Abstract
Background
Chronic respiratory diseases are risk factors for severe disease in coronavirus disease 2019 (COVID-19). Respiratory tract infection is one of the commonest causes of acute exacerbation of chronic obstructive pulmonary disease (AECOPD). There has not been evidence suggesting the link between COVID-19 and AECOPD, especially in places with dramatic responses in infection control with universal masking and aggressive social distancing.
Methods
This is a retrospective study to assess the number of admissions of AECOPD in the first three months of 2020 in Queen Mary Hospital with reference to the admissions in past five years. Log-linear model was used for statistical inference of covariates, including percentage of masking, air quality health index and air temperature.
Results
The number of admissions for AECOPD significantly decreased by 44.0% (95% CI 36.4%–52.8%, p < 0.001) in the first three months of 2020 compared with the monthly average admission in 2015–2019. Compare to same period of previous years, AECOPD decreased by 1.0% with each percent of increased masking (p < 0.001) and decreased by 3.0% with increase in 1 °C in temperature (p = 0.045). The numbers of admissions for control diagnoses (heart failure, intestinal obstruction and iron deficiency anaemia) in the same period in 2020 were not reduced.
Conclusions
The number of admissions for AECOPD decreased in first three months of 2020, compared with previous years. This was observed with increased masking percentage and social distancing in Hong Kong. We postulated universal masking and social distancing during COVID-19 pandemics both contributed in preventing respiratory tract infections hence AECOPD.
Keywords: Chronic obstructive pulmonary disease, Coronavirus disease 2019, Hospitalization
1. Introduction
In late 2019, coronavirus disease 2019 (COVID-19) due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections started off in Wuhan, China. The infection rapidly evolved and spread to most countries around the world, leading to a pandemic. As of 12 June 2020, more than 7.4 million people were infected, causing more than 418,000 deaths globally. Clinical presentation of COVID-19 ranges from asymptomatic to fatal pneumonia. Underlying chronic respiratory diseases was identified as one of the risk factors for severe COVID-19 disease [[1], [2], [3]].
Chronic obstructive pulmonary disease (COPD) is one of the commonest chronic respiratory diseases in the world and in Hong Kong. Acute exacerbation of COPD (AECOPD) requiring hospitalizations is associated with accelerated decline in lung function, worsened quality of life, increased risk of future exacerbations and increased mortality. It is the fourth leading cause of death in the world but is projected to be the third leading cause of death by 2020 [[4], [5], [6], [7], [8], [9]].
Respiratory tract infection is one of the commonest triggers of AECOPD in which influenza is associated with considerable mortality and morbidity [[10], [11], [12], [13], [14]]. Both exposure to certain air pollutants and low temperature are also shown to confer increased risk of AECOPD [15].
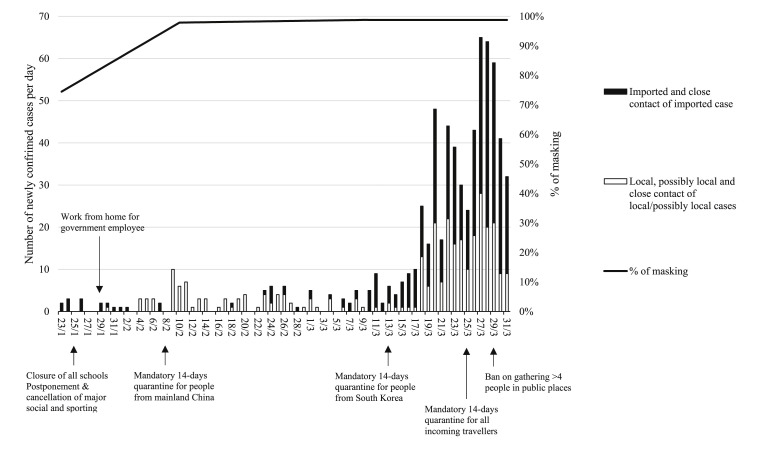
There is yet no evidence suggests the link between COVID-19 and AECOPD requiring hospitalization. As a respiratory tract pathogen, SARS-CoV-2 infections can potentially cause more AECOPD. Hong Kong society had dramatic responses in infection control and voluntarily adopted universal masking and aggressive social distancing since the first confirmed case of COVID-19 on 23th January 2020. The percentage of wearing masks by the public was 74.5% on 20th to 23rd January 2020, 97.5% on 11th to 14th February and 98.8% on 10th to 13rd March 2020 (n = 10,319, Fig. 1 ). It was obtained from a survey from the Hong Kong Public Opinion Research Institute (HKPORI), which carried three-cross sectional telephone survey among general adult population in Hong Kong, with self-reporting of wearing a face mask when going out. Telephone numbers were randomly generated by computer system. Masking was not specifically defined but was generally understood by the public as surgical masks, while some may use re-useable mask [16,17]. Social distancing was widely practised by Hong Kong citizens, with some government policy since 25th January 2020 including closure of all schools, work from home policy for most government employees, closure of recreational business and bars, and ban on gathering of more than four people in public places ([18], Fig. 1). As such, for a city in close proximity to China, Hong Kong has a relatively low case load of COVID-19. Whether universal masking can provide additional benefits on AECOPD, is the focus of our current study.
Fig. 1.
of masking and daily number of newly confirmed COVID-19 cases in January to March 2020.
2. Materials and methods
This was a retrospective study to assess number of admissions for AECOPD during the period of COVID-19 in Queen Mary Hospital (QMH) with reference to the admission number in the past 5 years. QMH is a tertiary hospital provides acute care under Hospital Authority, a public organization accountable for 90% of in-patient services in Hong Kong [19]. The study period was January to March 2020, when World Health Organization (WHO) confirmed the novel coronavirus, later called COVID-19 infection on 9 January 2020, with the first imported case from Wuhan to Hong Kong on 23 January 2020. Patients above 45 years old with known COPD admitted for AECOPD from the period 1st January 2015 to 31st March 2020 were included in the study. Data was obtained by retrieval of admission records from the Clinical Data Analysis and Reporting System (CDARS) of Hospital Authority. Principal diagnoses with ICD-9 codes of 469 and 491 were searched on CDARS. Inclusion criteria include 1) age above 45-year-old 2) with known diagnosis of COPD 3) and with AECOPD. Exclusion criteria include 1) Age of 45-year-old or below 2) with COPD admitted for causes of dyspnea other than AECOPD 3) with coexisting pulmonary diseases including asthma-COPD overlap syndrome and bronchiectasis, which are being identified as the secondary diagnoses in CDARS. Demographic data (including age, gender), clinical data/investigations (including date of admission, length of hospital stay, blood and sputum culture results, use of non-invasive ventilation and invasive mechanical ventilation) were collected. Length of stay (LOS) and mortality were used as markers of severity of AECOPD admission, with longer length of stay and higher mortality indicated more severe condition of patients. Data on other acute admissions within the same period including heart failure (ICD-9 code 428), intestinal obstruction (ICD-9 code 560) and iron deficiency anaemia (ICD-9 code 280) were taken as control diagnoses. These control diagnoses were taken as reference of health-seeking behavior during period of COVID-19 with evaluating possibility of decreased hospital attendance due to various reasons including fear of being infected by COVID-19 or not to overload hospital care.
Percentage of masking [16], air quality, as measured by Air Quality Health Index (AQHI), temperature and incidence of influenza A and B in the period from January 2015 to March 2020 in Hong Kong were also collected and their associations with COPD exacerbation were studied with highlights on the COVID-19 period. Relationship between percentage of mask usage and AECOPD was calculated with assumption of 1% on the period prior COVID-19, in accounting for the pregnant lady and immunocompromised patients who were advised to wear masks. AQHI was calculated by the Hong Kong Environmental Protection Department (HKEPD), based on the cumulative health risk attributable to a 3-hour moving average concentrations of four air pollutants, namely ozone (O3), nitrogen dioxide (NO2), sulphur dioxide (SO2) and particulate matter (PM2.5/PM10). The AQHI system provided different health advice for people having different degree of susceptibility to air pollution, including people with existing heart or respiratory illnesses, children and the elderly, outdoor workers and the general public. It was reported in scale of 1–10 and 10+ and grouped into five health risk categories, namely low [1–3], moderate [4–6], high [7], very high [8–10] and serious [10+] with different precautionary actions were advised. People with respiratory illness were advised to reduced outdoor physical exertion and to minimize their stay in outdoor when AQHI was high, very high or serious. The AQHI was reported hourly in 13 stations located in different area of Hong Kong [20]. The total number of hours with AQHI recorded as high, very high or serious were summed up and expressed as percentage of total number of hours collected in a month. Log-linear model was used for statistical analysis of the possible association between AQHI and AECOPD. Mean ambient temperature in Degree Celsius of each month was collected from the Hong Kong Observatory [21]. Influenza incidence was collated from territory-wide laboratory surveillance data for both in-patients and out-patients in both public and private medical sectors from the Centre for Health Protection, HKSAR, with relative static number of specimens collected over the period [22].
For statistical inference about the association between covariates (air temperature, AQHI and mask usage) and admission count, log-linear modeling was used in this study. It was also applied for statistical inference for admission count between the three different time periods, namely first three months of 2020, first three months of 2015–2019 and all months in 2015–2019. To balance the model fitness and complexity, Akaike information criterion (AIC) was used for model selection. Both traditional asymptotic test statistics and bootstrapping were considered. The later approach was a re-sampling method for statistical inference with less restrictive assumptions, which can help to handle relatively small sample size. It was designed to recover the distribution of model parameters and provided alternative estimates of key quantities such as confidence intervals and p-value based on some randomly shuffling the labels under the null hypothesis [23,24]. Bootstrap sample size was set as 9999 to achieve adequate precision for significance. Two-sided tests were conducted for general differences and p < 0.05 was taken as significant differences. Fisher exact test was used to compare the mortality rate and percentage of LOS of more than 5 days between the two time periods. Number of admission of the two time periods were classified into two categories (for mortality: death/alive or whether LOS exceeding 5 days) and hence formed a 2-by-2 contingency table. Further details of these biostatistical methods are listed in Appendix 1. The study was approved by the local Institutional Review Board for ethical and scientific review.
3. Results
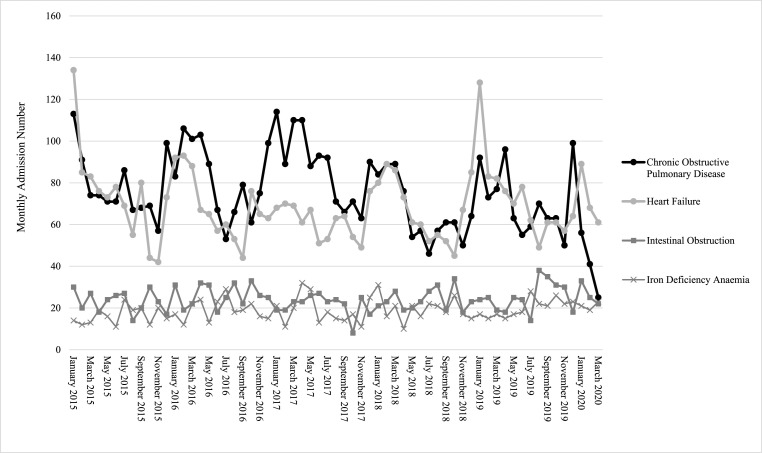
From January 2015 to March 2020, total of 4749 admissions for AECOPD were recorded, of which 4627 admissions were from the period of 2015–2019 and 122 admissions in first three months of 2020 (Fig. 2 ). In the five-year period of 2015–2019 as a whole, the monthly average number of admissions was 77 (ranged from 66 to 89 in each year). We observed that the admission for AECOPD was highest in the first three months every year. By averaging the total number of admissions in the first three months in each year of 2015–2019, the monthly admission count was 92 (ranged from 81 to 105 in each year). The average monthly AECOPD admission was 41 in the first three months of 2020 (Table 1 ). Based on log-linear modeling, the estimated drop in admission counts in the first three months of 2020 was 44.0% (95% CI 36.4%–52.8%, p < 0.001). No patient in our included study population was COVID-19 positive.
Fig. 2.
Admission number of different diagnoses over time.
Table 1.
Admissions for AECOPD and control diagnoses, influenza detection and AECOPD severity indicators for different periods.
| Only Jan to Mar, 2020 (A) | Only Jan to Mar, 2015–2019 (B) | All months, 2015–2019 (C) | P value (A vs B)a | P value (A vs C)a | P value (Masking) | P value (Temp) | P value (AQHI) | |
|---|---|---|---|---|---|---|---|---|
| Admissions, monthly average no. | ||||||||
| AECOPD | 41 | 92 | 77 | <0.005 | <0.005 | <0.001 | 0.045 | 0.315 |
| Heart failure | 73 | 89 | 69 | 0.086 | 0.448 | 0.217 | 0.173 | 0.250 |
| Intestinal obstruction | 27 | 23 | 24 | 0.192 | 0.347 | 0.398 | 0.933 | 0.877 |
| Iron deficiency anaemia | 21 | 17 | 19 | 0.062 | 0.385 | 0.186 | 0.775 | 0.797 |
| Influenza A or B detection, monthly average no. | ||||||||
| No. of viruses | 1888 | 3958 | 1966 | <0.005 | <0.005 | – | – | – |
| AECOPD severity indicators | ||||||||
| LOS >5 days, % (No/total) | 6.6 (8/122) | 9.2 (128/1385) | 8.6 (396/4627) | 0.410 | 0.513 | – | – | – |
| Mortality, % (No deaths/total) | 3.3 (4/122) | 2.3 (32/1385) | 2.5 (117/4627) | 0.528 | 0.553 | – | – | – |
AECOPD, acute exacerbation of chronic obstructive pulmonary disease; AQHI = Air Quality Health Index; LOS = length of stay; Temp = Temperature; - not applicable.
Log-linear modeling or Fisher exact tests.
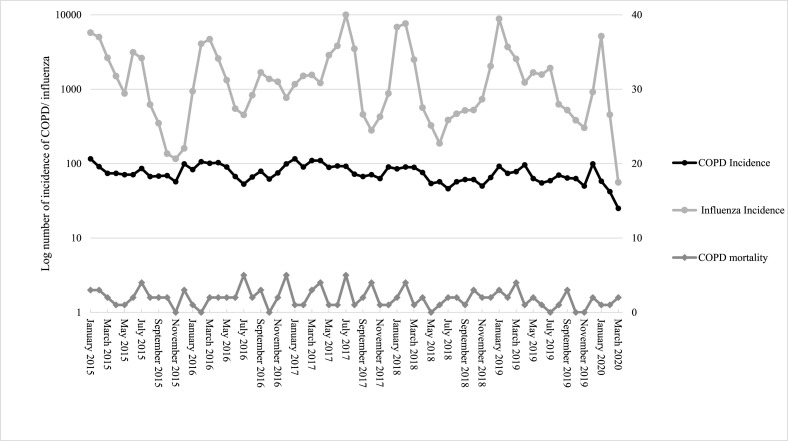
Further statistical analyze on the severity of admission and effects of different factors on AECOPD was performed with focus on the first three months in 2015–2019 and 2020 as more complete masking was observed in first three months of 2020. LOS and mortality were used as indicators of severity in admission. In first three months of 2015–2019, total number of patients with LOS of more than 5 days was 128 out of 1385 patients, while that in the first three months of 2020 was 8 out of 122 patients. Mortality in first three months of 2015–2019 was 32 and 4 in first three months of 2020 (Fig. 3). Comparing the proportion of LOS and mortality between the two periods by Fisher exact test, both LOS more than 5 days (p = 0.410) and mortality (p = 0.528) were statistically insignificant between the two periods (Table 1).
Fig. 3.
Incidence of influenza A and B in Hong Kong, COPD admission and mortality.
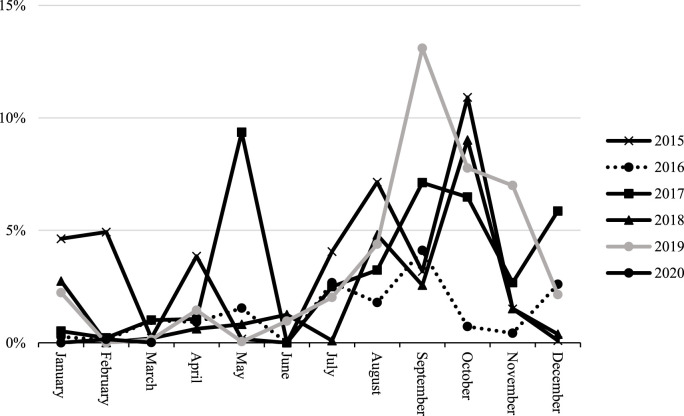
For the effect of wearing facemasks, the expected admission count would reduce by 1.0% with each percent of increase in masking (p < 0.001). Average monthly admission in the first three months of 2015–2019 was 92. Increase in masking from 1% to 98.8% would decrease admission number by 59.2% to 38 admissions per month, given temperature remained constant. Increase in 1 °C in temperature would reduce AECOPD by 3.0% (p = 0.045). The percentage of AQHI with high to serious levels ranged from 0 to 13% in the period and ranged from 0 to 4.9% in first three months with worse AQHI observed in October and November (Fig. 4). Increase in one percent of AQHI with high to severe would increase admission count by 1.6% but was statistically insignificant (p = 0.315).
Fig. 4.
Percentage of AQHI high to serious over months in 2015–2020.
Total number of patients with influenza A or B viruses detected from January 2015 to March 2020 in Hong Kong was 123,650. In the period of 2015–2019 as a whole, the monthly average was 1966. The number of influenza virus was peaked in the first three months of the year in 2015–2019, except in 2017, with monthly average 3958. In the first months of 2020, the monthly average dropped to 1888 and was correlated with the drop in AECOPD (Table 1 & Fig. 3 ).
The average monthly admission number for heart failure is 69 from 2015 to 2019. We observed a large decrease in admission between January and February 2015 and 2019 (Fig. 2). The average monthly admission number for heart failure was 73 in the first quarter of 2020. The effect of masking (p = 0.217), AQHI (p = 0.173) and temperature (p = 0.250) were statistically insignificant. The difference in admission number between periods was statistically insignificant (Table 1).
The average monthly admission for intestinal obstruction and iron deficiency anaemia were static over the period 2015 to 2020. Average number of admissions was 24 per month for intestinal obstruction and 19 per month for iron deficiency anaemia (Fig. 2). In the first three months of 2020, the average number of admissions for intestinal obstruction was 27 and for iron deficiency anaemia was 21. The effect of wearing facemasks, AQHI and temperature were statistically insignificant. The difference in admission number between periods was statistically insignificant (Table 1).
4. Discussion
Our study is the first to show the change in hospitalization number of AECOPD during COVID-19 pandemic and its relationship with percentage of masking, temperature and air quality. Compared with other conditions that require hospitalization for management, including heart failure, intestinal obstruction and iron deficiency anaemia, AECOPD admission number in the first three months of 2020 was significantly lower when compared to the same periods in previous years. The drastic drop in admission number cannot be fully explained by change in health-seeking behaviors in fear of attending hospitals as shown by admission of control diagnoses were not decreased. The COPD mortality and LOS more than 5 days were similar in the same period which suggested the severity of AECOPD could be the same. Universal masking and higher temperature were shown to associate with decrease in AECOPD. The possible explanation could be universal masking and social distancing could effectively prevent respiratory tract infections and hence AECOPD. This was further supported by the drastic concomitant drop in number of influenza in Hong Kong in the same period. The number of admissions of the conditions including heart failure, intestinal obstruction and iron deficiency anaemia, which are unaffected by universal masking was static. These results suggested that the decrease in AECOPD admission in the first quarter of 2020 was attributable to the effect from universal masking and social distancing, which was vigorously practiced in Hong Kong in time of COVID-19 pandemic.
Worsening of air pollution with higher percentage of AQHI with high to serious was associated with more AECOPD admission but was statistically insignificant in our study. However, air pollution is known to be associated with increase in AECOPD and this should be acknowledged. The statistical insignificance can be accountable by the relatively small variation of percentage with high to serious AQHI in the period (ranges from 0 to 4.9% in the first quarter of years).
AECOPD is one of the most important complications of COPD which could lead to adverse outcomes. Prevention of recurrent AECOPD is the main goal of respiratory physicians. Both non-pharmacological and pharmacological therapies, including standard treatment based on GOLD guideline and influenza and pneumococcal vaccine have been advocated but the number of hospitalizations for AECOPD remained static over the past five years [[25], [26], [27], [28], [29]]. The decrease in hospitalization number for AECOPD in the first three months of 2020 coincided with the well-observed phenomenon of universal masking and social distancing in Hong Kong, together with low case load and local transmission rate of COVID-19 and low incidence of influenza. Apart from reducing COVID-19 case numbers, these measures were likely to bring about additional benefit for non-SARS-CoV-2 infected patients, especially COPD patients by protecting them against respiratory tract infection via air-borne or droplet transmission. Our study results suggested a possible link between universal masking and social distancing with decrease in AECOPD admission.
Masking and social distancing could also contribute to the decrease in number of influenza from January to March 2020. The number of influenza in January 2020 was close to previous years with 5154 cases, with a drastic drop in February and March 2020, with commencement of universal masking and social distancing in end of January. The magnitude of drop in influenza case number was not observed following an increase in influenza vaccination number from 579,000 in year 2015/2016 to 1,372,300 in 2019/2020, hence cannot be completely accountable by seasonal influenza vaccination [30].
Apart from the drop in AECOPD in January to March 2020, we also observed there was a large decrease in admission for heart failure between January and February 2015 and 2019. Yet there is no obvious reason accountable for the decrease in admission for heart failure in the period. This phenomenon should be acknowledged that the drop on admission may or may not due to obvious external cause.
Our observational study in Hong Kong suggested the benefits of masking and social distancing can potentially extend beyond prevention of COVID-19, including early termination of influenza season and drop in the number of hospitalizations due to AECOPD in the first quarter of 2020.
5. Limitations
The potential limitation of this study was that it only involved a single centre, QMH. The centre served an area in Hong Kong with relatively stable population size with no major service change in the past five years [31]. Using districts with relatively stable population size and with only one acute hospital with Accident and Emergency Department would remove the bias from population size change and also that from loss of patients due to admission to another centre within the same district. This can also use as a reference for projection of the condition of healthcare system in Hong Kong.
Moreover, our study only included patients with AECOPD admitted to a regional tertiary hospital. Some patients with mild attack might visit outpatient clinics hence not all patients with AECOPD were included. However, patients with severe attack who attended outpatient clinics are generally referred to Emergency Department and admitted, hence they were included in our study. Our study focused on patient population with more severe symptoms who required hospital admission after triage by Emergency Department. The severity of exacerbation was comparable with other period as shown by the length of stay and mortality data.
Our study showed the observational effect of decrease in AECOPD with universal masking and social distancing which are both widely practiced in Hong Kong in COVID-19 period. Both factors occurred together and the possible effect of each component on decrease in AECOPD admission cannot be differentiated in our observational study.
6. Conclusion
The number of admissions for AECOPD decreased in the first three months of 2020, compared with the number in 2015–2019 in Hong Kong. This was observed with the widely practice of universal masking and social distancing. We postulated that universal masking and social distancing could prevented respiratory tract infections which were one of the triggers of AECOPD, hence was associated with decrease in AECOPD during the COVID-19 pandemic.
CRediT authorship contribution statement
King Pui Florence Chan: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Writing - original draft, Visualization. Ting Fung Ma: Conceptualization, Data curation, Formal analysis, Methodology. Wang Chun Kwok: Conceptualization, Formal analysis, Resources, Writing - original draft, Supervision. Jackson Ka Chun Leung: Data curation, Investigation. Ka Yan Chiang: Data curation, Investigation. James Chung Man Ho: Formal analysis, Supervision, Validation. David Chi Leung Lam: Supervision, Validation, Writing - review & editing. Terence Chi Chun Tam: Supervision, Validation, Writing - review & editing. Mary Sau Man Ip: Formal analysis, Resources, Supervision, Validation. Pak Leung Ho: Conceptualization, Formal analysis, Writing - review & editing, Supervision, Validation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmed.2020.106085.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. J. Am. Med. Assoc. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Liang W., Guan W., Chen R., Wang W., Li J., Xu K., et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seemungal T.A., Donaldson G.C., Paul E.A., Bestall J.C., Jeffries D.J., Wedzicha J.A. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 1998;157(5 Pt 1):1418–1422. doi: 10.1164/ajrccm.157.5.9709032. [DOI] [PubMed] [Google Scholar]
- 5.Suissa S., Dell'Aniello S., Ernst P. Long-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortality. Thorax. 2012;67(11):957–963. doi: 10.1136/thoraxjnl-2011-201518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donaldson G.C., Wedzicha J.A. COPD exacerbations .1: Epidemiology. Thorax. 2006;61(2):164–168. doi: 10.1136/thx.2005.041806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Slenter R.H., Sprooten R.T., Kotz D., Wesseling G., Wouters E.F., Rohde G.G. Predictors of 1-year mortality at hospital admission for acute exacerbations of chronic obstructive pulmonary disease. Respiration. 2013;85(1):15–26. doi: 10.1159/000342036. [DOI] [PubMed] [Google Scholar]
- 8.Global initiative for chronic obstructive lung disease GOLD guideline.
- 9.Ko F.W., Chan K.P., Hui D.S., Goddard J.R., Shaw J.G., Reid D.W., et al. Acute exacerbation of COPD. Respirology. 2016;21(7):1152–1165. doi: 10.1111/resp.12780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rohde G., Wiethege A., Borg I., Kauth M., Bauer T.T., Gillissen A., et al. Respiratory viruses in exacerbations of chronic obstructive pulmonary disease requiring hospitalisation: a case-control study. Thorax. 2003;58(1):37–42. doi: 10.1136/thorax.58.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tan W.C., Xiang X., Qiu D., Ng T.P., Lam S.F., Hegele R.G. Epidemiology of respiratory viruses in patients hospitalized with near-fatal asthma, acute exacerbations of asthma, or chronic obstructive pulmonary disease. Am. J. Med. 2003;115(4):272–277. doi: 10.1016/s0002-9343(03)00353-x. [DOI] [PubMed] [Google Scholar]
- 12.Greenberg S.B., Allen M., Wilson J., Atmar R.L. Respiratory viral infections in adults with and without chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2000;162(1):167–173. doi: 10.1164/ajrccm.162.1.9911019. [DOI] [PubMed] [Google Scholar]
- 13.Papi A., Bellettato C.M., Braccioni F., Romagnoli M., Casolari P., Caramori G., et al. Infections and airway inflammation in chronic obstructive pulmonary disease severe exacerbations. Am. J. Respir. Crit. Care Med. 2006;173(10):1114–1121. doi: 10.1164/rccm.200506-859OC. [DOI] [PubMed] [Google Scholar]
- 14.Falsey A.R., Hennessey P.A., Formica M.A., Cox C., Walsh E.E. Respiratory syncytial virus infection in elderly and high-risk adults. N. Engl. J. Med. 2005;352(17):1749–1759. doi: 10.1056/NEJMoa043951. [DOI] [PubMed] [Google Scholar]
- 15.Raji H., Riahi A., Borsi S.H., Masoumi K., Khanjani N., AhmadiAngali K., Goudarzi G. Dastoorpoor MAcute effects of air pollution on hospital admissions for asthma, COPD, and bronchiectasis in ahvaz, Iran. nt J Chron Obstruct Pulmon Dis. 2020 Mar 3;15:501–514. doi: 10.2147/COPD.S231317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Community health module Research reports, Hong Kong public opinion Research Institute. https://www.pori.hk/research-reports
- 17.Cowling B.J., Ali S.T., Ng T.W.Y., Tsang T.K., Li J.C.M., Fong M.W., et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5(5):e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan K.H., Lee P.W., Chan C.Y., Lam K.B.H., Ho P.L. Monitoring respiratory infections in covid-19 epidemics. BMJ. 2020;369:m1628. doi: 10.1136/bmj.m1628. [DOI] [PubMed] [Google Scholar]
- 19.Hospital authority statistical report. https://www3.ha.org.hk/data/HAStatistics/DownloadReport/2
- 20.Air quality health index monthly summary. https://www.aqhi.gov.hk/en/aqhi/statistics-of-aqhi/aqhi-monthly-summary.html
- 21.Kong Hong. Observatory. https://www.hko.gov.hk/en/wxinfo/pastwx/mws/mws.htm
- 22.Centre of Health Protection https://www.chp.gov.hk/en/resources/29/304.html
- 23.A. C. Davison Dvh. Bootstrap Methods and Their Application. Cambridge University Press.
- 24.Boos D.D. Introduction to the bootstrap world. Stat. Sci. 2003;18(2):168–174. [Google Scholar]
- 25.Au D.H., Bryson C.L., Chien J.W., Sun H., Udris E.M., Evans L.E., et al. The effects of smoking cessation on the risk of chronic obstructive pulmonary disease exacerbations. J. Gen. Intern. Med. 2009;24(4):457–463. doi: 10.1007/s11606-009-0907-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Criner G.J., Bourbeau J., Diekemper R.L., Ouellette D.R., Goodridge D., Hernandez P., et al. Prevention of acute exacerbations of COPD: American college of chest physicians and Canadian thoracic society guideline. Chest. 2015;147(4):894–942. doi: 10.1378/chest.14-1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Calverley P.M., Rabe K.F., Goehring U.M., Kristiansen S., Fabbri L.M., Martinez F.J., et al. Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trials. Lancet. 2009;374(9691):685–694. doi: 10.1016/S0140-6736(09)61255-1. [DOI] [PubMed] [Google Scholar]
- 28.Casaburi R., Mahler D.A., Jones P.W., Wanner A., San P.G., ZuWallack R.L., et al. A long-term evaluation of once-daily inhaled tiotropium in chronic obstructive pulmonary disease. Eur. Respir. J. 2002;19(2):217–224. doi: 10.1183/09031936.02.00269802. [DOI] [PubMed] [Google Scholar]
- 29.Ferguson G.T., Anzueto A., Fei R., Emmett A., Knobil K., Kalberg C. Effect of fluticasone propionate/salmeterol (250/50 microg) or salmeterol (50 microg) on COPD exacerbations. Respir. Med. 2008;102(8):1099–1108. doi: 10.1016/j.rmed.2008.04.019. [DOI] [PubMed] [Google Scholar]
- 30.Sun K.S., Lam T.P., Kwok K.W., Lam K.F., Wu D., Ho P.L. Seasonal influenza vaccine uptake among Chinese in Hong Kong: barriers, enablers and vaccination rates. Hum. Vaccines Immunother. 2020:1–10. doi: 10.1080/21645515.2019.1709351. 2020 Jan 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Census and statistics department. https://www.censtatd.gov.hk/home/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.