Abstract
Diabetes mellitus (DM) is a chronic condition characterised by β cell dysfunction and persistent hyperglycaemia. The disorder can be due to the absence of adequate pancreatic insulin production or a weak cellular response to insulin signalling. Among the three types of DM, namely, type 1 DM (T1DM), type 2 DM (T2DM), and gestational DM (GDM); T2DM accounts for almost 90% of diabetes cases worldwide.
Epigenetic traits are stably heritable phenotypes that result from certain changes that affect gene function without altering the gene sequence. While epigenetic traits are considered reversible modifications, they can be inherited mitotically and meiotically. In addition, epigenetic traits can randomly arise in response to environmental factors or certain genetic mutations or lesions, such as those affecting the enzymes that catalyse the epigenetic modification. In this review, we focus on the role of DNA methylation, a type of epigenetic modification, in the pathogenesis of T2DM.
Keywords: Diabetes mellitus, DNA methylation, Type 2 diabetes mellitus, Hypermethylation, Hypomethylation
Introduction
Diabetes mellitus
Diabetes mellitus (DM) is a chronic condition characterised by persistently elevated glucose levels in the bloodstream (i.e., hyperglycaemia) [1] and pancreatic β cell dysfunction [2]. In general, the disease is classified into three types, namely, type 1 DM (T1DM), type 2 DM (T2DM), and gestational DM (GDM), with T2DM accounting for approximately 90% of diabetes cases worldwide. In T2DM, the associated hyperglycaemia can be due to inadequate pancreatic insulin production or a weak cellular response to insulin signalling (i.e., insulin resistance). In addition, the development of T2DM depends, in part, on the balance between pancreatic β cell proliferation and apoptosis [1, 3].
T2DM is a multifactorial disease, with its aetiology affected by multiple genes (i.e., polygenic) in addition to environmental factors. Indeed, genome-wide association studies (GWASs) have linked aberrations in more than 40 different genes with an increased risk of T2DM. These genes are involved in the regulation of various biological processes, including cellular development, differentiation, and physiological functions. Environmental factors that have been associated with an increased risk of T2DM include age, obesity, and lack of physical activity [2].
The persistent hyperglycaemia in DM can ultimately lead to adverse complications, such as neuropathy, retinopathy, nephropathy, and cardiovascular diseases (CVDs). As a compounding factor, there is a prolonged pre-detection period in T2DM, during which one third to one half of all patients may go undiagnosed due to a lack of clinical symptoms. Indeed, some patients are only diagnosed with T2DM after the manifestation of complications associated with T2DM-induced hyperglycaemia [1, 3].
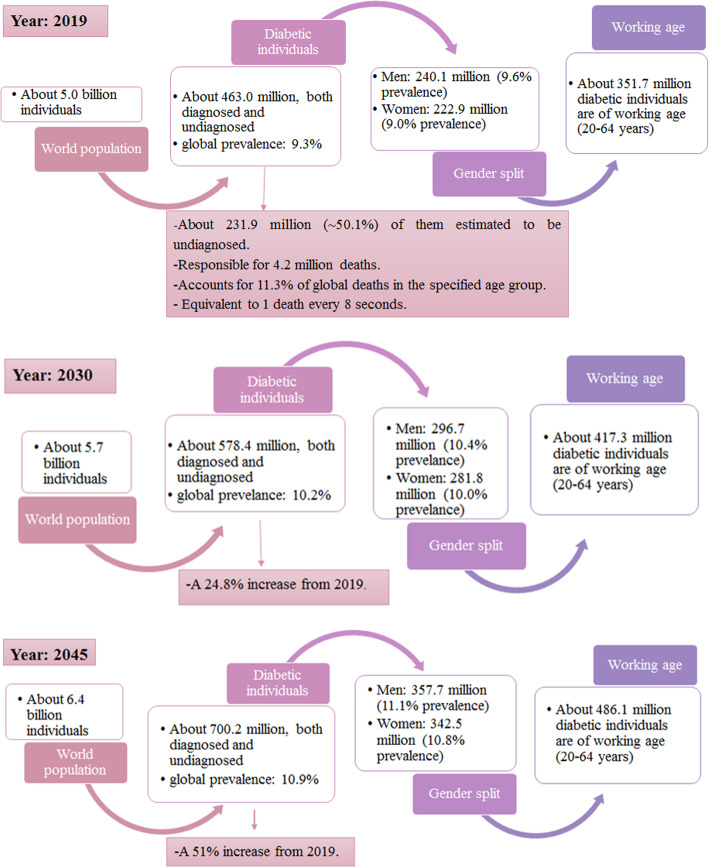
The latest statistics of the prevalence of DM (as of 2019) and the predicted statistics of the prevalence of DM for the years 2030 and 2045 are summarised in Fig. 1 [3]. Despite the high prevalence of DM, the exact mechanisms underlying the development of GDM, T1DM, and T2DM are not fully understood [1, 3]. Therefore, a greater understanding of the aetiology of DM is necessary to develop improved prevention and diagnostic tools and treatments for associated complications.
Fig. 1.
Worldwide DM statistics in 2019 for the age group 20–79 years old and the projections for years 2030 and 2045
Epigenetics
An epigenetic trait is a stably heritable phenotype resulting from certain changes in gene expression that do not alter the underlying DNA sequence [4]. Epigenetic traits are considered reversible modifications that can be inherited mitotically and meiotically. However, they can also randomly arise due to various environmental factors or genetic mutations such as those affecting the enzymes that catalyse the epigenetic modification [5, 6]. Important epigenetic modifications include DNA methylation; posttranslational histone tail modifications, such as methylation, phosphorylation, acetylation, and regulatory RNAs [7].
In general, epigenetic modifications do not occur independently but rather crosstalk with and regulate one another to create an epigenetic profile, which changes the function of the genome (gene expression) by altering the chromatin structure. The particular epigenetic profile can either lead to gene activation by relaxing the chromatin structure, thus allowing the transcription machinery to access the DNA, or to gene silencing by tightly packaging the chromatin structure and inhibiting access to the DNA [6]. Accordingly, the epigenetic profile has been shown to modulate gene expression in different cell types, developmental stages, and in health and disease states [8].
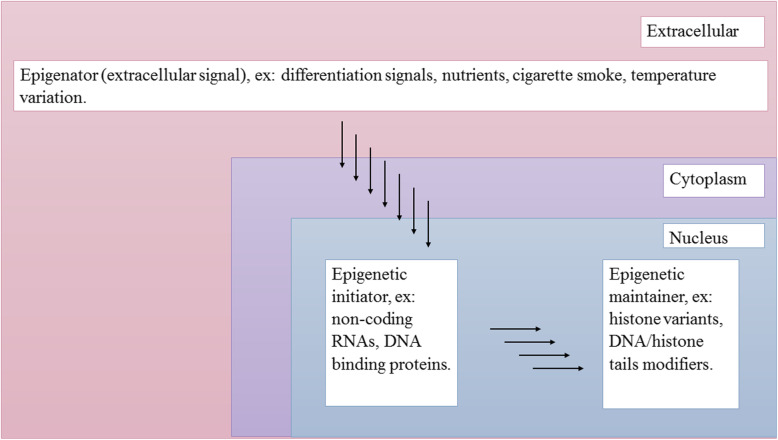
Three categories of signals that stimulate an epigenetic state have been proposed, namely, epigenators, epigenetic initiators, and epigenetic maintainers (Fig. 2). The epigenator signal is environmentally induced and triggers an intracellular pathway. It can be a modification-based event or a protein–protein interaction that releases the dormant activity of the epigenetic initiator. An example of an epigenator signal is temperature (in plants). The extracellular epigenator signal is received and transmitted by the intracellular epigenetic initiator signal, which translates the signal by initiating events required for establishing the signalled chromatin state at the chromatin location. The initiator signal can be non-coding RNAs, DNA-binding proteins and/or any entity capable of recognising DNA sequences and defining the chromatin state to be generated. An epigenetic maintainer signal maintains the chromatin state over subsequent generations, although not sufficiently enough to initiate it. This signal maintainer preserves the epigenetic profile in terminally differentiated cells and throughout the cell cycle. Examples include the DNA methylation of CpG islands [4].
Fig. 2.
The epigenetic pathway and the three categories of signals proposed. The extracellular epigenator signal triggers the initiation of the epigenetic pathway. The epigenetic initiator receives the signal from the epigenator and determines the chromatin state for establishing the epigenetic pathway. The epigenetic maintainer sustains the chromatin state in succeeding generations
DNA methylation
DNA methylation, which naturally occurs as a result of DNA replication, is the covalent addition of a methyl group (–CH3) to the 5’ position of the cytosine residue in the dinucleotide 5’-cytosine-phosphodiester bond-guanine-3’ (5’-CpG-3’) to form 5-methylcytosine (5mC). CpG DNA methylation is reversible [6, 9]. CpG islands have a high CpG density (> 50%) and are primarily located in the promoter region of genes but can also be found in enhancer and intragenic regions [5, 6]. Although 70% of CpG dinucleotides are methylated in humans, CpG dinucleotides of germ-line cells and promoters of somatic cells are relatively unmethylated [9].
In general, promoter CpG island hypomethylation is associated with transcriptional activation, whereas the hypermethylation of CpG islands is associated with transcriptional silencing. However, the methylation of CpG sites in regulatory regions outside the gene promoter also plays a role in regulating gene expression in a tissue-specific manner, thus making gene expression regulation through DNA methylation considerably more complex than simple promoter methylation. The process of gene silencing by DNA methylation is required for critical biological processes, such as cellular differentiation, genomic imprinting, X chromosome inactivation, and retrotransposon silencing. To date, two mechanisms have been proposed on how DNA methylation silences gene expression. The first mechanism posits that methylation prevents the binding of transcription factors to cytosine in the major DNA groove. The second mechanism suggests that methylation recruits proteins containing the methyl-CpG-binding domain to the 5mC, which in turn recruits certain histone modifiers, such as histone deacetylases, that change the chromatin state in a way that leads to a compact chromatin structure [6].
CpG methylation is mediated by the enzymatic family of DNA methyltransferases (DNMTs). In mammals, DNMTs use S-adenosyl methionine (SAM) as the methyl group donor to form the 5mC of the CpG. In humans, four main types of DNMTs exist, namely, DNMT1, DNMT3A, DNMT3B, and DNMT3L. DNMT1 is responsible for maintaining DNA methylation profiles during DNA replication in mitosis. DNMT1 recognises hemi-methylated CpGs and methylates them by copying the pre-existing DNA methylation profile from the parental DNA strands to the daughter DNA strands. DNMT3A and DNMT3B are considered de novo DNMTs. They recognise unmethylated CpGs and methylate them in response to various stimuli, thus creating new DNA methylation profiles. As such, DNMT3A and DNMT3B are responsible for establishing new DNA methylation profiles during early embryonic development and throughout postnatal life. DNMT3L, which functions in germ cells, enhances de novo methylation and increases the binding of methyl donors [6, 9, 10].
DNA demethylation can occur actively through deamination of the methylated or a nearby base through the action of activation-induced deaminase (AID), or through oxidising the methylated base through the action of ten-eleven translocation (TET) enzymes, both of which are independent of DNA replication. Base excision repair (BER) then replaces the modified nucleotide along with the surrounding nucleotides. DNA demethylation can also occur passively through diluting DNA methylation markers during DNA replication. However, the direct conversion of 5mC to cytosine does not occur [11].
DNA methylation in T2DM
All the T2DM genetic risk factors identified by GWASs thus far have been estimated to account for only approximately 10% of the estimated heritability of T2DM. Therefore, research has continued to focus on exploring the role of epigenetics in T2DM in the hope of explaining some, if not all, of the missing heritability [6]. Recent studies have found that T2DM environmental risk factors regulate, through epigenetic modifications, the expression of T2DM genetic risk factors that control the particular intracellular signalling pathways involved in the onset and development of T2DM [2]. The following section focuses on what is known regarding the role of DNA methylation in the development and pathogenesis of T2DM, although the exact mechanisms underlying the involvement of DNA methylation in T2DM pathogenesis remain unclear [12].
Single or multiple gene studies
Pancreas and related cell lines
Insulin
Insulin is a peptide hormone secreted by pancreatic β cells upon nutrient uptake. It regulates blood glucose levels by enhancing glucose uptake and glycolysis in skeletal and adipose tissues [13]. During this process, insulin stimulates the translocation of the glucose transporter GLUT4 to the cell membrane from intracellular pools. Insulin also regulates blood glucose levels by enhancing the rate of glycogen synthesis in the liver, skeletal muscle, and adipose tissue, thus lowering the rate of glycogen breakdown in these tissues and inhibiting hepatic gluconeogenesis and glycogenolysis [14].
A number of cis-acting regulatory elements in the insulin promoter can work over large distances. These elements have been shown to bind a range of tissue-specific and ubiquitous transcription factors. One of these regulatory elements is the cyclic adenosine monophosphate (cAMP) responsive element (CRE), which can bind a diverse array of transcription factors [15]. In rodents, only one CRE site exists in the insulin promoter, whereas in humans, there are four, with CRE2 being the sole CRE conserved between the species. cAMP responsive element-binding protein-1 (CREB-1) and activating transcription factor-2 (ATF-2) are CRE-associated transcription factors. CREB-1 has an inhibitory effect on transcription, whereas ATF-2 activates transcription. Interestingly, CRE2 mutations and not CREB-1 mutations inhibited the ATF-2 effect [15]. The CRE site also plays a crucial role in insulin gene regulation [16].
The analysis of the human insulin (INS) and mouse Ins2 promoters has identified the presence of nine and three CpG sites in the regions upstream of the transcription start site (TSS), respectively. Further analysis has revealed that the CpG sites present in the human INS and mouse Ins2 promoters were differentially unmethylated in β cells compared with other tissues. Using the NIT-1 mouse insulinoma cell line, the methylation of these CpG sites has been shown to suppress the expression of the insulin-promoter-driven reporter gene by almost 90% [17].
To assess the role of individual methylation events on insulin gene expression, individual CpG sites were methylated in the mouse Ins2 promoter and examined. The methylation of the CpG site within CRE was shown to independently suppress insulin promoter activity by approximately 50%. In addition, the methylation of one of the remaining two CpG sites had no effect on insulin gene expression, whereas the methylation of the other CpG site increased insulin gene expression by almost two folds. These findings indicate that methylation-dependent suppression of the insulin promoter is not simply additive, suggesting that other mechanisms are likely to cooperate with DNA methylation to suppress the expression of the insulin gene. Further analysis demonstrated that CRE CpG methylation inhibits the binding of CREB and ATF-2 to Ins2 CRE in vivo (NIT-1 cells), but not in vitro, and increases the binding of methyl CpG binding protein 2 (MeCP2). These findings indicate that MeCP2 binds to the methylated promoter to inhibit the binding of insulin transcriptional activators, thus decreasing insulin gene expression [17]. An in vitro examination of Ins2 in mouse embryonic stem cell cultures has previously indicated that the insulin gene is fully methylated; however, the gene becomes demethylated as the cells differentiate into insulin-producing β cells. Collectively, these findings suggest that the demethylation of the insulin promoter CpG sites plays a key role in β cell maturation and the tissue-specific expression of the insulin gene [17].
The role of DNA methylation was further examined in another study using human islets from T2DM and non-T2DM donors. The findings indicate that the glucose-stimulated insulin secretion (GSIS), insulin mRNA, and insulin content were reduced in the pancreatic islets of T2DM in comparison with the non-T2DM donors. In addition, four CpG sites (− 234, − 180, − 102, and + 63) showed increased DNA methylation in the T2DM pancreatic islets. Furthermore, insulin mRNA expression was found to negatively correlate with the degree of methylation in three of these CpG sites (− 234, − 180, and + 63). Researchers then investigated the effect of hyperglycaemia on the DNA methylation of the insulin promoter with clonal rat insulinoma-derived INS 832/13 β cells. When the cells were cultured under hyperglycaemic conditions (16.7 mmol/L glucose) for 72 h, the DNA methylation of two of the CpG sites (− 1057 and + 58) in the insulin gene promoter was found to be increased in β cells [18].
The effects of overnutrition on the DNA methylation status of the rat insulin-1 (Ins1) gene promoter were evaluated using a rat pancreatic insulin-producing β cell line (INS-1 cells) cultured under normal (11.2 mmol/L) or high (22.4 mmol/L) glucose concentrations for 14 days and Zucker diabetic fatty rats. The investigators found that the high glucose concentration increased Dnmt1 mRNA expression levels and activity. This resulted in the increased DNA methylation of the five CpG sites within the Ins1 promoter, including the CRE, and the suppression of Ins1 mRNA expression, all in a glucose concentration and time-dependent manner [12]. In addition, increased Ins1 promoter methylation was observed in pancreatic islets isolated from the Zucker diabetic fatty rats. Furthermore, insulin promoter-driven reporter gene (luciferase) activity was significantly suppressed by the artificial methylation of the Ins1 promoter. Ins1 mRNA suppression by high glucose concentration was significantly improved by a DNA methylation inhibitor. Moreover, the experimental high glucose conditions were found to significantly decrease TET activity and increase DNA methyltransferase activity. Metformin, the first line of T2DM treatment, has been shown to significantly suppress insulin promoter DNA methylation and upregulate Ins1 mRNA expression [12]. Studies have also found reduced DNA CpG methylation at the Ins1 promoter during the trans differentiation of fibroblasts, pancreatic exocrine cells, and WB-F344 (WB) rat liver epithelial cells to β cells [2].
Aristaless-related homeobox
The aristaless-related homeobox (ARX) gene is an X-linked transcription factor that functions in humans and mice to regulate the development of the pancreas among various other tissues. In the mouse pancreas, Arx has been found to be expressed throughout all stages of pancreatic development [19]. As such, Arx is first observed in the pancreatic anlage, followed by the differentiating precursors of the pancreatic endocrine cells and, finally, the ensuing α cells [20]. Arx deficiency in mice causes the loss of mature endocrine α cells, with a concomitant elevation in the numbers of δ cells and β cells [19] to maintain the total mass of the endocrine portion of the pancreas [21]. Humans with ARX-null mutations display a loss of α cells, indicating the essential role of ARX in mammalian α cell specification and differentiation [20].
A study, using a mouse pancreatic α cell line (α-TC1) and a mouse pancreatic insulinoma β cell line (Min6), was conducted to investigate the methylation of the CpG sites within α cells and β cells, respectively. The CpG-rich sites in the regulatory region of the lineage determination of the Arx gene were divided into two main groups, namely, UR1 (CpG-rich sites within the proximal promoter and close to the TSS) and UR2 (CpG-rich sites 2 Kb upstream of the TSS). The authors found that the majority of the CpG sites within the UR2 region were methylated in the β cells but remained unmethylated in the α cells [22].
Furthermore, in studies using mice and the Cre/loxP system, Dnmt1-deficient β cells have been shown to gradually convert to α cells. This alteration appears to be associated with the Dnmt1 small interfering RNA (siRNA) on Min6 cells, along with the methylation status of the Arx UR2 region. This region is normally methylated (i.e., silenced Arx) in mature β cells but becomes hypomethylated (i.e., expressed Arx) in mature α cells and mature Dmnt1-deficient β cells. The methylated Arx UR2 region has been found to bind to MeCP2, which then recruits more proteins, such as Prmt6, a histone H3R2 methylase, to further suppress Arx expression. Although the methylation status of Arx has not yet been definitively linked with T2DM pathogenesis, an association has been suggested [22].
Pancreatic and duodenal homeobox-1
The pancreatic and duodenal homeobox-1 (PDX-1) is a transcription factor necessary for the differentiation of all pancreatic cell lineages. PDX-1 expression is maintained at low levels in exocrine cells, where its function is yet to be fully understood. It is expressed at high levels in β cells, where it promotes the transcription of the insulin gene (i.e., insulin synthesis) [23].
The DNA methylation and mRNA expression levels of the PDX-1 gene appear to play a crucial role in the differentiation of β cells. This process was analysed in the clonal rat insulinoma-derived INS 832/13 β cell line and human pancreatic islets from T2DM and non-T2DM donors. In comparison with non-T2DM, T2DM-derived pancreatic islets were shown to have a reduced PDX-1 mRNA expression. This reduction was considered to be the result of the hypermethylation of 10 CpG sites located in the PDX-1 distal promoter and enhancer regions. Accordingly, the reduction in PDX-1 mRNA was positively correlated with GSIS and insulin mRNA expression. Furthermore, the hypermethylation of the CpG sites was negatively correlated with the PDX-1 expression, a finding supported by the reduced expression of the reporter gene in clonal β cells. Although the data indicated that the hypermethylation in β cells from both humans and the cell line was due to hyperglycaemia, only in the cultured β cell line was the hyperglycaemia associated with significant increase in DNMT1 expression [24].
Glucagon-like peptide-1 receptor
Glucagon-like peptide-1 receptor (GLP-1R) is widely distributed in pancreatic islets [25]. The activation of GLP-1R in the β cells serves to enhance GSIS in a short-term manner. Although it cannot be directly monitored in humans, the continuous activation of GLP-1R is believed to increase β cell neogenesis and proliferation and overall insulin synthesis [26].
T2DM studies in humans and rats have indicated reduced GLP-1R expression in pancreatic islets, although whether this reduction is due to a change in the DNA methylation status of the GLP-1R gene and/or other mechanisms was initially unclear. Further analysis using pancreatic islets from T2DM and non-T2DM human donors was conducted to determine the mRNA expression levels of MECP2, DNMT1, DNMT3A, and DNMT3B, along with the DNA methylation status of 12 CpG sites (five upstream and seven downstream) associated with the GLP-1R TSS. Two of these CpG sites, at positions + 199 and + 205 bp from the TSS, were further analysed as a single CpG unit due to GLP-1R sequence characteristics [25]. This analysis showed decreased GSIS and reduced GLP-1R expression in pancreatic islets from the T2DM donors compared to non-T2DM donors. In addition, the CpG unit had a small increase in the level of DNA methylation in the T2DM islets compared with the non-T2DM islets. However, this increase was considered too small to persist after correction for multiple testing, and it did not demonstrate a significant correlation with GLP-1R mRNA expression. A trend toward reduced DNMT3A expression in the T2DM islets compared with the non-T2DM islets was also suggested. However, no difference was found between the T2DM and non-T2DM islets in terms of MECP2, DNMT1, and DNMT3B expression levels [25].
Furthermore, the DNA methylation status of the GLP-1R promoter was analysed using isolated α cells and β cells from the pancreatic islets. The DNA methylation level of the GLP-1R CpG site at position − 376 was significantly higher in α cells than in β cells, and this was found to be inversely correlated with the GLP-1R expression [25].
Peroxisome proliferator-activated receptor gamma coactivator-1 alpha
The peroxisome proliferator-activated receptor gamma coactivator-1 alpha (PPARGC1A) is a transcriptional coactivator of various transcription factors and nuclear receptors [27], including the peroxisome proliferator-activated receptor gamma (PPARG or PPARγ) [28]. PPARGC1A controls the activity of a wide range of transcription factors functioning in various cellular and metabolic processes, such as glycogenolysis, gluconeogenesis, fatty acid oxidation, oxidative phosphorylation, and glucose transport [29]. PPARGC1A is expressed predominantly in tissues with high energy demand including the skeletal muscle, pancreas, and liver [28].
A study was conducted to investigate whether the expression of PPARGC1A gene is altered in T2DM pancreatic islets and whether this alteration (if present) is due to DNA methylation (among other factors). In addition, the effect of the experimental downregulation of PPARGC1A on insulin secretion in human islets was investigated using human islets from T2DM and non-T2DM organ donors. The findings show that PPARGC1A mRNA expression was significantly reduced in T2DM islets compared with the non-T2DM islets. Furthermore, this study found a two-fold increase in the DNA methylation of the PPARGC1A promoter (four CpG sites analysed) in the T2DM islets, with a trend towards an inverse correlation between the level of PPARGC1A mRNA and PPARGC1A promoter methylation expression. In addition, the reduced PPARGC1A mRNA expression in the T2DM islets was positively correlated with reduced GSIS in the islets. These findings were confirmed by the experimental downregulation of PPARGC1A expression in human islets by siRNA, which resulted in the reduced expression of insulin mRNA and reduced insulin secretion, thus demonstrating a link between PPARGC1A expression level and GSIS [30].
Blood
FOS-like antigen 2
In mice osteoblasts, the transgenic expression of FOS-like antigen 2 (Fosl2) leads to decreased body weight and increased bone mass, along with decreased serum levels of glucose, improved insulin sensitivity, and improved glucose tolerance. These findings indicate that Fosl2 expression plays a role in the positive regulation of insulin and glucose metabolism [29]. A detailed investigation into the blood DNA methylation status and expression level of the FOSL2 gene found that eight CpG units within the FOSL2 gene had higher methylation rates in T2DM patients, resulting in a significant reduction in FOSL2 mRNA and protein levels compared with normal glucose tolerance (NGT) group [31].
Protein tyrosine-protein phosphatase non-receptor type 1
Protein tyrosine phosphatases non-receptor type 1 (PTPN1) inactivates the transduction of the insulin signal cascade by dephosphorylating phosphotyrosine residues in insulin-signalling molecules [32]. Research into the association between T2DM susceptibility and the DNA methylation status of the PTPN1 gene found a significant correlation between the risk for T2DM and the hypermethylation of the eight CpGs in the PTPN1 promoter. A further breakdown analysis by gender showed that this correlation was female specific, as no significant differences were observed between T2DM males and control males in terms of PTPN1 methylation [33].
Transcription factor 7-like 2
The transcription factor 7-like 2 (TCF7L2) gene plays an important role in various processes, including the activation of target genes in the Wnt signalling pathway [34], pancreatic β cell proliferation, and glucose homeostasis [35]. In addition, TCF7L2 is the most significant and consistently replicated gene associated with an increased risk of T2DM [34]. Certain TCF7L2 SNPs have been shown to be associated with increased T2DM risk [35]. Investigation into the DNA methylation profile of the TCF7L2 gene promoter found a correlation between the methylation of specific CpGs, fasting glucose, total cholesterol, and LDL cholesterol. In addition, 13 out of the 22 TCF7L2 promoter CpGs analysed were differentially methylated in the T2DM group compared with the control. However, the overall methylation pattern of the TCF7L2 promoter did not show a clear differential pattern related to T2DM [36].
Solute carrier family 30 member 8
Pancreatic β cells are rich in zinc, which is essential for the zinc–insulin crystallisation that occurs within insulin-secretory vessels [37]. Solute carrier family 30 member 8 (SLC30A8) encodes the ZnT 8 (ZnT-8) protein, which is expressed in the insulin secretory granules of pancreatic β cells. ZnT-8 co-localises with insulin granules in the INS-1 pancreatic β cell line [38]. Genetic variation in the SLC30A8 gene is associated with increased T2DM risk [39]. The genetic association between the SLC30A8 gene and the increased risk of T2DM and diabetic nephropathy (DN) was investigated, by examining the DNA methylation status of six CpG sites in the SLC30A8 promoter using blood samples. The methylation level of the SLC30A8 promoter was found to be higher in T2DM patients compared with NGT individuals. There was no significant difference in DNA methylation between T2DM with or without DN[40].
Insulin-like growth factor-1
Insulin-like growth factor-1 (IGF-1) is involved in metabolism of carbohydrates, proteins, and lipids. Furthermore, IGF-1 has known insulin-like effects, as it has been experimentally demonstrated that the administration of recombinant human IGF-1 improves insulin sensitivity and reduces blood glucose levels in patients with T2DM [41]. Research into the DNA methylation status of IGF-1 using blood samples of T2DM found one CpG site with increased DNA methylation in the T2DM patients. Moreover, IGF-I serum levels were reduced in the T2DM patients compared with the NGT individuals [42].
Insulin-like growth factor-binding protein 1
Insulin-like growth factor-binding protein 1 (IGFBP-1) is believed to play a role in glucose metabolism through its regulatory effect on IGF-1. Evidence has suggested an inverse correlation between endogenous IGFBP-1 levels and free IGF-I levels, with the injection of exogenous IGFBP-1 serving to reduce circulating glucose and free IGF-I levels. Furthermore, the insulin resistance state is associated with the reduced synthesis and circulating level of IGFBP-1. Free IGF-I levels have been shown to be elevated, whereas IGFBP-1 levels are reduced in patients with T2DM [43]. Analysis of DNA methylation status of IGFBP-1 and its association with serum IGFBP-1 levels in T2DM found that the DNA methylation levels of six CpG sites were higher in T2DM patients compared with the control individuals. Newly diagnosed patients with T2DM with a familial history of the disease showed higher IGFBP-1 DNA methylation levels compared with those without a familial history of the disease. These findings suggest that increased IGFBP-1 DNA methylation levels and decreased IGFBP-1 serum levels are features of newly diagnosed T2DM [44].
Insulin-like growth factor-binding protein 7
Insulin-like growth factor-binding protein 7 (IGFBP-7) has low affinity for IGF-1, but binds insulin with a higher affinity. A study found significantly greater IGFBP-7 serum levels in T2DM patients undergoing haemodialysis compared with non-diabetic haemodialysis patients [45]. Studies on the DNA methylation status of IGFBP-7 gene and its association with serum levels in T2DM found that three CpG sites had increased DNA methylation in men newly diagnosed with T2DM compared with control individuals. However, IGFBP-7 serum levels were similar among all the groups (newly diagnosed T2DM, treated T2DM, and control subjects) and did not show a correlation with IGFBP-7 DNA methylation levels. In addition, IGFBP-7 serum levels were positively correlated with the serum levels of IGFBP-1, which has been shown to be an insulin production marker, in T2DM newly diagnosed men but not women. Thus, the authors concluded that low IGFBP-7 may be associated with T2DM insulin resistance [46].
B cell CLL/lymphoma 11A
B cell CLL/lymphoma 11A (BCL11A) gene is believed to be involved in various important processes, including neuronal regulation of hormonal secretion, cell–cell signal transduction [47], expression of human foetal haemoglobin, negative regulation of p53 activity, and lymphopoiesis [48]. A GWAS conducted in non-diabetic participants found that rs243021 SNP in BCL11A gene is associated with reduced insulin secretion and increased fasting glucagon levels, suggesting an increased risk of T2DM [47]. The findings of this study are in agreement with those of a previous study where SNPs in five loci, representing ADAM metallopeptidase with thrombospondin type 1 motif 9 (ADAMTS9, rs4607103), BCL11A (rs10490072), cell division cycle protein 123/calcium/calmodulin-dependent protein kinase 1D (CDC123/CAMK1D, rs12779790), melatonin receptor 1B (MTNR1B, rs10830963), and THADA armadillo repeat containing (THADA, rs7578597), were found to affect β cell function [49].
In another study, the correlation between the DNA methylation of five CpG sites within an intragenic CpG island in the BCL11A gene and T2DM was studied. No significant association was found between BCL11A DNA methylation and either T2DM or non-T2DM individuals. However, when the association analysis was broken down by gender, a significant association between BCL11A DNA methylation and T2DM in males was identified. In addition, a substantial correlation between the mean level of DNA methylation in BCL11A and triglyceride levels in females was found. These findings suggest that BCL11A DNA methylation may directly contribute to T2DM risk in males but may contribute indirectly to T2DM risk in females through its influence on triglyceride metabolism [48].
Glucokinase
The glucokinase (GCK) gene is predominantly expressed in the liver and, to a lesser extent, in the pancreas [50]. Studies have found that one of the main roles of insulin is to stimulate GCK expression to activate relevant glycolytic genes, thus increasing glucose utilisation. Indeed, insulin resistance due to downregulated glucokinase activities in patients with T2DM has been reported, indicating that GCK is a T2DM susceptibility gene [51].
Whether the degree of DNA methylation in 11 CpG sites of the hepatic Gck promoter influences its expression and activity and whether age influences its expression and age-related diabetes were investigated in Wistar rats. The results demonstrate an age-associated reduction in hepatic Gck mRNA expression and glucokinase activity, with an increasing decline with increasing age. Furthermore, the 11 CpG sites analysed showed age-related progressive methylation changes. Treatment with the DNA methyltransferase inhibitor 5-aza-2’-deoxycytidine (5-Aza-CdR) increased Gck expression in the rat primary hepatocytes by fourfold. The study also demonstrated that the age-related increase in hepatic Gck DNA methylation was negatively associated with its expression, suggesting that DNA methylation may have a role in increasing age-dependent susceptibility to hepatic insulin resistance, ultimately leading to diabetes [51].
Further research was conducted to investigate the correlation between the DNA methylation of four CpG sites within an intragenic CpG island in the GCK gene and T2DM. Only CpG4 had increased DNA methylation in T2DM patients compared with the controls. When the association analysis was broken down by gender, it was found to be male specific. In addition, the authors found that the increased CpG4 DNA methylation was also associated with higher total cholesterol concentration in a male-specific manner. The study concluded that the increased CpG4 DNA methylation may contribute to the increased T2DM risk in males [52].
Monocyte chemoattractant protein-1
Monocyte chemoattractant protein-1 (MCP-1) is a chemokine essential for regulating the migration and infiltration of monocytes, natural killer cells, macrophages, and memory T lymphocytes. MCP-1 can be produced either constitutively or in response to cytokines, oxidative stress, or growth factors [53]. A study was conducted to investigate variations in MCP-1 protein serum levels in patients with DM and metabolic syndrome (MetS) and found the serum MCP-1 protein levels were significantly higher in the MetS group. In addition, the DM group had higher MCP-1 levels compared with the MetS group. A correlation analysis found a significantly positive correlation between MCP-1 and waist circumference, the waist–hip rate, body mass index (BMI), triglyceride levels, HOMA-IR, systolic blood pressure, and diastolic blood pressure [54].
As a follow-up, a study was conducted to investigate the blood DNA methylation status of MCP-1 promoter CpG sites and their association with serum MCP-1 and blood glucose levels in patients with T2DM and healthy (control) individuals. The MCP-1 promoter was found to be methylated in 8 out of 32 patients with T2DM and 12 out of 15 control individuals, suggesting that the MCP-1 promoter region was methylated primarily in control individuals compared with the patients with T2DM. In addition, the DNA methylation levels of the MCP-1 promoter correlated negatively with MCP-1 serum levels, fasting blood glucose, glycated haemoglobin A1c (HbA1c), triglyceride levels, and BMI. The study concluded that blood glucose and triglyceride levels may contribute to the hypomethylation of MCP-1 promoter CpG sites, resulting in increased MCP-1 serum levels [55].
Breast cancer 1 DNA repair associated, peroxiredoxin 2, tumour protein p53 and scavenger receptor class A member 3
In an attempt to investigate the role of DNA methylation in the pathogenesis and progression of T2DM, a study analysed the blood DNA methylation changes in 22 genes known to be involved in cellular stress and toxicity, along with the expression levels of methyl-CpG-binding domain protein 2 (MBD2) as a marker of DNA methylation. The study found that MBD2 mRNA expression levels were higher in T2DM patients compared with control individuals. In addition, the authors found that increased T2DM duration was associated with a consistent increase in the DNA methylation fraction of certain tumour suppressor genes, including tumour protein p53 (TP53) and breast cancer 1 DNA repair associated (BRCA1), along with the oxidative stress protection genes scavenger receptor class A member 3 (SCARA3) and peroxiredoxin 2 (PRDX2). This hypermethylation suggested a possible underlying mechanism for increased cancer risk and the disruption of oxidative stress protection in patients with T2DM. The study concluded that the increased MBD2 mRNA expression in the T2DM patients may be responsible for the general dysregulation of DNA methylation resulting from the disease [56].
Protein kinase C epsilon zeta
The protein kinase C epsilon zeta (PRKCZ) is believed to be involved in the translocation of the GLUT4 protein and in the insulin-signalling pathway downstream of PI 3-kinase. Certain SNPs in PRKCZ gene were shown to be associated with T2DM risk in Han Chinese population [57]. A study was conducted to assess the correlation between T2DM and the DNA methylation of nine CpG sites in the promoter of the PRKCZ gene. The authors found that T2DM patients had higher DNA methylation levels compared with controls. Furthermore, T2DM patients had reduced PRKCZ serum levels, indicating reduced expression. These findings suggest that PRKCZ hypermethylation may be involved in the pathogenesis of T2DM [58].
Gastric inhibitory polypeptide receptor
Gastric inhibitory polypeptide (GIP) is an incretin gastrointestinal hormone that function in stimulating the insulin response following an oral glucose challenge. Studies have found that the GIP action is reduced in patients with T2DM, although its secretion seems to be normal. Studies have also demonstrated the role of the gastric inhibitory polypeptide receptor (GIPR) in promoting the function and survival of pancreatic β cells. Therefore, GIPR may play a role in the mediation of insulin secretion following an oral glucose challenge [59]. A study was performed based on the hypothesis that altered GIPR DNA methylation profiles may be involved in the reduced GIP action observed in patients with T2DM. The study evaluated differences in DNA methylation of 13 CpG sites of the GIPR promoter using blood. The authors found that GIPR promoter was hypomethylated in patients with T2DM compared to the control individuals. The mean methylation levels of the GIPR promoter were negatively correlated with fasting glucose and HOMA-IR in the patients with T2DM, where the reduced DNA methylation of the GIPR promoter was associated with increased HOMA-IR and increased fasting glucose levels [60].
Calmodulin 2, calmodulin-dependent protein kinase 1D, and cryptochrome circadian regulator 2
Calmodulin 2 (CALM2) functions in Ca2+ sensing and signal transduction [61]. A specific polymorphism in CALM2 (rs815815) has been associated with the dialysis survival of African-American patients with T2DM-associated end-stage renal disease [62]. The calmodulin-dependent protein kinase 1D (CAMK1D) gene is a member of the Ca2+/calmodulin-dependent protein kinase family, which relays important intracellular calcium signals required for various cellular processes. When calcium influx occurs in hippocampal neurons and granulocyte cells, CAMK1D activates CREB-dependent gene transcription. Considering the role of CREB in β cell survival, along with the role of cytosolic calcium in regulating the exocytosis machinery in β cells, CAMK1D may play a role in β cell insulin secretion [63].
Studies have found that mice carrying null mutations in cryptochrome circadian regulator 2 (Cry2) gene have a number of metabolic abnormalities, including increased insulin sensitivity, impaired glucose tolerance, reduced adipose tissue and body weight, and abnormal circadian rhythmicity. A meta-analysis of 21 GWASs investigating fasting insulin, fasting glucose, HOMA-IR, and homeostatic model assessment of β cell function (HOMA-B) identified several loci, one of which was a particular locus in or near CRY2 (rs11605924), that was associated with fasting glucose [64]. A study investigated the contribution of promoter DNA methylation of CALM2 (four CpG dinucleotides), CAMK1D (nine CpG dinucleotides), and CRY2 (five CpG dinucleotides) to T2DM risk. The study concluded that these three genes do not contribute to T2DM risk [65].
Multiple organs/tissues
Protein tyrosine phosphatase receptor type D
The protein tyrosine phosphatases receptor type D (PTPRD) catalyses the hydrolytic removal of phosphate group(s) from the tyrosine residues of target proteins. This reaction is crucial because the phosphorylation status of protein tyrosine residues is considered an important cellular signal transduction mechanism [66].
A GWAS was conducted to investigate T2DM susceptibility genes in a Han Chinese population. The study identified, a specific SNP (rs17584499) in PTPRD that was associated with increased T2DM risk in the population studied [67]. A replication study of the previous GWAS was conducted to identify the mechanism by which the PTPRD SNP (rs17584499) influences glucose homeostasis. The results of the study revealed that PTPRD SNP (rs17584499) was associated with increased in HOMA-IR over time. The expression of PTPRD in adipose tissue negatively associated with HOMA-IR and fasting insulin levels, thus facilitating the progression to T2DM [68]. Furthermore, another SNP in PTPRD (rs649891) that has been associated with increased T2DM risk in a Mexican population was identified by another GWAS and meta-analysis [69]. However, the exact mechanism by which PTPRD interacts with the insulin-signalling pathway and increases T2DM risk and whether epigenetics is involved remain unclear [70].
As a follow-up study, an evaluation of DNA methylation-induced changes in the PTPRD expression in T2DM and non-T2DM individuals was conducted. This study used blood samples from patients with T2DM and healthy (control) individuals, along with the human liver carcinoma cell line HepG2 and liver tissue from male KK and KK-Cg-Ay/J mice of three age groups. The age groups of the mice consisted of 6 weeks old (representing the early disease stage), 16 weeks old (representing the middle disease stage), and 42 weeks old (representing the late disease stage). The study found that the PTPRD mRNA expression level was lower in patients with T2DM compared with that in the controls. In addition, the PTPRD mRNA expression was correlated with the duration of T2DM in these patients, in whom there was a general decrease in the PTPRD mRNA expression with increasing T2DM duration. When the human PPARG2 was overexpressed in HepG2 cells, it induced the insulin receptor and PTPRD overexpression. When PTPRD was knocked down, the insulin receptor was downregulated, indicating that PTPRD may be involved in the insulin-signalling pathway through PPARG2 [70].
The study also demonstrated that the expression of the Ptprd protein was significantly reduced in late-stage diabetic mice compared with the early-stage, middle-stage, and control mice. Similar to humans, the mRNA expression level of Ptprd decreased with the increasing disease stage (duration), and the Ptprd promoter was found to be hypermethylated in the middle- and late-stage diabetic mice but not early-stage mice. Further analysis revealed that the Dnmt1 expression was significantly higher in the late-stage mice. In contrast to the results obtained in the mice, patients with T2DM from all disease durations showed PTPRD promoter hypermethylation. In addition, the DNMT1 mRNA expression was found to be higher in patients with T2DM compared with the controls. Collectively, the findings of the study suggest that DNMT1 caused PTPRD DNA hypermethylation and silenced insulin signalling in patients with T2DM [70].
Growth factor receptor-bound protein-10
The growth factor receptor-bound protein-10 (GRB10) is an adapter protein that functions as a down regulator of the insulin receptor through its interaction with various signalling molecules and receptor tyrosine kinases, thus it has been implicated in T2DM pathogenesis. GRB10 is expressed in a variety of tissues, with the highest expression in pancreas. In addition, GRB10 is imprinted in a parent-of-origin manner in various tissues [71].
A large-scale meta-analysis for GSIS during oral glucose tolerance test (OGTT) was conducted on non-diabetic individuals. The analysis identified impaired β cell function-associated variants in the GRB10 gene. The study then investigated the contribution of GRB10 risk alleles to T2DM risk, along with their transmission patterns and the effect they may have on glucose and insulin levels during OGTT. The methylation status and gene expression of GRB10 was also analysed in human pancreatic islets from T2DM and non-T2DM donors and peripheral blood lymphocytes from T2DM. The mechanisms of GRB10 effect on pancreatic α and β cell functions was also analysed in human pancreatic islets and in rat insulinoma INS-1 cells [71].
Interestingly, the study associated a specific GRB10 variant, namely, the A-allele of rs933360, with decreased insulin sensitivity, non-affected GSIS, increased fasting plasma glucose level and increased risk of T2DM if inherited from the father and an enhanced insulin sensitivity, reduced GSIS, and reduced fasting plasma glucose level if inherited from the mother. The results also show an allelic imbalance and tissue-specific differences in GRB10 DNA methylation levels in the human pancreatic islets compared to the peripheral blood lymphocytes with higher GRB10 DNA methylation in human pancreatic islets. The disruption of GRB10 in human pancreatic islets resulted in reduced insulin and glucagon expression and secretion and significant reduction in the number of viable pancreatic islets. The disruption of Grb10 in rat insulinoma INS-1 832/13 cell line resulted in reduced GSIS. Taken together, these findings suggest that GRB10 tissue-specific DNA methylation, within the context of imprinting, contributes to T2DM pathogenesis through the modulation of glucose metabolism, placing more emphasis on the need to investigate whether T2DM-associated risk alleles are maternally or paternally inherited [71].
Peroxisome proliferator-activated receptor gamma and pyruvate dehydrogenase lipoamide kinase isozyme 4
The ability of a system to alternate between glucose and lipid oxidation as a fuel source based on the nutrient availability is termed as metabolic flexibility. Failure of metabolic flexibility is often accompanied by a number of symptoms such as insulin resistance. The competition between glucose and fatty acid oxidation occurs at the pyruvate dehydrogenase complex (PDC) level, which is normally active during healthy and well-fed state. Pyruvate dehydrogenase kinase (PDK), of which PDK4 is an isozyme, works to supress PDC when glucose is scarce, to maintain energy homeostasis. The inappropriate suppression of PDC activity may be involved in the development of metabolic diseases [72].
A study was conducted to investigate the DNA methylation of certain candidate genes and whether differential levels of DNA methylation in the blood could be used as biomarkers for T2DM and/or MetS. The candidate genes were fat mass and obesity-associated (FTO), KCNJ11, potassium voltage-gated channel subfamily Q member 1 (KCNQ1), PDK4, PDX-1, paternally expressed gene-3 (PEG3), PPARG, and stearoyl-coenzyme A desaturase-1 (SCD1). These genes were chosen based on their functional relevance to certain metabolic processes, including glucose metabolism, β cell maturation and pancreatic development, insulin secretion, adipogenesis, and fatty acid storage and metabolism, along with their potential contribution to the development of various metabolic diseases. Indeed, five of these candidate genes (FTO, KCNQ1, PDK4, PDX-1, and PPARG) have previously been identified to have differential DNA methylation levels in patients with T2DM. The study utilised peripheral blood leukocytes from three groups of individuals: those with T2DM and MetS, those with T2DM only and healthy (control) individuals. All of the patients diagnosed with T2DM and MetS (first group) had central obesity [73].
Although a trend toward significance was observed for PEG3, the study did not detect any significant differential gene-specific DNA methylation between the patients and controls for any of the other candidate genes. However, a trend toward a positive correlation was detected between HDL cholesterol levels, which can be downregulated by p53 and the methylation of the p53 mediator PEG3. When the patients were divided into T2DM and MetS subgroups and single CpG loci were analysed, differential DNA methylation levels between the groups were observed for 4 out of the 42 loci tested. The four CpG loci were found to be located within the promoters of FTO, KCNJ11, PDK4, and PPARG [73].
The authors of this study also found that the CpG locus in KCNJ11 had significantly higher methylation levels in MetS patients compared with the patients with T2DM and controls. The authors speculated that the elevated DNA methylation in this locus may mimic genetic KCNJ11 defects. In addition, the CpG locus in the PPARG promoter was found to have higher methylation levels in patients with T2DM compared with controls [73].
The study demonstrated that the differentially methylated CpG locus in PDK4 also showed decreased methylation levels in T2DM and MetS patients compared with the control group [73]. This finding is consistent with a previous study that reported an increase in PDK4 mRNA expression in the skeletal muscle of patients with T2DM due to PDK4 promoter hypomethylation [74].
ATP-binding cassette subfamily G member 1, sterol regulatory element-binding transcription factor 1, phosphoethanolamine/phosphocholine phosphatase 1, and thioredoxin-interacting protein
ATP-binding cassette subfamily G member 1 (ABCG1) is a cholesterol transporter important for maintaining cellular cholesterol homeostasis in pancreatic β cells [75]. The phosphoethanolamine/phosphocholine phosphatase 1 (PHOSPHO1) gene encodes a hydrolase enzyme (phosphatase) that is involved in vascular and skeletal mineralisation. Indeed, T2DM is a common cause of cardiovascular calcification. As such, PHOSPHO1 is a candidate marker for T2DM-linked CVD [76, 77]. Suppressor of cytokine signalling 3 (SOCS3) is a member of the intracellular, cytokine-inducible SOCS family that functions in regulating the JAK/STAT pathway in various cell types. SOCS3 acts as a regulator of insulin signalling [78].
The sterol regulatory element-binding transcription factor 1 (SREBF1) gene encodes the sterol regulatory element-binding transcription factor proteins SREBP-1a and SREBP-1c, which function in the regulation of fatty acid and cholesterol synthesis. The skeletal muscle and adipose tissue from patients with T2DM have demonstrated reduced SREBP-1c expression, suggesting a possible contribution of low levels of SREBP-1c towards insulin resistance. Furthermore, several studies have associated variations in the SREBF1 gene with increased T2DM risk [79]. Thioredoxin-interacting protein (TXNIP) plays an important role in the regulation of the cellular redox status. Studies have shown that hyperglycaemia causes glucose toxicity (i.e., β cell dysfunction and apoptosis), with TXNIP considered a key mediator of these effects primarily through the mitochondrial death pathway. Moreover, TXNIP overexpression has been shown to cause β cell apoptosis. In DM, the TXNIP expression is increased in β cells, so increased TXNIP expression may be a key player in the pathogenesis of DM. In support of this notion, the deletion and mutation of Txnip have been found to protect against diabetes in a variety of T1DM and T2DM mouse models [80].
A nested case–control study investigated blood DNA methylation levels in Indian Asians (the discovery group) and Europeans (the replication group) to determine if there was an association with T2DM risk. The participants were identified from 25,372 participants in the 8-year follow-up London Life Sciences Prospective Population study (LOLIPOP). The result of the investigation reported five T2DM-associated DNA methylation CpG loci in blood DNA, namely, ABCG1, PHOSPHO1, SOCS3, SREBF1, and TXNIP [81].
A follow-up study was then conducted to examine the potential use of these five loci to predict the future occurrence of T2DM in subjects from the family-based Botnia prospective study. The study also investigated whether these five loci and, by extension, their associated genes, displayed altered DNA methylation and gene expression in the primary T2DM target tissues, including adipose tissue, pancreatic islets, liver and skeletal muscle, in T2DM and non-T2DM individuals. The study utilised blood samples from T2DM and non-T2DM participants from the Botnia prospective study, in addition to blood, skeletal muscle and adipose tissue from monozygotic twins discordant for T2DM, pancreatic islets from T2DM and non-T2DM donors and human liver DNA methylation data from the Kuopio Obesity Surgery Study (KOBS) [77].
The investigators found that the blood DNA methylation of the PHOSPHO1 locus (cg02650017) was associated with a 15% decreased risk of T2DM, whereas the methylation of the ABCG1 locus (cg06500161) was associated with a 9% increased risk for future T2DM. Blood DNA methylation at SREBF1 (cg11024682), TXNIP (cg19693031), and SOCS3 (cg18181703) was not associated with T2DM risk in subjects from the Botnia prospective study. In addition, the blood DNA methylation levels of the PHOSPHO1 locus showed a positive correlation with HDL levels. PHOSPHO1 DNA methylation level was decreased in the skeletal muscle from the T2DM subjects, although this decrease did not result in an altered gene expression. The blood DNA methylation of the ABCG1 locus showed a positive correlation with fasting insulin, HbA1c, BMI, and triglyceride levels in the Botnia subjects. Moreover, ABCG1 DNA methylation level was increased in the blood and adipose tissue of T2DM subjects, while its expression altered in muscle tissue from T2DM subjects [77].
In addition, the blood DNA methylation levels of the SREBF1 locus (cg11024682) showed a positive correlation with age, BMI, fasting glucose, and HbA1c in subjects from the Botnia prospective study. Furthermore, SREBF1 DNA methylation was increased in T2DM pancreatic islets, while its expression was found to be altered in a diabetic liver and muscle tissues. The blood DNA methylation of the SOCS3 locus (cg18181703) showed a negative correlation with BMI and age. Moreover, SOCS3 DNA methylation demonstrated a positive correlation with its expression in human pancreatic islets, but correlated negatively with its expression in the adipose tissue. The blood DNA methylation levels of the TXNIP locus (cg19693031) showed a negative correlation with triglyceride levels. In addition, TXNIP DNA methylation was found to be decreased in the blood, skeletal muscle, and pancreatic islets from the T2DM subjects, while its expression altered in the muscle tissue of subjects with T2DM [77].
The authors also found that the blood DNA methylation levels of the CpG loci at SOCS3 and SREBF1 correlated with the degree of methylation in the adipose tissue. The authors concluded that DNA methylation biomarkers in blood might be used as surrogate biomarkers when the target tissue is inaccessible [77]. An epigenome-wide association study (EWAS) investigating the association between DM and blood DNA methylation in ischemic stroke patient cohorts found that cg19693031 CpG (TXNIP) DNA hypomethylation was associated with T2DM. The authors also found that TXNIP DNA methylation was inversely associated with HbA1c levels in patients with T2DM with a poor control of their blood glucose levels [82].
Genome-wide methylation studies
Pancreas
CpG-SNPs
Although previous studies have identified approximately 40 T2DM-associated SNPs, the exact mechanism by which these SNPs affect their target genes in a way that increases the risk of T2DM remains unclear. One suggested mechanism by which SNPs change gene expression is through epigenetics via the introduction or removal of CpG sites, which are potential DNA methylation sites. In addition, these CpG-SNPs may affect the expression of their target gene(s) through other mechanisms, such as interfering with the binding of certain proteins [83] or affecting intragenic DNA methylation through exonic splicing enhancers. Previous studies have shown that intragenic DNA methylation plays a key role in the regulation of alternative splicing [84].
Few studies have explored the role of CpG-SNPs in T2DM pathogenesis. A study was conducted to investigate whether any of the 40 previously reported T2DM-associated SNPs serve to introduce or remove potentially important DNA methylation sites, including CpG sites. The study also investigated whether these CpG-SNPs were associated with differential DNA methylation levels, which may induce changes in the hormone secretion of human pancreatic islets via changes in gene expression and/or alternative splicing events. The authors utilised human pancreatic islet tissue from non-T2DM donors [83].
The findings of the study indicated that 19 of the 40 (48%) T2DM-associated SNPs either introduced or removed a CpG site. Of these, four were determined to be coding SNPs, while five were considered intronic and the other ten were intergenic. DNA methylation data were successfully generated for 16 of the 19 CpG-SNP loci and identified the candidate genes, adenylate cyclase 5 (ADCY5, rs11708067), cyclin-dependent kinase inhibitor 2A (CDKN2A, rs564398), dual specificity phosphatase 8 (DUSP8, rs2334499), dual specificity phosphatase 9 (DUSP9, rs5945326), PPARG (rs1801282), insulin receptor substrate 1 (IRS1) (rs7578326), and wolframin ER transmembrane glycoprotein (WFS1, rs1801214) (CpG-SNP risk alleles which removed a CpG site), CDK5 regulatory subunit-associated protein 1-like 1 (CDKAL1, rs7754840), coiled-coil-helix-coiled-coil-helix domain-containing 2 pseudogene 9 (CHCHD9, rs13292136), haematopoietically expressed homeobox (HHEX, rs5015480), high-mobility group AT-hook 2 (HMGA2, rs1531343), KCNQ1 (rs2237895), SLC30A8 (rs13266634), serine racemase (SRR, rs391300), TCF7L2 (rs7901695), and tetraspanin 8 (TSPAN8, rs7961581) (CpG-SNPs which introduced a CpG site) in human islets. DNA methylation data were then successfully generated for a total of 22 CpG sites located near ADCY5, CDKN2A, DUSP9, HHEX, HMGA2, KCNQ1, PPARG, SLC30A8, TCF7L2, and WFS1, all of which were found to be T2DM-risk SNPs. However, DNA methylation data could not be generated for the remaining three T2DM-associated CpG-SNPs, namely, CDC123 (rs12779790), KCNJ11 (rs5219), and zinc finger BED-type containing 3 (ZBED3, rs4457053) due to design/technical issues [83].
From this study, all of the 16 T2DM-associated CpG-SNPs that generated successful data were associated with CpG-SNP sites of differential DNA methylation in the human islets. In addition, six CpG-SNP loci, representing ADCY5, CDKN2A, HMGA2, KCNQ1, TCF7L2, and WFS1, were associated with differential DNA methylation of the surrounding CpG sites. Furthermore, some of the differentially methylated T2DM-associated CpG-SNP sites in the study were associated with gene expression, alternative splicing events, and hormone secretion in human islets. For example, carriers of the CpG-SNPs rs391300 (SRR) and rs5945326 (DUSP9), which showed increased DNA methylation, had decreased mRNA expression of replication protein A1 (RPA1) and arginine vasopressin receptor 2 (AVPR2), respectively, in human islets [83].
Furthermore, the T2DM-associated CpG-SNPs located in CDKAL1, SLC30A8, TCF7L2, and WFS1 were found to be associated with alternative splicing events in their respective genes in human islets. Moreover, some of the differentially methylated T2DM-associated CpG-SNP sites were found to be associated with hormone secretion in the human islets, where CpG-SNPs in ADCY5 (rs11708067) and KCNQ1 (rs2237895) were associated with glucagon secretion, whereas those of ADCY5 (rs11708067) and HHEx (rs5015480) were associated with insulin secretion, and that of CDKN2A (rs564398) was associated with insulin content. The study also found that the 19 identified T2DM-associated CpG-SNP sites were in strong linkage disequilibrium with 295 other SNPs, 91 of which were CpG-SNPs. Collectively, the study suggests that the introduction and/or removal of CpG sites should be considered a molecular mechanism through which T2DM-associated SNPs may contribute to the pathogenesis of T2DM [83].
Similarly, another study was conducted to investigate the association between a particular WFS1 CpG-SNP (rs1801214-T allele) located in the coding sequence and T2DM risk in an Iranian population. The study utilised blood samples and found that this specific CpG-SNP, which removes a CpG site, was significantly associated with lower T2DM risk in this population. However, the authors did not perform any measurements of WFS1 expression, nor did they investigate its methylation status [85].
Cyclin-dependent kinase inhibitor 1A, Exocyst complex component -3 like 2, Phosphodiesterase-7B, and Septin-9
A genome-wide DNA methylation profiling analysis was performed to assess the human pancreatic islet DNA methylome and the epigenetic basis of T2DM pathogenesis. The study assessed the transcriptome and DNA methylation of 479,927 CpG sites utilising pancreatic islets from T2DM and non-diabetic donors. They also utilised INS-1 832/13 β cells and αTC 1-6 cells for expression and functional analyses. A total of 1649 CpG sites were identified to be differentially methylated in the T2DM islets with ≥ 5% differences in methylation, of which 561 were considered intergenic, and 1008 were located near or in 853 genes. Of the 853 genes, 102 were found to be differentially expressed in the T2DM islets [86]. In addition, 26 genes (~ 25%) were considered to be positively correlated with DNA methylation, where DNA hypomethylation was associated with reduced gene expression. By contrast, 77 genes (~75%) had an inverse relationship with DNA methylation, where DNA hypomethylation was associated with elevated gene expression. The authors then performed KEGG pathway analysis on these 853 differentially expressed genes and identified MAPK signalling pathway, pathways in cancer, ECM-receptor interaction, focal adhesion, and axon guidance, and regulation of actin cytoskeleton as some of the pathways involved [86].
The authors identified 75 genes exhibiting decreased DNA methylation and increased gene expression in T2DM pancreatic islets compared to non-diabetic islets. The authors then selected three of these genes and overexpressed them in clonal β cells, to gain better understanding on the mechanisms by which these genes may contribute to impaired β cell function and T2DM development and to model the situation in humans. The genes septin-9 (Sept9), cyclin-dependent kinase inhibitor 1A (Cdkn1a), and phosphodiesterase-7B (Pde7b) were selected based on their potential role in islet function and DM, along with their differential DNA methylation in multiple CpG sites and differential expression in T2DM islets. Overexpression of Sept9 had no significant effect, while overexpression of Pde7b and CDKN1A significantly reduced GSIS in clonal β cells. Moreover, increased Cdkn1a expression decreased β cell proliferation. Then, the authors overexpressed these three genes in clonal α cells to examine the effect on α cells. Overexpression of Sept9 produced a significant increase in glucagon expression, while overexpression of Pde7b and Cdkn1a increased glucagon release [86].
In this study, exocyst complex component 3-like 2 (EXOC3L2) demonstrated increased DNA methylation and reduced expression in T2DM islets compared to non-diabetic islets. The authors silenced Exoc3l2 in clonal β cells, to model the decreased EXOC3L2 expression in human T2DM islets, and to examine the effect on β cell exocytosis. The authors found that silencing Exoc3l2 reduced β cell exocytosis. The authors concluded that the findings of this study can serve as a reference for human pancreatic islets methylome [86].
Solute carrier family 2 member 2, suppressor of cytokine signalling 2, Parkin RBR E3 ubiquitin protein ligase, nuclear receptor subfamily 4 group A member 3, and phosphotyrosine interacting domain-containing 1
In humans, mutations in solute carrier 2 member 2 (SLC2A2, also known as GLUT2) have been associated with autosomal recessive neonatal diabetes [87]. GWASs have found several SLC2A2 variants that are associated with an increased risk of various disorders, including T2DM, cardiovascular disease, and hypercholesterolemia [88]. Parkin RBR E3 ubiquitin protein ligase (PARK2) has been linked to several diseases, including T2DM [89]. Certain SNPs in PARK2 have been shown to be associated with fasting plasma glucose level and insulin secretion in non-diabetic males. Moreover, downregulation of Park2 in rat insulinoma INS-1 β cells caused significant reduction in intracellular ATP level, GSIS, and intracellular insulin expression [90].
Suppressor of cytokine signalling 2 (SOCS2) function as modulator of growth factor and cytokine signalling. SOCS2 is ubiquitously expressed in pancreatic islets [91]. It has been found that the constitutive production of Socs2 in the β cells of mice causes glucose intolerance and hyperglycaemia by interfering with cytosolic calcium fluxes and proinsulin processing and secretion [92]. Nuclear receptor subfamily 4 group A member 3 (NR4A3) plays a role in the regulation of glucose homeostasis. siRNA-mediated knockdown of NR4A3 in both INS-1 832/13 β cells and human islet was found to prevent cytokine-induced β cell death, whereas overexpression of NR4A3 caused apoptosis [93]. Phosphotyrosine interacting domain-containing 1 (PID1) is a negative regulator of glucose uptake in the muscle and adipose tissue. In addition, under diabetogenic conditions, Pid1 inactivation has been shown to improve hyperinsulinemia and hyperglycaemia by stimulating glucose uptake in the muscle and adipose tissue of Pid1-/- mice [94].
A study was conducted to analyse whole-genome DNA methylation in human pancreatic islets and to identify diabetic islet-specific differentially methylated regions (DMRs). To this end, whole-genome bisulfite sequencing was performed on human islets from patients with T2DM and healthy controls from the Nordic Network for Islet Transplantation. The study identified a total of 25,820 T2DM DMRs, of which 12,124 DMRs exhibited a reduced and 13,696 DMRs exhibited elevated levels of methylation in T2DM islets. The majority of T2DM DMRs were identified in loci with known functions in pancreatic islets, including ADCY5, PDX-1, and TCF7L2. In addition, the study identified 457 genes with DMRs representing significant changes in the gene expression in T2DM islets, including SLC2A2, PARK2, SOCS2, NR4A3, and PID1 [95].
Blood
Dishevelled segment polarity protein 1 and H4 clustered histone 4
Dishevelled segment polarity protein 1 (DVL1) has been shown to play a key role in the canonical and non-canonical Wnt signalling pathways and govern several cellular processes including cell survival, proliferation, differentiation, migration, and stem cell renewal [96]. To investigate the role of epigenetic variations in oxidative stress markers and the subsequent development of T2DM and CVD, a genome-wide blood DNA methylation analysis was conducted along with analysis of ten oxidative stress markers. The results identified a total of 66 CpG sites that had an oxidative stress marker-associated DNA methylation profile, with some demonstrating profiles associated with more than one marker. These CpG sites were found to be enriched in the regulatory regions of the genome. The association of these 66 differentially methylated oxidative marker CpG sites with the incident of T2DM during a 10-year follow-up was also investigated. Hypomethylation at the CpG site in the gene body of DVL1 (cg03465880) and the CpG site in the 3’-UTR of H4 clustered histone 4 (HIST1H4D, cg08170869), was shown to be associated with a higher T2DM risk [97].
Thioredoxin interacting protein, ATP-binding cassette sub-family G member 1, and sterile alpha motif domain-containing 12
A family-based study was conducted to investigate the role of epigenome-wide DNA methylation in the pathogenesis of T2DM in blood from members of a high-risk minority population of Mexican-American families. The methylation levels at 51 CpG sites were identified to be significantly associated with T2DM risk, 24 with HOMA-IR and 19 with fasting blood glucose. The top five CpG sites were cg19693031 (3’UTR of TXNIP), cg06500161 (body of ABCG1), cg07960624 (3’UTR of sterile alpha motif domain-containing 12, SAMD12), cg25217710 (intergenic), and cg08309687 (intergenic). These associations remained significant even after adjustments for BMI. Moreover, these five CpG sites were found to account for 7.8% of T2DM heritability in the study cohort [98].
ATP-binding cassette sub-family G member 1, lysyl oxidase like 2, thioredoxin-interacting protein, solute carrier family 1 member 5, and sterol regulatory element-binding transcription factor 1
Elevated lysyl oxidase like 2 (LOXL2) expression has been associated with tissue fibrosis. As such, ongoing studies are investigating the role of LOXL2 in DM-associated renal fibrosis [99]. A systematic review of recent EWASs linking certain DNA methylation markers to T2DM, HbA1c levels, and fasting blood glucose was conducted. The study replicated the most significant CpG site associations originally identified in the pancreas, liver, peripheral blood, and adipose tissue from the EWASs in blood. The study selected 52 T2DM-associated CpG sites identified in the blood for replication, of which 15 CpG sites demonstrated nominal association with T2DM patients, of which five CpG sites demonstrated a significant association with T2DM after a strict multiple-testing correction. The five CpG sites included cg06500161 (ABCG1), cg24531955 (LOXL2), cg19693031 (TXNIP), cg02711608 (solute carrier family 1 member 5, SLC1A5), and cg11024682 (SREBF1) [100].
ABCG1 and SREBF1 demonstrated hypermethylation, whereas LOXL2, SLC1A5, and TXNIP demonstrated hypomethylation in patients with T2DM compared with healthy controls. However, only the CpG site in ABCG1 showed a significant association with T2DM after adjustment for BMI. Furthermore, the authors analysed 17 T2DM-associated CpG sites identified in the pancreas and liver in blood samples from the study cohort, and found no significant association for these tissue-specific CpG sites in blood samples, suggesting that DNA methylation patterns in blood may not reflect those of metabolically active tissues [100].
Mucosa-associated lymphoid tissue lymphoma translocation protein 1
Mucosa-associated lymphoid tissue lymphoma translocation protein 1 (MALT1) is a signalling protein involved in the regulation of insulin and various energy pathways, along with the development and function of B and T cells. This regulation occurs through the MALTI-induced activation of antigen receptor-mediated lymphocytes via the nuclear factor-κB pathway [101]. A genome-wide methylated DNA immunoprecipitation sequencing (MeDIP-seq) study conducted on blood samples identified a number of hypermethylated T2DM-associated DMRs in a discovery group, and replicated the highest signals in a replication group. The strongest signal was annotated to the MALT1 promoter [101].
Fat mass and obesity-associated
The FTO gene is believed to play a critical role in the regulation of energy homeostasis, lipolysis, and nucleic acid demethylation. Common genetic variants in FTO have been associated with an increased risk of T2DM and obesity [102]. To investigate T2DM-associated DNA methylation, a stepwise study was conducted utilising blood samples. First, a pool-based genome-scale screen identified various previously reported T2DM-associated risk loci to be differentially methylated in T2DM patients. A further in-depth analysis of top-ranking regions was then conducted. The authors found a CpG site (rs1121980) located in the first intron of the FTO gene that displayed small but significant hypomethylation in T2DM compared with the controls. In addition, for every 1% decrease in methylation at the CpG site (rs1121980), the odds of belonging to the T2DM group increased by 6.1% [103].
Interestingly, no correlation was observed between FTO (rs1121980) DNA methylation and BMI as this locus was hypomethylated in obese and non-obese T2DM patients compared with controls, suggesting that the association between FTO (rs1121980) DNA methylation and T2DM may not be mediated through obesity. A follow-up prospective study found a significant hypomethylation of FTO (rs1121980) in young individuals that were later diagnosed with T2DM compared with those who remained T2DM-free. This finding not only confirms the initial finding of FTO (rs1121980) hypomethylation in patients with T2DM but also suggests that this hypomethylation may represent an early T2DM risk factor rather than a consequence of T2DM. Further genomic analyses demonstrated that FTO (rs1121980) colocalises with the binding sites for methylation-sensitive transcriptional regulators and gene enhancers. Taken together, these findings suggest that the T2DM-associated differential methylation of FTO (rs1121980) may function as an early T2DM marker. It also suggests that it may function as a distant regulator of gene expression (transcription). However, whether the gene under regulation is FTO itself or another (neighbouring or distant) gene remains to be determined [103].
Adipose tissue
Insulin receptor substrate 1, potassium voltage-gated channel subfamily Q member 1, peroxisome proliferator-activated receptor gamma, transcription factor 7-like 2, and others
IRS1 plays a role in signal transduction from insulin and insulin-like growth factor-1 (IGF) receptors and is involved in glycometabolism. Variants of IRS1 have been shown to be associated with insulin resistance [104]. The KCNQ1 gene encodes a subunit of a potassium channel that is expressed in human pancreatic β cells, although the role of this channel in insulin secretion is unknown. KCNQ1 has two independent variants, namely, intron 10 and intron 15, that have been associated with an increased risk of T2DM through impaired islet function. However, KCNQ1 regions are considered T2DM risk factors only when they are maternally inherited. Interestingly, knockdown of KCNQ1 in human islets does not alter insulin secretion [105].
By regulating the expression of several genes, PPARG has a number of functions related to the immune response, insulin sensitivity, glucose homeostasis, lipid metabolism, cell fate, and inflammation. In addition, dominant-negative mutations in PPARG have been shown to cause severe hyperglycaemia. Furthermore, PPARG has been found to be downregulated in T2DM. Studies have also found that PPARG agonists improve insulin sensitivity and glucose tolerance in T2DM patients, reducing the need for β cell insulin secretion and hepatic glucose output and ultimately leading to improved glycaemic control [106].
A genome-wide expression and DNA methylation analysis was conducted on the adipose tissue from monozygotic twin pairs discordant for T2DM and independent case–control cohorts. In the adipose tissue from the monozygotic twin pairs, the authors found an increased expression of the genes involved in glycan degradation and inflammation and decreased expression of the genes involved in carbohydrate, lipid, amino acid metabolism, and those involved in oxidative phosphorylation in diabetic verses non-diabetic co-twins. The most differentially expressed genes included C-C motif chemokine ligand 18 (CCL18), ELOVL fatty acid elongase 6 (ELOVL6), fatty acid desaturase 1 (FADS1), glycogen synthase 2 (GYS2), interleukin 1 receptor antagonist (IL1RN), and secreted phosphoprotein 1 (SPP1). These results were successfully replicated in the adipose tissue from an independent case–control cohort of unrelated subjects with T2DM or NGT. Moreover, a number of candidate genes previously linked through GWAS to T2DM and obesity were found to be differentially expressed in the adipose tissue from discordant twins, including PPARG, GLIS family zinc finger 3 (GLIS3) (T2DM), vascular endothelial growth factor A (VEGFA), and IRS1 (obesity) [107].
In addition, the study identified 15,627 differentially methylated CpG sites in the adipose tissue from unrelated subjects with T2DM compared with control subjects. These sites represented 7046 genes, including IRS1, KCNQ1, PPARG, and TCF7L2. Interestingly, 6754 of the 15,627 sites showed increased methylation, whereas the remaining 8873 sites showed decreased methylation in patients with T2DM. In addition, 1410 of the 15,627 sites showed differential DNA methylation levels in the twins discordant for T2DM, and approximately 50% of the genes differentially expressed in the discordant twins were associated with DNA methylation [107].
However, the findings of this study investigating the differential expression and methylation of IRS1 in T2DM contradicted those from a previous single-gene study, in which the association between the DNA methylation of three CpG dinucleotides within the IRS1 promoter and increased risk of T2DM was investigated. In this single-gene study, blood samples from patients with T2DM and healthy (control) individuals were used. Surprisingly, no significant association between IRS1 promoter methylation and increased risk of T2DM was observed. A breakdown analysis by gender also revealed no association with T2DM, although two CpG dinucleotides showed significantly lower methylation levels in males compared with females [104].
Multiple tissues/organs
Musashi RNA binding protein 2
The Mushashi (MSI) protein is an RNA-binding protein that has two isoforms, namely, MSI1 and MSI2, and exerts a regulatory effect on the transcription of the insulin gene and β cell proliferation [108].
A study was conducted to investigate the relationship between glucose homeostasis and differential DNA methylation using the OGTT in a population-based cohort, where all the subjects were recruited from the Korean Genome Epidemiology Study (KoGES). In this study, the subjects were divided into two subgroups, namely, a hyperglycaemic group and a T2DM group, which were then compared with a control group. Blood samples were taken for analysis, and non-tumour human pancreatic islet samples were obtained from pancreatectomy procedures performed at the Asian Medical Centre in Seoul, Korea. The results of the study found a total of 382 differentially methylated positions in the blood samples from the two subgroups, annotating to 280 genes. Among them, three CpG sites were overlapped in the two subgroups. Two of these sites were found to be hypomethylated and were mapped to the MSI2 and CXXC finger protein-4 (CXXC4) genes. A further analysis showed that MSI2 was significantly associated with T2DM, with the DNA methylation of this gene considerably decreased in the blood and pancreatic islets from the T2DM donors. In addition, increased MSI2 DNA methylation was positively correlated with increased insulin sensitivity (QUICKI) and decreased insulin resistance (HOMA-IR) [109].
This differentially hypomethylated CpG site (chr17:55484635) is located within intron 6 of the MSI2 gene. The DNA methylation analysis of the 280 CpG sites in the MSI2 promoter found no significant differences in terms of methylation, and none of the sites were found to be associated with T2DM. From these findings, it was hypothesised that the differential methylation at chr17:55484635 may not be directly related to MSI2 expression. However, no gene expression analysis was conducted in this study to confirm or deny this conclusion. The authors also suggested that the hypomethylation at chr17:55484635 may affect the expression of other genes [109].
A previous study [108] characterised the presence and function of the two Musashi isoforms in pancreatic islets and β cells. Although this study did not address the methylation status of the MSI2 gene, it did find the expression of Msi2 in mouse insulinoma Min6 β cells to be unaffected by either hypoglycaemic or hyperglycaemic conditions. In these cells, MSI2 overexpression significantly downregulated Ins1 and Ins2 gene expressions and blocked MIN6 proliferation, while Msi2 knockdown resulted in the upregulation of Ins2 expression and augmented MIN6 proliferation [108].
Nuclear receptor subfamily 4 group A, member 1
Nuclear receptor subfamily 4 group A, member 1 (NR4A1) is a transcriptional regulator for glucose metabolism present in the skeletal muscle and liver [110].
The evaluation of the role of DNMT1 in T2DM was performed as part of a genome-wide DNA methylation array study, utilising blood samples from patients with T2DM and healthy (control) individuals, in addition to RIN-m5F rat pancreatic β cells, 293T cells, and male KK and KK.Cg-Ay/J mice (as a T2DM animal model). This study found that the promoter of the NR4A1 gene was hypermethylated in the patients with T2DM and resulting in a reduced NR4A1 mRNA expression. Nr4a1 was also found to be hypermethylated in a mouse T2DM model [110].
In addition, the transient transfection of human NR4A1 into the RIN-m5F and 293T cells was shown to induce the inhibition of DNMT1 and the overexpression of the insulin receptor. The short hairpin RNA (shRNA)-mediated knockdown of NR4A1 in RIN-m5F and 293T cells resulted in DNMT1 induction and insulin receptor downregulation in RIN-m5F cells, suggesting that NR4A1 gene is somehow part of the overall epigenetic regulation of the insulin-signalling pathway [110].
The T2DM mouse model showed a reduced activation of pancreatic β cell Dnmt1 and reduced Nr4a1 hypermethylation when treated with the DNMT1 inhibitor aurintricarboxylic acid (ATA). This reduction managed to reverse the changes in Nr4a1 expression and reduce blood glucose levels in the mice. Therefore, the authors of the study hypothesised that these findings may represent a possible novel therapy, through the utilisation of ATA to reverse the impaired NR4A1-dependent insulin signalling and lower the blood glucose levels in patients with T2DM [110].
Other regulatory elements
T2DM-specific DNA methylation profiles are not limited to genes, but rather extend to some non-gene genomic sequences. For example, Alu elements DNA methylation was found to be significantly reduced in blood from T2DM, with Alu DNA hypomethylation directly correlating with high HbA1C and high fasting blood glucose [111]. In addition, lower blood DNA methylation levels of long interspersed nucleotide element 1 (LINE-1) were associated with an increased metabolic risk, independent of the classic risk factors (e.g., age, sex, physical activity, and BMI) [112]. However, a more recent study reported opposite findings, where higher blood DNA methylation levels of LINE-1 were found in T2DM patients compared to control, and lower blood DNA methylation levels of LINE-1 were associated with reduced T2DM risk [113].
Finally, DNA hypermethylation of the micro RNA (miRNA) cluster in the imprinted 14q32 locus was found to substantially downregulate its expression in T2DM pancreatic β cells. The expression of this miRNA cluster was found to play an important role in regulating the expression of two T2DM-relevant genes, namely tumour protein p53-inducible nuclear protein-1 (TP53INP1) and islet amyloid polypeptide (IAPP). These findings indicate an important role for miRNAs in the pathogenesis of T2DM, along with their epigenetic regulation by DNA methylation [114].
Conclusion
In this review, we provide examples of a long list of genes whose altered DNA methylation profiles have been associated with the pathogenesis of T2DM (Table 1). In addition, we discuss the T2DM-related altered DNA methylation profiles associated with these genes. However, altered epigenetic profiles include alterations in other epigenetic modifications, along with the aberrant expression of non-coding RNAs and miRNAs.
Table 1.
List of T2DM-associated genes and their methylation status
| Gene | Species | Organ/tissue | Sample size | Findings | Reference |
|---|---|---|---|---|---|
| Ins | Human | Pancreatic islets | Non-diabetic = 48, T2DM = 9 | Hypermethylation | [18] |
| Rat | INS 832/13 β cell line | ||||
| Rat | INS-1 β cell line | Hypermethylation | [12] | ||
| Rat | Pancreatic islets from Zucker diabetic fatty rats | 10 rats | |||
| Human | Pancreatic islets | Non-diabetic = 34, T2DM = 15 | Hypermethylation | [86] | |
| PDX-1 | Human | Pancreatic islets | Non- diabetic = 55, T2DM = 9 | Hypermethylation | [24] |
| Rat | INS 832/13 β cell line | ||||
| Human | Pancreatic islets | Non-diabetic = 34, T2DM = 15 | Hypermethylation | [86] | |
| PPARGC1A | Human | Pancreatic islets | Non-diabetic = 48, T2DM = 12 | Hypermethylation | [30] |
| FOSL2 | Human | Blood | NGT = 50, T2DM = 50 | Hypermethylation | [31] |
| PTPN1 | Human | Blood | Non-diabetic = 97, T2DM = 97 | Hypermethylation | [33] |
| SLC30A8 | Human | Blood | NGT = 27, T2DM = 161 | Hypermethylation | [40] |
| IGF-1 | Human | Blood | NGT = 242, T2DM = 164 | Hypermethylation | [42] |
| IGFBP-1 | Human | Blood | NGT = 242, T2DM = 164 | Hypermethylation | [44] |
| IGFBP-7 | Human | Blood | NGT = 100, T2DM =240 | Hypermethylation | [46] |
| GCK | Human | Blood | Non-diabetic = 47, T2DM = 47 | Hypermethylation | [52] |
| MCP-1 | Human | Blood | Non-diabetic = 15, T2DM = 32 | Hypomethylation | [55] |
| TP53 | Human | Blood | Non-diabetic = 12, T2DM = 27 | Hypermethylation | [56] |
| BRCA1 | Human | Blood | Non-diabetic = 12, T2DM = 27 | Hypermethylation | [56] |
| SCARA3 | Human | Blood | Non-diabetic = 12, T2DM = 27 | Hypermethylation | [56] |
| PRDX2 | Human | Blood | Non-diabetic = 12, T2DM = 27 | Hypermethylation | [56] |
| PRKCZ | Human | Blood | Non-diabetic = 120, T2DM = 152 | Hypermethylation | [58] |
| GIPR | Human | Blood | Non-diabetic = 93, T2DM = 93 | Hypomethylation | [60] |
| PTPRD | Human | Blood | Non-diabetic = 98, T2DM = 94 | Hypermethylation | [70] |
| Mouse | Liver tissue from KK and KK-Cg-Ay/J mice | ||||
| PDK4 | Human | Blood | Normal = 11, T2DM = 25, MetS = 9 | Hypomethylation (in T2DM+MetS groups vs control) | [73] |
| Human | Skeletal muscle | NG = 79, T2DM = 33 | Hypomethylation | [74] | |
| PPARG | Human | Blood | Normal = 11, T2DM = 25, MetS = 9 | Hypermethylation | [73] |
| ABCG1 | Human | Blood | 19 monozygotic twins discordant for T2DM | Hypermethylation | [77] |
| Human | Adipose tissue | 14 monozygotic twins discordant for T2DM | |||
| Human | Blood | Non-diabetic = 98, T2DM = 100 | Hypermethylation | [100] | |
| PHOSPHO1 | Human | Skeletal muscle | 17 monozygotic twins discordant for T2DM | Hypomethylation | [77] |
| TXNIP | Human | Blood | 19 monozygotic twins discordant for T2DM | Hypomethylation | [77] |
| Human | Skeletal muscle | 17 monozygotic twins discordant for T2DM | |||
| Human | Pancreatic islets | Non-diabetic = 34, T2DM = 15 | |||
| Human | Blood |
Discovery: BASICMAR_1 cohort: non-DM = 204, DM = 151 Replication: BASICMAR_2 cohort: non-DM = 108, DM = 59 REGICOR cohort: non-DM = 582, DM = 63 |
Hypomethylation | [82] | |
| Human | Blood | Non-diabetic = 98, T2DM = 100 | Hypomethylation | [100] | |
| SREBF1 | Human | Pancreatic islets | Non-diabetic = 34, T2DM = 15 | Hypermethylation | [77] |
| Human | Blood | Non-diabetic = 98, T2DM = 100 | Hypermethylation | [100] | |
| EXOC3L2 | Human | Pancreatic islets | Non-diabetic = 34, T2DM = 15 | Hypermethylation | [86] |
| CDKN1A | Human | Pancreatic islets | Non-diabetic = 34, T2DM = 15 | Hypomethylation | [86] |
| PDE7B | Human | Pancreatic islets | Non-diabetic = 34, T2DM = 15 | Hypomethylation | [86] |
| SEPT9 | Human | Pancreatic islets | Non-diabetic = 34, T2DM = 15 | Hypomethylation | [86] |
| SLC2A2 | Human | Pancreatic islets | Non-diabetic = 8, T2DM = 6 | Hypermethylation | [95] |
| DVL1 | Human | Blood | 966 individuals from the general population | Hypomethylation | [97] |
| HIST1H4D | Human | Blood | 966 individuals from the general population | Hypomethylation | [97] |
| LOXL2 | Human | Blood | Non-diabetic = 98, T2DM = 100 | Hypomethylation | [100] |
| SLC1A5 | Human | Blood | Non-diabetic = 98, T2DM = 100 | Hypomethylation | [100] |
| FTO | Human | Blood |
Pool-based cross-sectional study: Non-diabetic = 459, T2DM = 710 Individual-based cross-sectional study: Non-diabetic = 233, T2DM = 198 Longitudinal study: 515 individuals |
Hypomethylation | [103] |
| MSI2 | Human | Blood |
Discovery group: Non-diabetic = 13, hyperglycaemic = 8, T2DM = 5 Replication group: Non-diabetic = 220, T2DM = 220 |
Hypomethylation | [109] |
| Human | Pancreatic islets | Non-diabetic = 16, T2DM = 2 | |||
| NR4A1 | Human | Blood | Non-diabetic = 98, T2DM = 94 | Hypermethylation | [110] |
| Mouse | Pancreatic islets and blood from KK and KK.Cg-Ay/J mice |
In conclusion, although T2DM is a considerably complex disease, the above-mentioned studies provide some insights into the significant role played by epigenetics and DNA methylation in particular in the pathogenesis of T2DM, including insulin production, β cell secretion, and resistance. This regulation can either occur by affecting the DNA methylation of the insulin gene itself or by affecting the DNA methylation status of other genes that regulate insulin production, secretion, and sensing. Accordingly, these recent findings highlight a promising new route in terms of the development of novel therapeutics for T2DM, targeting DNA methylation in a way that enhances pancreatic β cell insulin production and secretion, along with targeting insulin sensitivity.
Future scope
Disease-associated epigenetic profiles can be considered either causative of the disease or the consequence (or a combination of both). Similar to the chicken and egg paradox, dissecting whether the disease or epigenetic profile came first is often hard. Accordingly, Volkmar et al. [115], pointed out that the methylation landscape, although associated with T2DM, can be either one of the contributing factors in the development of T2DM or the result of the reaction of β cells to T2DM hyperglycaemia.
In this review, we discussed the T2DM-associated DNA methylation profiles, but these profiles only represent a fraction of the bigger picture. Indeed, the overall T2DM-associated altered epigenetic profile includes alterations in several, if not all, of the epigenetic modifications identified to date. Accordingly, a number of altered histone tail modification profiles, along with those of altered non-coding RNAs, such as miRNAs, have been associated with the pathogenesis of T2DM. In addition to T2DM, a number of diseases have been found to be associated with altered epigenetic profiles. Furthermore, different types of epigenetic modifications likely do not operate in isolation but rather work together as they crosstalk with and regulate each other. Hence, a revisit to the already identified genes to analyse the entire epigenetic profile of each gene, along with the expressions of their respective regulators, may prove beneficial.
In addition, the majority of the DNA profiles discussed in this review were identified using peripheral blood samples. However, some DNA methylation profiles (and even entire epigenetic profiles) are tissue specific. Thus, further in-depth analysis of DNA methylation profiles in T2DM-specific tissues, such as the pancreas, liver, and skeletal muscle, is warranted.
Taken together, the identified changes in the DNA methylation profiles (or the entire epigenetic profiles) of certain genes may be further utilised to develop T2DM risk assessments and/or prognosis prediction tools in either a generic, population, or race-specific manner. Such novel findings, like the ones discussed in this review, are carving a new route for the development of novel therapeutics for T2DM targeting DNA methylation in a way that enhances pancreatic β cell insulin production and secretion, along with targeting insulin sensitivity. A greater understanding of the role of epigenetics in T2DM is expected to lead to improved interventions and treatments, which will hopefully reduce the global incidence of T2DM.
Acknowledgements
The authors thank Dr. Ernesto Guccione, Department of Oncological Sciences and Pharmacological Sciences, Icahn School of Medicine at Mount Sinai for critical comments and suggestions.
Abbreviations
- 5’-CpG-3’
5’-cytosine-phosphodiester bond-guanine-3’
- 5-Aza-CdR
5-aza-2’-deoxycytidine
- 5mC
5-methylcytosine
- ABCG1
ATP-binding cassette subfamily G member 1
- ADAMTS9
ADAM metallopeptidase with thrombospondin type 1 motif 9
- ADCY5
Adenylate cyclase 5
- AID
Activation induced deaminase
- Arx
Aristaless-related homeobox
- ATA
Aurintricarboxylic acid
- ATF2
Activating transcription factor 2
- AVPR2
Arginine vasopressin receptor 2
- BCL11A
B cell CLL/lymphoma 11A
- BER
Base excision repair
- BMI
Body mass index
- bp
Base pairs
- BRCA1
Breast cancer 1
- CALM2
Calmodulin 2
- cAMP
Cyclic adenosine monophosphate
- CCL18
C-C motif chemokine ligand 18
- CDC123/CAMK1D
Cell division cycle protein 123/calcium/calmodulin-dependent protein kinase 1D
- CDKAL1
CDK5 regulatory subunit-associated protein 1-like 1
- CDKN1A
Cyclin-dependent kinase inhibitor 1A
- CDKN2A
Cyclin-dependent kinase inhibitor 2A
- -CH3
Methyl group
- CHCHD9
Coiled-coil-helix-coiled-coil-helix domain-containing 2 pseudogene 9
- CRE
cAMP responsive element
- CREB-1
cAMP responsive element-binding protein-1
- CRY2
Cryptochrome 2
- CVD
Cardiovascular disease
- CXXC4
CXXC finger protein-4
- DM
Diabetes mellitus
- DM-MetS
DM plus MetS
- DMRs
Differentially methylated regions
- DN
Diabetic nephropathy
- DNMT
DNA methyltransferase
- DUSP8
Dual specificity phosphatase 8
- DUSP9
Dual specificity phosphatase 9
- DVL1
Dishevelled segment polarity protein 1
- ELOVL6
ELOVL fatty acid elongase 6
- EWAS
Epigenome-wide association study
- EXOC3L2
Exocyst complex component 3-like 2
- FADS1
Fatty acid desaturase 1
- FOSL2
FOS-like antigen 2
- FTO
Fat mass and obesity-associated
- GCK
Glucokinase
- GDM
Gestational DM
- GIP
Gastric inhibitory polypeptide
- GIPR
Gastric inhibitory polypeptide receptor
- GLIS3
GLIS family zinc finger 3
- GLP-1R
GLP-1 receptor
- GRB10
Growth factor receptor-bound protein-10
- GSIS
Glucose-stimulated insulin secretion
- GWAS
Genome-wide association studies
- GYS2
Glycogen synthase 2
- HbA1c
Glycated haemoglobin A1c
- HHEX
Haematopoietically expressed homeobox
- HIST1H4D
Histone cluster 1, H4d
- HMGA2
High-mobility group AT-hook 2
- HOMA-B
Homeostatis model assessment of β-cell function
- HOMA-IR
Homeostasis model assessment of insulin resistance
- IAPP
Islet amyloid polypeptide
- IGF-1
Insulin-like growth factor-1
- IGFBP-1
Insulin-like growth factor-binding protein 1
- IGFBP-7
Insulin-like growth factor-binding protein 7
- IL1RN
Interleukin 1 receptor antagonist
- Ins
Insulin
- IRS1
Insulin receptor substrate 1
- Kb
Kilobase pairs
- KCNJ11
Potassium voltage-gated channel subfamily J member-11
- KCNQ1
Potassium voltage-gated channel subfamily Q member-1
- LINE-1
Long interspersed nucleotide element 1
- LOXL2
Lysyl oxidase like 2
- MALT1
Mucosa-associated lymphoid tissue lymphoma translocation protein 1
- MBD2
Methyl-CpG-binding domain protein 2
- MCP-1
Monocyte chemoattractant protein-1
- MeCP2
Methyl CpG binding protein 2
- MeDIP-seq
Methylated DNA immunoprecipitation sequencing
- MetS
Metabolic syndrome
- miRNA
MicroRNA
- MSI2
Musashi RNA binding protein 2
- MTNR1B
Melatonin receptor 1B
- NGT
Non-impaired (normal) glucose tolerance
- NR4A1
Nuclear receptor subfamily 4 group A, member 1
- NR4A3
Nuclear receptor subfamily 4 group A member 3
- OGTT
Oral glucose tolerance test
- PDC
Pyruvate dehydrogenase complex
- PDE7B
Phosphodiesterase-7B
- PDK4
Pyruvate dehydrogenase kinase
- PDX-1
Pancreatic and duodenal homeobox-1
- PEG3
Paternally expressed gene-3
- PHOSPHO1
Phosphoethanolamine/phosphocholine phosphatase 1
- PID1
Phosphotyrosine interacting domain-containing 1
- PPARG / PPARγ
Peroxisome proliferator-activated receptor gamma
- PPARGC1A
Peroxisome proliferator-activated receptor gamma coactivator-1 alpha
- Prdx2
Peroxiredoxin 2
- PRKCZ
Protein kinase C epsilon zeta
- PARK2
Parkin RBR E3 ubiquitin protein ligase
- PTPN1
Protein tyrosine phosphatases non-receptor type 1
- PTPRD
Protein tyrosine phosphatases receptor type D
- RPA1
Replication protein A1
- SAM
S-adenosyl methionine
- SAMD12
Sterile alpha motif domain-containing 12
- SCARA3
Scavenger receptor class A member 3
- SCD1
Stearoyl-coenzyme A desaturase-1
- SEPT9
Septin-9
- shRNA
Short hairpin RNA
- siRNA
Small interfering RNA
- SLC2A2
Solute carrier family 2 member 2
- SLC30A8
Solute carrier family 30 member 8
- SOCS2
Suppressor of cytokine signalling 2
- SOCS3
Suppressor of cytokine signalling 3
- SPP1
Secreted phosphoprotein 1
- SREBF1
Sterol regulatory element-binding transcription factor 1
- SRR
Serine racemase
- T1DM
Type 1 DM
- T2DM
Type 2 DM
- TCF7L2
Transcription factor 7-like 2
- TETs
Ten-eleven translocations
- THADA
THADA armadillo repeat containing
- Tp53
Tumour protein p53
- TP53INP1
Tumour protein p53-inducible nuclear protein-1
- TSPAN8
Tetraspanin 8
- TSS
Transcription start site
- TXNIP
Thioredoxin-interacting protein
- VEGFA
Vascular endothelial growth factor A
- WFS1
Wolframin ER transmembrane glycoprotein
- ZBED3
Zinc finger BED-type containing 3
- ZnT-8
Zinc transporter 8
Authors’ contributions
SAHA wrote the paper with contribution from BSE, EMB, and SAA. BSE secured the funds. All authors reviewed, edited the manuscript, and approved the final manuscript.
Funding
The work in the lab was supported by research grants from United Arab Emirates University, UPAR grant # 3IM307; Zayed Center for Health Sciences grants #31R089, #3IM336, and #31R228; and Abu Dhabi Award for Research Excellence (AARE) grants 21M123 and 21M128. The open acess fee for this article is in part covered by a grant from Emirates Health Services.
Availability of data and materials
Not applicable
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.International Diabetes Federation. IDF Diabetes Atlas. 8th ed. Brussels; 2017.
- 2.Al-Haddad R, Karnib N, Assaad RA, Bilen Y, Emmanuel N, Ghanem A, et al. Epigenetic changes in diabetes. Neurosci Lett. 2016;625:64–69. doi: 10.1016/j.neulet.2016.04.046. [DOI] [PubMed] [Google Scholar]
- 3.International Diabetes Federation. IDF Diabetes Atlas. 9th ed. Brussels; 2019.
- 4.Berger SL, Kouzarides T, Shiekhattar R, Shilatifard A. An operational definition of epigenetics. Genes Dev. 2009;23:781–783. doi: 10.1101/gad.1787609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li E, Zhang Y. DNA methylation in mammals. Cold Spring Harb Perspect Biol. 2014;6:a019133. doi: 10.1101/cshperspect.a019133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Mello VDF, Pulkkinen L, Lalli M, Kolehmainen M, Pihlajamäki J, Uusitupa M. DNA methylation in obesity and type 2 diabetes. Ann Med. 2014;46:103–113. doi: 10.3109/07853890.2013.857259. [DOI] [PubMed] [Google Scholar]
- 7.Gibney ER, Nolan CM. Epigenetics and gene expression. Heredity (Edinb) 2010;105:4–13. doi: 10.1038/hdy.2010.54. [DOI] [PubMed] [Google Scholar]
- 8.Chen QW, Zhu XY, Li YY, Meng ZQ. Epigenetic regulation and cancer (review). Oncol Rep. 2014:523–32. [DOI] [PubMed]
- 9.Bansal A, Pinney SE. DNA methylation and its role in the pathogenesis of diabetes. Pediatr Diabetes. 2017;18:167–177. doi: 10.1111/pedi.12521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dayeh T, Ling C. Does epigenetic dysregulation of pancreatic islets contribute to impaired insulin secretion and type 2 diabetes? Biochem Cell Biol. 2015;93:511–521. doi: 10.1139/bcb-2015-0057. [DOI] [PubMed] [Google Scholar]
- 11.Bochtler M, Kolano A, Xu G-L. DNA demethylation pathways: additional players and regulators. BioEssays. 2017;39:e201600178. doi: 10.1002/bies.201600178. [DOI] [PubMed] [Google Scholar]
- 12.Ishikawa K, Tsunekawa S, Ikeniwa M, Izumoto T, Iida A, Ogata H, et al. Long-term pancreatic beta cell exposure to high levels of glucose but not palmitate induces DNA methylation within the insulin gene promoter and represses transcriptional activity. PLoS One. 2015;10:e0115350. doi: 10.1371/journal.pone.0115350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Czech MP. Insulin action and resistance in obesity and type 2 diabetes. Nat Med. 2017;23:804–814. doi: 10.1038/nm.4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dimitriadis G, Mitrou P, Lambadiari V, Maratou E, Raptis SA. Insulin effects in muscle and adipose tissue. Diabetes Res Clin Pract. 2011;93:S52–S59. doi: 10.1016/S0168-8227(11)70014-6. [DOI] [PubMed] [Google Scholar]
- 15.Hay CW, Ferguson LA, Docherty K. ATF-2 stimulates the human insulin promoter through the conserved CRE2 sequence. Biochim Biophys Acta Gene Struct Expr. 2007;1769:79–91. doi: 10.1016/j.bbaexp.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 16.Hay CW, Docherty K. Comparative analysis of insulin gene promoters: implications for diabetes research. Diabetes. 2006;55:3201–3213. doi: 10.2337/db06-0788. [DOI] [PubMed] [Google Scholar]
- 17.Kuroda A, Rauch TA, Todorov I, Ku HT, Al-Abdullah IH, Kandeel F, et al. Insulin gene expression is regulated by DNA methylation. PLoS One. 2009;4:e6953. doi: 10.1371/journal.pone.0006953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang BT, Dayeh TA, Kirkpatrick CL, Taneera J, Kumar R, Groop L, et al. Insulin promoter DNA methylation correlates negatively with insulin gene expression and positively with HbA1c levels in human pancreatic islets. Diabetologia. 2011;54:360–367. doi: 10.1007/s00125-010-1967-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yu H, Pask AJ, Hu Y, Shaw G, Renfree MB. ARX/Arx is expressed in germ cells during spermatogenesis in both marsupial and mouse. Reproduction. 2014;147:279–289. doi: 10.1530/REP-13-0361. [DOI] [PubMed] [Google Scholar]
- 20.Liu J, Hunter CS, Du A, Ediger B, Walp E, Murray J, et al. Islet-1 Regulates Arx transcription during pancreatic islet α-cell development. J Biol Chem. 2011;286:15352–15360. doi: 10.1074/jbc.M111.231670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilcox CL, Terry NA, May CL. Arx polyalanine expansion in mice leads to reduced pancreatic α-cell specification and increased α-cell death. PLoS One. 2013;8:e78741. doi: 10.1371/journal.pone.0078741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dhawan S, Georgia S, Tschen S, Fan G, Bhushan A. Pancreatic β cell identity is maintained by DNA methylation-mediated repression of Arx. Dev Cell. 2011;20:419–429. doi: 10.1016/j.devcel.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roy N, Takeuchi KK, Ruggeri JM, Bailey P, Chang D, Li J, et al. PDX1 dynamically regulates pancreatic ductal adenocarcinoma initiation and maintenance. Genes Dev. 2016;30:2669–2683. doi: 10.1101/gad.291021.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang BT, Dayeh TA, Volkov PA, Kirkpatrick CL, Malmgren S, Jing X, et al. Increased DNA methylation and decreased expression of PDX-1 in pancreatic islets from patients with type 2 diabetes. Mol Endocrinol. 2012;26:1203–1212. doi: 10.1210/me.2012-1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hall E, Dayeh T, Kirkpatrick CL, Wollheim CB, Dekker Nitert M, Ling C. DNA methylation of the glucagon-like peptide 1 receptor (GLP1R) in human pancreatic islets. BMC Med Genet. 2013;14:76. doi: 10.1186/1471-2350-14-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Doyle ME, Egan JM. Mechanisms of action of glucagon-like peptide 1 in the pancreas. Pharmacol Ther. 2007;113:546–593. doi: 10.1016/j.pharmthera.2006.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yoon JC, Xu G, Deeney JT, Yang S-N, Rhee J, Puigserver P, et al. Suppression of β cell energy metabolism and insulin release by PGC-1α. Dev Cell. 2003;5:73–83. doi: 10.1016/s1534-5807(03)00170-9. [DOI] [PubMed] [Google Scholar]
- 28.Wu H, Deng X, Shi Y, Su Y, Wei J, Duan H. PGC-1α, glucose metabolism and type 2 diabetes mellitus. J Endocrinol. 2016;229:R99–115. doi: 10.1530/JOE-16-0021. [DOI] [PubMed] [Google Scholar]
- 29.Bozec A, Bakiri L, Jimenez M, Rosen ED, Catala-Lehnen P, Schinke T, et al. Osteoblast-specific expression of Fra-2/AP-1 controls adiponectin and osteocalcin expression and affects metabolism. J Cell Sci. 2013;126:5432–5440. doi: 10.1242/jcs.134510. [DOI] [PubMed] [Google Scholar]
- 30.Ling C, Del Guerra S, Lupi R, Rönn T, Granhall C, Luthman H, et al. Epigenetic regulation of PPARGC1A in human type 2 diabetic islets and effect on insulin secretion. Diabetologia. 2008;51:615–622. doi: 10.1007/s00125-007-0916-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li J, Li S, Hu Y, Cao G, Wang S, Rai P, et al. The expression level of mRNA, protein, and DNA methylation status of FOSL2 of Uyghur in XinJiang in type 2 diabetes. J Diabetes Res. 2016;2016:1–7. doi: 10.1155/2016/5957404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Florez JC, Agapakis CM, Burtt NP, Sun M, Almgren P, Rastam L, et al. Association testing of the protein tyrosine phosphatase 1B gene (PTPN1) with type 2 diabetes in 7,883 people. Diabetes. 2005;54:1884–1891. doi: 10.2337/diabetes.54.6.1884. [DOI] [PubMed] [Google Scholar]
- 33.Huang Q, Han L, Liu Y, Wang C, Duan D, Lu N, et al. Elevation of PTPN1 promoter methylation is a significant risk factor of type 2 diabetes in the Chinese population. Exp Ther Med. 2017;14:2976–2982. doi: 10.3892/etm.2017.4924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ali O. Genetics of type 2 diabetes. World J Diabetes. 2013;4:114. doi: 10.4239/wjd.v4.i4.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhu L, Xie Z, Lu J, Hao Q, Kang M, Chen S, et al. TCF7L2 rs290481 T>C polymorphism is associated with an increased risk of type 2 diabetes mellitus and fasting plasma glucose level. Oncotarget. 2017;8:77000–77008. doi: 10.18632/oncotarget.20300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Canivell S, Ruano EG, Sisó-Almirall A, Kostov B, González-de Paz L, Fernandez-Rebollo E, et al. Differential methylation of TCF7L2 promoter in peripheral blood DNA in newly diagnosed, drug-naïve patients with type 2 diabetes. PLoS One. 2014;9:e99310. doi: 10.1371/journal.pone.0099310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chimienti F, Devergnas S, Pattou F, Schuit F, Garcia-Cuenca R, Vandewalle B, et al. In vivo expression and functional characterization of the zinc transporter ZnT8 in glucose-induced insulin secretion. J Cell Sci. 2006;119:4199–4206. doi: 10.1242/jcs.03164. [DOI] [PubMed] [Google Scholar]
- 38.Chimienti F, Devergnas S, Favier A, Seve M. Identification and cloning of a β-cell-specific zinc transporter, ZnT-8, localized into insulin secretory granules. Diabetes. 2004;53:2330–2337. doi: 10.2337/diabetes.53.9.2330. [DOI] [PubMed] [Google Scholar]
- 39.Tamaki M, Fujitani Y, Uchida T, Hirose T, Kawamori R, Watada H. Downregulation of ZnT8 expression in pancreatic β-cells of diabetic mice. Islets. 2009;1:124–128. doi: 10.4161/isl.1.2.9433. [DOI] [PubMed] [Google Scholar]
- 40.Seman N, Mohamud W, Östenson C-G, Brismar K, Gu HF. Increased DNA methylation of the SLC30A8 gene promoter is associated with type 2 diabetes in a Malay population. Clin Epigenetics. 2015;7:30. doi: 10.1186/s13148-015-0049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.LeRoith D, Yakar S. Mechanisms of disease: metabolic effects of growth hormone and insulin-like growth factor 1. Nat Clin Pract Endocrinol Metab. 2007;3:302–310. doi: 10.1038/ncpendmet0427. [DOI] [PubMed] [Google Scholar]
- 42.Gu T, Gu HF, Hilding A, Östenson C-G, Brismar K. DNA Methylation analysis of the insulin-like growth factor-1 (IGF1) gene in Swedish men with normal glucose tolerance and type 2 diabetes. J Diabetes Metab. 2014;05:1–6. [Google Scholar]
- 43.Rajpathak SN, Gunter MJ, Wylie-Rosett J, Ho GYF, Kaplan RC, Muzumdar R, et al. The role of insulin-like growth factor-I and its binding proteins in glucose homeostasis and type 2 diabetes. Diabetes Metab Res Rev. 2009;25:3–12. doi: 10.1002/dmrr.919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gu T, Gu HF, Hilding A, Sjöholm LK, Östenson C-G, Ekström TJ, et al. Increased DNA methylation levels of the insulin-like growth factor binding protein 1 gene are associated with type 2 diabetes in Swedish men. Clin Epigenetics. 2013;5:21. doi: 10.1186/1868-7083-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kutsukake M, Ishihara R, Momose K, Isaka K, Itokazu O, Higuma C, et al. Circulating IGF-binding protein 7 (IGFBP7) levels are elevated in patients with endometriosis or undergoing diabetic hemodialysis. Reprod Biol Endocrinol. 2008;6:54. doi: 10.1186/1477-7827-6-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gu HF, Gu T, Hilding A, Zhu Y, Kärvestedt L, Östenson C-G, et al. Evaluation of IGFBP-7 DNA methylation changes and serum protein variation in Swedish subjects with and without type 2 diabetes. Clin Epigenetics. 2013;5:20. doi: 10.1186/1868-7083-5-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jonsson A, Ladenvall C, Ahluwalia TS, Kravic J, Krus U, Taneera J, et al. Effects of common genetic variants associated with type 2 diabetes and glycemic traits on α- and β-cell function and insulin action in humans. Diabetes. 2013;62:2978–2983. doi: 10.2337/db12-1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tang L, Wang L, Ye H, Xu X, Hong Q, Wang H, et al. BCL11A gene DNA methylation contributes to the risk of type 2 diabetes in males. Exp Ther Med. 2014;8:459–463. doi: 10.3892/etm.2014.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Simonis-Bik AM, Nijpels G, van Haeften TW, Houwing-Duistermaat JJ, Boomsma DI, Reiling E, et al. Gene variants in the novel type 2 diabetes loci CDC123/CAMK1D, THADA, ADAMTS9, BCL11A, and MTNR1B affect different aspects of pancreatic β-cell function. Diabetes. 2010;59:293–301. doi: 10.2337/db09-1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bogdarina I, Murphy HC, Burns SP, Clark AJ. Investigation of the role of epigenetic modification of the rat glucokinase gene in fetal programming. Life Sci. 2004;74:1407–1415. doi: 10.1016/j.lfs.2003.08.017. [DOI] [PubMed] [Google Scholar]
- 51.Jiang MH, Fei J, Lan MS, Lu ZP, Liu M, Fan WW, et al. Hypermethylation of hepatic Gck promoter in ageing rats contributes to diabetogenic potential. Diabetologia. 2008;51:1525–1533. doi: 10.1007/s00125-008-1034-8. [DOI] [PubMed] [Google Scholar]
- 52.Tang L, Ye H, Hong Q, Wang L, Wang Q, Wang H, et al. Elevated CpG island methylation of GCK gene predicts the risk of type 2 diabetes in Chinese males. Gene. 2014;547:329–333. doi: 10.1016/j.gene.2014.06.062. [DOI] [PubMed] [Google Scholar]
- 53.Deshmane SL, Kremlev S, Amini S, Sawaya BE. Monocyte chemoattractant protein-1 (MCP-1): an overview. J Interf Cytokine Res. 2009;29:313–326. doi: 10.1089/jir.2008.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li H, Deng X, Li Z, Luo C, Liu J, Wang Y. Variation of serum monocyte chemoattractant protein-1 in patients with diabetes and metabolic syndrome. J Huazhong Univ Sci Technol [Medical Sci] 2011;31:312–316. doi: 10.1007/s11596-011-0373-8. [DOI] [PubMed] [Google Scholar]
- 55.Liu ZH, Chen LL, Deng XL, Song HJ, Liao YF, Zeng TS, et al. Methylation status of CpG sites in the MCP-1 promoter is correlated to serum MCP-1 in type 2 diabetes. J Endocrinol Investig. 2012;35:585–589. doi: 10.3275/7981. [DOI] [PubMed] [Google Scholar]
- 56.Karachanak-Yankova S, Dimova R, Nikolova D, Nesheva D, Koprinarova M, Maslyankov S, et al. Epigenetic alterations in patients with type 2 diabetes mellitus. Balkan J Med Genet. 2015;18:15–24. doi: 10.1515/bjmg-2015-0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Li Y-F. Protein kinase C/ζ ( PRKCZ ) Gene is associated with type 2 diabetes in Han population of North China and analysis of its haplotypes. World J Gastroenterol. 2003;9:2078. doi: 10.3748/wjg.v9.i9.2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zou L, Yan S, Guan X, Pan Y, Qu X. Hypermethylation of the PRKCZ gene in type 2 diabetes mellitus. J Diabetes Res. 2013;2013:1–4. doi: 10.1155/2013/721493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wheeler E, Barroso I. Genome-wide association studies and type 2 diabetes. Brief Funct Genomics. 2011;10:52–60. doi: 10.1093/bfgp/elr008. [DOI] [PubMed] [Google Scholar]
- 60.Canivell S, Ruano EG, Sisó-Almirall A, Kostov B, González-de Paz L, Fernandez-Rebollo E, et al. Gastric inhibitory polypeptide receptor methylation in newly diagnosed, drug-naïve patients with type 2 diabetes: a case-control study. PLoS One. 2013;8:e75474. doi: 10.1371/journal.pone.0075474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Boczek NJ, Gomez-Hurtado N, Ye D, Calvert ML, Tester DJ, Kryshtal DO, et al. Spectrum and prevalence of CALM1-, CALM2-, and CALM3-encoded calmodulin variants in long QT syndrome and functional characterization of a novel long QT syndrome-associated calmodulin missense variant, E141G. Circ Cardiovasc Genet. 2016;9:136–146. doi: 10.1161/CIRCGENETICS.115.001323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Murea M, Lu L, Ma L, Hicks PJ, Divers J, McDonough CW, et al. Genome-wide association scan for survival on dialysis in African-Americans with type 2 diabetes. Am J Nephrol. 2011;33:502–509. doi: 10.1159/000327985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fogarty MP, Cannon ME, Vadlamudi S, Gaulton KJ, Mohlke KL. Identification of a regulatory variant that binds FOXA1 and FOXA2 at the CDC123/CAMK1D type 2 diabetes GWAS locus. PLoS Genet. 2014;10:e1004633. doi: 10.1371/journal.pgen.1004633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dupuis J, Langenberg C, Prokopenko I, Saxena R, Soranzo N, Jackson AU, et al. New genetic loci implicated in fasting glucose homeostasis and their impact on type 2 diabetes risk. Nat Genet. 2010;42:105–116. doi: 10.1038/ng.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cheng J, Tang L, Hong Q, Ye H, Xu X, Xu L, et al. Investigation into the promoter DNA methylation of three genes (CAMK1D, CRY2 and CALM2) in the peripheral blood of patients with type 2 diabetes. Exp Ther Med. 2014;8:579–584. doi: 10.3892/etm.2014.1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ruddraraju KV, Zhang Z-Y. Covalent inhibition of protein tyrosine phosphatases. Mol BioSyst. 2017;13:1257–1279. doi: 10.1039/c7mb00151g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tsai F-J, Yang C-F, Chen C-C, Chuang L-M, Lu C-H, Chang C-T, et al. A Genome-wide association study identifies susceptibility variants for type 2 diabetes in Han Chinese. PLoS Genet. 2010;6:e1000847. doi: 10.1371/journal.pgen.1000847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chang Y-C, Chiu Y-F, Liu P-H, Shih K-C, Lin M-W, Sheu WH-H, et al. Replication of genome-wide association signals of type 2 diabetes in Han Chinese in a prospective cohort. Clin Endocrinol. 2012;76:365–372. doi: 10.1111/j.1365-2265.2011.04175.x. [DOI] [PubMed] [Google Scholar]
- 69.Below JE, Gamazon ER, Morrison JV, Konkashbaev A, Pluzhnikov A, McKeigue PM, et al. Genome-wide association and meta-analysis in populations from Starr County, Texas, and Mexico City identify type 2 diabetes susceptibility loci and enrichment for expression quantitative trait loci in top signals. Diabetologia. 2011;54:2047–2055. doi: 10.1007/s00125-011-2188-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chen Y-T, Lin W-D, Liao W-L, Lin Y-J, Chang J-G, Tsai F-J. PTPRD silencing by DNA hypermethylation decreases insulin receptor signaling and leads to type 2 diabetes. Oncotarget. 2015;6:12997–13005. doi: 10.18632/oncotarget.4092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Prokopenko I, Poon W, Mägi R, Prasad BR, Salehi SA, Almgren P, et al. A central role for GRB10 in regulation of islet function in man. PLoS Genet. 2014;10:e1004235. doi: 10.1371/journal.pgen.1004235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhang S, Hulver MW, McMillan RP, Cline MA, Gilbert ER. The pivotal role of pyruvate dehydrogenase kinases in metabolic flexibility. Nutr Metab (Lond) 2014;11:10. doi: 10.1186/1743-7075-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.van Otterdijk SD, Binder AM, Szarc vel Szic K, Schwald J, Michels KB. DNA methylation of candidate genes in peripheral blood from patients with type 2 diabetes or the metabolic syndrome. PLoS One. 2017;12:e0180955. doi: 10.1371/journal.pone.0180955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kulkarni SS, Salehzadeh F, Fritz T, Zierath JR, Krook A, Osler ME. Mitochondrial regulators of fatty acid metabolism reflect metabolic dysfunction in type 2 diabetes mellitus. Metabolism. 2012;61:175–185. doi: 10.1016/j.metabol.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 75.Kruit JK, Wijesekara N, Westwell-Roper C, Vanmierlo T, de Haan W, Bhattacharjee A, et al. Loss of both ABCA1 and ABCG1 results in increased disturbances in islet sterol homeostasis, inflammation, and impaired β-cell function. Diabetes. 2012;61:659–664. doi: 10.2337/db11-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Willmer T, Johnson R, Louw J, Pheiffer C. Blood-based DNA methylation biomarkers for type 2 diabetes: potential for clinical applications. Front Endocrinol (Lausanne) 2018;9:744. doi: 10.3389/fendo.2018.00744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dayeh T, Tuomi T, Almgren P, Perfilyev A, Jansson P-A, de Mello VD, et al. DNA methylation of loci within ABCG1 and PHOSPHO1 in blood DNA is associated with future type 2 diabetes risk. Epigenetics. 2016;11:482–488. doi: 10.1080/15592294.2016.1178418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mahony R, Ahmed S, Diskin C, Stevenson NJ. SOCS3 revisited: a broad regulator of disease, now ready for therapeutic use? Cell Mol Life Sci. 2016;73:3323–3336. doi: 10.1007/s00018-016-2234-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Grarup N, Stender-Petersen KL, Andersson EA, Jorgensen T, Borch-Johnsen K, Sandbaek A, et al. Association of variants in the sterol regulatory element-binding factor 1 (SREBF1) gene with type 2 diabetes, glycemia, and insulin resistance: a study of 15,734 Danish subjects. Diabetes. 2008;57:1136–1142. doi: 10.2337/db07-1534. [DOI] [PubMed] [Google Scholar]
- 80.Thielen L, Shalev A. Diabetes pathogenic mechanisms and potential new therapies based upon a novel target called TXNIP. Curr Opin Endocrinol Diabetes Obes. 2018;25:75–80. doi: 10.1097/MED.0000000000000391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chambers JC, Loh M, Lehne B, Drong A, Kriebel J, Motta V, et al. Epigenome-wide association of DNA methylation markers in peripheral blood from Indian Asians and Europeans with incident type 2 diabetes: a nested case-control study. Lancet Diabetes Endocrinol. 2015;3:526–534. doi: 10.1016/S2213-8587(15)00127-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Soriano-Tárraga C, Jiménez-Conde J, Giralt-Steinhauer E, Mola-Caminal M, Vivanco-Hidalgo RM, Ois A, et al. Epigenome-wide association study identifies TXNIP gene associated with type 2 diabetes mellitus and sustained hyperglycemia. Hum Mol Genet. 2016;25:609–619. doi: 10.1093/hmg/ddv493. [DOI] [PubMed] [Google Scholar]
- 83.Dayeh TA, Olsson AH, Volkov P, Almgren P, Rönn T, Ling C. Identification of CpG-SNPs associated with type 2 diabetes and differential DNA methylation in human pancreatic islets. Diabetologia. 2013;56:1036–1046. doi: 10.1007/s00125-012-2815-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Karambataki M, Malousi A, Tzimagiorgis G, Haitoglou C, Fragou A, Georgiou E, et al. Association of two synonymous splicing-associated CpG single nucleotide polymorphisms in calpain 10 and solute carrier family 2 member 2 with type 2 diabetes. Biomed Rep. 2017;6:146–158. doi: 10.3892/br.2016.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Torkamandi S, Bastami M, Ghaedi H, Tarighi S, Shokri F, Javadi A, et al. Association of CpG-SNP and 3’UTR-SNP of WFS1 with the risk of type 2 diabetes mellitus in an Iranian population. Int J Mol Cell Med. 2017;6:197–203. doi: 10.22088/BUMS.6.4.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dayeh T, Volkov P, Salö S, Hall E, Nilsson E, Olsson AH, et al. Genome-wide DNA methylation analysis of human pancreatic islets from type 2 diabetic and non-diabetic donors identifies candidate genes that influence insulin secretion. PLoS Genet. 2014;10:e1004160. doi: 10.1371/journal.pgen.1004160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sansbury FH, Flanagan SE, Houghton JAL, Shuixian Shen FL, Al-Senani AMS, Habeb AM, et al. SLC2A2 mutations can cause neonatal diabetes, suggesting GLUT2 may have a role in human insulin secretion. Diabetologia. 2012;55:2381–2385. doi: 10.1007/s00125-012-2595-0. [DOI] [PubMed] [Google Scholar]
- 88.Thorens B. GLUT2, glucose sensing and glucose homeostasis. Diabetologia. 2015;58:221–232. doi: 10.1007/s00125-014-3451-1. [DOI] [PubMed] [Google Scholar]
- 89.La Cognata V, Iemmolo R, D’Agata V, Scuderi S, Drago F, Zappia M, et al. Increasing the coding potential of genomes through alternative splicing: the case of PARK2 gene. Curr Genomics. 2014;15:203–216. doi: 10.2174/1389202915666140426003342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jin H-S, Kim J, Lee S-J, Kim K, Go MJ, Lee J-Y, et al. The PARK2 gene is involved in the maintenance of pancreatic β-cell functions related to insulin production and secretion. Mol Cell Endocrinol. 2014;382:178–189. doi: 10.1016/j.mce.2013.09.031. [DOI] [PubMed] [Google Scholar]
- 91.Letellier E, Haan S. SOCS2: physiological and pathological functions. Front Biosci (Elite Ed) 2016;8:189–204. doi: 10.2741/E760. [DOI] [PubMed] [Google Scholar]
- 92.Lebrun P, Cognard E, Gontard P, Bellon-Paul R, Filloux C, Berthault MF, et al. The suppressor of cytokine signalling 2 (SOCS2) is a key repressor of insulin secretion. Diabetologia. 2010;53:1935–1946. doi: 10.1007/s00125-010-1786-9. [DOI] [PubMed] [Google Scholar]
- 93.Close A-F, Dadheech N, Villela BS, Rouillard C, Buteau J. The orphan nuclear receptor Nor1/Nr4a3 is a negative regulator of β-cell mass. J Biol Chem. 2019;294:4889–4897. doi: 10.1074/jbc.RA118.005135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fischer AW, Albers K, Schlein C, Sass F, Krott LM, Schmale H, et al. PID1 regulates insulin-dependent glucose uptake by controlling intracellular sorting of GLUT4-storage vesicles. Biochim Biophys Acta Mol basis Dis. 1865;2019:1592–1603. doi: 10.1016/j.bbadis.2019.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Volkov P, Bacos K, Ofori JK, Esguerra JLS, Eliasson L, Rönn T, et al. Whole-genome bisulfite sequencing of human pancreatic islets reveals novel differentially methylated regions in type 2 diabetes pathogenesis. Diabetes. 2017;66:1074–1085. doi: 10.2337/db16-0996. [DOI] [PubMed] [Google Scholar]
- 96.Sharma M, Castro-Piedras I, Simmons GE, Pruitt K. Dishevelled: a masterful conductor of complex Wnt signals. Cell Signal. 2018;47:52–64. doi: 10.1016/j.cellsig.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hedman ÅK, Zilmer M, Sundström J, Lind L, Ingelsson E. DNA methylation patterns associated with oxidative stress in an ageing population. BMC Med Genet. 2016;9:72. doi: 10.1186/s12920-016-0235-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kulkarni H, Kos MZ, Neary J, Dyer TD, Kent JW, Göring HHH, et al. Novel epigenetic determinants of type 2 diabetes in Mexican-American families. Hum Mol Genet. 2015;24:5330–5344. doi: 10.1093/hmg/ddv232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Stangenberg S, Saad S, Schilter HC, Zaky A, Gill A, Pollock CA, et al. Lysyl oxidase-like 2 inhibition ameliorates glomerulosclerosis and albuminuria in diabetic nephropathy. Sci Rep. 2018;8:9423. doi: 10.1038/s41598-018-27462-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Walaszczyk E, Luijten M, Spijkerman AMW, Bonder MJ, Lutgers HL, Snieder H, et al. DNA methylation markers associated with type 2 diabetes, fasting glucose and HbA1c levels: a systematic review and replication in a case–control sample of the Lifelines study. Diabetologia. 2018;61:354–368. doi: 10.1007/s00125-017-4497-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yuan W, Xia Y, Bell CG, Yet I, Ferreira T, Ward KJ, et al. An integrated epigenomic analysis for type 2 diabetes susceptibility loci in monozygotic twins. Nat Commun. 2014;5:5719. doi: 10.1038/ncomms6719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zdrojowy-Wełna A, Tupikowska M, Kolackov K, Bednarek-Tupikowska G. The role of fat mass and obesity-associated gene (FTO) in obesity—an overview. Endokrynol Pol. 2014;65:224–231. doi: 10.5603/EP.2014.0031. [DOI] [PubMed] [Google Scholar]
- 103.Toperoff G, Aran D, Kark JD, Rosenberg M, Dubnikov T, Nissan B, et al. Genome-wide survey reveals predisposing diabetes type 2-related DNA methylation variations in human peripheral blood. Hum Mol Genet. 2012;21:371–383. doi: 10.1093/hmg/ddr472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ma J, Cheng J, Wang L, Wang H, Xu L, Liu P, et al. No association between IRS-1 promoter methylation and type 2 diabetes. Mol Med Rep. 2013;8:949–953. doi: 10.3892/mmr.2013.1569. [DOI] [PubMed] [Google Scholar]
- 105.Travers ME, Mackay DJG, Dekker Nitert M, Morris AP, Lindgren CM, Berry A, et al. Insights into the molecular mechanism for type 2 diabetes susceptibility at the KCNQ1 locus from temporal changes in imprinting status in human islets. Diabetes. 2013;62:987–992. doi: 10.2337/db12-0819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lecarpentier Y, Claes V, Vallée A, Hébert J-L. Interactions between PPAR gamma and the canonical Wnt/beta-catenin pathway in type 2 diabetes and colon cancer. PPAR Res. 2017;2017:1–9. doi: 10.1155/2017/5879090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Nilsson E, Jansson PA, Perfilyev A, Volkov P, Pedersen M, Svensson MK, et al. Altered DNA methylation and differential expression of genes influencing metabolism and inflammation in adipose tissue from subjects with type 2 diabetes. Diabetes. 2014;63:2962–2976. doi: 10.2337/db13-1459. [DOI] [PubMed] [Google Scholar]
- 108.Szabat M, Kalynyak TB, Lim GE, Chu KY, Yang YH, Asadi A, et al. Musashi expression in β-cells coordinates insulin expression, apoptosis and proliferation in response to endoplasmic reticulum stress in diabetes. Cell Death Dis. 2011;2:e232. doi: 10.1038/cddis.2011.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jeon J-P, Koh I-U, Choi N-H, Kim B-J, Han B-G, Lee S. Differential DNA methylation of MSI2 and its correlation with diabetic traits. PLoS One. 2017;12:e0177406. doi: 10.1371/journal.pone.0177406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Chen Y-T, Liao J-W, Tsai Y-C, Tsai F-J. Inhibition of DNA methyltransferase 1 increases nuclear receptor subfamily 4 group A member 1 expression and decreases blood glucose in type 2 diabetes. Oncotarget. 2016;7:39162–39170. doi: 10.18632/oncotarget.10043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Thongsroy J, Patchsung M, Mutirangura A. The association between Alu hypomethylation and severity of type 2 diabetes mellitus. Clin Epigenetics. 2017;9:93. doi: 10.1186/s13148-017-0395-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.María Martín-Núñez G, Rubio-Martín E, Cabrera-Mulero R, Rojo-Martínez G, Olveira G, Valdés S, et al. Type 2 diabetes mellitus in relation to global LINE-1 DNA methylation in peripheral blood: a cohort study. Epigenetics. 2014;9:1322–1328. doi: 10.4161/15592294.2014.969617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wu Y, Cui W, Zhang D, Wu W, Yang Z. The shortening of leukocyte telomere length relates to DNA hypermethylation of LINE-1 in type 2 diabetes mellitus. Oncotarget. 2017;8:73964–73973. doi: 10.18632/oncotarget.18167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kameswaran V, Bramswig NC, McKenna LB, Penn M, Schug J, Hand NJ, et al. Epigenetic regulation of the DLK1-MEG3 microRNA cluster in human type 2 diabetic islets. Cell Metab. 2014;19:135–145. doi: 10.1016/j.cmet.2013.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Volkmar M, Dedeurwaerder S, Cunha DA, Ndlovu MN, Defrance M, Deplus R, et al. DNA methylation profiling identifies epigenetic dysregulation in pancreatic islets from type 2 diabetic patients. EMBO J. 2012;31:1405–1426. doi: 10.1038/emboj.2011.503. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable