Abstract
Immunotherapy is one of the most effective treatments for patients with advanced lung cancer. In many advanced non-small cell lung cancer (NSCLC) cases, the tumor is centrally located. For such patients, sleeve lobectomy has been considered as a more effective therapeutic option compared with pneumonectomy, achieving better long-term survival and quality of life with no increase in morbidity or mortality. Until now, there have been no studies regarding the efficacy and safety of neo-adjuvant chemo-immunotherapy prior to sleeve lobectomy for lung cancer. From January 2019 through October 2019, nine patients were diagnosed as NSCLC and evaluated to undergo sleeve lobectomy surgery (SLS). Of these patients, four received two cycles of pembrolizumab plus paclitaxel and cisplatin (PPC) followed by sleeve lobectomy, while five patients underwent SLS alone. The patients’ clinical characteristics, perioperative parameters, and postoperative outcomes were analyzed. Multiplex fluorescent immunohistochemistry was performed to determine the number of macrophages, CD4+ and CD8 T cells, and Treg cells in the bronchial mucosa. Three of the four patients achieved a complete pathological response [0% viable tumor, pathologic complete response (pCR)]. All of the patients in the PPC group achieved major pathological response (≤10% viable tumor, MPR). No grade 3 or 4 treatment-related adverse events occurred in the PPC group, nor did any of the patients in the group experience treatment-related surgical delays. The mean surgical time and the number of lymph nodes dissected were the same in the two groups. The PPC group had a higher number of CD8 + T cells compared to the SLS group (P<0.01). No postoperative chylothorax, pneumonia, or other postoperative complications occurred in either group. The surgical difficulty and post-surgical complication rate of sleeve lobectomy with neo-adjuvant chemo-immunotherapy were similar to those of SLS alone. Neo-adjuvant chemo-immunotherapy is effective and safe with sleeve lobectomy for NSCLC patients. Additional prospective multi-center randomized studies using larger patient cohorts are necessary to validate our findings.
Keywords: Neo-adjuvant chemo-immunotherapy, sleeve lobectomy, non-small cell lung cancer (NSCLC)
Introduction
Immunotherapy is one of the most effective treatment methods for patients with advanced lung cancer. Several clinical studies have focused on neoadjuvant immunotherapy prior to tumor resection for advanced non-small cell lung cancer (NSCLC). It has been reported that neoadjuvant anti-programmed death-1 (PD-1) immunotherapy does not delay surgery and achieves a major pathological response in 83% of patients who undergo tumor resection (1,2). Many cases of advanced NSCLC are centrally located. Compared with pneumonectomy, sleeve lobectomy has been considered as a more effective therapeutic option for patients with central NSCLC, with better long-term survival and quality of life without increasing the morbidity and mortality. To date, there has been no report regarding the efficacy and safety of neo-adjuvant chemo-immunotherapy prior to sleeve lobectomy for lung cancer. Herein, we evaluated the feasibility and safety of using neoadjuvant chemotherapy combined with PD-1 treatment before sleeve lobectomy to treat NSCLC patients.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/tlcr-20-539).
Methods
The study was conducted in accordance with the Declaration of Helsinki and approved by the TJMUCH Institutional Review Board, and informed consent was obtained from all participants.
Between January and August in 2019, nine patients who were diagnosed with NSCLC were evaluated to undergo sleeve lobectomy surgery (SLS). The patients were divided into two groups: four of the patients received neo-adjuvant chemo-immunotherapy followed by sleeve lobectomy [the pembrolizumab plus paclitaxel and cisplatin (PPC) group]; and five of the patients underwent SLS alone (the SLS group). The PPC group were given pembrolizumab (100 mg), paclitaxel (135 mg/m2) and cisplatin (75 mg/m2) every 3 weeks for 2 cycles before the surgery. SLS was performed on each patient by the same surgical team. A two-tailed Student’s t-test was used to determine p values between two groups. All the statistical analyses were done with GraphPad Prism 6 (GraphPad Software, La Jolla, CA, USA). A probability value of P less than 0.05 was considered statistically significant.
Results
The patients in the PPC group experienced no grade 3 or 4 treatment-related adverse events. No immune-related adverse events were reported to be associated with the administration of pembrolizumab. In addition, no treatment-related surgical delays were encountered in the PPC group. The median interval between the administration of the second dose of pembrolizumab and SLS was 30.33 days (range, 27 to 33 days). The median follow-up was 6 months (range, 3 to 9 months). None of the patients died or suffered disease recurrence in either group during follow-up (Table 1).
Table 1. Demographic and clinical characteristics of the patients.
| No. | Age/sex | Smoking | Diagnosis | Pathological stage | PFT (FVC%/FEV1%) | Risk factors | Neoadjuvant chemotherapy combined with pembrolizumab |
|---|---|---|---|---|---|---|---|
| 1 | 63/M | + | SqCC | T3N0M0, stage IIB | 72/83 | Hypertension | + |
| 2 | 56/F | − | SqCC | T4N0M0, stage IIIA | 74/86 | – | + |
| 3 | 74/M | + | SqCC | T3N0M0, stage IIB | 62/77 | Hypertension | + |
| 4 | 57/M | + | SqCC | T3N0M0, stage IIB | 83/88 | – | + |
| 5 | 70/M | + | SqCC | T2aN2M0, stage IIIA | 84/80 | – | – |
| 6 | 52/M | + | SqCC | T3N0M0, stage IIB | 82/96 | – | – |
| 7 | 66/F | + | SqCC | T2aN2M0, stage IIIA | 77/90 | Diabetes | – |
| 8 | 68/F | – | SqCC | T3N0M0, stage IIB | 89/106 | Hypertension | – |
| 9 | 70/M | + | SqCC | T2aN2M0, stage IIIA | 87/91 | – | – |
The mean duration of surgery was 108.8 and 110 min for the PPC group and the SLS group, respectively. No significant difference was observed in surgical duration between the two groups (P>0.05). The number of lymph nodes dissected was 38.5 and 35.6 for the PPC group and the SLS group, respectively, and no significant difference was found. The mean length of stay in the intensive care unit (ICU) was 1.5 and 2.2 days for the PPC group and the SLS group, respectively, while the total length of stay in the hospital was 4.3 and 4.6 days for the PPC group and the SLS group, respectively. No significant differences were found between the two groups (P>0.05). None of the patients in either of the two patient groups suffered postoperative chylothorax, pneumonia, or other postoperative complications (Table 2).
Table 2. Perioperative parameters and postoperative outcomes.
| Case No. | Procedure | LND No. | Operation time (min) | Bleeding (mL) | Hospital stay (days) | Chest tube stay (days) | Morbidity | Recurrence |
|---|---|---|---|---|---|---|---|---|
| 1 | LLLSL | 43 | 110 | Minimal | 4 | 2 | – | – |
| 2 | RULSL | 38 | 105 | 100 | 4 | 3 | – | – |
| 3 | LLLSL | 33 | 90 | 100 | 5 | 3 | – | – |
| 4 | RULSL | 40 | 130 | 200 | 4 | 2 | – | – |
| 5 | LULSL | 40 | 120 | 200 | 4 | 3 | – | – |
| 6 | RML/RLLSBL | 35 | 110 | Minimal | 5 | 2 | – | – |
| 7 | RULSL | 44 | 130 | 100 | 5 | 3 | – | – |
| 8 | LULSL + PA | 28 | 100 | 100 | 5 | 4 | – | – |
| 9 | RML/RLLSBL | 31 | 90 | 200 | 4 | 3 | – | – |
LND No., number of dissected lymph nodes; LULSL, left upper lobe sleeve lobectomy; PA, pulmonary arterioplasty; RML/RLLSBL, right middle and lower lobe sleeve bilobectomy; RULSL, right upper lobe sleeve lobectomy; LLLSL, left lower lobe sleeve lobectomy.
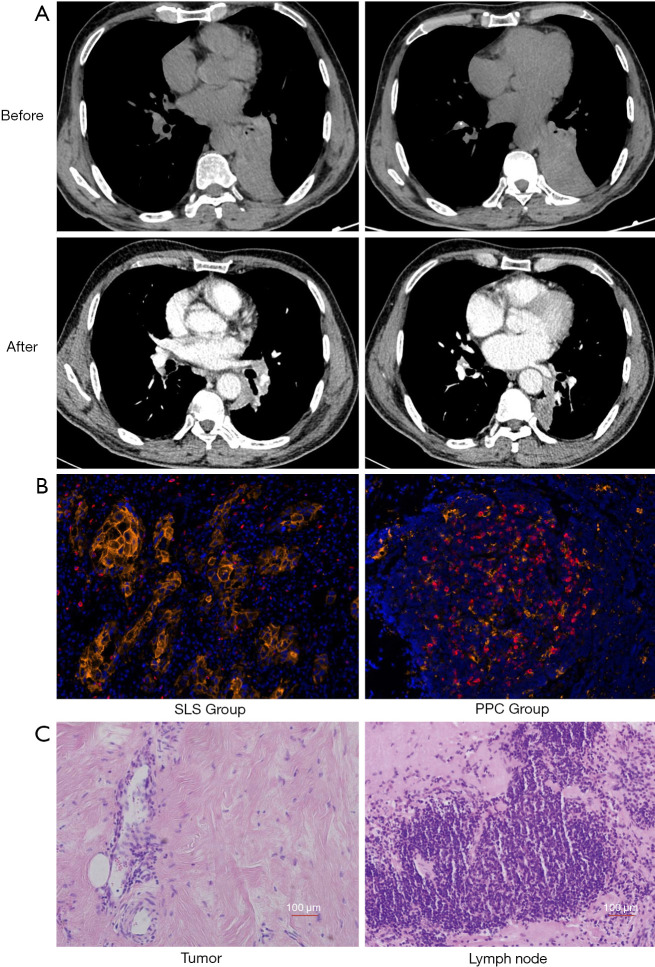
Three of the four patients in the PPC group achieved a complete pathological response [0% viable tumor, pathologic complete response (pCR)]. All patients in the PPC group achieved a major pathological response (≤10% viable tumor, MPR, including pCR). The pCR and MPR rates were 75% and 100% in the PPC group, respectively. Representative images of the lesion before and after two cycles of neoadjuvant chemotherapy combined with pembrolizumab are shown in Figure 1A. Computed tomography images revealed that the lesion was significantly reduced after two cycles of treatment. Expression levels of programmed death-ligand 1 (PD-L1) and PD-1 were evaluated in pretreatment biopsy samples obtained from all patients in the PPC group (Figure 1B). PD-L1 expression was approximately 42.1%, 6.3%, and 25.8% in patients who achieved pCR, and about 7.8% in the patients who achieved only MPR in the PPC group (Figure 1B).
Figure 1.
Images of lesions before and after two cycles of neoadjuvant chemotherapy in combination with pembrolizumab (Case 1). (A) Computed tomography images before and after two cycles of treatment. The lesion was significantly reduced after two cycles of treatment. (B) Programmed death-1 (PD-1) and programmed death-ligand 1 (PD-L1) expression levels in the tumors. Photomicrographs of representative multiplex fluorescent immunohistochemistry for PD-1 and PD-L1 expression levels (Cases 2 and 8). PD-1 and PD-L1 expression levels in formalin-fixed, paraffin-embedded (FFPE) samples from a representative patient sample. Tumors stained with anti-PD-L1 antibody [PD-L1 (CD274) Monoclonal Antibody (RM320), Invitrogen], and anti-PD-1 (Anti-PD1 antibody, Abcam). The mean percentages of PD-1 and PD-L1 expression in the pembrolizumab plus paclitaxel and cisplatin (PPC) group was 7.2% and 27.8% respectively. The mean percentages of PD-1 and PDL1 expression in the sleeve lobectomy surgery (SLS) group was 1.71% and 4.88%, respectively. PD-L1 expression is indicated in yellow and PD-1 in red. Scale bar, 100 µm. (C) HE staining of the tumor and lymph node (Case 2) from the PPC group. A large number of infiltrating lymphocytes and macrophages were present. No residual tumor tissue was observed in patients after two cycles of treatment. The patients achieved a pathologic complete response (pCR). The presence of fibrosis, patchy necrosis, and macrophages was observed in the lymph node after two cycles of treatment.
We observed large numbers of infiltrating lymphocytes and macrophages in primary tumors that had a complete or major pathological response, which was consistent with immunological response. Tumor necrosis was associated with fibrotic tissue repair (Figure 1C).
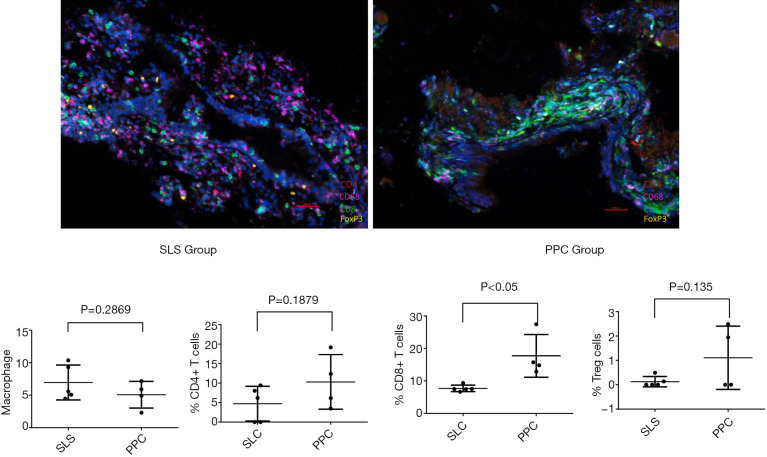
As the immune system may influence bronchial mucosa wounding healing, multiplex fluorescent immunohistochemistry was performed to determine the number of macrophages, CD4+ and CD8 T cells, and Treg cells in the bronchial mucosa. The mean percentages of macrophages (6.96% vs. 5.08%), CD4 T cells (4.72% vs. 10.29%) and CD8+ T cells (7.71% vs. 17.72%), and Treg cells (0.13% vs. 1.1%) were calculated in the SLC and PPC groups, respectively. The number of CD8+ T cells were higher in the PPC group than in the SLS group (P<0.05). There were no significant differences in the number of CD4 T cells, macrophages, or Treg cells between the two groups (P>0.05) (Figure 2).
Figure 2.
Presence of Macrophages, CD4 and CD8 positive T cells, and Treg cells in the bronchial stump detected by multiplex fluorescent immunohistochemistry (Cases 2 and 5). The mean percentages of macrophages, CD4 and CD8 positive T cells, and Treg cells in the sleeve lobectomy surgery (SLS) group and pembrolizumab plus paclitaxel and cisplatin (PPC) group were 6.96% vs. 5.08%, 4.72% vs. 10.29%, 7.71% vs. 17.72%, and 0.13% vs. 1.1%, respectively. Scale bar, 100 µm.
Discussion
Lung cancer is the leading cause of cancer-related mortality worldwide. The development of cancer immunotherapy has been focused on various ligands and receptors that inhibit or stimulate the immune system, with immune checkpoint inhibitors, including agents that target the anti-PD-1 or PD-L1 molecules, receiving the most attention to date (3-5). Several clinical studies have focused on neoadjuvant immunotherapy prior to tumor resection in advanced lung cancer. It has been reported that neoadjuvant anti-PD-1 immunotherapy does not delay surgery and achieves a major pathological response in 83% of resected tumors. The NADIM study (a neo-adjuvant immunotherapy clinical study, NCT number 03081689) that was published by the American Society of Clinical Oncology in 2019, reported an MPR rate of 85.36% (2). The high MPR and pCR rates were unprecedented and presented a promising future treatment strategy, although it was unknown as to whether MPR and pCR rates could eventually prolong OS and PFS. Neo-adjuvant chemo-immunotherapy was a very effective treatment that had not been previously observed. The NADIM study reported that 13% of the patients encountered G3–5 TRAEs, and the most common postsurgical complication was respiratory infections. In our study, none of the patients encountered G3–5 TRAEs, and none of the patients experienced postsurgical complications, including respiratory infections. Because of financial costs, a 100 mg IV dose of pembrolizumab was administered over 30 minutes every 3 weeks; this was lower than the recommended dose. Our results demonstrated that this lower dose was also very effective and reduced post-surgical complications.
Sleeve lobectomy has been considered a more suitable therapeutic option for central NSCLC compared with pneumonectomy, with better long-term survival and quality of life and no increase in morbidity or mortality (6,7). To our knowledge, there has been no report regarding the efficacy and safety of neo-adjuvant chemo-immunotherapy prior to sleeve lobectomy for patients with lung cancer. Based on our experience, neo-adjuvant chemo-immunotherapy can induce tissue adhesion, which increases the difficulty of the surgery. However, it can also shrink the tumor, consequently making the surgery easier to perform. We observed that the mean surgical duration was similar between the PPC and SLS groups. We believe that sufficiently separating the tissue along the pulmonary artery, vein, and trachea is extremely important in reducing surgical difficulty and the risk of bleeding. Most anastomotic complications result from disruption of the blood supply, and it is therefore fundamental for the surgeon to have an optimal knowledge of the bronchial blood supply. Another cause of potential complications is anastomotic tension. To avoid this, the distal lobe must adequately mobilized. Interrupted or continuous suture makes no significant difference to the outcome.
PD-1 regulates T-cell activation by binding to its ligands, PD-L1 and programmed death-ligand 2 (PD-L2). PD-1 binding inhibits T-cell proliferation, and interferon-γ (IFN-γ), tumor necrosis factor-α, and IL-2 production, and reduces T-cell survival (8). If a T cell experiences coincident TCR and PD-1 binding, PD-generated signals prevent phosphorylation of key TCR signaling intermediates, terminating early TCR signaling and reducing T-cell activation (9,10). PD-1 expression is a hallmark of “exhausted” T cells that have experienced high levels of stimulation or reduced CD4+ T-cell help (11). Goldberg MV found that PD-1 blockade enhanced the early stages of T-cell activation in lymph nodes (12). Liu reported that neoadjuvant PD-1 blockade could enhance the systemic priming of antitumor T cells, thereby potentially eliminating micrometastatic cancer that might otherwise cause postsurgical relapse (13). Salmon H also found the importance of dendritic cells to the antitumor effects of PD-1 pathway blockade, which suggested that PD-1 blockade not only worked to directly unleash intratumoral T-cell killing but also enhanced tumor antigen–driven priming of T cells (14). In our study, the number of CD8 + T cells of the bronchial stump were higher in the PPC group than in the SLS group (P<0.01), while the levels of macrophages, CD4+ T cells, and Treg cells were similar in both groups. The PD-1 blockade could increase the CD8 + T in the bronchial stump; therefore, it may have no influence on bronchial healing.
The surgical difficulty and post-surgery complication rate of sleeve lobectomies after neo-adjuvant chemo-immunotherapy were similar to those of SLS alone. The use of neo-adjuvant chemo-immunotherapy prior to sleeve lobectomy is effective and safe for NSCLC patients. Additional prospective, multicenter, randomized studies using larger patient cohorts are needed to validate our findings.
Supplementary
The article’s supplementary files as
Acknowledgments
We thank Professor Bingsheng Sun from Tianjin Medical University for providing suggestions for data extraction and analysis in the experiments.
Funding: Tianjin Cancer Hospital Clinical Trial Project (grant number C1705).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki and approved by the TJMUCH Institutional Review Board, and informed consent was obtained from all participants.
Footnotes
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/tlcr-20-539
Data Sharing Statement: Available at http://dx.doi.org/10.21037/tlcr-20-539
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tlcr-20-539). The authors have no conflicts of interest to declare.
References
- 1.Forde PM, Chaft JE, Smith KN, et al. Neoadjuvant PD-1 blockade in resectable lung cancer. N Engl J Med 2018;379:e14. 10.1056/NEJMc1808251 [DOI] [PubMed] [Google Scholar]
- 2.Jove M, Vilariño N, Nadal E. Impact of baseline steroids on efficacy of programmed cell death-1 (PD-1) and programmed death-ligand 1 (PD-L1) blockade in patients with advanced non-small cell lung cancer. Transl Lung Cancer Res 2019;8:S364-8. 10.21037/tlcr.2019.06.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brahmer JR, Pardoll DM. Immune checkpoint inhibitors: making immunotherapy a reality for the treatment of lung cancer. Cancer Immunol Res 2013;1:85-91. 10.1158/2326-6066.CIR-13-0078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.D'Incecco A, Andreozzi M, Ludovini V, et al. PD-1 and PD-L1 expression in molecularly selected non-small-cell lung cancer patients. Br J Cancer 2015;112:95-102. 10.1038/bjc.2014.555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer 2012;12:252-64. 10.1038/nrc3239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma Z, Dong A, Fan J, et al. Does sleeve lobectomy concomitant with or without pulmonary artery reconstruction (double sleeve) have favorable results for non-small cell lung cancer compared with pneumonectomy? A meta-analysis. Eur J Cardiothorac Surg 2007;32:20-8. 10.1016/j.ejcts.2007.03.018 [DOI] [PubMed] [Google Scholar]
- 7.Ferguson MK, Lehman AG. Sleeve lobectomy or pneumonectomy: optimal management strategy using decision analysis techniques. Ann Thorac Surg 2003;76:1782-8. 10.1016/S0003-4975(03)01243-8 [DOI] [PubMed] [Google Scholar]
- 8.Keir ME, Butte MJ, Freeman GJ, et al. PD-1 and its ligands in tolerance and immunity. Annu Rev Immunol 2008;26:677-704 10.1146/annurev.immunol.26.021607.090331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parry RV, Chemnitz JM, Frauwirth KA, et al. CTLA-4 and PD-1 receptors inhibit T-cell activation by distinct mechanisms. Mol Cell Biol. 2005;25:9543-53. 10.1128/MCB.25.21.9543-9553.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bennett F, Luxenberg D, Ling V, et al. Program death-1 engagement upon TCR activation has distinct effects on costimulation and cytokine-driven proliferation: attenuation of ICOS, IL-4, and IL-21, but not CD28, IL-7, and IL-15 responses. J Immunol. 2003;170:711-8. 10.4049/jimmunol.170.2.711 [DOI] [PubMed] [Google Scholar]
- 11.Wherry EJ. T cell exhaustion. Nat Immunol. 2011;12:492-9. 10.1038/ni.2035 [DOI] [PubMed] [Google Scholar]
- 12.Goldberg MV, Maris CH, Hipkiss EL, et al. Role of PD-1 and its ligand, B7-H1, in early fate decisions of CD8 T cells. Blood 2007;110:186-92. 10.1182/blood-2006-12-062422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu J, Blake SJ, Yong MC, et al. Improved efficacy of neoadjuvant compared to adjuvant immunotherapy to eradicate metastatic disease. Cancer Discov 2016;6:1382-99. 10.1158/2159-8290.CD-16-0577 [DOI] [PubMed] [Google Scholar]
- 14.Salmon H, Idoyaga J, Rahman A, et al. Expansion and activation of CD103(+) dendritic cell progenitors at the tumor site enhances tumor responses to therapeutic PD-L1 and BRAF inhibition. Immunity 2016;44:924-38. 10.1016/j.immuni.2016.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as