Abstract
Scapholunate ligament is the most commonly injured ligament in the wrist and requires accurate diagnosis and treatment. It presents with pain, stiffness and can lead to carpal instability as well as degenerative arthritis if left untreated, with subsequent loss of function and disability. There are several management options currently available but there is no consensus on how best to manage a wrist with chronic sequelae of scapholunate ligament injury. This review explores available evidence in the literature on optimal treatment options including non-operative and operative procedures, relevant surgical techniques and their associated outcomes. A summary of the current concepts in the management of Chronic Scapholunate ligament injury is presented.
Keywords: Scapholunate ligament, Chronic, Reconstruction, Inter carpal ligament, Advance collapse, Tenodesis, Capsulodesis, Fusion
1. Introduction
Scapholunate (SL) ligament injury is a common presentation in wrist trauma with SL ligament instability the commonest cause of carpal instabilty.3, 4, 5, 6 Acute injury of the SL ligament can occur in isolation after a fall on an outstretched hand (FOOSH) or in association with distal radius fractures.2 Untreated injury of the SL ligament, at 6 weeks, is termed chronic SL instability.1 Biomechanical changes and altered tensile forces, in the long-term, lead to palmar-flexion of the scaphoid, dorsiflexion of the lunate and a widened scapholunate interval.2,4 Chronic instability of the SL joint causes scapholunate advanced collapse (SLAC), subsequently progressing to wrist arthritis.1,4 The SL joint is stabilised primarily by the scapholunate interosseous ligament (SLIL) which is an intrinsic ligament made up of three segments.9, 10, 11 Isolated injury of the intrinsic SLIL results in dynamic SL instability. However, damage to both the in SLIL, and the extrinsic ligaments is a prerequisite for the development of static SL instability.1,8,9 Consequently, many surgical procedures emphasise on reconstruction of the dorsal segment of the SLIL in treatment of chronic SL instability.
Patients often present with pain, reduced range of motion and loss of strength affecting their activities of daily living (ADLs).2,3,7 The management of chronic SL tears remains controversial despite these disabling symptoms. Early diagnosis is crucial for prompt treatment which aims at providing stability and preventing onset/progression of arthritis. One in twenty wrist sprains have an associated SL tear.7 Patients with a potential tear present with ongoing symptoms beyond the first few weeks after injury and require careful investigation. Plain radiographs classically show scaphoid ring sign, increased Scapholunate gap (SLG) and an increased Scapholunate angle (SLA).6 Magnetic Resonance (MR) imaging and MR arthrography are more accurate, but a negative result cannot rule out intrinsic or extrinsic ligament tear.5,6 Wrist arthroscopy remains the gold standard investigation for the wide spectrum of SLIL injuries. It allows real-time grading of the tear and immediate treatment if appropriate. Surgical management of SLIL injuries varies with severity of the tear, reducibility of the SL joint and chronicity of the injury. Treatments include arthroscopic debridement ± percutaneous pinning, bone-ligament-bone graft, three-ligament tenodesis, dorsal and volar capsulodesis, scapholunate axis method (SLAM) and intercarpal fusion and wrist fusion as the last resort. However, there is no consensus between hand surgeons on the optimal treatment for chronic SL ligament tears.
2. Anatomy
The anatomy of the carpal bones is well understood. Complex arrangement of carpal bones with scaphoid, lunate, triquetrum and pisiform forming the proximal row (lateral to medial); and hamate, capitate, trapezoid and trapezium forming the distal row (lateral to medial) is key for Carpal kinematics. The dynamics between these carpal bones allows movement at the wrist joint, namely, wrist flexion and extension and radial and ulnar deviation along with opposition of the thumb. A number of soft tissue hold the carpal bones together, amongst these the scapholunate ligament complex and the lunotriqueal interosseous ligaments are the primary carpal stabilisers.6 The scapholunate ligament complex involves both the intrinsic and extrinsic ligaments. The SLIL is a horseshoe shaped structure made of three components: dorsal, proximal and palmar (Fig. 1).10 It gets its blood supply primarily through the radial artery.5, 6, 7 The dorsal segment is the strongest portion with a tensile strength of 260–300 N and approximate thickness of 3 mm.12 It is responsible for flexion and extension and prevents rotation.
Fig. 1.
The scapholunate interosseous ligament (SLIL) viewed from the proximal/radial side with scaphoid removed.10
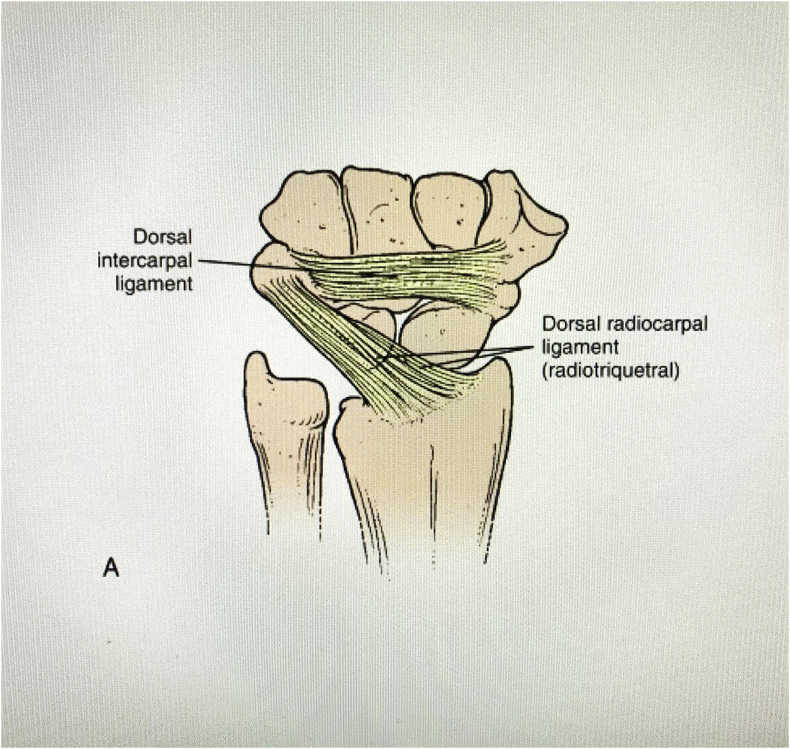
On the contrary, the weakest portion is the proximal avascular membranous component which has a tensile strength of 20–65 N. This membranous structure is often perforated in the elderly population with little functional consequences. Diagnostically this can give a positive SLIL tear result during wrist arthrography despite the dorsal and palmar ligamentous portions being intact. This does not cause true scapholunate instability. The palmar portion of the ligament is made of oblique fibres with a tensile strength of 120–150 N and approximate thickness of 1 mm. The palmar and dorsal segments work collectively to prevent rotational translation between scaphoid and lunate, whereas the intermediate segment has little role in stability.9, 10, 11,9,13 The Key extrinsic secondary stabilisers of Scapholunate interval are the radioscaphocapitate(RSC), long radiolunate (LRL), and radioscapholunate (RSL) on the Volar aspect; and the dorsal intercarpal (DIC) and dorsal radiocarpal (DRC) ligaments on the dorsal aspect (Fig. 2).16, 2 The SLIL and the extrinsic ligaments can undergo a spectrum of injuries some of which progressing to irreversible joint damage due to a change in carpal dynamics.
Fig. 2.
Dorsal Extrinsic Wrist Ligaments14
3. Classification
Chronic SLIL injuries are classified according to the stability of the scapholunate joint assessed radiographically or arthroscopically. Pre-dynamic instability represents a partial tear/sprain of the SLIL with no radiographic findings. Further damage to the SLIL can cause dynamic instability which can remain concealed on a standard radiograph. The instability is exposed on adding load (ulnar/radial deviation and clenched fist views) to the joint in a series of stress radiographs, hence the term ‘dynamic’. Radiographically there is a widened SLG > 3 mm or increased SLA > 600. In static instability the SLIL is injured along with the extrinsic ligaments and consequently, the above-mentioned features are seen in a standard radiograph, without the need for loading/stressing the joint.7,15
In 1996, Geissler et al. popularised the arthroscopic evaluation of SLIL using a 4-stage grading system.16 Grade 1–3 of this intraoperative classification represent pre-dynamic instability whereas grade 4 is equivalent with dynamic instability. More recently in 2006 and 2013, Garcia-Elias et al. and Andersson et al. respectively, theorised that the extent and nature of the injury to the SLIL will be of value diagnostically and help guide treatment.17,18 The Andersson-Garcia-Elias arthroscopic classification system (Fig. 3) is a culmination of these ideas. They introduced a 4-stage system that is applicable to both acute and chronic dorsal SL injuries.7,18
Fig. 3.
Anderson-Garcia-Elias Arthroscopic Classification of dorsal SL Ligament Injury. (Type 1: lateral avulsion; type 2: medial avulsion; type 3: mid-substance rupture; type 4: partial rupture plus elongation.18).
The European Wrist Arthroscopy Society (EWAS) classification of SLIL ruptures (Table 1) builds on existing arthroscopic classifications by considering the site of SLIL tear, especially on its volar aspect. Stage 1 relates to elongation. Stage 2 relates to rupture of the proximal membrane. Stage 3 is an extension of stage 2 with a degree of disruption of the SLIL. Stage 3 is further subdivided into three sections. Stage 3a and 3b involve the volar and dorsal portions of the SLIL, respectively. Arthroscopically this can be tested by measuring the SL joint space and laxity with a probe. This subdivision of Stage 3 helps highlight that a dorsal tear is more severe than a volar tear given the anatomical importance of the dorsal portion of SLIL. Stage 3c involves both, volar and dorsal, portions of SLIL. Arthroscopically there is complete widening of the SL joint space on dynamic testing. Stage 4 is a progression of stage 3c where a widened SL joint space is present without dynamic assessment. Stage 5 is the presence of a widened SL joint space (Stage 4) with carpal malalignment and radiographic abnormalities.19
Table 2.
Procedures included in Montgomery et al. systematic review.15
| Bone-tissue bone reconstruction | Intentional fibrous nonunion procedure | Capsulodesis | Tenodesis |
|---|---|---|---|
| Dorsal retinaculum or ligament graft Trapezoid to second metacarpal graft Capitohamate ligament graft |
Pin fixation with Arthroscopic debridement Arthroscopic RASL procedure with Herbert Whipple screw Arthroscopic RASL procedure with Herbert/Whipple/TriMed/HBS screws Open RASL procedure with HSC screw |
Blatt Dorsal intercarpal ligament Viegas Berger Mayo Lavernia + primary repair Arthroscopic capsuloplasty |
Tenodesis via dorsal/palmar FCR loop with fibre wire augmentation Brunelli tenodesis/Van Den Abbeele modification Garcia-Elias 3-ligmant tenodesis Scapholunotriquetral tenodesis Dynodesis (dynamic extension assisted and volar tenodesis |
FCR = flexor carpi radialis; HBS = headless bone screw; HCS = headless compression screw; RASL = reduction and association of the scaphoid and lunate.
Table 1.
European Wrist Arthroscopy Society (EWAS) Classification of Scapho-Lunate Injuries (Messina et al.: The EWAS Classification of Scapholunate Tears An anatomic Arthroscopic study)19
| Stage I | No Passage of the probe in SL space, but Synovitis |
|---|---|
| Stage IIA | Volar passage in the SL space without widening |
| Stage IIB | Dorsal passage in the SL space without widening |
| Stage IIC | Complete passage in e the SL space without widening |
| Stage IIIA | Volar partial widening at dynamic instability test from MC joint (volar instability) |
| Stage IIIB | Dorsal partial widening at dynamic instability test from MC joint (dorsal instability) |
| Stage IIIC | Complete widening of the space at dynamic test |
| Stage IV | Gap with passage of the arthroscope from MC to RC joint |
4. Management
Non-surgical treatment for chronic SL injury is limited to symptomatic management in patients either not fit for surgery or not keen on surgery. The natural history of the condition will eventually lead the patients to develop degenerative changes, but not all need surgical/invasive intervention. The non-surgical management includes immobilisation in a splint, NSAIDs, and intraarticular steroid injection.9 Surgical intervention is indicated if the above measures fail to control patients’ symptoms.
The exact operative intervention and surgical technique is based on intraoperative findings including articular cartilage status, status of any repairable remnants of scapholunate ligament, and reducibility of scapholunate joint.9 Michelotti et al. suggested that the results of an ideal repair or reconstruction of the scapholunate ligament should include; 1) Healing of the dorsal scapholunate interosseous ligament, 2) Maintenance of reduction of the scapholunate interval and preservation of anatomic relationships of the carpus, 3) Prevention of the biomechanical alteration that can lead to arthrosis, and 4) Limited morbidity of the other uninjured structures in the wrist.6
Different procedures and surgical techniques have been described in the literature with subsequent modifications, but there is no consensus on the most appropriate technique.11,15,22, 23, 24, 25, 26, 27, 28, 29, 30, 31 In 2018, Montgomery et al. set out to compare patient outcomes from current surgical techniques, performing subgroup analysis to establish whether there is a difference in outcomes between patients with static and dynamic instability.15 Due to diversity of procedures, they were divided in four groups as shown in Table 1.15
The first group included capsulodesis procedure, where a part of the wrist capsule or ligament is rearranged and reattached to the dorsum of scaphoid to act as restraint against flexion (Fig. 4).23, 1 The tenodesis group comprised of procedures where part of a tendon near the scapholunate joint was redirected through the carpus to restore and maintain alignment (Fig. 5).1,11 The bone-tissue-bone procedure entailed the use of harvested tissue with two bone fragments connected by a soft tissue bridge, and transplanted to the scapholunate articulation as an autograft.20 The last group included procedures that involved debridement and stabilisation of the scapholunate joint with a temporary or dynamic fixation (termed intentional fibrous non-union).15,21
Fig. 4.
Type 4a & 4b, Dorsal Intercarpal ligament Capsulodesis from Lateral and Dorsal Perspectives.30a,b
Fig. 5.
SL tenodesis described by Brunelli,11 Van Den Abbeele31 and Garcia-Elias.17
Their systematic review combined data from 35 papers providing a total sample size of 805 procedures, of which 391 patients from 14 studies who had capsulodesis, 319 patients from 12 studies who had tenodesis, 51 patients from 4 studies who had bone-tissue-bone technique and 43 patients from 4 studies who underwent “intentional fibrous non-union” type operations. Comparison of the pre- and postoperative outcomes against uninjured side demonstrated a statistically significant improvement in mean grip strength (67.0% v. 82.6%), Disabilities of the Arm, Shoulder and Hand (DASH) score (42.2 v. 18.5) and Patient-Rated Wrist Evaluation (PRWE) score (79.6 v. 32.1).15 There was also statistically significant reduction in the Visual Analogue Scale (VAS) score for pain (4.9 v. 3.0) and wrist flexion (52.3° v. 46.3°) with p < .05 for all.7
Radiological parameters (reported in 26 studies) showed a reduction of the SLG from 3.1 mm to 2.7 mm (p = .05) whilst the SLA showed a change from 62° to 57.9° (p < .05).15 Their analysis of procedure types did not reveal any statistically significant difference between outcomes of the clinical and radiological parameters. Their findings were based on similar patient demographical characteristics across the groups, with only difference being a significantly older patient population in the “intentional fibrous non-union” group by an average of 12.1 years (p < .05), and tenodesis group by an average of 10.8 years (p=<.05).15
Interestingly, they also analysed data from studies that reported radiographic instability. Their findings included 147 procedures from 14 studies for dynamic instability and 282 procedures from 19 studies done for static instability. Their findings revealed that static instability group patients had a larger mean preoperative SLG (3.9 mm vs 2.5 mm) and SLA (71.4° vs 56.0°) (p < .05) compared to dynamic instability group.15 Due to variability in reporting and follow up duration, Montgomery et al. could not compare complications for each procedure in the four groups.15
However, the reported complications included conversion to salvage procedure (5.4%), failure of graft or fixation (4.3%), CRPS (2.7%), neuroma or scar tissue concerns (1.9%), and infection (1.9%). The progression to SLAC wrist arthritis was 8.4% for the whole cohort, where the highest occurrence was in the bone-tissue-bone group (21.6%), and lowest (3.1%) was reported in tenodesis group.
The above results are further supported by similar findings in a recent systematic review by Wang et al. who compared capsulodesis to scapholunate ligament reconstructions.32 Their sample size was 11 studies that comprised of 308 patients. Their analysis of wrist flexion after ligament reconstruction and after capsulodesis identified an average of 40.9° and 45.6° respectively. Likewise, the average wrist extension was 47.3° after ligament reconstruction and 56.0° post capsulodesis. Radiologic findings revealed an average postoperative SLG of 2.72 mm in the ligament reconstruction group and 3.44 mm in the capsulodesis group. Average SLA was 56.5° for ligament reconstruction group, and 60.3° in the capsulotomy group at follow up.32
A most recent systematic review published by Daly et al., in 2020, compared preoperative and postoperative Radiographic, Clinical and Functional outcomes of tenodesis and capsulodesis as a surgical treatment for chronic scapholunate interosseous ligament (SLIL) disruption. Their review identified 40 studies (978 wrists), of which 23 assessed tenodesis, 14 assessed capsulodesis and 3 assessed both capsulodesis and tenodesis. The Radiographic data mainly relied on SLG widening or changes in the SLA as tools for detection of SLIL injury. Functional outcomes comprised of wrist range of motion (ROM); flexion; extension; radial deviation; ulnar deviation; grip strength; DASH score Mayo Wrist Score; and Wrightington Wrist Score.33, 34, 35 VAS pain score and time to return to work were used to assess for clinical outcomes.
SLA for tenodesis reconstruction was reported in 13 studies, and 11 studies reported SLA for capsulodesis reconstruction. SLA between preoperative and last follow up had a Standardised Mean Difference (SMD) of 0.7 (CI, 0.29 to 1.11, P = .001) in tenodesis reconstruction, and 0.04 (CI, −0.27 to 0.38, P = .8) for capsulodesis reconstruction. The capsulodesis group had an average pre-operative SLA of 59.9° as opposed to 73.9° for the tenodesis group. The post-operative SLA was however, 58.8° and 61.0° respectively. Thus, there was significant SLA improvement in tenodesis compared to capsulodesis (P = .01).36
SLG was reported in thirteen studies for tenodesis reconstruction and 10 studies for capsulodesis reconstruction. SLG between preoperative and last follow up had a SMD of 1.1 (CI, 0.6 to 1.55, P < .001) in tenodesis reconstruction, and 0.13 (CI, −0.36 to 0.59, P = .6) for capsulodesis reconstruction. The SLG was 1 mm narrower in tenodesis procedures when compared with capsulodesis reconstruction. Thus, tenodesis also had a significantly improved SLG.36
On comparing the clinical outcomes, it was noted that tenodesis demonstrated significant improvement in VAS 3.4 (P < .001) and DASH scores 27.3 (P < .01) point improvement. On the other hand, Capsulodesis demonstrated a reduction in VAS of 3.2 points (P = .5) and DASH of 20.2 points (P = .7). However, both groups exhibited a similar number of patients being able to return to work at their latest follow up (87% for tenodesis v/s 86% for capsulodesis).36
On evaluating pre-operative and latest follow up radial deviation, ulnar deviation and wrist ROM, no significant difference was found between the two groups. However, there was significant improvement in Grip strength, in tenodesis patients, by 16.8% on the contralateral hand (P < .001) and by 11.1% on the contralateral hand for capsulodesis patients (P = .2).36 Daly et al. compared complications amongst studies that published them, and reported infection rates of 3% and 5% in tenodesis and capsulodesis respectively. They noted that 6% of tenodesis patients required a second surgery as opposed to 4% of capsulodesis patients.
5. The SLAC wrist (Scapho-lLunate Advance Collapse)
The untreated SLIL injury will eventually lead to degeneration of the articular cartilage of the carpus. A chronic untreated injury creates a Dorsal Intercalated Segment Instability (DISI) leading to DISI deformity where the scaphoid is flexed and the lunate is extended as the SLIL is unable to provide a restraint to this articlulation. A scapho-lunate angle of greater than 70° and lunate extension of more than 10° past neutral is considered pathognomonic of DISI deformity. This leads to abnormal distribution of forces across the mid carpal and radio carpal joints leading to eventual degeneration of the joints. The diagnosis is usually made on plain radiographs, but may require MRI scans to look for any sparing of specific joints.
6. Discussion
Patients with Scapholunate Interosseous Ligament (SLIL) injury usually present with dorsal wrist pain exacerbated by lifting or axial loading.6 Clinical examination including palpation distal to the Lister tubercle and the Watson scaphoid shift test may provoke pain and discomfort. Standard plain film radiograph may reveal a static scapholunate ligament injury, including a gap of more than 3 mm in the SL interval (also known as Terry Thomas sign), and scaphoid ring sign-due to the flexion of the proximal pole of the scaphoid. Furthermore, there may be disruption of the Gilula arcs indicating carpus malalignment. An increase in the SLA of more than 60° (normal between 30° and 60°) due to flexion of scaphoid and extension of lunate causing characteristic dorsal intercalated segment instability (DISI) deformity.6
Different operative techniques have been suggested based on condition of the remaining ligament and type of instability. For predynamic instability, arthroscopic debridement and percutaneous pinning of SL interval followed by proprioceptive rehabilitation may suffice. However, for dynamic instability where direct repair is possible, authors have suggested dorsal SLIL repair ± capsulodesis. If direct repair is not possible, then the following procedures would be necessary; ligament reconstruction using dorsal intercarpal ligament, bone-tissue-bone graft, capsulodesis, reduction and association of the scaphoid and lunate and arthroscopic assisted ligamentoplasty.6 For static and reducible instability literature suggests four ligament tenodesis, modified Brunelli 3-ligament tenodesis, scapholunate axis method (SLAM) and scapholunotriquetral tenodesis.
Despite advancements in surgical techniques, treatment for chronic scapholunate ligament injuries remain challenging. Daly et al. reported superior overall radiographic results in patients who underwent tenodesis compared to capsulodesis with similar follow up duration.36 Their findings indicated SLG to be 1 mm narrower in tenodesis procedures compared to capsulodesis reconstruction. Furthermore, they also found that SLA was 12° narrower in tenodesis patients compared to those who had capsulodesis.
When comparing pre and postoperative results, Daly et al. also reported favourable outcomes in terms of pain reduction, improved hand functionality, increased grip strength, and significant improvements in VAS and DASH scores compared to capsulodesis.36 However, there was around 10%–15% decrease in wrist flexion and approximately 10% wrist extension reduction in both tenodesis and capsulodesis scapholunate ligament reconstruction groups. Therefore, patients should be counselled accordingly. Montgomery et al. also reported statistically significant reduction in pain and increase in grip strength at the expense of decrease in wrist flexion of 6°.15 There was also statistically significant improvement in DASH score, PRWE scores but not in Mayo Wrist Score. However, the radiographic improvements in SLG and SLA through surgical reduction were lost over time across all surgical procedures and instabilities.15 Although no significant difference was found within each instability subgroups, pre and postoperative radiographic improvement in the static instability was significantly better than those in the dynamic subgroup for both SLG and SLA. Furthermore, Montgomery et al. did not detect any statistically significant differences in outcomes between all surgical procedure categories. This finding was also supported by a systematic review by Wang et al. comparing capsulodesis procedure to scapholunate ligament reconstructions.32
Although the thickest and strongest portion of the SLIL is the dorsal limb, both dorsal and volar SLIL integrity is essential for normal carpal mechanics, and their reconstruction would provide multiaxial stability. Many open reconstruction methods do not address the volar portion of SLIL; therefore, there is higher risk of failure to reduce the SL interval. However, Henry et al. proposed an open surgical technique using an FCR tendon graft to create a bone-to-bone connections at specific locations to resist the multiplanar deforming force.37 Their one case example demonstrated improvement in pain, grip strength, range of wrist motions and maintenance of SL reduction at 8 years postoperatively. Arthroscopic reconstruction of both limbs of SLIL reported by Ho et al. and Corella et al. had favourable improvement in the wrist range of motion, pain, and activity of daily living as well as significant reduction in the SL interval postoperatively.38,39
Untreated scapholunate dissociation causing scaphoid rotatory subluxation and lunate dorsiflexion, also termed dorsal intercalated segment instability (DISI), contribute to development of SLAC wrist.1 Treatments for symptomatic SLAC wrist depend on the stage of degeneration, patients’ demands and requirements.. Nonoperative management encompasses oral NSAIDs, wrist splinting, activity modification, physiotherapy and intra-articular steroid injection, although there are no long-term studies on their efficacy. Surgical options entail partial or complete wrist arthrodesis, proximal row carpectomy (PRC), partial wrist denervation, styloidectomy with scaphoid stabilisation, as well as wrist arthroplasty.40 A study by Kiefhaber et al. found favourable outcomes for PRC and 4-corner arthrodesis with 85% of patients reporting better pain relief.41 They preferred 4-bone arthrodesis for patients under 35 years or high demand patients in their 40s and 50s. PRC was treatment of choice for older or less active patients. The details of the treatments are beyond the scope of this article.
7. Conclusion
The surgical management of chronic scapholunate injuries continues to present many challenges for surgeons. There is substantial evidence in the reported literature suggesting improved clinical outcomes in terms of functional outcome scores, pain score and grip strength with surgical intervention, that were statistically significant when comparing with preoperative findings. Some procedures such as tenodesis, for example, was reported to have superior results compared to capsulodesis but this was not statistically significant. Another study comparing four main categories of surgical intervention including, capsulodesis, tenodesis, bone-tissue-bone reconstruction and intentional fibrous procedures did not reveal any statistically significant difference in outcomes at final follow up. Therefore, our findings suggest that the exact surgical intervention should be based on the nature of injury, stage of pathology and degree of ligament deficiency as well as surgical familiarity of the operating surgeon. If a primary repair is not possible, then the surgeon should be aware of the available treatment options, and proficient surgical skills to perform required surgical procedure. Moving forward, there is a definite need for a multicentre prospective randomised control trial with long follow up period using validated measurement tools to evaluate both clinical and radiological outcomes.
Illustrations
To be published in colour.
IRB approval
Not applicable.
CRediT authorship contribution statement
Karim Wahed: Data curation, Writing - original draft. Saurabh Deore: Data curation, Writing - original draft. Kavyansh Bhan: Data curation, Writing - original draft. Sheela Vinay: Data curation, Writing - original draft. Gihan Jayasinghe: Data curation, Writing - original draft. Agneish Dutta: Data curation, Writing - original draft. Bijayendra Singh: Data curation, Writing - original draft.
Declaration of competing interest
None.
References
- 1.Athlani L., Pauchard N., Detammaecker R. Treatment of chronic scapholunate dissociation with tenodesis: a systematic review. Hand Surg Rehabil. 2018;37(2):65–76. doi: 10.1016/j.hansur.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 2.Dolderer J.H., Zimny K., Klein S.M., Koller M., Prantl L., Geis S. Reconstruction of chronic scapholunate dissociation with the modified scapholunate axis method (SLAM) Arch Orthop Trauma Surg. 2019;139(11):1641–1647. doi: 10.1007/s00402-019-03248-x. [DOI] [PubMed] [Google Scholar]
- 3.Alnaeem H., Alnaeem K., Tsai T.M. Chronic reducible scapholunate ligament dissociation: a simple surgical technique for a complex injury. Tech Hand Up Extrem Surg. 2020;24(2):55–61. doi: 10.1097/BTH.0000000000000261. [DOI] [PubMed] [Google Scholar]
- 4.Athlani L., Pauchard N., Dap F., Dautel G. Treatment of chronic scapholunate instability: results with three-ligament tenodesis vs. scapholunate and intercarpal ligamentoplasty. Hand Surg Rehabil. 2019;38(3):157–164. doi: 10.1016/j.hansur.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Geissler W.B. Arthroscopic management of scapholunate instability. J Wrist Surg. 2013;2(2):129–135. doi: 10.1055/s-0033-1343354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Michelotti B.F., Adkinson J.M., Chung K.C. Chronic scapholunate ligament injury: techniques in repair and reconstruction. Hand Clin. 2015;31(3):437–449. doi: 10.1016/j.hcl.2015.04.013. [DOI] [PubMed] [Google Scholar]
- 7.Andersson J.K. Treatment of scapholunate ligament injury: current concepts. EFORT Open Rev. 2017;2(9):382–393. doi: 10.1302/2058-5241.2.170016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim J.K., Lee S.J., Kang S.H., Park J.S., Park J., Kim G.L. Long-term results of arthroscopic debridement and percutaneous pinning for chronic dynamic scapholunate instability. J Hand Surg Eur. 2019;44(5):475–478. doi: 10.1177/1753193418822680. [DOI] [PubMed] [Google Scholar]
- 9.Sammer D.M., Shin A.Y. Wrist surgery: management of chronic scapholunate and lunotriquetral ligament injuries. Plast Reconstr Surg. 2012;130(1):138e–156e. doi: 10.1097/PRS.0b013e318254b5de. [DOI] [PubMed] [Google Scholar]
- 10.Wolff A.L., Wolfe S.W. Rehabilitation for scapholunate injury: application of scientific and clinical evidence to practice. J Hand Ther. 2016;29(2):146–153. doi: 10.1016/j.jht.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 11.Brunelli G.A., Brunelli G.R. A new technique to correct carpal instability with scaphoid rotary subluxation: a preliminary report. J Hand Surg Am. 1995;20(3 Pt 2):S82–S85. doi: 10.1016/s0363-5023(95)80175-8. [DOI] [PubMed] [Google Scholar]
- 12.Rajan P.V., Day C.S. Scapholunate interosseous ligament anatomy and biomechanics. J Hand Surg Am. 2015;40(8):1692–1702. doi: 10.1016/j.jhsa.2015.03.032. [DOI] [PubMed] [Google Scholar]
- 13.Pappou I.P., Basel J., Deal D.N. Scapholunate ligament injuries: a review of current concepts. Hand. 2013;8(2):146–156. doi: 10.1007/s11552-013-9499-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fress E., Gettle K., Phillips C., Janson J. St Louis: Mosby. third ed. 2005. Hand and upper extremity splinting principles and methods. [Google Scholar]
- 15.Montgomery S.J., Rollick N.J., Kubik J.F., Meldrum A.R., White N.J. Surgical outcomes of chronic isolated scapholunate interosseous ligament injuries: a systematic review of 805 wrists. Can J Surg. 2019;62(3):1–12. doi: 10.1503/cjs.006918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Geissler W.B., Freeland A.E., Savoie F.H., McIntyre L.W., Whipple T.L. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78(3):357–365. doi: 10.2106/00004623-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Garcia-Elias M., Lluch A.L., Stanley J.K. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg Am. 2006;31(1):125–134. doi: 10.1016/j.jhsa.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 18.Andersson J.K., Garcia-Elias M. Dorsal scapholunate ligament injury: a classification of clinical forms. J Hand Surg Eur. 2013;38(2):165–169. doi: 10.1177/1753193412441124. [DOI] [PubMed] [Google Scholar]
- 19.Messina J.C., Van Overstraeten L., Luchetti R., Fairplay T., Mathoulin C.L. The EWAS classification of scapholunate tears: an anatomical arthroscopic study. J Wrist Surg. 2013;2(2):105–109. doi: 10.1055/s-0033-1345265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cizmar I., Ira D., Visna P., Pilny J. Early results of reconstruction of the dorsal scapholunate ligament. J Plast Surg Hand Surg. 2010;44(4-5):245–251. doi: 10.3109/02844311.2010.503089. [DOI] [PubMed] [Google Scholar]
- 21.Blatt G. Capsulodesis in reconstructive hand surgery. Dorsal capsulodesis for the unstable scaphoid and volar capsulodesis following excision of the distal ulna. Hand Clin. 1987;3(1):81–102. [PubMed] [Google Scholar]
- 22.Bleuler P., Shafighi M., Donati O.F., Gurunluoglu R., Constantinescu M.A. Dynamic repair of scapholunate dissociation with dorsal extensor carpi radialis longus tenodesis. J Hand Surg Am. 2008;33(2):281–284. doi: 10.1016/j.jhsa.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 23.Hyrkas J., Antti-Poika I., Virkki L.M., Ogino D., Konttinen Y.T. New operative technique for treatment of arthroscopically-confirmed injury to the scapholunate ligament by volar capsuloplasty augmented with a free tendon graft. Scand J Plast ReConstr Surg Hand Surg. 2008;42(5):260–266. doi: 10.1080/02844310802210822. [DOI] [PubMed] [Google Scholar]
- 24.Cognet J.M., Levadoux M., Martinache X. The use of screws in the treatment of scapholunate instability. J Hand Surg Eur. 2011;36(8):690–693. doi: 10.1177/1753193411410154. [DOI] [PubMed] [Google Scholar]
- 25.Almquist E.E., Bach A.W., Sack J.T., Fuhs S.E., Newman D.M. Four-bone ligament reconstruction for treatment of chronic complete scapholunate separation. J Hand Surg Am. 1991;16(2):322–327. doi: 10.1016/s0363-5023(10)80120-0. [DOI] [PubMed] [Google Scholar]
- 26.Lutz M., Kralinger F., Goldhahn J. Dorsal scapholunate ligament reconstruction using a periosteal flap of the iliac crest. Arch Orthop Trauma Surg. 2004;124(3):197–202. doi: 10.1007/s00402-003-0620-y. [DOI] [PubMed] [Google Scholar]
- 27.Wolf J.M., Weiss A.P. Bone-retinaculum-bone reconstruction of scapholunate ligament injuries. Orthop Clin N Am. 2001;32(2):241–246. doi: 10.1016/s0030-5898(05)70246-7. viii. [DOI] [PubMed] [Google Scholar]
- 28.Seradge H., Baer C., Dalsimer D., Seradge A., Shafi R.A., Parker W. Treatment of dynamic scaphoid instability. J Trauma. 2004;56(6):1253–1260. doi: 10.1097/01.ta.0000075520.11052.64. [DOI] [PubMed] [Google Scholar]
- 29.Rosenwasser M.P., Miyasajsa K.C., Strauch R.J. The RASL procedure: reduction and association of the scaphoid and lunate using the Herbert screw. Tech Hand Up Extrem Surg. 1997;1(4):263–272. [PubMed] [Google Scholar]
- 30.Szabo R.M., Slater R.R., Jr., Palumbo C.F., Gerlach T. Dorsal intercarpal ligament capsulodesis for chronic, static scapholunate dissociation: clinical results. J Hand Surg Am. 2002;27(6):978–984. doi: 10.1053/jhsu.2002.36523. [DOI] [PubMed] [Google Scholar]
- 31.Van Den Abbeele K.L., Loh Y.C., Stanley J.K., Trail I.A. Early results of a modified Brunelli procedure for scapholunate instability. J Hand Surg Br. 1998;23(2):258–261. doi: 10.1016/s0266-7681(98)80191-5. [DOI] [PubMed] [Google Scholar]
- 32.Wang P., Stepan J.G., An T., Osei D.A. Equivalent clinical outcomes following favored treatments of chronic scapholunate ligament tear. HSS J. 2017;13(2):186–193. doi: 10.1007/s11420-016-9525-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Amadio P.C., Berquist T.H., Smith D.K., Ilstrup D.M., Cooney W.P., Linscheid R.L. Scaphoid malunion. J Hand Surg Am. 1989;14(4):679–687. doi: 10.1016/0363-5023(89)90191-3. [DOI] [PubMed] [Google Scholar]
- 34.Hudak P.L., Amadio P.C., Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 35.Talwalkar S.C., Edwards A.T., Hayton M.J., Stilwell J.H., Trail I.A., Stanley J.K. Results of tri-ligament tenodesis: a modified Brunelli procedure in the management of scapholunate instability. J Hand Surg Br. 2006;31(1):110–117. doi: 10.1016/j.jhsb.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 36.Daly L.T., Daly M.C., Mohamadi A., Chen N. Chronic scapholunate interosseous ligament disruption: a systematic review and meta-analysis of surgical treatments. Hand. 2020;15(1):27–34. doi: 10.1177/1558944718787289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Henry M. Reconstruction of both volar and dorsal limbs of the scapholunate interosseous ligament. J Hand Surg Am. 2013;38(8):1625–1634. doi: 10.1016/j.jhsa.2013.05.026. [DOI] [PubMed] [Google Scholar]
- 38.Corella F., Del Cerro M., Ocampos M., Simon de Blas C., Larrainzar-Garijo R. Arthroscopic scapholunate ligament reconstruction, volar and dorsal reconstruction. Hand Clin. 2017;33(4):687–707. doi: 10.1016/j.hcl.2017.07.019. [DOI] [PubMed] [Google Scholar]
- 39.Ho P.C., Wong C.W., Tse W.L. Arthroscopic-assisted combined dorsal and volar scapholunate ligament reconstruction with tendon graft for chronic SL instability. J Wrist Surg. 2015;4(4):252–263. doi: 10.1055/s-0035-1565927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Strauch R.J. Scapholunate advanced collapse and scaphoid nonunion advanced collapse arthritis--update on evaluation and treatment. J Hand Surg Am. 2011;36(4):729–735. doi: 10.1016/j.jhsa.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 41.Kiefhaber T.R. Management of scapholunate advanced collapse pattern of degenerative arthritis of the wrist. J Hand Surg Am. 2009;34(8):1527–1530. doi: 10.1016/j.jhsa.2009.06.020. [DOI] [PubMed] [Google Scholar]