85:660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Camargo D.M., Santisteban S., Paredes E., Flórez M., Bueno D.A. Confiabilidad de un cuestionario para medir actividad física y comportamientos sedentarios en niños desde preescolar a cuarto grado de primaria. Biomédica. 2015;35:347–356. doi: 10.7705/biomedica.v35i3.2502. [DOI] [PubMed] [Google Scholar]
- 31.Moreiras O., Carbajal A., Cabrera L. Ingestas Diarias Recomendadas de Energía y Nutrientes Para la Población Española. Tablas de Composición de Alimentos. 19th ed. Ediciones Pirámide (Grupo Anaya, SA); Madrid, Spain: 2018. [Google Scholar]
- 32.Fundación Española de la Nutrición (FEN) Software VD-FEN 2.1 Programa de Valoración Dietética de la FEN. Fundación Española de la Nutrición (FEN); Madrid, Spain: 2013. [Google Scholar]
- 33.Ruiz-López M., Martínez de Victoria E., Gil A. Guía Fotográfica de Porciones de Alimentos Consumidos en España. Fundación Iberoamericana de Nutrición; Granada, Spain: 2019. [Google Scholar]
- 34.Ocké M., de Boer E., Brants H., van der Laan J., Niekerk M., van Rossum C., Temme L., Freisling H., Nicolas G., Casagrande C., et al. PANCAKE–Pilot study for the Assessment of Nutrient intake and food Consumption Among Kids in Europe. EFSA Support. Publ. 2012;9:339E. doi: 10.2903/sp.efsa.2012.EN-339. [DOI] [Google Scholar]
- 35.European Food Safety Authority (EFSA) Dietary Reference Values for the European Union. [(accessed on 14 June 2020)]; Available online: https://www.efsa.europa.eu/en/topics/topic/dietary-reference-values.
- 36.Krebs-Smith S.M., Kott P.S., Guenther P.M. Mean proportion and population proportion: Two answers to the same question? J. Am. Diet. Assoc. 1989;89:671–676. [PubMed] [Google Scholar]
- 37.Börnhorst C., Huybrechts I., Ahrens W., Eiben G., Michels N., Pala V., Molnár D., Russo P., Barba G., Bel-Serrat S., et al. Prevalence and determinants of misreporting among European children in proxy-reported 24 h dietary recalls. Br. J. Nutr. 2013;109:1257–1265. doi: 10.1017/S0007114512003194. [DOI] [PubMed] [Google Scholar]
- 38.Schofield W.N. Predicting basal metabolic rate, new standards and review of previous work. Hum. Nutr. Clin. Nutr. 1985;39:5–41. [PubMed] [Google Scholar]
- 39.European Food Safety Authority (EFSA) Guidance on the EU Menu methodology. EFSA J. 2014;12:3944. [Google Scholar]
- 40.Serra-Majem L., Ribas-Barba L., Pérez-Rodrigo C., Bartrina J.A. Nutrient adequacy in Spanish children and adolescents. Br. J. Nutr. 2006;96:S49–S57. doi: 10.1079/BJN20061701. [DOI] [PubMed] [Google Scholar]
- 41.Nusser S.M., Carriquiry A.L., Dodd K.W., Fuller W.A. A Semiparametric Transformation Approach to Estimating Usual Daily Intake Distributions. J. Am. Stat. Assoc. 1996;91:1440–1449. doi: 10.1080/01621459.1996.10476712. [DOI] [Google Scholar]
- 42.López-Sobaler A.M., Aparicio A., Rubio J., Marcos V., Sanchidrián R., Santos S., Pérez-Farinós N., Dal-Re M.Á., Villar-Villalba C., Yusta-Boyo M.J., et al. Adequacy of usual macronutrient intake and macronutrient distribution in children and adolescents in Spain: A National Dietary Survey on the Child and Adolescent Population, ENALIA 2013–2014. Eur. J. Nutr. 2019;58:705–719. doi: 10.1007/s00394-018-1676-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Agencia Española de Consumo Seguridad Alimentaria y Nutrición . Estudio ALADINO 2015: Estudio de Vigilancia del Crecimiento, Alimentación, Actividad Física, Desarrollo Infantil y Obesidad en España. Ministerio de Sanidad, Servicios Sociales e Igualdad; Madrid, Spain: 2016. [Google Scholar]
- 44.Pérez-Farinós N., López-Sobaler A.M., Dal Re M.Á., Villar C., Labrado E., Robledo T., Ortega R.M. The ALADINO Study: A National Study of Prevalence of Overweight and Obesity in Spanish Children in 2011. Biomed Res. Int. 2013;2013:163687. doi: 10.1155/2013/163687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chouraqui J.-P., Turck D., Tavoularis G., Ferry C., Dupont C. The Role of Young Child Formula in Ensuring a Balanced Diet in Young Children (1–3 Years Old) Nutrients. 2019;11:2213. doi: 10.3390/nu11092213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jiménez-Aguilar A., González Castell D., Flores-Aldana M., Mundo-Rosas V., Hernández-Cordero S., García-Feregrino R. Dietary intake and adequacy in Mexican preschool children: National Health and Nutrition Survey 2012. Nutr. Hosp. 2018;35:1186. doi: 10.20960/nh.1843. [DOI] [PubMed] [Google Scholar]
- 47.Mensink G.B.M., Fletcher R., Gurinovic M., Huybrechts I., Lafay L., Serra-Majem L., Szponar L., Tetens I., Verkaik-Kloosterman J., Baka A., et al. Mapping low intake of micronutrients across Europe. Br. J. Nutr. 2013;110:755–773. doi: 10.1017/S000711451200565X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zimmer M.C., Rubio V., Kintziger K.W., Barroso C. Racial/Ethnic Disparities in Dietary Intake of U.S. Children Participating in WIC. Nutrients. 2019;11:2607. doi: 10.3390/nu11112607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rubio-López N., Llopis-González A., Morales-Suárez-Varela M. Calcium Intake and Nutritional Adequacy in Spanish Children: The ANIVA Study. Nutrients. 2017;9:170. doi: 10.3390/nu9020170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hojsak I., Bronsky J., Campoy C., Domellöf M., Embleton N., Fidler Mis N., Hulst J., Indrio F., Lapillonne A., Mølgaard C., et al. Young Child Formula. J. Pediatr. Gastroenterol. Nutr. 2018;66:177–185. doi: 10.1097/MPG.0000000000001821. [DOI] [PubMed] [Google Scholar]
- 51.Salamoun M.M., Kizirian A.S., Tannous R.I., Nabulsi M.M., Choucair M.K., Deeb M.E., El-Hajj Fuleihan G.A. Low calcium and vitamin D intake in healthy children and adolescents and their correlates. Eur. J. Clin. Nutr. 2005;59:177–184. doi: 10.1038/sj.ejcn.1602056. [DOI] [PubMed] [Google Scholar]
- 52.Tornaritis M.J., Philippou E., Hadjigeorgiou C., Kourides Y.A., Panayi A., Savva S.C. A study of the dietary intake of Cypriot children and adolescents aged 6-18 years and the association of mother’s educational status and children’s weight status on adherence to nutritional recommendations. BMC Public Health. 2014;14:13. doi: 10.1186/1471-2458-14-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Elmadfa I., Meyer A., Nowak V., Hasenegger V., Putz P., Verstraeten R., Remaut-DeWinter A A.M., Kolsteren P., Dostálová J., Dlouhý P., et al. European Nutrition and Health Report 2009. Volume 61. Forum of nutrition; Basel, Switzerland: 2009. [DOI] [PubMed] [Google Scholar]
- 54.Loughrill E., Wray D., Christides T., Zand N. Calcium to phosphorus ratio, essential elements and vitamin D content of infant foods in the UK: Possible implications for bone health. Matern. Child Nutr. 2017;13:e12368. doi: 10.1111/mcn.12368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kostecka M. Frequency of consumption of foods rich in calcium and vitamin D among school-age children. Rocz. Panstw. Zakl. Hig. 2016;67:23–30. [PubMed] [Google Scholar]
- 56.Lee K.-J., Kim K.-S., Kim H.-N., Seo J.-A., Song S.-W. Association between dietary calcium and phosphorus intakes, dietary calcium/phosphorus ratio and bone mass in the Korean population. Nutr. J. 2014;13:114. doi: 10.1186/1475-2891-13-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vorland C.J., Stremke E.R., Moorthi R.N., Hill Gallant K.M. Effects of Excessive Dietary Phosphorus Intake on Bone Health. Curr. Osteoporos. Rep. 2017;15:473–482. doi: 10.1007/s11914-017-0398-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Horikawa C., Murayama N., Ishida H., Yamamoto T., Hazano S., Nakanishi A., Arai Y., Nozue M., Yoshioka Y., Saito S., et al. Association between parents’ work hours and nutrient inadequacy in Japanese schoolchildren on weekdays and weekends. Nutrition. 2020;70:110598. doi: 10.1016/j.nut.2019.110598. [DOI] [PubMed] [Google Scholar]
- 59.Gwynn J.D., Flood V.M., D’Este C.A., Attia J.R., Turner N., Cochrane J., Louie J.C.-Y., Wiggers J.H. Poor food and nutrient intake among Indigenous and non-Indigenous rural Australian children. BMC Pediatr. 2012;12:12. doi: 10.1186/1471-2431-12-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Verduci E., Banderali G., Montanari C., Berni Canani R., Cimmino Caserta L., Corsello G., Mosca F., Piazzolla R., Rescigno M., Terracciano L., et al. Childhood Dietary Intake in Italy: The Epidemiological “MY FOOD DIARY” Survey. Nutrients. 2019;11:1129. doi: 10.3390/nu11051129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cribb V.L., Northstone K., Hopkins D., Emmett P.M. Sources of vitamin D and calcium in the diets of preschool children in the UK and the theoretical effect of food fortification. J. Hum. Nutr. Diet. 2015;28:583–592. doi: 10.1111/jhn.12277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ahluwalia N., Herrick K.A., Rossen L.M., Rhodes D., Kit B., Moshfegh A., Dodd K.W. Usual nutrient intakes of US infants and toddlers generally meet or exceed Dietary Reference Intakes: Findings from NHANES 2009–2012. Am. J. Clin. Nutr. 2016;104:1167–1174. doi: 10.3945/ajcn.116.137752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Damsgaard C.T. Can vitamin D supplementation improve childhood cardiometabolic status?—data from 2 randomized trials. Am. J. Clin. Nutr. 2020;111:737–738. doi: 10.1093/ajcn/nqaa021. [DOI] [PubMed] [Google Scholar]
- 64.Holick M.F., Binkley N.C., Bischoff-Ferrari H.A., Gordon C.M., Hanley D.A., Heaney R.P., Murad M.H., Weaver C.M. Evaluation, Treatment, and Prevention of Vitamin D Deficiency: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2011;96:1911–1930. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 65.Huybrechts I., Lin Y., De Keyzer W., Sioen I., Mouratidou T., Moreno L.A., Slimani N., Jenab M., Vandevijvere S., De Backer G., et al. Dietary sources and sociodemographic and economic factors affecting vitamin D and calcium intakes in Flemish preschoolers. Eur. J. Clin. Nutr. 2011;65:1039–1047. doi: 10.1038/ejcn.2011.71. [DOI] [PubMed] [Google Scholar]
- 66.Omidvar N., Neyestani Tirang R., Hajifaraji M., Eshraghian M.-R., Rezazadeh A., Armin S., Haidari H., Zowghi T. Calcium Intake, Major Dietary Sources and Bone Health Indicators in Iranian Primary School Children. Iran. J. Pediatr. 2015;25 doi: 10.5812/ijp.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Murphy M.M., Douglass J.S., Johnson R.K., Spence L.A. Drinking Flavored or Plain Milk Is Positively Associated with Nutrient Intake and Is Not Associated with Adverse Effects on Weight Status in US Children and Adolescents. J. Am. Diet. Assoc. 2008;108:631–639. doi: 10.1016/j.jada.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 68.Eloranta A.-M., Venäläinen T., Soininen S., Jalkanen H., Kiiskinen S., Schwab U., Lakka T.A., Lindi V. Food sources of energy and nutrients in Finnish girls and boys 6–8 years of age–the PANIC study. Food Nutr. Res. 2016;60:32444. doi: 10.3402/fnr.v60.32444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fidler Mis N., Braegger C., Bronsky J., Campoy C., Domellöf M., Embleton N.D., Hojsak I., Hulst J., Indrio F., Lapillonne A., et al. Sugar in Infants, Children and Adolescents. J. Pediatr. Gastroenterol. Nutr. 2017;65:681–696. doi: 10.1097/MPG.0000000000001733. [DOI] [PubMed] [Google Scholar]
- 70.Sette S., D’Addezio L., Piccinelli R., Hopkins S., Le Donne C., Ferrari M., Mistura L., Turrini A. Intakes of whole grain in an Italian sample of children, adolescents and adults. Eur. J. Nutr. 2017;56:521–533. doi: 10.1007/s00394-015-1097-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bischofova S., Dofkova M., Blahova J., Kavrik R., Nevrla J., Rehurkova I., Ruprich J. Dietary Intake of Vitamin D in the Czech Population: A Comparison with Dietary Reference Values, Main Food Sources Identified by a Total Diet Study. Nutrients. 2018;10:1452. doi: 10.3390/nu10101452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Moe S.M. Disorders Involving Calcium, Phosphorus, and Magnesium. Prim. Care Clin. Off. Pract. 2008;35:215–237. doi: 10.1016/j.pop.2008.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.