Abstract
Background
Cutaneous leishmaniasis (CL) may be emerging among international travellers and migrants. Limited data exist on mucocutaneous leishmaniasis (MCL) in travellers. We describe the epidemiology of travel-associated CL and MCL among international travellers and immigrants over a 20-year period through descriptive analysis of GeoSentinel data.
Methods
Demographic and travel-related data on returned international travellers diagnosed with CL or MCL at a GeoSentinel Surveillance Network site between 1 September 1997 and 31 August 2017 were analysed.
Results
A total of 955 returned travellers or migrants were diagnosed with travel-acquired CL (n = 916) or MCL during the study period, of whom 10% (n = 97) were migrants. For the 858 non-migrant travellers, common source countries were Bolivia (n = 156, 18.2%) and Costa Rica (n = 97, 11.3%), while for migrants, they were Syria (n = 34, 35%) and Afghanistan (n = 22, 22.7%). A total of 99 travellers (10%) acquired their disease on trips of ≤ 2 weeks. Of 274 cases for which species identification was available, Leishmania Viannia braziliensis was the most well-represented strain (n = 117, 42.7%), followed by L. major (n = 40, 14.6%) and L. V. panamensis (n = 38, 13.9%). Forty cases of MCL occurred, most commonly in tourists (n = 29, 72.5%) and from Bolivia (n = 18, 45%). A total of 10% of MCL cases were acquired in the Old World.
Conclusions
Among GeoSentinel reporting sites, CL is predominantly a disease of tourists travelling mostly to countries in Central and South America such as Bolivia where risk of acquiring L. V. braziliensis and subsequent MCL is high. The finding that some travellers acquired leishmaniasis on trips of short duration challenges the common notion that CL is a disease of prolonged travel. Migrants from areas of conflict and political instability, such as Afghanistan and Syria, were well represented, suggesting that as mass migration of refugees continues, CL will be increasingly encountered in intake countries.
Keywords: cutaneous leishmaniasis, GeoSentinel, mucosal leishmaniasis, skin lesions after travel, tegumentary leishmaniasis, vector-borne disease
Introduction
Cutaneous leishmaniasis (CL) may be an emerging infection among international travellers.1 Few data exist on the epidemiology of mucocutaneous leishmaniasis (MCL) or mucosal leishmaniasis (ML) in travellers.2 Recent literature on leishmaniasis in travellers indicates that more than half of published cases have been reported in the past 15 years.1,3 In the UK, the annual number of imported cases of CL rose over 4-fold from 1995 to 2003, an increase attributed to more frequent travel by British to South America.3 A network-wide GeoSentinel Surveillance Network analysis demonstrated that CL was the second most frequent microbiologically confirmed skin infection encountered in returned travellers from Latin America and the Caribbean, the Middle East and North Africa, Europe and South Central Asia.4 Moreover, CL is consistently reported as a top 10 cause of dermatosis in travellers returning to Canada from endemic areas.5
Leishmania spp. and locally acquired human leishmaniasis have been reported on every continent but Antarctica, although the organisms are primarily endemic in approximately 70 countries in the tropics and sub-tropics.6 In the USA, Leishmania spp. have been isolated in Texas, Arizona, Oklahoma and Ohio from humans, dogs, rodents and insects,7–11 with human infections occurring in Texas, which borders Mexico where leishmaniasis is endemic,12–16 and neighboring Oklahoma.17 Autochthonous transmission of Leishmania donovani has led to CL as far north as North Dakota.18 In their ecological niche model of vector distribution, Gonzalez and colleagues concluded that ‘climate change will exacerbate the ecological risk of human exposure to leishmaniasis in areas outside its present range in the United States and, possibly, in parts of southern Canada’19 and thus suggest adoption of surveillance for this disease. Thus, travellers to parts of the US where autochthonous transmission has been established are theoretically at risk of acquisition, as are residents of these areas.
Leishmaniasis is also well established in parts of Southern Europe, posing a potentially unrecognized risk to travellers and challenging clinicians unfamiliar with the expanding epidemiology of CL. Several species of Phlebotomidae sandflies are distributed widely throughout Western Europe,20 and autochthonous CL cases of L. infantum are regularly reported in Southern Europe, while L. donovani (Cyprus), and L. tropica (Greece) infections have emerged more recently.21 Over a 13-year period, 317 autochthonous cases of L. infantum were reported to the National Reference Centre for Leishmaniases in France.22 As with all communicable diseases that are neither nationally nor regionally notifiable to public health authorities, surveillance is passive and variable, with under-reporting commonplace.22
Suggestive changes in the ecology and epidemiology of CL led us to undertake an analysis of CL and MCL reported to the GeoSentinel Surveillance System. These changes include the presence of competent vectors and autochthonous transmission in historically non-endemic well-resourced countries of the Americas and Europe, the increase of travel from non-endemic to endemic areas, the possible rising frequency of CL among travellers and the dearth of recent large-scale surveillance data on this imported infection. Our aim was to examine the demographic and travel-related epidemiology of CL and MCL in travellers and migrants to inform development of international surveillance and risk-stratification guidelines for international travellers.
Methods
Data Source
Data were collected using the GeoSentinel Surveillance Network data platform. This surveillance network is comprised of 72 specialized travel/tropical medicine clinics on 6 continents that contribute denominalized travel-specific data on all ill travellers to a centralized Structured Query Language database4,23 (for additional details see www.istm.org/geosentinel). The GeoSentinel data collection protocol has been reviewed by the institutional review board officer at the National Center for Zoonotic and Emerging Infectious Diseases at the Centers for Disease Control and Prevention and classified as public health surveillance and not as human-subjects research requiring submission to institutional review boards. Data collected include patient demographics, details of recent travel, 5-year travel history, purpose of travel and pre-travel encounter history. Final diagnoses are made by site physicians and assigned a diagnostic code selected from a standardized list of >500 diagnostic entities, including aetiologic (e.g. CL) and syndromic (e.g. rash, skin and soft tissue infection) diagnoses. All GeoSentinel sites contribute microbiologically confirmed data, where available, based on the best national reference diagnostic tests (including molecular diagnostics) available at the time. ‘Probable’ diagnoses are restricted to those with highly characteristic epidemiological and physical findings (e.g. ulcer with raised violaceous border in a traveller with potential exposure) and clinical response to highly specific therapy, or classical presentation and highly suggestive exposure history with laboratory exclusion of other possible aetiologies.
Inclusion Criteria
Demographic, clinical and travel-related data on all travellers evaluated at a GeoSentinel site between 1 September 1997 and 31 August 2017 who sought care during or after travel and who had a final diagnosis of CL and/or MCL were included (Figure 1). A proportion of these travellers have been represented in aggregate in prior single- or multi-site GeoSentinel analyses with overlapping enrolment periods2,4,5; however, this analysis synthesizes prior cases and captures the overall 20-year network experience with CL and MCL. Only patients with probable or confirmed final diagnosis of CL or MCL (specific aetiology as described previously) were included. Records with an unusual region or country of exposure were manually reviewed and excluded if region of acquisition could not be resolved.
Figure 1.
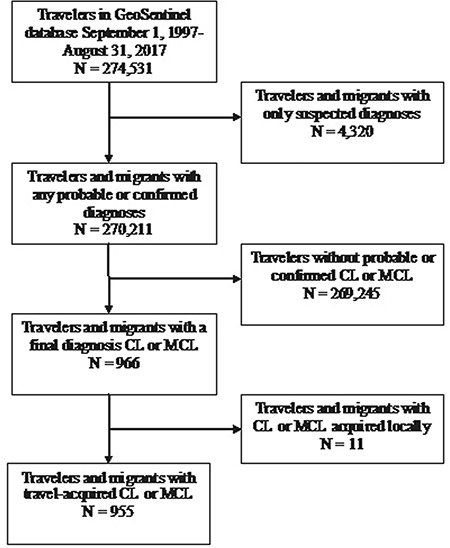
Migrants and travellers with CL or MCL seen at GeoSentinel Surveillance Network sites between 1 September 1997 and 31 August 2017.
Definitions and Classifications
Purpose of travel was assigned one of six designations, including migration (immigrants and refugees), tourism, business, missionary/volunteer research/aid work, visiting friends and relatives (VFR) and ‘Other’, which included students, military personnel and medical tourists. VFRs were defined as immigrants who return to their country of origin to ‘visit friends and relatives’. The VFR designation also includes children of foreign-born parents (i.e. second generation immigrants) who return to their parent’s homeland to visit friends and relatives. The term VFR is typically applied to individuals travelling from a high-income country of current residence to a low-income country of origin.24
Countries of exposure and travel were assigned to one of eight hard-coded regional classifications (within the GeoSentinel database) where leishmaniasis is transmitted: Central America, South America, Western Europe, Eastern Europe, the Middle East, North Africa, Sub-Saharan Africa and South Central Asia.
‘Case clustering’ at individual sites was defined as >1 case of CL and/or MCL among travellers to the same country with similar travel dates and reported by a single site. This involved manual review of records.
Statistical Analysis
Extracted data were managed in a password-protected and encrypted Microsoft Access database. Descriptive statistics [means with standard deviation (SD), medians with range, proportions] were performed for all continuous and categorical demographic, clinical and travel-related variables. A sub-analysis was performed for those travellers with a diagnosis of MCL. Differences between demographics and travel characteristics were compared between groups of travellers using Student’s t-test or Yates’ corrected Chi-square analysis. All statistical computations were performed using GraphPad Prism 6.0 software (GraphPad Inc., La Jolla, CA).
Results
Of the 966 travellers or new immigrants diagnosed with CL or MCL during the study period, 955 (98.9%) were travel acquired, while 11 (1.1%) were temporally associated with recent travel but acquired locally in Israel, France or Spain and therefore were not analysed further (Figure 1). Tables 1 and 2 describe the demographic and travel-related metrics stratified by purpose of travel and diagnosis (CL, MCL). Of travel-acquired cases of CL (n = 916) or MCL (n = 40), males accounted for 62.4% (n = 596), while females accounted for 37.5% (n = 358) (Table 1). Median age was 30 years (range < 1 to 95 years) (Table 1). Median trip duration for those with travel-acquired CL or MCL was 47 days (range < 1 –12 541 days; IQR, 22–157 days). Ninety-nine travellers (10%) acquired their disease on trips of ≤ 2 weeks (Table 1), and 29 (3%) acquired CL or MCL on trips lasting ≤ 7 days. Of the 955 travel-acquired cases, the most common reasons for travel were tourism (n = 501, 52.5%), VFR (n = 119, 12.5%) and missionary, volunteer, research or aid work (‘missionaries’) (n = 88, 9.2%). Migration-related cases accounted for 10% (n = 97). Although a pre-travel medical encounter was sought by 38.5% of travellers with CL or MCL, only 10% of VFRs had a pre-travel consultation (P < 0.0001 compared to non-VFR travellers).
Table 1.
Demographic characteristics of 955 returned travellers or new immigrants presenting to a GeoSentinel Surveillance Network site for travel-acquired cutaneous or mucocutaneous leishmaniasis, 1997–2017a, by purpose of travel
| Purpose of travel | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | All travellers, n = 955 | Tourism, n = 501 | Visiting friends and relatives, n = 119 | Migration, n = 97 | Missionary, volunteer, researcher and aid, n = 88 | Business, n = 72 | Otherb, n = 78 | |||||||
| Sexc, n (%) | ||||||||||||||
| Male | 596 | 62.4 | 312 | 62.3 | 60 | 50.4 | 58 | 59.8 | 51 | 58.0 | 50 | 69.4 | 65 | 83.3 |
| Female | 358 | 37.5 | 189 | 37.7 | 59 | 49.6 | 39 | 40.2 | 36 | 40.9 | 22 | 30.6 | 13 | 16.7 |
| Age, median (range), y | 30 | 1–95 | 30 | 1–78 | 40.5 | 1–95 | 27 | 1–78 | 30 | 18–76 | 37 | 21–68 | 25 | 15–68 |
| Type of patientd, n (%) | ||||||||||||||
| Inpatient | 77 | 8.1 | 41 | 8.2 | 5 | 4.2 | 9 | 9.3 | 4 | 4.5 | 4 | 5.6 | 14 | 17.9 |
| Outpatient | 871 | 91.2 | 458 | 91.4 | 114 | 95.8 | 86 | 88.7 | 82 | 93.2 | 68 | 94.4 | 63 | 80.8 |
| Travel duration, median (range) | 47 d | <1 d–34 y | 37.5 d | 5 d–10.5 y | 31 d | <1 d–9.3 yrs | NA | NA | 89 d | 9 d–34 y | 35 d | 5 d–8 y | 123 d | 7 d–4.4 y |
| Short duration travel (≤14 days), n (%) | 99 | 10.4 | 76 | 15.2 | 5 | 4.2 | NA | NA | 4 | 4.5 | 11 | 15.3 | 3 | 3.8 |
| Pretravel medical encounter, n (%) |
||||||||||||||
| Yes | 368 | 38.5 | 236 | 47.1 | 12 | 10.1 | NA | NA | 44 | 50.0 | 26 | 36.1 | 50 | 64.1 |
| No | 340 | 35.6 | 147 | 29.3 | 75 | 63 | NA | NA | 25 | 28.4 | 24 | 33.3 | 11 | 14.1 |
| Unknown | 247 | 25.9 | 118 | 23.6 | 32 | 26.9 | NA | NA | 19 | 21.6 | 22 | 30.6 | 17 | 21.8 |
| Region of acquisition, n (%) | ||||||||||||||
| South America | 335 | 35.1 | 214 | 42.7 | 8 | 6.7 | 6 | 6.2 | 47 | 53.4 | 26 | 36.1 | 34 | 43.6 |
| Central America | 176 | 18.4 | 118 | 23.6 | 5 | 4.2 | 9 | 9.3 | 20 | 22.7 | 13 | 18.1 | 11 | 14.1 |
| Middle East | 101 | 10.6 | 30 | 6.0 | 13 | 10.9 | 38 | 39.2 | 3 | 3.4 | 10 | 13.9 | 7 | 9.0 |
| South Central Asia | 97 | 10.2 | 10 | 2.0 | 27 | 22.7 | 31 | 32.0 | 3 | 3.4 | 5 | 6.9 | 21 | 26.9 |
| North Africa | 91 | 9.5 | 24 | 4.8 | 53 | 44.5 | 1 | 1.0 | 4 | 4.5 | 6 | 8.3 | 3 | 3.8 |
| Western Europe | 81 | 8.5 | 74 | 14.8 | 4 | 3.4 | 1 | 1.0 | 0 | 0 | 2 | 2.8 | 0 | 0 |
| Sub-Saharan Africa | 43 | 4.5 | 14 | 2.8 | 8 | 6.7 | 7 | 7.2 | 9 | 10.2 | 4 | 5.6 | 1 | 1.3 |
| Eastern Europe | 2 | 0.2 | 0 | 0 | 1 | 0.8 | 1 | 1.0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Unknown | 29 | 3.0 | 17 | 3.4 | 0 | 0 | 3 | 3.1 | 2 | 2.3 | 6 | 8.3 | 1 | 1.3 |
aVisit dates between 29 September 1997 and 31 August 2017
bIncludes 52 military personnel, 25 students, and 1 medical tourist.
cSex unknown for one missionary traveller
dUnknown care setting in seven (0.7%) travellers (two tourists, two missionaries, two migrants and one ‘other’)
Table 2.
Demographic characteristics of 955 returned travellers or new immigrants presenting to a GeoSentinel Surveillance Network site for travel-acquired cutaneous or mucocutaneous leishmaniasis, 1997–2017a, by clinical phenotype
| Characteristic | All travellers, n = 955 | Type of Leishmaniasisb | ||||
|---|---|---|---|---|---|---|
| CL, n = 916 | MCL, n = 40 | |||||
| Sexd, n (%) | ||||||
| Male | 596 | 62.4 | 568 | 62.0 | 29 | 72.5 |
| Female | 358 | 37.5 | 347 | 37.9 | 11 | 27.5 |
| Age, median (range), y | 30 | 1–95 | 30 | 1–95 | 31.5 | 14–78 |
| Diagnosis statusb | ||||||
| Confirmed | 837 | 87.6 | 798 | 87.1 | 39 | 97.5 |
| Probable | 119 | 12.4 | 118 | 12.9 | 1 | 2.5 |
| Type of patiente | ||||||
| Inpatient | 77 | 8.1 | 68 | 7.4 | 9 | 22.5 |
| Outpatient | 871 | 91.2 | 841 | 91.8 | 31 | 77.5 |
| Purpose of travel | ||||||
| Tourism | 501 | 52.5 | 472 | 51.5 | 29 | 72.5 |
| Visiting friends and relatives | 119 | 12.5 | 116 | 12.7 | 3 | 7.5 |
| Missionary, volunteer, researcher and aid | 88 | 9.2 | 86 | 9.4 | 3 | 7.5 |
| Migration | 97 | 10.2 | 94 | 10.3 | 3 | 7.5 |
| Business | 72 | 7.5 | 70 | 7.6 | 2 | 5.0 |
| Otherc | 78 | 8.2 | 78 | 8.5 | 0 | 0 |
| Travel duration for non-migration travellers, median (range) | 47 d | <1 d–34 y | 48 d | <1 d–34 y | 28 d | 7–273 d |
| Short duration travel, for non-migration travellers (≤14 days), n (%) | 99 | 10.4 | 95 | 10.4 | 5 | 12.5 |
| Pretravel medical encounter, for non-migration travellers, n (%) | ||||||
| Yes | 368 | 38.5 | 347 | 37.9 | 21 | 52.5 |
| No | 340 | 35.6 | 330 | 36.0 | 10 | 25.0 |
| Unknown | 247 | 25.9 | 239 | 26.1 | 9 | 22.5 |
| Region of acquisition | ||||||
| South America | 335 | 35.1 | 307 | 33.5 | 29 | 72.5 |
| Central America | 176 | 18.4 | 172 | 18.8 | 4 | 10.0 |
| Middle East | 101 | 10.6 | 101 | 11.0 | 0 | 0 |
| South Central Asia | 97 | 10.2 | 97 | 10.6 | 0 | 0 |
| North Africa | 91 | 9.5 | 89 | 9.7 | 2 | 5.0 |
| Western Europe | 81 | 8.5 | 79 | 8.6 | 2 | 5.0 |
| Sub-Saharan Africa | 43 | 4.5 | 43 | 4.7 | 0 | 0 |
| Eastern Europe | 2 | 0.2 | 2 | 0.2 | 0 | 0 |
| Unknown | 29 | 3.0 | 26 | 2.8 | 3 | 7.5 |
aVisit dates between 1 September 1997 and 31 August 2017
bOne missionary traveller had intercurrent CL and MCL and therefore counts in totals for both (955 total individual cases, with 916 cases of CL and 40 cases of MCL).
cIncludes 52 military personnel, 25 students and 1 medical tourist
dSex unknown for one traveller with CL
eUnknown care setting in seven (0.8%) travellers with CL
For all non-migration travellers, the most common source countries were Bolivia (n = 156, 18.2%) and Costa Rica (n = 97, 11.3%), while for migrants, they were Syria (n = 34, 35%) and Afghanistan (n = 22, 22.7%) (Table 3). Peru and/or Bolivia, the two countries with the greatest relative risk of MCL acquisition, were in the top 5 countries of exposure for several groups of non-migration travellers including tourists, ‘missionaries’ and business travellers (Table 3). Moreover, of all cases acquired in Bolivia (n = 156), 18 (11.5%) presented with MCL, compared to 8.7% (n = 29) of cases from all continental South America, 6.5% (n = 33) of cases from the New World, in general, and 1% (n = 4) of cases from the Old World.
Table 3.
Top 5 countries of exposure by travel reason for 955 returned travellers or new immigrants presenting at a GeoSentinel Surveillance Network site for travel-acquired cutaneous or mucocutaneous leishmaniasis, 1997–2017
| Country of exposure | Travel unrelated to migration | ||||||
|---|---|---|---|---|---|---|---|
| Rank | Recent migration travel; country: n (%); n = 97 |
All non-migration travellers; country: n (%); n = 858 | Tourism; country: n (%); n = 501 | Visiting friends and relatives; country: n (%); n = 119 | Missionary, volunteer, researcher and aid; country: n (%); n = 88 | Business; country: n (%); n = 72 | Othera; country: n (%); n = 78 |
| 1 | Syria: 34 (35.0) |
Bolivia: 156 (18.2) |
Bolivia: 147 (29.3) |
Tunisia: 26 (21.8) |
Peru: 15 (17.0) |
Peru: 7 (9.7) |
Afghanistan: 21 (26.9) |
| 2 | Afghanistan: 22 (22.7) |
Costa Rica: 97 (11.3) |
Costa Rica: 75 (15.0) |
Morocco: 16 (13.4) |
Ecuador: 14 (15.9) |
Costa Rica: 5 (6.9) |
French Guiana: 19 (24.4) |
| 3 | Burkina Faso: 4 (4.1) |
Afghanistan: 60 (7.0) |
Spain: 51 (10.2) |
Afghanistan: 13 (10.9) |
Costa Rica: 12 (13.6) |
French Guiana: 5 (6.9) |
Belize: 8 (10.3) |
| 4 | El Salvador: 3 (3.1) |
Spain: 54 (6.3) |
Israel: 21 (4.2) |
Iran: 8 (6.7) |
Brazil: 6 (6.8) |
Morocco: 5 (6.9) |
Ecuador: 5 (6.4) |
| 5 | Pakistan: 3 (3.1) |
Peru: 49 (5.7) |
Peru: 19 (3.8) |
Algeria: 6 (5.0) |
Bolivia: 5 (5.7); Sudan: 5 (5.7) |
Suriname: 5 (6.9) |
Peru: 4 (5.1) |
aIncludes 52 military personnel, 25 students, and 1 medical tourist
Species identification was available for 274 cases (28.7%) (Table 4). Leishmania Viannia braziliensis was the most common strain (n = 117, 42.7%), followed by L. major (n = 40, 14.6%) and L. V. panamensis (n = 38, 13.9%). For CL or MCL due to L. V. braziliensis, the top 3 source countries were Bolivia, Peru and Ecuador, while for L. major they were Israel, Morocco and Tunisia (Table 4). For CL or MCL due to L. V. panamensis, the top 3 source countries were Costa Rica, Ecuador and Panama (Table 4).
Table 4.
Top represented species among 274 travellers or new immigrants who sought care at a GeoSentinel Surveillance Network site for travel-acquired cutaneous or mucocutaneous leishmaniasis with definite species identification, 1997–2017
| Species | Patientsa | Top 3 source countries | |
|---|---|---|---|
| No. | % | ||
| New World | |||
| Leishmania Viannia braziliensisb | 117 | 42.7 | Bolivia (n = 73); Peru (n = 17); Ecuador (n = 7) |
| L. V. panamensisb | 38 | 13.9 | Costa Rica (n = 24); Ecuador (n = 4); Panama (n = 4) |
| L. V. guyanensisb | 20 | 7.3 | French Guiana (n = 15); Peru (n = 2); Suriname (n = 2) |
| L. mexicana | 10 | 3.6 | Belize (n = 4); Mexico (n = 4); Honduras (n = 1) |
| L. Viannia spp. not otherwise specifiedb | 7 | 2.6 | Costa Rica (n = 3); Peru (n = 2); Belize (n = 1); Suriname (n = 1) |
| L. V. lainsonib | 1 | 0.4 | Peru (n = 1) |
| Old World | |||
| L. major | 40 | 14.6 | Israel (n = 12); Morocco (n = 7); Tunisia (n = 7) |
| L. donovani Complexb | 22 | 8.0 | Spain (n = 14); Turkey (n = 3); Italy (n = 2) |
| L. infantum | 14 | 5.1 | Spain (n = 10); Italy (n = 1); Malta (n = 1); Morocco (n = 1); Tunisia (n = 1); Turkey (n = 1) |
| L. donovani | 8 | 2.9 | Spain (n = 4); Turkey (n = 2); Italy (n = 1) |
| L. tropica | 17 | 6.2 | Syria (n = 7); Afghanistan (n = 3); Kenya (n = 2); Iran (n = 2) |
| L. aethiopica | 2 | 0.7 | Ethiopia (n = 2) |
| Total | 274 | 28.7c | Bolivia (n = 73); Costa Rica (n = 28); Peru (n = 22) |
aPercentages calculated using number of patients with definitive species identification as denominator (n = 274)
bDiscrimination among species within the Viannia sub-genus and between L. donovani and L. infantum requires highly sophisticated molecular diagnostics that may not have been available to all contributing sites at all times, thus, the precise species identification represented herein must be interpreted with caution.
c28.7% of travellers received definitive species identification that was recorded in the database.
Eight percent (n = 77) of all travellers with CL or MCL were initially hospitalized for diagnosis and treatment (Table 1). Inpatient management was over-represented among those travelling for the purpose of military, education or medical tourism (P = 0.0033 compared to other types of travellers).
Forty cases of MCL occurred, most of which were in tourists (n = 29, 72.5%); Bolivia was the most common country of acquisition (n = 18, 45.0%) (Table 4). Median age for those with MCL was 31.5 years (range, 14–78 years), with a male-to-female ratio of 2.6 (Table 2). Median attributable trip duration for those with MCL was 28 days (range, 7–273 days; IQR, 14–181 days) (Table 2). Almost a quarter of returned travellers with MCL required inpatient management of their disease (Table 2). Leishmania Viannia braziliensis was identified in all 14 cases of MCL for whom a causative species was reported. We do not have information on the immune status of those travellers and migrants with MCL; therefore it is unknown if immunosuppression contributed to these presentations.
Case clustering was noted in 4.3% (n = 41) of cases, with most of the case clusters having travelled to Bolivia. Figure 2 represents cases of CL and MCL by year of presentation to a GeoSentinel site, along with the number of cases of CL/MCL per 10 000 travellers in the GeoSentinel database. Over the past decade cases of CL/MCL per 10 000 travellers encountered annually in the network has slowly increased from under 30 to 35–40 (Figure 2).
Figure 2.
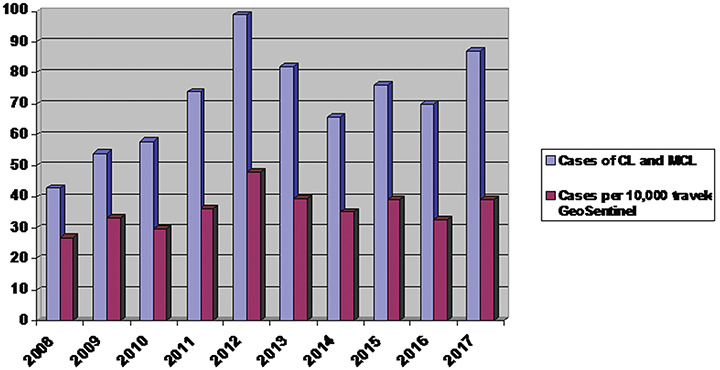
Year of presentation of returned travellers or new immigrants presenting to a GeoSentinel Surveillance Network site for travel-acquired cutaneous or mucocutaneous leishmaniasis, 2008–2017*. *Visit dates between 1 January 2017 and 31 August 2017; year 2017 extrapolated to full year. Prior to 2008, less than 40 surveillance sites contributed data and less than 15 000 total records entered per year, thus, only data from past 10 years included.
Discussion
CL is a potentially emerging vector-borne disease of international travellers and migrants, groups for whom large-scale, global, multi-site data on travel preponderances of the disease are lacking. Surveillance data are critical to understanding the emergence of vector-borne diseases in new areas and transmission patterns over time and to informing diagnostic and therapeutic guidelines. Key features alerting clinicians to the possibility of CL in returning travellers are highlighted in Box 1. We have described the collective experience of our network with CL and MCL in travellers and migrants over a 20-year period, which is the largest such study to date.
Box 1. When to think about cutaneous leishmaniasis and how to diagnose it
Who: traveller or migrant
What: ulcerative, nodular, or verrucous skin lesion
When: presenting typically within a few months of travel
Where: Central or South America, Mediterranean or the Middle East
How (to diagnose): lesion scraping, brushing, impression, aspirate, or biopsy sent for microscopy, culture, and/or PCR.
New World CL Was Imported by Tourists Who Are at Risk of Future MCL/ML
Imported CL in our population was most often a disease of tourist travellers, particularly to areas such as Bolivia where risk of acquiring L. V. braziliensis and subsequent MCL is high for those visiting at risk areas. It is estimated that 5–10% of those with CL due to L. V. braziliensis will go on to develop MCL in the future,25–27 though whether these data from endemic regions can be extrapolated to travellers is unknown. A recent analysis of Israeli travellers returning from Bolivia with CL documented that almost 12% developed ML and that a lack of systemic treatment of the initial CL was associated with future mucosal involvement.2 Among previously untreated patients with CL, 41% developed ML compared to 3% of patients treated with a systemic antileishmanial regimen.2 The true risk of late mucosal involvement following CL in travellers is difficult to estimate for several reasons, including the lack of accurate denominator due to the infrequent and self-healing nature of much CL, the prolonged follow-up of travellers required to estimate the incidence of mucosal involvement28,29, the years-long latency of MCL potentially contributing to a lack of perceived association with specific prior travel and a potential selection bias towards inclusion of more complicated, persistent and relapsing forms of CL.30 The Andean countries of Peru and especially Bolivia appear to carry the highest relative risk of MCL following CL due to L. V. braziliensis.2,31,32 Thus, it is a particular concern that both these countries were in the top 5 source countries for cases among tourists, missionaries, volunteers, researchers, aid workers and business travellers. However, it appears that MCL in travellers tends to be mild in nature and responsive to treatment, perhaps related partly to the rapidity with which travellers tend to present for care of mucosal symptoms compared to what is observed in endemic areas, where MCL can present in a severe, mutilating manner with failure of treatments.3,27,33–36 Our findings support recommendations for careful and prolonged clinical follow-up of travellers returning from Bolivia and Peru with CL, and, given the proportionate representation of L. V. braziliensis in this cohort, that most CL in travellers from these regions should be considered for treatment with systemic therapy, particularly those who have acquired L. V. braziliensis in Peru, Bolivia or Brazil.37–39
Costa Rica also emerged in this analysis as a top source country for New World CL in tourist travellers. Over the past three decades, Costa Rica has gained increasing popularity as a destination for ecotourism due to its political stability, accessibility, biodiversity, climate and ecology, which combines beach destinations, volcanoes and jungle regions in a relatively small geographic footprint. Next to Nicaragua and Panama, Costa Rica contributes the greatest number of cases of CL to the burden in Central America,40 and despite its classification as a high-income country, ~6% of Costa Ricans continue to live in extreme poverty.41 Coupled with well-known mammalian reservoirs such as rodents and sloths, rural poverty intersecting with ecology to which sandfly vectors are perfectly adapted continue to challenge the control of CL in Costa Rica. With close to 3 million annual tourist arrivals to Costa Rica, and a 1–2% year-to-year increase,42 CL cases in tourists to Costa Rica are likely to continue to emerge.
Old World CL Was Imported by Migrants and VFRs
For VFRs and migrants in this analysis, top countries of acquisition were predominantly in the Middle East (Afghanistan, Syria, Iran) or North Africa (Tunisia, Morocco, Algeria), areas that are intermittently affected by regional conflicts and political instability, suggesting that as mass migration of refugees continues, CL will be increasingly encountered in intake countries. Thus, it is critical that intake programming includes initiatives to enhance awareness of CL and ensures adequate availability of diagnostic tests and therapeutic options, ideally with access to local therapies that should be favoured in simple Old World CL37 (and are now discussed in New World CL38) to reduce associated morbidity in these vulnerable populations, particularly children.
Short-Term and Non-‘Exotic’ Travel Carry Risk for CL
Our finding that many travellers acquired their illness on trips lasting ≤ 2 weeks challenges the notion that CL is a disease of prolonged travel. One in six tourists and the same proportion of business travellers acquired CL while travelling to an endemic area for less than 2 weeks, and 3% of travellers had travelled for 1 week or less. Furthermore, one in eight travellers with MCL acquired their disease on a trip lasting ≤ 2 weeks. Interestingly, two in five travellers with CL and more than half with MCL in this cohort had sought a pre-travel medical consultation, suggesting that measures for prevention of arthropod bites were either poorly communicated, ignored, or ineffective (e.g. mosquito nets would have little effect on the prevention of CL).43 The lack of a vaccine, effective chemoprophylaxis and good mapping of regional transmission intensity are obstacles to effective prevention. More than half of those with CL and almost three-quarters of those with MCL in this analysis were tourists. This finding runs counter to the common view that leishmaniasis is of minimal risk during tourist travel, a perception that is corroborated the limited information available for CL on expert travel websites such as CDC’s Traveler’s Health (https://wwwnc.cdc.gov/travel/) and the Government of Canada’s Travel and Tourism site (https://travel.gc.ca/). Our findings suggest a change in the way many tourists travel—visiting more remote locations, living under more basic conditions or being less covered by clothing—represents a pattern that may be associated with a wider range of arthropod vector exposures and health risks. This finding could also represent referral bias at our centres, which mostly serve a tourist population.
MCL Is Primarily Imported From Bolivia and Other Andean Countries
MCL was almost exclusively imported from South and Central America, predominantly by men of all ages. Overall, only 10% of MCL cases were imported from the Old World. Although all cases of MCL where causative species was recorded were due to L. V. braziliensis in this analysis, echoing the findings of others,2 non-braziliensis species including L. V. panamensis and L. V. guyanensis, both well represented in this analysis, accounting for over a fifth of those with CL and species identification, have also been associated with MCL.29,44,45 Again, it is unknown if non-braziliensis strains acquired in the at-risk regions of northern South America or Central America will confer risk of future MCL in travellers, as anecdotal clinical experience suggests that it is uncommon. Prospective long-term studies are required to fill this knowledge gap.
Almost three-quarters of travellers with MCL in this analysis were male, a finding that has been documented previously29,46 and may be explained by increased susceptibility,46 or by a higher likelihood of riskier ‘adventure’ travel. Other known and postulated risk factors for the development of MCL include large lesions, head and neck localization, lesions present for > 4 months, micronutrient deficiency and immunosuppression,38,46 none of which were assessed in this analysis.
Almost a quarter of those with MCL in this analysis (which is a likely underestimate) required inpatient management of their leishmaniasis, likely because standard treatment with pentavalent antimonials or liposomal formulations of amphotericin B (now favoured over non-liposomal amphotericin B deoxycholate) requires close monitoring to prevent and detect complications, which can include cardiac arrhythmia, hepatitis, pancreatitis, thrombocytopenia and acute kidney injury.37 Drug toxicities, infusion reactions and local drug licencing are barriers to in-home treatment, often leading to admission to hospital wards, medical day units or the emergency department for daily infusions. Miltefosine is a well-tolerated and FDA-approved oral option for the treatment of New World CL and MCL, though published data on its use in travellers are limited.37
Limitations and Approaches
There are several limitations of this analysis. First, attribution of specific country of exposure is difficult in the setting of a multi-country itinerary. We resolved such cases down to region of exposure with manual review of records and classification of countries into strata based on level of endemicity. Second, our data pertain to ill travellers with clinical features suggestive of tegumentary leishmaniasis presenting to a GeoSentinel clinic and may not extend to all ill returned travellers. Given the complex nature of CL and MCL diagnosis and treatment, we feel that the cases evaluated at GeoSentinel sites would likely be representative of all imported cases, and probably generalizable to the broader population. Third, only a quarter of cases of CL or MCL in the database were assigned a definitive causative species, thereby limiting our ability to draw conclusions about associations based on species. Fourth, the GeoSentinel Surveillance Network captures epidemiologic data pertaining to ill returning international travellers and is not designed to collect comprehensive or objective clinical and laboratory details. Furthermore, as one of the criteria for entry into GeoSentinel is recent international travel, our database misses those individual travellers presenting for care at a GeoSentinel site, but whose disease was acquired locally. Thus, for countries where local transmission of leishmaniasis occurs (e.g. Israel, France, Spain, Italy and US), our GeoSentinel data from sites within those countries only reflects imported cases. Fifth, we are unable to provide data on incubation period for CL and MCL entered into the database prior to mid-2013, as prior to that, date of symptom onset had not yet been added to the GeoSentinel data collection instrument. Sixth, due to the structure of many GeoSentinel sites, children are under-represented in the database. Seventh, there is only a single code for mucosal or MCL in the database, thereby eliminating our ability to determine the type of mucosal involvement (e.g. primary isolated ML versus intercurrent CL and ML). Similarly, we lack data on the possible contribution of immunosuppression to the cases of MCL. Eighth, species identification was recorded for only 30% of cases, limiting our understanding of true molecular epidemiology of CL and MCL/ML in travellers. Ninth, ~12% of CL cases were not microbiologically confirmed but were rather diagnosed on clinical, epidemiological and treatment response grounds with exclusion of alternate diagnoses. In only one case of MCL, the diagnosis status was probable. Finally, calculation of incidence rates for CL and MCL is impossible as the denominator of all travellers from all countries to specific regions is unavailable.47
In summary, CL may be an emerging disease among travellers, and to date, there have been no large-scale multi-site epidemiologic surveillance reports on this infection imported to non-endemic areas, and few MCL cases among travellers have been reported in the peer-reviewed literature. As cases of CL and MCL are often not tracked at national levels under notifiable disease programmes, understanding the scope of imported CL and MCL to non-endemic areas is essential for adequate resourcing of diagnostic procedures and potential therapies, such as liposomal amphotericin B, oral miltefosine, paromomycin ointment and pentavalent antimonials, which are often difficult to acquire on short-notice in non-endemic countries or have restricted access. Our data challenge the common perception that acquisition of cutaneous or mucosal leishmaniasis requires prolonged travel to an unusual destination, and underscore that with mass migration of refugees from areas of conflict and political instability, familiarity with and planning for imported cases are required.
Acknowledgments
Additional members of the GeoSentinel Surveillance Network who contributed data but did not author this article are Frank von Sonnenburg and Camilla Rothe (Munich, Germany), Sabine Jordan and Christof Vinnemeier (Hamburg, Germany), Cedric Yansouni (Montreal, Canada), Anne McCarthy (Ottawa, Canada), Mogens Jensenius (Oslo, Norway), Abraham Goorhuis (Amsterdam, The Netherlands), Christina Coyle (New York, New York, USA), Frank Mockenhaupt and Gundel Harms-Zwingengerger (Berlin, Germany), Daniel Leung and Scott Benson (Salt Lake City, Utah, USA), Philippe Gautret and Emilie Javelle (Marseille, France), Francois Chappuis (Geneva, Switzerland), Christophe Rapp and Cecile Ficko (Saint-Mande, France), Perry van Genderen (Rotterdam, The Netherlands), Hedvig Glans (Stockholm, Sweden), Michael Beadsworth and Nicholas Beeching (Liverpool, UK), Francesco Castelli and Alberto Matteelli (Brescia, Italy), Katherine Plewes and Yazdan Mirzanejad (Vancouver, Canada), Rogelio Lopez-Velez and Sandra Chamorro (Madrid, Spain), Jesse Waggoner and Henry Wu (Atlanta, Georgia, USA), Karin Leder and Joseph Torresi (Victoria, Australia), Emmanuel Bottieau and Ralph Huits (Antwerp, Belgium), Lin Chen and Daniel Bourque (Cambridge, Massachusetts, USA), Jonathan Alpern and William Stauffer (St. Paul, Minnesota, USA), John Cahill and Ben Wyler (New York, New York, USA), Jean Haulman and Anne Terry (Seattle, Washington, USA), Carmelo Licitra and Ashley Taylor (Orlando, Florida, USA), Cecilia Perret Perez and Thomas Weitzel (Santiago, Chile), Effrossyni Gkrania-Klotsas and Ben Warne (Cambridge, UK), Patricia Schlagenhauf and Rainer Weber (Zurich, Switzerland), Carsten Schade Larsen and Christian Wejse (Aarhus, Denmark), Elizabeth Barnett and Natasha Hochberg (Boston, Massachusetts, USA), Sapha Barkati and Jean Vincelette (Montreal, Canada), Israel Molina (Barcelona, Spain), Denis Malvy and Alexandre Duvignaud (Bordeaux, France), Marc Mendelson and Salim Parker (Cape Town, South Africa), Victoria Johnston and Vanessa Field (London, UK), Susan Kuhn (Calgary, Canada), Watcharapong Piyaphanee and Udomsak Silachamroon (Bangkok, Thailand), Marta Diaz-Menendez (Madrid, Spain), Paul Kelly (New York, New York, USA), Lucille Blumberg and Albie de Frey (Johannesburg, South Africa), Prativa Pandey and Bhawana Amatya (Kathmandu, Nepal), Kunjana Mavunda (Miami, Florida, USA), Mauro Saio (Nairobi, Kenya).
Contributor Information
GeoSentinel Surveillance Network:
Frank von Sonnenburg, Camilla Rothe, Sabine Jordan, Christof Vinnemeier, Cedric Yansouni, Anne McCarthy, Mogens Jensenius, Abraham Goorhuis, Christina Coyle, Frank Mockenhaupt, Gundel Harms-Zwingengerger, Daniel Leung, Scott Benson, Philippe Gautret, Emilie Javelle, Francois Chappuis, Christophe Rapp, Cecile Ficko, Perry van Genderen, Hedvig Glans, Michael Beadsworth, Nicholas Beeching, Francesco Castelli, Alberto Matteelli, Katherine Plewes, Yazdan Mirzanejad, Rogelio Lopez-Velez, Sandra Chamorro, Jesse Waggoner, Henry Wu, Karin Leder, Joseph Torresi, Emmanuel Bottieau, Ralph Huits, Lin Chen, Daniel Bourque, Jonathan Alpern, William Stauffer, John Cahill, Ben Wyler, Jean Haulman, Anne Terry, Carmelo Licitra, Ashley Taylor, Cecilia Perret Perez, Thomas Weitzel, Effrossyni Gkrania-Klotsas, Ben Warne, Patricia Schlagenhauf, Rainer Weber, Carsten Schade Larsen, Christian Wejse, Elizabeth Barnett, Natasha Hochberg, Sapha Barkati, Jean Vincelette, Israel Molina, Denis Malvy, Alexandre Duvignaud, Marc Mendelson, Salim Parker, Victoria Johnston, Vanessa Field, Susan Kuhn, Watcharapong Piyaphanee, Udomsak Silachamroon, Marta Diaz-Menendez, Paul Kelly, Lucille Blumberg, Albie de Frey, Prativa Pandey, Bhawana Amatya, Kunjana Mavunda, and Mauro Saio
Author contributions
All authors serve as guarantors of the work, and all critically appraised the manuscript for content. A.K.B.—study conception and design; construction and querying of study database; data collection, analysis and interpretation; drafting the manuscript; revision and critical appraisal of the manuscript. E.C.—data collection and interpretation; revision and critical appraisal of the manuscript. M.P.G.—data collection and interpretation; revision and critical appraisal of the manuscript. E.S.—data collection and interpretation; revision and critical appraisal of the manuscript. N.A.H.—data collection and interpretation; revision and critical appraisal of the manuscript. B.A.C.—data collection and interpretation; revision and critical appraisal of the manuscript. S.C.—data collection and interpretation; critical appraisal of the manuscript. P.P.—data collection and interpretation; revision and critical appraisal of the manuscript. J.S.K.—data collection and interpretation; critical appraisal of the manuscript. M.L.—data collection and interpretation; revision and critical appraisal of the manuscript. T.N.—data collection and interpretation; revision and critical appraisal of the manuscript. A.J.S.—data interpretation; revision and critical appraisal of the manuscript. M.S.—data interpretation; critical appraisal of the manuscript. H.A.—data collection and interpretation; revision and critical appraisal of the manuscript. D.H.H.—data collection and interpretation; revision and critical appraisal of the manuscript. K.C.K.—study design; data collection and interpretation; revision and critical appraisal of the manuscript.
Funding
GeoSentinel, the Global Surveillance Network of the International Society of Travel Medicine (ISTM), is supported by Cooperative Agreement 5 NU50CK000478-02-00 from the Centers for Disease Control and Prevention (CDC), as well as the ISTM and Public Health Agency of Canada (PHAC). The GeoSentinel Surveillance Network has independent Data Use and Publications Committees that oversee analyses of the database from conception to final knowledge product and comprise of a selection of elected site directors outside of the CDC. Staff from the CDC were not involved in the design; analysis and interpretation of data; nor writing of the manuscript.
Conflict of interest: None declared.
References
- 1. Pavli A, Maltezou HC. Leishmaniasis, an emerging infection in travellers. Int J Infect Dis 2010; 14:e1032–9. [DOI] [PubMed] [Google Scholar]
- 2. Solomon M, Sahar N, Pavlotzky F et al. Mucosal leishmaniasis in travellers with Leishmania braziliensis complex returning to Israel. Emerg Infect Dis 2019; 25:642–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lawn SD, Whetham J, Chiodini PL et al. New world mucosal and cutaneous leishmaniasis: an emerging health problem among British travellers. QJM 2004; 97:781–8. [DOI] [PubMed] [Google Scholar]
- 4. Leder K, Torresi J, Libman M et al. GeoSentinel surveillance of illness in returned travellers, 2007–2011. Ann Intern Med 2013; 158:456–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Stevens MS, Geduld J, Libman M et al. Dermatoses among returned Canadian travellers and immigrants: surveillance report based on CanTravNet data, 2009–2012. CMAJ Open 2015; 3:E119–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization Control of the leishmaniasis: report of a meeting of the WHO Expert Committee on the Control of Leishmaniases, Geneva, 22–26 March 2010. WHO Technical Report Series 949 http://whqlibdoc.who.int/trs/WHO_TRS_949_eng.pdf (accessed 17 May 2019).
- 7. McHugh CP, Thies ML, Melby PC et al. Short report: a disseminated infection of Leishmania mexicana in an eastern wood rat, Neotoma floridana collected in Texas. Am J Trop Med Hyg 2003; 69:470–2. [PubMed] [Google Scholar]
- 8. Kerr SF, McHugh CP, Dronen NOJ. Leishmaniasis in Texas: prevalence and seasonal transmission of Leishmania mexicana in Neotoma micropus. Am J Trop Med Hyg 1995; 53:73–7. [PubMed] [Google Scholar]
- 9. Kerr SF, McHugh CP, Merkelz R. Short report: a focus of Leishmania mexicana near Tucson, Arizona. Am J Trop Med Hyg 1999; 61:378–9. [DOI] [PubMed] [Google Scholar]
- 10. Raymond RW, McHugh CP, Witt LR, Kerr SF. Temporal and spatial distribution of Leishmania mexicana in a population of Neotoma micropus. Mem Inst Oswaldo Cruz 2003; 92:171–80. [DOI] [PubMed] [Google Scholar]
- 11. Furner BB. Cutaneous leishmaniasis in Texas: report of a case and review of the literature. J Am Acad Dermatol 1990; 23:368–71. [PubMed] [Google Scholar]
- 12. Gustafson TL, Reed CM, McGreevy PB et al. Human cutaneous leishmaniasis acquired in Texas. Am J Trop Med Hyg 1985; 34:58–63. [DOI] [PubMed] [Google Scholar]
- 13. Wright NA, Davis LE, Aftergut KS, Parrish CA, Cockerell CJ. Cutaneous leishmaniasis in Texas: a northern spread of endemic areas. J Am Acad Dermatol 2008; 58:650–2. [DOI] [PubMed] [Google Scholar]
- 14. Maloney DM, Maloney JE, Dotson D, Popov VL, Sanchez RL. Cutaneous leishmaniasis: Texas case diagnosed by electron microscopy. J Am Acad Dermatol 2002; 47:614–6. [DOI] [PubMed] [Google Scholar]
- 15. Gramiccia M, Gradoni L. The current state of zoonotic leishmaniasis and approaches to disease control. Int J Parasitol 2005; 35:1169–80. [DOI] [PubMed] [Google Scholar]
- 16. McHugh CP, Melby PC, LaFon SG. Leishmaniasis in Texas: epidemiology and clinical aspects of human cases. Am J Trop Med Hyg 1996; 55:547–55. [DOI] [PubMed] [Google Scholar]
- 17. Clarke CF, Bradley KK, Wright JH, Glowicz J. Case report: emergence of autochthonous cutaneous leishmaniasis in northeastern Texas and southeastern Oklahoma. Am J Trop Med Hyg 2013; 88:157–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Douvoyiannis M, Khromachou T, Byers N, Hargreaves J, Murray HW. Cutaneous leishmaniasis in North Dakota. Clin Infect Dis 2014; 59:e73–5. [DOI] [PubMed] [Google Scholar]
- 19. González C, Wang O, Strutz SE et al. Climate change and risk of leishmaniasis in North America: predictions from ecological niche models of vector and reservoir species. PLoS Negl Trop Dis 2010; 4:e585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. European Centre for Disease Prevention and Control Phlebotomine sandflies—distribution map. http://www.ecdc.europa.eu/en/activities/diseaseprogrammes/emerging_and_vector_borne_diseases/Pages/VBORNET_maps_sandflies.aspx?MasterPage=1 (accessed 17 May 2019).
- 21. Dujardin J-C, Campino L, Cañavate C et al. Spread of vector-borne diseases and neglect of leishmaniasis, Europe. Emerg Infect Dis 2008; 14:1013–8http://wwwnc.cdc.gov/eid/article/14/7/07-1589.htm (accessed 17 May 2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lachaud L, Dedet JP, Marty P et al. Working Group for the Notification of human Leishmanioses in France. Surveillance of leishmaniases in France, 1999 to 2012. Euro Surveill 2013; 18:18. [PubMed] [Google Scholar]
- 23. Wilder-Smith A, Boggild AK. Sentinel surveillance in travel medicine: twenty years of GeoSentinel publications (1999–2018). J Travel Med 2018; 25. doi 10.1093/jtm/tay139. [DOI] [PubMed] [Google Scholar]
- 24. Leder K, Tong S, Weld L et al. GeoSentinel surveillance network. Illness in travellers visiting friends and relatives: a review of the GeoSentinel surveillance network. Clin Infect Dis 2006; 43:1185–93. [DOI] [PubMed] [Google Scholar]
- 25. Reithinger R, Dujardin JC, Louzir H, Pirmez C, Alexander B, Brooker S. Cutaneous leishmaniasis. Lancet Infec Dis 2007; 7:581–96. [DOI] [PubMed] [Google Scholar]
- 26. Arevalo J, Ramirez L, Adaui V et al. Influence of Leishmania (Viannia) species on the response to antimonial treatment in patients with American tegumentary leishmaniasis. J Infect Dis 2007; 195:1846–51. [DOI] [PubMed] [Google Scholar]
- 27. Blum J, Buffet P, Visser L et al. LeishMan recommendations for treatment of cutaneous and mucosal leishmaniasis in travellers, 2014. J Travel Med 2014; 21:116–29. [DOI] [PubMed] [Google Scholar]
- 28. Schleucher RD, Zanger P, Gaessler M, Knobloch J. Successful diagnosis and treatment 50 years after exposure: is mucocutaneous leishmaniasis still a neglected differential diagnosis? J Travel Med 2008; 15:466–7. [DOI] [PubMed] [Google Scholar]
- 29. Jara M, Valencia BM, Adaui V et al. Quantitative kinetoplast DNA assessment during treatment of mucosal leishmaniasis as a potential biomarker of outcome: a pilot study. Am J Trop Med Hyg 2016; 94:107–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Laynez-Roldán P, Fuertes I, Almuedo A et al. Sporotrichoid dissemination of cutaneous leishmaniasis possibly triggered by a diagnostic puncture. J Travel Med 2019; pii: taz044. doi: 10.1093/jtm/taz044. [DOI] [PubMed] [Google Scholar]
- 31. Garcia AL, Parrado R, Rojas E et al. Leishmaniases in Bolivia: comprehensive review and current status. Am J Trop Med Hyg 2009; 80:704–11. [PubMed] [Google Scholar]
- 32. David C, Dimier-David L, Vargas F, Torrez M, Dedet JP. Fifteen years of cutaneous and mucocutaneous leishmaniasis in Bolivia: a retro-spective study. Trans R Soc Trop Med Hyg 1993; 87:7–9. [DOI] [PubMed] [Google Scholar]
- 33. Franke ED, Wignall FS, Cruz ME et al. Efficacy and toxicity of sodium stibogluconate for mucosal leishmaniasis. Ann Intern Med 1990; 113:934–40. [DOI] [PubMed] [Google Scholar]
- 34. Soto J, Toledo J, Valda L et al. Treatment of Bolivian mucosal leishmaniasis with miltefosine. Clin Infect Dis 2007; 44:350–6. [DOI] [PubMed] [Google Scholar]
- 35. Amato VS, Tuon FF, Bacha HA, Neto VA, Nicodemo AC. Mucosal leishmaniasis. Current scenario and prospects for treatment. Acta Trop 2008; 105:1–9. [DOI] [PubMed] [Google Scholar]
- 36. Amato VS, Tuon FF, Siqueira AM, Nicodemo AC, Neto VA. Treatment of mucosal leishmaniasis in Latin America: systematic review. Am J Trop Med Hyg 2007; 77:266–74. [PubMed] [Google Scholar]
- 37. Aronson N, Herwaldt BL, Libman M et al. Diagnosis and treatment of leishmaniasis: clinical practice guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). Clin Infect Dis 2016; 63:e202–64. [DOI] [PubMed] [Google Scholar]
- 38. Blum J, Lockwood DNJ, Visser L et al. Local or systemic treatment for New World cutaneous leishmaniasis? Re-evaluating the evidence for the risk of mucosal leishmaniasis. Int Health 2012; 4:153–63. [DOI] [PubMed] [Google Scholar]
- 39. Hodiamont CJ, Kager PA, Bart A et al. Species-directed therapy for leishmaniasis in returning travellers: a comprehensive guide. PLoS Negl Trop Dis 2014; 8:e2832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Alvar J, Vélez ID, Bern C et al. The WHO leishmaniasis control team. Leishmaniasis worldwide and global estimates of its incidence. PLoS One 2012; 7:e35671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hotez PJ, Woc-Colburn L, Bottazzi ME. Neglected tropical diseases in Central America and Panama: review of their prevalence, populations at risk and impact on regional development. Int J Parasitol 2014; 44:597–603. [DOI] [PubMed] [Google Scholar]
- 42. World Tourism Organization Yearbook of Tourism Statistics dataset, 2018. Data updated 06 December 2018. https://www.e-unwto.org/doi/abs/10.5555/unwtotfb0188011120132017201806 (accessed 17 May 2019).
- 43. Schofield S, Plourde P. Committee to advise on tropical medicine and travel (CATMAT). Statement on personal protective measures to prevent arthropod bites. Can Commun Dis Rep 2012; 38:1–18www.phac-aspc.gc.ca/publicat/ccdr-rmtc/12vol38/acs-dcc-3/index-eng.php (accessed 17 May 2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Santrich C, Segura I, Arias AL, Saravia NG. Mucosal disease caused by Leishmania braziliensis guyanensis. Am J Trop Med Hyg 1990; 42:51–5. [DOI] [PubMed] [Google Scholar]
- 45. Oliveira Guerra JA, Prestes SR, Silveira H et al. Mucosal leishmaniasis caused by Leishmania (Viannia) braziliensis and Leishmania (Viannia) guyanensis in the Brazilian Amazon. PLoS Negl Trop Dis 2011; 5:e980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Machado-Coelho GL, Caiaffa WT, Genaro O, Magalhães PA, Mayrink W. Risk factors for mucosal manifestation of American cutaneous leishmaniasis. Trans R Soc Trop Med Hyg 2005; 99:55–61. [DOI] [PubMed] [Google Scholar]
- 47. Leder K, Steffen R, Cramer JP et al. Risk assessment in travel medicine: how to obtain, use, and interpret risk data for informing pre-travel advice. J Travel Med 2015; 22:13–20. [DOI] [PubMed] [Google Scholar]


