Abstract
Objectives
To investigate the magnitude of effect nurse staffing had on decreasing the newborn mortality rates in member countries of Organisation for Economic Co-operation and Development (OECD).
Methods
The statistical technique of panel data analysis was applied to explore the possibility of association between the number of nurses’ density per 1,000 population and infant, neonatal and perinatal mortality rates (IMR, NMR and PMR) per 1000 births. The observations of 35 OECD countries were collected over the period of 2000 through 2016.
Results
There were significant associations between nurse staffing and IMR, NMR and PMR i.e. a 1% increase in nurse-staffing level reduced IMR, NMR and PMR by 0.98%, 0.97% and 0.96%, respectively. Furthermore, the role of nursing-related services in declining the average of newborn mortality rates were investigated at the highest level in Slovenia (−5.50), Sweden (−3.34), Iceland (−2.51), Czech Republic (−1.86), Japan (−1.64) and Finland (−1.64). Moreover, if the current relationship between nurse-staffing level and newborn mortality rates are disturbed with nursing shortage (e.g. in Slovak Republic and Israel), then it takes about 17 years for the mortality rates to reduce and restore back to the previous equilibrium.
Conclusions
A higher proportion of nurses’ density per 1,000 population is associated with lower newborn mortality rates. In addition, the nursing-related services of Slovenia, Sweden, Iceland, Czech Republic, Japan and Finland with the highest impact on improving the health level of newborns would be good patterns for other developed countries in maternity and child health care .
Keywords: Health manpower, Infant mortality, Nursing staff, Organisation for Economic Co-operation and Development, Perinatal mortality
What is known?
-
•
The association between the nursing-related services and lower risk-adjusted mortality has been proved in previous studies, but there is a lack of cross-national studies to analyze the possible role of practicing nurses in reducing newborn mortality rates.
What is new?
-
•
Our findings verified that the long-run elasticity of nurse-staffing level on IMR, NMR and PMR were −0.98, −0.97 and −0.96, respectively.
-
•
Among OECD countries, the highest effect of practicing nurses on improving health level of newborns were estimated in Slovenia, Sweden, Iceland, Czech Republic, Japan and Finland.
-
•
If the long-run relationships between nurse staffing and newborn mortality rates are disturbed with nursing shortage e.g. observed in Slovak Republic and Israel, it lasts for 17 years to restore back to long-run equilibriums.
1. Introduction
According to the global measurements of health care performance, infant and neonatal mortality rates (IMR and NMR), i.e. the rate of newborn deaths per 1,000 live births of one year and less than four weeks of age, as well as perinatal mortality rate (PMR), i.e. early neonatal mortality, are the most predominant indicators of mothers’ and newborns’ health level. In member countries of Organisation for Economic Co-operation and Development (OECD), about 70% of total number of baby deaths which occur during less than one year of birth are neonatal deaths i.e. happen in less than four weeks of birth, whereas birth defects, prematurity, sudden infant death syndrome (SID), infections as well as accidents are reported as the major causes of neonatal mortality [1].
In the most of developed countries, the average of IMR, NMR and PMR in 2016 were quite low about 3.76, 2.56 and 5.19 deaths per 1,000 live births, respectively, except in Turkey and Mexico. Since 2000, there has been a significant decrease in the trend of newborn mortality observed in all OECD countries, particularly in Turkey, Mexico, Latvia, Estonia, Hungary, Lithuania and Poland contributed to differences in characteristics and effectiveness of health care systems, economic and social conditions, education level together with mothers and newborns lifestyles – see Ref. [1,2].
As nurses play a critical role in providing health care services in hospital and long-term care along with primary and home care settings, whereas nurses obviously outnumber physicians in the most of OECD countries, it is substantial to compute the effects of nurse staffing on improving the health level of mothers and newborns among different health care systems of OECD countries. Despite the significant rise in the average number of nurse density per 1,000 population from 7.3 in 2000 to 9 in 2015, in Slovak Republic, followed by Ireland, Israel and United Kingdom the number of nurses per capita has declined since 2000 i.e. the size of nurse staffing rose slower than population growth. Thus, there are growing concerns about potential future shortages of nurses in the process of aging reformation and retirement of current generation of nurses observed in many OECD countries [3].
In response to shortages of practicing nurses and physicians to ensure proper care delivery and to enhance the quality of newborn care in health facilities, it is critical for governments, policy makers and researchers to look for more efficient care services aimed to advance the health level of mothers and newborns [4]. To do this, the first step is to estimate the impact of nurse staffing on improving newborn health outcomes among different health care systems of developed countries [5].
To our knowledge, nursing literature has strongly argued the association between nurse staffing and lower risk-adjusted mortality [[6], [7], [8]], reviewed in Ref. [9]. Besides, the results of multinational studies have drawn the same conclusion with patient mortality [[9], [10], [11], [12], [13], [14], [15], [16], [17], [18]], failure to rescue [10,12] and safety failures [13,[19], [20], [21], [22], [23]]. However, there is a lack of empirical research to measure the possible role of practicing nurses in reducing newborn mortality rates in national level.
The aim of this study is to provide empirical information about the relationship from nursing characteristics to reducing newborn mortality rates. To do this, the most comprehensive source of cross-national statistics across developed countries is applied in this study. The statistical technique of panel data analysis is conducted to measure the association between nurses’ density per 1,000 population and improving the quality of newborn care services among 35 OECD countries during the period of 2000–2016.
2. Data description
The number of practicing professional nurses’ density per 1,000 population, which defined as the determinant of health care performances, covered nursing professionals who deliver clinical and hospital care services directly to patients including general care nurses, specialist nurses, clinical nurses, district nurses, nurse anesthetists, nurse educators, nurse practitioners and public health nurses were collected from OECD [24] as the index of nurse-staffing level [25,26]. The nursing data is available at Health Care Resources Package for 35 OECD countries from 2000 to 2016.
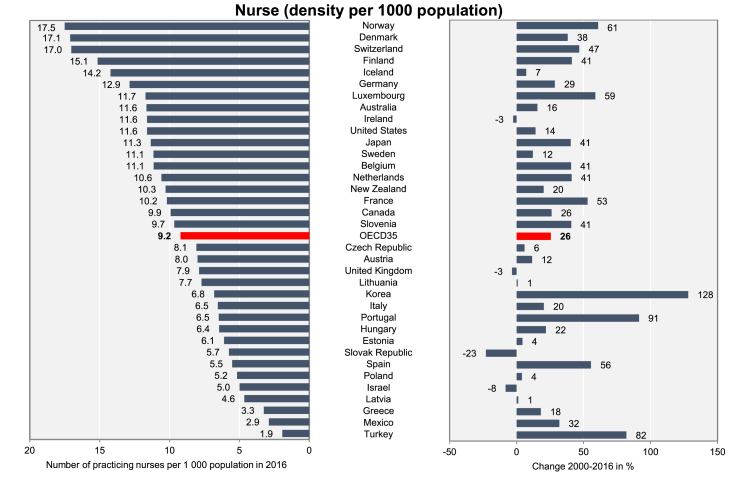
The column chart of practicing nurse’s ratio for 35 OECD countries in years 2016 and change from 2000 to 2016 is available in Fig. 1. In 2016, the highest number of practicing nurses per 1,000 population was recorded in Norway (17.49), followed by Denmark (17.10), Switzerland (17.02), Finland (15.14) and Iceland (14.22) among the other OECD countries. Interestingly, out of 35 OECD countries, there was a significant rise in the number of practicing nurses in 31 countries from 2000 to 2016 and Korea with 128.2%, Portugal with 91.4%, Turkey with 82.1%, Norway with 60.9% and Luxembourg with 58.9% had the highest growth during this period. At the other end of the range, the lowest level of practicing nurses in 2016 was recorded in Turkey, where on average, only 1.93 practicing nurses per 1,000 inhabitants; Mexico (2.98), Greece (3.25), Latvia (4.64) and Israel (4.99) had the lowest number of nurses in OECD countries. Furthermore, there was a reduction in the trends of nurse staffing during 2000–2016 period in Ireland (−2.5%), United Kingdom (−3.3%), Israel (−8.1%) and Slovak Republic (−22.8%). The average amounts of practicing nurses’ ratios in 2000 and 2016 were 7.34 and 9.22 with the ranges of 13.26–1.06 and 17.49–1.93, respectively.
Fig. 1.
Number of practicing nurses’ density per 1,000 population, 2016 and change 2000–2016. Source: OECD [24].
The number of newborn deaths aged under one year of age together with under 28 days of age that happened each year both expressed per 1,000 live births are defined as IMR and NMR without considering birthweight or minimum threshold of gestation period. Perinatal mortality per 1,000 total births is described as the ratio of child deaths within one week of birth (early neonatal deaths) plus fetal deaths of minimum gestation period 28 weeks or minimum fetal weight of 1,000g. The observations of IMR, NMR and PMR were collected from OECD Health Statistics [27] for 35 OECD countries over the period 2000–2016.
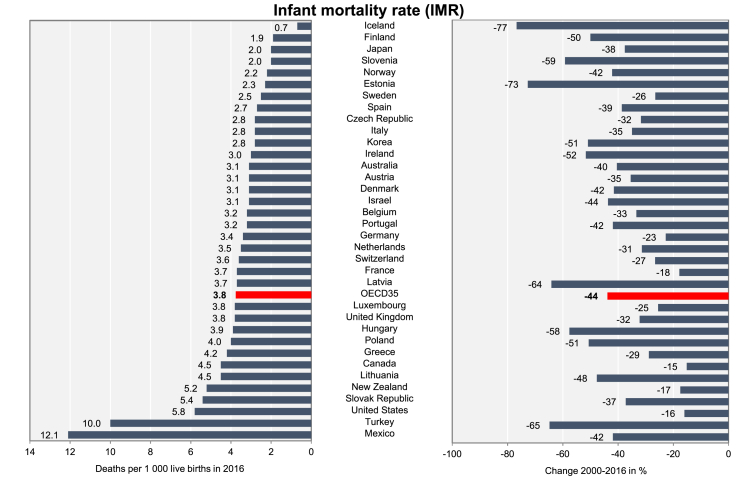
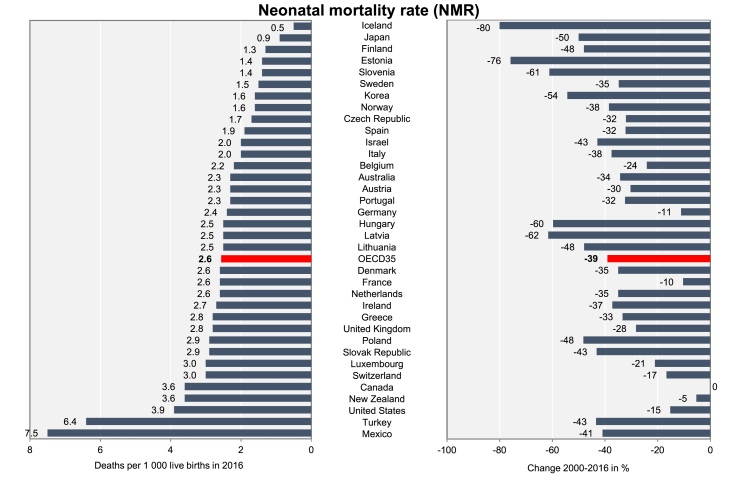
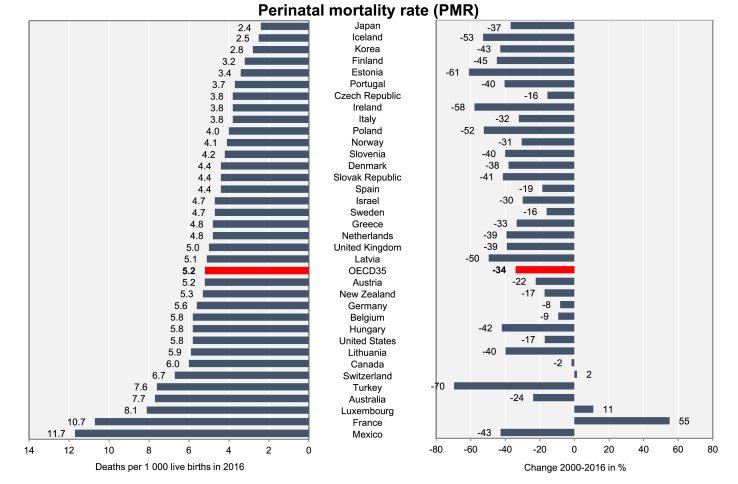
The column chart of newborn mortality rates for 35 OECD countries in years 2016 and change from 2000 to 2016 are available in Fig. 2, Fig. 3, Fig. 4. Obviously, the rates of newborn deaths in OECD countries were quite low, except in Turkey and Mexico (as well as PMR in France). Among the 35 OECD countries, the lowest newborn mortality rates in 2016 were observed in Iceland (0.70), followed by Finland (1.90), Japan (2.00) and Slovenia (2.00) for infant mortality, Iceland (0.50), Japan (0.90), Finland (1.30) and Estonia (1.40) for neonatal mortality along with Japan (2.40), Iceland (2.50), Korea (2.80) and Finland (3.20) for perinatal mortality.
Fig. 2.
Number of infant deaths per 1,000 live births, 2016 and change 2000–2016. Source: OECD Health Statistics [27].
Fig. 3.
Number of neonatal deaths per 1,000 live births, 2016 and change 2000–2016. Source: OECD Health Statistics [27].
Fig. 4.
Number of perinatal deaths per 1,000 live births, 2016 and change 2000–2016. Source: OECD Health Statistics [27].
Since 2000, there has been a drop in the trend of newborn mortality rates observed in almost all OCED countries except in Switzerland (1.5%), Luxemburg (11.0%) and France (55.1%) with positive perinatal mortality growth and the highest reduction of newborn mortality rates were estimated in Iceland (−76.7%), followed by Estonia (−72.6%), Turkey (−64.8%) and Latvia (−64.1%) for infant mortality, in Iceland (−80.0%), Estonia (−75.9%), Latvia (−61.5%) and Slovenia (−61.1) for neonatal mortality, as well as in Turkey (−69.6%), Estonia (−60.9%), Ireland (−57.8%) and Iceland (−52.8%) for perinatal mortality. Overall, the average changes in IMR, NMR and PMR in OECD countries during 2000–2016 period were −40.2%, −39.1% and −34.0%, respectively.
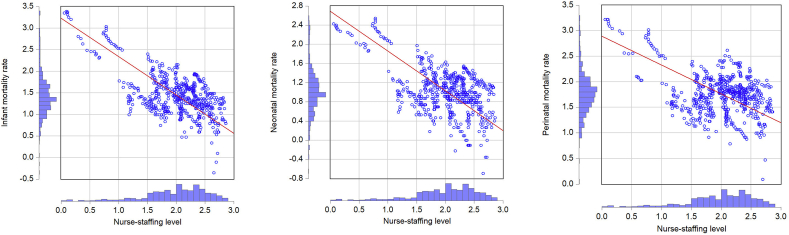
Fig. 5 relates the level of nurse staffing to newborn mortality rates (all in logs) within orthogonal non-parametric regression curve, and histogram of marginal distributions. As can be seen, there exists a clear inverse relationship from the level of practicing nurses to all newborn mortality rates. However, this finding may be spurious because of the possibility of stochastic trends in panels of our series. Thus, to provide statistical conclusion about the possible effect of nurse-staffing level on IMR, NMR and PMR, the information of unit root test and co-integration analysis in the form of panel data analysis are needed. The summary of descriptive statistics for variables is available in Appendix A.
Fig. 5.
Cross plot of logarithms of infant, neonatal and perinatal mortalities per 1,000 live births and nurse density per 1,000 population in 35 OECD countries 2000–2016.
3. Panel data analysis
Due to the nature of our data that statistically defined in cross-sectional time-series framework (35 countries during 2000–2016 period), we have the possibility to evaluate the association between nurse-staffing level and IMR, NMR and PMR in long-run using the statistical technique of panel data analysis. The instruction of panel data analysis starts with providing the essential information about the stationary process of our panel series from unit root test and continues with co-integration analysis to examine the association between the non-stationary variables. In co-integration analysis, if the existence of a co-integration relationship between the panel series is confirmed statistically, the significant coefficient of this relationship can be measured by dynamic long-run analysis. In the final step, the sensitivity of the long-run equilibrium between the co-integrated series may be analyzed with panel error correction model.
3.1. Unit root test
Unit root test is the first step in time-series analysis to identify the plausible effects of time variation on panel series i.e. whether series are stationary (mean and variance are constant in long-term) or non-stationary and possesses a unit root (mean and variance vary during time). Statistically, the null hypothesis of unit root test is the presence of stationarity based on intercept and trend stationarity according to different test models. Statistics and probabilities of several types of unit root test are available in Table 1. Due to significant statistics in level and 1st difference of integration tests, the result of unit root test verifies that nurse staffing variable was non-stationary i.e. its integration was sensitive to the trend presentation, while newborn mortality rates were stationary. Thus, the results of integration test open the way to co-integration analysis to investigate whether there existed a meaningful association between nurse-staffing level and newborn mortality rates in long-run or not.
Table 1.
Panel unit root test results (35 OECD countries, 2000–2016).
| Null hypothesis: Unit root |
Level |
1st Difference |
||
|---|---|---|---|---|
| Method | Intercept | Intercept and trend | None | Intercept |
| Nurse | ||||
| Levin, Lin & Chu t-stat | −1.95∗ | −2.40∗∗ | 10.80 | −9.39∗∗ |
| Im, Pesaran and Shin W-stat | 1.97 | 0.66 | - | −8.35∗∗ |
| ADF – Choi Z-stat | 72.66 | 65.98 | 18.52 | 195.59∗∗ |
| PP - Choi Z-stat |
144.96∗∗ |
84.02 |
15.40 |
203.84∗∗ |
| IMR | ||||
| Levin, Lin & Chu t-stat | −5.82∗∗ | −5.59∗∗ | −11.30∗∗ | −19.59∗∗ |
| Im, Pesaran and Shin W-stat | 1.62 | −4.98∗∗ | - | −19.21∗∗ |
| ADF - Choi Z-stat | 61.663 | 157.69∗∗ | 282.60∗∗ | 423.75∗∗ |
| PP - Choi Z-stat |
74.81 |
194.27∗∗ |
386.50∗∗ |
572.20∗∗ |
| NMR | ||||
| Levin, Lin & Chu t-stat | −4.24∗∗ | −9.35∗∗ | −9.48∗∗ | −27.23∗∗ |
| Im, Pesaran and Shin W-stat | 0.92 | −5.89∗∗ | - | −23.83∗∗ |
| ADF - Choi Z-stat | 60.47 | 147.65∗∗ | 253.60∗∗ | 500.45∗∗ |
| PP - Choi Z-stat |
64.50 |
184.15∗∗ |
327.00∗∗ |
605.34∗∗ |
| PMR | ||||
| Levin, Lin & Chu t-stat | −2.29∗ | −9.19∗∗ | −9.59∗∗ | −23.73∗∗ |
| Im, Pesaran and Shin W-stat | 0.39 | −5.23∗∗ | - | −20.84∗∗ |
| ADF - Choi Z-stat | 84.62 | 143.62∗∗ | 224.10∗∗ | 446.24∗∗ |
| PP - Choi Z-stat | 87.70 | 153.40∗∗ | 351.70∗∗ | 617.45∗∗ |
Notes: Null hypothesis was no integration and the optimum lag lengths were selected by Schwarz Information Criterion (SIC) from 0 to 3; ∗P < 0.05 and ∗∗P < 0.01; OECD = Organisation for Economic Co-operation and Development; IMR = infant mortality rates; NMR = neonatal mortality rates; PMR = neonatal mortality rates.
3.2. Co-integration analysis
In this step, we examine the existence of long-run relationship between the level of nurse staffing and newborn mortality series in the form of co-integration analysis. The results of Pedroni panel co-integration test [28,29] based on Engle-Granger model are reported in Table 2 and confirm that nurse staffing series and IMR, NMR and PMR were significantly co-integrated in the long-run.
Table 2.
Pedroni co-integration test (35 OECD countries, 2000–2016).
| Co-integration test between | Pedroni’s criteria | Unweighted |
Weighted |
Conclusion | ||
|---|---|---|---|---|---|---|
| Statistic | P | Statistic | P | |||
| Nurse & IMR |
Panel v-Statistic | 2.21 | 0.013 | 1.86 | 0.031 | Co-integrated |
| Panel rho-Statistic | −1.86 | 0.031 | −2.25 | 0.012 | ||
| Panel PP-Statistic | −2.68 | 0.003 | −3.65 | 0.000 | ||
| Panel ADF-Statistic | −2.94 | 0.001 | −4.06 | 0.000 | ||
| Group rho-Statistic | −0.75 | 0.225 | ||||
| Group PP-Statistic | −4.58 | 0.000 | ||||
| Group ADF-Statistic |
−5.02 |
0.000 |
||||
| Nurse & NMR |
Panel v-Statistic | 0.82 | 0.206 | 0.72 | 0.235 | Co-integrated |
| Panel rho-Statistic | −1.51 | 0.065 | −1.80 | 0.035 | ||
| Panel PP-Statistic | −2.15 | 0.015 | −3.55 | 0.000 | ||
| Panel ADF-Statistic | −1.19 | 0.115 | −3.47 | 0.000 | ||
| Group rho-Statistic | −0.77 | 0.218 | ||||
| Group PP-Statistic | −4.78 | 0.000 | ||||
| Group ADF-Statistic |
−4.77 |
0.000 |
||||
| Nurse & PMR | Panel v-Statistic | −1.15 | 0.876 | −0.78 | 0.781 | Co-integrated |
| Panel rho-Statistic | 0.32 | 0.627 | 0.13 | 0.555 | ||
| Panel PP-Statistic | −1.62 | 0.052 | −1.57 | 0.057 | ||
| Panel ADF-Statistic | −2.39 | 0.008 | −1.87 | 0.030 | ||
| Group rho-Statistic | 1.18 | 0.881 | ||||
| Group PP-Statistic | −1.63 | 0.050 | ||||
| Group ADF-Statistic | −1.83 | 0.033 | ||||
Notes: Null hypothesis was no co-integration and the optimum lag lengths were selected by SIC (from 0 to 9); OECD = Organisation for Economic Co-operation and Development; IMR = infant mortality rates; NMR = neonatal mortality rates; PMR = perinatal mortality rate.
3.3. Dynamic long-run analysis
Based on the results of Pedroni co-integration test, there existed a significant relationship between nurse-staffing level and newborn mortality rates in long-run. The aim of this step is to calculate the magnitudes of these relationships based on dynamic long-run analysis in panel and pooled data frameworks. Results of dynamic long-run models demonstrate that the long-run elasticities of nurse staffing on IMR, NMR and PMR were −0.98, −0.97 and −0.96, respectively. In another word, one percent rise in the number of nurses’ density per 1000 population would decline the rates of infant, neonatal and perinatal mortality per 1,000 child births about one percent in long-run. Results of dynamic long-run panel models are available in Table 3.
Table 3.
Dynamic long-run models: panel fixed-effect with cross-section weights (35 OECD countries, 2000–2016).
| Dependent Variable | Variable | Coefficient | Std. Error | t | P | r2 | Durbin-Watson |
|---|---|---|---|---|---|---|---|
| IMR |
Constant | 0.4828 | 0.09 | 4.82 | 0.000 | 0.992 |
2.58 |
| Nurse(-1) | −0.1407 | 0.03 | −3.80 | 0.000 | |||
| IMR(-1) |
0.8381 |
0.02 |
38.30 |
0.000 |
|||
| Long-run elasticity of effect nurse had on IMR: −0.1407/(1–0.8381) = −0.9789 | |||||||
| NMR |
Constant | 0.5840 | 0.09 | 6.05 | 0.000 | 0.986 |
2.55 |
| Nurse(-1) | −0.1935 | 0.03 | −5.07 | 0.000 | |||
| NMR(-1) |
0.7791 |
0.02 |
30.85 |
0.000 |
|||
| Long-run elasticity of effect nurse had on NMR: −0.1935/(1–0.7791) = −0.9727 | |||||||
| PMR |
Constant | 0.6166 | 0.09 | 6.29 | 0.000 | 0.983 |
2.54 |
| Nurse(-1) | −0.1499 | 0.03 | −4.57 | 0.000 | |||
| PMR(-1) |
0.8069 |
0.02 |
33.55 |
0.000 |
|||
| Long-run elasticity of effect nurse had on PMR: −0.1499/(1–0.8069) = −0.9569 | |||||||
Notes: OECD = Organisation for Economic Co-operation and Development; IMR = infant mortality rates; NMR = neonatal mortality rates; PMR = perinatal mortality rate.
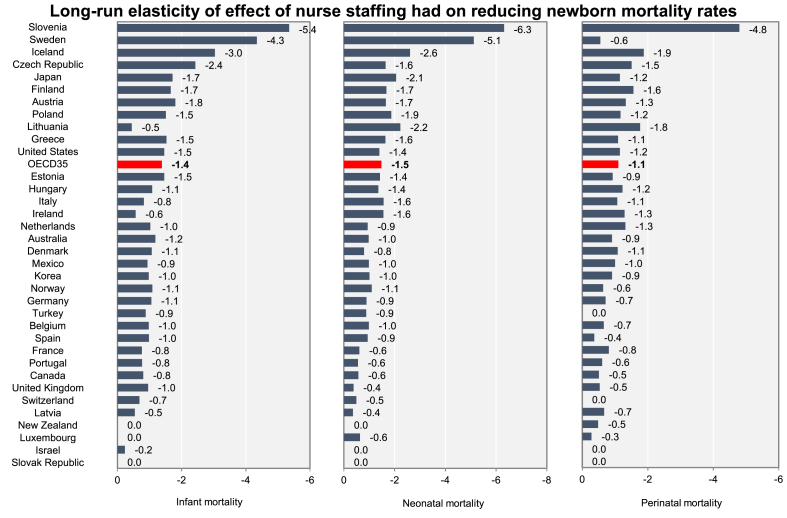
Dynamic long-run model analysis based on pooled data framework is used in this step to calculate the magnitude of the effect nurses had on distinct types of newborn deaths in every country. Result of panel fixed effect method with cross-sectional weights is available in Table 4 and Fig. 6. The highest magnitude of nurse-staffing level on infant mortality reduction per 1,000 births in long-run was estimated in Slovenia with −5.35, followed by Sweden with −4.35, Iceland with −3.04 and Czech Republic with −2.43. By contrast, the lowest magnitudes of this relationship were investigated in Ireland (−0.57), Latvia (−0.54), Lithuania (−0.45) and Israel (−0.24). There was not any committed relationship from nurse density per 1,000 population to IMR in Luxembourg, New Zealand and Slovak Republic and for the rest of countries, the range of this long-run elasticity was between −1.81 in Austria and −0.69 in Switzerland with the average of −2.02 for OECD.
Table 4.
Dynamic long-run model: pooled fixed-effect with cross-section weights (35 OECD countries, 2000–2016).
| Countries | Magnitude of the effect nurse had on: |
|||
|---|---|---|---|---|
| IMR | NMR | PMR | Average | |
| Australia | −1.1827 | −0.9772 | −0.9141 | −1.0247 |
| Austria | −1.8059 | −1.6519 | −1.3311 | −1.5963 |
| Belgium | −0.9789 | −0.9901 | −0.6613 | −0.8768 |
| Canada | −0.8061 | −0.5732 | −0.5109 | −0.6301 |
| Czech Republic | −2.4285 | −1.6470 | −1.5122 | −1.8626 |
| Denmark | −1.0740 | −0.7967 | −1.0858 | −0.9855 |
| Estonia | −1.4654 | −1.4273 | −0.9296 | −1.2741 |
| Finland | −1.6629 | −1.6793 | −1.5650 | −1.6358 |
| France | −0.7668 | −0.6107 | −0.8150 | −0.7309 |
| Germany | −1.0606 | −0.8944 | −0.7135 | −0.8895 |
| Greece | −1.5316 | −1.6387 | −1.0964 | −1.4222 |
| Hungary | −1.0847 | −1.3608 | −1.2343 | −1.2266 |
| Iceland | −3.0402 | −2.6095 | −1.8770 | −2.5089 |
| Ireland | −0.5678 | −1.5568 | −1.2940 | −1.1395 |
| Israel | −0.2379 | No significant | No significant | −0.2379 |
| Italy | −0.8248 | −1.5712 | −1.0707 | −1.1556 |
| Japan | −1.7175 | −2.0580 | −1.1547 | −1.6434 |
| Korea | −0.9777 | −1.0120 | −0.9142 | −0.9680 |
| Latvia | −0.5443 | −0.3575 | −0.6738 | −0.5252 |
| Lithuania | −0.4531 | −2.2298 | −1.7688 | −1.4839 |
| Luxembourg | No significant | −0.6339 | −0.2847 | −0.4593 |
| Mexico | −0.9433 | −0.9865 | −1.0019 | −0.9772 |
| Netherlands | −1.0282 | −0.9373 | −1.3173 | −1.0943 |
| New Zealand | No significant | No significant | −0.4876 | −0.4876 |
| Norway | −1.0927 | −1.0972 | −0.6403 | −0.9434 |
| Poland | −1.5128 | −1.8684 | −1.1697 | −1.5170 |
| Portugal | −0.7740 | −0.5611 | −0.6078 | −0.6476 |
| Slovak Republic | No significant | No significant | No significant | 0.0000 |
| Slovenia | −5.3534 | −6.3165 | −4.7989 | −5.4896 |
| Spain | −0.9846 | −0.9403 | −0.3663 | −0.7637 |
| Sweden | −4.3460 | −5.1244 | −0.5560 | −3.3422 |
| Switzerland | −0.6877 | −0.4915 | No significant | −0.5896 |
| Turkey | −0.8830 | −0.8859 | No significant | −0.8845 |
| United Kingdom | −0.9594 | −0.3824 | −0.5338 | −0.6252 |
| United States | −1.4608 | −1.4006 | −1.1526 | −1.3380 |
| OECD35 | −1.3824 | −1.4771 | −1.0980 | - |
Note: Dynamic long-run models for individual countries were the same as panel models in Table 3; OECD = Organisation for Economic Co-operation and Development; IMR = infant mortality rates; NMR = neonatal mortality rates; PMR = perinatal mortality rate.
Fig. 6.
Long-run elasticity of effect of nurses’ density per 1000 population on newborn mortality rates (2000–2016).
The highest magnitude of role of practicing nurses on NMR reduction in long-run was calculated Slovenia (−6.32), followed by Sweden (−5.12), Iceland (−2.61) and Lithuania (−2.23). For the rest of developed countries, the range of this magnitude was simulated between −2.06 in Japan and −0.36 in Latvia with the average of −1.48 for OECD countries, except in Israel, New Zealand and Slovak Republic which there was not any significant relationship between nurse-staffing level and NMR.
Slovenia with −4.80, followed by Iceland with −1.88, Lithuania with −1.77 and Finland with −1.56 had the highest magnitudes of the effect nurse staffing had on decreasing perinatal mortality per 1,000 live births in long-run. By contrast, Canada (−0.51), New Zealand (−0.49), Spain (−0.37) and Luxembourg (−0.28) had the lowest magnitudes of association between nurses and PMR, whereas there was no evidence for the possibility of such a relationship in Israel, Slovak Republic, Switzerland and Turkey in long-run. The magnitude of this relationship for the rest of OECD had a range from −1.15 in Czech Republic to −0.53 in United Kingdom with the average of −1.10 for OECD countries.
Overall, nurse-staffing level had the highest effect on declining the average of newborn mortality rates in Slovenia (−5.50), followed by Sweden (−3.34), Iceland (−2.51), Czech Republic (−1.86), Japan (−1.64) and Finland (−1.64). By contrast, the lowest effect of nurses on dropping the trend of newborn mortality rates in long-run were estimated in Latvia (−0.52), New Zealand (−0.49), Luxembourg (−0.46) and Israel (−0.24) and there was not any evidence for concluding the existence of association between these series in Slovak Republic.
3.4. Panel error correction model
As the results of panel data analysis confirmed the existence of meaningful association between nurse staffing and infant, neonatal and perinatal mortalities in long-run, it would be interesting to analyze if an external factor such as nursing shortage disrupt the long-run equilibrium between these variables, what would be the speed of correcting back to long-run steady state. To examine this, the result of panel error correction model is presented in Table 5 and proves that if the long-run relationship between practicing nurses level and newborn mortality rates are disturbed with nursing shortage, then it takes at least 17 years (1/0.0585) for IMR, 15 years for NMR (1/0.0659) and 17 years (1/0.0599) for PMR to restore back to the previous long-run equilibrium with nurse staffing.
Table 5.
Panel error correction model (35 OECD countries, 2000–2016).
| Dependent variable | Variable | Coefficient | Std. Error | t | P | r2 | Durbin-Watson |
|---|---|---|---|---|---|---|---|
| ΔIMR |
Constant | −0.0329 | 0.00 | −5.27 | 0.000 | 0.027 |
2.50 |
| ΔNurse | −0.0718 | 0.19 | −0.35 | 0.719 | |||
| EC(-1) |
−0.0585 |
0.01 |
−3.93 |
0.000 |
|||
| ΔNMR |
Constant | −0.0321 | 0.00 | −4.48 | 0.000 | 0.028 |
2.55 |
| ΔNurse | 0.0357 | 0.22 | 0.15 | 0.876 | |||
| EC(-1) |
−0.0659 |
0.01 |
−4.02 |
0.000 |
|||
| ΔPMR | Constant | −0.0243 | 0.00 | −3.85 | 0.000 | 0.027 | 2.91 |
| ΔNurse | −0.0134 | 0.20 | −0.06 | 0.946 | |||
| EC(-1) | −0.0599 | 0.01 | −3.96 | 0.000 |
Notes: EC means the error correction term, i.e. the residuals from the static long run panel model between the series. The optimum lag lengths were selected by SIC (from 0 to 3); OECD = Organisation for Economic Co-operation and Development; IMR = infant mortality rates; NMR = neonatal mortality rates; PMR = perinatal mortality rate.
4. Discussion
There has been much interest in measuring the possible role of nursing-related services due to the level of nurse staffing in proficiency of mothers and newborns care management. To our knowledge, there is a lack of cross-national studies to examine the association between practicing nurses and reducing newborn mortality rates in OECD countries. Across the traditional statistical approaches used in nursing research which typically have relied on stochastic models [9], this article considered the effects of time variation on the relationship between professional nurses’ density per 1,000 population and newborn mortality rates, including IMR, NMR and PMR, using the most comprehensive source of cross-national observations across OECD countries. The statistical technique of panel data analysis was conducted to calculate the magnitudes of the role of nurse staffing in reducing newborn mortality rates using a panel of 35 OECD countries during the period of 2000–2016.
Result of unit root test verified that nurse staffing series were nonstationary which opened the way to dynamic long-run analysis based on panel and pooled estimations. According to the results of co-integration analysis and panel dynamic long-run models, there were meaningful associations between the level of nurse staffing and IMR, NMR and PMR in the long-run and the elasticity of these relationships in OECD countries were −0.98, −0.97 and −0.96, respectively. Overall, the impact of practicing nurses on decreasing the average of newborn mortality rates in the long-run were recorded at the highest level in Slovenia, Sweden, Iceland, Czech Republic, Japan and Finland. On the other hand, the lowest effect of nurse staffing on declining the long-run trend of newborn mortality rates were estimated in Latvia, New Zealand, Luxembourg and Israel. In addition, the result of panel error correction model verified that if the long-run association between nurse-staffing level and newborn mortality rates are disturbed with nursing shortage, e.g. in Slovak Republic and Israel, then it takes at least 17 years for mortality rates to restore back to the previous long-run equilibriums.
In all, the results of this study highlight the significant association between higher levels of nurse staffing and lower newborn mortality rates in developed countries. Moreover, as the effects of nurse staffing on improving the health level of newborns are at the highest level in Slovenia, Sweden, Iceland, Czech Republic, Japan and Finland among the other OECD countries, the recommendation for the other countries is to pattern the hospital nursing characteristics in mothers and newborns care management of this group of countries. A principal direction of future research is to explore what factors drive the efficiency of nursing care on newborn health as well as analyze if the current trends continue across the countries to monitor the possible effect of nursing shortage.
Due to the lack of data, the missing of relevant control variables like the level of nursing education, years of work experience etc. in statistical analysis was the limitation of this study. As the lack of data availability is the biggest obstacle in nursing research, it is recommended by OECD and the Commission on Information and Accountability for Women’s and Children’s Health in WHO along with other relevant organizations, in co-operating with researchers, to support countries in collecting and analyzing cross-national observations, which can be used to further study the interaction between nursing characteristics and health outcomes [[30], [31], [32]].
Funding
No funding to declare.
CRediT authorship contribution statement
Arshia Amiri: Conceptualization, Methodology, Software, Data curation, Writing - original draft, Visualization, Investigation, Writing - review & editing. Katri Vehviläinen-Julkunen: Validation, Writing - review & editing. Tytti Solankallio-Vahteri: Validation, Writing - review & editing. Sirpa Tuomi: Validation, Writing - review & editing.
Declaration of competing interest
The authors have declared that no conflicts of interest exist.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2020.02.002.
Appendices. Supplementary data
The following is the supplementary data to this article:
References
- 1.OECD . Health at a glance 2017: OECD indicators. OECD Publishing; Paris: 2017. Infant mortality. [DOI] [Google Scholar]
- 2.OECD . Health at a glance 2015: OECD indicators. OECD Publishing; Paris: 2015. Infant mortality. [DOI] [Google Scholar]
- 3.OECD . Health at a glance 2017: OECD indicators. OECD Publishing; Paris: 2017. Nurses. [DOI] [Google Scholar]
- 4.Park J., Kim J.S. Factors influencing developmental care practice among neonatal intensive care unit nurses. J Pediatr Nurs. 2019;47:e10–e15. doi: 10.1016/j.pedn.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 5.Symon A., McFadden A., White M., Fraser K., Cummins A. Using the Quality Maternal and Newborn Care Framework to evaluate women’s experiences of different models of care: a qualitative study. Midwifery. 2019;73:26–34. doi: 10.1016/j.midw.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Kane R.L., Shamliyan T., Mueller C., Duval S., Wilt T. The association of registered nurse staffing levels and patient outcomes systematic review and meta-analysis. Med Care. 2007;45(12):1195–1204. doi: 10.1097/MLR.0b013e3181468ca3. [DOI] [PubMed] [Google Scholar]
- 7.Shekelle P.G. Nurse–patient ratios as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158:404–409. doi: 10.7326/0003-4819-158-5-201303051-00007. [DOI] [PubMed] [Google Scholar]
- 8.Brownie S.M. The economic impact of nursing. J Clin Nurs. 2018;27:3825–3826. doi: 10.1111/jocn.14182. [DOI] [PubMed] [Google Scholar]
- 9.Amiri A., Solankallio-Vahteri T. Nurse-staffing level and quality of acute care services: evidence from cross-national panel data analysis in OECD countries. Int J Nurs Sci. 2019;6(1):6–16. doi: 10.1016/j.ijnss.2018.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aiken L.H., Clarke S.P., Sloane D.M., Sochalski J., Silber J.H. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. J Am Med Assoc. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 11.Estabrooks C.A., Midodzi W.K., Cummings G.G., Ricker K.L., Giovannetti P. The impact of hospital nursing characteristics on 30-day mortality. Nurs Res. 2005;54(2):74–84. doi: 10.1097/00006199-200503000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Rafferty A.M., Clarke S.P., Coles J., Ball J., James P., McKee M. Outcomes of variation in hospital nurse staffing in English hospitals: cross-sectional analysis of survey data and discharge records. Int J Nurs Stud. 2007;44(2):175–182. doi: 10.1016/j.ijnurstu.2006.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van den Heede K., Lesaffre E., Diya L., Vleugels A., Clarke S.P., Aiken L.H. The relationship between inpatient cardiac surgery mortality and nurse numbers and educational level: analysis of administrative data. Int J Nurs Stud. 2009;46(6):796–803. doi: 10.1016/j.ijnurstu.2008.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aiken L.H., Cimiotti J.P., Sloane D.M., Smith L., Flynn L., Neff D.F. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Med Care. 2011;49(12):1047–1053. doi: 10.1097/MLR.0b013e3182330b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aiken L.H., Sloane D.M., Bruyneel L., van Den Heede K., Griffiths P., Busse R. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet. 2014;383(9931):1824–1830. doi: 10.1016/S0140-6736(13)62631-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cho E., Sloane D.M., Kim E.Y., Kim S., Choi M., Yoo I.Y. Effects of nurse staffing, work environments, and education on patient mortality: an observational study. Int J Nurs Stud. 2015;52(2):535–542. doi: 10.1016/j.ijnurstu.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manojlovich M. Increasing nurse staffing levels and a higher proportion with bachelor’s degrees could decrease patient mortality risk. Evid Base Nurs. 2015;18(2):62. doi: 10.1136/eb-2014-101913. [DOI] [PubMed] [Google Scholar]
- 18.Aiken L.H., Cerón C., Simonetti M., Lake E.T., Galiano A., Garbarini A. Hospital nurse staffing and patient outcomes. Revista Médica Clínica Las Condes. 2018;29(3):322–327. doi: 10.1016/j.rmclc.2018.04.011. [DOI] [Google Scholar]
- 19.Aiken L.H., Sermeus W., Van den Heede K., Sloane D.M., Busse R., McKee M. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012;344:e1717. doi: 10.1136/bmj.e1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu Y., Fujita S., Seto K., Ito S., Matsumoto K., Huang C.C. The impact of nurse working hours on patient safety culture: a cross-national survey including Japan, the United States and Chinese Taiwan using the Hospital Survey on Patient Safety Culture. BMC Health Serv Res. 2013;13:394. doi: 10.1186/1472-6963-13-394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ausserhofer D., Zander B., Busse R., Schubert M., De Geest S., Rafferty A.M. Prevalence, patterns and predictors of nursing care left undone in European hospitals: results from the multicountry cross-sectional RN4CAST study. BMJ Qual Saf. 2014;23(2):126–135. doi: 10.1136/bmjqs-2013-002318. [DOI] [PubMed] [Google Scholar]
- 22.Cho E., Lee N.J., Kim E.Y., Kim S., Lee K., Park K.O., Sung Nurse staffing level and overtime associated with patient safety, quality of care, and care left undone in hospitals: a cross-sectional study. Int J Nurs Stud. 2016;60:263–271. doi: 10.1016/j.ijnurstu.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 23.Amiri A., Solankallio-Vahteri T., Tuomi S. Role of nurses in improving patient safety: evidence from surgical complications in 21 countries. Int J Nurs Sci. 2019;6(3):239–246. doi: 10.1016/j.ijnss.2019.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.OECD Nurses (indicator) 2018. [DOI]
- 25.Amiri A., Solankallio-Vahteri T. Analyzing economic feasibility for investing in nursing care: evidence from panel data analysis in 35 OECD countries. Int J Nurs Sci. 2019 doi: 10.1016/j.ijnss.2019.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amiri A., Solankallio-Vahteri T. Nurse staffing and life expectancy at birth and at 65 years old: evidence from 35 OECD countries. Int J Nurs Sci. 2019 doi: 10.1016/j.ijnss.2019.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.OECD Health Statistics Health status. 2018. https://stats.oecd.org/Index.aspx?DataSetCode=HEALTH_HCQI
- 28.Pedroni P. Critical values for cointegration tests in heterogeneous panels with multiple regressors. Oxf Bull Econ Stat. 1999;61(S1):653–670. doi: 10.1111/1468-0084.0610s1653. [DOI] [Google Scholar]
- 29.Pedroni P. Panel cointegration; asymptotic and finite sample properties of pooled time series tests with an application to the PPP hypothesis. Econ Theor. 2004;20:597–625. doi: 10.1017/S0266466604203073. [DOI] [Google Scholar]
- 30.Amiri A., Linden M. Impact of child health on economic growth: New evidence based on Granger non-causality tests. Econ Bull. 2016;36(2):1127–1137. [Google Scholar]
- 31.Amiri A., Ventelou B. Granger causality between total expenditure on health and GDP in OECD: evidence from the Toda-Yamamoto approach. Econ Lett. 2012;116(3):541–544. doi: 10.1016/j.econlet.2012.04.040. [DOI] [Google Scholar]
- 32.Amiri A., Gerdtham U., Ventelou B. HIV/AIDS-GDP Nexus? Evidence from panel-data for African countries. Econ Bull. 2012;32(1):1060–1067. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.