Abstract
Crush injuries of the hand involve damage to multiple structures within the hand, loss of tissue, devascularisation and possibly amputation of digits. They are complex and difficult to classify. Each injury has a unique pattern and requires a unique plan of management. There are no set procedures that can be described, however fundamental principles can be laid down to guide surgical management.
Optimum management requires a planned and decisive approach. The surgeon or the team must be well versed with techniques necessary for management of all the structures within the hand, microsurgery and free tissue transfer.
The essential components of management are, accurate assessment of the injury and creating a reconstructive plan by structures. The essential components for primary surgery are precise and complete debridement, skeletal stabiliation, vascular repair and if vessels are exposed, soft tissue cover. Secondary surgery should include procedures to enhance the function of the hand or to improve the aesthetics of the hand. These include bone grafting, fusion, tendon and nerve reconstruction, flap de-bulking and toe to hand transfers.
The following article is a concise synthesis of the fundamental principles which a hand surgeon must understand while undertaking these challenging procedures.
Keywords: Hand, Trauma, Amputation, Crush, Reconstruction
1. Introduction
The hand is a complex structure comprising of several tissues (skin, nerves, blood vessels, tendons, bones joints and intrinsic muscles) that are closely packed in a small space.
Crush injuries of the hand can present with wide variety of patterns and generally involve multiple tissues. Optimal management of such injuries requires a clear understanding of principles of management, correct decision making and wide repertoire of surgical techniques. Poor decision making and poorly executed surgery may result in prolonged recovery time and poor outcomes for the patient.
The common features of these injuries are:
-
•
Severe injury
-
•
Multiple structures are damaged
-
•
Different tissues are damaged to varying degrees
-
•
Tissue loss
-
•
Devascularisation
Due to the varying patterns there is no standard operating procedure, however based on principles and guidelines correct treatment can be formulated for each patient.
The principles of management are derived from evolving principles of wound management, antibiotic therapy, osteosynthesis, microsurgery, tissue transfer and rehabilitation.
The concepts of management have evolved from multiple debridement, and delayed reconstruction to single stage procedures.
The overriding principle of reconstruction is to provide a maximally functional hand in the shortest period of time with minimum number of surgical procedures. Each procedure must be performed with clear goals and should set stage for the next procedure.
Primary surgery is aimed to excise all devitalised structures and salvage the potentially viable structures. Once this is achieved secondary surgery is aimed to improve the existing function or the appearance of the hand. At the most two to three procedures should be necessary. However, if feasible all reconstruction should be performed in a single stage.
Midgeley and Entin in 19791 provided a succinct list of characteristics that constitute functionality in the hand, These are.
-
•
Strength,
-
•
Position,
-
•
Length,
-
•
Stability,
-
•
Mobility,
-
•
and Sensibility
These parameters also form the guide to what aspect need to be restored in order to provide a functional digit or a functional hand.
Functionality of the hand depends on the structures available. For a chuck pinch a minimum of two mobile fingers are needed to function with a thumb post,2 however a single sensate, mobile digit can provide a hook function. In absence of all fingers the thumb can act with the metacarpals to provide some degree of grasp.
-
1.
Assessment: A complete assessment is crucial. Accurate assessment leads to better planning
History should include the following:
When (Time of injury): indicates ischemia time and risk of infection.
How (Mechanism): Indicates severity of injury.
Where (Environment): indicates the possible infective agent, for example anaerobes in barnyard injuries, and marine organisms in injuries involving sea water.
Age of the patient and co-morbidities: such as associated diabetes, cardiac and renal conditions which may compromise the safety of surgical procedures.
If the patient is found to have life threatening comorbidities attempts should be made to optimise the patient for anaesthesia or the surgery may be considered under regional anaesthesia if possible.
1.1. Examination of the patient: life before limb
It is easy to be focussed on the injured hand, however in any trauma an overall examination of the patient must be performed in order to rule out any associated life threatening trauma.
Crush injuries of the hand may be associated with head injuries, thoracic injuries or abdomino-pelvic injuries causing the patient to collapse or decompensate during surgery.
This should be followed by lifesaving procedures if necessary which includes fluid resuscitation, blood transfusions, chest tube etc.
Amputated Parts: Amputated parts should be cleaned with saline, wrapped in a moist gauze and placed in a dry plastic bag. The bag should be placed in a container with ice. The container should be labelled clearly with patient’s name and identification number. The parts should never be discarded. They can either be replanted or used for spare parts.
1.2. Examination of the hand
A conventional examination of the hand may not be possible. Light touch sensation may be carried out to assess sensation in the digits; formal muscle testing may be impossible due to pain, bleeding and anxiety. However synthesis of anatomical knowledge, the posture of the hand, the colour of digits and visible location and depth of trauma can provide a fairly accurate diagnosis of the injury.
Skin: Skin flaps with a narrow bas: unlikely to survive and need to be replaced with skin flaps or grafts.
Loss of cascade: indicates injury to tendons or proximal innervation. Extended posture of digits indicates flexor tendon injuries, whereas finger drop indicates extensor injuries.
Pale or cyanosed digits: indicate devascularisation. Since arteries and nerves are within the same sheath, concomitant nerve injury should be anticipated.
Rotation or deviation of fingers: indicates fractures or joint dislocations.
The nature of skin separation and the length-breadth ratio of skin flaps will indicate whether the skin flaps will survive or will need to be excised and primary or secondary skin cover may be needed.
-
2.
Antibiotics: Intravenous antibiotic therapy should be commenced in the emergency department itself. In general broad spectrum coverage for gram positive, gram negative and anaerobic organisms is necessary. Specific antibiotics may be needed in special circumstances such as exposure to biological contaminants (agricultural or barnyard injuries) or sea water.
-
3.
X-rays: x-rays are essential in all cases. However it may be impossible to obtain good X-ray views particularly when the hand has been bandaged. Hence it may be necessary to perform X-Rays preoperatively on table when the patient is under anaesthesia and the wounded hand can be positioned without pain. X-ray images of the amputated parts should also be obtained.
-
4.
Recording: Once the patient has been resuscitated the hand may be inspected in the emergency department. Photographs should be taken which can be reviewed without having to repeatedly open the wounds. These photographs also serve as records for future reference. The photographs should be stored in secure electronic medical records or secure servers and not shared on social media.
-
5.
Planning: Once a visual examination has been performed, a systematic record of injuries should be made in structure by structure manner. This is essential for creating a reconstructive plan.
The list should include.
-
1.
Palmar skin
-
2.
First dorsal interossei, Thenar and hypothenar muscles
-
3.
Palmar/Digital arteries
-
4.
Palmar/digital nerves
-
5.
Metacarpals/phalanges of individual digits and joints
-
6.
Dorsal skin
-
7.
Vascularity of individual digits (highlighting devascularised or congested digits)
Each structural loss should be complemented with a reconstructive plan. For example.
-
•
Palmar skin: groin flap
-
•
First dorsal interossei, Thenar and hypothenar muscles: debridement
-
•
Palmar/Digital arteries: vein grafts from ipsilateral forearm
-
•
Palmar/digital nerves: sural nerve graft
-
•
Metacarpals/phalanges of individual digits and joints: K wire fixation& cerclage wiring
-
•
Dorsal skin: groin flap may need a combined superficial epigastric flap
-
•
Vascularity of individual digits (highlighting devascularised or congested digits): devascularised Middle finger (arterial injury in the palmar region)
-
6.
Preparation: The above plan guides preemptive surgical positioning and preparation and avoids setbacks during surgery.
1.3. Surgical preparation
-
•
Sural nerve graft, saphenous vein graft: Prepare the leg or use spare-parts
-
•
smaller vein grafts: Prepare the Forearm
-
•
Tendon: Prepare the forearm Palmaris longus, sacrifice FDS, use spare-parts
-
•
Flap: Prepare the Groin/abdomen and prepare the ipsilateral thigh for skin grafting the abdominal donor defect.
-
7.Goals of surgical management
-
•Restoration of maximal function
-
•In shortest possible time
-
•Through minimum number of procedures
-
•Each procedure should be performed with clear goals and should set stage for the next procedure
-
•
-
8.Primary (Emergency) surgery: A well performed primary surgery is critical for optimum outcomes. It should accomplish the following goals
-
•Excisional debridement
-
▪Skeletal stabilisation
-
▪Revascularisation
-
▪Skin cover
-
▪May or may not include tendon and nerve reconstruction/bone grafts.
-
•
-
9.
Excisional debridement: Excisional debridement is performed in layer by layer fashion. Skin flaps are excised to healthy bleeding skin. Contused or de-vascularised fat and muscles should be completely excised as they will form nidus for infections that may compromise the vascular repairs and the flaps. Contaminated fracture ends should be shortened using saw and medullary cavity should be curetted.
Longitudinal structures: intact arteries and nerves are preserved. Contamination should be removed through excision of the adventitia under magnification. Cut or crushed arties and nerves should be debrided under magnification until healthy ends are seen. Intact tendons should be preserved and paratenon or partial longitudinal excision may be carried out to remove contamination. Cut tendon ends should be debrided.
Repeated and incomplete debridement should be avoided. This potentially results in secondary infection of non-viable tissue and delays reconstructive procedures. However in certain circumstances such as biological or faecal contamination a cautious approach of staged debridement may have to be taken.
Intraoperative ‘triage’ and decision making: Decide Early What is salvageable, what is not3, 4, 5
-
1.
Thumb ray reconstruction is the first priority, if distal stump is available, any suitable digital stump can be used to restore the thumb
-
2.
The least injured fingers are then salvaged irrespective of the position.
-
3.
The best amputated segment is transferred to the best available stump.
-
4.
Severely traumatized digits may be used as a source of spare parts
Skeletal stabilisation: Forms the foundation for the entire reconstruction. Decision regarding the method of stabilisation is governed by the nature of contamination, adequacy of debridement, and presence of bone loss. If contamination is minimal plate and screw fixation can be performed. Bridge plates are used for maintaining length. However in cases of significant contamination K-wire fixation or external fixation is preferred. The placement of implants especially external fixation should be planned such that it does not interfere with the placement of the flap. Bone grafts represent non-viable tissue and are preferably performed as secondary procedures in open contaminated injuries.
Revascularisation: The next essential step is that of revascularisation. For successful revascularisation the vessels should be adequately debrided and healthy ends approximated. Whenever necessary reversed vein grafts should be used for arteries. For circumferential wounds it is essential to anastomose veins or venae commitans.
Skin cover: Flap cover is essential if blood vessels are exposed. Skin cover can be performed as a secondary procedure if vessels have a viable skin or muscle cover. In situations of major vascular injuries abdominal or groin flaps are performed as they do not sacrifice donor vessels from the injured limb.6 However if the hand requires revascularisation, anterolateral thigh flap7 or a radial artery forearm flap from the contralateral upper limb may be used a flow through flaps. Some composite flaps such as the dorsalis pedis flap can be used to provide simultaneous reconstruction of tendons and skin.8,9
If vessels are not exposed the wound can be sealed using a sterile dressing and a flap cover may be planned electively within next 48 h. Undue delay may result in tissue desiccation and microbial colonisation. Vacuum assisted dressing (V.A.C) may assist in providing a sterile closure.
-
9.
Rehabilitation: Rehabilitation in crush injuries may be complex and needs to be tailored to each injury. It can be affected by several factors such as strength and stability of skeletal fixation, combined flexor and extensor injuries in the same digit, and repaired ligaments such as collateral ligaments.
The aim should be to allow wound healing, maintain joint mobility, prevent adhesions and contractures and enhance scar maturation.
-
10.
Secondary surgery: secondary surgery is performed after complete healing of the initial surgery. It is usually timed beyond 6 weeks from the initial trauma. During this period joints are mobilised to prevent stiffness, and soft tissue massage is performed to reduce oedema which may compromise the results of final reconstruction. The aim of secondary surgery is to enhance function and the appearance of the hand.
Secondary surgery is used to address the following.
-
•
Nerve reconstruction using nerve grafts
-
•
Tendon grafts or tendon transfers
-
•
Bone grafting
-
•
Joint fusion
Other reconstructive procedures such as toe transfer are planned either in the secondary stage or tertiary stage. Flap de-bulking is performed as a secondary or as the final procedure to improve the appearance of the hand as well as to enhance the function.
1.4. Case illustration
History: A 35 year old male presented within an hour of his injury (when). His hand was crushed by a metal rolling machine (how). The machine had dirt and grease on it but no biological contaminants (where).
Primary and secondary surveys demonstrated no associated injuries. He was healthy without any associated comorbidities.
The hand was examined and photographs taken. The wound was irrigated with saline and covered with a sterile dressing. A single view (PA) portable x-ray was done. Broad spectrum antibiotics were commenced and arrangement was made for immediate transfer to the operating room.
1.5. Assessment
Severe crush injury extending from palm to dorsum of the hand. Likely to involve all tissue layers (Fig. 1).
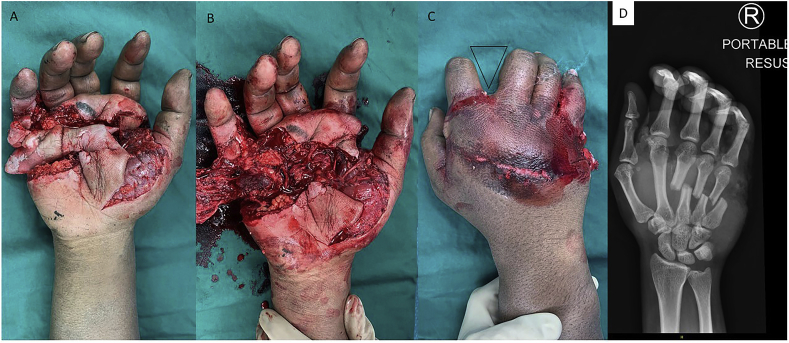
Fig. 1.
Severe crush injury involving the palmar to the dorsal aspect of the hand. The flexed posture of fingers indicates intact flexors (A,B,C). V-sign (C) between index finger and the rest of the fingers indicates fractures of metacarpals. X-ray of the hand (D).
Posture: The fingers are flexed hence flexors are likely to be intact. The V-sign between index and middle fingers indicated metacarpal fracture.
Colour: all digits appear to be oink, however capillary refill was sluggish indicating likely arterial damage.
The palmar skin: is de-gloved and unlikely to survive resulting in skin defect and exposure of common digital vessels nerves and tendons. (Primary flap needed, groin flap or flow through flap? preparation of the abdomen for flap and the thigh to harvest skin graft)
Superficial palmar arch and common digital vessels: Likely to be crushed or avulsed given the visual severity of injury and sluggish capillary refill. (Vein grafts/nerve grafts will be needed, prepare the lower limb)
Flexor tendons: all fingers show flexed position, flexors (likely deep flexors) are intact (No flexor reconstruction will be needed).
Metacarpals: Fractures seen on x-ray. (Stabilisation will be needed. However there is contamination with dirt and a risk of infection, plates would need to be avoided. External fixator can be used but it may interfere with placement of groin flap. K wires could be placed, however they should be removable easily if infection appears below the flap, will the K wires pierce through the flap?)
Interosseous muscles: are likely to be severely crushed.(Should be debrided completely)
Extensor tendons: couldn’t be assessed (May need tendon grafts primarily or can be planned as secondary surgery)
Dorsal skin: severely contused (will need to be excised resulting in exposed extensor tendons and fractures, flap should be able to cover palmar as well as dorsal skin: a bilobed groin and superficial epigastric flap may be suitable).
An operative plan was created on paper (Fig. 2A and B).
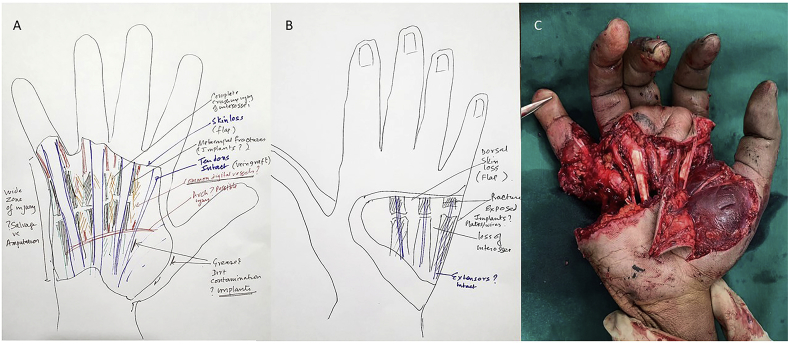
Fig. 2.
A preoperative visualisation of the expected trauma based on initial examination and the operative plan (A&B). Picture of the hand after debridement(C).
1.6. Operative steps
Debridement of all devitalised skin, interosseous muscles, bone ends sparing tendons and common digital vessel stumps. Wide zone of injury to the hypothenar muscles and crush injury extending to the middle phalanx of little finger, (Fig. 2C). Decision made to sacrifice the little finger.
Fracture stabilisation (unconventional): Decision to use K wires (Fig. 3A) in view of high risk of infection under the flap. The fractures ends were debrided using a mini power saw, creating oblique osteotomies in the coronal plane. K-wires were placed in the coronal plane and left long so as to exit at the edge of the flap without penetrating the flap. This facilitated easy removal without the need for detachment of the groin flap in case of infection. If the fracture went into non-union, the plan was to perform a secondary bone grafting.
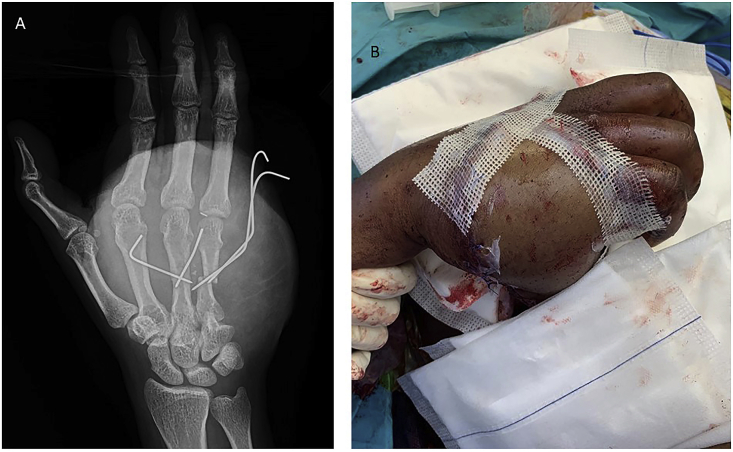
Fig. 3.
Unconventional fixation of the metacarpals using K wires in single coronal plane to avoid penetration of the flap and allow removal of implants if infection developed under the flap(A). Combined groin and superficial epigastric flap (B).
Neurovascular repair: vein grafts obtained from the same forearm were placed to revascularise the middle and ring fingers. Nerve grafts were not needed.
Flap: a combined groin and superficial epigastric flap was elevated and used to cover the pam and dorsum. The donor site was covered using skin graft obtained from the right thigh. The flap was divided 3 weeks later. Final outcome is seen in Fig. 4 at approximately four months following injury. Complete bone union was seen. Secondary flap de-bulking would be needed for aesthetic and functional improvment.
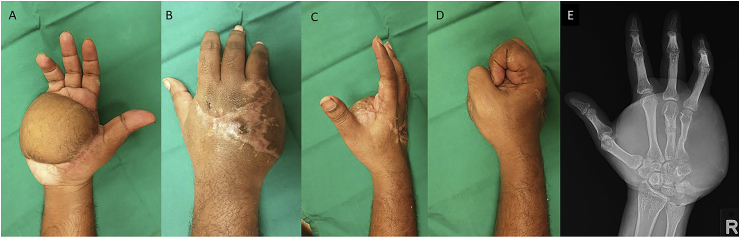
Fig. 4.
Function of the hand approximately four months after trauma (A through D). Complete bone union (E).
2. Summary: A practical check list
-
1.
Manage the patient first: Resuscitate the patient and rule out associated trauma or co-morbid conditions
-
2.
Preserve all amputated parts
-
3.Take a specific history:
-
•When (time of injury),
-
•How (mechanism of injury),
-
•Where (Environment of injury)
-
•
-
4.
Antibiotics: Broad spectrum antibiotics including anaerobic cover
-
5.
Make photographic records
-
6.
Take X-ray:(intraoperative X-rays if needed)
-
7.
Document injury by structure: Breakdown the injury by seven structural layers
-
8.
Construct a Plan: Based on seven structural layers
-
9.
Surgical preparation: Prepare potential donor sites for flaps, skin grafts, nerve and vein grafts
-
10.
Spare parts: use spare parts whenever possible
-
11.Primary surgery: achieve the following essential goals
-
•Debridement: The primary debridement should be complete and definitive
-
•Skeletal stabilisation: External fixators should be planned such that they do not obstruct flap coverage
-
•Revascularisation
-
•Flap cover if blood vessels are exposed. If vessels are not exposed a sterile dressing can be applied and flap cover can be planned within next 48 h
-
•Primary nerve and tendon repairs
-
•Tendon and nerve grafting or reconstruction can be primary or secondary.
-
•
2.1. Decision making in primary surgery
-
•
Prioritise thumb salvage or reconstruction
-
•
Salvage the least injured digits first
-
•
The best amputated segment is transferred to the best available stump.
-
•
Severely traumatized fingers may be used as a source of spare parts
-
12.
Rehabilitation: maintain joint mobility, prevent adhesions and contractures and enhance scar maturation.
-
13.Secondary surgery: achieve the following goals
-
•Nerve grafting
-
•Tendon drafting or tendon transfer
-
•Bone grafting, joint fusion
-
•Toe transfer
-
•Flap de-bulking
-
•
3. Conclusion
The management of crush injuries of the hand requires early accurate assessment of the injuries and a planned systematic approach which is tailored to each patient. Broadly, the primary emergency surgery should be aimed to remove all non-salvageable tissues and achieve skeletal stability and revascularisation. Secondary surgery is performed to enhance the function of the hand.
References
- 1.Midgley R.D., Entin M.A. Management of mutilating injuries of the hand. Clin Plast Surg. 1976;3:99–109. [PubMed] [Google Scholar]
- 2.Moran S.L., Berger R.A. Biomechanics and hand trauma: what you need. Hand Clin. 2003;19:17–31. doi: 10.1016/s0749-0712(02)00130-0. [DOI] [PubMed] [Google Scholar]
- 3.Peng Y.P., Lahiri A. Spare-part surgery. Semin Plast Surg. 2013;27(4):190–197. doi: 10.1055/s-0033-1360586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soucacos P.N. Indications and selection for digital amputation and replantation. J Hand Surg Br. 2001;26:572–581. doi: 10.1054/jhsb.2001.0595. [DOI] [PubMed] [Google Scholar]
- 5.Buchler U. Traumatic soft-tissue defects of the extremities. Implications and treatment guidelines. Arch Orthop Trauma Surg. 1990;109:321–329. doi: 10.1007/BF00636170. [DOI] [PubMed] [Google Scholar]
- 6.Sabapathy S.R., Bajantri B. Indications, selection, and use of distant pedicled flap for upper limb reconstruction. Hand Clin. 2014;30:185–199. doi: 10.1016/j.hcl.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Qing L., Wu P., Liang J., Yu F., Wang C., Tang J. Use of flow-through anterolateral thigh perforator flaps in reconstruction of complex extremity defects. J Reconstr Microsurg. 2015;31:571–578. doi: 10.1055/s-0035-1555138. [DOI] [PubMed] [Google Scholar]
- 8.Caroli A., Adani R., Castagnetti C., Pancaldi G., Squarzina P.B. Dorsalis pedis flap with vascularized extensor tendons for dorsal hand reconstruction. Plast Reconstr Surg. 1993;92:1326–1330. [PubMed] [Google Scholar]
- 9.Katsaros J. Indications for free soft-tissue flap transfer to the upper limb and the role of alternative procedures. Hand Clin. 1992;8:479–507. [PubMed] [Google Scholar]