Abstract
In the coronavirus disease 2019 (COVID-19) era, the presence of acute respiratory failure is generally associated with acute respiratory distress syndrome; however, it is essential to consider other differential diagnoses that require different, and urgent, therapeutic approaches. Herein we describe a COVID-19 case complicated with bilateral spontaneous pneumothorax. A previously healthy 45-year-old man was admitted to our emergency department with sudden-onset chest pain and progressive shortness of breath 17 days after diagnosis with uncomplicated COVID-19 infection. He was tachypneic and presented severe hypoxemia (75% percutaneous oxygen saturation). Breath sounds were diminished bilaterally on auscultation. A chest X-ray revealed the presence of a large bilateral pneumothorax. A thoracic computed tomography (CT) scan confirmed the large bilateral pneumothorax, with findings consistent with severe COVID-19 infection. Chest tubes were inserted, with immediate clinical improvement. Follow-up chest CT scan revealed resolution of bilateral pneumothorax, reduction of parenchymal consolidation, and formation of large bilateral pneumatoceles. The patient remained under observation and was then discharged home. Bilateral spontaneous pneumothorax is a very rare, potentially life-threatening complication in patients with COVID-19. This case highlights the importance of recognizing this complication early to prevent potentially fatal consequences.
Keywords: Bilateral spontaneous pneumothorax, COVID-19, SARS-CoV-2, Spontaneous pneumothorax
1. Introduction
The outbreak of infections with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing coronavirus disease 2019 (COVID-19) began in Wuhan, the capital of Hubei Province, China, and then rapidly spread globally [1]. Although most patients with COVID-19 have a good prognosis, in some cases, the disease progresses rapidly, and patients develop acute respiratory distress syndrome (ARDS), the most severe form of acute lung injury seen in patients with COVID-19, leading to a very high mortality rate among those requiring mechanical ventilation [2]. Some evidence suggests that ARDS has been closely related to very high levels of proinflammatory cytokines, or a “cytokine storm” [3].
However, large bilateral spontaneous pneumothorax (BSP) in those infected with SARS-CoV-2 has not yet been widely reported in the literature [4]. Herein, we report a case of a patient with COVID-19 who developed simultaneous BSP.
2. Case report
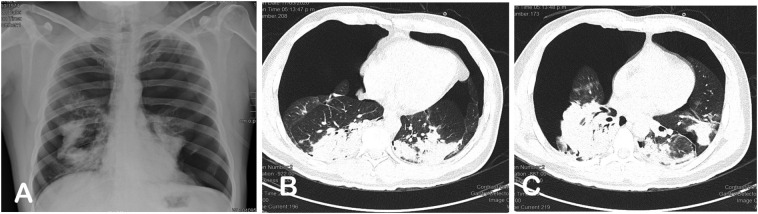
On May 17, 2020, a previously healthy 45-year-old male nonsmoker was admitted to the emergency department of our hospital with sudden-onset chest pain and progressive shortness of breath. Seventeen days prior, the patient had been diagnosed with uncomplicated COVID-19, with fever, sore throat, and headache; he had no respiratory distress, and his pulse oximetry was greater than 90%. The test for nasopharyngeal-swab SARS-CoV-2 nucleic acid detection by real-time Reverse Transcription-Polymerase Chain Reaction was positive. Consequently, treatment was initiated using ivermectin, azithromycin (for 5 days), and paracetamol. His condition remained stable but with fever. At admission, he denied cough or recent thorax trauma. Clinical examination revealed a heart rate of 100 beats/min, blood pressure 100/60 mmHg, respiration rate 26 breaths/min, and pulse oximetry 75% on ambient air. Breath sounds were diminished bilaterally on auscultation. The dramatic result of the initial chest x-ray was unexpected, as it showed a large bilateral pneumothorax and bilateral lung collapse (Fig. 1 -A). Under emergency conditions, a chest tube was placed in the left hemithorax with immediate clinical improvement; immediately thereafter, a thoracic computed tomography (CT) scan demonstrated ongoing pneumothorax and collapse of the right lung and partial resolution of the left pneumothorax with ill-defined patchy ground-glass opacities and lobar consolidations in the left lower lobe, findings consistent with severe COVID-19 infection (Fig. 1B,C). A right hemithorax chest tube was placed, and the patient was transferred to the COVID area of our Intensive Care Unit (ICU). Laboratory studies at that time were: hemoglobin 15.3 g/L; leukocytes 16,000/μL; lymphocytes 1900/μL; high-sensitivity C-reactive protein 7.17 mg/L (normal range, 1–3 mg/L); ferritin 438 ng/mL (normal range, 23–336 ng/mL); D-dimer 280 mg/mL (normal range, 0–224 mg/mL); troponin I 8.3 ng/mL (normal range, 0.10–0.16 ng/mL); NT-proBNP 104 pg/mL (normal range, 15–125 pg/mL); and IL-6 (4.58 pg/mL; normal range, 0.10–2.90 pg/mL).
Fig. 1.
(A) Chest X-rays at admission reveal bilateral pneumothorax with signs of tension and bilateral lung collapse. (B, C) Chest thoracic computed tomography scan, after chest tube placement in the left hemithorax, shows persistence of pneumothorax and collapse of the right lung and partial resolution of the left pneumothorax with patchy, ground-glass opacities and consolidations.
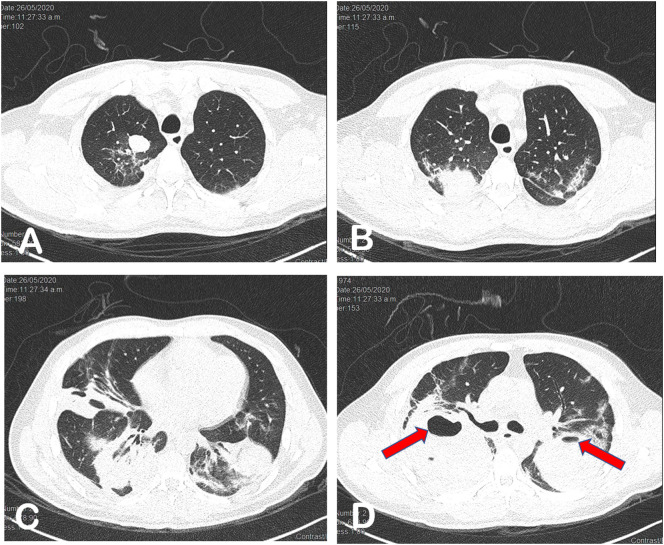
During ICU hospitalization, treatment included supplemental oxygen, lopinavir/ritonavir, and thromboprophylaxis with enoxaparin; during this time, he remained afebrile and did not require intubation or mechanical ventilation. Continuous suction was used, and complete expansion of the lungs was successful. The chest tubes were removed on the ninth day. Follow-up chest CT revealed resolution of the previous bilateral pneumothorax, reduction of parenchymal consolidation, and formation of large bilateral pneumatoceles (Fig. 2 ). The patient remained under observation over the next three days, while he showed significant clinical improvement, after which he was discharged home.
Fig. 2.
Follow-up chest thoracic computed tomography (CT) scan nine days later shows resolution of previous bilateral pneumothorax. (A, B, C) CT scan shows bilateral, patchy, ground-glass opacities and consolidations. (D) Chest CT scan disclosing large cavities in both lungs with fluid content, suggestive of pneumatoceles (red arrows). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3. Discussion
Herein, we report an unusual case of a previously healthy young individual in whom the initial manifestation of acute lung damage from COVID-19 was a simultaneous BSP. The association between COVID-19 and unilateral spontaneous pneumothorax has recently been reported [5,6]; however, the presence of large simultaneous BPS in a patient with COVID-19 has not been reported.
In the COVID-19 era, the presence of acute respiratory failure is generally associated with acute respiratory distress syndrome. However, the detection of different acute complications, such as pulmonary embolism [7] and pneumothorax [5,6], may require different and urgent therapeutic approaches.
In patients with SARS-CoV-2 infection, acute lung damage is the major contributor to morbidity and mortality. Yet to date, the incidence of spontaneous pneumothorax in these patients is unknown. Chest computed tomography studies have shown that pneumothorax is a rare finding, but its actual prognostic significance is unknown [8]. Nevertheless, the British Thoracic Society considers both spontaneous tension pneumothorax and SBP to be potentially life-threatening events that require urgent chest drain insertion [9]. Flower et al. [5] and Spiro et al. [10] reported that two patients with SARS-CoV-2 infection developed tension pneumothorax unassociated with mechanical ventilation that caused acute deterioration. In addition, our patient presented acute respiratory failure caused by the development of simultaneous bilateral spontaneous pneumothorax.
Opportune detection by clinical examination and confirmed with imaging techniques, in this uncommon complication in COVID-19 patients that show progressive worsening of respiratory function, may avoid use of treatments such as continuous positive airway pressure, which can have catastrophic consequences in these cases.
Many respiratory disorders have been described as causes of spontaneous pneumothorax. The most frequent underlying disorders are chronic obstructive pulmonary disease with emphysema, cystic fibrosis, blebs, tuberculosis, lung cancer, and HIV-associated pneumocystis carinii pneumonia; the presence of BSP is an indicator of advanced lung pathology with a poor prognosis [11]. Although the precise mechanism of spontaneous pneumothorax in COVID-19 is unknown, it may be linked to a variety of factors. The presence of pneumatoceles in patients with COVID-19 [5,12] is an uncommon pathological finding, which may contribute to the likelihood of developing pneumothorax, including distal airway inflammation [13].
It remains to be determined whether the presence of spontaneous pneumothorax in this population of patients with COVID-19 is associated with increased severity and worse prognosis.
This case highlights the importance of considering spontaneous pneumothorax in patients presenting with SARS-CoV-2 infection. We suggest that spontaneous pneumothorax should be considered in the diagnosis of these patients because immediate recognition and management of large tension pneumothorax is required to prevent potentially fatal consequences.
Declaration of Competing Interest
The authors declare that they have no competing interests.
References
- 1.Bogoch I.I., Watts A., Thomas-Bachli A., et al. Potential for global spread of a novel coronavirus from China. J Travel Med. 2020;27 doi: 10.1093/jtm/taaa011. taaa011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Richardson S., Hirsch J.S., Narasimhan M., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ye Q., Wang B., Mao J. The pathogenesis and treatment of the `cytokine Storm' in COVID-19. J. Inf. Secur. 2020;80:607–613. doi: 10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.López Vega J.M., Parra Gordo M.L., Diez Tascón A., Ossaba Vélez S. Pneumomediastinum and spontaneous pneumothorax as an extrapulmonary complication of COVID-19 disease. Emerg. Radiol. 2020:1–4. doi: 10.1007/s10140-020-01806-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flower L., Carter J.L., Rosales Lopez J., Henry A.M. Tension pneumothorax in a patient with COVID-19. BMJ Case Rep. 2020;13 doi: 10.1136/bcr-2020-235861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rohailla S., Ahmed N., Gough K. SARS-CoV-2 Infection Associated With Spontaneous Pneumothorax. CMAJ. 2020;192(E510) doi: 10.1503/cmaj.200609. cmaj.200609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bavaro D.F., Poliseno M., Scardapane A., et al. Occurrence of Acute Pulmonary Embolism in COVID-19 - A Case Series [published online ahead of print, 2020 Jun 22] Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.06.066. S1201–9712(20)30501–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salehi S., Abedi A., Balakrishnan S., Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am. J. Roentgenol. 2020;215:87–93. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 9.MacDuff A., Arnold A., Harvey J. BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010;65(Suppl. 2):ii18–ii31. doi: 10.1136/thx.2010.136986. [DOI] [PubMed] [Google Scholar]
- 10.Spiro J.E., Sisovic S., Ockert B., Böcker W., Siebenbürger G. Secondary tension pneumothorax in a COVID-19 pneumonia patient: a case report [published online ahead of print, 2020 Jun 18] Infection. 2020:1–4. doi: 10.1007/s15010-020-01457-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noppen M. Spontaneous pneumothorax: epidemiology. Pathophysiol. and Cause Eur Respir Rev. 2010;19:217–219. doi: 10.1183/09059180.00005310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu J., Pan J., Teng D., Xu X., Feng J., Chen Y.C. Interpretation of CT signs of 2019 novel coronavirus (COVID-19) pneumonia published online ahead of print. Eur. Radiol. 2020;2020 May 4:1–8. doi: 10.1007/s00330-020-06915-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schramel F.M., Meyer C.J., Postmus P.E. Inflammation as a cause of spontaneous pneumothorax and emphysema-like changes: results of bronchoalveolar lavage [abstract] Eur. Respir. J. 1995;8 397s. [Google Scholar]