Abstract
Background: This study aimed at investigating haematological changes in malaria patients across different demographic settlements. Malaria parasites trigger changes in certain haematological parameters, which may result in a number of clinical manifestations. Differences in demographic settlements, such as rural, peri-urban and urban settlements, may also influence these changes, but this has rarely been studied.
Methods: We conducted a hospital-based, cross-sectional study from January to December 2018 in three different settlements. A total of 598 participants were recruited. Giemsa-stained blood smears were examined to detect and quantify malaria parasitaemia, while haematological parameters were measured using a haematology analyser.
Results: The rural settlement had the highest malaria prevalence compared to the other study communities (p=0.009). The difference in parasite densities across the three communities was also significant (p=0.0149). When the malaria-infected population was compared to the uninfected, there were differences in red blood cell count (p=0.0170), haemoglobin levels (p=0.0165), mean corpuscular volume (p=0.0139) and platelet counts (p<0.0001). The difference in median white blood cell (p-value <0.0001), neutrophil (p-value <0.0001) and lymphocyte (p-value <0.0269) count were significantly higher in infected patients from the peri-urban area compared to malaria patients from the rural and urban areas. There were also significant differences in platelet ( p=0.0002), plateletcrit ( p=0.0041), mean platelet volume ( p=0.0009) and platelet large cell ratio ( p=0.0046) levels between patients from the urban, peri-urban and rural areas.
Conclusions: Patients infected with malaria generally had low red blood cell, haemoglobin and platelets in comparison to uninfected patients. There were also significant differences in several haematological parameters between malaria-infected patients from the three demographic settlements. Atypical results from routine haematological assays, especially findings of anaemia and thrombocytopenia, may be indicative of malaria and, in cases where the infection is asymptomatic, may improve diagnosis by prompting a more thorough search for the parasite in the peripheral circulation.
Keywords: malaria, anaemia, parasitaemia, WBC count, thrombocytopeania
Introduction
Malaria remains the most important protozoan infection of humans and continues to have an immense impact on the health and quality of life of people across the world. Despite the decrease in incidence of mortality due to malaria in the last decade, the most recent World Malaria Report revealed that malaria cases increased by about two million in 2018 compared to 2017, resulting in approximately 435,000 deaths, the majority of which were reported in sub-Saharan Africa 1.
The introduction of malaria parasites into the host peripheral blood by an infected female Anopheles mosquito triggers changes in many host haematological parameters. These changes may subsequently affect the general physiology of the host, resulting in a number of clinical manifestations 2, 3. In fact, the most common complications arising from malaria are associated with changes in host haematological parameters that play a role in malaria pathogenesis, with thrombocytopenia being the most common 4. Haematological parameters that are most often affected include the relative numbers of circulating cell types such as platelets, granulocytes, lymphocytes and erythrocytes, as well as parameters like haemoglobin concentration. A recent study showed a significant reduction in platelet, erythrocyte and leukocyte levels in malaria-infected study participants compared to the control group 5. Moreover, Kotepui et al. (2014) reported that low platelet, white blood cell (WBC) and lymphocyte counts are important predictors of malaria infection and, when used with other clinical methods, could improve malaria diagnosis and treatment 6. Yet another study has reported elevated leukocyte levels in the malaria-infected group compared to uninfected study participants 7.
While haematological changes associated with malaria have been well-characterized 6, 8, 9, it is possible that factors such as differences in demographic settlements also influence observed changes. However, there is relatively limited data on the differences in haematological indices of malaria patients in rural, peri-urban and urban settlements, especially in forested zones. The aim of this study was to investigate haematological changes that occur in malaria patients across these different settlements.
Methods
This is a hospital-based study. In order to avoid bias and prevent including only ‘sick' or symptomatic participants, we extended our sampling to include ‘healthy' participants who accompanied their relatives or friends to the hospital. This increased the chance of having both symptomatic and asymptomatic participants.
Ethical statement
The protocol for data collection was reviewed and approved by the Committee on Human Research Publication and Ethics of the Kwame Nkrumah University of Science and Technology (KNUST) and the Komfo Anokye Teaching Hospital (CHRPE/KATH). All study participants provided written informed consent prior to study enrolment, with parental or guardian consent obtained for children.
Study sites
We carried out a hospital-based, cross-sectional study that was conducted concurrently at the Kumasi South Hospital (KSH), the Kuntanase Government Hospital (KGH) and the Agona Government Hospital (AGH) in the Ashanti region of Ghana. KSH is located in Atonsu, a suburb of Kumasi, the regional capital and second largest city in Ghana, and served as the urban site. KGH is situated in Kuntanase, the capital of the Bosomtwe district. The Bosomtwe district is one of the 27 districts in the Ashanti region and is located approximately 28 kilometers from Kumasi. AGH is in the Sekyere East district and is located approximately 37 kilometres away from Kumasi. KGH and AGH served as the peri-urban and rural study sites, respectively.
Study participants
The sample size was determined using the binomial model. Confidence intervals of 95% and a precision level of 5% was used. In the equation below, n is the sample size, z is the critical value of the standard normal distribution at 5% level (1.96), p is the estimated malaria prevalence, q = 1 – p and d is the precision level. The prevalence of malaria had previously been determined by Paintsil et al. (2019) to be about 26% 10.
The minimum sample size required was calculated to be 295; however, we sampled 601 participants to make up for the different transmission seasons (January to December 2018) across which samples were collected. The study targeted patients accessing healthcare at the various hospitals. They included patients referred to the laboratory for malaria test and accompanying caregivers who were not sick. The purpose of the study was explained to potential participants using a participant information leaflet to seek their informed consent, a copy of which is provided as Extended data 11. An interpreter was employed to translate the written document into their local dialect (Akan) for those who could not read. In addition, thumbprints were obtained for those who could not sign/write. Patients who were critically ill and those refusing consent were excluded from the study. All age groups were considered for the study except infants under six months. Demographic data such as malaria drug use and insecticide-treated net (ITN) use were obtained from participants using a semi-structured questionnaire, a copy of which is provided as Extended data 11.
Haematological analysis
From each participant, 2 ml of venous blood was drawn by a trained phlebotomist in the hospital laboratory as part of their routine medical care. This was transferred into an EDTA tube with a unique patient identifier. The blood sample was used to prepare thin and thick films for microscopic examination and automated complete blood counts (CBCs). Blood parameters were estimated using the Sysmex XP-300 Automated Haematology Analyzer. The cell counter provided data on red blood cell (RBC) count, haemoglobin (Hb) level, mean corpuscular volume (MCV), mean corpuscular haemoglobin (MCH) level, WBC, lymphocyte, neutrophil, platelet counts, mean platelet volume (MPV), plateletcrit and the red blood cell distribution width (RDW).
Parasitological analysis
From the EDTA-treated blood, 6 µL and 3 µL were used to prepare thick and thin blood films, respectively. After air-drying, the thin blood smears were fixed with methanol and both smears subsequently stained with 10% Giemsa for 15 minutes. Two experienced microscopists independently examined the slides under ×100 oil immersion to determine the presence or absence of malaria parasites. Parasites were quantified after counting 200 or 500 WBCs. Parasite densities were calculated as parasite per microliter of blood (parasite counted / WBCs counted × total WBC in 1µL of blood). A slide was only declared negative when no malaria parasite was seen after scanning 100 high power fields (HPFs).
Statistical analysis
The data collected were coded and entered into Microsoft Excel 2016. The data were checked for completeness. Samples with missing data were excluded from the analysis. Thus, three samples with missing microscopy data were excluded completely from all analysis. Data analysis was performed using GraphPad Prism v6 (GraphPad Software, Inc., San Diego, CA, USA). Data normality was checked using the Shapiro-Wilk normality test. For normally distributed data, comparisons were carried out using one-way ANOVA, whilst data not conforming to the normal distribution were compared using the Kruskall-Wallis or Mann-Whitney Tests. Pairwise multiple comparison across communities was done using Dunn’s multiple comparison test. Categorical data on community and age groups were compared using Pearson’s chi-squared test. Results were considered statistically significant if p ≤ 0.05.
Results
Three samples had demographic data only and thus were excluded completely. In total, 598 participants samples were examined for parasite prevalence and density of infections. A further 16 were excluded from the haematological analysis because the sample obtained was either too small or the haematological indices were not determined.
Out of the 598 analysed in the study, 75.4% ( n=451) were female 11. While the overall median age was 27 years ( IQR=19–40), there was a statistically significant difference in the age profiles of patients from the three study sites ( p<0.0001). Patients in the rural area were comparatively younger, with a median age of 24.5 years ( IQR=14–35), followed by those in the peri-urban area, with a median age of 27 years ( IQR=19.5–41.5). Patients in the urban area were the oldest, with a median age of 29 years ( IQR=22.5–43.0). This observation is conceivable because, typically, the youth tend to leave their rural communities in search of jobs as they get older. 16% ( n=93) of study participants had Plasmodium falciparum infection, confirmed by microscopy, while the remaining uninfected patients were used as controls.
Malaria causes significant changes in several haematological parameters
The median haematological parameters of the infected and non-malaria groups were compared using the Mann-Whitney test due to the non-parametric distribution of the data. There was no significant difference in the median counts of neutrophils, lymphocytes or WBCs between the infected and non-infected groups; however, malaria-infected patients in our study population ( n=93) had significantly lower median values of RBCs ( p=0.017), Hb ( p=0.0165), haematocrit ( p=0.0015), MCV ( p=0.00139), platelets ( p<0.0001) and plateletcrit ( p<0.0001) compared to control patients ( Table 1).
Table 1. Levels of haematological parameters in infected vs uninfected study participants.
| Variable | Malaria-infected | Uninfected | P-value |
|---|---|---|---|
| Median (IQR) | Median (IQR) | ||
| Red blood cells (RBC) (×10 6 /µL) a | 4.16 (3.78 – 4.67) | 4.42 (3.93 – 4.85) | 0.0170 |
| Haemoglobin (g/dL) a | 11.10 (9.5 – 12.4) | 11.60 (10.40 – 12.80) | 0.0165 |
| Haematocrit (%) a | 39.30 (34.40 – 44.60) | 42.80 (38.20 – 46.20) | 0.0015 |
| Mean corpuscular volume (MCV) (fL) a | 94.20 (89.3 – 100.5) | 97.80 (91.70 – 102.70) | 0.00139 |
| Mean corpuscular haemoglobin (MCH) (pg) a | 26.60 (25.2 – 28.0) | 26.80 (24.80 – 28.50) | 0.5413 |
| Red cell distribution width (RDW-SD) (fL) a | 50.90 (47.40 – 57.10) | 51.00( 47.70 – 57.40) | 0.7782 |
| Red cell distribution width (RDW-CV) (%) a | 14.30 (14.30 – 15.90) | 13.80 (12.60 – 15.80) | 0.1482 |
| Platelet (×10 3/µL) a | 128.00 (72.0 – 186.0) | 172 (119.0 – 229.0) | <0.0001 |
| Plateletcrit (PCT) (%) a | 0.15 (0.08 – 0.22) | 0.20 (0.13 – 0.26) | <0.0001 |
| Platelet distribution width (PDW) (fL) a | 16.30 (14.30 – 19.60) | 16.20 (13.60 – 19.05) | 0.1544 |
| Mean platelet volume (MPV) (fL) a | 11.20 (10.20 – 12.30) | 11.20 (10.10 – 12.20) | 0.9878 |
| Platelet large cell ratio (P-LCR) (%) a | 35.70 (29.40 – 43.0) | 35.50 (28.30 – 43.90) | 0.7465 |
| White blood cells (WBC) (×10 3/µL) b | 3.50 (2.20 – 5.35) | 3.50 (2.40 – 4.80) | 0.5078 |
| Neutrophil (×10 3/µL) a | 1.00 (0.50 – 2.10) | 1.00 (0.70 – 1.70) | 0.9702 |
| Lymphocyte (×10 3/µL) a | 1.80 (1.20 – 3.0) | 2.20 (1.50 – 3.10) | 0.8222 |
aT.test; bMan-Whitney U; IQR=Interquartile range
ITN usage and malaria prevalence vary significantly with age and settlement
There was a significant relationship between ITN usage and malaria prevalence ( χ 2=48.41; p<0.0001). When we tested the relationship between these two variables and age or settlement, we found a statistically-significant association between age and ITN usage ( p<0.0001), with children less than five years constituting the majority of those who slept under insecticide-treated mosquito nets, while children between the ages of six and 14 (inclusive) recorded the lowest ITN usage. Malaria prevalence was also significantly related to age ( p<0.0001), with the highest prevalence seen in children from six to 14 years of age ( Table 2). Furthermore, there was a significant difference in the parasite densities of infected patients across the different age groups ( H=8.64; p=0.0133). Children under five years harboured the highest number of parasites, with a median parasite density of 665 (IQR=327–1038), followed by patients 6–14 years, with a median density of 504 ( IQR=160–4139), and patients ≥15 years, with a median density of 24.5 ( IQR=13–40).
Table 2. Relationship between age & settlement type and insecticide-treated net (ITN) usage & malaria prevalence.
| ITN usage (%) | χ 2 | P-value | Malaria prevalence | χ 2 | P-value | |
|---|---|---|---|---|---|---|
| Age | ||||||
| 0–5 | 58.9 | 26.8 | ||||
| 6–14 | 28.9 | 34.8 | ||||
| 15+ | 30.2 | 34.34 | <0.0001 | 12.7 | 21.29 | <0.0001 |
| Settlement | ||||||
| Urban | 32.3 | 11.8 | ||||
| Peri-urban | 29.2 | 13.3 | ||||
| Rural | 30.3 | 10.73 | 0.0017 | 21.3 | 8.05 | 0.0179 |
χ 2 is the chi-squared value. The results were considered significant if p ≤ 0.05.
As shown in Table 2, ITN usage was also significantly related to settlement type ( p=0.0017). Patients from the urban area reported the highest ITN usage (32.3%; n=66/204), with patients from the peri-urban (29.2%; n=57/195) and rural areas (30.3%; n=61/202) reporting significantly lower percentages of usage. Malaria prevalence was similarly significantly related to settlement type ( p=0.0144). In this case, however, the highest malaria prevalence was recorded in rural patients (21.3%; n=43/202), followed by the peri-urban area (13.3%; n=26/195), with the urban centre recording the lowest prevalence (11.8%, n=24/204).
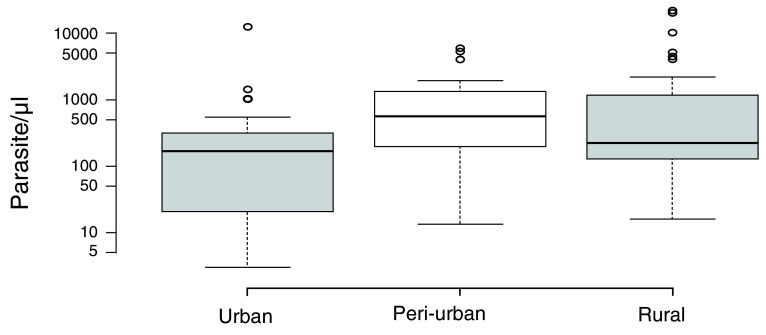
There was a significant difference in the parasite densities of infected patients across the three communities ( H=8.41; p=0.0149). Patients in the peri-urban area recorded the highest median parasite density (568; IQR=190–1312), followed by the rural area (224; IQR=126–1198), with the urban area recording the lowest median parasite density (167; IQR=20.5–311.5) ( Figure 1).
Figure 1. Parasite density across the three types of settlements.
Centre lines show the median counts; box limits indicate the 25th and 75th percentiles as determined by R software; whiskers extend 1.5 times the interquartile range from the 25th and 75th percentiles. Widths of boxes are proportional to square-roots of the number of observations, Urban=24, Peri-urban=26 and Rural=43 sample points. The Y-axis shows the estimated number of parasites per microlitre in blood in logarithmic scale. The results were considered significant if p ≤ 0.05.
Haematological indices differ significantly in patients from different areas
The median haematological parameter values of malaria-infected patients from the three study areas were compared using the Kruskal-Wallis test. The difference in median WBC (p<0.0001), neutrophil (p<0.0001) and lymphocyte (p<0.0269) counts were significantly different across the three communities and higher in infected patients from the peri-urban area compared to malaria patients from the rural and urban areas. Red blood cell indices such as MCV ( p=0.0006), RDW-SD ( p=0.0005) and RDW-CV ( p=0.0218) were significantly different across the three communities, with the lowest values recorded from malaria patients from the peri-urban area compared to those from the rural and urban areas. There were also significant differences in platelet ( p=0.0002), plateletcrit ( p=0.0041), mean platelet volume ( p=0.0009) and platelet large cell ratio ( p=0.0046) levels between patients from the urban, peri-urban and rural areas ( Table 3).
Table 3. Haematological parameter levels in infected patients from the three communities.
| Variable | Urban
Median (IQR) |
Peri-urban
Median (IQR) |
Rural
Median (IQR) |
P-value |
|---|---|---|---|---|
| Red blood cells (RBC) (×10 6 /µL) a | 4.16 (3.50 – 4.39) | 4.12 (3.81– 4.89) | 4.23 (3.72 – 4.67) | 0.3758 |
| Haemoglobin (g/dL) a | 10.60 (8.85–11.45) | 11.70 (10.30–12.90) | 11.10 (9.30–12.45) | 0.1455 |
| Hematocrit (%) a | 40.80 (33.20– 44.30) | 38.05 (34.40 – 41.60) | 41.40 (36.10–44.85) | 0.2797 |
| Mean corpuscular volume (MCV) (fL) a | 97.45 (90.20–103.5) | 90.35 (86.4–92.0) | 97.2 (90.25–103.0) | 0.0006 |
| Mean corpuscular haemoglobin (MCH)
(pg) b |
97.45 (90.20–103.15) | 90.35(86.40–92.20) | 97.20 (92.25–103.0) | 0.3488 |
| Red cell distribution width (RDW-SD) (fL) b | 55.95(50.20– 66.00) | 47.40 (44.80–51.30) | 50.90 (48.70–57.30) | 0.0005 |
| Red cell distribution width (RDW-CV) (%) b | 15.00(13.70–16.50) | 14.45(13.40–16.30) | 13.60(12.30–15.05) | 0.0218 |
| Platelet (×10 3/µL) b | 121.50 (87.0–87.0) | 195.50 (138.0–233.0) | 103 (55.0–170) | 0.0002 |
| Plateletcrit (PCT) (%) a | 0.12 (0.08– 0.17) | 0.24 (0.16– 0.28) | 0.12 (0.06– 0.18) | 0.0041 |
| Platelet distribution width (PDW) (fL) a | 16.00(13.70–19.80) | 15.95(14.60–19.40) | 17.60 (15.05–19.65) | 0.3497 |
| Mean platelet volume (MPV) (fL) a | 10.30 (9.45–11.15) | 12.00 (10.90–12.50) | 11.30 (9.90–12.15) | 0.0009 |
| Platelet large cell ratio (P-LCR) (%) a | 29.90 (24.15–38.75) | 41.55 (34.60–46.50) | 34.70 (29.90–41.95) | 0.0046 |
| White blood cells (WBC) (10 3/µL) b | 1.85 (1.35–3.60) | 4.70 (3.40–6.70) | 3.50 (2.35–5.20) | <0.0001 |
| Neutrophil (10 3/µL) b | 0.50 (0.30–1.30) | 2.20 (1.60–3.30) | 0.90 (0.50–1.55) | <0.0001 |
| Lymphocyte (10 3/µL) a | 0.90 (0.30–2.40) | 2.10 (1.40–2.80) | 2.00 (1.40–3.50) | 0.0269 |
aANOVA; bKruskall-Wallis test; IQR=Interquartile range
Anaemia and thrombocytopenia comprise two of the most common complications associated with malaria. Anaemia and acute anaemia are defined as having Hb levels <11g/dl or <5g/dl, respectively 12, while thrombocytopenia is defined as platelet count<150×10 3/μL 13. It was found that 48.4% ( n=45/93) of all malaria-infected patients in this study were anaemic compared to 33.3% ( n=164/492) of the control group ( p=0.0054), with two malaria-infected patients matching the criteria for acute anaemia. In addition, 58.1% ( n=54/93) of patients from the infected group were thrombocytopenic. We therefore tested the relationship between these two conditions and settlement type to determine if the occurrence of either anaemia or thrombocytopenia in malaria-infected patients was influenced by the type of settlement. The prevalence of thrombocytopenia was significantly influenced by the type of settlement ( p=0.0006), with malaria-infected patients in the urban area recording the highest prevalence. There was a strong relationship between anaemia and settlement type, although it was not statistically significant ( p=0.072). Similar to thrombocytopenia, the highest prevalence of anaemia was observed in patients from the urban area ( Table 4).
Table 4. Relationship between anaemia & thrombocytopenia and settlement type.
| Anaemia (%) | χ 2 | P-value | Thrombocytopenia (%) | χ 2 | P-value | |
|---|---|---|---|---|---|---|
| Settlement | ||||||
| Urban | 66.7 | 75.0 | ||||
| Peri-urban | 52.9 | 26.9 | ||||
| Rural | 46.5 | 5.25 | 0.072 | 67.4 | 14.74 | 0.0006 |
χ 2 is the chi-squared test statistic. The results were considered significant if p ≤ 0.05.
Discussion
We investigated haematological changes in malaria patients across three different demographic settlements: urban, peri-urban and rural communities. Consistent with findings from other studies 2, 6, 14, this study found significant differences in several red blood cell parameters between malaria-infected and non-malaria patients. Plasmodium falciparum, the parasite that causes the most severe form of malaria in humans, invades and multiplies inside red blood cells in a destructive cycle that is responsible for much of the severity and mortality associated with the disease 15, 16. Haemolytic mechanisms are usually employed by the host immune system to eliminate parasitized red blood cells in a process that may lead to anaemia 17, 18. Anaemia is considered to be one of the most common complications of malaria, especially in children and pregnant women 19. The present study revealed significantly lower Hb levels in the infected population compared to the uninfected group ( Table 1); however, a substantial proportion of the uninfected study participants also met the criteria for anaemia. The suspected anaemia cases observed in the control population may be due in part to poor nutritional status, undetectable malaria infection or, to a lesser extent, helminth infections 2. Peripheral leukocyte or WBC counts have been noted as being in the low to normal range during malaria, a phenomenon which is counterintuitive as one would expect increased production of WBCs during infection. The lack of increased numbers of circulating WBCs is believed to be due to the redistribution and sequestration of leukocytes in organs like the spleen, rather than actual depletion of the cell population 20. However, there are reports of both increased (leukocytosis) 4 and decreased (leucopenia) 2, 7 WBC levels in malaria-infected individuals. The present study did not observe any significant changes in the WBCs levels of patients with malaria compared to the uninfected group. One of the most striking results from the study was the low levels of platelet and plateletcrit (a measure of total platelet mass) observed in malaria-infected patients compared to uninfected patients, a finding that is consistent with results from other studies 6, 7, 13. This trend has been well recognized and consistently found in Plasmodium falciparum 4, 21 and Plasmodium vivax infections 22, 23. In this present study, 58.1% of malaria-infected patients were thrombocytopenic. There are several hypotheses about the reduction of platelets during malaria infection. This abnormality may be the result of blood clots developing in the bloodstream, thereby blocking small blood vessels. The intermittent clotting subsequently depletes the number of circulating platelets in the bloodstream 24. The reduction in platelet levels may also be attributable to an immune-mediated mechanism, whereby specific immunoglobulin G (IgG) produced as a result of the parasite invasion, forms a complex with parasite antigens. The resulting complex then binds to and damages platelets, with damaged platelets subsequently removed from circulation 24, 25.
By 2050, it is predicted that 58% of people in sub-Saharan Africa will be living in urban areas, compared with approximately 40% currently 26. This is expected to have a significant impact on the prevalence and clinical outcomes of infectious diseases like malaria as the increasing urban population further widens urban-rural economic and resource divides. In this study, patients from the rural area recorded the highest prevalence of malaria compared to patients from the urban and peri-urban areas, a finding that is consistent with results from other studies conducted in Ghana 14, 27. Rural areas are often described as intense and perennial transmission areas as there are often several suitable Anopheles breeding sites available, coupled with poor access and/or adherence to vector control measures by rural inhabitants 28, 29. The relatively younger age observed in the rural area may also be a contributing factor to the high prevalence observed in this study area, as children represent a high risk group for malaria infection 30. In line with this, the majority of infected individuals in the rural area were children less than five years. Children under five years may not have a fully developed immune system and are, therefore, more susceptible to infections. Adults, on the other hand, have relatively stronger immune systems and often have partial immunity to malaria from previous exposure 31. This might explain why the older generation recorded the lowest parasite densities. A comparison of haematological parameters of malaria-infected patients across the three areas revealed significant differences in the levels of key platelet and WBC indices, including plateletcrit, platelet, WBC, lymphocyte and neutrophil counts. Interestingly, higher levels of all the above blood indices were recorded in patients from the peri-urban area compared to those from the rural and urban areas, though the significance of this observation is unclear at present.
Observation of abnormal values of haematological parameters that are associated with malaria infection may prompt a more vigilant search for the parasite in routine microscopic diagnosis and could help avoid missing cases of malaria. Furthermore, differences in the haematological parameters of malaria patients can also serve as an auxiliary criterion for malaria diagnosis, especially in cases of low parasite density. With the increasing rates of urbanisation in Africa, it is more important than ever to better understand the impact of such socio-geographic and demographic changes on infectious diseases.
Data availability
Underlying data
Harvard Dataverse: Replication Data for: Impact of malaria on haematological parameters of urban, peri-urban and rural patients in the Ashanti region of Ghana. https://doi.org/10.7910/DVN/NGBMZM 11
This project contains the following underlying data:
-
-
Combined data.xlsx (raw demographic, haematological and parasitological data for all participants)
-
-
Combined Data_Age.tab (raw demographic, haematological and parasitological data for all participants, including ages)
-
-
Malaria Infected population.xlsx (raw demographic, haematological and parasitological data for malaria infected participants)
-
-
Malaria Uninfected.xlsx (raw demographic, haematological and parasitological data for uninfected participants)
-
-
Peri-Urban population.xlsx (raw demographic, haematological and parasitological data for participants in the peri-urban area)
-
-
Rural population.xlsx (raw demographic, haematological and parasitological data for participants in the rural area)
-
-
Urban population.xlsx (raw demographic, haematological and parasitological data for participants in the urban area)
-
-
Data Dictionary.xlsx
Extended data
Harvard Dataverse: Replication Data for: Impact of malaria on haematological parameters of urban, peri-urban and rural patients in the Ashanti region of Ghana. https://doi.org/10.7910/DVN/NGBMZM 11
This project contains the following extended data:
-
-
CHRPE Participant Information Leaflet_Malaria.pdf
-
-
Questionnaire- Malaria.pdf
Data are available under the terms of the Creative Commons Zero "No rights reserved" data waiver (CC0 1.0 Public domain dedication).
Acknowledgements
We are grateful to the Kumasi South, Kuntanase and the Agona district hospitals for their support during data collection. We are also grateful to the KNUST Graduate Assistantship programme which supported AHM and SKA. KB, the corresponding author, is an AAS affiliate (2017–2022).
Funding Statement
AHM and SKA received graduate assistantship from the KNUST College of Science. KB received funds for laboratory supplies from the Africa Research Excellence Fund (AREF) Research Development Fellowship [MRF-157-0007-F-BADU]. Kingsley Badu is an Affiliate of the African Academy of Sciences.
[version 1; peer review: 1 approved with reservations, 1 not approved]
References
- 1. World Health Organization: World malaria report 2018. World Health Organization;2018. Reference Source [Google Scholar]
- 2. Maina RN, Walsh D, Gaddy C, et al. : Impact of Plasmodium falciparum infection on haematological parameters in children living in Western Kenya. Malar J. 2010;9 Suppl 3:S4. 10.1186/1475-2875-9-S3-S4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Waitumbi JN, Opollo MO, Muga RO, et al. : Red cell surface changes and erythrophagocytosis in children with severe plasmodium falciparum anemia. Blood. 2000;95(4):1481–1486. [PubMed] [Google Scholar]
- 4. Erhart LM, Yingyuen K, Chuanak N, et al. : Hematologic and clinical indices of malaria in a semi-immune population of western Thailand. Am J Trop Med Hyg. 2004;70(1):8–14. [PubMed] [Google Scholar]
- 5. Bakhubaira S: Hematological Parameters in Severe Complicated Plasmodium falciparum Malaria among Adults in Aden. Turk J Haematol. 2013;30(4):394–399. 10.4274/Tjh.2012.0086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kotepui M, Phunphuech B, Phiwklam N, et al. : Effect of malarial infection on haematological parameters in population near Thailand-Myanmar border. Malar J. 2014;13:218. 10.1186/1475-2875-13-218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ladhani S, Lowe B, Cole AO, et al. : Changes in white blood cells and platelets in children with falciparum malaria: relationship to disease outcome. Br J Haematol. 2002;119(3):839–847. 10.1046/j.1365-2141.2002.03904.x [DOI] [PubMed] [Google Scholar]
- 8. Kotepui M, Piwkham D, PhunPhuech B, et al. : Effects of malaria parasite density on blood cell parameters. PLoS One. 2015;10(3):e0121057. 10.1371/journal.pone.0121057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Anabire NG, Aryee PA, Helegbe GK: Hematological abnormalities in patients with malaria and typhoid in Tamale Metropolis of Ghana. BMC Res Notes. 2018;11(1):353. 10.1186/s13104-018-3456-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Paintsil EK, Omari-Sasu AY, Addo MG, et al. : Analysis of Haematological Parameters as Predictors of Malaria Infection Using a Logistic Regression Model: A Case Study of a Hospital in the Ashanti Region of Ghana. Malar Res Treat.hindawi.com;2019; 1486370. 10.1155/2019/1486370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Badu K: Replication Data for: Impact of malaria on haematological parameters of urban, peri-urban and rural patients in the Ashanti region of Ghana.Harvard Dataverse, V1.2019. 10.7910/DVN/NGBMZM [DOI] [PMC free article] [PubMed]
- 12. World Health Organization: Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity [Internet]. World Health Organization;2011. Report No.: WHO/NMH/NHD/MNM/11.1. Reference Source [Google Scholar]
- 13. Lacerda MV, Mourão MP, Coelho HC, et al. : Thrombocytopenia in malaria: who cares? Mem Inst Oswaldo Cruz. 2011;106 Suppl 1:52–63. 10.1590/s0074-02762011000900007 [DOI] [PubMed] [Google Scholar]
- 14. Iqbal SA, Botchway F, Badu K, et al. : Hematological Differences among Malaria Patients in Rural and Urban Ghana. J Trop Pediatr. 2016;62(6):477–486. 10.1093/tropej/fmw038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mkumbaye SI, Wang CW, Lyimo E, et al. : The Severity of Plasmodium falciparum Infection Is Associated with Transcript Levels of var Genes Encoding Endothelial Protein C Receptor-Binding P. falciparum Erythrocyte Membrane Protein 1. Infect Immun. 2017;85(4): pii: e00841-16. 10.1128/IAI.00841-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Haldar K, Mohandas N: Malaria, erythrocytic infection, and anemia. Hematology Am Soc Hematol Educ Program. 2009;87–93. 10.1182/asheducation-2009.1.87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Weatherall DJ, Miller LH, Baruch DI, et al. : Malaria and the red cell. Hematology Am Soc Hematol Educ Program. 2002;35–57. 10.1182/asheducation-2002.1.35 [DOI] [PubMed] [Google Scholar]
- 18. Price RN, Simpson JA, Nosten F, et al. : Factors contributing to anemia after uncomplicated falciparum malaria. Am J Trop Med Hyg. 2001;65(5):614–622. 10.4269/ajtmh.2001.65.614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Menendez C, Fleming AF, Alonso PL: Malaria-related anaemia. Parasitol Today. 2000;16(11):469–476. 10.1016/S0169-4758(00)01774-9 [DOI] [PubMed] [Google Scholar]
- 20. McKenzie FE, Prudhomme WA, Magill AJ, et al. : White blood cell counts and malaria. J Infect Dis. 2005;192(2):323–330. 10.1086/431152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wickramasinghe SN, Abdalla SH: Blood and bone marrow changes in malaria. Baillieres Best Pract Res Clin Haematol. 2000;13(2): 277–299. 10.1053/beha.1999.0072 [DOI] [PubMed] [Google Scholar]
- 22. Oh MD, Shin H, Shin D, et al. : Clinical features of vivax malaria. Am J Trop Med Hyg. 2001;65(2):143–146. 10.4269/ajtmh.2001.65.143 [DOI] [PubMed] [Google Scholar]
- 23. Lee HK, Lim J, Kim M, et al. : Immunological alterations associated with Plasmodium vivax malaria in South Korea. Ann Trop Med Parasitol. 2001;95(1):31–39. 10.1080/00034980020035898 [DOI] [PubMed] [Google Scholar]
- 24. Essien EM: The circulating platelet in acute malaria infection. Br J Haematol. 1989;72(4):589–590. 10.1111/j.1365-2141.1989.tb04329.x [DOI] [PubMed] [Google Scholar]
- 25. Moulin F, Lesage F, Legros AH, et al. : Thrombocytopenia and Plasmodium falciparum malaria in children with different exposures. Arch Dis Child. 2003;88(6):540–541. 10.1136/adc.88.6.540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. United Nations, Department of Economic and Social Affairs, Population Division: World Urbanization Prospects: The 2018 Revision [Internet].2018[cited 27 May 2018]. Reference Source [Google Scholar]
- 27. Ronald LA, Kenny SL, Klinkenberg E, et al. : Malaria and anaemia among children in two communities of Kumasi, Ghana: a cross-sectional survey. Malar J. 2006;5:105. 10.1186/1475-2875-5-105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Molina Gómez K, Caicedo MA, Gaitán A, et al. : Characterizing the malaria rural-to-urban transmission interface: The importance of reactive case detection. PLoS Negl Trop Dis. 2017;11(7):e0005780. 10.1371/journal.pntd.0005780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Trape JF, Zoulani A: Malaria and urbanization in central Africa: the example of Brazzaville. Part II: Results of entomological surveys and epidemiological analysis. Trans R Soc Trop Med Hyg. 1987;81 Suppl 2:10–18. 10.1016/0035-9203(87)90472-x [DOI] [PubMed] [Google Scholar]
- 30. Vorasan N, Pan-Ngum W, Jittamala P, et al. : Long-term impact of childhood malaria infection on school performance among school children in a malaria endemic area along the Thai--Myanmar border. Malar J.BioMed Central;2015;14:401 10.1186/s12936-015-0917-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Weng NP: Aging of the immune system: how much can the adaptive immune system adapt? Immunity. 2006;24(5):495–499. 10.1016/j.immuni.2006.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]