Abstract
The global pandemic of severe acute respiratory coronavirus 2 (SARS-CoV-2), which causes the novel beta coronavirus 2019 disease (COVID-19), has become an unprecedented medical, economic, and psychosocial crisis. The pandemic and its management strategies have resulted in immense challenges for health systems, not only in caring for those with COVID-19 but also in the ongoing management of chronic medical conditions. Kidney transplant recipients present a unique challenge given their need for ongoing monitoring and management as well as their higher risk of COVID-19 infection. In the absence of clear guidelines, it is unclear how to best provide routine care to this unique patient population during the pandemic. Rigorous medical and psychosocial patient-centered risk stratification strategies are needed to avoid adverse outcomes in stable solid organ transplant recipients. This review will focus on the challenges faced by kidney transplant recipients and health care providers and provides strategies to address these issues.
Keywords: COVID-19 pandemic, Kidney transplant recipients, Socio-economic effects, Strategies to take care
Abbreviations: CDC, Center for Disease Control; CKD-T, Chronic kidney disease after transplantation; CMS, Centers for Medicare and Medicaid Services; CMV, cytomegalovirus; COVID-19, beta coronavirus 2019; DART, Cell-Free DNA and Active Rejection in Kidney Allograft; DASS-21, depression, anxiety, and stress scale-21; ICU, intensive care unit; KTR, kidney transplant recipients; RRT, renal replacement therapy; SARS-CoV-2, severe acute respiratory coronavirus 2; WHO, World health organization
1. Introduction
Severe acute respiratory coronavirus 2 (SARS-CoV-2), which causes the novel beta coronavirus 2019 disease (COVID-19), has emerged as a life-threatening infection affecting more than 5.7 million people worldwide and caused the death of more than 350,000 patients as of May 2020 [1]. Categorized as a global pandemic by the Center for World Health Organization (WHO), COVID-19 has created global health care and economic crisis [2]. The immediate objective of healthcare systems is to facilitate the management of critically ill patients with severe respiratory symptoms requiring hospitalization due to COVID-19. Given the lack of effective treatment strategies and herd immunity, the main focus of public health efforts have been social distancing to “flatten the curve” of COVID-19 case growth rates thereby offsetting the significant influx of patients into the healthcare environment [3,4]. However, social distancing, along with additional psychosocial factors, including fear of healthcare systems and economic strain resulting in potential hardships including loss of employment or health insurance in the private payor model, can impact the behavior of the patients with chronic medical conditions, including those with history of transplant [5]. In general, solid organ transplant recipients require extensive monitoring of patient and graft well-being and close follow up by a multidisciplinary team that includes members from the transplant center including nephrology, surgery, nursing, social work, and pharmacy as well as the patient's local primary care provider [6]. How these issues associated with social distancing and COVID-19 will influence long-term outcomes in the transplant recipients is unknown. [6].
2. COVID-19 infection in kidney transplant recipients (KTR)
COVID-19 appears to more negatively affect patients with chronic co-morbid conditions. Studies exist demonstrating patients with cardiovascular disease, diabetes, and the elderly have more severe clinical manifestations and have an increased risk of negative outcomes [7]. Many of these are co-occurring conditions found in KTRs [8]. Recent case series describing KTRs with COVID-19 have demonstrated an incidence of intensive care unit admission from 27% to 100%, acute kidney injury from 16% to 50%, and mortality rates ranging from 6% to 50% [[9], [10], [11], [12], [13], [14]].. When reviewing reports of COVID-19 infection published in journals with impact factor > 2.5 between January 1st and April 24th 2020 it appears KTRs have more negative outcomes overall. Indeed, patient-level incidence of AKI (KTR 27.5% vs. non-KTR 13.3%, p < .001), renal replacement therapy (KTR 15.4% vs. non-KTR 3.3%, p < .001), requirement for ICU care (KTR 34.1% vs. non-KTR 15.1%, p < .001), and death (KTR 22.7% vs non-KTR 16.2%, p = .10) representing relative risks of 2.06 (1.44, 2.96), 4.72 (2.62, 8.51), 2.25 (1.67, 3.03), and 1.41 (0.95, 2.08), favored non-KTRs in all categories [9,10,12,13,[15], [16], [17], [18], [19], [20], [21], [22], [23]].
While it seems clear that KTR with suppressed immune systems and baseline chronic kidney disease after transplantation (CKD-T), appear to be at a higher risk of COVID-19 related morbidity and mortality, the collateral damage of the massive changes to the provision of chronic medical care due to the pandemic in this population is less apparent [14,15]. Therefore, the purpose of this manuscript is to review and describe potential ramifications of the pandemic on the routine care of the renal transplant recipient and present strategies to address these challenges in an attempt to prevent adverse outcomes.
3. Challenges in the provision of care of KTRs in COVID-19 pandemic (Table 1)
Table 1.
Summary of Strategies to Mitigate COVID-19 related challenges.
| Challenges in taking care of KTs in pandemic | Strategies to mitigate the challenges |
|---|---|
| Disruption in the routine care of KTRs |
|
| |
| |
| |
| Issues with access and adherence with immunosuppressants |
|
| |
| |
| Psychological stress to the patients |
|
| |
| |
| Economic hardships for the transplant centers. |
|
|
As outlined above, the COVID-19 pandemic has created several challenges in the care of the KTR. These challenges occur at three levels, including; region/national issues which encompass stay at home orders and the economy, local issues that are specific to the transplant center, and finally, patient-specific issues.
3.1. Regional/national challenges
3.1.1. Stay-at-home orders and the resultant increase in telehealth
As aforementioned, the primary public health measure to contain COVID-19 has been government-mandated social distancing practices. These orders are endorsed by national health bodies, including the Center for Disease Control (CDC) and WHO, and practically interpreted at the discretion of state governments [24]. In the healthcare setting, these orders have resulted in the cancelation of non-emergent, elective procedures to limit face-to-face contact with patients [25,26]. To maintain contact with patients, centers have turned to the use of telehealth.
Telehealth is a complex enterprise and raises multiple challenges at different levels. Multiple studies showed that telehealth implementation involves a set of professional, legal, technological, and strategic factors [[27], [28], [29]]. Telemedicine also offers significant potential for improving access, continuity of care, and quality for the benefit of society [30,31].
The CDC recommends increased utilization of telehealth services to maintain provider/patient contact while still following social distancing measures [32]. While telemedicine can help fill the void created by COVID-19, several factors limit its effectiveness, including barriers to using the technology (lack of internet, lack of device, etc.), hesitancy from patients to share less severe problems with providers and difficulty in understanding changes in medications over the telephone. Furthermore, physical examination by providers cannot effectively take place via a virtual visit, and significant findings like an assessment of volume status may be missed. Although this approach helps to maintain social distancing, it can expose KTRs to potential unintended consequences.
3.2. Local challenges
3.2.1. Economic hardship
Due to ongoing economic pressures, healthcare systems have been required to adopt cost-reduction strategies, which include reducing work hours and income of the transplant providers, coordinators, nurses, and pharmacists. Furthermore, in areas more significantly impacted by COVID-19, redeployment of transplant providers to the front-line for COVID-19 related care also functionally reduces transplant-related work hours. The effect of these on the care of KTRs is unknown but may affect both short-term and long-term patient and allograft outcomes.
The pandemic exposes the weaknesses of the current private payor health system in the United States, where help from the federal government has been required to keep the system functional [33].
3.3. Patient-related challenges
3.3.1. Access and adherence: immunosuppression
Non-adherence to immunosuppressant medications by KTRs is associated with increased risk of allograft rejection, which in turn is associated with increased morbidity and mortality [34,35]. Despite the adverse outcomes associated with non-adherence, rates of non-adherence to medication in KTRs has been reported to be 20 to 70% [36]. The government-issued shelter at home orders, increasing unemployment, and loss of health insurance during the COVID-19 pandemic can threaten adherence, again highlighting the limitations of a private payor based healthcare system over a public system, as is found in Europe. This non-adherence can then be amplified by difficulties in procuring medications due to issues with transportation, accessibility, and affordability. Indeed, in our center-specific experience, we have had a number of KTRs present with acute allograft rejection due to non-adherence with laboratory monitoring and medications due to their interpretation of shelter at home orders, and fear of healthcare exposure [54].
3.3.2. Psychological stress
Several studies have shown that KTRs are at increased risk of emotional distress and affective disorders such as anxiety and depression [[37], [38], [39]]. The enormity of social distancing, economic crisis, and grief over the death of loved ones related to COVID-19 has the potential to affect mental health significantly. Wang et al. conducted an online survey using snowball sampling techniques in immunocompetent people. The survey collected information on demographic data, physical symptoms, COVID-19 exposure, and symptoms. They also looked into the psychological impact of COVID-19 by using depression, anxiety, and stress scale (DASS-21). The study found that 53.8% of respondents rated the psychological impact of the pandemic as moderate or severe, 16.5% reported moderate to severe depressive symptoms, 28.8% reported moderate to severe anxiety symptoms, and 8.1% reported moderate to severe stress levels. Female gender, student status, specific physical symptoms, and poor self-related health status were significantly associated with the psychological impact of the pandemic (p < .05) [40]. Based on previous experiences from prior outbreaks, patients with chronic health conditions are most susceptible to the stress of this crisis [41]. Beyond COVID-19 related exacerbation of anxiety and depression, the lack of access to primary care physicians, social workers, and transplant providers can potentiate anxiety and depression in the KTRs. There is also concern that the current crisis can trigger unhealthy behaviors, including excessive smoking, increased alcohol intake, poor sleep, reduced activity, and dysregulated eating in patients with pre-existing psychiatric or other medical conditions [[42], [43], [44]]. This maladaptive stress response can have a significant impact on KTRs, given their reliance on medication adherence for positive outcomes, as well as common co-morbid conditions that would be exacerbated by these behaviors.
4. Strategies to enhance the care of KTRs during COVID-19 pandemic (Table 1)
4.1. Regional/national opportunities
4.1.1. Optimization of telehealth
To minimize viral exposure for patients and transplant providers, many transplant centers have adopted virtual modalities for routine visits. A virtual visit, despite its shortcomings, is preferable to delaying or skipping a routine visit. Increased frequency of virtual visits may be needed for those patients considered to be at the highest risk, including patients with multiple medical conditions, underlying anxiety, and depression. Devices and platforms that facilitate visual communication, including video chat, allow for interpretation of visual conversational cues, as well as some physical examination.
With the recent changes in reimbursement policies by the Centers for Medicare and Medicaid Services (CMS) to expand virtual visits, most of the virtual visits will be reimbursed [45]. Reimbursement for Medicaid varies by state, though many states have expanded telehealth coverage in response to this crisis.
4.2. Local opportunities
4.2.1. Remote monitoring improvement strategies
To improve the monitoring of KTRs during the COVID-19 era, we suggest several potential strategies.
4.2.1.1. Patient self-monitoring
Frequent checking of vitals and reporting to the transplant team when abnormal is encouraged. Patients should be educated about the symptoms of COVID-19 infection. With any concerning symptoms, patients should inform their primary care physicians and/or the transplant centers and should be instructed if COVID-19 testing is warranted. It is important to note that even if a patient has not had an exposure or is at low risk for COVID-19 due to social distancing, a fever in a KTR still requires clinical workup. The infectious complications that plague kidney transplantation continues during this era, including urinary tract infection, cytomegalovirus infection, pneumonia, and other opportunistic infections. Patients should be similarly educated about the need for ongoing vigilance in monitoring for these and other infections.
4.2.1.2. Alternative laboratory procurement strategies
Mobile phlebotomy services to obtain routine laboratory blood work from transplant patients are an exciting avenue to explore during the pandemic. Services such as this are available for cytomegalovirus virus (CMV) molecular diagnostics, as well as routine blood work. These alternative strategies will both allow the transplant team to monitor important indicators of kidney function and avoid potential COVID-19 exposure from visiting phlebotomy laboratories.
4.2.1.3. Alternatives to renal biopsy
The Cell-Free DNA and Active Rejection in Kidney Allograft (DART) study suggests that the use of a non-invasive AlloSure test to measure donor-derived cell-free DNA can be used to diagnose rejection in the kidney allograft [46]. The AlloSure test has been approved by Medicare for clinical use when kidney transplant rejection is suspected. High-risk patients who might previously have undergone a protocol biopsy for routine surveillance can be closely monitored by AlloSure testing during the evolving pandemic. The negative AlloSure testing will be reassuring, and patients can potentially be observed without being called into the hospital for the kidney allograft biopsy. Those protocol biopsies can be delayed based on the AlloSure testing in patients with stable renal allograft function. However, the patients with abnormal kidney allograft function with elevated creatinine, increasing urine protein creatinine ratio, or denovo or rising donor-specific antibodies, will still need transplant kidney biopsy as standard of their care.
4.3. Patient-related opportunities
4.3.1. Strategies to enhance medication access and adherence
While the COVID-19 pandemic presents challenges to medication adherence, we offer several strategies to address these issues below
-
1.
Pharmacy avoidance: Utilization of mail order over brick and mortar pharmacies should be encouraged. The education of patients regarding delays related to shipments should occur to avoid disruption of therapy.
-
2.
Stockpiling: The CDC has encouraged patients to obtain an extended supply of medications during the COVID-19 pandemic to avoid the need for frequent refilling [47,48].
-
3.
Cost Mitigation Strategies: Manufacturer sponsored patient assistance programs (PAP) should be explored for patients that qualify based on income. Those who are under-insured or have high deductibles may be eligible for manufacturer-sponsored co-pay assistance plans. Both PAP and co-pay assistance are typically only available in the setting of branded drug products. Pharmacy specific generic-drug programs, as well as the Good Rx drug credit program, can be explored in the setting of generically available drugs or those patients that do not qualify for PAP/co-pay assistance (i.e., patients with State and Government-funded insurance programs). Co-payment waivers during COVID-19 is another option that has been suggested [49,50]. Most importantly, the 3-year Medicare coverage issue needs to be addressed to improve access to ongoing coverage of immunosuppressive medications and avoid returns to dialysis.
4.4. Strategies for dealing with stress, anxiety, and depression
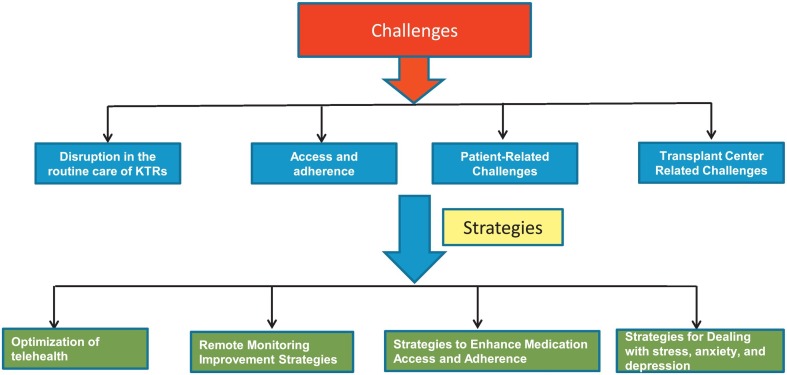
As mentioned earlier, KTRs are at increased risk of depression, anxiety, and stress, especially during the time of the COVID-19 pandemic. Specific strategies should be adopted to deal with this. KTRs should be encouraged to stay in touch with their family and friends through phone or video technologies. With more severe symptoms of anxiety and depression, they should contact their health care providers. Several studies have shown that mediation programs can reduce multiple negative dimensions of psychological stress [51]. The continuation of physical activity during this crisis is essential. Regular exercise is an effective reducer of stress and anxiety [52,53]. Although many government policies enforce quarantines/lockdown, if physical distancing is upheld, outdoor exercise is allowed. Even when outdoor activities are not possible, regular indoor exercise should be done. Many virtual exercise classes are now available for high-risk individuals and should be encouraged. Various challenges and strategies are summarized in Fig. 1 .
Fig. 1.
Challenges and strategies.
5. Conclusion
The COVID-19 pandemic will have a long-lasting effect on our health system. To avoid long-lasting effects on our patients, strategies to prevent adverse outcomes are needed. These strategies must address both risks associated with COVID-19 as well as risks associated with a lack of proper maintenance care of the allograft. In the absence of clear guidelines for the type or frequency of monitoring during the pandemic, we suggest that rigorous medical and psychosocial patient-centered, risk stratification strategies avoid adverse outcomes in stable solid organ transplant recipients. Increased utilization of technology, newly developed immune-monitoring assays, and patient and provider vigilance will all contribute to this goal. This era of COVID-19 necessitates the multidisciplinary collaboration and inventive spirit that is central to the field of solid organ transplants.
Disclosure
The authors have no financial disclosures.
Sources of funding
No grant funding directly supports this manuscript.
Declaration of Competing Interest
All authors declare no conflict of interest.
References
- 1.John Hopkins Coronavirus resource center. 2020. https://coronavirus.jhu.edu/map.html Available from.
- 2.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gavin K. Flattening the curve for COVID-19: what does it mean and how can you help? 2020. https://healthblog.uofmhealth.org/wellness-prevention/flattening-curve-for-covid-19-what-does-it-mean-and-how-can-you-help [updated 03/11/2020]. Available from.
- 4.Coronavirus Disease 2019 COVID-19 Prevent getting sick. 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html [updated 04/24/2020]. Available from.
- 5.Coronavirus Disease 2019 (COVID-19) daily life & coping. 2020. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html [updated 04/30/2020]. Available from.
- 6.National kidney Foundation The health care team national kidney foundation. 2020. https://www.kidney.org/atoz/content/healthcareteam Available from.
- 7.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4683. PMID: 32203977. [DOI] [PubMed] [Google Scholar]
- 8.Neale J., Smith A.C. Cardiovascular risk factors following renal transplant. World J Transplant. 2015;5:183–195. doi: 10.5500/wjt.v5.i4.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akalin E.A.Y., Bartash R., Seethamraju H., Parides M., Hemmige V., Ross M., et al. Covid-19 and kidney transplantation. NEJM. 2020;382(25):2475–2477. doi: 10.1056/NEJMc2011117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Banerjee D.P.J., Shah S., Ster I.C., Quan V., Phanish M. COVID-19 infection in kidney transplant recipients. Kidney Int. 2020;97(6):1076–1082. doi: 10.1016/j.kint.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alberici F.D.E., Manenti C., Econimo K., Valerio F., Pola A., Maffei C., et al. A single center observational study of the clinical characteristics and short-term outcome of 20 kidney transplant patients admitted for SARS-CoV2 pneumonia. Kidney Int. 2020;97(6):1083–1088. doi: 10.1016/j.kint.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fernandez-Ruiz M., Andres A., Loinaz C., Delgado J.F., Lopez-Medrano F., San Juan R., et al. COVID-19 in solid organ transplant recipients: a single-center case series from Spain. Am J Transplant. 2020;20(7):1849–1858. doi: 10.1111/ajt.15929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gandolfini I., Delsante M., Fiaccadori E., Zaza G., Manenti L., Degli Antoni A., et al. COVID-19 in kidney transplant recipients. Am J Transplant. 2020;20(7):1941–1943. doi: 10.1111/ajt.15891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Montagud-Marrahi E., Cofan F., Torregrosa J.V., Cucchiari D., Ventura-Aguiar P., Revuelta I., et al. Preliminary data on outcomes of SARS-CoV-2 infection in a Spanish single Centre cohort of kidney recipients. Am J Transplant. 2020 doi: 10.1111/ajt.15970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alberici F., Delbarba E., Manenti C., Econimo L., Valerio F., Pola A., et al. A single center observational study of the clinical characteristics and short-term outcome of 20 kidney transplant patients admitted for SARS-CoV2 pneumonia. Kidney Int. 2020;97(6):1083–1088. doi: 10.1016/j.kint.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen T., Wu D., Chen H., Yan W., Yang D., Chen G., et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368 doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grein J., Ohmagari N., Shin D., Diaz G., Asperges E., Castagna A., et al. Compassionate use of Remdesivir for patients with severe Covid-19. N Engl J Med. 2020;382(24):2327–2336. doi: 10.1056/NEJMoa2007016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cao B., Wang Y., Wen D., Liu W., Wang J., Fan G., et al. A trial of Lopinavir-ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382(19):1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Su H.Y.M., Wan C., Yi L.X., Tang F., Zhu H.Y., Yi F., et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;98(1):219–227. doi: 10.1016/j.kint.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Center for Disease Control Coronavirus Disease 2019 (COVID-19) prevent getting sick. 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html Available from.
- 25.Center for Disease Control Coronavirus disease 2019 (COVID-19) healthcare facilities: preparing for community transmission. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html Available from.
- 26.Center for Disease Control Coronavirus Disease 2019 (COVID-19). Steps healthcare facilities can take now to prepare for COVID-19. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/steps-to-prepare.html Available from.
- 27.Greenhalgh T., Wherton J., Papoutsi C., Lynch J., Hughes G., A’Court C., et al. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res. 2017;19:e367. doi: 10.2196/jmir.8775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Greenhalgh T., Russell J., Ashcroft R.E., Parsons W. Why national eHealth programs need dead philosophers: Wittgensteinian reflections on policymakers’ reluctance to learn from history. Milbank Q. 2011;89:533–563. doi: 10.1111/j.1468-0009.2011.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alami H., Gagnon M.P., Wootton R., Fortin J.P., Zanaboni P. Exploring factors associated with the uneven utilization of telemedicine in Norway: a mixed methods study. BMC Med Inform Decis Mak. 2017;17 doi: 10.1186/s12911-017-0576-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alami H., Gagnon M.P., Fortin J.P. Some multidimensional unintended consequences of Telehealth utilization: a multi-project evaluation synthesis. Int J Health Policy Manag. 2019;8:337–352. doi: 10.15171/ijhpm.2019.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krupinski E.A., Patterson T., Norman C.D., Roth Y., ElNasser Z., Abdeen Z., et al. Successful models for telehealth. Otolaryngol Clin North Am. 2011;44:1275–1288. doi: 10.1016/j.otc.2011.08.004. [vii-viii] [DOI] [PubMed] [Google Scholar]
- 32.Telehealth Health care from the safety of our homes. 2020. https://telehealth.hhs.gov/ Available from.
- 33.King J.S. Covid-19 and the need for health care reform. N Engl J Med. 2020;382:e104. doi: 10.1056/NEJMp2000821. [DOI] [PubMed] [Google Scholar]
- 34.Prihodova L., Nagyova I., Rosenberger J., Majernikova M., Roland R., Groothoff J.W., et al. Adherence in patients in the first year after kidney transplantation and its impact on graft loss and mortality: a cross-sectional and prospective study. J Adv Nurs. 2014;70:2871–2883. doi: 10.1111/jan.12447. [DOI] [PubMed] [Google Scholar]
- 35.Butler J.A., Roderick P., Mullee M., Mason J.C., Peveler R.C. Frequency and impact of nonadherence to immunosuppressants after renal transplantation: a systematic review. Transplantation. 2004;77:769–776. doi: 10.1097/01.tp.0000110408.83054.88. [DOI] [PubMed] [Google Scholar]
- 36.Paterson T.S.E., O’Rourke N., Shapiro R.J., Loken Thornton W. Medication adherence in renal transplant recipients: a latent variable model of psychosocial and neurocognitive predictors. PLoS One. 2018;13 doi: 10.1371/journal.pone.0204219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.De Vito Dabbs A., Dew M.A., Stilley C.S., Manzetti J., Zullo T., McCurry K.R., et al. Psychosocial vulnerability, physical symptoms and physical impairment after lung and heart-lung transplantation. J Heart Lung Transplant. 2003;22:1268–1275. doi: 10.1016/s1053-2498(02)01227-5. [DOI] [PubMed] [Google Scholar]
- 38.Dew M.A., Roth L.H., Schulberg H.C., Simmons R.G., Kormos R.L., Trzepacz P.T., et al. Prevalence and predictors of depression and anxiety-related disorders during the year after heart transplantation. Gen Hosp Psychiatry. 1996;18:48S–61S. doi: 10.1016/s0163-8343(96)00077-1. [DOI] [PubMed] [Google Scholar]
- 39.Erim Y., Beckmann M., Valentin-Gamazo C., Malago M., Frilling A., Schlaak J.F., et al. Quality of life and psychiatric complications after adult living donor liver transplantation. Liver Transpl. 2006;12:1782–1790. doi: 10.1002/lt.20907. [DOI] [PubMed] [Google Scholar]
- 40.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10:1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gross G., Maruani J., Vorspan F., Benard V., Benizri C., Brochard H., et al. Association between coffee, tobacco, and alcohol daily consumption and sleep/wake cycle: an actigraphy study in euthymic patients with bipolar disorders. Chronobiol Int. 2020:1–11. doi: 10.1080/07420528.2020.1725542. [DOI] [PubMed] [Google Scholar]
- 43.Faulenbach M., Uthoff H., Schwegler K., Spinas G.A., Schmid C., Wiesli P. Effect of psychological stress on glucose control in patients with type 2 diabetes. Diabet Med. 2012;29:128–131. doi: 10.1111/j.1464-5491.2011.03431.x. [DOI] [PubMed] [Google Scholar]
- 44.Lemmens S.G., Martens E.A., Born J.M., Martens M.J., Westerterp-Plantenga M.S. Lack of effect of high-protein vs. high-carbohydrate meal intake on stress-related mood and eating behavior. Nutr J. 2011;10 doi: 10.1186/1475-2891-10-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Medicare telemedicine health care provider fact sheet. 2020. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet [cited 2020 5/10/2020]. Available from:
- 46.Bloom R.D., Bromberg J.S., Poggio E.D., Bunnapradist S., Langone A.J., Sood P., et al. Cell-free DNA and active rejection in kidney allografts. J Am Soc Nephrol. 2017;28:2221–2232. doi: 10.1681/ASN.2016091034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Healthcare Facilities Preparing for community transmission. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html Available from.
- 48.McCook A. COVID-19: stockpiling refills may strain the system. 2020. https://www.idse.net/Policy--Public-Health/Article/03-20/COVID-19-Stockpiling-Refills-May-Strain-the-System/57583 updated 03/11/2020. Available from.
- 49.To waive COVID-19 copays Medicaid must waive all co-pays: CMS. 2020. https://www.modernhealthcare.com/medicaid/waive-covid-19-copays-medicaid-must-waive-all-co-pays-cms Available from.
- 50.Health insurance providers respond to coronavirus (COVID-19) 2020. https://www.ahip.org/health-insurance-providers-respond-to-coronavirus-covid-19/ Available from.
- 51.Goyal M., Singh S., Sibinga E.M., Gould N.F., Rowland-Seymour A., Sharma R., et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174:357–368. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Romano G., Simonella R., Falleti E., Bortolotti N., Deiuri E., Antonutto G., et al. Physical training effects in renal transplant recipients. Clin Transplant. 2010;24:510–514. doi: 10.1111/j.1399-0012.2009.01098.x. [DOI] [PubMed] [Google Scholar]
- 53.Romano G., Lorenzon E., Montanaro D. Effects of exercise in renal transplant recipients. World J Transplant. 2012;2:46–50. doi: 10.5500/wjt.v2.i4.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Aziz F., Muth B., Parajuli S., Garg N., Mohamed M., Mandelbrot D., et al. Unusually High Rates of Acute Rejection During the COVID-19 Pandemic: Cause for Concern? Kidney Int. 2020;S0085-2538(20):30683–30689. doi: 10.1016/j.kint.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]