Abstract
Background
Inadequate awareness and control remain the major obstacles for hypertension management worldwide. This observational study intended to assess the current status of hypertension management in Taiwan.
Methods
The Taiwan May Measurement Month (MMM) campaign was a nationwide survey for public alertness to hypertension initiated in 2017 and conducted in local pharmacies. Participants were asked about body habitus, comorbidities, smoking/drinking, use of anti-hypertensive drugs, and frequency of self-measured blood pressure (SMBP) monitoring. Three blood pressure (BP) readings were then measured by trained pharmacists. The mean BP was obtained by averaging all readings.
Results
BP recordings were obtained from 49,522 participants (average age, 56.9 ± 16.0 years), of whom 26.1% had an elevated pharmacist-measured BP (≥ 140/90 mmHg). The rate of BP control, defined as pharmacist-measured BP < 140/90 mmHg at the MMM visit, was 63.1% among treated hypertensive participants (n = 21,410). Participants who had uncontrolled hypertension were associated with a higher body mass index, currently smoking/drinking, diabetes, and stroke. More active SMBP monitoring (≥ weekly) was more often implemented in the participants with advanced age and cardiovascular diseases. More active SMBP (≥ weekly) was associated with lower measured BP among treated hypertensive participants but not overall control rate (control rate: 56.4% for ≥ weekly vs. 55.8% for < weekly, p = 0.363).
Conclusions
In the Taiwan MMM 2017, the hypertension control rate surpassed 60% in treated hypertensive participants. Suboptimal BP control was related to cardiovascular risk factors and prior stroke. Treated hypertensives had a lower measured BP but similar hypertension control rate for more active versus less active SMBP.
Keywords: Blood pressure monitoring, Control, Cross-sectional studies, Hypertension, Prevention
INTRODUCTION
Hypertension is a major burden for global healthcare systems. The high prevalence and related cardiovascular disabilities remain the center of discussion among different societies and guidelines. The overall prevalence of hypertension is around 20 to 30% in adults worldwide.1-3 There is also an increasing trend in the prevalence of hypertension in the Asia-Pacific region.4 This trend could be explained by aging, lifestyle changes and various pollution problems.5
Knowledge and self-awareness have been associated with better control of hypertension,6 whereas male sex, young age, and fewer healthcare visits have been associated with unawareness.7 Currently, diagnosis of hypertension is mainly based on office brachial blood pressure (BP) measurement, while completed with home or ambulatory BP measurement.8 Recently, non-invasive central BP measurement was proposed as a better tool for diagnosis and predicting target organ damage than brachial BP alone.9 However, it is still major concern that hypertension control is suboptimal worldwide, despite various diagnostic tools and treatment options.10 In view of this, global hypertension societies have taken action to promote better public awareness of elevated BP. The May Measurement Month (MMM) initiative was launched in 2017 with the purpose of screening the BP status of one million adult volunteers worldwide. Promotion sites were set up at various local facilities among more than 100 countries.11 Taiwan MMM was part of this global initiative, with goals to address the status quo of hypertension management in addition to BP screening. The first objective of this study was to explore possible associations between demographic factors and management behavior. The second objective was to evaluate the effect of more frequent self-measured blood pressure (SMBP) monitoring on pharmacist-measured BP during MMM visits.
METHODS
Taiwan MMM was carried out by the Taiwan Hypertension Society in 2017. The study protocol was approved by the Research Ethics Committee of National Taiwan University Hospital (No. 201704016RINA).
Local pharmacies in all regions of Taiwan were involved as screening sites. Adults aged 20 years or above were recruited. Participants signed informed consent before joining the study. They were asked about their body habitus, comorbidities and current use of tobacco or alcohol. Those who were recruited in six major cities were coded as metropolitans. They were also queried about the use of anti-hypertensive medications and the frequency of SMBP monitoring in the previous year. Trained pharmacists then performed BP measurements. The participants were required to sit quietly for 10 minutes beforehand. Left or right brachial BP was obtained using automated oscillometric sphygmomanometers. Three BP readings were taken with one minute between each reading. An average of all three BP readings was recorded.
For further analysis, the participants were categorized by each 10-year age period, and also trichotomized according to their body-mass index (BMI). All other demographic factors were categorical. Hypertension and related outcomes were defined as follows. Elevated BP was defined as mean systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg. Hypertension was defined as having elevated pharmacist-measured BP or being treated with anti-hypertensive drugs. Controlled hypertension was defined as pharmacist-measured BP below 140/90 mmHg at MMM visits. The frequency of SMBP monitoring was classified as one of the following: never, less than weekly, 1 to 3 times per week, 4 to 6 times per week, or daily. SMBP frequency was dichotomized as ≥ or < weekly for further analysis.
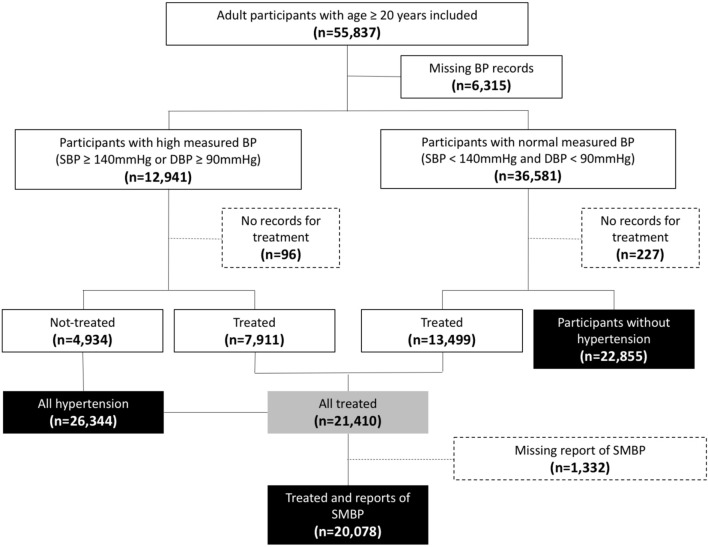
We processed data with Stata MP 14 (Statacorp, College Station, TX, USA). The study flowchart is shown in Figure 1. Hypertension control rate and SMBP frequencies were calculated among the treated hypertensive participants. For each demographic factor, the χ2 test and logistic regression were performed to identify significant determinants associated with controlled hypertension and more active SMBP monitoring (≥ weekly).
Figure 1.
Flowchart of all participants entering the study of Taiwan MMM 2017. BP, blood pressure; SMBP, self-measured blood pressure.
Finally, we used propensity score to assess whether SMBP monitoring ≥ weekly was related to pharmacist-measured BP and hypertension control rate among the treated hypertensive participants. We applied logistic regression to establish the score, which was matched for age, metropolitan area, smoking and cardiovascular diseases (factors significantly associated with SMBP frequency). One-to-one matching was performed with the nearest neighbor and without replacement. Actual differences in control rates were verified using the paired t-test.
RESULTS
Baseline characteristics of the participants in Taiwan MMM
A total of 55,837 volunteers were recruited from over 1,200 local pharmacies. All three BP readings were available or valid from a total of 49,522 participants. The average age was 56.9 ± 16.0 years, 49.2% of all participants were men, and 70.8% were metropolitans. Detailed demographic data are shown in Table 1.
Table 1. Demographic factors and comorbidities (all participants, N = 49,522).
| Age (mean ± SD) | 56.9 ± 16.0 |
| Men (n, %) | 24,188 (49.2) |
| Metropolitans* (n, %) | 35,066 (70.8) |
| Elevated blood pressures# (n, %) | 12,941 (26.1) |
| Hypertension† (n, %) | 26,440 (53.4) |
| Treated with anti-hypertensive drugs (n, %) | 21,409 (43.2) |
| Active smoking (n, %) | 8,735 (17.6) |
| Active drinking (n, %) | 2,543 (5.1) |
| Overweight (BMI ≥ 25 kg/m2) (n, %) | 19,252 (38.9) |
| Central obesity‡ (n, %) | 18,673 (37.7) |
| Diabetes mellitus (n, %) | 10,403 (21.0) |
| Coronary artery disease (n, %) | 5,361 (10.8) |
| Prior stroke (n, %) | 1,351 (2.7) |
BMI, body-mass index; SD, standard deviation.
* Defined as participants recruited at 6 major cities in Taiwan.
# Defined as pharmacist-measured systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg during the May Measurement Month visit. † Defined as elevated pharmacist-measured blood pressures or taking anti-hypertensive drugs. ‡ Men with waist circumference ≥ 90 cm or women with waist circumference ≥ 80 cm.
The average systolic BP increased with advancing age from 120 to 135 mmHg in men and 110 to 140 mmHg in women. The average diastolic BP peaked at 80 mmHg around the age of mid 50s for both men and women. Overall, 26.1% of the participants had elevated pharmacist-measured BP. The overall prevalence of hypertension was 53.4%. The male participants had a higher prevalence of elevated BP than the female participants (31.2% vs. 21.1%, p < 0.001). A higher BP was also observed in the participants who were taking anti-hypertensive medications, and in those with advanced age, higher BMI, currently smoking/drinking, diabetes, coronary artery disease (CAD) and prior stroke (all p < 0.001).
Control rates and SMBP monitoring frequencies among treated hypertensives
In the treated hypertensive participants, the mean systolic and diastolic BP values were 133.1 (±15.8) mmHg and 80.2 (±11.3) mmHg, respectively. Nearly two thirds (63.1%) of the treated hypertensives achieved control with a pharmacist-measured BP < 140/90 mmHg (Table 2). The control rate was similar among all age groups. Patients who were overweight, currently smoking/drinking, and those who had diabetes, coronary artery disease (CAD) or prior stroke were associated with lower hypertension control rates (all p < 0.001).
Table 2. Pharmacist-measured blood pressures, control rate, and frequency of self-measured blood pressure (SMBP) monitoring for treated hypertensives (n = 21,410).
| SBP, mmHg (mean ± SD) | 133.1 ± 15.8 |
| DBP, mmHg (mean ± SD) | 80.2 ± 11.3 |
| Controlled hypertension* (n, %) | 13,499 (63.1) |
| Coronary artery disease (n, %) | 4,560 (21.3) |
| Prior stroke (n, %) | 1,096 (5.1) |
| SMBP frequency# (n, %)† | |
| Never | 2,547 (12.7) |
| Less than weekly | 7,288 (36.3) |
| 1-3 times/week | 5,020 (25.0) |
| 4-6 times/week | 1,867 (9.3) |
| Daily | 3,356 (16.7) |
BMI, body-mass index; DBP, diastolic blood pressure; SBP, systolic blood pressure; SD, standard deviation; SMBP, self-measured blood pressure.
* Defined as averaged pharmacist-measured SBP < 140 mmHg and DBP < 90 mmHg during the May Measurement Month visit. # Percentages of all treated hypertensive participants who reported their SMBP frequencies; n = 20,078.
The characteristics of the treated hypertensives are shown in Table 2. Approximately half (49.0%) of the treated hypertensives had performed SMBP monitoring < weekly over the past year. A significant portion (42.3%) of the non-treated hypertensives did not perform SMBP at all. More hypertensive participants with advanced age, living in an urban area, diabetes, CAD or prior stroke performed SMBP ≥ weekly (all p < 0.001). The participants who were overweight or were currently smoking/drinking performed SMBP monitoring less frequently (p < 0.001 for smoking/drinking; p = 0.002 for overweight).
Logistic regression was used to determine the odds ratio of each demographic factor for hypertension control and active SMBP (≥ weekly) (Table 3). Worse control of hypertension was associated with metropolitans, higher BMI, currently smoking or drinking, diabetes and prior stroke. Those with advanced age, metropolitans, lower BMI, CAD and prior stroke had higher rates of active SMBP monitoring.
Table 3. Multivariate regression analyses for controlled hypertension and frequency of self-measured blood pressure monitoring ≥ weekly.
| Factors | Controlled hypertension | SMBP ≥ weekly† |
| Women (men as reference) | 1.06 (1.00-1.13) | 0.97 (0.92-1.04) |
| Age* (20-29 years as reference) | 0.99 (0.97-1.01) | 1.12 (1.09-1.15) |
| Metropolitan | 0.91 (0.85-0.97) | 1.29 (1.21-1.39) |
| Active smoking | 0.80 (0.74-0.86) | 0.86 (0.79-0.93) |
| Active drinking | 0.66 (0.58-0.75) | 0.89 (0.79-1.02) |
| BMI# (lowest tertile as reference) | 0.85 (0.82-0.88) | 0.93 (0.90-0.97) |
| Diabetes mellitus | 0.68 (0.64-0.72) | 1.01 (0.95-1.08) |
| CAD | 0.94 (0.87-1.01) | 1.13 (1.05-1.21) |
| Prior stroke | 0.79 (0.69-0.91) | 1.16 (1.02-1.33) |
BMI, body-mass index; CAD, coronary artery disease; SMBP, self-measured blood pressure.
Data shown are odds ratio (95% confidence interval).
* Each 10-year increment. # Each tertile increment. † Defined as performing self-measured blood pressure monitoring at least weekly in the previous year.
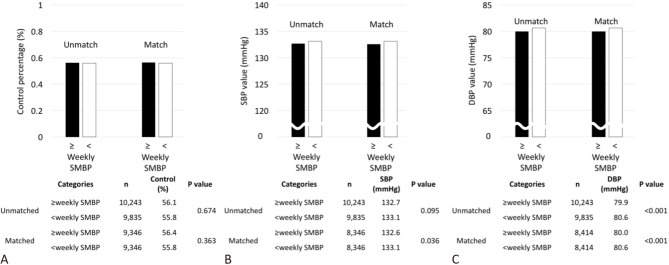
Among the treated hypertensive participants matched by propensity score, there were no differences in hypertension control rates based on pharmacist-measured BP between the patients who monitored SMBP ≥ weekly and those who monitored SMBP < weekly (56.4% for ≥ weekly vs. 55.8% for < weekly, p = 0.363). Nonetheless, the participants who monitored SMBP ≥ weekly had lower measured BP compared to those who monitored SMBP < weekly (systolic BP: 132.6 mmHg for ≥ weekly vs. 133.1 mmHg for < weekly, p = 0.036; diastolic BP: 80.0 mmHg for ≥ weekly vs. 80.6 mmHg for < weekly, p < 0.001) (Figure 2).
Figure 2.
Propensity-score matching of actual BP difference and percentages of hypertensives under control. DBP, diastolic blood pressure; SBP, systolic blood pressure; SMBP, self-measured blood pressure.
DISCUSSION
The control rates in this study were higher than 60% for treated hypertensives, which is higher than previous domestic studies.12,13 On the other hand, almost half (49.0%) of all treated hypertensive participants reported SMBP frequencies < weekly in the previous year. Hypertension control was worse in those who lived in urban areas, those with a higher BMI, currently smoking and drinking, diabetes and prior stroke. SMBP monitoring was better implemented in the treated hypertensive participants with advanced age, living in urban areas, and prior cardiovascular diseases. Weekly or more frequent SMBP monitoring was associated with lower measured BP but not with a better control rate of hypertension at MMM visits.
The reported prevalence of hypertension among participants in Taiwan was higher than that in the other geographical regions in the global MMM campaign (unadjusted prevalence, Taiwan 53.4% vs. global 34.6%).14 Several reasons may account for this finding. First, our recruited participants had an average age of 56.9 (±16.0) years, while the global MMM reported an average age of 44.9 (±16.9) years. Second, more individuals had cardiovascular diseases in the Taiwan MMM. This is not surprising given that circulatory diseases are the most common diagnosis for medical visits based on Taiwan National Health Insurance data.15 Both advanced age and more cardiovascular comorbidities may contribute to the higher percentage of hypertension.
Young age was associated with suboptimal self-monitoring of blood pressure in this study. Previous studies have reported that young adults are less aware of hypertension, mainly because of subjective well-being.16 Nonetheless, they will be exposed to certain subclinical organ damage with an elevated BP.17 This study also found a similar hypertension control rate across all age groups. We speculate that hypertensives, regardless of age, generally follow health advices once they opt for medical therapy. Old age was inevitably associated with elevated BP, which may have diminished the advantage of better treatment compliance.
The relationship between gender and hypertension was complex. For participants younger than 65 years of age, men had a higher prevalence of hypertension than women (50.5% vs. 34.3%). This disparity decreased in the participants older than 65 years (75.0% vs. 72.6%). The higher BP in younger men may be due to gender differences in renal-mediated BP regulation. In addition, previous studies have suggested that "masculine behavior" may cause a delay in seeking medical attention, and that this could lead to less active treatment among male hypertensives.18 However, there were no significant difference in gender regarding control and SMBP, suggesting similar compliance once under medical treatment.
We found that more active SMBP behavior but worse control rates were concomitantly associated with metropolitans. Inferior control of hypertension in the metropolitans may be the result of diet, lifestyle and pollution problems.19 More frequent SMBP monitoring associated with metropolitans may reveal higher health awareness and proximity to medical care.
Higher BMI, currently smoking and drinking are all risk factors for elevated BP. Overweight subjects are prone to have a blunted response to subjective health status.20 Thus, the participants with a higher BMI had a lower control rate and less frequent SMBP monitoring. Currently smoking and drinking were correlated with inferior hypertension control and SMBP at MMM visits. As Org et al. and Gooding et al. reported, patients with more unhealthy behaviors care less about subjective well-being.17,21 This may have led to a generally lower control rate and less frequent SMBP monitoring.
The participants with diabetes and stroke were associated with more active SMBP monitoring but worse BP control. As most practicing physicians nowadays adjust medications based on self-measured BP results, participants with cardiovascular diseases or diabetes may have already received instructions to perform SMBP.22 In addition, those with worse control and co-existing cardiovascular diseases may have received more stringent BP measurement instructions. Our study showed that history of CAD is in favor but not predictive of worse BP control. Physicians use more angiotensin converting enzyme inhibitors, angiotensin receptor blockers or even aldosterone receptor blockers to treat participants with CAD, which all contribute to effective BP reduction.23
Lastly, the participants with weekly or more SMBP monitoring were not associated with more controlled hypertension than less active matched counterparts. Although there was an actual BP difference between the two groups, the magnitude was lower than expected.24,25 SMBP monitoring can provide a more realistic overview of daytime BP with lower cost and higher convenience. Previous studies have reported the importance of SMBP in improving awareness, and that persistently abnormal home BP results may lead to an adverse prognosis. We speculate that hypertension control could still be linked with yet unknown social or educational factors in addition to monitoring. For instance, remote monitoring with timely feedback, upcoming digital applications, or evolving patient-physician interactions may all have the potential to improve BP control and SMBP behavior.
Our study has some limitations. First, the Taiwan MMM study was cross-sectional in nature. This precluded the ability to infer causal relationships between SMBP performance and measured differences in BP for the same individual. Second, all participants were recruited at local pharmacies. This could have resulted in selection bias. Finally, we did not include additional factors regarding treatment behavior, such as income status, educational level or polypharmacy. These factors are expected to affect awareness and compliance to hypertension treatment.
CONCLUSIONS
This study reports the latest picture of hypertension management in Taiwan. The control rate for treated hypertensives exceeded 60% in this study. Control of hypertension was worse in metropolitans and those with diabetes, higher BMI, currently smoking or drinking, and prior stroke. More active SMBP monitoring was correlated with advanced age, living in a metropolitan area, CAD and prior stroke, but not with more controlled hypertension.
CONFLICT OF INTEREST
All the authors declare no conflict of interest.
REFERENCES
- 1.Kim KI, Chang HJ, Cho YS, et al. Current status and characteristics of hypertension control in community resident elderly Korean people: data from a Korean longitudinal study on health and aging (KLoSHa study). Hypertens Res. 2008;31:97–105. doi: 10.1291/hypres.31.97. [DOI] [PubMed] [Google Scholar]
- 2.Lu FH, Tang SJ, Wu JS, et al. Hypertension in elderly persons: its prevalence and associated cardiovascular risk factors in Tainan City, southern Taiwan. J Gerontol A Biol Sci Med Sci. 2000;55:M463–M468. doi: 10.1093/gerona/55.8.m463. [DOI] [PubMed] [Google Scholar]
- 3.Malhotra R, Chan A, Malhotra C, Ostbye T. Prevalence, awareness, treatment and control of hypertension in the elderly population of Singapore. Hypertens Res. 2010;33:1223–1231. doi: 10.1038/hr.2010.177. [DOI] [PubMed] [Google Scholar]
- 4.Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jin CN, Yu CM, Sun JP, et al. The healthcare burden of hypertension in Asia. Heart Asia. 2013;5:238–243. doi: 10.1136/heartasia-2013-010408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang X, Zhu M, Dib HH, et al. Knowledge, awareness, behavior (KAB) and control of hypertension among urban elderly in western China. Int J Cardiol. 2009;137:9–15. doi: 10.1016/j.ijcard.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Paulose-Ram R, Gu Q, Kit B. Characteristics of U.S. adults with hypertension who are unaware of their hypertension, 2011-2014. NCHS Data Brief. 2017:1–8. [PubMed] [Google Scholar]
- 8.Chiang CE, Wang TD, Ueng KC, et al. 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension. J Chin Med Assoc. 2015;78:1–47. doi: 10.1016/j.jcma.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 9.Cheng HM, Chuang SY, Sung SH, et al. 2019 Consensus of the Taiwan Hypertension Society and Taiwan Society of Cardiology on the clinical application of central blood pressure in the management of hypertension. Acta Cardiol Sin. 2019;35:234–243. doi: 10.6515/ACS.201905_35(3).20190415B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–968. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 11.Poulter NR, Lackland DT. May Measurement Month: a global blood pressure screening campaign. Lancet. 2017;389:1678–1680. doi: 10.1016/S0140-6736(17)31048-6. [DOI] [PubMed] [Google Scholar]
- 12.Su TC, Bai CH, Chang HY, et al. Evidence for improved control of hypertension in Taiwan: 1993-2002. J Hypertens. 2008;26:600–606. doi: 10.1097/HJH.0b013e3282f3b352. [DOI] [PubMed] [Google Scholar]
- 13.Pan WH, Chang HY, Yeh WT, et al. Prevalence, awareness, treatment and control of hypertension in Taiwan: results of Nutrition and Health Survey in Taiwan (NAHSIT) 1993-1996. J Hum Hypertens. 2001;15:793–798. doi: 10.1038/sj.jhh.1001268. [DOI] [PubMed] [Google Scholar]
- 14.Beaney T, Schutte AE, Tomaszewski M, et al. May Measurement Month 2017: an analysis of blood pressure screening results worldwide. Lancet Glob Health. 2018;6:e736–e743. doi: 10.1016/S2214-109X(18)30259-6. [DOI] [PubMed] [Google Scholar]
- 15.Hsu WC, Hsu YP. Patterns of outpatient care utilization by seniors under the National Health Insurance in Taiwan. J Formos Med Assoc. 2016;115:325–334. doi: 10.1016/j.jfma.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Zhang Y, Moran AE. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension. 2017;70:736–742. doi: 10.1161/HYPERTENSIONAHA.117.09801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gooding HC, McGinty S, Richmond TK, et al. Hypertension awareness and control among young adults in the national longitudinal study of adolescent health. J Gen Intern Med. 2014;29:1098–1104. doi: 10.1007/s11606-014-2809-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galdas PM, Cheater F, Marshall P. Men and health help-seeking behaviour: literature review. J Adv Nurs. 2005;49:616–623. doi: 10.1111/j.1365-2648.2004.03331.x. [DOI] [PubMed] [Google Scholar]
- 19.Yang F, Qian D, Liu X. Socioeconomic disparities in prevalence, awareness, treatment, and control of hypertension over the life course in China. Int J Equity Health. 2017;16:100. doi: 10.1186/s12939-017-0597-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Musich S, MacLeod S, Bhattarai GR, et al. The impact of obesity on health care utilization and expenditures in a medicare supplement population. Gerontol Geriatr Med. 2016;2:2333721415622004. doi: 10.1177/2333721415622004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Org E, Veldre G, Viigimaa M, et al. HYPEST study: profile of hypertensive patients in Estonia. BMC Cardiovasc Disord. 2011;11:55. doi: 10.1186/1471-2261-11-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jackson SL, Ayala C, Tong X, Wall HK. Clinical implementation of self-measured blood pressure monitoring, 2015-2016. Am J Prev Med. 2019;56:e13–e21. doi: 10.1016/j.amepre.2018.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Attar A, Sadeghi AA, Amirmoezi F, Aghasadeghi K. Low dose spironolactone monotherapy in the management of stage I essential hypertension: a pilot randomized, double-blind, placebo-controlled trial. Acta Cardiol Sin. 2018;34:59–65. doi: 10.6515/ACS.201801_34(1).20170903B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tucker KL, Sheppard JP, Stevens R, et al. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS Med. 2017;14:e1002389. doi: 10.1371/journal.pmed.1002389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Uhlig K, Patel K, Ip S, et al. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med. 2013;159:185–194. doi: 10.7326/0003-4819-159-3-201308060-00008. [DOI] [PubMed] [Google Scholar]