Abstract
Purpose
Black physicians remain disproportionately underrepresented in certain medical specialties, yet comprehensive assessments in radiation oncology (RO) are lacking. Our purpose was to report current and historical representation trends for Black physicians in the US RO workforce.
Methods and Materials
Public registries were used to assess significant differences in 2016 representation for US vs RO Black academic full-time faculty, residents, and applicants. Historical changes from 1970 to 2016 were reported descriptively. Linear regression was used to assess significant changes for Black residents and faculty from 1995 to 2016.
Results
In 2016, Black people represented 3.2% vs 1.5% (P < .001), 5.6% vs 3.2% (P = .005), and 6.5% vs 5.4% (P = .352) of US vs RO faculty, residents, and applicants, respectively. Although RO residents nearly doubled from 374 (1974) to 720 (2016), Black residents peaked at 31 in 1984 (5.9%; 31 of 522) and fell to 23 (3.2%; 23 of 720) in 2016 across 91 accredited programs; Black US graduate medical education trainees nearly doubled over the same period: 3506 (1984) to 6905 (2016). From 1995 to 2016, Black US resident representation significantly increased by 0.03%/y, but decreased significantly in RO by –0.20%/y before 2006 and did not change significantly thereafter. Over the same period, Black US faculty representation significantly increased by 0.02%/y, whereas Black RO faculty significantly increased by 0.07%/y before 2006, then decreased significantly by –0.16%/y thereafter. The number of Black RO faculty peaked at 37 in 2006 (3.1%; 37 of 1203) and was 27 (1.5%; 27 of 1769) in 2016, despite the nearly 1.5-fold increase in the number of both RO faculty and Black US faculty overall (4169 in 2006 and 6047 in 2016) during that period.
Conclusions
Black physicians remain disproportionately underrepresented in RO despite an increasing available pipeline in the US physician workforce. Deliberate efforts to understand barriers to specialty training and inclusion, along with evidence-based targeted interventions to overcome them, are needed to ensure diversification of the RO physician workforce.
Introduction
National attention has shifted to how health disparities based on race and ethnicity affect population health as a result of the coronavirus disease 2019 (COVID-19) pandemic and calls for racial justice surrounding the fatal asphyxiation of George Floyd. Although Black or African American and American Indian or Alaskan Native populations have the poorest overall health status among population groups in the United States, Black people experience the worst cancer outcomes of all races and ethnicities.1 The lack of diversity within the physician workforce is a potential contributor to disparities, particularly those related to cancer outcomes,2 and thus, increasing physician workforce diversity has been identified as a means to address health disparities and improve health equity.3 For example, Black academic faculty are more likely to conduct health disparities research than their White counterparts,4 and minority physicians are more likely to practice in underserved communities and treat uninsured patients than their White counterparts.5 In fact, a physician’s race and ethnicity are more predictive of their likelihood to care for the underserved than growing up with a socioeconomically disadvantaged background.6 , 7
Underrepresentation of specific minority groups may be driven by structural barriers, including inadvertent or overt exclusion of these populations (ie, structural racism) throughout society and the academic pipeline.8 Although there have been efforts to address physician workforce diversity and increase the representation of individuals from racial and ethnic demographic groups that are historically underrepresented in medicine (URM),9 , 10 Black physicians remain disproportionately underrepresented in certain medical specialties such as radiation oncology, despite the current available pipeline. An analysis of 2012 data found that radiation oncology ranked near the bottom of the largest 20 training specialties with respect to racial, ethnic, and gender diversity, with significantly less women, Black people, Hispanic people, and combined URMs compared with the total graduate medical education (GME) pool of trainees.11 Between 2003 and 2010, there was a significant declining trend in Black representation among radiation oncology trainees.12 Yet more recent and comprehensive historical analyses are lacking. The purpose of our study was to assess current and historical representation trends for Black physicians in the US radiation oncology workforce.
Methods and Materials
Measures
Variables evaluated included race, ethnicity, and sex, defined consistently with the US Census Bureau.13 Racial groups included White; Black; Asian or Asian American (referred to as Asian); American Indians, Alaska Natives, Native Hawaiians, and Pacific Islanders, grouped as one category; and Other, defined in this study as any person with unknown racial information or not classifiable into one of the listed racial categories. Ethnic groups included Hispanic and non-Hispanic. Sex included men and women, which was self-reported in the primary data sources.
Data sources
Primary data on race, ethnicity, and sex were obtained from publicly available sources. For race and ethnicity variable measures, unduplicated totals were obtained of the US medical school graduates, residency applicants, residents, faculty, and practicing physicians for race and ethnicity groups separately. US medical school graduate numbers14 and Electronic Residency Applicant Service (ERAS) residency applicant data15 for 2016 were obtained from the Association of American Medical Colleges (AAMC). Historical data from 1970 to 2016 for Accreditation Council for Graduate Medical Education (ACGME) US and radiation oncology residents were obtained from annual Journal of the American Medical Association supplements of actual trainee numbers as previously described16; the specific years available were 1970 to 1972, 1974, 1977 to 1990, and 1995 to 2016. Historical data on academic, full-time faculty from 1970 to 2016 were obtained from the AAMC,17 , 18 with all years available; racial distribution by sex was only available for faculty data. Practicing physician data were obtained from the 2015 American Medical Association Masterfile, which represented 2013 data—the most recent year available for this group.19 All data sources and selected years represent the entire population in question, providing an estimate of the race, ethnicity, and sex of all applicants, trainees, faculty, and practicing physicians within the US and radiation oncology physician workforce.
Statistical analysis
To assess current representation for the most recent year (2016) with publicly available data at the time of the analysis, binomial tests were used to investigate differences in the proportion of Black doctors among US vs radiation oncology faculty, residents, and applicants, separately; US vs radiation oncology practicing physician representation was compared for the year 2013, representing the most recent year available for that group. Next, the proportion of Black radiation oncology as residents in 2016 was compared with applicants in 2016, faculty in 2016, and practicing physicians in 2013, due to the aforementioned availability of current data. Adjusting for a total of 7 comparisons, a Bonferroni correction, P < .00714 was considered statistically significant. The actual, unadjusted P values are presented. Fisher exact test was used to compare the rank distribution of Black faculty in radiation oncology versus the US academic faculty workforce for 2016.
Descriptive statistics were used to assess historical changes in the representation of Black residents and faculty from 1970 to 2016. To assess the significance of changes in the proportions of Black representation over the past 31 academic years (1995-2016), we estimated the slope (ie, change in percent per year) and the associated 95% confidence intervals for residents and full-time faculty using a simple linear regression model where year was used as an independent variable. Because we observed different linear patterns for Black RO residents and RO faculty before and after 2006, we fitted a piecewise linear regression model that allowed for the changing slope at 2006. A weighted least-squared method was used to account for nonconstant variance because the dependent variables of the regressions were proportions. The fitted lines under the piecewise models were more consistent with the observed RO data based on R-squared statistics rather than a simple linear trend line.
Results
Current status
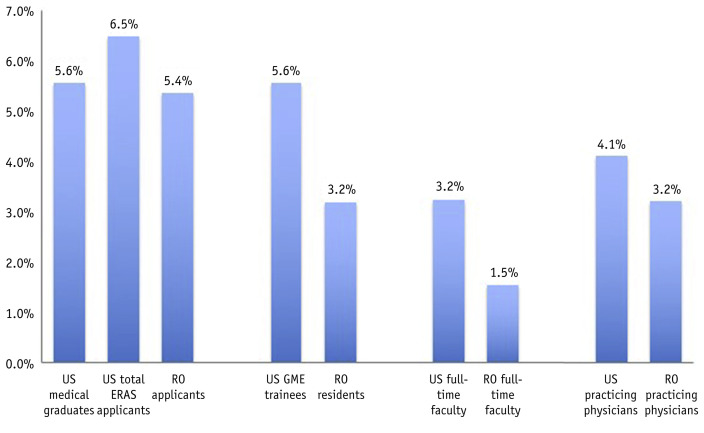
In 2016, Black people represented 5.6%, 6.5%, 5.6%, and 3.2% of US medical graduates, ERAS applicants, GME trainees, and faculty, respectively (Table E1). Within radiation oncology, Black doctors 5.4%, 3.2%, and 1.5% of ERAS applicants, GME residents, and faculty, respectively. Black doctors in radiation oncology were significantly underrepresented as faculty (P < .0001), and residents (P = .0052), but not as applicants (P = .3519) compared with their proportions in the corresponding US pool (Table 1 and Fig. 1 ). Black doctors were similarly underrepresented as practicing physicians in 2013 in radiation oncology compared with the US pool (respectively, 3.2% vs 4.1%, P < .0001). In 2016, Black representation as radiation oncology residents (3.2%) differed significantly compared with radiation oncology faculty (1.5%, P = .0071), but not radiation oncology applicants (5.4%, P = .0664) or 2013 radiation oncology practicing physicians (3.2%, P = .9547). Black faculty in radiation oncology were mostly junior rank (17 of 27; 63.0%): full (7), associate (3), assistant (15), or instructor (2); this distribution did not differ significantly (P = .402) from the US Black faculty overall: junior rank (4140 of 5879; 70.4%): full (676), associate (1063), assistant (3533), and instructor (607).
Table 1.
Comparisons of Black physician representation in the United States vs radiation oncology workforce
| Total N | Black N (%) | ||
|---|---|---|---|
| US ERAS applicants | 44,346 | 2871 (6.5%) | P = .3519 |
| RO applicants | 429 | 23 (5.4%) | |
| US GME trainees | 124,096 | 6905 (5.6%) | P= .0052 |
| RO residents | 720 | 23 (3.2%) | |
| US practicing physicians∗ | 1,045,910 | 42,844 (4.1%) | P <.0001 |
| RO practicing physicians∗ | 5210 | 169 (3.2%) | |
| US full-time faculty | 172,979 | 5592 (3.2%) | P <.0001 |
| RO full-time faculty | 1769 | 27 (1.5%) |
Abbreviations: ERAS = Electronic Residency Applicant Service; GME = graduate medical education; RO = radiation oncology.
Bold represents significant P values.
All comparisons represent 2016 data, except practicing physicians, which represents 2013 data.
Fig. 1.
Representation of Black in the United States physician workforce and radiation oncology in 2016∗. Abbreviations: ERAS = Electronic Residency Applicant Service; GME = graduate medical education. ∗with the exception of practicing physicians, which represents 2013 data.
Historical trends
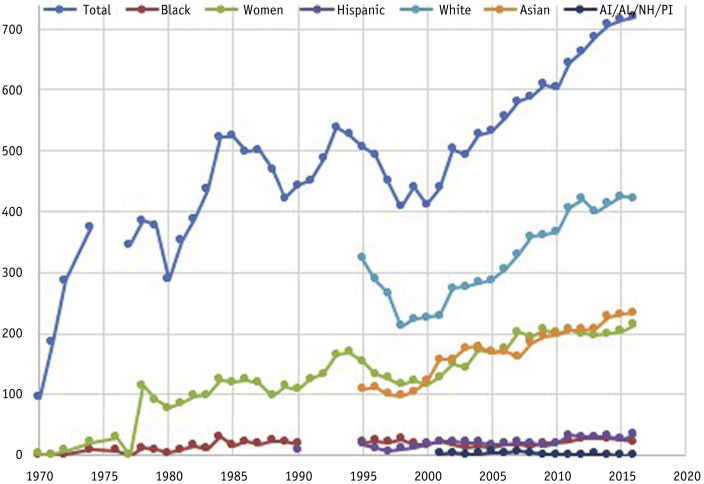
Historically, Black GME representation averaged 2.3% (1970-1977—the first 5 years publicly reported) and 5.7% (2012-2016) for 3.4% absolute increase over more than 40 years. Black representation as radiation oncology residents averaged 1.0% (1970-1977) and 3.9% (2012-2016) for a 2.9% absolute increase. Although radiation oncology residents nearly doubled from 374 (1974) to 720 (2016), the number of Black residents peaked at 31 in 1984 (5.9%; 31 of 522) and most recently was 23 (2016) across 91 ACGME residency programs (Fig. 2 ); Black GME trainees nearly doubled over the same period: 3506 (1984) to 6905 (2016).When assessing for the significance of changes in demographic representation for radiation oncology residents between 1995 and 2016 (Table E2), representation was found to be significantly increasing at the following percentages per year for Asians (0.424%, P < .001) and Hispanics (0.085%, P = .006), but not for White people (0.207%, P = .087) or combined American Indians, Alaska Natives, Native Hawaiians, and Pacific Islanders (–0.033%, P = .015). Representation of Black residents in radiation oncology was significantly decreasing (–0.199%/y, P < .001) before 2006, and not significantly changing thereafter (0.113%/y, P = .018) (Fig. 3 ). Representation for Black trainees in the US overall increased significantly at 0.030%/y from 1995 to 2016.
Fig. 2.
Absolute number of United States radiation oncology residents by race, ethnicity, and sex from 1970 to 2016.
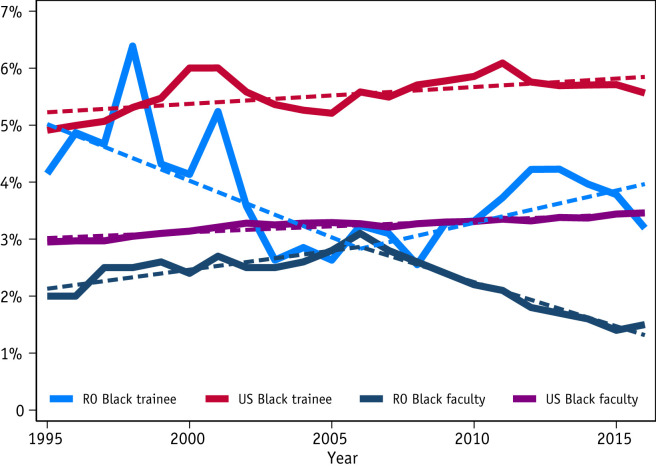
Fig. 3.
Representation of Black physicians as United States and Radiation Oncology residents and faculty from 1995 to 2016. Fitted line represents results of the linear regression.
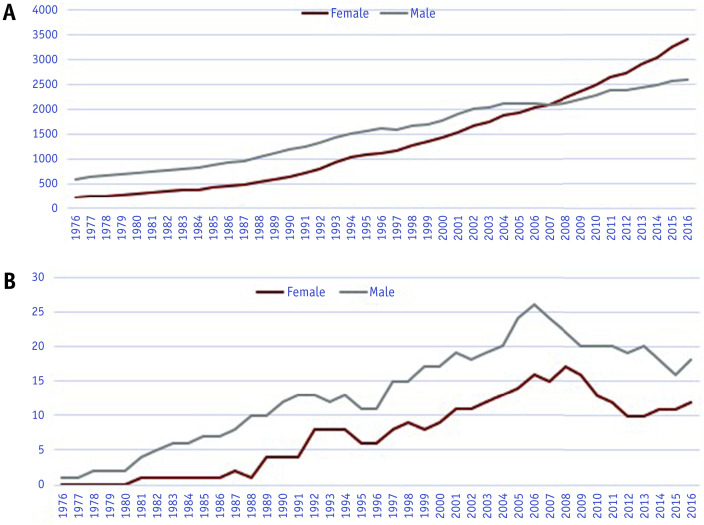
Black radiation oncology faculty representation averaged 0.1% (1970-1977) and 1.6% (2012-2016) for an absolute increase of 1.5%. The number of Black radiation oncology faculty (Fig. 3) peaked at 37 in 2006 (3.1%; 37 of 1203) and was 27 (1.5%; 27 of 1769) in 2016 despite the nearly 1.5-fold increase in the number of both radiation oncology faculty and Black US faculty overall (4169 in 2006 and 6047 in 2016) during that same period. Black female representation increased for both US and radiation oncology faculty, respectively representing 41% and 35% of Black faculty in 1995 and 56% and 40% of Black faculty in 2016 (Fig. 4 ). When assessing for the significance of changes in the representation of Black faculty between 1995 and 2016 (Table 2 ), representation was found to be significantly increasing at 0.021%/y (P < .001) for US Black faculty overall. Black faculty in radiation oncology were significantly increasing in representation before 2006 at 0.067%/y (P < .001), then significantly decreasing in representation thereafter at –0.155%/y (P < .001).
Fig. 4.
Number of Black full-time female and male faculty in (A) the United States and (B) radiation oncology from 1976 to 2016.
Table 2.
Immediate strategies to mitigate racial bias and increase Black representation in radiation oncology
| Barrier | Supporting Evidence | Intervention |
|---|---|---|
| Interpersonal racial bias against trainees and faculty |
|
|
| Systemic bias in residency selection criteria |
|
|
| Disparate trainee exposure and financial toxicities |
|
|
| Recruitment and retention of Black faculty |
|
|
Discussion
In this analysis of Black representation in the US radiation oncology physician workforce, we found that Black residents remain disproportionately underrepresented compared with the overall US trainee pool with declines in more recent years. The number of overall radiation oncology residents and the number of Black trainees in the US have nearly doubled over the past 40 years and 30 years, respectively, indicating an available pipeline. Unfortunately, the absolute number of Black radiation oncology residents was highest in 1984 and has decreased over those same periods. Currently, most programs do not have a single Black resident—with only 23 Black residents across 91 ACGME residency programs in 2016. Similar declines were noted for Black faculty in radiation oncology, who will inevitably remain underrepresented owing to the lack of increasing representation of Black residents in radiation oncology. Although there remain challenges in the Black medical student pipeline,20 the percentage of Black medical student applicants approximates that of Black matriculants.21 This is distinctly not the case for the yield of Black applicants to radiation oncology residency training programs.
Further confirming the notion of a readily available pipeline, data show that Black representation in the radiation oncology resident applicant pool was similar to their representation in the general US resident applicant pool. Black US (6.5%) and radiation oncology (5.4%) ERAS applicant representation did not differ significantly. However, by comparison, Black trainees were were significantly underrepresented as radiation oncology residents compared with their representation as US residents (US 5.6% vs radiation oncology 3.2%), suggesting that potential biases during the matching process should be explored as contributors to the effective exclusion of Black trainees. Previous studies have demonstrated such interpersonal bias by race, ethnicity, and gender when evaluating equally qualified candidates in grant awarding, publication submissions, mentorship opportunities, evaluations, and hiring.22, 23, 24, 25 Because demographic data by race, ethnicity, and gender are not publicly available from the National Residency Matching Program as they exist for ERAS applicants, the question of implicit selection bias during the residency interviewing and matching process is not readily assessable, although it should be pursued.
Such biases may manifest in a variety of ways and affect Black representation in radiation oncology. Although the attainment of research skills and comprehension are necessary in radiation oncology training, an example of systemic bias is the strong emphasis placed on research productivity and the possession of a basic doctor of science degree during the residency applicant interview and selection process.26 Black students, through structural societal barriers and systemic racism and discrimination, may not have the opportunity to obtain research opportunities.27 For example, Black medical students are less likely to attend schools that have affiliated radiation oncology residency programs12 and may face financial barriers to performing research within or outside of their school curriculum.28 Furthermore, Black students, in addition to other URMs and women, are not sufficiently represented as master or doctorate students, which may be driven by the leakage and aforementioned exclusion that occurs throughout the educational pipeline and STEM sciences.29 Although basic science PhD research training may be important for those who go on to pursue academic careers, it has not been demonstrated to predict for success among those who choose to advance the field via other avenues, including leadership and delivery of high-quality patient care. By using selection criteria that presume to be merit-based, yet are “blind” to privilege and societal inequities, the end results include perpetuation of unjust societal structures and reduction in diverse, intellectual capital for our field and patients. Interventions that may facilitate greater diversity and inclusion in radiation oncology resident selection include investigating whether the heavy weighting of preresidency research experiences or a basic science PhD as selection criteria is unbiased and implementing more widespread use of holistic review and selection practices. According to the AAMC, holistic review refers to mission-aligned selection processes that consider a broad range of factors—experiences, attributes, and academic metrics—when reviewing applications, allowing consideration of the “whole” applicant, rather than disproportionately focusing on any one factor.30 The increased compositional diversity of medical school matriculants, for example, has been correlated with the widespread implementation of holistic review by medical school admissions committees since 2009.31
Although the lack of a significant difference between Black US and radiation oncology ERAS applicants may also suggest that disparate exposure may not be a barrier to training, this comparison is likely an inadequate measure to fully assess demographic differences in exposure. Given the small overall number of Black radiation oncology applicants, it may not be possible to detect small but still meaningful differences relative to US applicants overall, and thus disparities in exposure should still be explored. Prior analyses have shown that Black (and Hispanics) are less likely to attend medical schools with affiliated programs,12 which may be detrimental to specialty selection and matching because the majority of residents (82%) in radiation oncology generally emanate from medical schools with affiliated radiation oncology programs, with 30% staying at their home institution as evidenced in an analysis of 2013 residents.32 Providing funded exposure opportunities for students at medical schools with unaffiliated residency programs may therefore foster increased diversity. It is also vital to address how the financial costs of the entire residency exposure, interview, and selection process may impose structural barriers to inclusive recruitment and retention33; greater implementation of remote learning and use of electronic interview processes, as is currently being discussed as part of managing ACGME activities during the COVID-19 pandemic, may help reduce these costs and provide improved access for URMs in addition to geographically and socioeconomically disadvantaged groups.
Black representation as radiation oncology faculty showed the greatest relative disparity compared with other physician categories. The proportion of Black female faculty compared with Black men was notably less in radiation oncology compared with the US workforce (Fig. 4), likely representing an intersectional issue related to gender diversity.34 The male predominance of the field further acts to decrease Black representation when considering that Black female medical students now outnumber Black men nearly 2:1.26 Additionally, rank distribution of Black faculty demonstrated significant attrition. Because the relative proportions were similar to the US faculty, this suggests more pervasive structural issues with the retention of Black faculty in academia which may not be unique to radiation oncology. Previous explanations for attrition and barriers to career advancement for URM and Black physicians at the midcareer levels include absent institutional and executive commitment to diversity and inclusion; the minority tax/majority subsidy (terms used to describe the additional and usually unrewarded work of promoting diversity and inclusion that falls disproportionately to URM physicians); social isolation and exclusion; burnout; overt discrimination, harassment, and bias; and undervaluing of activities that do not meet traditional metrics of academic promotion, such as community outreach and engagement and exercises in social justice.33 The lack of recruited and/or retained Black faculty to provide visibility and mentorship in our relatively obscure specialty often omitted from the medical school core curriculum inevitably contributes to the lack of Black trainees and further exacerbates the perpetual circle of underrepresentation. The aforementioned implicit bias against minorities when seeking mentorship may therefore further inhibit Black people and other URMs from being able to successfully match into the field. The strategies and points of intervention discussed in this section are summarized in Table 2.
Limitations of this study include the small number of Black physicians in radiation oncology overall, which limits the power to detect small yet potentially relevant differences, and the single year assessed for the comparative analysis, which represented the most recent year of publicly available data given the 2-year lag in reporting. Historical trends over time were assessed to mitigate this potential limitation. Moreover, we acknowledge that the racial categories used—as defined by the US census and consistent with the AAMC and ACGME—fail to discern the geographic and cultural heterogeneity (eg, country of origin) within these groups, which may influence representation trends over time.
Conclusions
Black physicians remain disproportionately underrepresented in radiation oncology with minimal historical improvements and decreased representation despite an increasing available pipeline in the US physician workforce. Deliberate efforts to understand the barriers and structural determinants to specialty training and inclusion relative to other successful specialties, along with evidence-based targeted interventions to overcome them, are needed to ensure diversification of the radiation oncology physician workforce.
Footnotes
Disclosures: There are no actual or potential conflicts of interest to disclose for any of the authors.
The majority of the data generated and analyzed during this study are included in this published article and its supplementary information files. The remainder may be shared upon reasonable request to the corresponding author.
Supplementary material for this article can be found at https://doi.org/10.1016/j.ijrobp.2020.07.015.
Supplementary Data
References
- 1.National Cancer Institute Surveillance, epidemiology, and end results program. Cancer stat facts: cancer disparities. https://seer.cancer.gov/statfacts/html/disparities.html Available at:
- 2.Winkfield K.M., Flowers C.R., Mitchell E.P. Making the case for improving oncology workforce diversity. Am Soc Clin Oncol Educ Book. 2017;37:18–22. doi: 10.1200/EDBK_100010. [DOI] [PubMed] [Google Scholar]
- 3.Iglehart J.K. Diversity dynamics—challenges to a representative U.S. medical workforce. N Engl J Med. 2014;371:1471–1474. doi: 10.1056/NEJMp1408647. [DOI] [PubMed] [Google Scholar]
- 4.Hoppe T.A., Litovitz A., Willis K.A. Topic choice contributes to the lower rate of NIH awards to African-American/black scientists. Sci Adv. 2019;5 doi: 10.1126/sciadv.aaw7238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marrast L.M., Zallman L., Woolhandler S., Bor D.H., McCormick D. Minority physicians’ role in the care of underserved patients: Diversifying the physician workforce may be key in addressing health disparities. JAMA Intern Med. 2014;174:289–291. doi: 10.1001/jamainternmed.2013.12756. [DOI] [PubMed] [Google Scholar]
- 6.Cantor J.C., Miles E.L., Baker L.C., Barker D.C. Physician service to the underserved: Implications for affirmative action in medical education. Inquiry. 1996;33:167–180. [PubMed] [Google Scholar]
- 7.Smedley B.D., Stith A.Y., Colburn L. The Right Thing to Do, The Smart Thing to Do: Enhancing Diversity in the Health Professions: Summary of the Symposium on Diversity in Health Professions in Honor of Herbert W. Nickens, M.D. National Academies Press; Washington, DC: 2001. Increasing racial and ethnic diversity among physicians: An intervention to address health disparities? [PubMed] [Google Scholar]
- 8.Boyd R.W. The case for desegregation. Lancet. 2019;393:2484–2485. doi: 10.1016/S0140-6736(19)31353-4. [DOI] [PubMed] [Google Scholar]
- 9.Butler P.D., Britt L.D., Richard C.E. The diverse surgeons’ initiative: Longitudinal assessment of a successful national program. J Am Coll Surg. 2015;220:362–369. doi: 10.1016/j.jamcollsurg.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 10.Mason B.S., Ross W., Ortega G., Chambers M.C., Parks M.L. Can a strategic pipeline initiative increase the number of women and underrepresented minorities in orthopaedic surgery? Clin Orthop Relat Res. 2016;474:1979–1985. doi: 10.1007/s11999-016-4846-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deville C., Hwang W.T., Burgos R. Diversity in graduate medical education in the United States by race, ethnicity, and sex, 2012. JAMA Intern Med. 2015;175:1706–1708. doi: 10.1001/jamainternmed.2015.4324. [DOI] [PubMed] [Google Scholar]
- 12.Chapman C.H., Hwang W.T., Deville C. Diversity based on race, ethnicity, and sex, of the US radiation oncology physician workforce. Int J Radiat Oncol Biol Phys. 2013;85:912–918. doi: 10.1016/j.ijrobp.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 13.Humes K.R., Jones N.A., Ramirez R.R. Overview of race and Hispanic origin: 2010. www.census.gov/prod/cen2010/briefs/c2010br-02.pdf Available at:
- 14.Association of American Medical Colleges Table B-4: Total US medical school graduates by race/ethnicity and sex, 2013-2014 through 2017-2018. https://www.aamc.org/download/321536/data/factstableb4.pdf Available at:
- 15.Association of American Medical Colleges ERAS. Historical Specialty specific applicant data, radiation oncology 2014-2018. https://www.aamc.org/system/files/reports/1/radiationoncology.pdf Available at:
- 16.Deville C., Chapman C.H., Burgos R. Diversity by race, Hispanic ethnicity, and sex of the United States medical oncology physician workforce over the past quarter century. J Oncol Pract. 2014;10:e328–e334. doi: 10.1200/JOP.2014.001464. [DOI] [PubMed] [Google Scholar]
- 17.Association of American Medical Colleges Table 3: U.S. medical school faculty by rank and race/ethnicity. https://www.aamc.org/download/475546/data/16table3.pdf Available at:
- 18.Association of American Medical Colleges Faculty Roster. https://www.aamc.org/data/facultyroster/reports/ Available at:
- 19.Smart D. Physician characteristics and distribution in the US 2015. https://www.r2librarycom.ezp.welch.jhmi.edu/Resource/Title/1622021037 Available at:
- 20.Association of American Medical Colleges Altering the course: Black males in medicine. https://store.aamc.org/altering-the-course-black-males-in-medicine.html Available at:
- 21.Association of American Medical Colleges Diversity in medicine: Facts and figures 2019. https://www.aamc.org/data-reports/workforce/report/diversity-medicine-facts-and-figures-2019 Available at:
- 22.Ginther D.K., Haak L.L., Schaffer W.T., Kington R. Are race, ethnicity, and medical school affiliation associated with NIH R01 type 1 award probability for physician investigators? Acad Med. 2012;87:1516–1524. doi: 10.1097/ACM.0b013e31826d726b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moss-Racusin C.A., Dovidio J.F., Brescoll V.L., Graham M.J., Handelsman J. Science faculty’s subtle gender biases favor male students. Proc Natl Acad Sci U S A. 2012;109:16474–16479. doi: 10.1073/pnas.1211286109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Milkman K.L., Akinola M., Chugh D. What happens before? A field experiment exploring how pay and representation differentially shape bias on the pathway into organizations. J Appl Psychol. 2015;100:1678–1712. doi: 10.1037/apl0000022. [DOI] [PubMed] [Google Scholar]
- 25.Ross D.A., Boatright D., Nunez-Smith M., Jordan A., Chekroud A., Moore E.Z. Differences in words used to describe racial and gender groups in Medical Student Performance Evaluations. PloS One. 2017;12 doi: 10.1371/journal.pone.0181659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chapman C.H., Hwang W.T., Wang X., Deville C. Factors that predict for representation of women in physician graduate medical education. Med Educ Online. 2019;24 doi: 10.1080/10872981.2019.1624132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bailey Z.D., Krieger N., Agénor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389:1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- 28.Vapiwala N., Winkfield K.M. The hidden costs of medical education and the impact on oncology workforce diversity. JAMA Oncol. 2018;4:289–290. doi: 10.1001/jamaoncol.2017.4533. [DOI] [PubMed] [Google Scholar]
- 29.Asplund M., Welle C.G. Advancing science: How bias holds us back. Neuron. 2018;99:635–639. doi: 10.1016/j.neuron.2018.07.045. [DOI] [PubMed] [Google Scholar]
- 30.Association of American Medical Colleges Holistic review. https://www.aamc.org/services/member-capacity-building/holistic-review Available at:
- 31.Grbic D., Morrison E., Sondheimer H.M., Conrad S.S., Milem J.F. The association between a holistic review in admissions workshop and the diversity of accepted applicants and students matriculating to medical school. Acad Med. 2019;94:396–403. doi: 10.1097/ACM.0000000000002446. [DOI] [PubMed] [Google Scholar]
- 32.Ahmed A.A., Holliday E.B., Ileto J. Close to home: Employment outcomes for recent radiation oncology graduates. Int J Radiat Oncol Biol Phys. 2016;95:1017–1021. doi: 10.1016/j.ijrobp.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 33.Ziegelstein R.C., Crews D.C. The majority subsidy. Ann Intern Med. 2019;171:845–846. doi: 10.7326/M19-1923. [DOI] [PubMed] [Google Scholar]
- 34.Ahmed A.A., Hwang W.-T., Holliday E.B. Female representation in the academic oncology physician workforce: Radiation oncology losing ground to hematology oncology. Int J Radiat Oncol Biol Phys. 2017;98:31–33. doi: 10.1016/j.ijrobp.2017.01.240. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.