Abstract
Rapid transmission of the severe acute respiratory syndrome coronavirus 2 has led to the novel coronavirus disease 2019 (COVID-19) pandemic. The current emphasis is on preventive strategies such as social distancing, face mask, and hand washing. The technique of nasopharyngeal wash to prevent the virus from inhabiting and replicating in the nasal and pharyngeal mucosa has been suggested to be useful in reducing symptoms, transmission, and viral shedding in cases of viral acute respiratory tract infections. In rapid systematic review, we found studies showing some improvement in prevention and treatment of upper respiratory tract infections. We postulate that hypertonic saline gargles and nasal wash may be useful in prevention and for care of patients with COVID-19. The present evidence emphasizes the need of randomized controlled trials to evaluate the role and mechanism of nasopharyngeal wash in COVID-19.
KEY WORDS: Coronavirus, COVID-19, jal-neti, nasal irrigation, nasal wash, oral gargles
INTRODUCTION
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) leading to the novel coronavirus disease 2019 (COVID-19) has a rapid human to human transmission of the virus through droplet infection and aerosols.[1,2] One infected case of COVID-19 on an average infects 3 new cases, the reproductive number (R0) being 3 for SARS-CoV-2.[3] Since this is a novel viral infection in humans, antiviral drugs, and vaccines have not yet been developed for this illness. Thus, the major emphasis is on social distancing, hand wash, and facemask.
The route of entry for SARS-CoV-2 is either through the nose mouth and eyes. Similar to the concept of hand washing, flushing of the nose and mouth; the portals of entry of the virus to the respiratory tract; may bring down the viral load; reduce transmission, symptoms, and duration of illness. Reduction of viral load with hypertonic saline gargles and nasal wash may bring down the transmission to close-contacts and subsequently prevent viral infections in nasopharynx.
Japan was the second country to contract COVID 19 infection after China. However, so far, it has infectivity of only 60 cases and death rate of 1.0 case per million population. It is quite low in comparison to majority of the countries.[4] Social distancing, facemask, and hand washing are the most important measures to halt the progression of the virus. In Japan, they also practice warm saline oral gargles and it is also included in the flu management guidelines of the country.[5] During gargles throat gets washed with warm saline. On similar lines the process of nose and stomach wash has also been described in yoga and has been called as ”Jalneti” and “Kunjal” respectively.[6]
The purpose of this review of literature is to analyze the efficacy of oral gargles and nasal wash in improvement of symptoms, reduction in viral load and transmission in cases of acute upper respiratory tract infections (URTI). We hypothesize that this technique may work in prevention and care of some subset of patients with COVID-19.
METHODS
Randomized controlled trials (RCTs), case–control and cohort studies comparing nasal saline treatment/gargling/steam inhalation/kunjal/stomach saline wash with at least one other intervention or placebo. Studies with population groups including adults and children diagnosed with acute upper respiratory tract infections (URTIs) were included. URTIs comprised of: rhinitis, rhinosinusitis, sinusitis, pharyngitis, otitis media, tonsillitis, common cold, and influenza. The following interventions were included:
Nasal wash including isotonic and hypertonic solutions compared with a placebo
Gargling saline or tea compared with other standard treatment
Kunjal/stomach saline wash compared with standard treatment
Steam inhalation compared with standard treatment.
We excluded studies applying another therapy where saline was used as a control treatment. We excluded studies involving patients with allergic respiratory symptoms, chronic respiratory infections, or chronic diseases with respiratory features, such as cystic fibrosis, or those recovering from sinus surgery. We also included the studies that examined the prevention of developing URTIs from regular use of saline wash.
Outcome measures
Primary outcomes
Change in onset or severity of acute URTI-related symptoms (e.g. nasal discharge, congestion, sneezing, headache, sore throat, and fever) over periods up to 28 days
Time to resolution of symptomatic illness.
Secondary outcomes
Viral shedding
Transmission to household contacts
Adverse events associated with treatment.
Days or work or school.
Antibiotic and URTI medication use.
Electronic searches
PRISMA guidelines were followed and an initial search was conducted on PubMed, SCOPUS, and Web of Science.[7] Later, the search was modified for Embase and Medline, and ProQuest on April 6, 2020. The search was restricted for the past 10 years (2010–2020) and did not included key-terms such as “animal/s,” “mice,” and “mouse.” We applied English language or publication limitation. Cross-referencing was done by going through the bibliographies of the retrieved studies.
Search Strategy
We prepared a comprehensive search strategy for all interventions. For the first intervention group, we included “neti,” “jal neti,” “nasal wash,” “nasal rinse,” “nasal irrigation,” “nasal spray,” “nasal lavage,” “hypertonic,” “isotonic,” “saline,” “gargling,” “steam inhalation,” “kunjal,” and “stomach saline wash” terms. Study population was defined as cases of “rhinitis,” “rhinosinusitis,” “sinusitis,” “common cold,” “upper respiratory tract infection,” “coronavirus,” and “rhinovirus.” Irrelevant articles were excluded through limiting our search to the title and abstract.
RESULTS
A PRISMA flow chart [Figure 1] shows the search results of various databases and the final included articles for the analysis were eight; one for combined nasal wash and oral gargles, four for oral gargles, and three for nasal wash. All the articles and their characteristics are listed in Table 1. For the evaluation of Kunjal and steam inhalation, we could not include any article. The four studies with oral gargles as an intervention in healthy volunteers of varying age groups of children, teenagers, adults, and elderly, respectively. All studies were conducted in Japan from 2001 to 2012.
Figure 1.
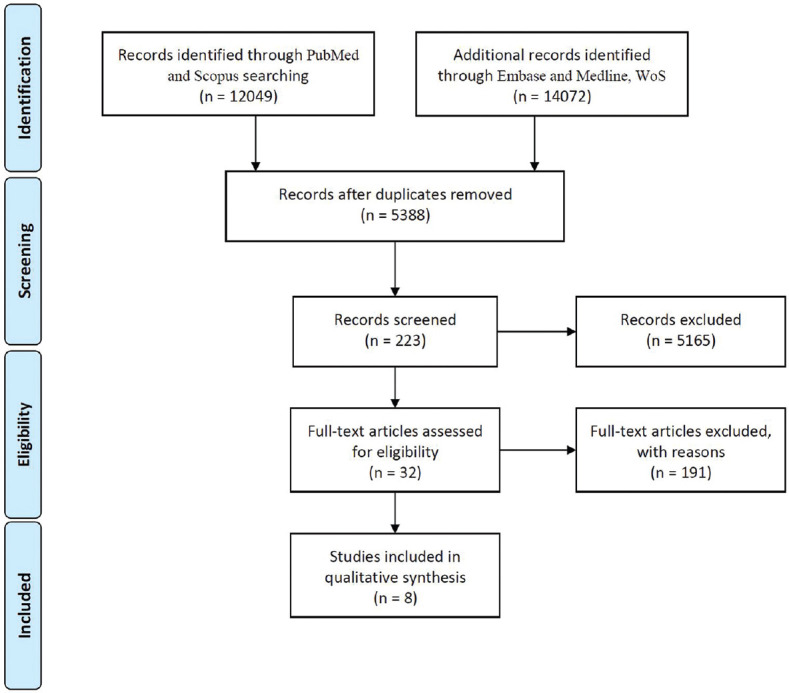
PRISMA flow diagram depicting the search process for inclusion and exclusion of articles
Table 1.
Characteristics of the studies analyzed
| Study | Methods | Participants characteristics | Intervention | Outcome | OR (95%CI) |
|---|---|---|---|---|---|
| Oral gargles | |||||
| Satomura et al., 2005[8] (Japan) | RCT 3 groups randomly |
Healthy volunteers in the ages of 18-65 years | 1. Gargles (n=104) 2. Iodine (n=119) 3. Usual care (n=115) Observed for 60 days |
1.First URTI 2. Symptom score |
Incidence rate in intervention versus control group was 0.64 (95% CI 0.41-0.99) and 0.89 (95% CI 0.60-1.33). Positive effect in URTI prevention |
| Yamada et al., 2006[10] (Japan) | Prospective nonrandomized controlled trial | Elderly >65 years | Gargling 3/day for 3 months Tea group (n=76) Water group (n=48) |
Incidence of Influenza | Incidence of influenza was less in group gargling with tea (OR=15.711; 95% CI 1.883-399.658, P=0.028). Positive effect in Influenza prevention |
| Noda et al., 2012[9] (Japan) | Prospective nonrandomized controlled trial | 145 schools 19,595 children in 2-6 years of age group |
1. Gargle group (n=15859): tap water, saline, green tea 2. No gargle (n=3736) observed for 20 days |
1. Fever 2. Sickness absence |
Odds of developing fever was significantly lower in children practicing gargles with either green tea (0.32) or water (0.70). Positive effect in fever prevention |
| Ide et al., 2014[11] (Japan) | Randomized, open label controlled trial | 757 high school students (15-17 years of age) was conducted in 6 schools during flu season | 1. Green tea gargling (n=384) 2. Water gargling (n=363) Both gargled 3/day for 90 days |
Incidence of Influenza | No significant difference in incidence of influenza in the two groups (P=0.24) |
| Oral gargles and nasal wash | |||||
| Ramalingam et al., 2019[18] (Scotland) | Randomized controlled trial, open labeled | Within 48 hours of onset of URTI in otherwise healthy adults | Intervention: Hypertonic saline nasal irrigation and gargles (n=32) Control: No intervention (n=34) |
Duration of illness, over the counter medication use, transmission to household contacts, viral shedding | In the intervention arm, duration of illness was lower by 1.9 days (P=0.01), OTCM use by 36% (P=0.004), transmission within household contacts by 35% (P=0.006) and viral shedding by ≥0.5 log10/day (P=0.04). Positive effect in URTI treatment |
| Nasal wash | |||||
| Wang et al., 2009[13] (Taiwan) | Randomized, placebo-controlled trial | Children with acute sinusitis | Nasal saline irrigation: 30 No irrigation: 39 |
PRQLQ, nPEFR test, nasal smear examination, radiography | Normal saline wash had significantly improved mean PRQLQ values and nPEFR values compared to group who did not perform the nasal wash (P<0.05). Positive effect in acute sinusitis |
| King et al., 2015[17] (Cochrane systematic review) | Included 5 studies Adam et al., 1998[14] Bollag et al., 1984[15] Slapak et al., 2008[16] Wang et al., 2009[13] King et al., 2012 (unpublished)** |
544 children (3 studies) and 205 adults (2 studies) with acute URTIs <4 weeks. (Rhinosinusitis, pharyngitis, otitis media, tonsillitis, common cold and influenza were included in URTI) |
Nasal lavage, irrigation or topical nasal saline compared with a placebo or standard treatment | Change in severity of acute URTI-related symptoms, time to resolution of symptomatic illness, adverse outcome associated with technique, loss of work/school, antibiotic or over the counter medication use |
The studies analysed were small and had methodological issues. Larger studies with defined outcomes are required to establish the role of nasal saline wash in reducing the severity and duration of URTI |
| Köksal et al., 2016[12] (Turkey) | Randomized, controlled, double blind | Children (<2 years) with URTI | Intervention Group A: Sea water: 38 Group B: Saline: 36 Control: 35 (no intervention) |
Nasal congestion, weakness, sleep quality, and nutrition | Nasal congestion, weakness, rhinorrhea, sleep quality: Was significantly lesser in children who received saline or seawater drops versus those who did not get the intervention Nasal Bleeding: No significant difference. Positive effect in nasal congestion |
**King D, Belt KM, Ware R, Askew D, Spurling G. A randomized control trial of isotonic saline nasal spray for symptoms of acute upper respiratory tract infections. Unpublished. RCT: Randomized controlled trial, CI: Confidence interval, URTI: Upper respiratory tract infection, OTCM: Over-the-counter medications, PRQLQ Pediatric Rhinoconjunctivitis Quality of Life Questionnaires, nPEFR: Nasal peak expiratory flow rate, OR: Odd’s ratio
Satomura et al. studied healthy adult volunteers from 2002 to 03; randomized to receive either water gargles or povidone-iodine gargles or standard care. The incidence and severity of influenza infection were studied. Of the 387 volunteers, 130 developed influenza. The incidence rates were 0.64 (95% confidence interval [CI] 0.41–0.99) and 0.89 (95% CI 0.60–1.33) for povidone-iodine and water group versus control who did not practice gargling.[8]
Another study by Noda et al.[9] studied 19595 children for 20 days in 2006 for the incidence of fever in two groups of children; one who gargled with tap water, green tea or saline water and another group who did not gargle. Lower odds of developing fever was there in the group of children who were gargling with green tea (odds ratio [OR] =0.32) or water (OR =0.70).
Yamada et al.[10] studied 124 elderly patients residing in nursing homes in 2005 with 76 performing gargles with tea extract and the 48 controls performing gargles with water. It was found that the group performing gargles with tea extract had a lower risk of developing influenza (OR =15.711; 95% CI 1.883–399.658, P = 0.028).
Ide et al.[11] performed a nonrandomized controlled study in December 2011-February 2012 comparing gargles with green tea (n = 384) versus water (n = 363) in teenagers attending high school. However, they did not report a lower risk of influenza in this age group with green tea versus water gargles (adjusted OR, 0.69; 95% CI, 0.37–1.28; P = 0.24).
In a randomized study in children who developed URTI conducted in Turkey in 2012 received either seawater nasal drops (n = 38), saline nasal drops (n = 36), or no intervention (n = 35). There was no significant difference in the seawater and saline group; however, the children who received these interventions had significant relief in nasal congestion, sleep, and nutrition in comparison to placebo.[12]
Another randomized controlled trial conducted in children with acute sinusitis in Taiwan compared 30 children who received nasal irrigation versus 39 who did not receive nasal irrigation.[13] It was found that nasal irrigation significantly improved the symptoms, quality of life and nasal expiratory flow rates (P < 0.05). A Cochrane meta-analysis included 5 studies in 2015.[13,14,15,16] They noted that there is probable improvement in symptoms, however, most studies were small and they did not have definitive outcomes and therefore larger studies were needed to substantiate the role of nasal saline wash in reducing the severity and duration of URTI symptoms, transmission, and medication usage.[17]
Subsequently in 2019 in a randomized open labeled trial, adults getting acute URTI in the last 48 h were randomized to perform oral gargles and nasal wash with hypertonic saline (n = 32) versus no intervention (n = 34). There was a significant reduction in the duration of illness, use of symptomatic medication, the transmission of household contacts, and viral shedding measured by sequential nasal swabs (P < 0.05).[18] Interestingly, the viral typing in this study revealed that 56% cases were due to rhinovirus and 31% coronaviruses.
DISCUSSION
In pathogenesis of COVID-19, hands play an important role by transporting virus from fomites mainly to nose and mouth. From mouth and nose virus spreads in the body. Saline wash of the nasal passage, mouth, and throat would probably eliminate or reduce viral load in the body mechanically at least in the initial stage of the pathogenesis [Figures 2 and 3]. This could be similar to hand washing to contain the spread of the infection. Therefore, hypertonic saline gargles and nasal wash may work in preventing the disease and may also be useful in reducing nasopharyngeal viral load to provide symptomatic relief. Further, it may reduce viral shedding and reduce the transmission of the illness. This may break the chain of infection. COVID 19 disease is mild in eighty percent of patients and resolves spontaneously. Therefore, nasopharyngeal wash may be useful especially in subgroup of the population at high risk such as subjects with comorbid conditions and above 60 years of age.
Figure 2.

The neti-pot used for the nasal saline wash
Figure 3.

Demonstration of the technique of nasal saline wash. The stream of saline water is flushed through one nostril and drained through the other with help of gravity; all throughout the process the person breathes through the mouth
Satomura et al.[8] found a reduced incidence of influenza in healthy adult volunteers practicing oral gargles versus those who did not practice gargles. Similarly, Noda et al.[9] noted a reduced incidence of fever in school going children practicing gargles versus those who were not. Fever was taken as marker of URTI in this age group in Japan. These Japanese studies analyzing the role of oral gargles noted reduced incidence rates of influenza in healthy adult and elderly volunteers, but not in teenage volunteers.[8,10,11]
Nasal saline drops reduced nasal congestion, weakness, rhinorrhea, and sleep quality in children <2 years who developed URTI.[12] Similarly, Wang et al.[13] found nasal saline wash benefited children with acute sinusitis in symptoms as assessed by the Pediatric Rhinoconjunctivitis Quality of Life Questionnaires. However, Cochrane meta-analysis emphasized the need of random control studies with larger number of subjects to substantiate beneficial effects of nasal wash.
Subsequently, in a random control trial Ramalingam et al.[18] noted that after the onset of viral illness, volunteers who were practicing hypertonic nasal saline irrigation and gargles had 36% lesser use of over-the-counter medications (P = 0.004), 35% lesser transmission (P = 0.006), and viral shedding (P = 0.04). Viral shedding was assessed by taking mid turbinate nasal swab by the patient.
The possible mechanism of action of hypertonic saline gargles and nasal wash is the chlorite ion; which the cells in nasal and pharyngeal mucosa convert to hypochlorous acid (HOCl), which has anti-viral properties.[19] This hypothesis is further substantiated by the fact that the HOCl is an active component of bleaching powder, which has antiviral properties and is used for disinfection for SARS-CoV-2, which is a single-stranded RNA virus. Halide salts have anti-viral properties on cell cultures also and inhibit RNA viruses.[20]
Saline is also used in washing and cleaning wounds traditionally. Probably, this therapy may also act similarly in providing relief in inflamed upper airways. Clearance of excess mucus, improving ciliary function thereby mucociliary clearance, decongestion, improving breathing, and reducing cough due to postnasal drip are the other potential mechanisms by which this technique may work.[21,22,23]
Limitations and adverse effects
COVID 19 infection starts in nasopharynx but involves lungs and other organs of the body. Therefore the effect of nasopharyngeal wash may have a limited action at nasopharynx; however, it may be more useful in prevention. The potential disadvantages of the nasal wash therapy are the discomfort in performing the procedure, however, in previous studies, it has been shown to be accepted in around 87% individuals.[18] The second disadvantage would be the possible transmission of viral infection through the equipment used for the wash and the area where the procedure is performed. This limitation could be addressed easily by maintaining strict measures with each person use one's own equipment with no sharing amongst each other. Further, the washbasin/sink where the procedure is performed can be cleaned postprocedure. Certain precautions should be followed prior to the procedure including the use of clean water which can be ensured by boiling and subsequently cooling it. The technique of learning of nasopharyngeal wash should be supervised initially.
Another point to be noted is that both nostrils should be open prior to performing the procedure.
CONCLUSION
In this rapid systematic review to evaluate effect of nasopharyngeal wash majority of studies had methodological limitations. However, few studies using hypertonic saline gargles and nasal wash showed to prevent symptoms and reduce transmission, symptoms, need for symptomatic medication, and viral loads in patients of the common cold. Its utility, however, has to be studied for SARS-CoV-2 which has significant mutations from the coronaviruses that causes the common cold.[23] Since it has been shown to work for a multitude of common viruses, logically, it should work for SARS-CoV-2 as well. The therapy could be studied as an easily available, and affordable add on modality to curb the transmission of the SARS-CoV-2. As we await definitive therapy to fight the pandemic this relative safe technique may give a ray of hope especially in prevention.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflict of interest.
REFERENCES
- 1.van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–7. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ong SW, Tan YK, Chia PY, Lee TH, Ng OT, Wong MS, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020 doi: 10.1001/jama.2020.3227. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu Y, Gayle AA, Wilder-Smith A, Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Travel Med. 2020;27 doi: 10.1093/jtm/taaa021. pii: taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.COVID-19 CORONA Virus Pandemic: Worldometer. [Last updated on 2020 April 14]. Available from: https://wwwworldometersinfo/coronavirus/
- 5.Pandemic Influenza Preparedness Action Plan of the Japanese Government. 2005. Dec 6, Available from: https://wwwmhlwgojp/english/topics/influenza/dl/pandemic02pdf .
- 6.Singh V. Kunjal: A nonspecific protective factor in management of bronchial asthma. J Asthma. 1987;24:183–6. doi: 10.3109/02770908709070936. [DOI] [PubMed] [Google Scholar]
- 7.Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Satomura K, Kitamura T, Kawamura T, Shimbo T, Watanabe M, Kamei M, et al. Prevention of upper respiratory tract infections by gargling: A randomized trial. Am J Prev Med. 2005;29:302–7. doi: 10.1016/j.amepre.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 9.Noda T, Ojima T, Hayasaka S, Murata C, Hagihara A. Gargling for oral hygiene and the development of fever in childhood: A population study in Japan. J Epidemiol. 2012;22:45–9. doi: 10.2188/jea.JE20100181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yamada H, Takuma N, Daimon T, Hara Y. Gargling with tea catechin extracts for the prevention of influenza infection in elderly nursing home residents: A prospective clinical study. J Altern Complement Med. 2006;12:669–72. doi: 10.1089/acm.2006.12.669. [DOI] [PubMed] [Google Scholar]
- 11.Ide K, Yamada H, Matsushita K, Ito M, Nojiri K, Toyoizumi K, et al. Effects of green tea gargling on the prevention of influenza infection in high school students: A randomized controlled study. PLoS One. 2014;9:e96373. doi: 10.1371/journal.pone.0096373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Köksal T, Çizmeci MN, Bozkaya D, Kanburoǧlu MK, Şahin Ş, Taş T, et al. Comparison between the use of saline and seawater for nasal obstruction in children under 2 years of age with acute upper respiratory infection. Turk J Med Sci. 2016;46:1004–13. doi: 10.3906/sag-1507-18. [DOI] [PubMed] [Google Scholar]
- 13.Wang YH, Yang CP, Ku MS, Sun HL, Lue KH. Efficacy of nasal irrigation in the treatment of acute sinusitis in children. Int J Pediatr Otorhinolaryngol. 2009;73:1696–701. doi: 10.1016/j.ijporl.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Adam P, Stiffman M, Blake RL., Jr A clinical trial of hypertonic saline nasal spray in subjects with the common cold or rhinosinusitis. Arch Fam Med. 1998;7:39–43. doi: 10.1001/archfami.7.1.39. [DOI] [PubMed] [Google Scholar]
- 15.Bollag U, Albrecht E, Wingert W. Medicated versus saline nose drops in the management of upper respiratory infection. Helv Paediatr Acta. 1984;39:341–5. [PubMed] [Google Scholar]
- 16.Slapak I, Skoupá J, Strnad P, Horník P. Efficacy of isotonic nasal wash (seawater) in the treatment and prevention of rhinitis in children. Arch Otolaryngol Head Neck Surg. 2008;134:67–74. doi: 10.1001/archoto.2007.19. [DOI] [PubMed] [Google Scholar]
- 17.King D, Mitchell B, Williams CP, Spurling GK. Saline nasal irrigation for acute upper respiratory tract infections. Cochrane Database Syst Rev. 2015:CD006821. doi: 10.1002/14651858.CD006821.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramalingam S, Graham C, Dove J, Morrice L, Sheikh A. A pilot, open labelled, randomised controlled trial of hypertonic saline nasal irrigation and gargling for the common cold. Sci Rep. 2019;9:1015. doi: 10.1038/s41598-018-37703-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramalingam S, Cai B, Wong J, Twomey M, Chen R, Fu RM, et al. Antiviral innate immune response in non-myeloid cells is augmented by chloride ions via an increase in intracellular hypochlorous acid levels. Sci Rep. 2018;8:13630. doi: 10.1038/s41598-018-31936-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hicks LA, Shepard CW, Britz PH, Erdman DD, Fischer M, Flannery BL, et al. Two outbreaks of severe respiratory disease in nursing homes associated with rhinovirus. J Am Geriatr Soc. 2006;54:284–9. doi: 10.1111/j.1532-5415.2005.00529.x. [DOI] [PubMed] [Google Scholar]
- 21.Passàli D, Damiani V, Passàli FM, Passàli GC, Bellussi L. Atomized nasal douche vs. nasal lavage in acute viral rhinitis. Arch Otolaryngol Head Neck Surg. 2005;131:788–90. doi: 10.1001/archotol.131.9.788. [DOI] [PubMed] [Google Scholar]
- 22.Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007:CD006394. doi: 10.1002/14651858.CD006394.pub2. [DOI] [PubMed] [Google Scholar]
- 23.Fehr AR, Perlman S. Coronaviruses: An overview of their replication and pathogenesis. Methods Mol Biol. 2015;1282:1–23. doi: 10.1007/978-1-4939-2438-7_1. [DOI] [PMC free article] [PubMed] [Google Scholar]


