Abstract
Background
The proportion of older citizens is increasing worldwide. A well-known syndrome in old age is physical frailty which is associated with a greater risk of disabilities in activities of daily living, greater reliance on in-home services, hospitalization, institutionalization, and premature mortality. The purpose of this study is to determine the effects of an intervention with high-protein diet alone or in combination with power training in pre-frail and frail old adults.
Methods
The study is a community-based assessor-blinded parallel randomized controlled trial (RCT), consisting of two phases. Phase 1 is a 1-month stabilization phase, where self-reliant community-dwelling adults + 80 years old will receive individual guidance regarding protein intake, to prevent the risk of negative protein balance prior to phase 2 and to only include participants who have reached the minimum recommended level of protein intake (1.0 g/kg/day) in the randomized controlled trial. Phase 2 is a 4-month RCT where 150 participants will be randomized into the following three arms: protein-only where participants will be provided with dairy products to increase their protein intake to 1.5 g/kg/day, protein + exercise where participants will be provided with the protein intervention in combination with power training two times a week, and recommendation group where participants will continue as in phase 1. Primary outcome is lower leg muscle power. Secondary outcomes include physical function and mobility, frailty status, muscle mechanical function, body composition, nutritional status, and health-related quality of life. The statistical analysis will include an intention-to-treat analysis of all randomized participant and per-protocol analysis of all compliant participants. The study hypothesis will be tested with mixed linear models to assess changes in the main outcomes over time and between study arms.
Discussion
The finding of this study may add to the knowledge about the beneficial effects of high-protein diet from dairy products combined with power training to counteract frailty in community-dwelling older adults. This may ultimately have an impact on the ability to live well and independent for longer.
Trial registration
ClinicalTrials.gov NCT03842579. Registered on 15 February 2019, version 1
Keywords: Frailty, Aging, High-protein diet, Protein supplementation, Resistance training, Strength training, Muscle power, Muscle strength, Muscle mass, Functional performance, Nutritional status
Background
The proportion of older citizens aged + 80 years old is increasing in the western population at faster rate than any other age group [1]. In Denmark, projections indicate that this group will represent 10% of the total population in 2060 from the current 4.4% [2].
Older age has been associated with greater prevalence of physical frailty a complex syndrome with multiple causes [3] characterized by reduced physiologic reserve and increased vulnerability to external and internal stressors [4]. The SHARE-FI75+ screening tool is specifically developed for + 75 years community-dwelling adults and operationalize non-frail, pre-frail, or frail condition by considering age, gender, and the presence of fatigue, low appetite, weakness, slowness, and low physical activity [5]. The prevalence of pre-frail and frail syndrome has been recently estimated as high as 43% between the age of 65 and 73 years using a slightly different screening tool earlier developed by Fried and colleagues [6], but data on the + 80 years old is still limited.
Physical frailty has been associated with greater risk of disabilities in basic and instrumental activities of daily living, chronic illnesses, loneliness, psychological distress, poorer self-reported quality of life, and premature mortality [7]. In addition, physical frail individuals have greater reliance on in-home services, risk for hospitalization, institutionalization, and overall greater health care cost [6, 8–11]. Hence, physical frailty has important implications for the individual older citizen as well as for the health care system.
One of the key determinants of this syndrome is the excessive loss of muscle mass which is strongly associated with the modifiable lifestyle factors, dietary protein intake and exercise [12, 13], both recognized as anabolic agents pivotal for primary, secondary, and tertiary prevention of physical frailty [14].
Specifically, diets high in protein are associated with a reduced risk of frailty [13]. Milk proteins are high-quality proteins with a high content of the amino acid leucine, known to effectively stimulate muscle protein synthesis [15, 16]. The current recommendation of total protein intake for older adults is minimum 1.0 g protein/kg/day based on European recommendations [12, 17], but it has been suggested that older adults, and especially frail older adults, can benefit from an even higher protein intake of 1.5 g protein/kg/day [18–20]. However, there is growing evidence that a large proportion of the older adults do not meet the recommendations for protein intake, e.g., due to anorexia of aging, medical conditions, and physical and mental limitations [12, 21, 22].
Exercise interventions focusing on strength and resistance training have been consistently shown to counteract the age-related decline of muscle function (e.g., muscle strength), physical function (e.g., walking speed) and disability among older adults [23, 24]. In addition, muscle power (the product of force times velocity) has been earlier considered a critical determinant to maintain function and independence in older age and exercise interventions targeting muscle power may play a key role in counteracting frail and pre-frail condition [25–27]. Several systematic reviews have investigated the beneficial effect of combining protein and exercise, but only one have examined the beneficial effect of protein alone [28] and none of the studies included in this review have used off-the-shelf dairy products or exercise interventions designed with muscle power components. Furthermore, it is unclear whether the combination of exercise and nutrition may be superior to the single interventions to improve physical performance in pre-frail and frail older adults as highlighted in a recent systematic review [29]. Possibly, the heterogeneity of the interventions (self-administered or supervised exercise programs, nutritional interventions range from supplements of selected micronutrients to protein supplementation from 10 to 30 g/day), duration, and settings (primary vs. secondary care settings) may have contributed to such unclear results [29]. Optimizing protein intake before initiating exercise may be essential for older adults who are not in protein balance to prevent the risk of an accelerated loss of muscle mass [30]. According to our knowledge, the benefit of optimizing protein intake before exercise interventions has not been examined before.
Therefore, the aims in this two phased parallel RCT is to investigate in pre-frail and frail older adults whether:
-
A.
An increased protein intake from dairy products combined with power training increases (i) muscle power, and (ii) muscle mechanical function, maximal muscle strength, physical function, mobility, physical activity, muscle mass, health-related quality of life, and activities of daily living (iii) decrease pain, fear of falling, sedentary behavior, risk of malnutrition and (iv) modify physical frailty status and causes and contributors associated with such status.
-
B.
Protein and power training in combination has a superior effect compared to an increased protein intake from dairy products alone and to a third intervention based on current recommendations on diet and physical activity for older adults.
Methods
Study design
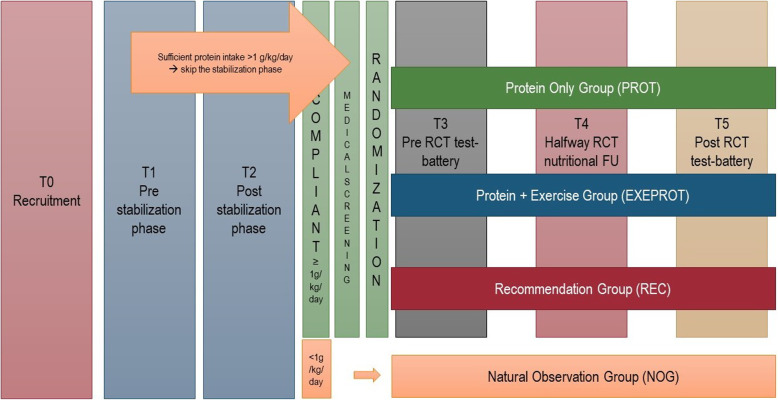
A 2-phase community-based assessor-blinded parallel RCT will be undertaken, to determine the effects of interventions with off-the-shelf dairy products alone or in combination with progressive power training, see Fig. 1.
Fig. 1.
Flow-chart of the phases in the study (stabilization and intervention phases). RCT, randomized controlled trial; FU, follow-up; T, test session; g/kg/day, refers to g of protein/kg/day
Study procedure
Inclusion criteria for participants
Participants are required to be (1) community-dwelling older adults + 80 years old; (2) pre-frail or frail, evaluated by SHARE-FI75+ [5]; (3) intact cognitive function, evaluated by a score ≥ 4 in the short form of the Mini-Mental State Evaluation (MMSE) [31, 32]; (4) medically stable as evaluated by medical screening (see details below); (5) able to participate in group-based exercise without need for transportation or individual exercise sessions; (6) signed informed consent; (7) able to speak and read Danish; (8) not allergic/intolerant to milk-products/protein; and (9) not on a weight losing diet.
Exclusion criteria for participants
Participants are excluded if they are not medical stable, including (1) eGFR < 40 ml/min/1.73 m2; (2) have received cancer treatment during the preceding 6 months; (3) received high doses of prednisolone and/or morphine, evaluated by medical doctor; and (4) have other medical issues that may affect the study.
Procedure for recruitment
Participants will be recruited through 3 pathways:
Nationally regulated preventive home visits service managed by the municipality, as earlier reported in [33]. Community-dwelling adults ≥ 80 years who are self-reliant in activities of daily living are offered a home visit by health-care personnel at least once a year. During the home visit, the older citizens will be informed about the study. As part of the preventive initiatives, the municipality may also invite groups of older citizens to presentations on selected health topics. When related to physical function, nutrition, or exercise, the I’m still standing study will also be presented.
Existing cohort of community-dwelling older citizens (the Healthy Aging Network of Competence in Southern Denmark - Northern Schleswig-Holstein, HANC-study [33, 34]). All former participants will receive an invitation letter to the I’m still standing project.
Advertisements in newspapers, on webpages, and social medias and presentations about the project at arrangements targeting older adults. All advertisements will be performed in close collaboration between the University of Southern Denmark and the Municipality of Odense targeting community-dwelling adults + 80 years and their relatives or health care personnel in primary prevention.
Recruitment to the project via all pathways is performed in collaboration with the municipality of Odense. The health care personnel will perform the screening for inclusion criteria (apart from the medical screening) and obtain informed consent from eligible participants.
Phase 1: Stabilization phase—1-month nutritional recommendation
The aim of the stabilization phase (phase 1) is to ensure that participants enrolled in the intervention (phase 2) will have a minimum daily protein intake according to the European recommendation, ≥ 1.0 g/kg/day [12] to prevent the risk of negative protein balance.
Risk of protein malnutrition in this phase will be first operationalized by the Protein Screener (Pro55+) [35] administered during the first home visit. The Protein Screener classifies participants according to the probability of being protein malnourished, with a probability above 30% considered as cutoff point for insufficient intake of protein. Different scenarios may occur during this phase:
Participants classified to have high probability of protein malnutrition (> 30%) by the Pro55+ will be individually guided to improve their intake of protein and receive publicly available material regarding nutritional guidelines specifically developed for older adults. One month later, participants will be asked to fill out a 4-day food record (three weekdays and 1 day during the weekend) to evaluate if the minimum requirement for daily protein intake is met.
Participants classified to have a low probability of protein malnutrition (≤ 30%) by the Pro55+ will be immediately asked to fill out a 4-day food record (three weekdays and 1 day during the weekend). This step is to confirm that the average protein intake is ≥ 1.0 g/kg/day. If the 4-day food records indicate a protein intake below 1.0 g/kg/day, participants will be enrolled in the stabilization phase and an additional 4-day food records will be collected after 1 month.
Participants with a minimum intake of 1.0 g protein/kg/day will be invited to the medical screening. Participants not meeting the recommended protein intake after the stabilization phase will be followed as “natural observation group” but will not be considered for statistical purposes. They will receive two seminars on specific topics related to healthy aging and be asked to fill out self-reported questionnaires (at baseline and after 4 months) including demographic data, chronic diseases, activities of daily living, quality of life, appetite, nutritional status, sedentary behavior, function, pain and depression. Semi-structured interviews to identify potential barriers for not meeting the recommended level of daily protein intake will be conducted on a sub-group. The phases in the study are illustrated in Fig. 1.
Medical screening
The medical screening will be performed by a physician and will include blood pressure, auscultation of heart and lungs, blood sample, and an evaluation of medical history. Participants will be asked to bring their medications and direct count of name and dose will be performed. Medical stable is defined as no kidney diseases and eGFR ≥ 40 ml/min/1.73 m2, no cancer treatment within the last 6 months, no high doses of prednisolone and/or morphine, and no other medical issues that may affect the study.
Phase 2: Four months randomized controlled intervention
Eligible participants will be randomized into three groups: (i) protein-only group (PROT), (ii) protein + exercise group (EXEPROT), and (iii) recommendation group (REC).
PROT intervention
The PROT group will receive protein-rich off-the-shelf dairy products with the aim of targeting a daily protein intake of 1.5 g protein/kg/day. At baseline, individual supplementation plans are made based on information about participants habitual protein intake (assessed by the food records) and taste preferences. A cutoff of 15 g of supplementary protein is used—if participants have a higher requirement for protein, there will be a stepwise increase in protein intake over the first 4 weeks. Examples of products are skimmed milk, low-fat yoghurts with a high protein content (skyr), chocolate milk, cottage cheese, and ordinary low-fat cheese. Products will be delivered once a week at the home of the participant or at the training facilities. The type of products consumed may be changed throughout the study in order to avoid sensory-specific satiety and keep the compliance high. The PROT intervention is performed by specifically trained nutritional specialists.
-
2.
EXEPROT intervention
The EXEPROT group will receive the same protein intervention as the PROT group combined with exercise program 1 h, twice a week. The exercise is designed as power training incorporating lower and upper body exercises with a training intensity of 65–80% of 1 repetition maximum (3 sets of 10–12 repetitions), which will be progressively adjusted throughout the entire intervention. Exercises will be performed explosively (i.e., as rapid as possible) during the concentric phase of the movement and controlled during the eccentric phase. At each session, participants register exercise activities, intensity, and rate of perceived exertion. The power training is performed by specially trained exercise specialists.
-
3.
REC intervention
The REC group will be asked to follow the European recommendations for older adults on diet and physical activity over the course of the study and will be provided with publicly available material. In addition, two seminars on specific topics related to healthy aging will be provided to the group.
In all intervention groups, participants will continue with concomitant care and activities, e.g., if they have a rehabilitation plan including exercise. If participants experience changes in their medical condition, an additional consultation with the physician will be arranged to evaluate if participation in the study potentially will be harmful.
Compliance with the intervention
For the PROT and EXEPROT interventions, adherence to the protein protocol will be evaluated as average protein intake ≥ 1.35 g/kg/day at the 2 months and 4 months follow-up. Compliance and reasons for lack of compliance will also be estimated during each delivery of products with a set of questions (e.g., supplement consumption, changes to habitual food intake) and regular phone follow-ups. If participants are unable to reach the protein target, additional face-to-face or phone interview will be planned to support adherence. For the EXEPROT intervention, adherence to the exercise protocol will be considered as achieving minimum to 75% of valid exercise sessions, considered as minimum 70% of the exercises planned for each session. Reasons for non-adherence will be documented.
Sample size determination
Muscle power is the primary outcome of this study. Due to lack of studies comparable to this study design (e.g., age and frailty status of the participants, type of exercise and level of protein supplementation), we have calculated sample size using a combination of studies and methods. Based on findings by Bechshøft et al. [36], the effect of 12 weeks of protein supplementation (two daily supplements of 20 g milk protein) in combination with resistance training in + 80-year-old healthy adults increased muscle power by 15% (SEM ± 5%) in comparison with − 7% (SEM ± 6%) in the control group (receiving protein supplementation only). In the study by Park et al. [37], 12 weeks of protein supplementation (0.8 g/kg/day, 1.2 g/kg/day, or 1.5 g/kg/day) to pre-frail or frail older adults above 70 years resulted in an increase in muscle mass (estimated by DXA) of approximately 4% in the group receiving 1.5 g/kg/day. Unpublished data from our own group shows that change in muscle mass (estimated by DXA) accounted for 1.95% of the change in muscle power (power-rig) in older adults following 12 weeks of explosive resistance training. Hence, the estimated effect of an increase in muscle mass of 4% on muscle power is 7.8%. Adding this to the results from Bechshøft et al. [36] gives us an estimated change on 0.8% in the PROT group. Assuming that the change in muscle mass are comparable in the three groups, we therefore expect a change in muscle power of 15%, 0.8%, and − 7% with a SD of 30 in the EXEPROT, PROT, and REC groups, respectively.
Setting a power of 0.8 a sample size with 37 participants in each arm should be enough to detect a significant difference in muscle power (significance level at 0.05). Adding 25% to account for dropouts a total of 150 participants is needed.
Strength calculation was made in PASS 14.
Randomization and blinding
After the baseline assessment, each participant will be randomized to one of the three study groups (PROT, EXEPROT, or REC) using a computer-based random-block randomization scheme, clustering by couples when cohabitees wish to be enrolled together. The code is generated, concealed (sealed envelopes), and stored by personnel who is not part of run of the study. This personnel reveals the allocation to interventions based on ID numbers only to the research assistants who will inform participants. The trial has an open design with blind assessment of outcomes, which means that participants will be asked not to reveal group allocation when undergoing follow-up measurements, as researchers conducting follow-up measurements will be blinded to group allocation. To assess the extent to which blinding has been preserved, researchers will record the number of cases in which allocation was revealed.
Outcome measures
A proposed schedule for enrolment, intervention, and assessment is shown in the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT), Table 1. In addition, recommended items to address for intervention trials are reflected in the SPIRIT Checklist [38] (Additional file 1) and in the WHO Trial Registration Data set (Additional file 2).
Table 1.
Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) figure: proposed schedule for enrolment, intervention, and assessment
| Time point | Study period | ||||||
|---|---|---|---|---|---|---|---|
| Enrolment | Stabilization phase | Allocation | Post-allocation | Close-out | |||
| t1 | t2 | t3 | t3 | t4 | t5 | t5 | |
| Enrolment | |||||||
| Eligibility screen | X | ||||||
| Informed consent | X | ||||||
| Medical screening | x | ||||||
| Nutrition check | x | x | x | ||||
| Allocation | x | ||||||
| Interventions* | |||||||
| [EXEPROT] | ↔ | ↔ | ↔ | ||||
| [PROT] | ↔ | ↔ | ↔ | ||||
| [REC] | x | x | |||||
| Assessments | |||||||
| [Baseline variables, gender, age, education, marital status, depression, incontinence, chronic diseases, use of medication, risk of poor protein intake, eating symptom questionnaire, risk of dysphagia, appetite, dental status] | X | ||||||
| [primary outcome variable lower leg muscle power] | x | x | X | ||||
| [secondary outcome variables physical frailty status, jump muscle power, leg press, hand grip strength, SPPB, waist and hip circumference, body weight, lean mass, fat mass, BMD, health-related QoL, pain, fatigue, ADL, fear of falling, blood markers, physical activity, sedentary behavior, nap and sleep, dietary intake, walking speed, rising from laying position, MNA, EVS, risk of poor protein intake, DDST] | x | x | x | ||||
DSST Digit Symbol Substitution Test, SPPB Short Physical Performance Battery, BMD bone mineral density, QoL quality of life, ADL activities of daily living, MNA Mini Nutritional Assessment, EVS Eating Validation Scheme
*See explanation in the text
Test sessions
Five test sessions will be performed (T1–T5), see Fig. 1 and Table 1.
T1, T2 and T4: The pre- and post-test of the stabilization period and the test halfway through the intervention will consist of a nutrition check including assessment of protein intake by Pro 55+, 4-day food records, and 24-h recall interviews.
T3 and T5: The pre- and post-intervention test will include assessment of baseline variables and primary and secondary outcomes (specified in Table 2).
Table 2.
An overview of variables and outcomes, outcome measures, instruments and time point for the assessment
| Outcome | Outcome measures | Instrument | Time point |
|---|---|---|---|
| Descriptive variables | |||
| Personal information | Age, gender, former job, marital status, educational background and chronic diseases | Self-report | T3 |
| Depression | The Major Depression Inventory (MDI) [39] | T3 | |
| Incontinence | International Consultation on Incontinence Questionnaire (ICIQ) [40] | T3 | |
| Eating ability | Self-reported dental state | T3 | |
| The Eating Symptom Questionnaire [41] | |||
| The EAT-10 Questionnaire [42] | |||
| Simplified Nutritional Appetite Questionnaire [43] | |||
| Primary outcome | |||
| Muscle power | Lower leg muscle power | The Nottingham Leg Rig [44–46] | T3 and T5 |
| Secondary outcomes | |||
| Muscle mechanical function | Countermovement jump | The countermovement jump is performed on a force platform (Kistler 9281 B, 40 × 60 × 5 cm) following the procedure described in [47]. Four maximal jumps will be performed with 1-min interval and the highest jump recorded | T3 and T5 |
| Maximal muscle strength | Leg press | Assessed on the dominant leg in a custom-built unilateral leg press device with a fixed footplate instrumented with piezoelectric force transducers (Kistler 9367/8 B). The force signals will be digitally sampled at 1 kHz while on-line visual feedback is provided to the subject. The contractile rate of force development and impulse will be determined in the trial with the highest resultant peak force [44, 48] | T3 and T5 |
| Handgrip strength | Handgrip strength is measured using a handheld dynamometer (Original Smedley’s Daynameter, Scandidact, 100 kg, Cat. No. 281128). Participants are instructed to sit with the elbow at a 90° angle, the wrist in neutral position. The inner lever of the dynamometer is adjusted to the hand of the participants (the second phalanxes against the lever) (Andersen-Ranberg et al. 2009). A minimum of three contractions in each hand will be performed and testing continues until participant produce less force than the prior test. | T3 and T5 | |
| Physical Frailty Status |
The SHARE-FI75+ Fried frailty phenotype |
The SHARE-FI75+ is a physical frailty assessment tool that is developed specifically for community-dwelling adults aged ≥ 75 years [5] | T3 and T5 |
| Fried frailty phenotype consists of five variables where three are based on questions: (i) unintentional weight loss, (ii) self-reported exhaustion, and (iii) low energy expenditure and the remaining two are based on objective assessment: (iv) slow gait speed and (v) weak hand grip strength [9]. The variable ‘low energy expenditure’ is modified to follow the current recommendations on physical activity in older adults from the World Health Organization [49]. | |||
| Risk of malnutrition | Protein intake | The Protein Screener Pro55+ is used to assess the risk of poor protein intake [35] | T1, T2, T3 and T5 |
| Four days food records (filled out on three weekdays and one day during the weekend) are calculated (Winfood 4.1) to estimate the average protein intake (g) per kg body weight per day and protein content per meal. In addition, energy intake and distribution of macronutrients are calculated. | |||
| Weight loss | Self-reported unintentional weight changes during the last month | T1, T2, T3, T4, and T5 | |
| Nutritional status | The Eating Validation Scheme (EVS) is composed of five questions about dietary intake and weight loss and three questions about risk factors (dysphagia, eating assistance, and acute illness) [50] | T3 and T5 | |
| The Mini Nutritional Assessment (MNA) is composed of 18 questions and measurements concerning appetite, eating ability, weight, need for help, illness, and medication [51] | |||
| Anthropometry | Weight | Measured in light clothes, without shoes and subtracting 0.5 kg for the weight of clothes using a calibrated TANITA scale (model DC430SMA) | T3 and T5 |
| Waist- and Hip- circumference | Following the protocol by the World Health Organization [52] | ||
| Height | Measured without shoes | T3 | |
| Body composition | Estimation of fat mass, fat-free mass and bone mass | Dual-energy X-ray absorptiometry (DXA) (Lunar Prodigy) scans will be used to assess whole body composition with special emphasis on lean mass and fat tissue as well as bone mineral density. | T3 and T5 |
| Foot-to-foot bioelectrical impedance analysis (BIA), using the TANITA Total Body Composition Analyzer (model DC430SMA). | |||
| Physical function and mobility | Gait speed, Chair stand, Balance | The Short Physical Performance Battery (SPPB) [53] | T3 and T5 |
| Rising from laying position on the floor and stand and reach test [54] | |||
| Self-selected and maximal gait speed (10 m) [55–57] | |||
| Distance walked during 2 min [58, 59] | |||
| Physical activity level | Objective measures of intensity, duration, and patterns of physical activity and sedentary behavior | Hip-worn accelerometers, ActiGraph (removed during sleep) | T3 and T5 |
| Thigh-worn accelerometers, Axivity (24 h/day) | |||
| Data will be continuously collected in a raw format at 30/50 Hz, respectively, over a period of 7 days. | |||
| Self-reported sedentary behavior | The Sedentary Behavior Questionnaire (SBQ) [60] | T3 and T5 | |
| Activities of daily living | Self-report | Questionnaire that combines items from the Most Efficient Lists and the Short-Form of Late-Life Function and Disability Instrument [61–63] | T3 and T5 |
| Pain, fatigue, and fatigability | Self-report | The Brief Pain Inventory - Short Form (BPI-sf) [64] | T3 and T5 |
| The Mobility fatigue scale “Mob-T” [65] | |||
| The Pittsburgh Fatigability Scale (PFS) for older adults (only the domain about physical fatigue will be assessed) [66] | |||
| Fear of falling | Self-report | The Falls Efficacy Scale – International (FES-I) [67] | T3 and T5 |
| Self-reported falls within the last year | |||
| Cognitive function | Pencil and paper test | The Digit Symbol Substitution Test (DSST) [68, 69] | T3 and T5 |
| Health-related quality of life | Self-report | The EQ-5D-3L questionnaire [70] | T3 and T5 |
| Biomarkers | Blood sample | Biomarkers related to nutritional status, physical activity, sedentary behavior, as well as physical and cognitive function—such as lipids, hormones, proteins, cytokines, vitamins, and minerals, e.g., cholesterol, HbA1c, adiponectin, suPAR, Crp, IL-6, B12 and vitamin D, vitamin B12 [71–74] | T3 and T5 |
T1 time of enrolment, T2 post the stabilization phase, T3 baseline pre-intervention, T4 half-way follow-up, T5 close-out post-intervention
Data collection
Collection of data will be performed by trained research assistants from the University of Southern Denmark. Training of the research assistants includes theoretical teaching in the applied methods and tests, supervision by other research assistant, and frequent meetings with colleagues to share experiences and answers any questions that may arise. The descriptive variables (personal information, information about chronic diseases, depression, incontinence and eating ability) will be collected at baseline (T3). The primary and secondary outcomes data will be collected at baseline pre-intervention (T3) and post-intervention (T5). Participants will be invited to test irrespectively of their compliance to the intervention protocol. Participants are offered personal feedback on selected outcomes after ending the interventions to promote retention in intervention and post-intervention tests (T5).
Primary outcome
Lower leg muscle power is the primary outcome. This will be assessed unilaterally using the Nottingham Leg Rig [44–46] on the dominant leg. A minimum of six trials will be conducted with approximately 45 s of rest between trials. Testing continues until participants produce less power than the prior test.
Secondary outcomes
The secondary outcomes include assessment of muscle mechanical function, maximal muscle strength, physical frailty status, protein intake, risk of malnutrition, anthropometry, body composition, physical function, mobility, physical activity, sedentary behavior, pain, fatigue, fear of falling, cognitive function, health-related quality of life, and biomarkers.
For an overview of descriptive variables, outcomes, instruments, and assessment time points, see Table 2.
Statistical analysis
Plans for data entry, coding, security, and storage including any related processes to promote data quality have been approved by the Danish Regional Data Protection Agency. The full analysis set will follow an intention-to-treat principle and will include all randomized participants. The study hypothesis will be tested with mixed linear models to assess changes in the main outcomes over time and between study arms controlling for confounders (e.g., age, sex, lifestyle factors). Per-protocol analysis of participants that are compliant to the protocol will be performed. Lastly, if sample size allows it, sub-group analysis by sex and by habitual lifestyle (protein intake and physical activity) will be performed based on baseline assessment. Wilcoxon signed rank sum test, Mann-Whitney U test, and odds ratio or chi-square test of relationships were used when appropriate. The statistical software programme STATA 16 (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC) will be used for the statistical analysis.
Discussion
This study provides a protocol for a community-based assessor-blinded RCT to determine the effects of interventions with high-protein diet alone or in combination with power training on muscle mechanical function (muscle power and strength), frailty status, functional performance, muscle mass, and quality of life. This may ultimately have an impact on the ability of older pre-frail and frail adults to maintain self-reliance for longer.
Currently, only few of the studies that have investigated the effect of combining protein and exercise have used individually assigned supplementation plans that take the participants’ habitual protein intake and preferences into account. Specifically, in relation to pre-frail or frail older adults, most former multidomain studies have focused on increasing intake of protein by means of supplements (protein powder or oral nutritional supplements) without individual adjustments in doses. In addition, several studies have been designed with resistance training protocol, but only few studies have used power training combining heavy loading with maximum intentional acceleration of the training load—and, to our knowledge, none of them in combination with a nutritional intervention. Further, none of the studies seemed to focus on optimizing the protein balance before starting the exercise all which contrasts with the present study.
Even though the current recommendation of total protein intake for older adults is ≥ 1.0 g protein/kg/day based on European recommendations [17], it has been suggested that older adults, and especially frail older people, can benefit from an even higher protein intake of 1.5 g protein/kg/day [18, 19]. To evaluate the effects of a higher intake in comparison with the current recommendation, we have included the REC group as one of the intervention arms (illustrated in Fig. 1).
Study limitations
The study faces several important challenges. One of the major challenges is recruitment, compliance with supplementation, and adherence to the exercise intervention because of the age (80+) and the pre-frail and frail syndrome of the participants. In addition, the high number of tests in the study may increase the risk of dropouts. In order to limit the impact of these challenges, recruitment is performed in collaboration with health care personnel from the department for the preventive home visits in the municipality of Odense. They are experienced in addressing this population and can contact community-dwelling + 80-year-old citizens that live within a geographically limited area. This gives the opportunity to offer exercise intervention in a local facility and to deliver the products directly to the homes of the participants and thereby limiting the impact of need for transportation. To limit the risk of dropouts during the study, participants are carefully informed about the different tests before and during the study. Participants are informed that they can always decline some of the tests and still be part of the study.
The 4-day food records are important components of this study both in phase 1 and phase 2. The method is demanding for the participants, and the self-reported intake may be affected by social desirability and memory impairments. This may translate into under- or overreporting and result in misclassification of protein status (phase 1) and miscalculation of additional need for protein (phase 2). Nevertheless, the method has been used and validated in other studies among older adults [75, 76]. In addition, the food records are qualified together with the participant during a face-to-face interview and supplemented with the probability scores from the Pro55+ [35].
The power calculation assumes that EXEPRROT is superior to PROT which is superior to REC. Since no former studies have used a study design comparable to the one used in the current study, we needed to base our power calculation on a combination of two studies. Furthermore, the power calculation is based on the number of participants needed for phase 2 of the study. However, it is unknown how many participants we have to include in phase 1 to find the 150 participants that have the required protein intake of 1 g/kg/day. To decrease the risk of having to recruit a very large sample, each participant will receive individual nutritional guidance in phase 1, together with written information about protein-rich diets specifically developed for our target group.
Study strengths
A major strength of the study is the design with recruitment of the participants in collaboration with the preventive home visit service of the municipality of Odense. Different recruitment pathways are used for recruitment in agreement with Danish National law. This dictates that the preventive home visit service should identify older adults at risk of functional loss and disability using original pathway (e.g., directly contact by phone and invitation letter to older adults who are 80+) as well as additional ad hoc pathways to reach older adults who may be eligible (pre-frail/frail) but are more difficult to enroll. This design allows us to study the effects of a targeted action plan developed in collaboration with primary preventive sector to community-dwelling citizens in a community setting.
Furthermore, we design a “decentralized” intervention model where the exercise facilities are close to the older citizen and require minimal transport. Selection bias cannot completely be ruled out, but the specific design of the study will contribute to minimize it. According to our knowledge, such a study set-up with a strong applied element has never been used before. If the used interventions appear to be effective, they may rapidly be implemented in the primary preventive sector.
Another strength is the exercise intervention applied in the study. The intervention is supervised by skilled instructors, but it is also carried out in the municipality and hence will not demand other than the available equipment which may ease the implementation (if proven successful). The REC group will receive available information about the recommendations on nutrition and physical activity in older age in addition to two talks about these topics. This resemble the current practice in many municipalities and makes the control group very realistic, which helps to illustrate the additional effect of a more targeted intervention.
In contrast to former studies, we have chosen to provide the participants in the EXEPROT and PROT with ordinary off-the-shell dairy-based protein-rich products. This type of intervention has several advantages: off-the-shelf products are cheap, known by the participants, there is a large range of products, and they are easy to buy—this may increase compliance as participants recognize the products, are less likely to experience sensory-specific satiety, and (if proven successful) make it easy to transfer into recommendations and apply. Further, if the PROT arm show an effect of only adding protein, this may be of relevance to several older adults who, due to severe physical limitations or other, are unable to participate in exercise interventions.
The intervention period is 16 weeks which in general is slightly longer than several intervention studies. The longer intervention period gives the opportunity to have a familiarization period to the interventions (stepwise increase in protein intake, focus on technique in the exercise sessions), which may increase compliance to the protein intervention and reduce the risk of injuries from the exercise intervention. In addition, a recent meta-analysis have illustrated that the combination of protein supplementation and exercise is superior to exercise alone, but longer interventions (> 12 weeks) are required in the population of older adults [77].
The stabilizations phase provides us with a lot of important knowledge about the participants “starting point” and makes it possible to investigate who benefits most from the intervention—the ones with a habitual high intake or the ones who largely increase their intake of protein? Also, we can investigate who is able to increase their intake and what are the barriers for not increasing.
In general, our initiatives to monitor protein intake and compliance with the power training might help us to understand who benefits, how much is needed, and how the results are affected by participants habitual habits in relation to dietary protein intake and physical activity.
In summary, this study will add important knowledge to understand the influence of protein supplementation alone with off-the-shelf dairy products or combined with structured power training on physical frailty. Developing action plans which counteract physical frailty is extremely important to increase the proportion of adults + 80 years who remain self-reliant. Maintaining the ability to perform activities of daily living is essential both for older citizens as well as for health care providers.
Trial status
Recruitment of intervention and control group participants was still ongoing at the time of manuscript submission. The protocol version number is NCT03842579 (15 February 2019), the date recruitment began was 13 February 2019, and the approximate date when recruitment will be completed is 01 June 2021.
Supplementary information
Additional file 1. The SPIRIT 2013 Checklist.
Additional file 2:. the WHO Trial Registration Data Set.
Acknowledgements
We would like to acknowledge Jenny Havn, chief of the department for preventive home visits in the Municipality of Odense, and her team for their collaboration on recruitment of participants.
We would like to acknowledge Marianne Skovsager Andersen, department of endocrinology at the University Hospital in the city of Odense, for sharing her expertise about blood markers.
Roles and responsibilities
University of Southern Denmark
- Overall responsible for the conduct of the study
- Preparation of protocol and registrations
- Responsible for the stabilization phase
- Responsible for the run of the interventions, including training, plan for the products, follow-up with participants, presentations to the REC and NOG groups etc.
- Data collection—including training of staff, organizing test days, entering of data
- Writing of manuscripts with results
The Municipality of Odense
- Responsible for the recruitment of participant in collaboration with partners at the University of Southern Denmark
- Part of the run of the interventions (deliverance of products, provision of training facilities, etc.)
Steering Committee (SFB, AMB, BC, & PC)
- See title page for members
- Design of the study and agreement of final protocol
- Administration of funding and budget
- Reviewing the progress of the study and if necessary, agree on changes to the protocol
Abbreviations
- RCT
Randomized controlled trial
- Pro55+
Protein Screener
- PROT
Protein-only group
- PROTEXE
Protein and exercise group
- REC
Recommendation group
- NOG
Natural observation group
- MMSE
Mini Mental State Examination
- DXA
Dual-energy X-ray absorptiometry
- QoL
Quality of life
- SPPB
Short Physical Performance Battery
- EVS
Eating Validation Scheme
- MNA
Mini Nutritional Assessment
Authors’ contributions
AB, BC, and PC drafted the study idea and SFB helped with the final design. AB drafted the study protocol, and SFB was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Funding
The study has been externally funded by The Danish Dairy Research Foundation and by the European Funding Agency Program INTERREG 5a (Welfare Innovation in Primary Prevention - “the WIPP-project”, work package 4.5). Arla Foods Amba has been a project partner in the application but has only been involved in the design of the study and will not be involved in the collection, analysis, interpretation of data, or decision to submit results. The remaining funding body had no role in the design of the study and collection, analysis and interpretation of data, and in writing the manuscript. In addition, they will not have any role in the decision to submit results.
Availability of data and materials
Not applicable, no datasets are included in this study protocol.
Ethics approval and consent to participate
The study has been approved by the Regional Committees on Health Research Ethics for Southern Denmark (project id: S-20180048). Written informed consent will be given from all eligible participants to health care personnel from the Municipality of Odense on behalf of the University of Southern Denmark prior to entry into the study. Any adverse events or unintended effects of the interventions will be reported to the committee. Participants are covered by the Danish Patient Insurance Association and can apply for financial compensation in case any damage occurs while participating in the research project. This information will be given to participants both verbally and written (in the pamphlets from The National Committee on Health Research Ethics) during recruitment. In addition, the study is reported to the Research & Innovation Organization at the University of Southern Denmark (reg. no.: 10.122). All management of data will follow their guidelines to ensure that data management is according to the current legislations. Participants will not receive any compensation for their participation in the study.
Changes to the protocol will be reported to the Regional Committees on Health Research Ethics for Southern Denmark and to the Research & Innovation Organization at the University of Southern Denmark, as appropriate. In addition, the changes will be documented on clinicaltrials.gov.
The results of the study will be disseminated through reports, publication of articles in scientific journals within the field of aging, nutrition and exercise, publication of articles for public dissemination (e.g., targeting stakeholders or staff working with primary prevention or targeting community-dwelling older adults), conference presentations, and presentations to older adults and personnel working with primary prevention. We will follow the Vancouver guidelines for authorship.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Paolo Caserotti is the Trial Sponsor.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sussi F. Buhl, Email: sbuhl@health.sdu.dk
Anne Marie Beck, Email: ambe@kp.dk, Email: anne.marie.beck@regionh.dk.
Britt Christensen, Email: britt.christensen@arlafoods.com.
Paolo Caserotti, Email: pcaserotti@health.sdu.dk.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13063-020-04572-z.
References
- 1.Lunenfeld B, Stratton P. The clinical consequences of an ageing world and preventive strategies. Best Pract Res Clin Obstet Gynaecol. 2013;27(5):643–659. doi: 10.1016/j.bpobgyn.2013.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Statistics D. Population prognosis 2018 for the whole country [cited 2019 April 17th ]. Available from: http://www.dst.dk/da/statistik/emner/befolkning-og-valg/befolkning-og-befolkningsfremskrivning/befolkningsfremskrivning.
- 3.Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–397. doi: 10.1016/j.jamda.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO. WHO clinical consortium on healthy ageing. topic focus: frailty and intrinsic capacity. report of consortium meeting 1–2 December 2016 in Geneva, Switzerland.; 2017.
- 5.Romero-Ortuno R, Soraghan C. A Frailty Instrument for primary care for those aged 75 years or more: findings from the Survey of Health, Ageing and Retirement in Europe, a longitudinal population-based cohort study (SHARE-FI75+) BMJ Open. 2014;4(12):e006645. doi: 10.1136/bmjopen-2014-006645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hanlon P, Nicholl BI, Jani BD, Lee D, McQueenie R, Mair FS. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493 737 UK Biobank participants. Lancet Public Health. 2018;3(7):e323–ee32. doi: 10.1016/S2468-2667(18)30091-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crocker TF, Brown L, Clegg A, Farley K, Franklin M, Simpkins S, et al. Quality of life is substantially worse for community-dwelling older people living with frailty: systematic review and meta-analysis. Qual Life Res. 2019;28(8):2041–2056. doi: 10.1007/s11136-019-02149-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hajek A, Bock JO, Saum KU, Matschinger H, Brenner H, Holleczek B, et al. Frailty and healthcare costs-longitudinal results of a prospective cohort study. Age Ageing. 2018;47(2):233–241. doi: 10.1093/ageing/afx157. [DOI] [PubMed] [Google Scholar]
- 9.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 10.Op het Veld LP, van Rossum E, Kempen GI, de Vet HC, Hajema K, Beurskens AJ. Fried phenotype of frailty: cross-sectional comparison of three frailty stages on various health domains. BMC Geriatr. 2015;15:77. doi: 10.1186/s12877-015-0078-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilson MG, Beland F, Julien D, Gauvin L, Guindon GE, Roy D, et al. Interventions for preventing, delaying the onset, or decreasing the burden of frailty: an overview of systematic reviews. Syst Rev. 2015;4:128. doi: 10.1186/s13643-015-0110-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deutz NE, Bauer JM, Barazzoni R, Biolo G, Boirie Y, Bosy-Westphal A, et al. Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr. 2014;33(6):929–936. doi: 10.1016/j.clnu.2014.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lorenzo-Lopez L, Maseda A, de Labra C, Regueiro-Folgueira L, Rodriguez-Villamil JL, Millan-Calenti JC. Nutritional determinants of frailty in older adults: a systematic review. BMC Geriatr. 2017;17(1):108. doi: 10.1186/s12877-017-0496-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sternberg SA, Wershof Schwartz A, Karunananthan S, Bergman H, Mark Clarfield A. The identification of frailty: a systematic literature review. J Am Geriatr Soc. 2011;59(11):2129–2138. doi: 10.1111/j.1532-5415.2011.03597.x. [DOI] [PubMed] [Google Scholar]
- 15.Phillips SM, Tang JE, Moore DR. The role of milk- and soy-based protein in support of muscle protein synthesis and muscle protein accretion in young and elderly persons. J Am Coll Nutr. 2009;28(4):343–354. doi: 10.1080/07315724.2009.10718096. [DOI] [PubMed] [Google Scholar]
- 16.Breen L, Phillips SM. Skeletal muscle protein metabolism in the elderly: interventions to counteract the ‘anabolic resistance’ of ageing. Nutr Metab (Lond) 2011;8:68. doi: 10.1186/1743-7075-8-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Volkert D, Beck AM, Cederholm T, Cruz-Jentoft A, Goisser S, Hooper L, et al. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin Nutr. 2019;38(1):10–47. doi: 10.1016/j.clnu.2018.05.024. [DOI] [PubMed] [Google Scholar]
- 18.Lancha AH, Jr, Zanella R, Jr, Tanabe SG, Andriamihaja M, Blachier F. Dietary protein supplementation in the elderly for limiting muscle mass loss. Amino Acids. 2017;49(1):33–47. doi: 10.1007/s00726-016-2355-4. [DOI] [PubMed] [Google Scholar]
- 19.Phillips SM. Nutrition in the elderly: a recommendation for more (evenly distributed) protein? Am J Clin Nutr. 2017;106(1):12–13. doi: 10.3945/ajcn.117.159863. [DOI] [PubMed] [Google Scholar]
- 20.Bauer J, Biolo G, Cederholm T, Cesari M, Cruz-Jentoft AJ, Morley JE, et al. Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc. 2013;14(8):542–559. doi: 10.1016/j.jamda.2013.05.021. [DOI] [PubMed] [Google Scholar]
- 21.Jyvakorpi SK, Pitkala KH, Puranen TM, Bjorkman MP, Kautiainen H, Strandberg TE, et al. High proportions of older people with normal nutritional status have poor protein intake and low diet quality. Arch Gerontol Geriatr. 2016;67:40–45. doi: 10.1016/j.archger.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 22.Volpi E, Campbell WW, Dwyer JT, Johnson MA, Jensen GL, Morley JE, et al. Is the optimal level of protein intake for older adults greater than the recommended dietary allowance? J Gerontol A Biol Sci Med Sci. 2013;68(6):677–681. doi: 10.1093/gerona/gls229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hvid LG, Strotmeyer ES, Skjodt M, Magnussen LV, Andersen M, Caserotti P. Voluntary muscle activation improves with power training and is associated with changes in gait speed in mobility-limited older adults - a randomized controlled trial. Exp Gerontol. 2016;80:51–56. doi: 10.1016/j.exger.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 24.Fragala MS, Cadore EL, Dorgo S, Izquierdo M, Kraemer WJ, Peterson MD, et al. Resistance training for older adults: position statement from the National Strength and Conditioning Association. J Strength Cond Res. 2019;33(8):2019–2052. doi: 10.1519/JSC.0000000000003230. [DOI] [PubMed] [Google Scholar]
- 25.Reid KF, Fielding RA. Skeletal muscle power: a critical determinant of physical functioning in older adults. Exerc Sport Sci Rev. 2012;40(1):4–12. doi: 10.1097/JES.0b013e31823b5f13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bean JF, Kiely DK, Herman S, Leveille SG, Mizer K, Frontera WR, et al. The relationship between leg power and physical performance in mobility-limited older people. J Am Geriatr Soc. 2002;50(3):461–467. doi: 10.1046/j.1532-5415.2002.50111.x. [DOI] [PubMed] [Google Scholar]
- 27.Evans WJ. Exercise strategies should be designed to increase muscle power. J Gerontol A Biol Sci Med Sci. 2000;55(6):M309–M310. doi: 10.1093/gerona/55.6.m309. [DOI] [PubMed] [Google Scholar]
- 28.Gade J, Pedersen RJ, Beck AM. Effect of protein or essential amino acid supplementation during prolonged resistance exercise training in older adults on body composition, muscle strength, and physical performance parameters: a systematic review. Rehabil Process Outcome. 2018;7:1179572718765760. [Google Scholar]
- 29.Kidd T, Mold F, Jones C, Ream E, Grosvenor W, Sund-Levander M, et al. What are the most effective interventions to improve physical performance in pre-frail and frail adults? A systematic review of randomised control trials. BMC Geriatr. 2019;19(1):184. doi: 10.1186/s12877-019-1196-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Minor BD, Heusinger DE, Melanson EL, Hamilton KL, Miller BF. Energy balance changes the anabolic effect of postexercise feeding in older individuals. J Gerontol A Biol Sci Med Sci. 2012;67(11):1161–1169. doi: 10.1093/gerona/gls080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haubois G, Annweiler C, Launay C, Fantino B, de Decker L, Allali G, et al. Development of a short form of Mini-Mental State Examination for the screening of dementia in older adults with a memory complaint: a case control study. BMC Geriatr. 2011;11:59. doi: 10.1186/1471-2318-11-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40(9):771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Kendall JC, Boyle E, Hartvigsen J, Hvid LG, Azari MF, Skjodt M, et al. Neck pain, concerns of falling and physical performance in community-dwelling Danish citizens over 75 years of age: a cross-sectional study. Scand J Public Health. 2016;44(7):695–701. doi: 10.1177/1403494816666414. [DOI] [PubMed] [Google Scholar]
- 34.Hvid LG, Nielsen MKF, Simonsen C, Andersen M, Caserotti P. Brain-derived neurotrophic factor (BDNF) serum basal levels is not affected by power training in mobility-limited older adults - a randomized controlled trial. Exp Gerontol. 2017;93:29–35. doi: 10.1016/j.exger.2017.03.019. [DOI] [PubMed] [Google Scholar]
- 35.Wijnhoven HAH, Elstgeest LEM, de Vet HCW, Nicolaou M, Snijder MB, Visser M. Development and validation of a short food questionnaire to screen for low protein intake in community-dwelling older adults: the Protein Screener 55+ (Pro55+) PLoS One. 2018;13(5):e0196406. doi: 10.1371/journal.pone.0196406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bechshoft RL, Malmgaard-Clausen NM, Gliese B, Beyer N, Mackey AL, Andersen JL, et al. Improved skeletal muscle mass and strength after heavy strength training in very old individuals. Exp Gerontol. 2017;92:96–105. doi: 10.1016/j.exger.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 37.Park Y, Choi JE, Hwang HS. Protein supplementation improves muscle mass and physical performance in undernourished prefrail and frail elderly subjects: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr. 2018;108(5):1026–1033. doi: 10.1093/ajcn/nqy214. [DOI] [PubMed] [Google Scholar]
- 38.Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gotzsche PC, Krle AJK, et al. SPIRIT 2013 Statement: defining standard protocol items for clinical trials. Rev Panam Salud Publica. 2015;38(6):506–514. [PMC free article] [PubMed] [Google Scholar]
- 39.Bech P, Rasmussen NA, Olsen LR, Noerholm V, Abildgaard W. The sensitivity and specificity of the Major Depression Inventory, using the Present State Examination as the index of diagnostic validity. J Affect Disord. 2001;66(2–3):159–164. doi: 10.1016/s0165-0327(00)00309-8. [DOI] [PubMed] [Google Scholar]
- 40.Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23(4):322–330. doi: 10.1002/nau.20041. [DOI] [PubMed] [Google Scholar]
- 41.Norden J, Gronberg AM, Bosaeus I, Forslund HB, Hulthen L, Rothenberg E, et al. Nutrition impact symptoms and body composition in patients with COPD. Eur J Clin Nutr. 2015;69(2):256–261. doi: 10.1038/ejcn.2014.76. [DOI] [PubMed] [Google Scholar]
- 42.Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, et al. Validity and reliability of the Eating Assessment Tool (EAT-10) Ann Otol Rhinol Laryngol. 2008;117(12):919–924. doi: 10.1177/000348940811701210. [DOI] [PubMed] [Google Scholar]
- 43.Wilson MM, Thomas DR, Rubenstein LZ, Chibnall JT, Anderson S, Baxi A, et al. Appetite assessment: simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am J Clin Nutr. 2005;82(5):1074–1081. doi: 10.1093/ajcn/82.5.1074. [DOI] [PubMed] [Google Scholar]
- 44.Caserotti P, Aagaard P, Larsen JB, Puggaard L. Explosive heavy-resistance training in old and very old adults: changes in rapid muscle force, strength and power. Scand J Med Sci Sports. 2008;18(6):773–782. doi: 10.1111/j.1600-0838.2007.00732.x. [DOI] [PubMed] [Google Scholar]
- 45.Aadahl M, Beyer N, Linneberg A, Thuesen BH, Jorgensen T. Grip strength and lower limb extension power in 19-72-year-old Danish men and women: the Health2006 study. BMJ Open. 2011;1(2):e000192. doi: 10.1136/bmjopen-2011-000192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Skelton DA, Kennedy J, Rutherford OM. Explosive power and asymmetry in leg muscle function in frequent fallers and non-fallers aged over 65. Age Ageing. 2002;31(2):119–125. doi: 10.1093/ageing/31.2.119. [DOI] [PubMed] [Google Scholar]
- 47.Caserotti P, Aagaard P, Simonsen EB, Puggaard L. Contraction-specific differences in maximal muscle power during stretch-shortening cycle movements in elderly males and females. Eur J Appl Physiol. 2001;84(3):206–212. doi: 10.1007/s004210170006. [DOI] [PubMed] [Google Scholar]
- 48.Aagaard P, Simonsen EB, Andersen JL, Magnusson P, Dyhre-Poulsen P. Increased rate of force development and neural drive of human skeletal muscle following resistance training. J Appl Physiol (1985) 2002;93(4):1318–1326. doi: 10.1152/japplphysiol.00283.2002. [DOI] [PubMed] [Google Scholar]
- 49.WHO . Physical activity and older adults. Recommended levels of physical activity for adults aged 65 and above. Geneva: World Health Organization; 2010. [Google Scholar]
- 50.Beck AM, Beermann T, Kjaer S, Rasmussen HH. Ability of different screening tools to predict positive effect on nutritional intervention among the elderly in primary health care. Nutrition. 2013;29(7–8):993–999. doi: 10.1016/j.nut.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 51.Garry PJ, Vellas BJ. Practical and validated use of the Mini Nutritional Assessment in geriatric evaluation. Nutr Clin Care. 1999;2(3):146–154. [Google Scholar]
- 52.Organization WH . Waist circumference and waist-hip ratio: report of a WHO expert consultation, Geneva, 8-11 December 2008. 2011. [Google Scholar]
- 53.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 54.Bergland A, Laake K. Concurrent and predictive validity of “getting up from lying on the floor”. Aging Clin Exp Res. 2005;17(3):181–185. doi: 10.1007/BF03324594. [DOI] [PubMed] [Google Scholar]
- 55.Cesari M, Kritchevsky SB, Penninx BW, Nicklas BJ, Simonsick EM, Newman AB, et al. Prognostic value of usual gait speed in well-functioning older people--results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53(10):1675–1680. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 56.Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54(5):743–749. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 57.Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. Jama. 2011;305(1):50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Simonsick EM, Fan E, Fleg JL. Estimating cardiorespiratory fitness in well-functioning older adults: treadmill validation of the long distance corridor walk. J Am Geriatr Soc. 2006;54(1):127–132. doi: 10.1111/j.1532-5415.2005.00530.x. [DOI] [PubMed] [Google Scholar]
- 59.Connelly DM, Thomas BK, Cliffe SJ, Perry WM, Smith RE. Clinical utility of the 2-minute walk test for older adults living in long-term care. Physiother Can. 2009;61(2):78–87. doi: 10.3138/physio.61.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rosenberg DE, Norman GJ, Wagner N, Patrick K, Calfas KJ, Sallis JF. Reliability and validity of the Sedentary Behavior Questionnaire (SBQ) for adults. J Phys Act Health. 2010;7(6):697–705. doi: 10.1123/jpah.7.6.697. [DOI] [PubMed] [Google Scholar]
- 61.Jette AM, Haley SM, Coster WJ, Kooyoomjian JT, Levenson S, Heeren T, et al. Late life function and disability instrument: I. Development and evaluation of the disability component. J Gerontol A Biol Sci Med Sci. 2002;57(4):M209–M216. doi: 10.1093/gerona/57.4.m209. [DOI] [PubMed] [Google Scholar]
- 62.Haley SM, Jette AM, Coster WJ, Kooyoomjian JT, Levenson S, Heeren T, et al. Late life function and disability instrument: II. Development and evaluation of the function component. J Gerontol A Biol Sci Med Sci. 2002;57(4):M217–M222. doi: 10.1093/gerona/57.4.m217. [DOI] [PubMed] [Google Scholar]
- 63.McAuley E, Konopack JF, Motl RW, Rosengren K, Morris KS. Measuring disability and function in older women: psychometric properties of the late-life function and disability instrument. J Gerontol A Biol Sci Med Sci. 2005;60(7):901–909. doi: 10.1093/gerona/60.7.901. [DOI] [PubMed] [Google Scholar]
- 64.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap. 1994;23(2):129–138. [PubMed] [Google Scholar]
- 65.Avlund K, Kreiner S, Schultz-Larsen K. Functional ability scales for the elderly. Eur J Pub Health. 1996;6(3):35–42. [Google Scholar]
- 66.Glynn NW, Santanasto AJ, Simonsick EM, Boudreau RM, Beach SR, Schulz R, et al. The Pittsburgh Fatigability Scale for older adults: development and validation. J Am Geriatr Soc. 2015;63(1):130–135. doi: 10.1111/jgs.13191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I) Age Ageing. 2005;34(6):614–619. doi: 10.1093/ageing/afi196. [DOI] [PubMed] [Google Scholar]
- 68.Lezak MD, Howieson DB, Loring DW, Fischer JS. Neuropsychological assessment. USA: Oxford University Press; 2004. [Google Scholar]
- 69.Wechsler D. Wechsler adult intelligence scale - third edition: administration and scoring manual. San Antonio: The Psykological Corporation; 1997. [Google Scholar]
- 70.Oppe M, Devlin NJ, Szende A. EQ-5D value sets: inventory, comparative review and user guide: Springer; 2007. [PubMed]
- 71.Schaap LA, Pluijm SM, Deeg DJ, Harris TB, Kritchevsky SB, Newman AB, et al. Higher inflammatory marker levels in older persons: associations with 5-year change in muscle mass and muscle strength. J Gerontol A Biol Sci Med Sci. 2009;64(11):1183–1189. doi: 10.1093/gerona/glp097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB, et al. Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: the Health ABC Study. J Gerontol A Biol Sci Med Sci. 2002;57(5):M326–M332. doi: 10.1093/gerona/57.5.m326. [DOI] [PubMed] [Google Scholar]
- 73.Komulainen P, Pedersen M, Hanninen T, Bruunsgaard H, Lakka TA, Kivipelto M, et al. BDNF is a novel marker of cognitive function in ageing women: the DR’s EXTRA Study. Neurobiol Learn Mem. 2008;90(4):596–603. doi: 10.1016/j.nlm.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 74.Tavenier J, Haupt TH, Andersen AL, Buhl SF, Langkilde A, Andersen JR, et al. A high-protein diet during hospitalization is associated with an accelerated decrease in soluble urokinase plasminogen activator receptor levels in acutely ill elderly medical patients with SIRS. Nutr Res. 2017;41:56–64. doi: 10.1016/j.nutres.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 75.Pedersen AN, Fagt S, Ovesen L, Schroll M. Quality control including validation in dietary surveys of elderly subjects. The validation of a dietary history method (the SENECA-method) used in the 1914-population study in Glostrup of Danish men and women aged 80 years. J Nutr Health Aging. 2001;5(4):208–216. [PubMed] [Google Scholar]
- 76.Haveman-Nies A, Tucker KL, de Groot LC, Wilson PW, van Staveren WA. Evaluation of dietary quality in relationship to nutritional and lifestyle factors in elderly people of the US Framingham Heart Study and the European SENECA study. Eur J Clin Nutr. 2001;55(10):870–880. doi: 10.1038/sj.ejcn.1601232. [DOI] [PubMed] [Google Scholar]
- 77.Liao CD, Tsauo JY, Wu YT, Cheng CP, Chen HC, Huang YC, et al. Effects of protein supplementation combined with resistance exercise on body composition and physical function in older adults: a systematic review and meta-analysis. Am J Clin Nutr. 2017;106(4):1078–1091. doi: 10.3945/ajcn.116.143594. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. The SPIRIT 2013 Checklist.
Additional file 2:. the WHO Trial Registration Data Set.
Data Availability Statement
Not applicable, no datasets are included in this study protocol.