Abstract
Purpose
The need for prolonged invasive mechanical ventilation in COVID-19 patients is placing the otorhinolaryngologist in front of an increasing request for tracheostomy. Nowadays, there is uncertainty regarding the timing of tracheostomy, the prognosis of these patients and the safety of healthcare workers. The aim of this study is to evaluate the efficacy and safety of tracheostomy placement in patients with COVID-19.
Methods
A retrospective cohort study on 23 COVID 19 patients, to analyse the timing of tracheostomy, the risk factors associated with in-hospital death and the infection of the involved health care workers. Early tracheostomy was defined as ≤ 10 days and late ones > 10 days.
Results
The mortality rate of COVID-19 patients admitted to ICU that underwent tracheostomy was 18%. The overall mortality of patients admitted to ICU was 53%. The univariate analysis revealed that early tracheostomy, SOFA score > 6, and D-dimer level > 4 were significantly associated with a greater risk of death. At the multivariate analysis SOFA score > 6 and D-dimer level > 4 resulted as significant factors for a higher risk of death. No health care workers associated with tracheostomy are confirmed to be infected by SARS-CoV2.
Conclusion
We suggest to wait at least 14 days to perform tracheostomy. In patients with SOFA score > 6 and D dimer > 4, tracheostomy should not be performed or should be postponed. Optimized procedures and enhanced personal protective equipment can make the tracheostomy safe and beneficial in COVID-19 patients.
Keywords: Tracheostomy, COVID-19, SOFA score, D-dimer level
Introduction
Up to May 18, 2020, a total of 224,760 had tested positive for COVID-19 in Italy and 31763 of them died. The metropolitan city of Venice, with an average population of 259414 inhabitants had 2617 confirmed cases with 256 deaths. In Venice, the incidence of SARS-COVID-2 was 1/110 inhabitants with a mortality rate of 9.8% [1]. As a Hub Hospital, our institution was one of the first in Veneto and in Italy to treat confirmed COVID-19, as this local area was recognized as one of the most critical areas of Northeastern Italy [2, 3].
The critical cases have been defined by the occurrence of respiratory failure requiring mechanical ventilation and treatment in the ICU [4]. Recent data from Europe suggest that in the most critically ill patients, the duration of invasive ventilation could go up to 21 days [5].
The prognosis of this novel disease is not yet fully understood and mortality rates for those requiring critical care varies a lot among different countries: 26% in Lombardy [6], 49% in Wuhan [7], 39% USA [8] and 51,6% UK [9].
The guidelines of performing a tracheostomy asserted that it is a standard of care due to its potentiality of reducing the duration of mechanical ventilation and length of stay on intensive care, but its utility in the recovery of patients with COVID-19 is unknown [9].
From the data found in the literature, the need for tracheostomies for ICU patients ranges normally from 2 to 11% [10, 11].
At the beginning of March 2020, the Italian Society of Otorhinolaryngology [12, 13], the British Association of Otorhinolaryngology [14], and the American Academy of Otolaryngology-Head and Neck Surgery [15] warned the otolaryngologists on a possible increase in the request for tracheostomies related to the COVID-19 infection.
During the COVID emergency, 23 of the 50 patients (46%), hospitalized in intensive care for COVID-19 in our hospital, underwent a temporary tracheostomy. Looking at the request for tracheostomy in the same period in 2019 and 2018, there was an increase in the execution of tracheostomies, respectively, of 69.5% and 56.5%.
As an aerosol-generating procedure, tracheostomy increases healthcare worker exposure to COVID-19 infection, but the duration of viral load and correlation with transmission rate are not yet precisely known [7].
Given these challenging issues, we have retrospectively analyzed our data to try to give an answer to three main problems related to tracheostomy in the COVID-19 patients:
For which patients is tracheostomy indicated?
What is the best timing for tracheostomy?
Which is the correlation between viral load and staff security?
We hypothesized that patients with poorer prognosis have a higher SOFA score and higher D-dimer level.
The aim of this study was to evaluate the timing, appropriateness and staff security of tracheostomy in patients receiving PMV in our medical-surgical ICU for SARS-COVID19.
Methods
This is a retrospective cohort study, which was conducted at Angel Hospital and Saints Giovanni e Paolo Hospital (Venice, Italy) from 22nd February 2020 to 26th April 2020.
The inclusion criteria for participants were (a) positive to COVID-19; (b) tracheostomy.
The following variables were selected:
Age.
Gender.
Comorbidities (diabetes, hypertension…).
Date of intubation.
Date of tracheostomy.
Type of tracheostomy (surgical vs percutaneous).
Mortality.
Sedation.
Date to sub-intensive unit.
Date of weaning from VAM.
Date of decannulation.
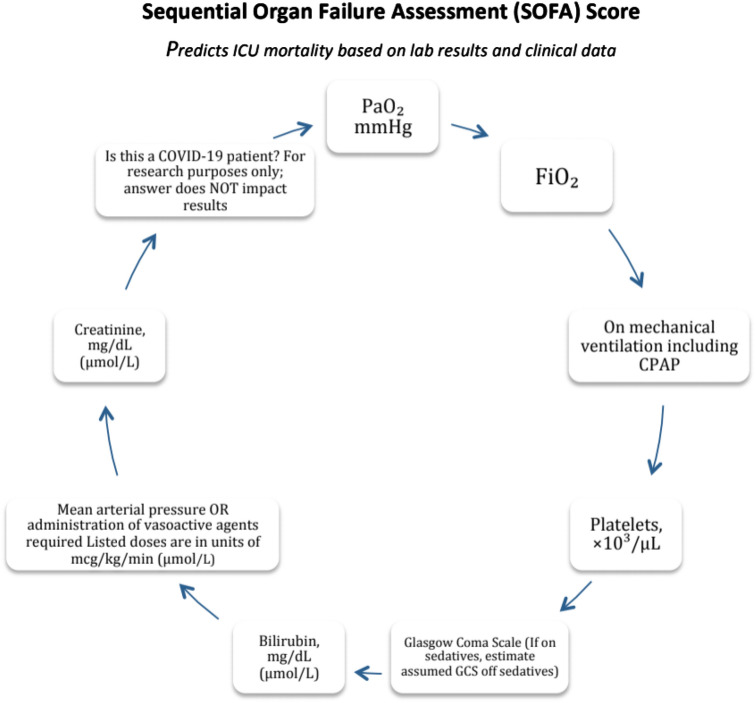
SOFA (Sequential Organ Failure Assessment)-score at the day of intubation and of the day before tracheostomy calculated using https://www.mdcalc.com/ (see Fig. 1 [16]).
D-dimer level.
Fig. 1.
Sequential organ failure assessment (SOFA) score
To explore the risk factors associated with in-hospital death, univariate and multivariate analyses were performed. Variables were chosen on the basis of previous findings and clinical constraints.
Previous studies have shown blood levels of D-dimer and Sequential Organ Failure Assessment (SOFA) scores to be higher in critically ill or fatal cases [17, 18].
Similar risk factors, including older age, have been reported to be associated with adverse clinical outcomes in adults with SARS and Middle East respiratory syndrome (MERS) [19]. Other studies underlined the negative effect of hypertension, cardiovascular disease and diabetes on survival [20].
Therefore, hypertension and cardiovascular disease, diabetes, pulmonary disease, simultaneous presence of two and/or three diseases, D-dimer, SOFA score at intubation and at tracheostomy and age were selected for our logistic regression model.
A statistical investigation was conducted to determine whether the timing of tracheostomy procedure was a prognostic factor for the survival status of the patients. Hence, tracheostomy was defined as early if performed within 10 days after intubation, as late otherwise. The average intubation time in this study was 13.7 days; thus, a 10-day threshold allowed to investigate the effect of an earlier-than-average tracheostomy. Moreover, previous studies have considered as early those procedures performed between 7 and 14 days from intubation [21, 22]. At the moment, there are no single criteria on the timing to perform the tracheostomy. In this study, patients were evaluated daily; the procedure was performed when the anesthesiologists verified that they could not be weaned from mechanical ventilation and the clinical conditions were stable, albeit the severity. Given the greater propensity in our hospital to perform surgical tracheostomies by otolaryngologists, this was the most used technique.
Open surgical tracheostomy procedures
We performed the first tracheostomy on 10th March 2020 when no ENT guidelines on safe tracheostomy were already been published [23].
The inclusion criteria in patients undergoing open surgical tracheostomy were patients have tested positive for COVID-19 with nasal pharyngeal swab for rtPCR assay testing and need for prolonged mechanical ventilation (for 5 or more days). The exclusion criteria, on the other hand, included patients with grave hypoxemia, severe incorrect coagulopathy or with multi-organ failure.
For each patient, we carried out a multidisciplinary discussion between the primary team, the team of procedures and the family to establish the objectives of the assistance, the general prognosis and the expected benefits of the tracheotomy.
For protective apparel, we adopted as a reference handbook of COVID-19 [24], where level III protection consisting of mask FFP3 (Europe) or N95, surgical cap, goggles and face shield (can be worn on top of goggles), surgical gown (use of double gown is preferable, where available) and gloves (use of double nitrile gloves) was suggested. Cap and shoe covers were considered necessary for safely dressing.
Even Personal Protective Equipment (PPE) doffing was a crucial moment which was carried out in a dedicated room. It is important to note that the wear and removal of PPE were sequential processes requiring proper training.
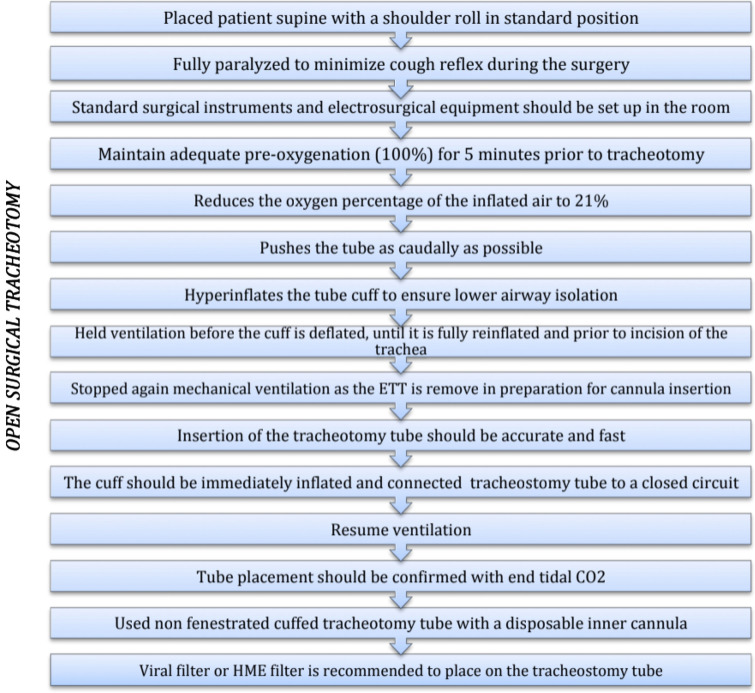
For the surgical tracheostomy placements, we followed the procedure contained in the “Safe tracheostomy for patients with severe acute respiratory syndrome” [25] summarized in Fig. 2.
Fig. 2.
Procedure of open surgical tracheotomy. ETT endotracheal tube, HME heat and moisture exchangers
We performed all tracheostomies in the ICU in negative-pressure rooms to avoid unnecessary transport of patients and repeated connection and disconnection of ventilatory circuits during transfer. Staff includes two surgeons, one intensive care specialist, one nurse of intensive care and two scrub nurses. One of the scrub nurses did not enter the room and supported the personnel in the wearing and removal of PPE and in preparing surgical instruments. Due to the respiratory issues, cannula with a large inner diameter was selected (Shiley 8 or 10). Cannula change was planned 7–10 days later using the same precautions (PPE utilization and airflow interruption). Afterwards, cannula change can be delayed 30 days after.
Statistical methods
At univariate level, the Fisher test was conducted to analyze the association between the response variable and all the categorical variables. Then a multivariate logistic regression was performed to investigate the effect of the variables on survival. A significance level of 10% was selected. Statistical analyses were performed using Software “R”.
Results
Totally, 50 patients were admitted in the ICU and ventilated with IVM with a diagnosis of COVID-19. The study cohort comprises 23 patients (21 men and 2 women with a median age of 69 years) who underwent a tracheostomy. Population characteristics are summarized in Tables 1 and 2.
Table 1.
COVID 19 patients medical value and follow up
| Case N | Gender | Age | No days intubated (E2T) | SOFA SCORE Intubation | SOFA SCORE tracheostomy | Weaned of sedation | Days of VAM | D | No Days to decanollation | D-Dimero | Alive | No Days from tracheostomy to deaths | Days in ICU | Outcome (Ward, ICU, discharge) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 81 | 10 | 7 | 4 | Yes | – | No | – | 1.59 | No | 12 | 13 | – |
| 2 | M | 84 | 17 | 4 | 5 | Yes | 48 | No | – | 2.11 | Yes | – | – | ICU |
| 3 | M | 75 | 16 | 4 | – | Yes | 46 | No | – | 0.53 | Yes | – | 35 | Ward |
| 4 | F | 77 | 9 | 7 | 6 | No | – | No | – | 1.44 | No | 7 | 15 | – |
| 5 | M | 81 | 10 | 10 | 5 | Yes | – | No | – | > 10 | No | 18 | 27 | – |
| 6 | M | 77 | 9 | 7 | 3 | Yes | 32 | Yes | 36 | 0.73 | Yes | – | 18 | Discharge |
| 7 | M | 72 | 15 | 6 | 8 | Yes | 40 | No | – | 0.87 | Yes | – | 32 | 1CU |
| 8 | M | 67 | 23 | 8 | 9 | Yes | 40 | No | – | 3.42 | Yes | – | 30 | Ward |
| 9 | M | 60 | 18 | 4 | 10 | Yes | 18 | No | – | 2.20 | Yes | – | 16 | ICU |
| 10 | M | 60 | 10 | 4 | 11 | No | – | No | – | > 10 | No | 15 | 24 | – |
| 11 | M | 61 | 15 | 3 | 4 | Yes | 38 | No | – | 1.61 | Yes | – | 27 | Ward |
| 12 | M | 48 | 26 | 8 | 8 | No | 46 | No | – | 6.67 | No | 18 | 44 | – |
| 13 | M | 49 | 13 | 4 | 3 | Yes | 31 | No | – | 4.83 | Yes | – | 22 | Ward |
| 14 | M | 76 | 15 | 4 | 7 | Yes | 28 | Yes | 21 | 3.66 | Yes | – | 20 | Discharge |
| 15 | 14 | 77 | 13 | 7 | 9 | No | – | No | – | 4.21 | No | 4 | 46 | – |
| 16 | M | 71 | 5 | 6 | 5 | Yes | 25 | Yes | 29 | 6.28 | Yes | – | 11 | Ward |
| 17 | M | 73 | 10 | 7 | 12 | Yes | 22 | No | – | 0.96 | Yes | – | 38 | ICU |
| 18 | M | 42 | 22 | 5 | 4 | Yes | 26 | Yes | 30 | 0.49 | Yes | – | 24 | Discharge |
| 19 | M | 68 | 14 | 3 | 8 | No | 25 | Yes | 17 | 0.46 | Yes | – | 38 | Discharge |
| 20 | F | 79 | 11 | 4 | 5 | Yes | 21 | Yes | 22 | 3.14 | Yes | – | 27 | Ward |
| 21 | M | 51 | 8 | 6 | 5 | No | – | No | – | > 10 | No | 14 | – | – |
| 22 | M | 79 | 7 | 10 | 3 | No | – | No | – | > 10 | No | 10 | 14 | – |
| 23 | M | 82 | 21 | 5 | 9 | No | – | No | – | 0.89 | No | 26 | 47 | – |
D decannulation, VAM ventilation assisted mechanical
Table 2.
Patients characteristics and comorbility
| Patients characteristics | ICU care (n = 23) |
|---|---|
| Age, years | 69 (42–84) |
| Sex | |
| Men | 21 (91%) |
| Women | 2 (8%) |
| Current smoking | 4 (17%) |
| Diabetes | 7 (30%) |
| Hypertension | 11 (47%) |
| Cardiovascular disease | 4 (17%) |
| Chronic obstructive pulmonary disease | 88 (34%) |
| Malignancy | 0 |
| Obesity | 3 (13%) |
| Chronic liver disease | 0 |
Twenty-two surgical tracheostomies and one percutaneous tracheostomy were performed.
The average time between the intubation date and the tracheostomy date was 13 days. The mean time that the patients were mechanically ventilated was 29 days. Mean time in ICU was 27 days. Patients with a longer hospital stay in intensive care were suffering from pre-existing pathologies and in this case, tracheostomy was necessary in the prevision of a more difficult weaning by mechanical ventilation.
Nine tracheostomies were performed early, while 14 tracheostomies were performed late. After a median follow-up of 50 days (IQR, 30.0–71.0 days), 9 patients (39%) died, 5 (22%) were receiving invasive mechanical ventilation in the ICU, 3 (13%) were discharged from the ICU and are in the pneumological sub-intensive unit, and 6 (26%) were decannulated and discharged. One patient has had complications; he presented post-tracheostomy bleeding, and he was on therapeutic anticoagulation.
In addition, a preliminary analysis of mortality rate of the entire sample of patients with COVID-19 recovered at ICU was carried out. The overall mortality rate was 53%; the mortality rate of patients with no tracheostomy was 35%; the mortality rate of patients with tracheostomy was 18%, of these, 6 (66.7%) tracheostomies were performed early and 3 (33.3%) late.
Among alive patients, mean time between tracheostomy and decannulation was 26.8 days (with a minimum of 17 and maximum of 36). Among dead patients mean time between intubation and death was 21 days and mean time between tracheostomy and death was 13.7 days. In our study, an early tracheostomy was associated with a greater risk of death. To date, none of our tracheostomy team has developed any symptoms of fever, general malaise, cough, shortness of breath and/or have tested positive for COVID-19 with nasal pharyngeal swab for rtPCR assay testing.
Statistical analysis
The univariate analysis revealed that early tracheostomy, SOFA score at intubation higher than 6 and D-dimer level higher than 4 were significantly associated with a greater risk of death with a p value, respectively, of 0.077, 0.077 and 0.023. At the multivariate analysis, SOFA score at intubation higher than 6 and D-dimer level higher than 4 were significantly associated with a greater risk of death with a p value, respectively, of 0.059 and 0.028. The variables age, sex, presence and number of comorbidities, and SOFA score at tracheostomy did not correlate with mortality rate. Results of statistical analysis are summarized in Table 3.
Table 3.
Statistical univariate and multivariate analysis results
| Total (n = 23) | Survivor (n = 14) 60% | Non survivor (n = 9) 40% | p value univariate analysis | p value multivariate analysis | |
|---|---|---|---|---|---|
| Early tracheostomy | 9 (39%) | 3 (21%) | 6 (66%) | 0.077 | – |
| SOFA score intubation > 6 | 9 (39%) | 3 (21%) | 6 (66%) | 0.077 | 0.059 |
| D-dimero > 4 | 8 (35%) | 2 (14%) | 6 (66%) | 0.023 | 0.028 |
Discussion
Tracheostomy in patients with COVID-19-associated respiratory failure is a challenging procedure due to both its severity, duration and risk of infections.
From data emerging in the literature and based on clinical experience, patients with COVID-19-associated respiratory failure required ventilatory support more than 4 weeks, which causes side effects such as prolonged rehabilitation as well as severe critical illness and neuropathy [5].
Tracheostomy is a widely used intervention in patients with acute respiratory failure needing prolonged IMV, but so far, no recommendation on COVID-19-affected patients exists [26].
At the moment, there are at least three unsolved questions regarding the execution of tracheostomies in COVID-19 patients.
The first concerns the prognosis of patients admitted to intensive care for COVID-19. Severe and critical illness occurred in approximately 20% of the patients after admission to hospital [5]. To decide whether to tracheostomize patients, it would be important to define prognostic survival indicators.
In contrast with Grasselli et al. [6], in our preliminary study, elder age and coexisting medical condition were not associated with a greater risk of poor outcome. On the other side, in accordance with Zhou, our preliminary experience identified as risk factors for COVID-19 mortality the high SOFA score and increased D-dimer [19]. Further studies are needed to better understand this association, but clinicians should be aware that for patients with SOFA score higher than 6 and D-dimer level higher than 4, tracheostomy could be not indicated or at least should be postponed.
The second problem concerns the timing of the execution of this operation [27, 28]: “Can an early tracheostomy improve the survival of patients since it reduces the ventilatory dead space, decreases the probability of ventilator pneumonia, decreases the stay in ICU, decreases the probability of developing septic shock and disseminated intravascular coagulation (CID) [19]?” In such a serious escalating pandemic, the aim of treating patients with COVID 19 disease is to maximize the likelihood of recovery as quickly as possible for the greatest number of patients.
In some hospitals, due to the short supply of resources such as ventilators and sedatives, an early tracheostomy, within 7 days of intubation, was initially proposed to be performed to reduce the patient’s need for sedation and to allow for an earlier transfer to the sub-intensive area. Others argued that reducing sedation and partially returning the patient to spontaneous breathing could cause negative effects on oxygenation and respiratory pattern [29]. Furthermore, Chao et al. [30] suggest to wait beyond 21 days for the viral load to decrease and to avoid unnecessary tracheostomies in particularly, critically ill patients.
The American Academy of Otolaryngology-Head and Neck surgery suggests that tracheostomy should be performed after 14 days of endotracheal intubation, but there is no evidence as to the optimal timing of tracheostomy [31].
Although outcome data on prone positioning in COVID-19 (used in 12% of patients in one ICU study from Wuhan) are currently lacking, the tendency for SARS-CoV-2 to affect the peripheral and dorsal areas of the lungs provides the ideal conditions for a positive oxygenation response to prone positioning [32]. Considering that some patients have to be prone in some cases for even 10 days and that tracheostomy within the first 24 h is a relative contraindication to pronation, it would be better to wait at least 10 days to perform tracheostomy [33].
The timing of tracheostomy is yet to be defined in such critically ill patients, but our results and recommendations worldwide would suggest performing a tracheostomy after at least 14 days of endotracheal intubation in patients who are unable to be weaned by ventilator but who have sufficient chances of survival.
Considering that in our study, mean time from intubation to death was 21 days, for patients with higher SOFA score and higher D-dimer level, we suggest to wait until 21 days to decide for tracheostomy to avoid clinically vain procedures for patients and to rule out health care workers from worthless exposure risks.
The third problem concerns the viral load of COVID-19 and the infectious capacity of the virus.
In Italy on April 5th, 12,252 health workers have tested positive for COVID-19, resulting in 10% of Italy’s COVID-19 cases; at the time we were writing, 165 medical doctors and 40 nurses have died [34, 35]. In China, more than 3300 healthcare workers were infected (4% of the 81,285 reported infections). In Spain, on 25th March, nearly 6500 medical personnel were infected, 13.6% of the country’s 47,600 total cases and 1% of the health system’s workforce [36].
As an aerosol-generating procedure, tracheostomy increases healthcare worker exposure to COVID-19 infection, but the duration of viral load and correlation with transmission rate is not yet precisely known [37].
Literature data show how the virus can remain in the body for up to 2 months [7]. However, in some cases, it may not be clinically or practically feasible to wait for a negative result prior to undertaking tracheostomy.
Our preliminary experience and early experience from other Italian [26, 38] and Chinese [39] studies support the safety of tracheostomy if appropriate protocols are strictly followed. After 1 month from the last tracheostomy we performed, none of our team developed symptoms of COVID-19. Specifically, recommendations contained in “Safe tracheostomy for patients with severe acute respiratory syndrome” revealed to be safe in our experience. The dress and undressing procedures and the use of specific DPI were of fundamental importance and limit the infections among clinicians; moreover, having a dedicated experienced team to fulfill tracheostomies will allow familiarity with the procedure, curtail the risk of contamination and decrease setup time.
This study has several limitations. First, our study might have selection bias because it was a single-center, retrospective study, with limited sample size, even if it had sufficient power to detect the significant differences between groups in mortality. Second, there is no assessment of the follow-up effect of the SARS-CoV-2 on discharged patients, although patients in this study were thought to have definite outcomes. Third, for the greater propensity in our hospital to perform surgical tracheostomies, it was not possible to carry out an analysis and comparison with percutaneous tracheostomies.
Finally, due to the short follow-up, we do not have data of beneficial effect of tracheostomy on long-term mortality and on the potential complications associated with tracheostomy; thus, further studies focusing on long-term outcomes are warranted.
The strength of our study is that is the first case series to report data on such a threatening issue and might help clinicians worldwide who will soon be dealing with the same challenges.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Emergenza Coronavirus SARS-CoV-2/COVID-19. https://www.regione.veneto.it/web/sanita/nuovo-coronavirus
- 2.Spinato G, Fabbris C, Polesel J, Cazzador D, Borsetto D, Hopkins C, Boscolo-Rizzo P. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA. 2020;323(20):2089–2090. doi: 10.1001/jama.2020.6771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boscolo-Rizzo P, Borsetto D, Spinato G, Fabbris C, Menegaldo A, Gaudioso P, Nicolai P, Tirelli G, Mosto MC, Rigoli R, Polesel J, Hopkins C. New onset of loss of smell or taste in household contacts of home-isolated SARS-CoV-2-positive subjects. Eur Arch Otorhinolaryngol. 2020;1:4. doi: 10.1007/s00405-020-06066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C, Wang Y, Li X, Ren L, Zhao J, Yi H, Zhang L, Fan G, Jiuyang X, Xiaoying G, Cheng Z, Ting Y, Xia J, Wei Y, Wenjuan W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with, novel coronavirus in Wuhan. China Lancet. 2019;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henrik PP, Thomas H, Anne P, Bülent U, Halfdan HK, Jakob R, Troels DP, Henning BN. Initial experiences from patients with COVID-19 on ventilatory support in Denmark. Dan Med J. 2020;67(5):A04200232. [PubMed] [Google Scholar]
- 6.Giacomo G, Alberto Z, Alberto Z, Massimo A, Luca C, Antonio C, Danilo C, Antonio C, Giuseppe F, Roberto F, Giorgio I, Nicola L, Luca L, Stefano M, Giuseppe N, Alessandra P, Marco VR, Anna MS, Enrico S, Maurizio C, Antonio P. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zunyou Wu, McGoogan Jennifer M. Characteristics of and important lessons from the coronavirus disease, (COVID-19) outbreak in China: summary of a report of 72,314 cases from the chinese center for disease control and prevention. JAMA. 2019 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 8.Matthew JC, Matthew RB, Darryl A, Samuel DJ, Benjamin JM, Elizabeth MB, Justin GA, Jan C, LeRoy ER, Jonathan H, Beth RH, John SS, Natalie HY, Daniel B, Max RO. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020 doi: 10.1016/s0140-6736(20)31189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Takhar A, Walker A, Tricklebank S, Wyncoll D, Hart N, Jacob T, Arora A, Skilbeck C, Simo R, Surda P. Recommendation of a practical guideline for safe tracheostomy during the COVID-19 pandemic. Eur Arch Otorhinolaryngol. 2020;21:1–12. doi: 10.1007/s00405-020-05993-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nora HC, Lena MN. Tracheostomy: epidemiology, indications, timing, technique, and outcomes. Respir Care. 2014;59(6):895–915. doi: 10.4187/respcare.02971. [DOI] [PubMed] [Google Scholar]
- 11.Mohammad WA, Ahmad AFN, Mohammad AS, Ahmed M, Alaa OK. Tracheostomy in the intensive care unit: a university hospital in a developing country study. Int Arch Otorhinolaryngol. 2017;1:33–37. doi: 10.1055/s-0036-1584227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.La tracheostomia in pazienti affetti da COVID-19. https://www.sioechcf.it/wp-content/uploads/2020/03/La-tracheostomia-in-pazienti-affetti-da-COVID-19.pdf
- 13.Ralli M, Greco A, De Vincentis M. The effects of the COVID-19/SARS-CoV-2 pandemic outbreak on otolaryngology activity in Italy. Ear Nose Throat J. 2020;1:1. doi: 10.1177/0145561320923893. [DOI] [PubMed] [Google Scholar]
- 14.Guidance for Surgical Tracheostomy and Tracheostomy Tube Change during the COVID-19 Pandemic. https://www.entuk.org/tracheostomy-guidance-during-covid-19-pandemic [DOI] [PMC free article] [PubMed]
- 15.Tracheotomy Recommendations During the COVID-19 Pandemic. https://www.entnet.org/content/tracheotomy-recommendations-during-covid-19pandemic
- 16.Sequential Organ Failure Assessment (SOFA) Score. https://www.mdcalc.com/sequential-organ-failure-assessment-sofa-score
- 17.Zhang L, Yan X, Fan Q, Liu H, Liu X, Liu Z, Zhang Z. D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19. J Thromb Haemost. 2020 doi: 10.1111/jth.14859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yao Q, Wang P, Wang X, Qie G, Meng M, Tong X, Bai X, Ding M, Liu W, Liu K, Chu Y. Retrospective study of risk factors for severe SARS-Cov-2 infections in hospitalized adult patients. Pol Arch Intern Med. 2020 doi: 10.20452/pamw.15312. [DOI] [PubMed] [Google Scholar]
- 19.Zhou F, Ting Y, Ronghui D, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Xiaoying G, Guan L, Wei Y, Li H, Xudong W, Jiuyang X, Shengjin T, Zhang Y, Chen H, Cao Bin. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):10541062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ren D, Ren C, Yao R, Feng Y, Yao Y. Clinical features and development of sepsis in patients infected with SARS-CoV-2: a retrospective analysis of 150 cases outside Wuhan, China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-06084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dochi H, Matsumura MN, Cammack I, Furuta Y. Effect of early tracheostomy in mechanically ventilated patients. Laryngoscope Investig Otolaryngol. 2019;4(3):292–299. doi: 10.1002/lio2.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adly A, Youssef TA, El-Begermy MM, Younis HM. Timing of tracheostomy in patients with prolonged endotracheal intubation: a systematic review. Eur Arch Otorhinolaryngol. 2018;275:679–690. doi: 10.1007/s00405-017-4838-7. [DOI] [PubMed] [Google Scholar]
- 23.Haen P, Caruhel JB, Laversanne S, Cordier PY. CORONA-steps for tracheotomy in COVID-19 patients: a staff-safe method for airway management. Oral Oncol. 2020;105:104729. doi: 10.1016/j.oraloncology.2020.104729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu L (2020) Handbook of COVID-19 Prevention and Treatment
- 25.Wei W, Tuen HH, Ng RW, Lam LK. Safe tracheostomy for patients with severe acute respiratorysyndrome. Laryngoscope. 2003;113(10):1777–1779. doi: 10.1097/00005537-200310000-00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mattioli F, Fermi M, Ghirelli M, Molteni G, Sgarbi N, Bertellini E, Girardis M, Presutti L, Marudi A. Tracheostomy in the COVID-19 pandemic. Eur Arch Otorhinolaryngol. 2020 doi: 10.1007/s00405-020-05982-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marcus JS, Rajyabardhan P, Arjen MD. Walking the line between benefit and harm from tracheostomy in COVID-19. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30231-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brendan AM, Michael JB, Stephen JW, Vinciya P, Asit A, Tanis SC, José MA, Gonzalo HM, Robert DT, Susan DB, Grace CYL, Christine M, Christopher HR, Joshua A, Li Q, Sébastien V, Pavel D, Johannes Z, Massimo A, Paolo P, Brian KW, Erin W, You S, Stefano G, Abele D, Mervyn S, Peter JMO, Neil T, Howard M, David JFK. Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.China With The World: COVID-19 Experts Dialogues—The 2nd Talk Transcript. https://healthmanagement.org/c/icu/pressrelease/china-with-the-world-covid-19-experts-dialogues-the-2nd-talk-transcript
- 30.Chao TN, Benjamin MB, Niels DM, Ara AC, Joshua HA, Andrew RH, Christopher HR. Tracheotomy task force, a working group of the airway safety committee of the university of pennsylvania health system. Tracheotomy in ventilated patients with COVID-19 guidelines from the COVID-19. Ann Surg. 2020 doi: 10.1097/sla.0000000000003956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American Academy of Otolaryngology and Head and Neck Surgery (2020) AAO position statement: tracheotomy recommendations during the COVID-19 pandemic. https://www.entnet.org/content/aao-position-statement-tracheotomy-recommendations-during-covid-19-pandemic. Accessed 2 Apr 2020
- 32.Phua J, Weng L, Ling L, Egi M, Lim CM, Divatia JV, Shrestha BR, Arabi YM, Ng J, Gomersall CD, Nishimura M (2020) Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med [DOI] [PMC free article] [PubMed]
- 33.Oliveira VM, Piekala DM, Deponti GN, Batista DC, Minossi SD, Chisté M, Bairros PM, Naue WD, Welter DI, Vieira SR. Safe prone checklist: construction and implementation of a tool for performing the prone maneuver. Rev Bras Ter Intensiva. 2017;29(2):131–141. doi: 10.5935/0103-507X.20170023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chirico F, Nucera G, Magnavita N. COVID 19. Protecting healthcare workers is a priority. Infect Control Hosp Epidemiol. 2020;1:1. doi: 10.1017/ice.2020.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Elenco dei Medici caduti nel corso dell’epidemia di Covid-19. https://portale.fnomceo.it/elenco-dei-medici-caduti-nel-corso-dellepidemia-di-covid-19/
- 36.COVID-19 How many Healthcare workers are infected? https://www.cebm.net/covid-19/covid-19-how-many-healthcare-workers-are-infected/
- 37.Mick P, Murphy R. Aerosol-generating otolaryngology procedures and the need for enhanced PPE during the COVID-19 pandemic: a literature review. J Otolaryngol Head Neck Surg. 2020;49(1):29. doi: 10.1186/s40463-020-00424-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Turri-Zanoni M, Battaglia P, Czaczkes C, Pelosi P, Castelnuovo P, Cabrini L. Elective tracheostomy during mechanical ventilation in patients affected by COVID-19: preliminary case series from lombardy, Italy. Otolaryngol Head Neck Surg. 2020 doi: 10.1177/0194599820928963. [DOI] [PubMed] [Google Scholar]
- 39.Zhang X, Huang Q, Niu X, Zhou T, Xie Z, Zhong Y, Xiao H. Safe and effective management of tracheostomy in COVID-19 patients. Head Neck. 2020 doi: 10.1002/hed.26261. [DOI] [PMC free article] [PubMed] [Google Scholar]