Abstract
The metacarpal fractures are common fractures which are treated by orthopaedic surgeons, plastic surgeons and hand surgeons equally. These are seen in young adults who have active life style. These have a major impact in life style of the patients if these are not treated adequately. The management of the fractures vary among surgeons to surgeons; two surgeons in the same centre can have a different treatment plan for a fracture. There are no standard guidelines for the treatment and it ranges from conservative management, Kirschner’s wire (K-wires), plates and screws. This review article is about the management of metacarpal fractures where the commonly done procedures are reviewed.
Keywords: Metacarpal, Fracture, Hand
1. Introduction
Metacarpal fractures are second most common fractures in the hand. The incidence of metacarpal fractures is 8.4 per 10,000 person-years.1These may present as isolated fracture, multiple metacarpal fractures or in combination with bony injuries to other extremity. The metacarpal fractures constitute 18–44% of hand fractures.2 The superficial presence of the bone and the use of hand for evasive action to trauma makes the metacarpals as commonly fractured bones. The metacarpal fractures occur more common in men who constitute up to 85% of the patients. The fifth metacarpal is the most common metacarpal to get fractured.3 The metacarpal fracture can be classified depending upon the site as fracture of head, neck, shaft or base of the metacarpal. The fracture pattern may be classified as transverse, short oblique, long oblique or comminuted one. Metacarpal fractures are commonly managed conservatively with plaster of Paris slab. The hand surgeons use different operative techniques for the management of these fractures. There are no standard guidelines regarding the operative techniques. The purpose of this article is to review the management of metacarpal fractures other than the first metacarpal.
2. Clinical anatomy and physical examination
The metacarpals are placed together in a fan shape manner. These are attached to carpals at their base. The second and third metacarpophalangeal joints (MCPJ) are relatively stiff and immobile in nature. The fourth and fifth MCPJ are relatively mobile in nature. Hence, The malunion of fractures of neck and shaft of second and third metacarpal is less tolerated than the fracture of fourth or fifth metacarpal. The metacarpals fan out in divergent manner from their base. These are stabilized distally by the intermetacarpal ligaments. The proximal migration of the fractured fragments is prevented because of this ligament. The middle finger is the longest metacarpal and it forms the pillar on which other metacarpals are stabilized distally. The distal dome shaped structure makes them more stable. The palmar surface of hand is concave and the dorsal surface of hand is convex. This spade shaped structure is important for prehensile grip. The alteration in this shape may give rise to saddle syndrome. The palmar and dorsal interossei muscles arise from the shaft of the metacarpals. The contraction of these muscles gives rise to dorsal angulation deformity of the fractured metacarpal. The metacarpal shaft fractures should be immobilised with MCPJ in flexion so the contraction force of interossei muscles is neutralised and the deformity is prevented. The other reason to immobilise the MCPJ in flexion is related to length of the collateral ligaments which are most tight in flexion. The collateral ligaments are relaxed with MCPJ in extension leading to slight mobility (up to 20°) in coronal plane. The volar plate is the capsular thickening and prevents hyperextension of the MCPJ. The flexor carpi ulnaris (FCU) is attached to base of fifth metacarpal. The fracture of base of fifth metacarpal leads to displacement similar to Bennett’s fracture. The extensor carpi radialis longus and brevis are attached to base of second and third metacarpal respectively. The fracture of the base of the second or third metacarpal can also lead to dorsal displacement because of the contraction of these muscles.
The metacarpal fractures present with swelling and tenderness over the dorsum of hand. The deformity of the fingers is obvious sometimes. Among all the deformities of the hand, rotation is most poorly tolerated. The rotational deformity should be identified in patients of suspected of metacarpal fracture. The overriding of the finger, one over the other, at the time of presentation is a tell tale sign for presence of the rotational deformity. Subtle presence of rotational deformity can be identified by asking the patient to flex the fingers. All the fingers should point towards the scaphoid tuberosity. In presence of the rotational deformity, the scissoring of the fingers becomes obvious. The tenodesis effect can be used to unmark the rotational deformity. When the wrist is extended, all the fingers get flexed due to tenodesis effect and these point towards the scaphoid tuberosity. Proximal compression of the forearm also produces the same effect and this manoeuvre can also be used (Fig. 1). All the nail plates are parallel to each other when these are seen in tangential view. The loss of parallelism among the nail plates is a sign of rotational deformity.
Fig. 1.
The rotational deformity of the ring finger is visible as scissoring of the ring and middle finger (1a). The deformity gets corrected after the surgery (1b) as there is no scissoring and all the fingers are pointing towards the tubercle of the scaphoid.
3. Patho-anatomy of the metacarpal fractures and conservative treatment
There are three issues that are very important for metacarpal fractures. These include (1) shortening (2) rotation and (3) angulation in different planes. There is no absolute value of shortening which is tolerated by the patient. Different surgeons have mentioned different amount of shortening that gives rise decreased functional status of the finger (Table 1). In the absence of rotational deformity; 3 mm–5mm shortening should be considered acceptable as this does not give rise to major functional deficit. Transient minor extensor lag is not a big problem in general population. In athletes who have major functional demand, attempts are made to restore the anatomy. The rotational deformity is most important decision making factor as more than 5° of rotational abnormality leads to scissoring of fingers. More than 30° of dorsal angulation hampers the flexion and extension forces.
Table 1.
This shows the different articles published about shortening of the metacarpal.
| Researchers | Shortening | Postulates |
|---|---|---|
| Jupiter and Belsky4 | 03 mm | Intrinsic-extrinsic imbalance |
| Burkhalter5 | Transient extensor lag | |
| Green and Rowland6 | 05 mm | No reason |
| Freeland et al.7 | 03–04 mm | Greater amount of shortening leads to rotation |
| Lumplesch et al.8 | 06 mm | Good hand function upto this level of shortening |
| Robert J. Strauch et al.9 | 02 mm shortening leads to 7° extensor lag | Cadaveric study, |
| MJ Meunier10 | 02 mm results in 8% loss in intrinsic function 55% loss when 10 mm shortening | Cadaveric study, |
| CK Low11 | 30° of dorsal angulation or 03 mm of shortening leads to decreased flexion and extension forces | Cadaveric study, |
The minimally displaced, stable fractures can be managed with conservative treatment. An unstable fracture cannot be reduced with a closed method, or, if reduced then it cannot be held in the reduced position without supplemental fixation. It is difficult to assess the shortening on a single radiograph. Ideally, radiograph of opposite hand should be taken and exact amount of shortening can be measured. Practically; it is not always possible. The shortening of the fifth metacarpal and index metacarpal can be assessed on a single radiograph by drawing tangential lines connecting the most distal part of the heads of third and fourth metacarpal.12,13The computed tomography can also be performed to assess the exact amount of shortening. Traditionally, the cast has been applied in functional position of the hand also called as Edinburgh cast.14The wrist in 30–40° of extension, MCPJ in 90° flexion, PIPJ in zero degree extension and DIPJ in zero degree extension. This flexed position of MCPJ leads to relaxation of the interossei muscles and hence deformation forces at the fracture site are minimized. The zero degree extension at PIPJ and DIPJ are the positions where the ligaments of the corresponding joints achieve their maximum length and hence the chances of limitation of range of motion of these joints are minimized. Barton cast is used for fracture of the shaft of the metacarpal. It is based on the principle of three point moulding of the POP cast.15 The MCPJ and wrist joint are kept free. Additional padding is kept dorsally and dorsal pressure is applied while moulding of the POP to achieve the reduction of the dorsally angulated fractures. These traditional methods have been challenged in a retrospective study by Tavassoli Jeff et al. They compared three cast techniques for the treatment extra-articular metacarpal fractures.16 They compared the metacarpophalangeal joints in flexion and full interphalangeal joint motion permitted (Group 1); with the metacarpophalangeal joints in extension and full interphalangeal joint motion permitted (Group 2); and with the metacarpophalangeal joints in flexion, the interphalangeal joints in extension, and no interphalangeal joint motion permitted (Group 3).16 When immobilization was discontinued at five weeks then the position of the MCPJ and the motion of interphalangeal joints during the immobilization had little effect on the outcome of range of motion, grip strength, or fracture alignment. Considering the short duration of immobilization, the patient discomfort in extreme positions must be take care. The surgeon’s technique and ease of application must be counted while determining the type of the cast. Functional treatment of the metacarpal fractures has been compared with the cast treatment of the metacarpal fractures.17 There was no functional difference between the two groups but the sick leaves were considerably reduced in the patients who were treated by functional cast treatment. The fingers and wrist was left free in functional cast treatment.17
The fracture of neck of the fifth metacarpal has drawn special attention of the surgeons. This has been called as ‘Boxer’s fracture’. Infact, it is less common among the professional boxers and it is seen in the occasional boxers who are not trained and hit with the knuckles of the fifth metacarpal. The relatively higher mobility at fifth CMC joint makes the malreduction acceptable. Jahss described reduction manoeuvre for this fracture.18 It involves flexion of the MCP joint and gentle pressure is given along the axis of the proximal phalanx so the deformity gets corrected. The maintenance of this reduction during a period of time has been questioned as unstable fracture tends to displace.
Muller et al. did a prospective randomized trial comparing immediate mobilization with cast immobilization for treatment of Boxer’s fractures with volar angulation up to 70°.19They noticed that immediate mobilization resulted in satisfied patients with no pain and they had a good range of motion of the fifth MCP joint. They observed that up to 70° angulation of the fractures neck of fifth metacarpal is acceptable and reduction is not required. Harris et al. did traction reduction and cast immobilization of Boxer’s fracture. They were able to reduce 80% of the fracture angulation in sagittal plane with only one degrees of this correction was lost after three to four weeks.20
The cosmetic loss of fifth knuckle is the only problem and it should be discussed with all the patients. There has been no functional loss with malreduced fracture of the fifth metacarpal. Special attention must be given in manual labourers as the head of the metacarpal becomes prominent volarly and this may hamper the grip while lifting heavy objects.
4. Operative management of metacarpal fractures
The metacarpal fractures can be stabilized by absorbable suture hemicercilage, K wires, multiple inter-fragmentary screws, intra-medullary screws, metallic plates (compression plating, locking screw construct etc.), absorbable plates and external fixators. The choice of implants depends upon many factors that include nature of the fracture (open/close), location of the fracture, fracture morphology, functional demand of the patient, compliance of the patient. The patient’s choice also plays a role as the patient can decide as per his need. In countries where healthcare is not provided by the insurance, the socioeconomic status of the patient also plays a role. The costly implants cannot be afforded by every patient and hence, the K wires in different innovative configurations become the choice of implant in these countries.
The balance between maintaining the biology and fracture stability is crucial. The closed reduction preserves the biology but fracture stability, maintained by the K wires is poor to fracture stability maintained by the plates.
5. Techniques of Kirschner’s wire (K wire) fixation
Intramedullary K wire fixation was first described by Vom Saal in 1953. He used K wire by inserting it from the head of the metacarpal.21 This technique of insertion from the head of the metacarpal is not advocated now as it leads to extensor tendon problems and MCPJ stiffness. Ante-grade wires are more commonly used.
6. Ante-grade K wires
In French literature, Foucher G described bouquet wiring technique for distal third of the fifth metacarpal fractures in 1976.22 The technique was revisited by him in English literature in 1995.23 After reduction of the fracture with Jahss manoeuvre; three, curved, round tip wires (0.8 mm) were inserted from the base of the fifth metacarpal. Two similar K wires were provided the same stability. Postoperatively, buddy strapping of ring and little finger was done. The wires were removed at six to eight weeks. This technique still remains a time tested surgical technique among hand surgeons. It has been utilised for the fracture of neck of other metacarpals also. The technique is used for transverse fracture of the neck and shaft of the metacarpals. It is not for comminuted, spiral or oblique fractures because of inherent problems of the proximal migration of the wires when used in unstable fracture pattern.
Orbay JL used flexible intra-medullary nail (1.1 or 1.6 mm) for unstable fractures of the metacarpal.24 The proximal locking of the nail by its locking sleeve provides stability. Its end is covered with a cap that covers the metal part. The nail is removed under the local anaesthesia when the fracture has healed. The nail prevents shortening and better control over the spiral fractures is obtained. Multiple nails are used if the fractures are overtly unstable.
7. Retrograde K wires
Open retrograde pinning of transverse fractures of the metacarpal and phalanges was described in 1982.25 Two retrograde K wires were used to stabilize the fracture. The K-wires were in crossed fashion and it was essential to engage both the cortices of the bone. This technique provided better stability as compared to ante-grade wires. The only disadvantage of the technique was that it required opening and draining of the fracture hematoma and the implant removal is a little more complicated. The implant removal leaves the weak points around the fracture and the fracture needs to be protected after removal of the k-wires.
8. Transverse metacarpal wiring
Lamb did transverse metacarpal wiring in 66 patients.26 All the patients were having unstable metacarpal fractures. All the fractures united within one month. The functional outcomes were good. He suggested use of the power drill for inserting the K wires and at least one K wire was required on either side of the fracture. This technique is very simple technique which has not gained much popularity. Zhang et al. described a reduction technique for the Boxer’s fracture.27 A single K wire is inserted from the dorsal side into the middle of the fracture (as in intrafocal pinning). The distal fragment is levered out and the deformity is corrected. Two transverse intermetacarpal K wires are used for the fixation of the distal fragment in reduced position.27
In authors experience, it is very good technique in open fractures where the metacarpals can be fixed with the intact metacarpal. In the presence of multiple metacarpal fractures, the central metacarpal can be plated and rest of the metacarpals are transfixed to this metacarpal. It is difficult to control the rotational deformity with this technique.
9. Techniques of plate fixation
The plating depends upon the principle of autogenous welding. When the fracture is reduced anatomically and absolute stability is provided with compression at the fracture site then consolidation happens without external callus because of direct osteonal remodelling. This principle was initially followed by Robert Danis in Belgium. In 1950, Dr. Maurice E. Muller who visited Danis, further developed this concept and established a laboratory for experimental surgery. In 1958; foundation of the Arbeitsgemeinschaft für Osteosynthesefragen or AO was established by Muller, Allgower, Willenegger and Schneider. The results were carefully documented for further improvement. The precision engineering was used to develop the necessary instruments. In hand surgery, the principles of compression plating, bridge plating, lag screws and buttress plating are used commonly.28 Compression plating needs screws to develop frictional force between plate and the bone. If the load along the fracture site exceeds the frictional force between the plate and the bone then the instability happens, leading to failure of the construct. To overcome this problem, the locking plates were developed which depend upon the principle of fixed angle implants. Locking plates does not require friction between the bone and the plate; the blood supply is preserved due to this feature.29 A combination of these two principles can be used but it must be remembered that a nonlocking compression screw or a lag screw is not inserted after locking screw construct assembly.29 The different types of commercial plates are available, the medical grade stainless steel or titanium plates are commonly used. The modulus of elasticity of titanium is closer to bone and hence the plates made of titanium are preferred by many surgeons. Bosscha et al. did prospective study of metacarpal and phalangeal fractures which were fixed with AO mini fragment screws and plates. 29 of 31 metacarpal fractures regained total active motion greater than 220°.30 Ochman compared the locking and non locking plates for fixation of metacarpal fractures in animal model.31 They noted that locking plates can be used to achieve higher stability for metacarpal fractures. Monocortical, stable fixation was enough and hence flexor tendon interference can be avoided. Stability provided by the bicortical locking screw construct and unicortical locking screw was almost same in experimental model (no statistically significant difference).31
Dorsal plates have shown the highest stability. Black et al. performed biomechanical testing in a metacarpal model with dorsal plating with and without lag screws, crossed K-wires, intraosseous wires, and K-wires with intraosseous wires. The dorsal plating along with the lagged screws has shown the highest stability in metacarpal model.32
The dorsal plate placement may lead to extensor tendon adherence to plate, tendon rupture, hard ware prominence and wound healing problems.33,34 These problems are higher when the plates are used for phalangeal fractures. Joint stiffness is a common problem if the plates are used in close proximity of MCPJ. The plates provide highest amount of stability but at the cost of the violation of the soft tissues. Plating should not be used unless absolutely necessary. Less than 5%of the metacarpal fractures need plating. The overuse of the plating should be avoided.
The lateral locking plates are more commonly used now days and hence these minimize the extensor tendons problem and hardware prominence problems. These plates can be covered with interossei muscles after application. The authors of this article use the plates frequently whenever the fracture geometry demands more stability (Fig. 2). It is essential to close the periosetum or the interossei or abductor digiti mini (Fig. 3) over the plate so that tendon related complications are avoided.
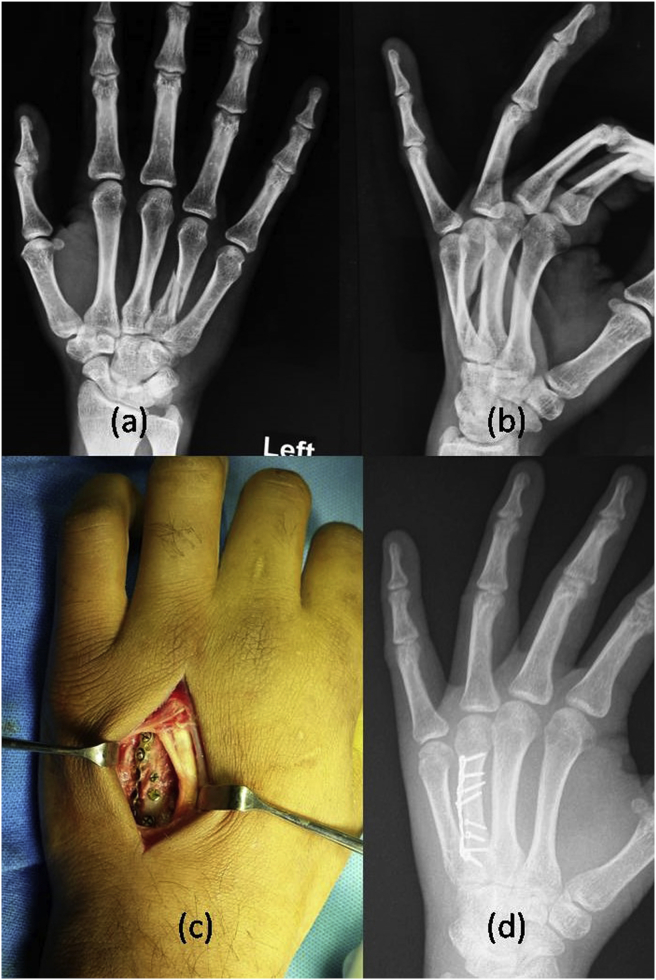
Fig. 2.
The preoperative postrero-anterior (2a) and oblique (2b) radiographs show fracture of the fourth metacarpal. The fracture has been fixed with titanium locking plate and the lag screws (2c). The postoperative radiographs show good healing after three months (2d).
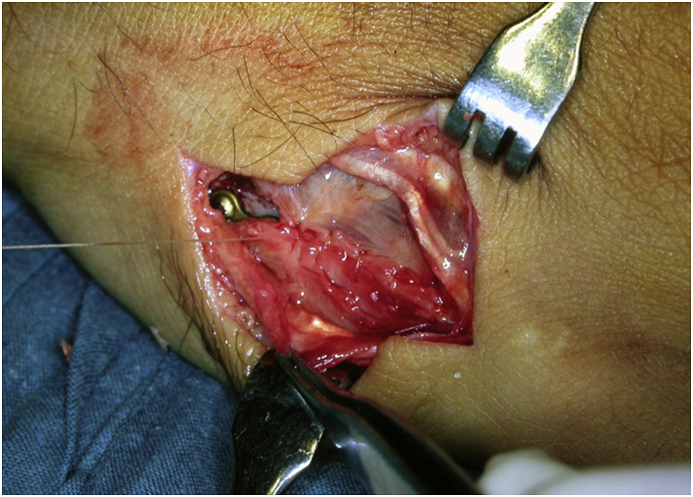
Fig. 3.
The meticulous closure of the periosteum and the abductor digiti mini is done over the plate.
10. Techniques of external fixation
The mini external fixator has been traditionally used for compound fractures in hand.35 These are very good treatment option as the chances of infection are minimized. The disadvantage with the external fixator is that these are slightly bulky and can bet caught in the clothing. The pin tract infections are uncommon and are usually superficial. In a prospective study, the pin tract reactions were found to be 9.8% of the metacarpal pins.36 Nonetheless, external fixator must be seen as an alternative or companion to other methods for the treatment of metacarpal fractures.
11. Techniques of inter-fragmentary screw fixation
The inter-fragmentary screw fixation van be used in long oblique fractures and short oblique fractures.37 The stability provided by two lag screw in oblique fracture in proximal phalanx is more than the stability provided by cross K wires, tension band wire, or dorsal plate fixation.38 In a biomechanical model, two constructs for metacarpal spiral fracture fixation were compared. Two large screws (2.0 mm) and three small screws (1.5 mm) were compared and they were found to be similar biomechanically. The construct with two large screws demonstrated led loosening during torsional cyclic loading, although the difference was small and may not be clinically significant.39 It must be remembered that the length of the fracture should be twice the diameter of the screw if using a single screw.28 The inter-fragmentary screws can be used in lag screw pattern or non-lag screw pattern. Lagging of the screw requires over drilling of the proximal cortex and which requires higher technical expertise as there are chances of the iatrogenic fracture at the site of the over drilling with a larger diameter drill bit. Ninklin et al. compared lagged and nonlagged screw fixation of metacarpal fractures in cadavers and they noted that nonlagged screw fixation with use of a pre-compression device provided comparable fracture site stiffness and biomechanical stability. Hence over drilling may not be required in metacarpal fractures.40
We use lag screws in various places (Fig. 4). We support the fixation with a plaster of Paris slab for three weeks after lag screw fixation alone. If we use if with plate then mobilize the patient in immediate postoperative period.
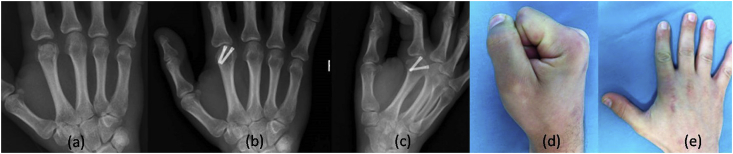
Fig. 4.
The preoperative postrero-anterior (3a) and oblique (3b) radiographs show fracture of distal third of the fifth metacarpal. The fracture has been fixed two lag screws (3c). The postoperative radiographs show good reductions (3d). These need to be supported with plaster of Paris slab for three weeks.
12. Techniques of intramedullary screw fixation
Del Pinal et al. described the minimally invasive technique for intramedullary fixation of the phanalegal and metacarpal fractures.41 They treated 69 patients with this technique with good outcomes. 3.0 mm cannulated screws were used for first four metacarpal. 4.00 mm screw was used for little finger metacarpal. This technique is most commonly used in transverse or short oblique fractures. A sturt with two screws can be made in unstable fractures which is technically a demanding procedure. There has been a concern about the cartilage defect which is created for the entry of the screw. The cartilage defect created by a single screw is a minor portion of the total surface of the metacarpal head.42 The articular defect are small and the midterm results have not shown any arthritis. The screw is inserted at the junction of the dorsal one third and volar two third of the head of the metacarpal. The load transmission from the MCPJ occurs with joint in flexion. The maximum force transmission is from the volar surface and hence the chances of arthritis are very low after intramedullary screw fixation via head of the metacarpal. Nonetheless, the long term results of this technique are still awaited. Esteban-Feliu et al. compared three different techniques as (1) plate screw, (2) K-wire, and (retrograde intramedullary screw for treatment of extra articular fractures of the phalanges and metacarpal.43 They concluded that the use of retrograde intramedullary screw is associated with shorter surgery duration and earlier return to work times.43
13. Metacarpal head fractures
Metacarpal head fractures are different from shaft fractures. These are rare and more commonly missed during the initial presentation. Usually three radiographic views as posteroanterior, oblique, and lateral views are recommended for hand trauma. If the metacarpal head fracture is suspected then the Brewerton view is done; it is done with MCPJ is flexed at 65° and fingers resting on the plate. The radiographic beam is tilted 15° ulnar to radial. This gives a clear picture of the metacarpal head. The metacarpal head fractures can be classified into epiphyseal fracture, avulsion fractures of the collateral ligaments, head split fractures as a two-part fracture (oblique, vertical, and horizontal), comminuted fracture, Boxers fracture with extension into the joint, loss of substance, and occult compression with avascular necrosis.44 The avulsion fractures can be fixed easily from the dorsal approach. Since MCPJ is not a weight-bearing joint the articular incongruence is easily tolerated. The articular step of more than 01 mm is considered as an indication for the surgery. Kumar et al. reported a surgical technique for reducing and stabilizing osteochondral fractures of the metacarpal and the phalanges.45 They reported that the space within the MCPJ is the only potential and small fragments can be placed on its place. The soft tissue attachments are covered and when the capsular closure is done carefully then the small fragments can be stabilized as a trap door. Early supervised mobilization was considered essential for good healing.45 The metacarpal head fractures into two parts can be stabilized from the dorsal approach. Two cannulated cancellous screws can be used for the fixation (Fig. 5). If the fragment size is small then two small screws (2 mm) can also be used with countersinking of the head technique. If K wires are used for the fixation then it is essential to remove. The tenolysis and arthrolysis of the MCPJ is not an uncommon procedure to gain range of motion if it is not achieved in the immediate postoperative period. The comminuted fractures are difficult to stabilize. The partial osteochondral defect can be managed with a contoured metatarso-phalangeal osteochondral autograft technique.46 The loss of the fragment or comminuted fractures may require MCPJ joint replacement rarely. The MCPJ replacement of the index finger is avoided because of excessive shear forces and early loosening of the joint.
Fig. 5.
The fracture of the head of the second metacarpal (5a) which has been fixed with two headless compression screws (5b and 5c) leading to near complete range of motion of the MCPJ of index finger.
14. Fracture of the base of the metacarpal
Fracture of the base of the metacarpal (second to fifth) is an uncommon injury.47 These are mostly associated with carpometacarpal joint (CMCJ) dislocation. These arer usually missed and hence if suspected then computed tomography scans should be done. Second and third CMCJ are relatively immobile joints. The avulsion injuries extensor carpi radials longus and extensor carpi radialis brevis are uncommon, athletic injuries.48,49 These are managed operatively and the tendon is anchored with suture anchors. Fifth and fourth CMC joints are mobile and the fracture of the base of the fifth metacarpal is an unstable injury. The deforming forces of the extensor carpi ulnaris lead to dorsal, ulnar, and proximal migration of the distal fragment. The injuries are treated as on the lines of the treatment of Bennet’s fracture-dislocation (Fig. 6).
Fig. 6.
The PA (6a) view of the hand shows the dislocation of the fifth CMC joint which has been fixed with two K-wires.
The fracture-dislocation of all the CMC joints (second to fifth) is high-velocity injury.50 Sometimes, it is associated with fracture of the carpal bones. It is usually not possible to treat these injuries with closed reduction. These usually require open reduction. Bridge plating is usually used to treat these injuries. The proximal end of the plate is fixed to carpal bones which are bridged over the reduced CMC joints. The plate is removed after six months.
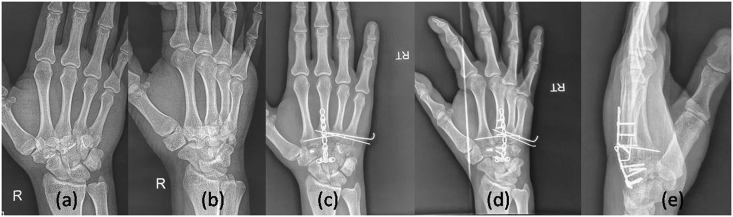
In case of comminution of the fractures, the central column (third metacarpal and capitate) is plated and the rest of the metacarpals are transversely fixed to this central column (Fig. 7).The symptomatic posttraumatic osteoarthritis of CMC joints (second to fifth) is very rare.
Fig. 7.
The PA 7(a) and oblique 7(b) views show CMC joint fracture dislocation of the second to fifth metacarpal. The central column was reconstructed with bridge plating and rest of the metacarpals were re aligned with transverse metacarpal wires 7(c), 7(d), and 7(e). The trapezoid fracture has also been fixed with a lag screw.
15. Complications of metacarpal fractures
The discussion of all the complications in detail is beyond the mandate of this review article. In brief, malunion is the most common complication which can present as dorsal angulation or rotatory malunion. The dorsal angulation is mainly a cosmetic problem and rarely may present as chronic pain due to tenosynovitis or sometimes as a manifestation of the saddle syndrome. It can easily be corrected by doing open or close wedge osteotomy. The rotatory malunions are more troublesome and present as scissoring of the fingers and it becomes difficult to hold the objects. These are usually treated by doing osteotomy at the base of the metacarpal. Other complications may be nonunion, infection, hardware problems, and stiffness of the MCP joints.
16. Wide awake local anaesthesia and no tourniquet (WALANT)
Lalonde et al. popularised use of WALANT in hand surgery. They have shown the use of Epinephrine in hand surgery is very safe and most of the procedures canbe performed.51 Feldman et al. reported a series of 10 patients, open reduction and internal fixation was performed under WALANT.52No significant pain or bleeding was recorded. All the patients were discharged on the same day.
In authors practice, WALANT is commonly used after a discussion with the patients. The choice of anaesthesia is decided by the patient. The patients usually make different choices.
17. Summary
Most of the metacarpal fractures can be managed conservatively and only few require operative intervention. K-wires are still most commonly used for the fixation of metacarpal fractures. Lag screws only and plating carry special value in unstable fractures. The intra-medullary screws have also opened a new window. The utility of different methods is summarized in Table 2 (see Table 1, Table 2). Sometimes different methods are used in a single patient (Fig. 8). The use of WALANT has made it possible to do these surgeries under local anaesthesia and its use will further expand in the horizon.
Table 2.
Summary of different Techniques.
| Types of implants | Preservation of Biology | Fracture stability | Tendon irritation | Need of hardware removal | Scar complications | Refracture | Cost |
|---|---|---|---|---|---|---|---|
| K wires | ++++ | ++ | + | + | – | – | + |
| Interfragmentary screws | + | +++ | + | _ | ++ | ++ | ++ |
| Intramedullary screws | ++++ | +++ | _ | _ | _ | _ | ++ |
| Metallic plates | + | ++++ | ++ | ++ | ++ | – | +++ |
| Absorbable plates | + | +++ | + | _ | ++ | – | ++++ |
| External fixators | +++ | ++ | + | + | – | + | + |
| Absorbable sutures hemicercilage | ++ | ++ | _ | _ | + | – | + |
Fig. 8.
Multiple methods have been used in a single patient. These include plate fixation with lag screws for fracture of the second metacarpal. Lag screws only for the third metacarpal, Transverse K wire fixation fourth and fifth metacarpal and crossed K wires for the middle phalanx of the index finger.
Funding statement
The authors received no financial support for research, authorship, and/or publication of this article.
Declaration of competing interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgements
Nil.
References
- 1.Karl J.W., Olson P.R., Rosenwasser M.P. The epidemiology of upper extremity fractures in the United States, 2009. J Orthop Trauma. 2015;29(8) doi: 10.1097/BOT.0000000000000312. [DOI] [PubMed] [Google Scholar]
- 2.Chung K.C., Spilson S.V. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg. 2001;26A:908–915. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 3.Court-Brown C.M., Caesar B.C. Overview of epidemiology. In: Bucholz R.W., Heckman J.D., Court-Brown C.M., Tornetta P., Koval K.J., editors. Rockwood and Green’s Fractures in Adults. sixth ed. Lippincott Williams & Wilkins; Philadelphia: 2006. pp. 102–110. [Google Scholar]
- 4.Jupiter J.E., Belsky M.R. Fractures and dislocations of thehand. In: Browner B.D., Jupiter J.B., Levine A.M., Trafton P.G., editors. vol. 2. WB Saunders; Philadelphia: 1992. pp. 925–959. (Skeletal Trauma). [Google Scholar]
- 5.Burkhalter W.E., Reyes F.A. Closed treatment of fractures of the hand. Bull Hosp Joint Dis. 1984;44:145–162. [PubMed] [Google Scholar]
- 6.Green D.P., Rowland S.A. Fractures and dislocations in the hand. In: Rockwood C.A. Jr., Green D.P., Bucholz R.W., editors. Fractures in Adults. third ed. JB Lippincott; New York: 1982. pp. 760–774. [Google Scholar]
- 7.Freeland A.E., Jabaley M.E., Burkhalter W.E., Chaves A.M.V. Delayed primary bone grafting in the hand and wrist after traumatic bone loss. J Hand Surg. 1984;9A:22–27. doi: 10.1016/s0363-5023(84)80179-3. [DOI] [PubMed] [Google Scholar]
- 8.Lumplesch R., Zilch H., Friedebold G. Frakturen der Mittelhandknochen II-V--Konservative und operative Behandlung. Unfallchirurg. 1985;11:115–118. doi: 10.1007/BF02587944. [DOI] [PubMed] [Google Scholar]
- 9.Strauch R.J., Rosenwasser M.P., Lunt J.G. Metacarpal shaft fractures: the effect of shortening on the extensor tendon mechanism. J Hand Surg Am. 1998 May;23(3):519–523. doi: 10.1016/S0363-5023(05)80471-X. [DOI] [PubMed] [Google Scholar]
- 10.Meunier M.J., Hentzen E., Ryan M., Shin A.Y., Lieber R.L. Predicted effects of metacarpal shortening on interosseous muscle function. J Hand Surg Am. 2004;29:689–693. doi: 10.1016/j.jhsa.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Low C.K., Wong H.C., Low Y.P. HP Wong: a cadaver study of the effects of dorsal angulation and shortening of the metacarpal shaft on the extension and flexion force ratios of the index and little fingers. J Hand Surg Br. 1995;20:609–613. doi: 10.1016/s0266-7681(05)80120-2. [DOI] [PubMed] [Google Scholar]
- 12.Manueddu C.A., Della Santa D. Fasciculated intramedullary pinning of metacarpal fractures. J Hand Surg Br. 1996 Apr;21(2):230–236. doi: 10.1016/s0266-7681(96)80104-5. [DOI] [PubMed] [Google Scholar]
- 13.Sletten I.N., Nordsletten L., Hjorthaug G.A. Assessment of volar angulation and shortening in 5th metacarpal neck fractures: an inter- and intra-observer validity and reliability study. J Hand Surg Eur. 2013 Jul;38(6):658–666. doi: 10.1177/1753193412461582. [DOI] [PubMed] [Google Scholar]
- 14.Haughton D.N., Jordan D., Malahias M. Principles of hand fracture management. Open Orthop J. 2012:43–53. doi: 10.2174/1874325001206010043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Debnath U., Nassab R., Oni J., Davis T. A prospective study of the treatment of fractures of the little finger metacarpal shaft with a short hand cast. J Hand Surg Br. 2004;3:214–217. doi: 10.1016/j.jhsb.2004.02.020. [DOI] [PubMed] [Google Scholar]
- 16.Tavassoli J., Ruland R., Hogan C., Cannon D. Three cast techniques for the treatment of extra-articular metacarpal fractures. Comparison of short -term outcomes and final fracture alignments. J Bone Joint Surg Am. 2005;(10) doi: 10.2106/JBJS.D.03038. 2,196–2,201. [DOI] [PubMed] [Google Scholar]
- 17.Konradsen L., Nielsen P.T., Beste E.A. Functional treatment of metacarpal fractures 100 randomized cases with or without fixation. Acta Orthop Scand. 1990;61(6):531–534. doi: 10.3109/17453679008993576. [DOI] [PubMed] [Google Scholar]
- 18.Jahss S.A. Fractures of the metacarpals. A new method of reduction and immobilisation. J Bone Jt Surg. 1938;20:178–186. [Google Scholar]
- 19.Muller M.G.S., Poolman R.W., van Hoogstraten M.J., Steller E.P. Immediate Mobilization gives good resultsin Boxer’s fracture with volar angulation upto 70 degrees: a prospective randomized trial comparing immediate mobilization with cast immobilization. Arch Orthop Trauma Surg. 2003 Dec;123(10):534–537. doi: 10.1007/s00402-003-0580-2. [DOI] [PubMed] [Google Scholar]
- 20.Harris A.R., Beckenbaugh R.D., Nettrour J.F. Metacarpal neck fractures: results of treatment with traction reduction and cast immobilization. Hand. 2009;4:161–164. doi: 10.1007/s11552-008-9150-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vom Saal F.H. Intramedullary fixation in fractures of the hand and fingers. J Bone Joint Surg Am. 1953;35:5–16. [PubMed] [Google Scholar]
- 22.Foucher G., Chemorin C., Sibilly A. Nouveau procede d’osteosynthbse original dans les fractures du tiers distal ducinqnibme m6tacarpien. Nouv Presse Med. 1976;5:1139–1140. [PubMed] [Google Scholar]
- 23.Foucher G. ‘Bouquet’ osteosynthesis inmetacarpal neck fractures: a sereies of 66 patients. J Hand Surg Am. 1995 May;20(3):86–90. doi: 10.1016/s0363-5023(95)80176-6. [DOI] [PubMed] [Google Scholar]
- 24.Orbay J.L., Touhami A. The treatment of unstable metacarpal and phalangeal shaft fractures with flexible nonlocking and locking intramedullary nails. Hand Clin. 2006 Aug;22(3):279–286. doi: 10.1016/j.hcl.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 25.Edward G.S., Obrien E.T., Heckman M.M. Retrograge cross pinning of transverse metacarpal and phalangeal fractures. Hand. 1982;Jun14(2):141–148. doi: 10.1016/s0072-968x(82)80005-3. [DOI] [PubMed] [Google Scholar]
- 26.Lamb D.W., Abernethy P.A. PA Raine: unstable fractures of the metacarpals. A method of treatment by transverse wire fixation to intact metacarpals. Hand. 1973;5:43–48. doi: 10.1016/0072-968x(73)90008-9. [DOI] [PubMed] [Google Scholar]
- 27.Zhang X., Huang X., Shao X. Reduction of fifth metacarpal neck fractures with a Kirschner wire. J Hand Surg Am. 2015;40(6):1225–1230. doi: 10.1016/j.jhsa.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 28.Schatzker J. Screws and plates and their application. In: Muller M.E., Allguwer M., Schneider R., editors. Manual of Internal Fixation: Techniques Recommendedby the AO-ASIF Group. Springer-Verlag; New York: 1991. pp. 179–290. [Google Scholar]
- 29.Egol K.A., Kubiak E.N., Fulkerson E. Biomechanics of locked plates and screws. J Orthop Trauma. 2004;18:488–493. doi: 10.1097/00005131-200409000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Bosscha K., Snellen J.P. Internal fixation of metacarpal and phalangeal fractures with AO minifragment screws and plates: a prospective study. Injury. 1993;24(3):166–168. doi: 10.1016/0020-1383(93)90283-c. [DOI] [PubMed] [Google Scholar]
- 31.Ochman S., Doht S., Paletta J., Langer M., Raschke M.J., Meffert R.H. Comparison between locking and non-locking plates for fixation of metacarpal fractures in an animal model. J Hand Surg Am. 2010;35(4):597–603. doi: 10.1016/j.jhsa.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 32.Black D., Mann R.J., Constine R., Daniels A.U. Comparison of internal fixation techniques in metacarpal fractures. J Hand Surg. 1985;10A:466–472. doi: 10.1016/s0363-5023(85)80067-8. [DOI] [PubMed] [Google Scholar]
- 33.Page S.M., Stern P.J. Complications and range of motion following plate following plate fixation of metacarpal and phalangeal fractures. J Hand Surg. 1998;23A:827–832. doi: 10.1016/S0363-5023(98)80157-3. [DOI] [PubMed] [Google Scholar]
- 34.Fusetti C., Meyer H., Borisch N., Stern R., Santa D.D., Papaloizos M. Complications of plate fixation in metacarpal fractures. J Trauma. 2002;52:535–539. doi: 10.1097/00005373-200203000-00019. [DOI] [PubMed] [Google Scholar]
- 35.De Kesel R., Burny F., Schuind F. Mini external fixation for hand fractures and dislocations: the current state of the art. Hand Clin. 2006;22(3):307–315. doi: 10.1016/j.hcl.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 36.Schuind F., Burny F. New techniques of osteosynthesis of the hand. Principles, clinical applications and biomechanics with special reference to external minifixation. Reconstr Surg Traumatol. 1990;21:1–159. [PubMed] [Google Scholar]
- 37.Adams J.E., Miller T., Rizzo M. The biomechanics of fixation techniques for hand fractures. Hand Clin. 2013;29(4):493–500. doi: 10.1016/j.hcl.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 38.Black D.M., Mann R.J., Constine R.M., Daniels A.U. The stability of internal fixation in the proximal phalanx. J Hand Surg Am. 1986;11(5):672–677. doi: 10.1016/s0363-5023(86)80010-7. [DOI] [PubMed] [Google Scholar]
- 39.Eu-Jin Cheah A., Behn A.W., Comer G., Yao J. A biomechanical analysis of 2 constructs for metacarpal spiral fracture fixation in a cadaver model: 2 large screws versus 3 small screws. J Hand Surg Am. 2017;42(12) doi: 10.1016/j.jhsa.2017.07.018. 1033.e1-1033.e6. [DOI] [PubMed] [Google Scholar]
- 40.Nicklin S., Ingram S., Gianoutsos M.P., Walsh W.R. In vitro comparison of lagged and nonlagged screw fixation of metacarpal fractures in cadavers. J Hand Surg Am. 2008;33(10):1732–1736. doi: 10.1016/j.jhsa.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 41.del Piñal F., Moraleda E., Rúas J.S., de Piero G.H., Cerezal L. Minimally invasive fixation of fractures of the phalanges and metacarpals with intramedullary cannulated headless compression screws. J Hand Surg Am. 2015;40(4):692–700. doi: 10.1016/j.jhsa.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 42.ten Berg P.W., Mudgal C.S., Leibman M.I., Belsky M.R., Ruchelsman D.E. Quantitative 3-dimensional CT analyses of intramedullary headless screw fixation for metacarpal neck fractures. J Hand Surg Am. 2013;38(2):322–330. doi: 10.1016/j.jhsa.2012.09.029. [DOI] [PubMed] [Google Scholar]
- 43.Esteban-Feliu I., Gallardo-Calero I., Barrera-Ochoa S., Lluch-Bergadà A., Alabau-Rodriguez S., Mir-Bulló X. Hand (N Y); 2019. Analysis of 3 Different Operative Techniques for Extra-articular Fractures of the Phalanges and Metacarpals. published online ahead of print, 2019 Sep. 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McElfresh E.C., Dobyns J.H. Intra-articular metacarpal head fractures. J Hand Surg Am. 1983;8(4):383–393. doi: 10.1016/s0363-5023(83)80196-8. [DOI] [PubMed] [Google Scholar]
- 45.Kumar V.P., Satku K. Surgical management of osteochondral fractures of the phalanges and metacarpals: a surgical technique. J Hand Surg Am. 1995;20(6):1028–1031. doi: 10.1016/S0363-5023(05)80154-6. [DOI] [PubMed] [Google Scholar]
- 46.Boulas H.J., Herren A., Büchler U. Osteochondral metatarsophalangeal autografts for traumatic articular metacarpophalangeal defects: a preliminary report. J Hand Surg Am. 1993;18(6):1086–1092. doi: 10.1016/0363-5023(93)90407-T. [DOI] [PubMed] [Google Scholar]
- 47.Stern P.J. Management of fractures of the hand over the last 25 years. J Hand Surg Am. 2000;25:817–823. doi: 10.1053/jhsu.2000.4214. [DOI] [PubMed] [Google Scholar]
- 48.Boles S.D., Durbin R.A. Simultaneous ipsilateral avulsion of the extensor carpi radialis longus and brevis tendon insertions: case report and review of the literature. J Hand Surg Am. 1999;24(4):845–849. doi: 10.1053/jhsu.1999.0845. [DOI] [PubMed] [Google Scholar]
- 49.Robert N., Zbili D., Bellity J., Doursounian L., Mauprivez R. Avulsion fracture of the extensor carpi radialis longus carpal insertion due to a basketball injury: case report and literature review. Chir Main. 2014;33(6):410–412. doi: 10.1016/j.main.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 50.Lawlis J.F., 3rd, Gunther S.F. Carpometacarpal dislocations: long-term follow-up. J Bone Joint Surg Am. 1991;73:52–59. [PubMed] [Google Scholar]
- 51.Lalonde D., Martin A. Epinephrine in local anesthesia in finger and hand surgery: the case for wide-awake anesthesia. J Am Acad Orthop Surg. 2013;21(8):443–447. doi: 10.5435/JAAOS-21-08-443. [DOI] [PubMed] [Google Scholar]
- 52.Feldman G., Orbach H., Rinat B., Rozen N., Rubin G. Internal fixation of metacarpal fractures using wide awake local anesthesia and no tourniquet. Hand Surg Rehabil. 2020;39(3):214–217. doi: 10.1016/j.hansur.2020.01.003. [DOI] [PubMed] [Google Scholar]