Abstract
Anomalies of the thumb development are not uncommon and may be associated with a number of syndromes also. These anomalies range from total absence to duplication. Reconstructive surgery for the creation of an opposable thumb is the most rewarding aspect of Hand Surgery and also the most challenging. Classification systems have been modified for better description. A number of procedures have been introduced to improve the functionality of the hand in anomalies and age old concepts are undergoing a metamorphosis to further this. A brief description of the common conditions and their treatment are discussed here and highlighted by selected clinical cases.
Keywords: Thumb anomalies, Thumb duplication, Polydactyly, Hypoplastic thumb, Trigger thumb, Triphalangeal thumb, Congenital
1. Introduction
The thumb is very important for the normal functionality of the human hand. The thumb ray in its position of rest is perpendicular to the plane of the other digits for grasp and pinch. The teleology of the 1st CMC joint for example, highlights the relationship of form with that of function in the hand.1 Anomalies in thumb development range from duplication of thumb to total absence of the thumb. Congenital trigger thumb may also be included in anomalies of the thumb, though there is much debate whether triggering is actually congenital or not.
1.1. Development of the thumb
The thumb is developmentally the last digit to form2 and also the subject of the maximum anomalies among all the digits. More than 1100 syndromic situations are associated with hypoplastic thumb as reported by the Online Mendelian Inheritance in Man (OMIM) database.3
The appearance of the upper limb bud at Day 28 of intra-uterine development leads to the formation of the hand.4 The signalling centre called the apical ectodermal ridge (AER) via the fibroblast growth factor (FGF) is responsible for the proximodistal longitudinal growth of the limb. The zone of polarizing activity (ZPA) via the sonic hedgehog (Shh) stimulates the radioulnar limb formation. The Wnt pathway via transcription factor Lmx-1 results in dorsoventral differentiation. On Day 33, the hand plate appears. By Day 41, webbed finger rays appear along with chondrification of radius, ulna and the metacarpals. and then programmed apoptosis leads to interdigital differentiation by Day 44. Day 48 sees the chondrification of the middle phalanges in the digits. Formation and differentiation of thumb is by a prolonged and concerted interplay of transcription factors such as HOXA13, GLI3,HOXD13 and TBX53.
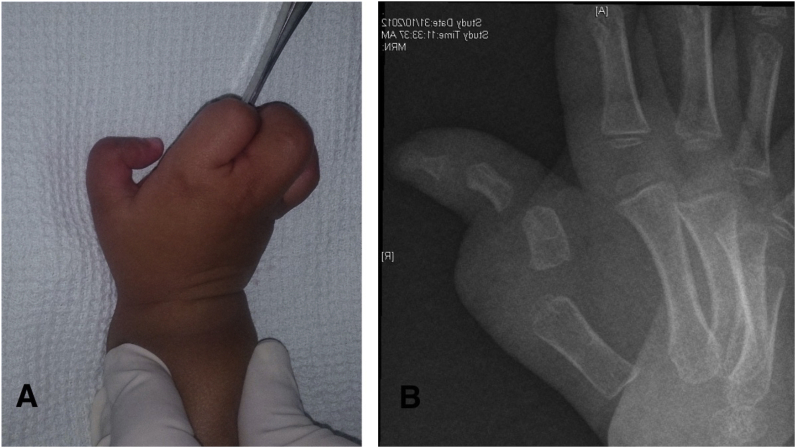
2. Trigger thumb
Congenital trigger thumb is now considered a misnomer as it is neither present at birth nor does the thumb in majority of the children, actually trigger.5,6 The affected children present with a flexion deformity of the thumb (See Fig. 1A), which can be bilateral in about 30% of the children. The incidence reported is about 3.3 per 1000 live births with most children showing the typical IP joint flexion deformity within 24 months of age without any triggering. The characteristic feature is the presence of a palpable nodule over the MCP joint in the volar aspect referred to as the Notta’s nodule. Forced extension of the persistently flexed IP joint maybe painful.
Fig. 1.
A. Photograph of the hand of a 2- year old child showing the flexion deformity of the Lt thumb interphalangeal joint. This is the usual presentation of trigger thumb.
Fig. 1B. A transverse incision at the level of the MCP joint crease to expose and incise the A1 pulley is used.
Fig. 1C. The flexor tendon is hooked and checked for gliding after the release of the pulley.
Sugimoto described the trigger thumb in children Table 1 in 4 stages.7
Table 1.
Classification of trigger thumb in children according to Sujimoto.
| Sugimoto Staging of Trigger Thumb | |
|---|---|
| Stage I | Palpable Notta nodule +, no triggering/snapping |
| Stage II | Active triggering, seen on active IP joint extension |
| Stage III | Passive triggering, seen on passive IP joint extension, active IP joint extension not possible |
| Stage IV | Rigid type, no active or passive extension possible. |
The cause of trigger is attributed to a size mismatch between the cross-sectional area of the tendon of flexor pollicis longus (FPL) and the A1 pulley. No obvious inflammation is found in the affected area. The Notta’s nodule which is a thickening within the flexor tendon is seen proximal to the A1 pulley.
Spontaneous resolution of triggering has been reported from 30 to 63% of the patients8,9 and this has been the authors experience also especially in children presenting with passively reducible triggering. Trigger thumb persisting beyond 3 years of age may result in bony changes in the IP joint and is difficult to correct.
2.1. Treatment
In spite of evidence in literature which proves otherwise, the majority of trigger thumb presenting to the surgeon are still conventionally operated.
Nonoperative treatment maybe simple observation or gentle massaging by the parents and splinting. A report comparing observation and splinting showed 23% resolution of symptoms in the former versus 71% in the latter.10 It is the authors practise to treat conservatively stage I and II and surgically treat stage III and IV trigger thumbs in children.
2.2. Surgical release
We prefer to use a transverse incision adjacent to the MCP joint flexion crease (Fig. 1B). The radial neurovascular bundle is quite superficial and is under risk. This is carefully identified and retracted. The ulnar neurovascular bundle is further away and also must be safely retracted. The thickened A1 pulley is identified and sharply incised. Avoid injuring the oblique and A2 pulleys. The flexor tendon is hooked and pulled with a blunt hook to ensure free gliding within the sheath (Fig. 1C). Any tenosynovial proliferation encounterd is removed. Skin is closed with absorbable sutures and soft dressings are applied. Physiotherapy post operatively is not mandatory.
3. Duplication of the thumb
This condition also termed radial or pre-axial polydactyly is usually clinically obvious with radiographs helping in classifying the extent of duplication. It is considered a sign of “good luck” in many cultures especially in the Indian subcontinent with parents refusing surgical correction. It is more common in the Caucasians with an incidence of 0.08–1.4 per 1000 live births11 and cases are usually unilateral and sporadic. Though originally grouped as a duplication in the IFSSH classification,12 it is now grouped under failure of axis formation/differentiation:hand plate in the OMT classification.13
3.1. Classification
Wassel with the guidance of Adrian Flatt described a classification based on the level of skeletal duplication.14 The phalanges or metacarpals can be bifid when they share a common base or duplicated when they are completely separated (See Table 2). The odd number types have bifid bones most proximally while the even number types have duplicated bones. No attempt has been made in this simplified classification to denote divergence or convergence of the duplicated segments (see Fig. 2A and B) even though this affects the final result following reconstructive surgery. More complex classification systems are available especially to clarify the triplication and triphalangeal elements.15
Table 2.
Wassel classification of thumb polydactyly.
| Wassel Classification of Thumb Polydactyly | |
|---|---|
| Type I | Bifid distal phalanx |
| Type II | Duplicated distal phalanx |
| Type III | Bifid proximal phalanx |
| Type IV | Duplicated proximal phalanx |
| Type V | Bifid metacarpal |
| Type VI | Duplicated metacarpal |
| Type VII | Triphalangeal thumb |
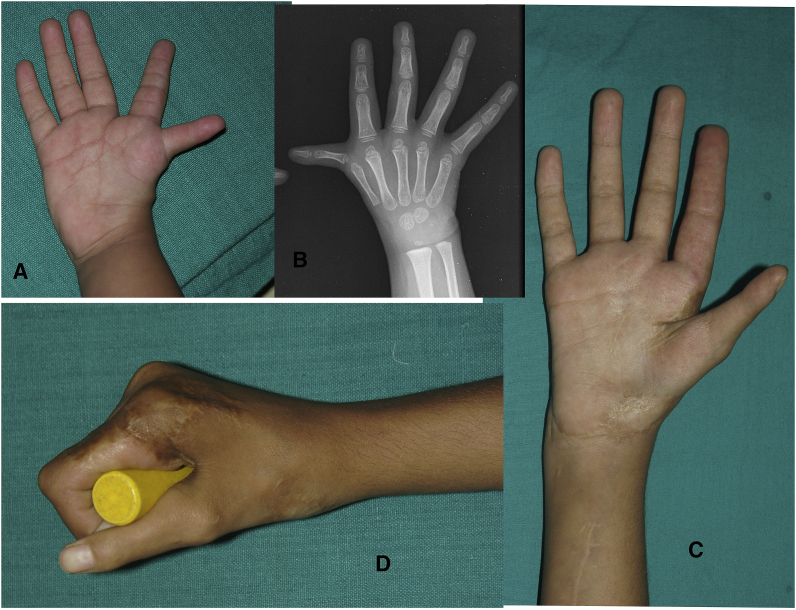
Fig. 2.
A. Preoperative photograph of a 12-year old child with Wassel Type IV duplication. Note that the radial element is much smaller than the radial one and can be removed for better function and cosmesis.
Fig. 2B. Radiographs of the thumb of the same patient as in Fig. 4 showing separate articulation of the two elements.
Fig. 2C. Intraoperative photograph showing removal of the radial element. The collateral ligament was attached to this part and was transferred to the retained segment. This is a very important step in the procedure.
Fig. 2D and E. Post-operative picture after ablation of the accessory segment.
Fig. 2F. The IP and MCP joints were transfixed with K-wires for healing of the wound and transferred collateral ligament.
Fig. 2G. Follow up composite picture of the patient 13 years after the primary surgery showing very good cosmesis and appearance of the thumb.
3.2. Clinical presentation
The presentation is usually obvious with the thumb appearing “split” in most cases with both the elements being smaller than the normal thumb. The size of the two elements maybe symmetric when both are the same size or asymmetric where one of the elements is bigger. Varying degrees of convergence or divergence of the split elements must be carefully noted. Type I and II can rarely present as a broad nail plate and the phalangeal anomaly is evident only on X-rays. Presence of flexion creases denotes active flexion in the segments and must be looked for. X-rays of the affected thumb identifies the type of duplication. Fig. 4, Fig. 5 shows a Wassel Type IV anomaly.
Fig. 4.
A & B. Photograph and X-ray appearance of the triphalangeal thumb in a 5-year old boy. Here the accessory phalanx is rectangular in shape. This was shortened and fused to the adjacent phalanx.
Fig. 5.
A &B. Preoperative photograph and X-ray of a three-year old child with right sided Type III hypoplastic thumb
Fig. 5C &D. Post-operative follow-up picture 8 years after multiple reconstructive procedures including thumb web release and dorsal sliding flap based on 1st dorsal metacarpal artery, ulnar collateral ligament reconstruction, metacarpal osteotomy and FDS opponensplasty. Note the good appearance and function. Patient also had closure of VSD and PDA at the age of 7.
3.3. Treatment
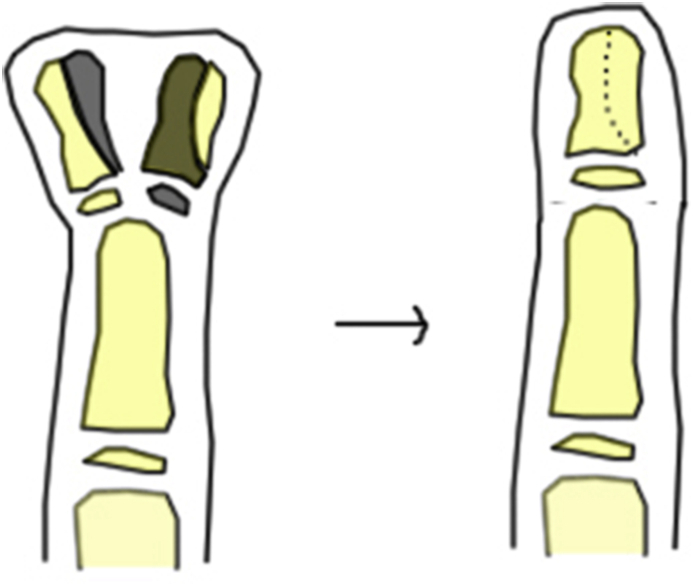
Surgical treatment aims at providing a cosmetically acceptable thumb of adequate size, ensuring that it is stable and also appropriately shaped (See Table 3). Surgery is preferably done around 1 year of age before the development of thumb to finger pinch. The procedures available are broadly categorized into 4 types16: 1) simple excision of the floating or severely hypoplastic segment, 2) reconstruction, where the larger segment is retained along with collateral ligament reattachment, augmentation of the retained segment with tissue from the excised segment, tendon reattachments etc, (Fig. 2C,D,E,F &G). (3)”on-top plasty” when one segment is adequate proximally while the nail and pulp is better on the other segment, 4) the Bilhaut -Cloquet (B–C) procedure17 and its modifications13,16,18,19. In the classic B–C procedure, the central parts of the duplicated segments is removed and the remaining part approximated by both bony fixation as well as tendon repair and skin closure. Duplications of similar size is more problematic as both segments are smaller than the normal thumb. The modifications of the original procedure attempt to improve the cosmesis and the range of motion of the MCP and IP joint (Fig. 3).
Table 3.
Recommended surgical reconstruction in various types of thumb duplication based on Wassels classification.
| Recommended surgical reconstruction | |
|---|---|
| Type of thumb | Surgery |
| Types I,III, V | Bilhaut Cloquet procedure (or modifications) in presence of angular deformity. In selected Type II also Bifid elements to be left to prevent angular deformity. Bifid elements removed at skeletal maturity. |
| Type II, IV, VI | Ablation of supernumerary thumb with collateral ligament reconstruction |
| Type VII | Ablation of triphalangeal thumb Retain biphalangeal thumb even when rudimentary |
Fig. 3.
Diagrammatic representation of the modified Bilhaut- Cloquet procedure used in reconstruction of Wassel type I,III and V thumb duplication (and selected Type II). The bony area shaded black in this diagram is removed and the fragments approximated.
The parents must be informed that the resultant thumb following reconstructive surgery will not be the same size as the normal one. The surgical treatment depends on the extend and size of the duplicated segment. Asymmetric types can be managed by ablation of the smaller segment and reconstruction of the collateral ligaments to provide stability. The extensor tendons is also centralized where necessary.
4. Triphalangeal thumb
The length of the “normal” thumb is widely variable between the proximal flexion crease and proximal interphalangeal joint crease of the index finger (when the thumb is adducted). Ninety percent of the adult population is reported to have a IP joint flexion crease of thumb corresponding with the distal palmar crease.20 Triphalangeal thumb (TPT) is a rare anomaly with an incidence of 1 in 25,000 live births 21where the thumb has three phalanges.22 It can present as isolated cases or as part of a syndrome such as Holt-Oram syndrome, or along with preaxial polydactyly and syndactyly. In 75% cases it is bilateral with family history of thumb anomalies. It can be inherited as autosomal dominant or may be sporadic. When associated with a syndrome, the thumb is usually hypoplastic.22 Two distinct types of TPT are seen, one with a fully developed extra phalanx, and another with the extra phalanx being wedge shaped, trapezoidal or rectangular in shape (Fig. 4A and B). In the former variant, the hand may appear as a “five fingered” hand with 1st web being narrowed and abduction restricted. There may be associated hypo/aplasia of the thumb musculature. Flexor tendons may have a superficialis and longus component at times. The epiphysis in the metacarpal can be present proximally, distally or both proximally. A wedge or trapezoidal extra phalanx, results in deviation of the thumb in the long axis.
4.1. Management
The management depends on the type of thumb anomaly on presentation. Milder forms with normal looking thumbs need no surgery. Best time for surgery is around the age of one. Milder deformities can be corrected later, before school going. Hovius et al. has described the following algorithm for the correction of TPT based on the anatomical variations. In children up to the age of 3 years, they advocate excision of the extra phalanx with plication of collateral ligaments on the convex side and V–Y advancement on the contracted side.22 In children older than 3 years, they recommend a distal interphalangeal reduction arthrodesis.
5. Thumb Hypoplasia
The normative values of a “normal” thumb is described as length in the adducted position, reaching up to 70% of the proximal phalanx of index, girth of 133% and nail width of 105% compared to the adjacent index finger.23 Underdeveloped thumb termed Thumb Hypoplasia (TH) can occur as a part of a broader spectrum of radial longitudinal deficiencies and also involving other organ systems or as an isolated anomaly. It can affect both the sides (20–60%) or may be unilateral. A number of well known syndromes are associated with thumb hypoplasia include Holt-Oram syndrome, VACTERL anomalies. Thrombocytopenia -Absent Radius (TAR) syndrome usually is associated with a broad flat thumb.
Children with TH will need to be assessed for these associations since it has bearing on the management, with specific precautions necessary in many situations, especially in Fanconis anemia, TAR syndrome and Holt Oram syndrome. The work up of this condition may require cardiac echo, renal ultrasound, spinal radiology and chromosome testing.
5.1. Clinical features
Minor degrees of hypoplasia may go unnoticed especially in early childhood, while more severe grades are obvious with definite functional impairment necessitating surgery.
Diagnosis is made after physical examination findings and appropriate X-Rays. The presence or absence of Intrinsic and Extrinsic muscles as well as stability of the MCP and CMC joints of the affected thumb greatly determine the plan of reconstruction.
The surgeon must be on the lookout for associated anomalies and syndromes and must take the help of a Paediatric specialist for identifying these situations.
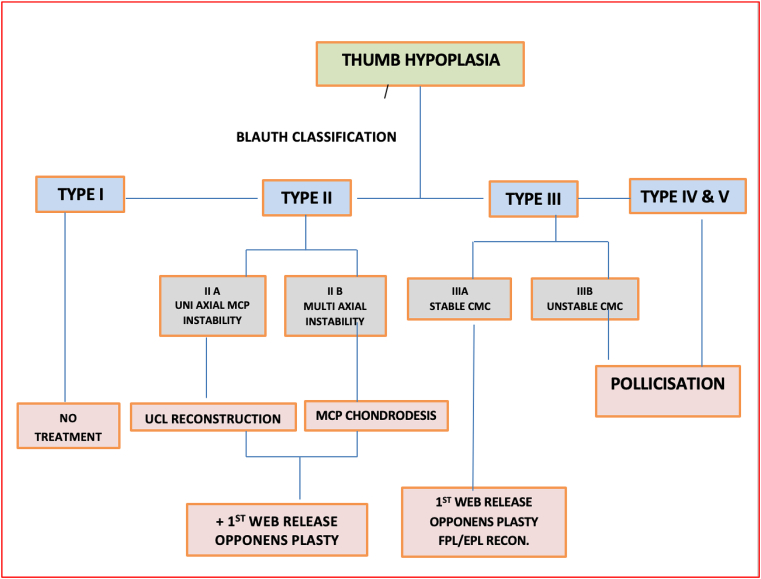
5.2. Classification and treatment
The original Blauth24 classification and modifications by Buck-Gramcko, Manske, Smith25,26 describes increasing dysplasia commencing from minimal hypoplasia to complete absence of the thumb. The modified Blauth classification assesses the degree of hypoplasia, associated anomalies and suggest possible treatment (See Table 4).
Table 4.
Classification and proposed surgical reconstruction of the hypoplastic thumb based on the Blauth classification.
| Type | Findings | Treatment |
| I | Minor generalized hypoplasia | No treatment |
| II | Absence of intrinsic thenar muscles First web space narrowing Ulnar collateral ligament (UCL) insufficiency
|
Opponensplasty First-web release
|
| III | Similar findings as Type II plus: Extrinsic muscle and tendon abnormalities Skeletal deficiency A: Stable carpometacarpal joint B: Unstable carpometacarpal joint |
A: Reconstruction B: Mostly Pollicization |
| IV | Pouce flottant, or Floating thumb | Pollicization |
| V | Absence | Pollicization |
Type I thumb shows mild hypoplasia with good stability and function. Type II hypoplasia has distinct findings that guide management. There is varying degrees of intrinsic thenar muscle deficiency, thumb web narrowing and laxity of the Ulnar Collateral Ligament (UCL) of the MCP joint. UCL laxity maybe due to attenuation because of a radially inserted FPL or an abnormal distal connection between EPL and FPL. It results in a thumb which appears abducted at the MCP joint and is referred to as pollex abductus. Type II is subdivided into IIA where the instability is uniaxial and II B where it is multiaxial. In Type III, there is extrinsic muscle involvement in addition to intrinsic muscle hypoplasia. It is subclassified as Type III A and B based on the stability of the 1st CMC joint. Radiographs to assess the 1st CMC joint before the age of 6 years is unreliable as the base of the 1st metacarpal and trapezium may not be ossified. The absence of the metacarpal flare and a tapering appearance of the metacarpal base suggests hypoplasia. An ultrasound helps to evaluate the CMC joint better.
5.3. Treatment
An algorithm for management of the different Blauth types is given in Table 5. The Type I hypoplastic thumb does not warrant surgical treatment.
Table 5.
Table 5. Algorithm in management of thumb hypoplasia.
Surgical reconstruction in type II and IIIA hypoplasia requires managing all the deficient elements. An algorithm for the treatment of Type II Blauth has been proposed by Smith et al..26 The narrowed thumb/index finger web space, MCP instability (uniaxial or multiaxial), and thenar muscle absence all require treatment (Fig. 5A and B,C & D).
Thumb/index finger web space narrowing is treated with skin rearrangement and soft tissue release. A four-flap “Z”-plasty lengthens the tight skin and provides a rounded contour to the web space. An extremely tight web space may also require partial release of the adductor pollicis muscle and/or first dorsal interosseous muscle to obtain adequate breadth. To avoid the development of “scissor pinch” between the index and middle finger, surgery is best done within the first 2 years of life.
Augmenting/providing metacarpophalangeal (MCP) joint stability may require strengthening or reconstruction of the Ulnar Collateral Ligament using locally available soft tissue or tendon graft in uniaxial instability pattern. and a MCP chondrodesis when multiaxial. The Snow-Fink transfer27 of FDS R to the abductor pollicis brevis muscle with an aperture made in the transverse carpal ligament as a pulley is useful in situations when the MCP joint is stable. In case of multiaxial instability an MCP joint chondrodesis provides stability and then opposition can be provided by a tendon transfer.
The main surgical options for providing opposition in a hypoplastic thumb include transfer of Flexor Digitorum Superficialis (FDS) of ring finger or the abductor digiti minimi muscle. The terminal portion of the FDS can also be used to reconstruct the ulnar collateral ligament of the MCP joint when it is deficient.28 The abductor digiti minimi ADM transfer for opponensplasty was first described by Huber in the 1920s and has been reported to be superior to the FDS transfer.29 In addition, it has been suggested that the appearance of the thenar eminence is also improved after an ADM opposition transfer as it provides additional bulk.
In case of Type III B, IV and V, the preferred option is a pollicization, where the index finger is transposed to form the thumb (Fig. 6, Fig. 7 A,B,C&D).
Fig. 6.
A,B,C, D. Preoperative and intraoperative photograph of a 4-year old child with Holt-Oram syndrome with Type IV hypoplastic thumb. She underwent ASD closure followed by centralization of the ulna at the age of 3. Filleting of the “poucce flottant “and pollicization was done 1 year later. Note the symphalangism in the digits including the index finger.
Fig. 7.
A, C. Preoperative and post operative photograph of a 2 year old child with bilateral radial club hand and Type IV hypoplastic thumb. The floating segment was previously removed along with centralization.
Fig. 7B and E. Preoperative and postoperative follow up radiographs of the child after pollicization.
Fig. 7D. Post-operative follow up photograph of the child 3 years after the pollicization.
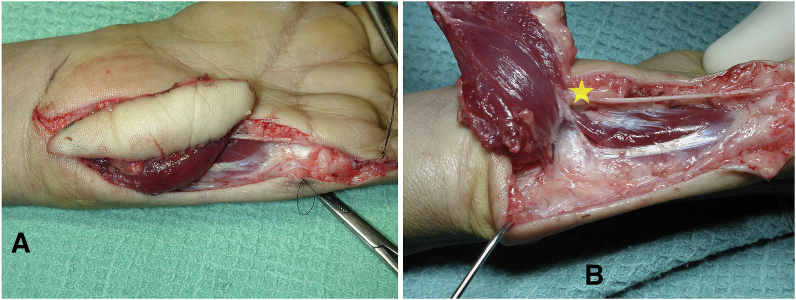
5.3.1. Huber transfer – surgical technique
A midlateral incision is made on the ulnar border of the little finger proximal phalanx and extended proximally and radially to the distal palmar crease. It then runs along the radial border of the hypothenar eminence and curves ulnarly as it crosses the distal wrist crease. The two ADM insertions (i.e., base of the proximal phalanx and extensor apparatus) are divided, and this muscle is then freed of soft tissue attachments by retrograde dissection toward its pisiform origin. When mobilizing the proximal portion of the ADM, great care must be taken to not damage its thin neurovascular pedicle, which is on its dorsoradial aspect (Fig. 8A and B).
Fig. 8.
A&B. Intraoperative photograph of a Huber’s transfer of the myo-cutaneous flap of abductor digiti minimi. Note the neurovascular bundle entering the deep aspect of the muscle (marked by the star).
Alternatively, this pedicle can be identified by exposing the ulnar nerve and artery proximally at the wrist and tracing them distally. Once the neurovascular bundle has been isolated, the transfer’s length is increased by elevating the abductor origin from the pisiform while carefully retaining an attachment on the FCU tendon by dissecting a tendinous slip proximally. The transfer’s only remaining soft tissue attachments are then its neurovascular pedicle and the FCU tendon. Next, a dorsoradial incision is made over the thumb MP joint and a wide subcutaneous tunnel is created between this incision and the area immediately proximal to the pisiform; this is easier if a third skin incision is made in the thenar crease at the base of the thenar eminence.
The ADM muscle is then turned through 180° on its long axis to reduce the tension on its neurovascular bundle (as if turning the page of a book), passed through the subcutaneous tunnel, and attached to the APB insertion. Because the ADM muscle has only sufficient length to just reach the APB insertion, it is invariably attached under adequate tension. Postoperatively, the thumb is immobilized in a cast in full opposition for 4 weeks. Fig. 9 is a composite picture showing the preop and post op photographs of a patient who underwent a Huber transfer.
Fig. 9.
A,B. Preoperative and intraoperative photographs of a child who underwent a myo-cutaneous Huber transfer for opposition in a Blauth Type III A thumb hypoplasia.
Fig. 9C&D. Postoperative follow up photographs showing the active abduction of the thumb and post-operative function after the Huber transfer.
Patients without a stable carpometacarpal joint, those with type IIIB, IV, or V thumb hypoplasia, are typically treated with pollicization30,30,31,32. In case of a type IIIB hypoplasia, it may be difficult to get the parents to consent for a removal of the hypoplastic thumb and then Index Pollicization. In such cases, reconstruction using Metatarsal (including the head) or Iliac Crest graft has been done.33
Index Pollicization provides for a satisfactory reconstruction of the Thumb that is severely hypoplastic (type IIIB, IV, or V thumb hypoplasia). The procedure is one of the most technically demanding procedures in Hand Surgery. An amalgamation of steps of pollicization described over many decades has been utilized to reach its current form. The skin incision must be designed to provide a generous 1st web after the pollicization. The length of the pollicized thumb must follow accepted standards of length. The head of the 2nd metacarpal is transferred and provides the reconstructed 1st CMC joint.
The actual procedure is too elaborate to be described here and readers are referred to excellent description of the technique by Kozin.34 In brief, the following points is to be noted.
-
•
Skin incision as described by Kozin.
-
•
Palmar skin is incised, and the radial neurovascular bundle is isolated
-
•
Dissection proceeds in an ulnar direction to identify the common digital vessels to the index finger/long finger web space
-
•
Proper digital nerves to the ulnar side of the index finger and the radial side of the long finger are isolated
-
•
Proper digital artery to the long finger is ligated
-
•
First annular pulley of the index finger is incised
-
•
Divide intermetacarpal ligament between index finger and long finger
-
•
Dorsal skin incision is sharply elevated with preservation of dorsal veins
-
•
The first dorsal and palmar interossei muscles are released with a portion of Kirschner wire drilled and used as a joystick to align the index metacarpal into 45° of abduction and 100–120° of pronation
-
•
Kirschner wire is driven retrograde across the metacarpal base into the carpus
-
•
Transfer the first dorsal interosseous to the radial lateral band and the first palmar interosseous to the ulnar lateral band about the PIP joint
-
•
Skin is closed with absorbable suture with resection of any redundant skin and Kirschner wire is cut short.
-
•
the hood
-
•
remaining metacarpal of index finger is shortened by a saw cut at the metaphyseal flare and a knife cut through the physis leading to an epiphysiodesis
-
•
Index metacarpophalangeal joint is fixed into hyperextension using nonabsorbable suture material passed through the epiphysis and dorsal capsule
Post-operatively, a spica cast is applied. K wire is removed at 4 weeks and a forearm based thermoplastic splint is to be used for about 3 months after surgery. Therapy is started with an aim on thumb usage. The initial goal is large object acquisition followed by acquisition of smaller objects and eventually fine pinch.
Pollicization has its fair share of complications35 with 10% cases developing venous congestion or marginal necrosis of skin that may necessitate intervention. One-third of patients have been reported to need further surgeries to improve rotational malalignment and extension.
6. Summary
Anomalies of the thumb range from total absence to duplication of the whole thumb. Management is best timed so that development of thumb function is not affected. Associated syndromes must always be looked for to prevent adverse events during surgical management.
Contributor Information
Binu P. Thomas, Email: binu@cmcvellore.ac.in.
Samuel Pallapati, Email: samuelpallapati@cmcvellore.ac.in.
References
- 1.Ladd A.L. The teleology of the thumb: on purpose and design. J Hand Surg. 2018;43(3):248–259. doi: 10.1016/j.jhsa.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fröbisch N.B., Carroll R.L., Schoch R.R. Limb ossification in the Paleozoic branchiosaurid Apateon (Temnospondyli) and the early evolution of preaxial dominance in tetrapod limb development. Evol Dev. 2007;9(1):69–75. doi: 10.1111/j.1525-142X.2006.00138.x. [DOI] [PubMed] [Google Scholar]
- 3.Oberg K.C. Review of the molecular development of the thumb: digit primera. Clin Orthop. 2014;472(4):1101–1105. doi: 10.1007/s11999-013-3008-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scott H Kozin. seventh ed. vol. 2. Elsevier; 2017. Embryology of upper extremity; pp. 1208–1217. (Green’s Operative Hand Surgery). [Google Scholar]
- 5.Slakey J.B., Hennrikus W.L. Acquired thumb flexion contracture in children: congenital trigger thumb. J Bone Joint Surg Br. 1996;78(3):481–483. [PubMed] [Google Scholar]
- 6.Kikuchi N., Ogino T. Incidence and development of trigger thumb in children. J Hand Surg. 2006;31(4):541–543. doi: 10.1016/j.jhsa.2005.12.024. [DOI] [PubMed] [Google Scholar]
- 7.Scott H Kozin. Paediatric hand. In: Green’s Operative Hand Surgery. Vol vol. 2. seventh ed. Elsevier; :1320-1323.
- 8.Dinham J.M., Meggitt B.F. Trigger thumbs in children. A review of the natural history and indications for treatment in 105 patients. J Bone Joint Surg Br. 1974;56(1):153–155. [PubMed] [Google Scholar]
- 9.Baek G.H., Kim J.H., Chung M.S., Kang S.B., Lee Y.H., Gong H.S. The natural history of pediatric trigger thumb. J Bone Joint Surg Am. 2008;90(5):980–985. doi: 10.2106/JBJS.G.00296. [DOI] [PubMed] [Google Scholar]
- 10.Lee Z.-L., Chang C.-H., Yang W.-Y., Hung S.-S., Shih C.-H. Extension splint for trigger thumb in children. J Pediatr Orthop. 2006;26(6):785–787. doi: 10.1097/01.bpo.0000235396.57160.f1. [DOI] [PubMed] [Google Scholar]
- 11.Manske M.C., Kennedy C.D., Huang J.I. Classifications in brief: the Wassel classification for radial polydactyly. Clin Orthop. 2017;475(6):1740–1746. doi: 10.1007/s11999-016-5068-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swanson A.B. A classification for congenital limb malformations. J Hand Surg. 1976;1(1):8–22. doi: 10.1016/s0363-5023(76)80021-4. [DOI] [PubMed] [Google Scholar]
- 13.Tonkin M.A. Thumb duplication: concepts and techniques. Clin Orthop Surg. 2012;4(1):1–17. doi: 10.4055/cios.2012.4.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wassel H.D. The results of surgery for polydactyly of the thumb. A review. Clin Orthop. 1969;64:175–193. [PubMed] [Google Scholar]
- 15.Zuidam J.M., Selles R.W., Ananta M., Runia J., Hovius S.E.R. A classification system of radial polydactyly: inclusion of triphalangeal thumb and triplication. J Hand Surg. 2008;33(3):373–377. doi: 10.1016/j.jhsa.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 16.Al-Qattan M.M., Kattan A.E., Al-Lazzam A., Gelidan A.G. A modified bilhaut–cloquet procedure for zigzag thumb polydactyly types III and IV. Plast Reconstr Surg Glob Open. 2017;5(12) doi: 10.1097/GOX.0000000000001589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maillet M., Fron D., Martinot-Duquennoy V., Herbaux B. Results after surgical treatment of thumb duplication: a retrospective review of 33 thumbs. J Child Orthop. 2007;1(2):135–141. doi: 10.1007/s11832-007-0019-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tonkin M.A., Bulstrode N.W. The bilhaut-cloquet procedure for Wassel types III, IV and VII thumb duplication. J Hand Surg Eur. 2007;32(6):684–693. doi: 10.1016/J.JHSE.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 19.Baek G.H., Gong H.S., Chung M.S., Oh J.H., Lee Y.H., Lee S.K. Modified bilhaut-cloquet procedure for Wassel type-II and III polydactyly of the thumb. J Bone Jt Surg. 2007;89(3):534–541. doi: 10.2106/JBJS.F.00812. [DOI] [PubMed] [Google Scholar]
- 20.Sunil T.M. Clinical indicators of normal thumb length in adults. J Hand Surg. 2004;29(3):489–493. doi: 10.1016/j.jhsa.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 21.Lapidus P.W., Guidotti F.P. Triphalangeal bifid thumb: report OF six cases. Arch Surg. 1944;49(4):228–234. doi: 10.1001/archsurg.1944.01230020236003. [DOI] [Google Scholar]
- 22.Hovius S.E.R., Potuijt J.W.P., van Nieuwenhoven C.A. Triphalangeal thumb: clinical features and treatment. J Hand Surg Eur. 2019;44(1):69–79. doi: 10.1177/1753193418797922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goldfarb C.A., Gee A.O., Heinze L.K., Manske P.R. Normative values for thumb length, girth, and width in the pediatric population. J Hand Surg. 2005;30(5):1004–1008. doi: 10.1016/j.jhsa.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 24.Blauth W., Schneider-Sickert F. Springer-Verlag; 1976. Congenital Deformities of the Hand: An Atlas of Their Surgical Treatment. [DOI] [Google Scholar]
- 25.Soldado F., Zlotolow D.A., Kozin S.H. Thumb hypoplasia. J Hand Surg. 2013;38(7):1435–1444. doi: 10.1016/j.jhsa.2013.03.021. [DOI] [PubMed] [Google Scholar]
- 26.Smith P., Sivakumar B., Hall R., Fleming A. Blauth II thumb hypoplasia: a management algorithm for the unstable metacarpophalangeal joint. J Hand Surg Eur. 2012;37(8):745–750. doi: 10.1177/1753193411432705. [DOI] [PubMed] [Google Scholar]
- 27.Yoon A.P., Jones N.F. The Snow-Fink technique as an opposition tendon transfer for children born with a hypoplastic or absent thumb. Handb Neuropsychol N. 2015;10(4):732–737. doi: 10.1007/s11552-015-9745-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kozin S.H., Ezaki M. Flexor Digitorum superficialis opponensplasty with ulnar collateral ligament reconstruction for thumb deficiency. Tech Hand Up Extrem Surg. 2010;14(1):46–50. doi: 10.1097/BTH.0b013e3181d4ed52. [DOI] [PubMed] [Google Scholar]
- 29.Littler J.W., Cooley S.G. Opposition OF the thumb and its restoration BY abductor digiti quinti transfer. J Bone Joint Surg Am. 1963;45:1389–1396. [PubMed] [Google Scholar]
- 30.Manske P.R., McCarroll H.R., James M. Type III-A hypoplastic thumb. J Hand Surg. 1995;20(2):246–253. doi: 10.1016/S0363-5023(05)80018-8. [DOI] [PubMed] [Google Scholar]
- 31.James M.A., McCarroll H.R., Manske P.R. Characteristics of patients with hypoplastic thumbs. J Hand Surg. 1996;21(1):104–113. doi: 10.1016/s0363-5023(96)80162-6. [DOI] [PubMed] [Google Scholar]
- 32.James M.A., Green H.D., McCarroll H.R., Manske P.R. The association of radial deficiency with thumb hypoplasia. J Bone Joint Surg Am. 2004;86(10):2196–2205. doi: 10.2106/00004623-200410000-00010. [DOI] [PubMed] [Google Scholar]
- 33.Tsujino A., Itoh Y., Hayashi K. Reconstruction of floating thumb by transplanting the fourth metatarsal. J Bone Joint Surg Br. 1994;76(4):551–554. [PubMed] [Google Scholar]
- 34.Kozin S.H. Pollicization: the concept, technical details, and outcome. Clin Orthop Surg. 2012;4(1):18–35. doi: 10.4055/cios.2012.4.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goldfarb C.A., Monroe E., Steffen J., Manske P.R. Incidence and treatment of complications, suboptimal outcomes, and functional deficiencies after pollicization. J Hand Surg. 2009;34(7):1291–1297. doi: 10.1016/j.jhsa.2009.04.001. [DOI] [PubMed] [Google Scholar]