Abstract
Background and Objectives:
Prescription opioid (PO) misuse is increasing and is associated with overdose. Individuals who experienced a recent sexual assault are at risk for increased substance use, yet limited interventions target PO misuse after sexual assault. The current study examined the efficacy of video interventions on PO misuse after sexual assault.
Methods:
Adolescent girls and women (n = 154) were recruited in the context of a sexual assault medical forensic exam in the emergency department. Effects of a Prevention of Post-Rape Stress (PPRS) video and a Pleasant Imagery and Relaxation Instruction (PIRI) video were compared to treatment as usual (TAU) during a sexual assault medical forensic exam on PO misuse. Participants reported if they had used POs for non-medical purposes since the sexual assault at 1.5 month follow-up.
Results:
Results from a logistic regression analysis indicated that participants with a prior sexual assault were less likely to misuse prescription opioids 1.5 months after the assault in the PIRI condition compared to TAU. There were no main effects for video condition and no interactions for the PPRS condition on PO misuse.
Discussion and Conclusions:
Providing the PIRI video, or teaching other types of mindfulness or relaxation exercises, may be warranted as a secondary prevention for individuals during the sexual assault medical forensic exam for those with a prior sexual assault history.
Scientific Significance:
This research provides an initial examination of the impact of mindfulness skills recently after traumatic event exposure on PO misuse.
Clinical Trials Registration:
Keywords: opioid misuse, rape, emergency department, women, randomized clinical trial
Non-medical pain medication use, or prescription opioid misuse, is a significant public health problem1. Women are particularly at risk as the rates of death from overdose from prescription opioids is on the rise among women2. Emergency department (ED) visits for opioid overdose increased 30% from 2016 to 20173. Although there are current initiatives to provide evidence-based medication-assisted treatment (MAT) to individuals who present to the ED for opioid use, it may be possible to intervene with prescription opioid misuse in other contexts within the ED. For example, individuals with a recent sexual assault who present to the ED for a sexual assault medical forensic exam (SAMFE) may be experiencing high levels of physical and psychological distress. However, little is known about non-medical pain medication use at this crucial time after a sexual assault.
Findings from cross-sectional studies have found that sexual assault history and prescription opioid misuse are associated among adolescent girls4–6. Specifically, among a national sample of adolescents, results indicated that girls with a sexual assault history were more than four times more likely to use drugs which included nonmedical use of prescription medications than those without a sexual assault history5. Similarly, adolescent girls with a history of penetrative sexual assault were five times more likely to have used opioids in the past year than those without a sexual assault history6. These findings combined with the consistent cross-sectional finding that sexual assault is associated with chronic pain among adults7–9, it is essential to target prescription opioid misuse after sexual assault. Although there is limited research regarding prescription opioid misuse after recent sexual assault among adults, there is evidence that histories of traumatic event exposure are associated with higher rates of prescription opioid misuse among adults10–12. To our knowledge, there are no studies examining the effect of interventions on prescription opioid misuse after a recent sexual assault.
The SAMFE presents a unique opportunity to intervene with pain medication use because there are already initiatives in place at EDs nationwide to increase prescriptions of MAT to individuals who misuse prescription opioids. One study found that 40% of adults presenting for a SAMFE had used prescription opioids in the past year when asked at a follow-up phone screen13; however, this was a cross-sectional study and prescription opioid misuse was not assessed. More work is necessary to identify, screen, and effectively deliver interventions to target prescription opioid misuse.
Video education in healthcare settings is associated with greater knowledge about treatment options and more active involvement in treatment plans following exposure to video education14. Some studies have demonstrated that videos that inform patients about their disease and treatment can directly impact psychological functioning15–16. In relation to post-sexual assault substance use and mental health symptoms, oftentimes individuals who experienced recent sexual assault do not know what to expect in terms of post-sexual assault mental health sequalae, and teaching coping skills concurrently with providing information about what to expect after a sexual assault has proven to be useful for some17–18. Only one intervention, the Prevention of Post-Rape Stress (PPRS) video17, has been used to target post-sexual assault substance use and mental health symptoms during a SAMFE among girls and women after recent sexual assault. The PPRS includes information such as self-directed exposure exercises, methods to recognize and stop avoidance, and strategies to engage in activities that did not involve alcohol or drug use. Prescription opioid misuse is not uniquely addressed within this video, but individuals are encouraged to use coping strategies other than substance use, including non-medical use of prescription medications, to cope with symptoms related to the sexual assault. Initial findings comparing the PPRS video to treatment as usual (TAU) among 268 women at the SAMFE found that the PPRS was associated with less post-rape cannabis use compared to treatment as usual among women who reported pre-rape cannabis use17.
More recently, the PPRS was compared to both TAU and an active control condition, a Pleasant Imagery and Relaxation Instruction (PIRI) video18. The PIRI video is a commercially available tool that provides relaxation techniques including diaphragmatic breathing, use of words such as “relax” paired with exhalation, instructions for muscle relaxation, and pleasant nature-related imagery and sounds. The PIRI video to our knowledge, has not yet undergone scientific testing, however, the mindfulness skills taught have been tested among a wide variety of populations. The PPRS was associated with less alcohol use at the 6-month follow-up compared to TAU among women who reported any binge drinking in the year before the sexual assault and among minority women. There was a similar finding for cannabis use such that women without a prior sexual assault in the PPRS condition reported fewer days of cannabis use at 6-month follow-up compared to those in TAU. Therefore, it would be expected that the PPRS would have similar effects on prescription opioid misuse. However, the comparison PIRI intervention was not associated with reductions in alcohol or cannabis use after the sexual assault. Mindfulness-based skills are efficacious at reducing chronic pain19–20, a factor associated with prescription opioid misuse, as well as substance misuse more generally21. Therefore, providing mindfulness skills may indirectly reduce prescription opioid misuse after a recent sexual assault compared to TAU.
To our knowledge, no studies have examined if video-based interventions are associated with reductions in prescription opioid misuse. Due to evidence suggesting that the PPRS is associated with reductions in alcohol and cannabis use among some women who experienced a recent sexual assault17–18, the PPRS video might be a viable intervention for also targeting pain medication. However, the PIRI video may target different factors that are associated with prescription opioid misuse including mindfulness and relaxation skills22. These techniques might be particularly useful for reducing prescription opioid misuse given that mindfulness is an evidence-based treatment for chronic pain14.
1.1. Current Study
The current study presents an initial examination of prescription opioid misuse among girls and women receiving a SAMFE using the same sample as Walsh et al.18. It was hypothesized that both the PPRS and the PIRI conditions would be associated with lower prescription opioid misuse 1.5 months after the assault relative to TAU. Due to previous findings that treatment effects for the PPRS are more effective for those with a prior SA17–18, it was hypothesized that the PPRS and PIRI would be associated with reductions in prescription opioid misuse at 1.5 months after the assault compared to TAU among those with a prior SA. Further, age, ethnic/racial minority status, drug or alcohol-facilitated assault, and prescription opioid misuse prior to the assault were examined as potential covariates.
2.0. Methods
2.1. Participants
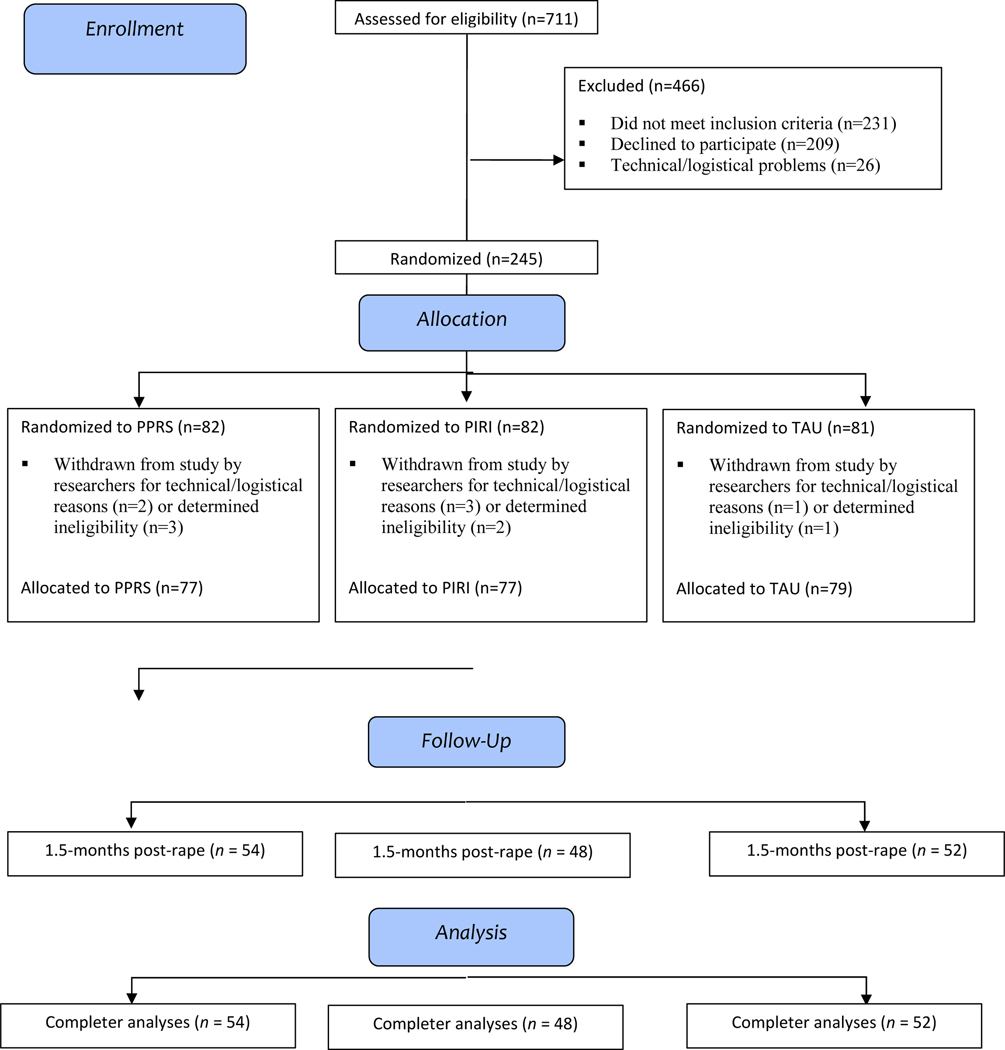
Participants were recruited from one of two medical centers in a Midwestern metropolitan area. Girls and women age 15 or older who received a SAMFE within 7 days post-sexual assault were recruited to be part of a larger study examining the efficacy of a video-based intervention for reducing substance use and mental health symptoms. Of the 711 participants who were screened for eligibility, 233 enrolled in the study. Individuals were excluded if they declined to participate (n = 209), did not meet inclusion criteria (n = 231), or because of technical/logistical problems (n = 26). A total of 154 participants were included in the current study because they completed the 1.5-month follow-up survey. Completers did not differ from non-completers on age or race/ethnicity. However, those that completed the follow-up survey were more likely to identify as more than one race than non-completers, [(11.6% vs. 1.7%, χ2 (1, N = 407) = 14.2, p < .0005)].
2.2. Measures
2.2.1. Demographics.
Participants provided self-report data on their age and race/ethnicity.
2.2.2. Prior SA.
Participants indicated if, other than the incident that brought them to the hospital, anyone had ever used force or threat of force to have unwanted sexual contact with them. They were asked both at the SAMFE and at initial follow-up.
2.2.3. Drug or alcohol-facilitated rape (DAFR).
Participants were asked about alcohol or drug use prior to or at the time of the assault during the initial follow-up. Individuals were classified as having DAFR if they reported either passing out due to substance use or being awake but too intoxicated to know what they were doing or to control their behavior.
2.2.4. Prescription Opioid Misuse and Non-Medical Use of Prescription Medication.
Participants were asked 1.5 months after the sexual assault, “Since the sexual assault, on how many days did you take on your own or non-medically…pain medicines like Codeine, Darvon, Percodan, Demerol, or Morphine.” If participants indicated that they took any of the listed drug types since the sexual assault, they were classified as having misused prescription opioids during the follow-up period. They were also asked about non-medical use of prescription medication use in the year before the sexual assault at this first follow-up.
2.3. Intervention Conditions
2.3.1. PPRS Video.
This video was entitled Steps to Recovery and focused on information about how to prevent emotional problems and substance use after a sexual assault. The video was 9 minutes1 in length and included a female narrator. Information included self-directed exposure exercises, methods to recognize and stop avoidance, and strategies to engage in activities that did not involve alcohol or drug use.
2.3.2. PIRI Video.
This 9-minute video1 was adapted from a commercial product entitled Relax©, David Garrigus Productions. This video included a female narrator providing instructions on relaxation techniques including diaphragmatic breathing, use of words such as “relax” paired with exhalation, instructions regarding muscle relaxation, and pleasant nature-related imagery and sounds. The original video was edited for length and content.
2.3.3. Treatment as Usual (TAU).
Although all participants received a SAMFE performed by a sexual assault nurse examiner, the TAU condition only received the SAMFE and no videos were provided.
2.4. Procedures
All procedures for the larger study are listed on clinicaltrials.gov (NCT01430624) and were approved by two University and two affiliated hospital Institutional Review Boards. Prescription opioid misuse was a secondary aim in the registered trial. After providing informed consent, participants were randomly assigned to the PPRS, PIRI, or TAU conditions (see Figure 1 for CONSORT). All procedures (exam and intervention) were administered in a private room within the hospital. Participants completed a structured telephone follow-up interview targeted at 1.5 months after the sexual assault conducted by Counseling Psychology doctoral students. For the larger study, participants also completed structured follow-up interviews at 3-and 6-months post-SA (for more information regarding procedures, see 18). However, analyses were not possible for these time points because at 3-month follow-up only 5.9% reported pain medication use and at 6-month follow-up only 9.9% reported pain medication use.
Figure 1.
CONSORT Diagram
2.5. Data Analytic Plan
A logistic regression analysis was conducted in MPlus 8 with Montecarlo integration. The outcome was pain medication use 1.5 months after the sexual assault, and predictors included condition, age, prior sexual assault, racial/ethnic minority status, drug- or alcohol-facilitated sexual assault, medications prescribed at the hospital, and prescription opioid misuse in the year before the sexual assault. Further, interactions between treatment condition and prior sexual assault were examined.
3.0. Results
3.1. Descriptive Analyses
In total, 42.9% (n = 66) of participants identified as White, 29.2% (n = 45) as Black/African American, 11.0% (n = 17) as Hispanic/Latina, 9.7% (n = 15) as multi-racial, and 7.1% (n = 11) as Native American. Thus, the majority identified as a racial/ethnic minority. Participants were on average 27.53 years old (SD = 9.28; range = 15 to 55). The majority (60.4%, n = 93) indicated that their most recent sexual assault was drug- or alcohol-facilitated and most (61.7%, n = 95) had a prior sexual assault. A total of 21.4% (n = 33) reported nonmedical use of prescription medication in the year before the sexual assault and 15.6% (n = 24) reported prescription opioid misuse at 1.5 month follow-up (17.3%, n = 9 in TAU condition; 18.5%, n = 10 in PPRS condition; 10.4%, n = 5 in PIRI condition).
3.2. Logistic Regression Findings
A logistic regression predicting pain medication use at 1.5-month follow-up indicated that past year non-medical prescription drug use was associated with prescription opioid misuse at follow-up (see Table 1). Further, there was a significant interaction between the PIRI condition and prior sexual assault such that, among those with a prior sexual assault, those in the PIRI condition reported significantly lower likelihood of misusing prescription opioids compared to those in TAU (B = −1.70, p = .02). There were no associations between video condition and prescription opioid misuse among those with no prior sexual assault (B = 1.43, p = .28). There were no other significant predictors of prescription opioid misuse at 1.5 months.
Table 1.
Logistic Regression Predicting Prescription Opioid Misuse 1.5 Months Post-assault
| Prescription Opioid Misuse at 1.5 Month Follow-Up | |||||
|---|---|---|---|---|---|
| Odds Ratio | B | SE | 95% CI | p | |
| Age | 1.028 | 0.028 | 0.026 | −0.024 – 0.080 | .320 |
| Racial/Ethnic Minority | 1.237 | 0.213 | 0.497 | −0.762 – 1.188 | .668 |
| Prior sexual assault | 4.681 | 1.544 | 1.258 | −0.923 – 4.010 | .220 |
| DAFR | 0.686 | −0.377 | 0.570 | −1.494 – 0.740 | .508 |
| Past year NMUPM | 12.505*** | 2.526 | 0.653 | 1.246 – 3.806 | <.001 |
| Prescription medications at discharge | 2.741 | 1.008 | 0.792 | −0.545 – 2.561 | .203 |
| PPRS vs. TAU | 1.420 | 0.351 | 1.689 | −2.959 – 3.661 | .835 |
| PIRI vs. TAU | 4.681 | 1.434 | 1.317 | −1.148 – 4.016 | .276 |
| PPRS X Prior sexual assault | 0.684 | −0.379 | 1.805 | −3.917 – 3.158 | .834 |
| PIRI X Prior sexual assault | 0.044* | −3.132 | 1.526 | −6.123 - −0.142 | .040 |
Note.
p < .001
p < .05
DAFR = drug or alcohol facilitated rape; NMUPM = nonmedical use of prescription medication; PPRS = Prevention of Post-Rape Stress; PIRI = Pleasant Imagery and Relaxation Instruction
4. Discussion
Given the increased public health concern of prescription opioid misuse among women, it is imperative to identify effective, scalable, and sustainable interventions that can be easily disseminated. The current findings provide initial support for one such intervention delivered in the context of the SAMFE. The SAMFE provides a unique opportunity for screening and intervention given that individuals are in the presence of a medical provider who can deliver medication-assisted treatment if an individual is misusing prescription opioids. Further, it provides an opportunity for behavioral or technology-based interventions for individuals misusing other prescription medications. Although the PPRS video was not associated with prescription opioid misuse at follow-up, the PIRI video was not associated with reductions in prescription opioid misuse for those with a prior sexual assault at 1.5-month follow-up compared to those in TAU.
It is interesting that the PIRI was associated with less prescription opioid misuse among those with prior sexual assault compared to TAU and the PPRS was not. The PPRS may not have been effective in reducing prescription opioid misuse because it did not directly address pain, only alcohol and drug use more globally. Whereas the PIRI used evidence-based techniques to reduce pain including mindfulness and relaxation23. It is likely that prescription opioid misuse is directly linked to experience of pain, and that the PIRI may have reduced pain. Pain was not assessed in the current study, but future research should examine if relaxation techniques taught in the ED is associated with reductions in prescription opioid misuse indirectly through reductions in pain. This finding adds to the emerging literature that behaviorally-focused interventions may be able to reduce prescription opioid misuse. Teaching mindfulness and relaxation techniques via technology-based interventions require only minimal burden to ED staff during the SAMFE.
Consistent with some of the previous research on technology-based interventions for alcohol and drug use, results indicated that the PIRI was only associated with reductions in prescription opioid misuse among those with prior sexual assault17, 24. It may be that individuals with a prior sexual assault attend to the content of the video because they are more familiar with their own substance use trajectory after sexual assault. Future research is needed to not only understand why technology-based interventions are more effective for those with more severe sexual assault histories, but also to understand why these interventions are not as effective for individuals without prior sexual assault.
Previous research indicated that the PPRS video is associated with decreases in alcohol use, cannabis use, and mental health disorders for some individuals17–18; however, these findings suggest that the relaxation content specific to the PIRI videos may be associated with reductions in prescription opioid misuse as well. Future work could consider incorporating some of these elements into brief interventions like the PPRS to maximally impact a variety of drug use phenotypes.
4.1. Limitations and Future Directions
Data collection for the current study was completed in 2013, which was prior to the influx of medication-assisted treatments available in the ED. Therefore, it is important for these findings to be replicated in more recent samples, as the patterns may change if treatment for prescription opioid misuse is available in the ED nationwide. The assessment of prescription medication misuse was limited, and future work should include a more comprehensive assessment of prescription opioid use disorder. The current study was conducted in a metropolitan area and future research should examine prescription opioid misuse after a recent sexual assault in rural populations as well given the significant burden of the opioid epidemic in rural areas25. The current study was designed to address both mental health and substance use after recent sexual assault, not just prescription opioid misuse. Given that the findings indicated that there was initial evidence of a video providing mindfulness skills in the ED after recent sexual assault on reducing prescription opioid misuse among some individuals, more research should be targeted to addressing prescription opioid misuse specifically in this population. Further, the larger study was a randomized clinical trial of a video intervention over three follow-up time points. However, the sample size was not large enough to assess the efficacy of the video intervention on prescription opioid misuse at the last two follow-up time points. Future research should examine the efficacy of the PPRS and PIRI videos on post-sexual assault outcomes among a larger sample of individuals who experienced a recent sexual assault. Finally, this study only included girls and women. Although this was necessary due to the limited research on post-sexual assault substance use and mental health sequelae among men and sexual/gender minority populations, future research should focus on understanding the mechanisms by which post-sexual assault substance use is developed and maintained among genders other than those who identify as girls and women, and subsequently test the efficacy of these videos with appropriate adaptations on post-sexual assault substance use and mental health among men and sexual/gender minority populations.
4.2. Conclusion
These findings contribute to the emerging literature regarding prescription opioid misuse after a recent sexual assault. Although these findings are limited to individuals who received a SAMFE, they provide an initial examination of prescription opioid misuse after a recent sexual assault. The data were collected prior to the wide dissemination of medication-assisted treatments for prescription opioid use disorders within EDs nationwide; therefore, current use rates may differ10. More research is needed to further understand the prospective correlates of prescription opioid misuse among samples of individuals who recently experienced a sexual assault.
Funding Acknowledgement
Data collection and manuscript preparation was supported by grants from the National Institute on Drug Abuse (NIDA; R01DA023099 to Dr. Resnick and K23DA042935 to Dr. Gilmore).
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
A small proportion (n = 28; 18%) of participants received longer (18-minute) versions of the intervention and active control videos that were shown prior to the SAFME and included either the PPRS or PIRI video plus information about the examination.
References
- 1.Ahrnsbrak R, Bose J, Hedden SL, Lipari RN, Park-Lee E. Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health 2017; Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration: Rockville, MD [Google Scholar]
- 2.Mack KA, Jones CM, Paulozzi LJ. Vital signs: overdoses of prescription opioid pain relievers and other drugs among women—United States, 1999–2010. MMWR. Morbidity and Mortality Weekly Report. 2013; 62, 537. [PMC free article] [PubMed] [Google Scholar]
- 3.Prevention, CDC. Opioid Overdoses Treated in Emergency Departments. Retrieved from: https://www.cdc.gov/vitalsigns/opioid-overdoses/index.html. March 16, 2018
- 4.Clayton HB, Lowry R, Basile KC, Demissie Z, Bohm MK. Physical and sexual dating violence and nonmedical use of prescription drugs. Pediatrics. 2017; e20172289. doi: 10/1542/peds.2017-2289 [DOI] [PubMed] [Google Scholar]
- 5.McCauley JL, Amstadter AB, Danielson CK, Ruggiero KJ, Kilpatrick DG, Resnick HS. Mental health and rape history in relation to non-medical use of prescription drugs in a national sample of women. Addictive Behaviors. 2009; 34(8), 641–648. doi: 10.1016/j.addbeh.2009.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Young A, Grey M, Boyd CJ, McCabe SE. Adolescent sexual assault and the medical and nonmedical use of prescription medication. Journal of Addictions Nursing. 2011; 22(1–2), 25–31. doi: 10.3109/10884601003628138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chandler HK, Ciccone DS, Raphael KG. Localization of pain and self-reported rape in a female community sample. Pain Medicine. 2006; 7(4), 344–352. doi: 10.1111/j.1526-4637.2006.00185. [DOI] [PubMed] [Google Scholar]
- 8.Haskell SG, Papas RK, Heapy A, Reid MC, Kerns RD. The association of sexual trauma with persistent pain in a sample of women veterans receiving primary care. Pain Medicine. 2008; 9(6), 710–717. doi: 10.1111/j.1526-4637.2008.00460.x [DOI] [PubMed] [Google Scholar]
- 9.Linton SJ. A population-based study of the relationship between sexual abuse and back pain: establishing a link. Pain. 1997; 73(1), 47–53. doi: 10.1016/S0304-3959(97)00071 [DOI] [PubMed] [Google Scholar]
- 10.Hassan AN, Le Foll B, Imtiaz S, Rehm J. The effect of post-traumatic stress disorder on the risk of developing prescription opioid use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. Drug and Alcohol Dependence. 2017; 179, 260–266. doi: 10.1016/j.drugalcdep.2017.07.012 [DOI] [PubMed] [Google Scholar]
- 11.Hawkins EJ, Malte CA, Grossbard JR, Saxon AJ. Prevalence and trends of concurrent opioid analgesic and benzodiazepine use among veterans affairs patients with post-traumatic stress disorder, 2003–2011. Pain Medicine. 2015; 16(10), 1943–1954. doi: 10.1111/pme.12787 [DOI] [PubMed] [Google Scholar]
- 12.Smith KZ, Smith PH, Cercone SA, McKee SA, Homish GG. Past year non-medical opioid use and abuse and PTSD diagnosis: Interactions with sex and associations with symptom clusters. Addictive Behaviors. 2016; 58, 167–174. doi: 10.1016/j.addbeh.2016.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gilmore AK, Hahn CK, Jaffe AE, Walsh K, Moreland AD, Ward-Ciesielski EF. Suicidal ideation among adults with a recent sexual assault: prescription opioid use and prior sexual assault. Addictive Behaviors. 2018; doi: 10.1016/j.addbeh.2018.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krouse HJ. Video modelling to educate patients. Journal of Advanced Nursing. 2001; 33(6), 748–757. doi: 10.1046/j.1365-2648.2001.01716.x [DOI] [PubMed] [Google Scholar]
- 15.Carpenter DJ, Gatchel RJ, Hasegawa T. Effectiveness of a videotaped behavioral intervention for dental anxiety: the role of gender and the need for information. Behavioral Medicine. 1994; 20(3), 123–132. doi: 10.1080/08964289.1994.9934627 [DOI] [PubMed] [Google Scholar]
- 16.Robertson C, Gatchel RJ, Fowler C. Effectiveness of a videotaped behavioral intervention in reducing anxiety in emergency oral surgery patients. Behavioral Medicine. 19911;17(2):77–85. doi: 10.1080/08964289.1994.9934627 [DOI] [PubMed] [Google Scholar]
- 17.Resnick H, Acierno R, Waldrop AE, King L, King D, Danielson C, et al. Randomized controlled evaluation of an early intervention to prevent post-rape psychopathology. Behaviour Research and Therapy. 2007; 45(10), 2432–2447. doi: 10.1016/j.brat.2007.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walsh K, Gilmore AK, Frazier P, Ledray L, Acierno R, Ruggiero KJ, et al. A Randomized Clinical Trial Examining the Effect of Video‐Based Prevention of Alcohol and Marijuana Use Among Recent Sexual Assault Victims. Alcoholism: Clinical and Experimental Research. 2017; 41(12), 2163–2172. doi: 10.1111/acer.13505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Veehof MM, Trompetter HR, Bohlmeijer ET, Schreurs KM. Acceptance-and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cognitive Behaviour Therapy. 2016; 45(1), 5–31. doi: 10.1080/16506073.2015.1098724 [DOI] [PubMed] [Google Scholar]
- 20.Zeidan F, Vago DR. Mindfulness meditation–based pain relief: a mechanistic account. Annals of the New York Academy of Sciences. 2016; 1373(1), 114–127. doi: 10.1111/nyas.13153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, Clifasefi S, Garner M, Douglass A, Larimer ME, Marlatt A. Mindfulness-based relapse prevention for substance use disorders: A pilot efficacy trial. Substance abuse. 2009; 30(4), 295–305. doi: 10.1080/08897070903250084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baker AK, Garland EL. Autonomic and affective mediators of the relationship between mindfulness and opioid craving among chronic pain patients. Experimental and Clinical Psychopharmacology. 2018; doi: 10.1037/pha0000225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, et al. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Annals of Behavioral Medicine. 2016; 51(2), 199–213. doi: 10.1007/s12160-016-9844-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gilmore AK, Lewis MA, George WH. A randomized controlled trial targeting alcohol use and sexual assault risk among college women at high risk for victimization. Behaviour Research and Therapy. 2015; 74, 38–49. doi: 10.1016/j.brat.2015.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Keyes KM, Cerdá M, Brady JE, Havens JR, Galea S. Understanding the rural–urban differences in nonmedical prescription opioid use and abuse in the United States. American Journal of Public Health. 2014; 104, e52–e59. doi: 10.2105/AJPH.2013.301709 [DOI] [PMC free article] [PubMed] [Google Scholar]