Abstract
Background.
Eating disorders (EDs) are serious mental illnesses that can be life-threatening. Stage of illness models and early intervention strategies could be informed by a better understanding of symptomatology that precedes the onset of an ED. This review aims to explore which symptoms (both ED and other psychiatric disorder-related) exist prior to the onset of an ED and whether there any prospective associations between these symptomatologies.
Methods.
A systematic literature review was conducted in MEDLINE, Embase, and PsycINFO for large, longitudinal, prospective studies in nonclinical cohorts of children/adolescents that report symptoms prior to the onset of an ED. A quality assessment of included studies was conducted using the Newcastle-Ottawa Quality Assessment Scale.
Results.
A total of 22 studies were included, and over half were assessed to be of good quality. Studies identified the presence of a broad range of ED and other psychiatric disorder-related symptoms prior to ED onset. Possible prospective associations were identified, including early eating and feeding difficulties in childhood, to ED-related symptoms (e.g., dieting and body dissatisfaction) and other psychiatric disorder-related symptoms (e.g., anxiety and depression) in childhood/early adolescence, progressing to severe symptomatology (e.g., extreme weight control behaviors and self-harm) in mid-adolescence/emerging adulthood.
Conclusion.
The trajectory of symptoms identified to precede and possibly predict onset of an ED may inform early intervention strategies within the community. Suggestions for further research are provided to establish these findings and the clinical implications of these discussed, in order to inform how best to target prodromal stages of EDs.
Key words: Child and adolescent psychiatry, comorbidity, early intervention, eating disorder, psychiatric symptoms
Introduction
The eating disorders (EDs) anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorder (BED) are characterized by aberrant eating patterns, significant psychopathology, distress, and/or impairment [1]. While disordered eating behaviors and cognitions have been reported in up to 48% of adolescents of either sex and up to 64% of female adolescents [2], full syndromal EDs affect around 8% of women and 2% of men in their lifetime. These disorders are associated with a range of physical [3] and mental health comorbidities [4,5], elevated mortality rates [6], and are difficult to treat [7]. Furthermore, EDs typically arise in early/mid-adolescence, last around 5–8 years [8,9], and are thought to be increasing in prevalence [10]. This means that they persist across the transition between adolescence and early adulthood [11], a crucial period of biopsychosocial development. As such, understanding the trajectory of symptoms leading to the onset of an ED is critical for the development of effective prevention and early intervention strategies.
Prevention and early intervention strategies are particularly pertinent given suggestions that neuroprogression may make symptoms more entrenched and less amenable to intervention over time [12]. A large body of research has evaluated preventative approaches for EDs, and selective prevention programs (i.e., those that target high-risk individuals/groups) have been shown to be most effective in reducing a range of psychopathology (e.g., body dissatisfaction, negative affect, and self-esteem[13,14]). These preventative approaches are informed by risk factor-related research. By definition, a risk factor is a measurable characteristic that precedes and increases the probability of the development of the outcome of interest [15]. In their seminal review, Jacobi et al. [16] identified a number of putative biological (e.g., gender and ethnicity), behavioral (e.g., early eating difficulties and dieting), psychological (e.g., body image difficulties and negative affect), and social (e.g., adverse experiences such as sexual abuse/physical neglect) risk factors for EDs. Recent research has added to these findings by exploring risk factors for EDs in relation to the more encompassing Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria and found that self-objectification was the largest contributor to ED onset in young women [17]. Recently, there has also been increased interest in and evidence for genetic risk factors of EDs, which has led to the identification of specific loci for AN [18].
While many recognized risk factors for EDs may be useful in identifying, targeting, and possibly preventing EDs in those at risk of developing an ED, some of these features could also be considered as representing the early stages of—or progression into—an ED. Indeed, an at-risk state for EDs has been distinguished from a defined prodromal stage, the latter differentiated by the presence of symptoms that are features of the full disorder and indicate ED onset [12,19]. Therefore, behavioral and psychological ED risk factors (e.g., dieting and body dissatisfaction) that exist prior to ED onset may constitute ED prodromes, while biological, genetic, and environmental risk-factors (e.g., sex, early puberty, familial history, maternal factors, and adverse events) merely render an individual more susceptible to developing an ED.
An enhanced understanding of ED prodromes could inform stage of illness models of EDs and further improve emerging early intervention strategies which have shown important clinical outcomes (i.e., quick and lasting weight restoration in AN [20,21]). Indeed, the utility of exploring, defining, and treating prodromal stages of illness has been demonstrated across other psychiatric disorders [22–24]. In particular within the field of psychosis, delineation of prodromal stages [25–31] has led to interventions and services specific to this early illness phase that demonstrate significant clinical and economic impact [29,32–36]. Unfortunately, little analogous research has been conducted in relation to EDs, and very few cross-sectional, retrospective studies exist.
Given such limited research, an improved understanding of symptomatology prior to the onset of an ED that may constitute a prodromal phase is warranted. Longitudinal research in nonclinical populations of children/adolescents reporting symptomatology, as delineated in the DSM, prior to the onset of EDs could provide such initial insights. While there are many relevant existing studies, there has yet to be a systematic review of this literature or a consideration of how these findings may inform our understanding of early, prodromal stages of illness in EDs.
The current study aims to explore symptom development prior to the onset of EDs. Specifically, this review aims to address the following two questions in relation to nonclinical, adolescent populations: Which psychiatric disorder-related symptomatology exists prior to the onset of an ED? and are there any prospective associations between these symptoms?
Methods
Search strategy
A systematic review was conducted following the recommendations outlined in the PRISMA guidance [37]. The protocol for this systematic review was registered on PROSPERO (May 01, 2018; registration number: CRD42018094441) and is available on the PROSPERO website (http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018094441).
Relevant studies were identified using three electronic databases (MEDLINE, Embase, and PsycINFO) and searched (via OvidSP) from inception until the date search carried out (March 05, 2020). Following are the key search terms: (eating disorder* OR anorexi* OR bulimi* OR binge eating; title/abstract) AND (cohort* OR longitudinal OR prospective; title/abstract) AND (symptom* OR behavio*; title/abstract).
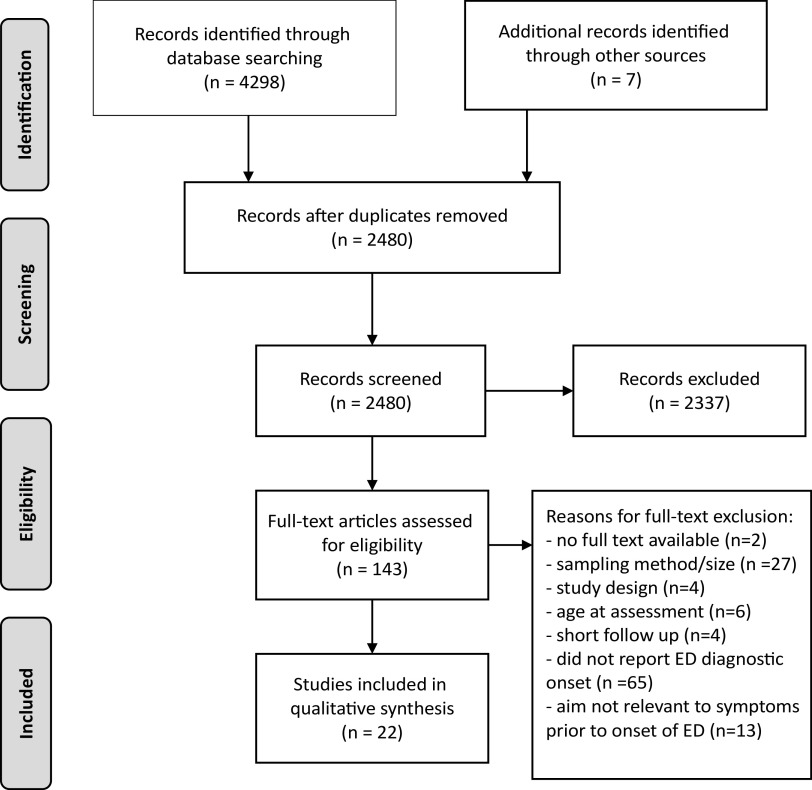
These searches were supplemented with Internet and hand-searches of reference lists. All identified articles were screened and included based on relevance to the topic via inspection of their title and abstract. The full text versions of the remaining articles were then assessed in more detail. An overview of the literature search is shown in Figure 1. Reviewers (J.M., L.R., and R.P.) conducted each stage of the literature search independently, and any disagreements were resolved by further examination, discussion, and via consensus.
Figure 1.
PRISMA flow chart of literature search and reviewed studies.
Inclusion criteria
We included articles in English, dated from the earliest date available up until the date the search was carried out (March 05, 2020) that aimed to explore the course/development of ED and other psychiatric disorder-related symptoms prior to the onset of an ED diagnosis including AN, BN, BED, and eating disorder not otherwise specified (EDNOS), and other specified feeding and eating disorders (OSFED). To be included in the review, studies were required to be large (N ≥ 100), nonclinical, population-based samples of children/adolescents (i.e., baseline assessments at 17 years of age or younger) who were followed prospectively for at least 12 months and which assessed onset of subclinical and full ED diagnoses (DSM or International Classification of Diseases-based criteria). Studies which investigated ED symptoms, without clinical or subclinical diagnoses, were not included in this review. Only studies to investigate the relation between symptoms of EDs and other psychiatric disorders, as listed in DSM and future onset of clinical or subclinical EDs, were included in this review. Behavioral and psychological ED risk factors (e.g., dieting and body dissatisfaction) that exist prior to ED onset thus have remained within the remit of this review.
Reviewers (J.M., L.R., and R.P.) extracted data from studies regarding sample characteristics, study design, and relevant findings. These reviewers also assessed the quality of each study, with discrepancies discussed and agreed upon following consultation with experts from the research group. The quality of included studies was appraised using the Newcastle-Ottawa Quality Assessment Scale (NOS) for cohort studies [38]. This scale was developed to assess the quality of nonrandomized studies in systematic reviews and meta-analyses. The NOS judges study quality on eight items from three broad criteria—the selection of the study groups, comparability of the groups, and the ascertainment of the outcome of interest. A maximum score of 9 can be given to a study and thresholds for converting the NOS to Agency for Healthcare Research and Quality [39] standards are as follows—“Poor”: selection ≤ 1 OR comparability = 0 OR outcome/exposure ≤ 1; “Fair”: selection = 2 AND comparability ≤ 2 AND outcome/exposure ≤ 3; “Good”: selection ≤ 4 AND comparability ≤ 2 AND outcome/exposure ≤ 3.
Results
Characteristics of included studies
We identified 22 studies (see Table 1) that met inclusion criteria for this review, and percentage agreement between reviewers for inclusion was 100%. These 22 studies included 56,164 participants from 15 cohorts across 6 countries. On average, individuals were 12 years of age at initial assessment (exclusion of two birth cohorts that did not report age at assessment), 49% male (aside from one female only study), and were followed up for a period of 8 years (minimum = 1.5 years; maximum = 30 years). In terms of the age at which studies assessed symptoms prior to ED onset, 2 out of 22 studies followed individuals from birth, 4 out of 22 began during childhood, and most studies (16/22) followed adolescents (i.e., between 12 and 17 years of age). Studies determined and reported ED onset through self-report (8/22), validated questionnaires (8/22), and/or interview measures (7/22) based on DSM-III-R, DSM-IV, or DSM-5 diagnostic criteria. A combination of full and partial/subthreshold ED diagnoses were investigated—most studies investigated full threshold ED cases (14/22), with others investigating a combination between full and subthreshold/partial EDs (8/22).
Table 1.
Characteristics and findings of reviewed studies.
| References | Country | N | Cohort | Age (M ± SD) | Gender | Follow-up | ED diagnosis | ED diagnostic threshold | Findings | Quality |
|---|---|---|---|---|---|---|---|---|---|---|
| Ackard et al. [40] | United States | 2,516 | Project EAT-II; 31 schools | 20.4 ± 0.8 at follow-up | 45% male | 5 years | Self-report questions re: ED criteria (DSM-IV) | Full threshold ED cases | 2.2% males and females with body image disturbance developed BED or BN. 0.9% of males and 3.7% of females with binge eating or compensatory behaviors developed BED, or BED and BN, respectively. | Poor |
| Allen et al. [41] | Australia | 1,597 | Raine study; birth cohort | 14.1 ± 0.1 at follow-up | 55% male | 14 years | Adapted child EDE and EDEQ (DSM-IV) | Full, partial, and “at risk” ED cases | A restricted diet predicted later ED cases. | Good |
| Beato-Fernandez et al. [42] | Spain | 1,076 | 22 schools | 12–13 at baseline | 46% male | 2 years | EAT-40 (DSM-III-R/IV) | Full (AN, BN) and EDNOS cases | Body dissatisfaction predicted later ED diagnosis. Those who developed an ED had more suicidal and self-harm tendencies, worse depressive symptoms, and body dissatisfaction at baseline. | Poor |
| Herle et al. [43] | United Kingdom | 4,760 | ALSPAC | 1.3 at baseline | 52% male | 8.7 years | Data from YRBSSQ and DEBQ (DSM-5) | Full threshold ED cases | Childhood overeating, persistent undereating, and persistent fussy eating were predictive of adolescent binge eating disorder, anorexia nervosa (girls only), and anorexia nervosa (whole sample), respectively. | Good |
| Johnson et al. [44] | United States | 726 | Families from two NY counties | 13.8 ± 2.6 at baseline | 49% male | 10 years | DISC-I (DSM-III-R) | Full Threshold ED cases and ED behaviors | Depressive and anxiety disorders were predictive of EDs. Disruptive and substance use disorders were not predictive of EDs. | Good |
| Killen et al. [45] | United States | 887 | 4 schools | 12.4 ± 0.7 at baseline | All female | 3 years | Self-report questions (diagnostic tool not reported) | Full and partial ED cases | Elevated weight concerns associated with onset of partial EDs. Earlier drive for thinness, body dissatisfaction, perfectionism, and restraint most characteristic of those who later develop partial EDs | Poor |
| Killen et al. [46] | United States | 825 | 4 schools | 14.9 at baseline | All female | 4 years | Interview and adapted EDE (DSM-III-R) | Full and partial ED cases | Elevated weight concerns associated with onset of partial EDs. Earlier drive for thinness, bulimia, body dissatisfaction, ineffectiveness, interoceptive awareness, temperament (distress, fear), dieting, restraint, and alcohol use most characteristic of those who later develop partial EDs. | Good |
| Kotler et al. [47] | United States | 976 | Families from two NY counties | 6.1 at baseline | 50% male | 17 years | DISC (DSM-III-R/IV) | Full threshold ED cases and ED behaviors | Eating conflicts, struggles with food and unpleasant meals predicted AN. | Good |
| Liechty and Lee [48] | United States | 14,322 | Add Health; 80 high schools | 15.9 ± 1.8 at baseline | 49% male | 7 years | Self-report (ever told have an ED? yes/no) | Implied full threshold ED cases | Depression, body image dissatisfaction (males only), and extreme weight loss behaviors (females only) was associated with unspecified ED diagnosis. | Good |
| Marchi and Cohen [49] | United States | 659 | 9 schools | ~6 years at baseline | 51% male | 10 years | DISC (DSM-III-R) | Full threshold ED cases | Risks in early childhood for subsequent symptoms of anorexia nervosa include picky eating and digestive problems. Early symptoms of AN/BN predictive of later diagnosis and pica predictive of BN. |
Good |
| Neumark-Sztainer et al. [50] | United States | 2,516 | Project EAT-II; 31 schools | 12.8/15.8 ± 0.8 at baseline | 45% male | 5 years | Self-report (ever told have an ED? yes/no) | Implied full threshold ED cases and ED behaviors | In females, dieting significantly associated with later EDs. | Poor |
| Nicholls and Viner [51] | United Kingdom | 16,567 | BCS70; birth cohort | From birth | 56% male | 30 years | Self-report (ever told have an ED? yes/no) | Implied full threshold ED cases | Infant feeding problems, under eating, and increased exercise (at 10 years) associated with later AN. | Poor |
| Nicholls et al. [52] | United Kingdom | 16,567 | BSC70; birth cohort | From birth | 49% male | 30 years | Self-report (ever told have an ED? yes/no) | Implied full threshold ED cases | Eating, sleep problems, and overeating (5 years) associated with later BN/BED. | Poor |
| Patton et al. [53] | Australia | 1,947 | 45 schools | 14.5 ± 0.5 at baseline | 47% male | 3 years | BET (DSM-IV) | Full and partial syndrome ED cases | In females, severe and moderate dieting increased risk of future ED. Psychiatric morbidity (independent of dieting) predicted onset of EDs. | Poor |
| Penas-Lledo et al. [54] | Sweden | 615 | TChAD; Twin study | 16–17 years at baseline | All female | 3 years | Self-report (ever had BN or AN? Yes/no) | Implied full threshold ED cases | Drive for thinness predicted later BN. Interaction between drive for thinness and anxious/depressed mood predicted risk of both BN and AN. | Poor |
| Ranta et al. [55] | Finland | 3,278 | Finnish Adolescent Mental Health Cohort Study | 15.5 ± 0.4 at baseline | 51% male | 2 years | Self-report questions re: ED criteria (DSM-IV-TR) | Implied full threshold ED cases | Depression predicted AN, while social phobia and depression both predicted BN. However, controlling for initial comorbidity, Eds, and socioeconomic factors removed this effect. | Poor |
| Schaumberg et al. [56] | United Kingdom | 7,767 | ALSPAC | 10 years | Not reported | 6 years | Data from YRBSSQ & DEBQ (DSM-5) | Full threshold ED cases | Physical anxiety symptoms predicted BN, while worries (e.g., about the future) predicted AN. | Fair |
| Stice et al. [57] | United States | 496 | 8 schools | 13.5 ± 0.7 at baseline | All female | 2 years | EDE (DSM-IV) | Full and partial threshold ED cases | Depressive symptoms (but not substance abuse) predicted onset of subthreshold BN. | Good |
| Stice et al. [58] | United States | 496 | 8 schools | 15.4 ± 0.7 at baseline | All female | 5 years | EDDI (DSM-IV) | Full and partial threshold ED cases | Fasting (not eating for 24 hours) for weight control more predictive of future sub/full BN than dietary restraint. | Good |
| Stice et al. [59] | United States | 496 | 8 schools | 13.5 ± 0.7 at baseline | All female | 8 years | EDDI (DSM-IV) | Full and partial threshold ED cases | Body dissatisfaction predictive of ED onset. Those with high or low body dissatisfaction and elevated depressive or dieting associated with increased ED onset respectively. | Good |
| Stice and Van Ryzin [60] | United States | 496 | 8 schools | 13.5 ± 0.7 at baseline | All female | 8 years | EDDI (DSM-IV) | Full and partial threshold ED cases | Growth curve models showed perceived pressure to be thin and/or thin-ideal internalization, before showing onset of disorder-predictive levels of body dissatisfaction, before showing onset of disorder-predictive levels of dieting and/or negative affect, before showing onset of the ED. | Good |
| Wilkinson et al. [61] | United Kingdom | 945 | Roots study | 14 at baseline | 47% male | 3 years | K-SADS-PL (DSM-IV) | Full threshold ED cases | Recurrent nonsuicidal self-injury predicted onset of EDs. | Good |
Abbreviations: ALSPAC, UK Avon Longitudinal Study of Parents and Children; AN: anorexia nervosa; BCS70, 1970 British Cohort Study; BED: binge eating disorder; BET, Branched Eating Disorders Test; BN: bulimia nervosa; DEBQ, Dutch Eating Behavior Questionnaire; DISC-II, Diagnostic Interview Schedule for Children, Version 2; DSM (-III-R/-IV/-5), Diagnostic and Statistical Manual of Mental Disorders, Third (Revised)/Fourth/Fifth Edition; EAT-40: Eating Attitudes Test; ED, eating disorder; EDDI: Eating Disorder Diagnostic Interview; EDE, Eating Disorder Examination; EDE-Q, Eating Disorder Examination Questionnaire; EDI: Eating Disorder Inventory; EDNOS, Eating Disorder Not Otherwise Specified; KSADS-PL, Kiddie Schedule for Affective Disorders and Schizophrenia, Present and Lifetime version; Project EAT-II, Eating Among Teens; TChAD, Twin study of Child and Adolescent Development; YRBSSQ, Youth Risk Behavior Surveillance System Questionnaire.
Quality of included studies
As detailed in the NOS, the quality of each study was assessed based on three broad categories pertaining to sample selection, comparability, and outcome evaluation. The percentage agreement between reviewers when assessing the quality of studies was 80%, with inconsistencies resolved via discussion. The quality assessment rating was poor for 41% (9/22), fair for 4% (1/22), and good for 55% (12/22) of studies. In terms of sample selection, 81% (18/22) of studies were found to be adequately (truly/somewhat) representative of children/adolescents in the community, all studies included individuals from the same community, 68% (15/22) used reliable methods (secure record and structured interview or questionnaire) to measure symptoms prior to ED onset, and 71% (15/22) demonstrated that EDs were not present at the start of the study (this included birth cohort studies). The proportion of studies that did not report details relating to representativeness was 18% (4/22). In terms of comparability, almost all studies (21/22) controlled for age, sex, and/or initial ED symptoms in their analyses (this included studies that were only in females or excluded individuals with EDs at the start of the study). In terms of follow-up, 59% (13/22) and 63% (14/22) of studies followed participants for at least 5 years and had adequate (>70%) follow-up rates, respectively.
Study findings
Studies reported the presence of a broad range of ED and other psychiatric disorder-related symptoms prior to ED onset. These are discussed and summarized in Table 1.
ED symptoms
Several studies reported that early eating difficulties were present prior to and predicted future EDs. Marchi and Cohen [49] first reported this in 6-year-olds followed for approximately 10 years. They reported that pica in early childhood was associated with later BN, as well as early AN/BN symptoms with later diagnosis. Early eating difficulties (e.g., digestive problems and picky eating) were also associated with later AN/BN symptoms. In a comparably aged group of children followed for up to 17 years, struggles and conflicts with food, as well as unpleasant mealtimes, predicted AN [47]. Two later studies demonstrated that at 30 years follow-up, infant feeding problems and undereating predicted and preceded AN while early overeating preceded and predicted BN/BED, respectively [51,52]. Most recently, childhood overeating, persistent undereating, and persistent fussy eating were predictive of adolescent BED, AN in girls only, and AN within the whole sample, respectively [43].
Several studies reported the preceding and predictive nature of body dissatisfaction on EDs. Beato-Fernandez et al. [42] found that body dissatisfaction predicted ED diagnosis in a group including AN, BN, and EDNOS 2 years later. Interestingly, two studies found that the presence of body image disturbance or dissatisfaction on the later development of BED/BN or EDs, respectively was only relevant to males [40,48]. The interaction between drive for thinness/body dissatisfaction and other symptomatology (e.g., anxious/depressed mood and dieting) on predicting EDs such as BN and AN was observed in several studies [59,60,62]. Growth curve models showed perceived pressure to be thin, and/or thin-ideal internalization predated the onset of disorder-predictive levels of body dissatisfaction, following disorder-predictive levels of dieting and/or negative affect, before showing onset of the ED [60]. Dietary restriction and dieting to control weight were all associated with future EDs, in particular BN or BED [63] or binge-related symptoms. Of note, Liechty and Lee [48] measured binge-related symptoms using the following question: “In the past seven days, have you been afraid to start eating because you thought you would not be able to stop or control your eating?” which may not capture an objective binge episode.
Other extreme dietary/compensatory behaviors in females, for example, self-induced vomiting and laxative use, have been reported to precede EDs, in particular BED and BN [40,48]. In Project EAT-II, among the 301 girls at time 1 with body image disturbance who did not endorse any binge eating or use of compensatory behaviors, nearly 30% worsened such that they reported binge eating, the use of compensatory behaviors, or met threshold diagnostic criteria for BN or BED. Conversely, less than one-fifth of the girls with BED or BN at time 1 were asymptomatic at time 2 [40]. In addition, “extreme weight loss behaviors,” including any reporting one or more of the following: diet pills, laxatives, or vomiting within the past 7 days to lose weight, were predicted a later self-reported ED diagnosis [48].
Other psychiatric disorder-related symptoms
The presence of other psychiatric disorder-related symptoms prior to the onset of an ED was reported in several studies. Both Johnson et al. [44] and Liechty and Lee [48] found that in adolescents (13/15 years of age), depression was associated with EDs up to 10 years later; however, the latter study found this only in males. Other findings suggest depressive symptoms (but not substance abuse or social phobia) predicted the onset of full/sub-threshold BN within the next 2 years [55,57]. However, findings in relation to AN were not significant when controlling for baseline comorbidity, EDs, and socioeconomic factors [54,59]. As previously mentioned, two studies noted the interaction between depressive mood and body dissatisfaction/drive for thinness in predicting EDs [54,59].
Along with depressive symptoms, anxiety was also found by Johnson et al. [44] to be predictive of EDs; however, this was dependent on whether responses to anxiety and/or later ED symptoms were ascertained via individual or maternal interview. As mentioned, an interaction between anxious/depressed mood and drive for thinness was found by Peñas‐Lledó and Bulik [62], and in this study, social phobia was found to precede BN, but not AN [55], albeit not when initial comorbidity, EDs, and socioeconomic factors were accounted for. In a recent study of children followed for 6 years, symptoms of generalized anxiety, specifically physical anxiety symptoms (e.g., feeling tense) were found to precede illness onset of BN and worries (e.g., about the future) were found to precede that of AN [56].
Findings related to other psychiatric disorder-related symptomatology were reported in some studies. For example, Killen et al. [46] found that alcohol use in 15-year-old girls was characteristic of those who developed EDs 4 years later. Patton et al. [53] reported that psychiatric morbidity, independent of dieting, predicted onset of EDs. Finally, in a recent study, Wilkinson et al. [61] reported that recurrent nonsuicidal self-injury behavior in 14-year-olds was predictive of EDs 4 years later [61].
Findings in relation to AN
As mentioned, childhood (i.e., under 5 years of age) eating problems (e.g., eating conflicts, struggles with food, and undereating) were found to be associated with AN up to 30 years later [47,51]. In addition, persistent undereating was associated with higher AN risk in adolescent girls only, and persistent fussy eating was associated with greater AN risk in girls and boys by 16 years of age [43]. One study found that depression alone predicted AN 2 years later [55]; however, not when comorbidity, EDs at baseline and socioeconomic factors were controlled for. The interaction of drive for thinness and anxious/depressed mood was associated with AN [54] and in terms of anxiety alone, generalized worries (but not social phobia specifically) were associated with later AN [55,56].
Findings in relation to BN and BED
Early sleeping difficulties and overeating were found to be characteristic of those who developed BN/BED-type EDs up to 30 years later [52]. In addition, childhood overeating was predictive of future BN and BED at 16 years of age [43]. In both males and females, body image disturbance and binge eating/compensatory behaviors were associated with BED and BN, respectively [40]. The interaction of drive for thinness and anxious/depressed mood was found to be associated with BN [54]. Physical anxiety-related symptoms also predicted BN [55,56]. Social phobia and depression (but not substance abuse) predicted BN [57] as well as physical anxiety-related symptoms [55,56].
Prospective associations between symptoms
As summarized above and in Figure 2, the earliest symptoms reported to be associated with future EDs (up to 30 years later) are problematic eating during early childhood, that is, under 10 years of age [41,47,49,51,52]. Then, during middle childhood/early adolescence (i.e., from 10 to 13 years of age), a range of symptoms emerge, including those relating to ED, that is, dieting [45,46,50,53,58], body dissatisfaction [40,42,45,48], and weight/shape concerns [45,46,54,59]; other psychiatric disorder-related, that is, anxiety [55,56] and depression [44,48,55,57]; [64]. Following these and at around 15 years of age, more severe symptoms such as binge eating, fasting, compensatory weight loss behaviors, and nonsuicidal self-injury arise and precede ED onset during the early 20s [40,48,58,61].
Figure 2.
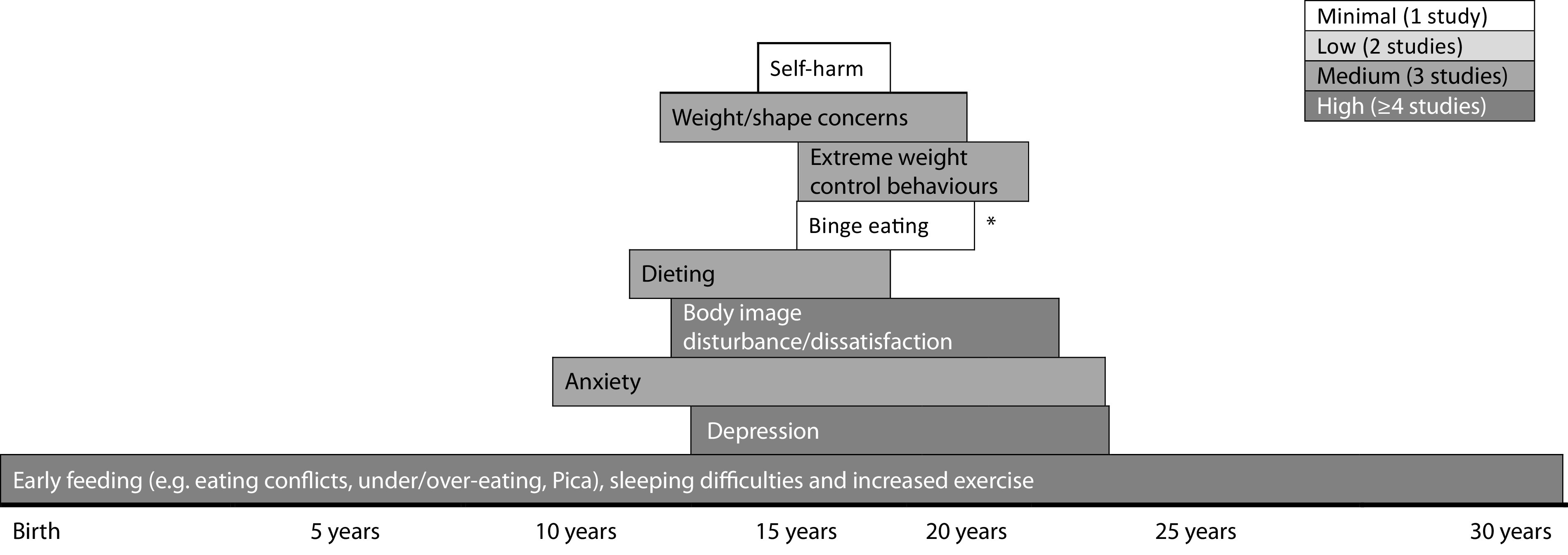
Emergence of symptoms prior to eating disorder onset. *This study was in relation to binge eating disorder only; length of rows indicates points of baseline and follow up assessments.
Discussion
To the best of our knowledge, this is the first systematic review of longitudinal cohort studies regarding the development of symptoms prior to the onset of diagnoses of EDs. This review aimed to address two questions: The extent to which ED symptoms and other psychiatric disorder-related symptoms occur prior to the onset of an ED [1] and the prospective relationship between these symptoms and ED diagnostic criteria including AN, BN, BED, and EDNOS or OSFED [2].
Our review highlights that the symptoms which exist prior to the onset of an ED are largely consistent with current diagnostic criteria of EDs and associated comorbidity. More specifically, our findings suggest that a range of ED symptoms (e.g., early eating difficulties, dietary restriction, fasting, body dissatisfaction, and weight/shape concerns), other psychiatric disorder-related symptoms (e.g., depression and anxiety) exist prior to the onset of EDs. Additionally, our review provides preliminary evidence that prospective associations may exist between these symptoms. Specifically, we found that eating difficulties in early childhood preceded the appearance of a cluster of ED (e.g., dieting, body dissatisfaction, and weight/shape concerns) and other psychiatric disorder-related symptoms (e.g., anxiety and depression) in middle childhood/early adolescence and later, more severe symptoms (e.g., binge eating, compensatory weight control behaviors, and self-harm) which tend to arise during mid-adolescence/emerging adulthood [47,48,60].
In terms of ED-specific symptoms prior to future illness onset, a significant proportion of studies indicate an age-related trajectory in their development. For example, childhood eating difficulties are the first to arise [43,47,49,51,52]. Interestingly, these are consistent with ED phenotypes, for example, conflicts, struggles, and undereating in relation to AN and overeating in relation to BN, both up to 30 years later [23,47,51,52]. However, larger studies and replication are required to tease apart possible ED diagnosis–specific trajectories into illness. These early eating difficulties were found to predate the emergence of late childhood/early adolescent body image dissatisfaction (particularly relevant for males and BN/BED-type EDs), weight/shape concerns, and dietary restraint [40,42,48,54], followed by the appearance of more extreme dieting/weight control behaviors (e.g., binge eating, fasting, self-induced vomiting, and laxative use) in mid/late adolescence [40,48]. These findings are similar to those reported by Allen et al. [63], in that, more established ED symptoms (e.g., purging, fasting, and binge eating) appear to persist between mid-adolescence/early adulthood. Additionally, the adolescent symptom clusters identified in this review tended to be associated with ED onset during emerging adulthood, apart from dietary restraint which often emerged at an earlier age and was associated with earlier ED onset. This is consistent with other findings whereby childhood undereating predicted the onset of adolescent AN [43]. It is important to note that while such findings could represent EDs in evolution and possible ED prodromes, these trajectories of ED symptoms could also be age-specific manifestations of full diagnoses and represent shortcomings of the current diagnostic criteria when applied to children/adolescents [65].
In terms of other psychiatric disorder-related symptoms, anxiety and depression were shown to commonly exist prior to ED onset [44,56]. This is consistent with other findings relating to the prediction of affective symptomatology on later ED symptoms [66–71]. However, studies reviewed here also suggest that affective symptomatology may appear concurrently [55] or interact with ED-related symptoms [54]. This latter finding has also been established in longitudinal studies investigating the onset of subthreshold EDs or ED symptoms, suggesting that the presence of early ED and affective symptoms (e.g., dietary restraint and depression) predict later ED behaviors/attitudes [72,73]. Fewer studies report the presence of other psychiatric disorder-related symptoms, such as alcohol use and nonsuicidal self-injury prior to EDs [46,61]. Overall, the presence of other psychiatric symptoms prior to ED onset is unsurprising given the high rates of lifetime comorbidity associated with EDs [5]. However, as the studies reviewed here and those outside the scope of this review have demonstrated, there is mixed evidence for any prospective association between affective and ED symptoms/disorders [74–76]. Further longitudinal research with frequent assessment points is warranted in order to tease apart any chronological patterns in the appearance of ED and other psychiatric disorder-related symptomatology or understand how they collectively contribute to the onset of EDs.
It is important to note that a number of important studies in this field were not included as they were outside the scope of the current review (e.g., investigated broad predictors of EDs or measured ED symptoms rather than diagnoses as outcomes). Specifically, findings that early traits such as impulsiveness and low self-esteem/efficacy are associated with EDs up to 30 years later [41,51,52] are particularly relevant for BN/BED-type EDs. Similarly, the predictive nature of hyperactivity/inattention and self-esteem on binge eating and purging behaviors [77,78] and symptom trajectories of hyperactivity and inattention subscores are predictive of later EDI subscales, including restrictive-eating and bulimia subscales [64]. In addition, there is a comprehensive literature on the relationship between EDs and autistic traits [79–82], although no studies to date have investigated autistic traits as predictors of future ED diagnoses in longitudinal cohort-based studies.
This is the first study to review longitudinal, cohort-based studies in relation to symptomatology prior to ED diagnostic onset. This systematic review involved independent double screening at all possible stages with minimal disagreement. Stringent inclusion criteria relating to sample sizes, length of follow-up, and the requirement for studies to report the progression to an ED were adhered to. Additionally, a thorough assessment of the quality of included studies was conducted. These factors demonstrate the originality of this review, provide confidence in its inclusion of relevant literature, and the thorough way in which this was reviewed.
There are several limitations to this review which must be considered. First, studies were heterogeneous in terms of their aims, design, methodology, and findings, making comparisons of findings difficult, meta-analyses impossible, and the generalizability of overall findings limited. Second, studies reviewed were based on stringent ED diagnostic criteria (i.e., DSM-III or DSM-IV) or self-report of an ED diagnosis from a medical professional, and therefore this review is likely to have missed information from many individuals who would meet current diagnostic criteria for an ED of subthreshold ED, given the broader consideration of symptoms (e.g., elimination of amenorrhea criterion in AN and reduction of binge/purge frequency in BN/BED) and new diagnoses (e.g., BED and avoidant/restrictive food intake disorder) in DSM-5. Third, we focused primarily on psychiatric disorder-related symptoms prior to the onset of EDs; therefore, are likely to have omitted other important factors that could constitute an ED prodrome (e.g., overweight/obesity and personality traits). Finally, it would have been informative to consider a psychiatric comparison group in order to evaluate how ED prodromes may differ from prodromal stages of other psychiatric disorders.
The identification of symptom trajectories into EDs and possible prospective associations elicited from the current review could have important clinical and research implications. For example, our findings inform stage models of illness in EDs, specifically the early prodromal phase. This improved understanding of ED prodromes could be useful in informing early intervention programs. Specifically, these could target a range of symptomatology earlier (i.e., early eating difficulties in childhood, affective symptomatology in childhood, dieting, and depression in early adolescence). Other studies have also suggested this in relation to the impact of childhood symptoms on later disordered eating [73,83]. In terms of research implications, a significant proportion of potentially relevant studies were excluded from this review as they did not report progression of symptoms into a clinical ED diagnosis. Future longitudinal research should aim to report this information. Additionally, efforts should be made to ensure large cohorts of children/adolescents are evaluated which are characteristic of the wider community, and data regarding representativeness should always be reported. Standardized, well-validated measures to assess a broad range of symptomatology prior to ED onset should be used, preferably consistently across studies. Assessment of EDs at baseline should be conducted, relevant individuals excluded, and analyses should control for important factors such as age and sex, as has been done in some of the highest quality papers included in this review [43,55]. Assessment of ED onset should preferably be via clinical interviews based on current diagnostic criteria (e.g., Eating Disorder Examination) and if not, via the use of well-validated questionnaire equivalents (e.g., Eating Disorder Examination Questionnaire). Follow-up should include early (i.e., before adolescence) and regular (i.e., yearly) assessments, over a long enough time period that would enable a better understanding of possible prospective associations of a broad range of symptomatology. Finally, larger sample sizes (ideally via combining information across similarly designed studies) and the inclusion of clinical comparison groups would help to elucidate symptom trajectories that are specific to EDs (e.g., compared to depression and body dysmorphic disorder), to individual ED diagnoses (e.g., AN compared to BN or BED), or differ according to factors such as sex.
Prospective and longitudinal designs as described would represent a gold standard in the assessment of symptoms prior to illness onset and therefore in evaluating prodromal stages of EDs. However, it is important to note that it was uncommon for a large population-based cohort study to be designed for the specific purpose of measuring trajectories into illness in ED diagnoses. Instead, many were designed to present the research community with a rich dataset to understand genetic and environmental influences on health and development, which were then used by researchers to investigate the trajectories into ED diagnoses. While retrospective assessments of symptoms prior to an ED are limited by biased retrospective recall or subjective, inaccurate memory, they have been shown to be informative in other psychiatric disorders such as psychosis [84]. Retrospective assessments could be equally informative in advancing our understanding of prodromal stages of EDs.
In conclusion, this review identified the presence of a broad range of psychiatric symptomatology that precedes and may be indicative of future ED onset, as well as an insight into potential prospective associations. These symptom profiles may represent prodromal stages of EDs; however, further work is required to establish these findings. Such research could inform early intervention strategies and ultimately deter the progression of EDs into chronic, life-threatening conditions.
Financial Support
R.P. is supported by a PhD studentship from the National Institute of Health Research (NIHR) Mental Health Biomedical Research Centre (BRC) at South London, Maudsley NHS Foundation Trust (SLaM), and King’s College London (KCL). U.S. and L.R. receive salary support from the NIHR Mental Health BRC at SLaM and KCL. U.S. is supported by an NIHR Senior Investigator Award. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, or the Department of Health.
Conflict of Interest
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
Data Availability Statement
As this is a systematic review, there are no empirical data. Qualitative resources (e.g., spreadsheets of studies evaluated) are available on request from the authors.
References
- [1].American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Association. [Google Scholar]
- [2].Bartholdy S, Allen K, Hodsoll J, O’Daly OG, Campbell IC, Banaschewski T, et al. Identifying disordered eating behaviours in adolescents: how do parent and adolescent reports differ by sex and age? Eur Child Adolesc Psychiatry. 2017;26(6):691–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Erskine HE, Whiteford HA, Pike KM. The global burden of eating disorders. Curr Opin Psychiatry. 2016;29(6):346–353. [DOI] [PubMed] [Google Scholar]
- [4].Keski-Rahkonen A, Mustelin L. Epidemiology of eating disorders in Europe: prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr Opin Psychiatry. 2016;29(6):340–345. [DOI] [PubMed] [Google Scholar]
- [5].Hudson JI, Hiripi E, Pope HG Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61(3):348–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Fichter MM, Quadflieg N. Mortality in eating disorders – results of a large prospective clinical longitudinal study. Int J Eating Disord. 2016;49(4):391–401. [DOI] [PubMed] [Google Scholar]
- [7].Ben-Tovim DI, Walker K, Gilchrist P, Freeman R, Kalucy R, Esterman A. Outcome in patients with eating disorders: a 5-year study. Lancet. 2001;357(9264):1254–1257. [DOI] [PubMed] [Google Scholar]
- [8].Vos T, Mathers C, Herrman H, Harvey C, Gureje O, Bui D, et al. The burden of mental disorders in Victoria, 1996. Social Psychiatry Psychiatr Epidemiol. 2001;36(2):53–62. [DOI] [PubMed] [Google Scholar]
- [9].Javaras KN, Runfola CD, Thornton LM, Agerbo E, Birgegard A, Norring C, et al. Sex- and age-specific incidence of healthcare-register-recorded eating disorders in the complete swedish 1979–2001 birth cohort. Int J Eating Disord. 2015;48(8):1070–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Galmiche M, Dechelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am J Clin Nutr. 2019;109(5):1402–1413. [DOI] [PubMed] [Google Scholar]
- [11].Slane JD, Klump KL, McGue M, Iacono WG. Developmental trajectories of disordered eating from early adolescence to young adulthood: a longitudinal study. Int J Eating Disord. 2014;47(7):793–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Treasure J, Stein D, Maguire S. Has the time come for a staging model to map the course of eating disorders from high risk to severe enduring illness? An examination of the evidence. Early Interv Psychiatry. 2015;9(3):173–184. [DOI] [PubMed] [Google Scholar]
- [13].Le LK, Barendregt JJ, Hay P, Mihalopoulos C. Prevention of eating disorders: a systematic review and meta-analysis. Clin Psychol Rev. 2017;53:46–58. [DOI] [PubMed] [Google Scholar]
- [14].Watson HJ, Goodman EL, McLagan NB, Joyce T, French E, Willan V, et al. Quality of randomized controlled trials in eating disorder prevention. Int J Eating Disord. 2017;50(5):459–470. [DOI] [PubMed] [Google Scholar]
- [15].Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, Kupfer DJ. Coming to terms with the terms of risk. Arch Gen Psychiatry. 1997;54(4):337–343. [DOI] [PubMed] [Google Scholar]
- [16].Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychol Bull. 2004;130(1):19–65. [DOI] [PubMed] [Google Scholar]
- [17].Dakanalis A, Clerici M, Bartoli F, Caslini M, Crocamo C, Riva G, et al. Risk and maintenance factors for young women’s DSM-5 eating disorders. Arch Women’s Ment Health. 2017;20(6):721–731. [DOI] [PubMed] [Google Scholar]
- [18].Watson HJ, Yilmaz Z, Thornton LM, Hubel C, Coleman JRI, Gaspar HA, et al. Genome-wide association study identifies eight risk loci and implicates metabo-psychiatric origins for anorexia nervosa. Nat Genet. 2019;15(10):019–0439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Stice E, Ng J, Shaw H. Risk factors and prodromal eating pathology. J Child Psychol Psychiatry. 2010;51(4):518–525. [DOI] [PubMed] [Google Scholar]
- [20].McClelland J, Hodsoll J, Brown A, Lang K, Boysen E, Flynn M, et al. A pilot evaluation of a novel First Episode and Rapid Early Intervention service for Eating Disorders (FREED). Eur Eating Disord Rev. 2018;26(2):129–140. [DOI] [PubMed] [Google Scholar]
- [21].Fukutomi A, Austin A, McClelland J, Brown A, Glennon D, Mountford V, et al. First Episode Rapid Early Intervention for Eating Disorders (FREED): a two-year follow-up. Early Interv Psychiatry. 2019. 14(1):137–141. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [22].Fava GA, Mangelli L. Subclinical symptoms of panic disorder: new insights into pathophysiology and treatment. Psychother Psychosomat. 1999;68(6):281–289. [DOI] [PubMed] [Google Scholar]
- [23].Pede VB, Jaiswal SV, Sawant VA. Study of prodromal and residual symptoms of depression. Ind Psychiatry J. 2017;26(2):121–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Van Meter AR, Burke C, Youngstrom EA, Faedda GL, Correll CU. The bipolar prodrome: meta-analysis of symptom prevalence prior to initial or recurrent mood episodes. J Am Acad Child Adolesc Psychiatry. 2016;55(7):543–555. [DOI] [PubMed] [Google Scholar]
- [25].Penttila M, Jaaskelainen E, Hirvonen N, Isohanni M, Miettunen J. Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2014;205(2):88–94. [DOI] [PubMed] [Google Scholar]
- [26].Barajas A, Pelaez T, Gonzalez O, Usall J, Iniesta R, Arteaga M, et al. Predictive capacity of prodromal symptoms in first-episode psychosis of recent onset. Early Interv Psychiatry. 2019;13(3):414–424. [DOI] [PubMed] [Google Scholar]
- [27].Valmaggia LR, Byrne M, Day F, Broome MR, Johns L, Howes O, et al. Duration of untreated psychosis and need for admission in patients who engage with mental health services in the prodromal phase. Br J Psychiatry. 2015;207(2):130–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Fusar-Poli P, Meneghelli A, Valmaggia L, Allen P, Galvan F, McGuire P, et al. Duration of untreated prodromal symptoms and 12-month functional outcome of individuals at risk of psychosis. Br J Psychiatry. 2009;194(2):181–182. [DOI] [PubMed] [Google Scholar]
- [29].Woodberry KA, Shapiro DI, Bryant C, Seidman LJ. Progress and future directions in research on the psychosis prodrome: a review for clinicians. Harvard Rev Psychiatry. 2016;24(2):87–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Modinos G, McGuire P. The prodromal phase of psychosis. Curr Opin Neurobiol. 2015;30:100–105. [DOI] [PubMed] [Google Scholar]
- [31].Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. 2012;69(3):220–229. [DOI] [PubMed] [Google Scholar]
- [32].Savill M, Sardo A, Patel P, Loewy R, Melnikow J, Niendam T. Which components of specialized early intervention for psychosis do senior providers see as most important? Early Interv Psychiatry. 2019;13(3):677–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Fusar-Poli P, Byrne M, Badger S, Valmaggia LR, PK MG. Outreach and support in south London (OASIS), 2001–2011: ten years of early diagnosis and treatment for young individuals at high clinical risk for psychosis. Eur Psychiatry. 2013;28(5):315–326. [DOI] [PubMed] [Google Scholar]
- [34].Fusar-Poli P, Diaz-Caneja CM, Patel R, Valmaggia L, Byrne M, Garety P, et al. Services for people at high risk improve outcomes in patients with first episode psychosis. Acta Psychiatr Scand. 2016;133(1):76–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Valmaggia LR, McCrone P, Knapp M, Woolley JB, Broome MR, Tabraham P, et al. Economic impact of early intervention in people at high risk of psychosis. Psychol Med. 2009;39(10):1617–1626. [DOI] [PubMed] [Google Scholar]
- [36].van der Gaag M, Smit F, Bechdolf A, French P, Linszen DH, Yung AR, et al. Preventing a first episode of psychosis: meta-analysis of randomized controlled prevention trials of 12 month and longer-term follow-ups. Schizophr Res. 2013;149(1–3):56–62. [DOI] [PubMed] [Google Scholar]
- [37].Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012. [DOI] [PubMed] [Google Scholar]
- [38].Wells GA, Shea B, O’Connell D, Peterson J, VWelch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses, http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp; 2003. Accessed 01 May 2018.
- [39].Viswanathan M, Ansari MT, Berkman ND, Chang S, Hartling L, McPheeters M, et al. Assessing the risk of bias of individual studies in systematic reviews of health care interventions Methods guide for effectiveness and comparative effectiveness reviews. Rockville, MD: Agency for Healthcare Research and Quality (US), 2008. [PubMed] [Google Scholar]
- [40].Ackard DM, Fulkerson JA, Neumark-Sztainer D. Stability of eating disorder diagnostic classifications in adolescents: five-year longitudinal findings from a population-based study. Eating Disord. 2011;19(4):308–322. [DOI] [PubMed] [Google Scholar]
- [41].Allen KL, Byrne SM, Forbes D, Oddy WH. Risk factors for full- and partial-syndrome early adolescent eating disorders: a population-based pregnancy cohort study. J Am Acad Child Adolesc Psychiatry. 2009;48(8):800–809. [DOI] [PubMed] [Google Scholar]
- [42].Beato-Fernandez L, Rodriguez-Cano T, Belmonte-Llario A, Martinez-Delgado C. Risk factors for eating disorders in adolescents. A Spanish community-based longitudinal study. Eur Child Adolesc Psychiatry. 2004;13(5):287–294. [DOI] [PubMed] [Google Scholar]
- [43].Herle M, De Stavola B, Hübel C, Abdulkadir M, Ferreira DS, Loos RJ, et al. A longitudinal study of eating behaviours in childhood and later eating disorder behaviours and diagnoses. Br J Psychiatry. 2020;216(2):113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Johnson JG, Cohen P, Kotler L, Kasen S, Brook JS. Psychiatric disorders associated with risk for the development of eating disorders during adolescence and early adulthood. J Consult Clin Psychol. 2002;70(5):1119–1128. [DOI] [PubMed] [Google Scholar]
- [45].Killen JD, Taylor CB, Hayward C, Wilson DM, Haydel KF, Hammer LD, et al. Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls: a three-year prospective analysis. Int J Eating Disord. 1994;16(3):227–238. [DOI] [PubMed] [Google Scholar]
- [46].Killen JD, Taylor CB, Hayward C, Haydel KF, Wilson DM, Hammer L, et al. Weight concerns influence the development of eating disorders: a 4-year prospective study. J Consult Clin Psychol. 1996;64(5):936–940. [DOI] [PubMed] [Google Scholar]
- [47].Kotler LA, Cohen P, Davies M, Pine DS, Walsh BT. Longitudinal relationships between childhood, adolescent, and adult eating disorders. J Am Acad Child Adolesc Psychiatry. 2001;40(12):1434–1440. [DOI] [PubMed] [Google Scholar]
- [48].Liechty JM, Lee MJ. Longitudinal predictors of dieting and disordered eating among young adults in the US. Int J Eating Disord. 2013;46(8):790–800. [DOI] [PubMed] [Google Scholar]
- [49].Marchi M, Cohen P. Early childhood eating behaviors and adolescent eating disorders. J Am Acad Child Adolesc Psychiatry. 1990;29(1):112–117. [DOI] [PubMed] [Google Scholar]
- [50].Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, Eisenberg M. Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: how do dieters fare 5 years later? J Am Diet Assoc. 2006;106(4):559–568. [DOI] [PubMed] [Google Scholar]
- [51].Nicholls D, Viner RM. Childhood risk factors for lifetime anorexia nervosa by age 30 years in a national birth cohort. J Am Acad Child Adolesc Psychiatry. 2009;48(8):791–799. [DOI] [PubMed] [Google Scholar]
- [52].Nicholls D, Statham R, Costa S, Micali N, Viner RM. Childhood risk factors for lifetime bulimic or compulsive eating by age 30 years in a British national birth cohort. Appetite. 2016;105:266–273. [DOI] [PubMed] [Google Scholar]
- [53].Patton GC, Selzer R, Coffey C, Carlin JB, Wolfe R. Onset of adolescent eating disorders: population based cohort study over 3 years. Br J Med. 1999;318(7186):765–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Penas-Lledo E, Bulik CM, Lichtenstein P, Larsson H, Baker JH. Risk for self-reported anorexia or bulimia nervosa based on drive for thinness and negative affect clusters/dimensions during adolescence: a three-year prospective study of the TChAD cohort. Int J Eating Dis. 2015;48(6):692–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Ranta K, Vaananen J, Frojd S, Isomaa R, Kaltiala-Heino R, Marttunen M. Social phobia, depression and eating disorders during middle adolescence: longitudinal associations and treatment seeking. Nordic J Psychiatry. 2017;71(8):605–613. [DOI] [PubMed] [Google Scholar]
- [56].Schaumberg K, Zerwas S, Goodman E, Yilmaz Z, Bulik CM, Micali N. Anxiety disorder symptoms at age 10 predict eating disorder symptoms and diagnoses in adolescence. J Child Psychol Psychiatry. 2019;60(6):686–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Stice E, Burton EM, Shaw H. Prospective relations between bulimic pathology, depression, and substance abuse: unpacking comorbidity in adolescent girls. J Consult Clin Psychol. 2004;72(1):62–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Stice E, Davis K, Miller NP, Marti CN. Fasting increases risk for onset of binge eating and bulimic pathology: a 5-year prospective study. JAP. 2008;117(4):941–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Stice E, Marti CN, Durant S. Risk factors for onset of eating disorders: evidence of multiple risk pathways from an 8-year prospective study. Behav Res Ther. 2011;49(10):622–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Stice E, Van Ryzin MJ. A prospective test of the temporal sequencing of risk factor emergence in the dual pathway model of eating disorders. J Abnormal Psychol. 2019;128(2):119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Wilkinson PO, Qiu T, Neufeld S, Jones PB, Goodyer IM. Sporadic and recurrent non-suicidal self-injury before age 14 and incident onset of psychiatric disorders by 17 years: prospective cohort study. Br J Psychiatry. 2018;212(4):222–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Peñas‐Lledó E, Bulik CM, Lichtenstein P, Larsson H, Baker JH. Risk for self‐reported anorexia or bulimia nervosa based on drive for thinness and negative affect clusters/dimensions during adolescence: a three‐year prospective study of the TChAD cohort. Int J Eating Disord. 2015;48(6):692–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Allen KL, Crosby RD, Oddy WH, Byrne SM. Eating disorder symptom trajectories in adolescence: effects of time, participant sex, and early adolescent depressive symptoms. J Eating Disord. 2013;1:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Yilmaz Z, Javaras KN, Baker JH, Thornton LM, Lichtenstein P, Bulik CM, et al. Association between childhood to adolescent ADHD symptom trajectories and late adolescent disordered eating. J Adolesc Health. 2017;61(2):140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Le Grange D, Loeb KL. Early identification and treatment of eating disorders: prodrome to syndrome. Early Interv Psychiatry. 2007;1(1):27–39. [DOI] [PubMed] [Google Scholar]
- [66].Herpertz-Dahlmann B, Dempfle A, Konrad K, Klasen F, Ravens-Sieberer U. Eating disorder symptoms do not just disappear: the implications of adolescent eating-disordered behaviour for body weight and mental health in young adulthood. Eur Child Adolesc Psychiatry. 2015;24(6):675–684. [DOI] [PubMed] [Google Scholar]
- [67].Le Grange D, O’Connor M, Hughes EK, Macdonald J, Little K, Olsson CA. Developmental antecedents of abnormal eating attitudes and behaviors in adolescence. Int J Eating Disord. 2014;47(7):813–824. [DOI] [PubMed] [Google Scholar]
- [68].Pearson CM, Miller J, Ackard DM, Loth KA, Wall MM, Haynos AF, et al. Stability and change in patterns of eating disorder symptoms from adolescence to young adulthood. Int J Eating Disord. 2017;50(7):748–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Pearson CM, Zapolski TC, Smith GT. A longitudinal test of impulsivity and depression pathways to early binge eating onset. Int J Eating Disord. 2015;48(2):230–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Presnell K, Stice E, Seidel A, Madeley MC. Depression and eating pathology: prospective reciprocal relations in adolescents. Clin Psychol Psychother. 2009;16(4):357–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Stice E, Killen JD, Hayward C, Taylor CB. Age of onset for binge eating and purging during late adolescence: a 4-year survival analysis. J Abnormal Psychol. 1998;107(4):671–675. [DOI] [PubMed] [Google Scholar]
- [72].Chen EY, McCloskey MS, Keenan KE. Subtyping dietary restraint and negative affect in a longitudinal community sample of girls. Int J Eating Disord. 2009;42(3):275–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Ferreiro F, Wichstrom L, Seoane G, Senra C. Reciprocal associations between depressive symptoms and disordered eating among adolescent girls and boys: a multiwave, prospective study. J Abnorm Child Psychol. 2014;42(5):803–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Sehm M, Warschburger P. Prospective associations between binge eating and psychological risk factors in adolescence. J Clin Child Adolesc Psychol. 2018;47(5):770–784. [DOI] [PubMed] [Google Scholar]
- [75].Skinner HH, Haines J, Austin SB, Field AE. A prospective study of overeating, binge eating, and depressive symptoms among adolescent and young adult women. J Adolesc Health. 2012;50(5):478–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Marmorstein NR, von Ranson KM, Iacono WG, Malone SM. Prospective associations between depressive symptoms and eating disorder symptoms among adolescent girls. Int J Eating Disord. 2008;41(2):118–23. [DOI] [PubMed] [Google Scholar]
- [77].Sonneville KR, Calzo JP, Horton NJ, Field AE, Crosby RD, Solmi F, et al. Childhood hyperactivity/inattention and eating disturbances predict binge eating in adolescence. Psychol Med. 2015;45(12):2511–2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Stephen EM, Rose J, Kenney L, Rosselli-Navarra F, Weissman RS. Adolescent risk factors for purging in young women: findings from the national longitudinal study of adolescent health. J Eating Disord. 2014;2:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Pooni J, Ninteman A, Bryant‐Waugh R, Nicholls D, Mandy W. Investigating autism spectrum disorder and autistic traits in early onset eating disorder. Int J Eating Disord. 2012;45(4):583–91. [DOI] [PubMed] [Google Scholar]
- [80].Coombs E, Brosnan M, Bryant‐Waugh R, Skevington SM. An investigation into the relationship between eating disorder psychopathology and autistic symptomatology in a non‐clinical sample. Br J Clin Psychol. 2011;50(3):326–38. [DOI] [PubMed] [Google Scholar]
- [81].Huke V, Turk J, Saeidi S, Kent A, Morgan JF. Autism spectrum disorders in eating disorder populations: a systematic review. Eur Eating Disord Rev. 2013;21(5):345–351. [DOI] [PubMed] [Google Scholar]
- [82].Dell’Osso L, Carpita B, Gesi C, Cremone I, Corsi M, Massimetti E, et al. Subthreshold autism spectrum disorder in patients with eating disorders. Comprehen Psychiatry. 2018;81:66–72. [DOI] [PubMed] [Google Scholar]
- [83].Evans EH, Adamson AJ, Basterfield L, Le Couteur A, Reilly JK, Reilly JJ, et al. Risk factors for eating disorder symptoms at 12 years of age: a 6-year longitudinal cohort study. Appetite. 2017;108:12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Register-Brown K, Hong LE. Reliability and validity of methods for measuring the duration of untreated psychosis: a quantitative review and meta-analysis. Schizophr Res. 2014;160(1–3):20–26. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
As this is a systematic review, there are no empirical data. Qualitative resources (e.g., spreadsheets of studies evaluated) are available on request from the authors.