Abstract
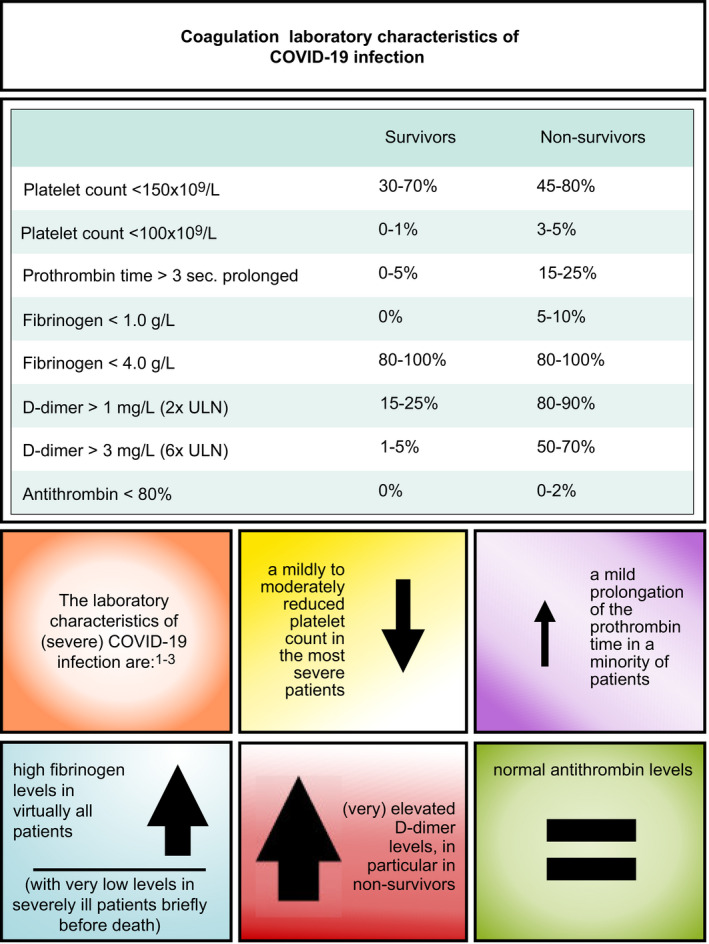
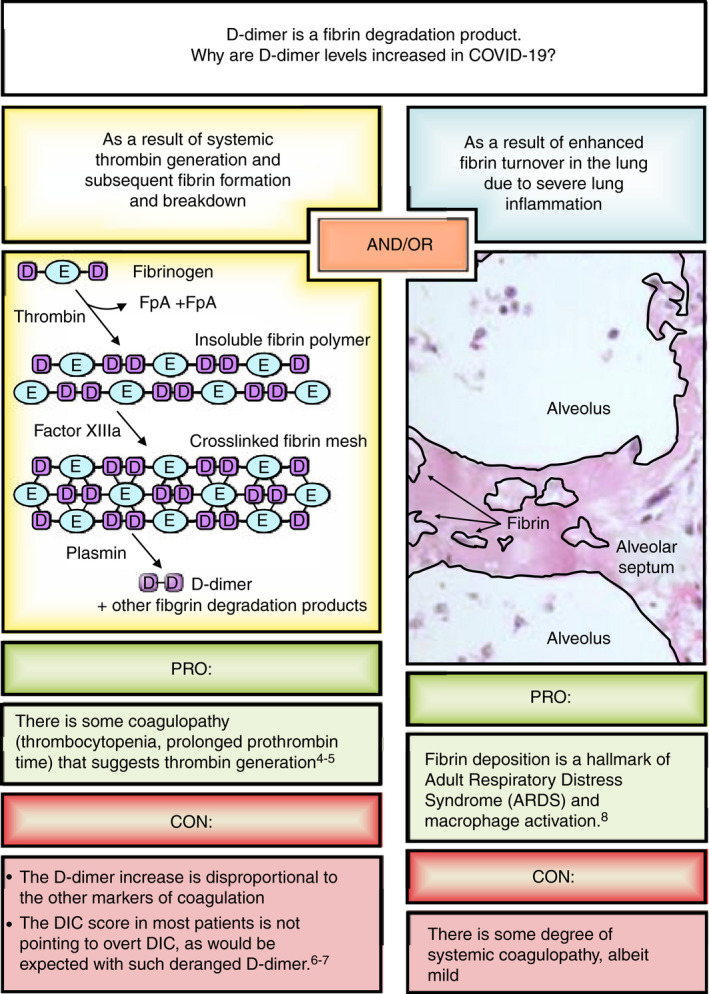
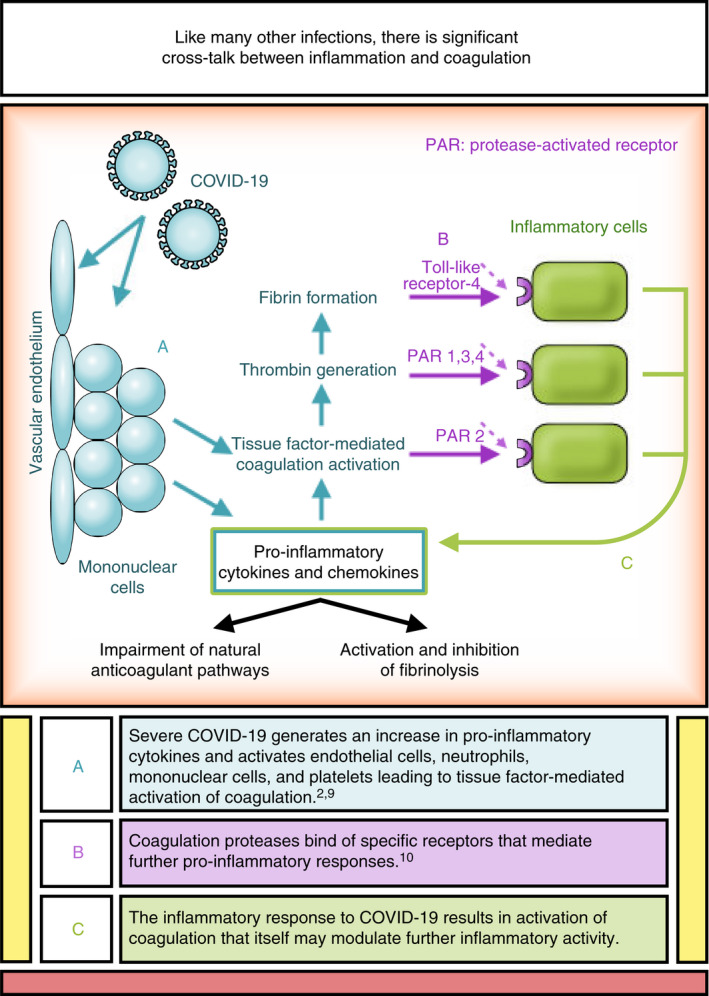
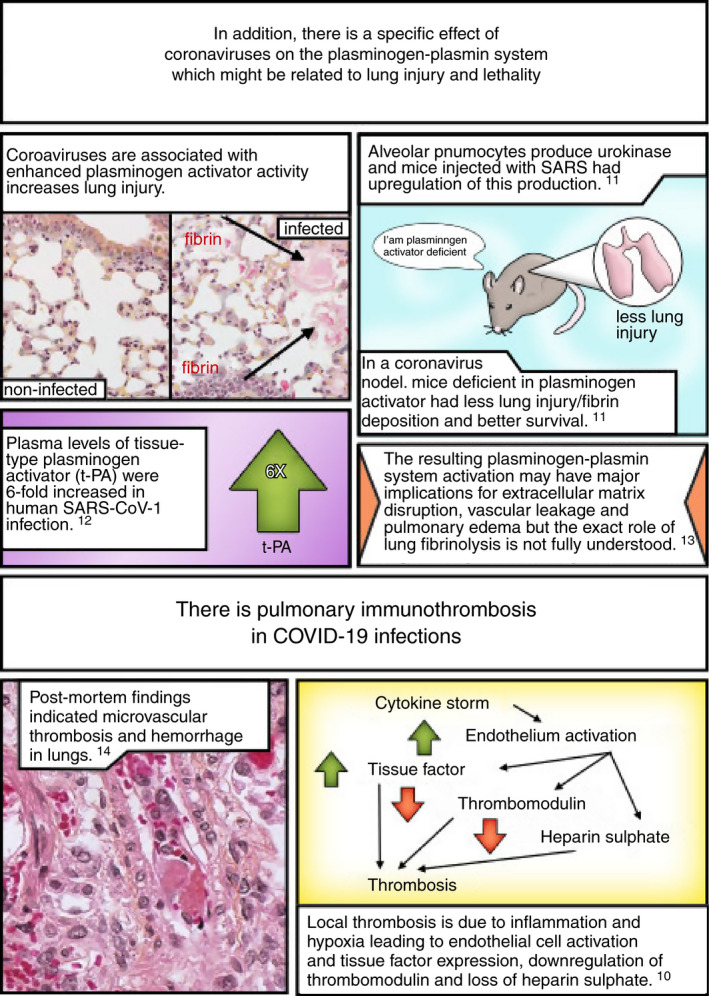
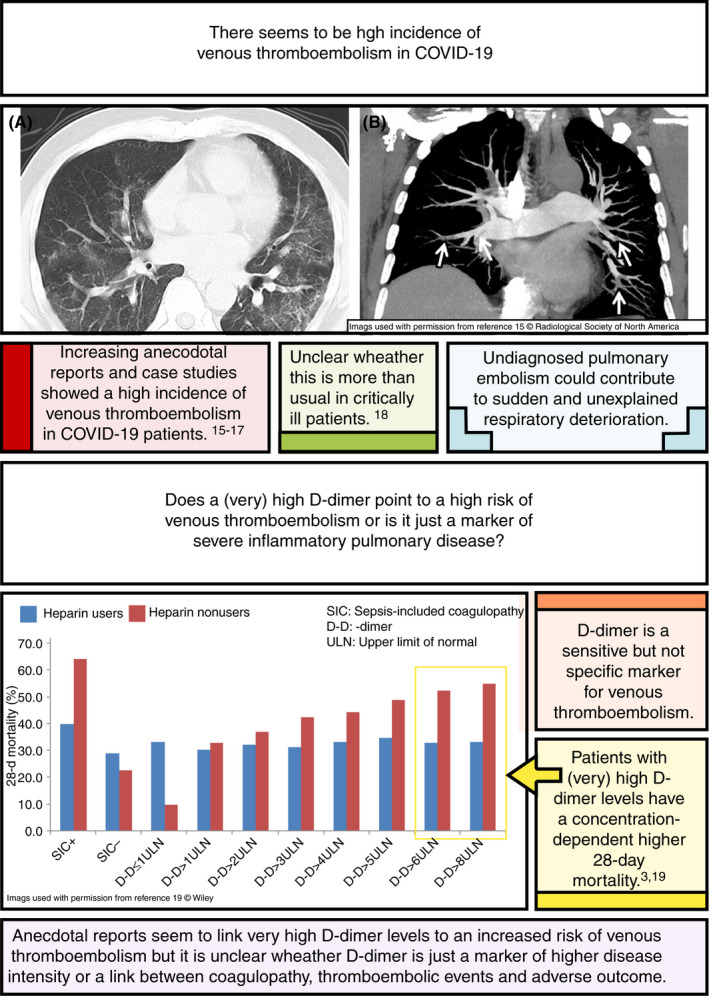
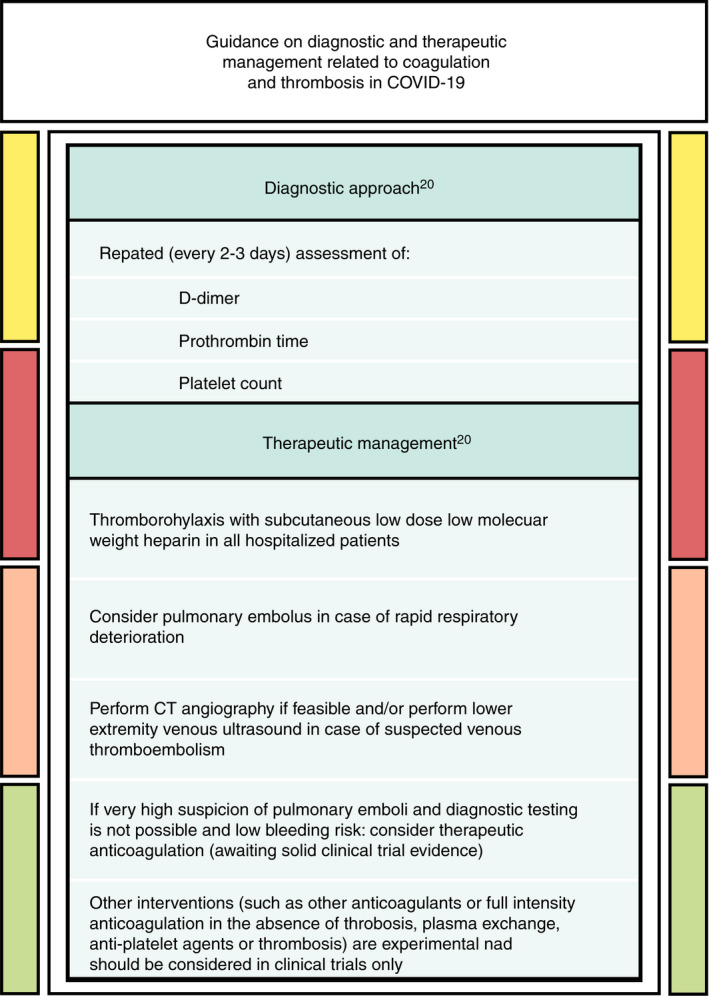
This illustrated review discusses the haemostatic changes seen in patients with severe coronavirus disease 2019 (COVID‐19) infection and their possible causes. We discuss the crosstalk between inflammation and coagulation resulting in high levels of acute‐phase proteins, very high levels of D‐dimers, and absence of disseminated intravascular coagulation seen in patients with severe COVID‐19. There appear to be high rates of venous thromboembolism and also, what has been poorly described before in acute lung injury, a high rate of pulmonary immunothrombosis (thrombosis secondary to inflammation).
Keywords: COVID‐19, novel coronavirus, thrombosis, coagulopathy, coagulation
Essentials.
There are marked increases in coagulation proteins in patients with severe coronavirus disease 2019 (COVID‐19) infection, consistent with a profound acute‐phase response.
D‐dimer levels are extremely high and reflect activation of fibrinolysis systemically and also in the lungs.
Disseminated intravascular coagulation is rarely seen in severe COVID‐19 infection outside of preterminal multiorgan failure.
Thrombosis rates appear high due to venous thromboembolism and pulmonary immunothrombosis.
Levi M, Hunt BJ. Thrombosis and coagulopathy in COVID‐19: An illustrated review. Res Pract Thromb Haemost. 2020;4:744–751. 10.1002/rth2.12400
Handling Editor: Dr Alisa Wolberg
Contributor Information
Marcel Levi, Email: marcel.levi@nhs.net, @MarcelLevi.
Beverley J. Hunt, @bhwords.
References
- 1. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Levi M, ten Cate H. Disseminated intravascular coagulation. N Engl J Med. 1999;341:586–92. [DOI] [PubMed] [Google Scholar]
- 5. Gando S, Levi M, Toh CH. Disseminated intravascular coagulation. Nat Rev Dis. 2016;2:16037. [DOI] [PubMed] [Google Scholar]
- 6. Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001;86:1327–30. [PubMed] [Google Scholar]
- 7. Suzuki K, Wada H, Imai H, Iba T, Thachil J, Toh CH. A re‐evaluation of the D‐dimer cut‐off value for making a diagnosis according to the ISTH overt‐DIC diagnostic criteria: communication from the SSC of the ISTH. J Thromb Haemost. 2018;16(7):1442–4. [DOI] [PubMed] [Google Scholar]
- 8. Bellingan GJ. The pulmonary physician in critical care: The pathogenesis of ALI/ARDS. Thorax. 2002;57:540–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID‐19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Levi M, van der Poll T, Buller HR. Bidirectional relation between inflammation and coagulation. Circulation. 2004;109:2698–704. [DOI] [PubMed] [Google Scholar]
- 11. Gralinski LE, Bankhead A, Jeng S, et al. Mechanisms of severe acute respiratory syndrome coronavirus‐induced acute lung injury. MBio. 2013;4:e00271‐e313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Liu ZH, Wei R, Wu YP, et al. Elevated plasma tissue‐type plasminogen activator (t‐PA) and soluble thrombomodulin in patients suffering from severe acute respiratory syndrome (SARS) as a possible index for prognosis and treatment strategy. Biomed Environment Sci. 2005;18:260–4. [PubMed] [Google Scholar]
- 13. Lijnen HR. Plasmin and matrix metalloproteinases in vascular remodeling. Thromb Haemost. 2001;86(1):324–33. [PubMed] [Google Scholar]
- 14. Fox SE, Atmakbekov A, Harbert JL, Li G, Brown Q, VanderHeide RS. Pulmonary and cardiac pathology in Covid‐19: The first autopsy series from New Orleans. MedRxiv 2020; in press/online. [Google Scholar]
- 15. Yuanliang X, Wang X, Yang P, Zhang S. COVID‐19 complicated by acute pulmonary embolism. Images Cardiothor Imaging. 2020; Published Online, March 16, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Boonyawat K, Crowther MA. Venous thromboembolism prophylaxis in critically ill patients. Semin Thromb Hemost. 2015;41:68–74. [DOI] [PubMed] [Google Scholar]
- 17. Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID‐19. Thromb Res. 2020;191:145–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kahn SR, Lim W, Dunn AS, et al. Prevention of VTE in nonsurgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines. Chest. 2012;141:e195S–e226S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost 2020;18:1094–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Thachil J, Wada H, Gando S, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID‐19. J Thromb Haemost 2020;18:1023–6. [DOI] [PMC free article] [PubMed] [Google Scholar]


